Vaccines to get before pregnancy
Vaccine Safety for Moms-to-Be | CDC
Pregnant women may safely receive inactivated vaccines (Tdap and flu), mRNA (Moderna and Pfizer), and viral vector vaccines (J&J).
Vaccines help protect pregnant people and babies against serious diseases
Pregnant people share everything with their babies. That means when a pregnant person gets vaccines, she isn’t just protecting herself— they are giving the baby some early protection too.
CDC has recommendations for the vaccines needed before, during, and after pregnancy. Currently, CDC routinely recommends Tdap and flu shots during pregnancy.
- Get the Tdap vaccine (to help protect against whooping cough), during pregnancy.
- The flu shot can be given before or during pregnancy, depending on whether or not it is flu season during a pregnancy.
- It is safe for pregnant people to receive vaccines right after giving birth, even while breastfeeding.
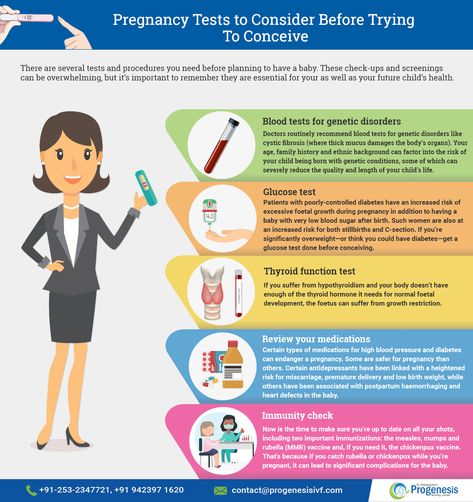
- Some vaccines, such as the measles, mumps, rubella (MMR) vaccine, should be given a month or more before pregnancy if a pregnant person didn’t get the vaccine as a child.
Live virus vaccines, such as the MMR and chickenpox, should not be given to pregnant people, but should be given to them before or after pregnancy, if indicated. Talk to your doctor about the MMR, Tdap, and flu vaccines before getting vaccinated. The COVID-19 vaccine is also recommended for pregnant people. The authorized and recommended COVID-19 vaccines for pregnant people are the mRNA Moderna and Pfizer-BioNTech vaccines, which contain no live virus, and the J&J/Janssen viral vector vaccine, meaning it uses a modified version of a different virus (the vector) to deliver important instructions to our cells. If you have any questions about these vaccines, talk to your doctor.
Vaccine safety before, during, and after pregnancy
It’s important to know that the Tdap and flu vaccines are safe for a pregnant person and their baby. Likewise, the limited information collected for COVID-19 vaccines given to pregnant people have not identified any safety concerns for them or their babies.
Likewise, the limited information collected for COVID-19 vaccines given to pregnant people have not identified any safety concerns for them or their babies.
- The Tdap and flu vaccines are inactivated vaccines, which means they are made by inactivating or killing the germ during the process of making the vaccine.
- Studies done on the Tdap vaccine have concluded that it is safe and effective for pregnant people and babies.
- Similarly, results from multiple studies on the flu shot continue to support the safety and effectiveness of the vaccine during pregnancy.
- There is limited information available about the safety of the COVID-19 vaccines for people who are pregnant; however, based on how these vaccines work in the body, experts believe they are unlikely to pose risk for pregnant people.
It is important to get MMR before becoming pregnant to reduce the risk of becoming infected with rubella which can pass on to the unborn child, causing Congenital Rubella Syndrome (CRS). CRS can cause severe birth defects and neurodevelopmental problems. Even though MMR is a safe and effective vaccine, there is a theoretical risk to the baby. This is because it is a live vaccine, meaning it contains a weakened version of the living viruses.
CRS can cause severe birth defects and neurodevelopmental problems. Even though MMR is a safe and effective vaccine, there is a theoretical risk to the baby. This is because it is a live vaccine, meaning it contains a weakened version of the living viruses.
- Live vaccines are generally not recommended during pregnancy.
- If a pregnant person did not get MMR as a child, she should get the vaccine before pregnancy.
All vaccines are held to the highest standards of safety—meaning they are carefully studied and monitored for side effects. Vaccines are like any medicine, which means they can have some side effects. However, most people who get vaccinated have no side effects or only mild side effects. CDC continually monitors vaccine safety, and the most common side effects seen are mild and go away quickly on their own (redness, swelling, and tenderness at the site where the shot was given. Other possible side effects associated with the COVID-19 vaccine are tiredness, headache, muscle pain, chills, fever, and nausea.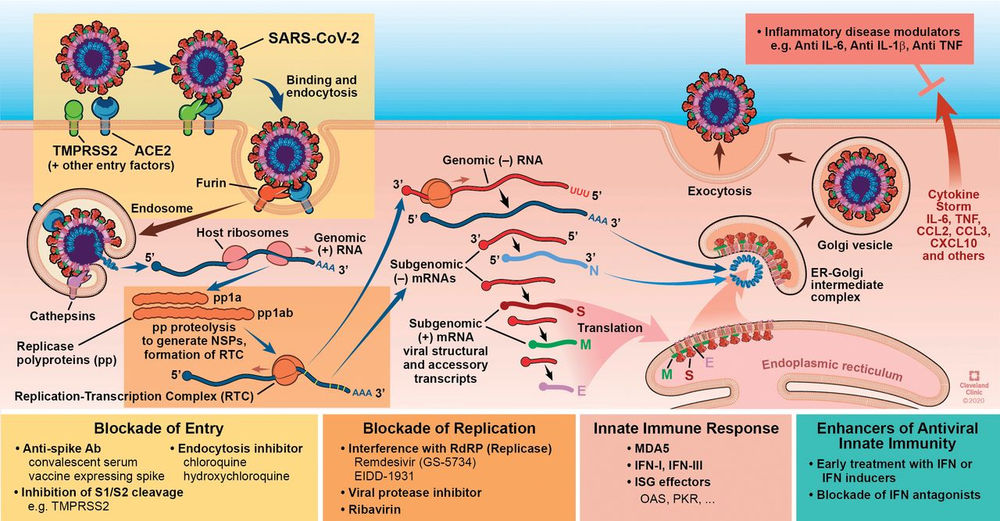 ).
).
For more studies, the FDA also has a pregnancy exposure registry,external icon which is a study that collects health information from pregnant persons who take medicines or vaccines when they are pregnant.
Vaccines for women: Before conception, during pregnancy, and after a birth
The rise of vaccine-preventable illnesses, such as measles and hepatitis, in the United States and around the globe has been alarming in recent years. For women — especially those hoping to become pregnant, as well as women who are pregnant or have recently had a baby — vaccines can be a worrisome topic. There are many misconceptions about vaccine safety in and around pregnancy that can lead to confusion and unnecessary fear of a lifesaving medical tool. As a practicing ob/gyn, I often discuss vaccines with my patients and help them sort out fears versus facts.
Which vaccines should you consider before conception?
The preconception period offers a unique opportunity to find your immunization records and review them with your primary care provider. Some vaccines should be considered for all women who are hoping to conceive. Others are recommended based on additional medical issues.
Some vaccines should be considered for all women who are hoping to conceive. Others are recommended based on additional medical issues.
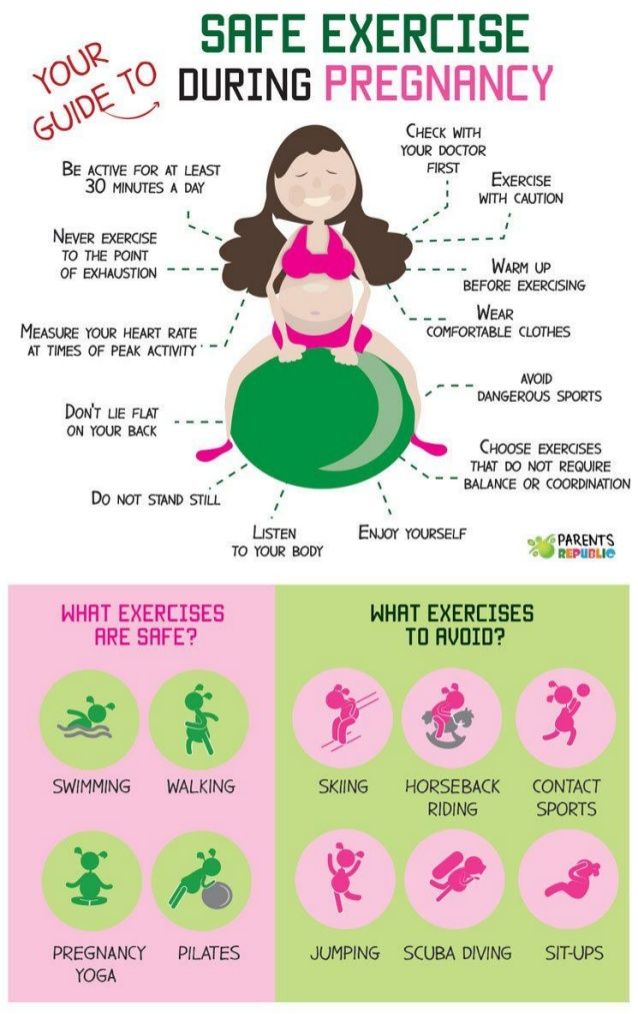
Influenza: Getting your flu shot in anticipation of pregnancy will help protect you during flu season. Flu shots are generally available each year from late August through March, to correspond with the influenza season (though timing may vary by region). You can get a flu shot at your doctor’s office or at many pharmacies. If you could be pregnant, ask for the inactivated influenza vaccine. The nasally administered live vaccine (LAIV, Flumist) is not recommended for women who may be pregnant, although children in your home can safely have this version of the vaccine.
Measles, mumps, and rubella (MMR): Given the ongoing global measles outbreak, the Centers for Disease Control and Prevention (CDC) and American College of Obstetrics and Gynecology (ACOG) recommend assessing measles immunity before a woman becomes pregnant. Your doctor can review your immunization record with you and determine if you have had an adequate number of MMR vaccines. If not, or if you cannot find your immunization record, your doctor can order a blood test to evaluate your immunity and give you a booster shot if needed.
Your doctor can review your immunization record with you and determine if you have had an adequate number of MMR vaccines. If not, or if you cannot find your immunization record, your doctor can order a blood test to evaluate your immunity and give you a booster shot if needed.
The MMR booster shot is a live-attenuated (weakened) virus vaccine. After a woman receives it, the CDC recommends waiting four weeks before attempting pregnancy because of theoretical risks to the fetus with live vaccines. However, if a pregnancy occurs within the four-week window, do not worry! This recommendation is based on theoretical risks. In fact, there have been no reports of harm to a fetus due to this type of exposure.
Varicella zoster virus (VZV): Many women of childbearing age have either had chickenpox (varicella) or received the vaccine during childhood. Because chickenpox can harm a pregnant woman and her fetus, assessing your immunity to chickenpox is a good idea before conceiving.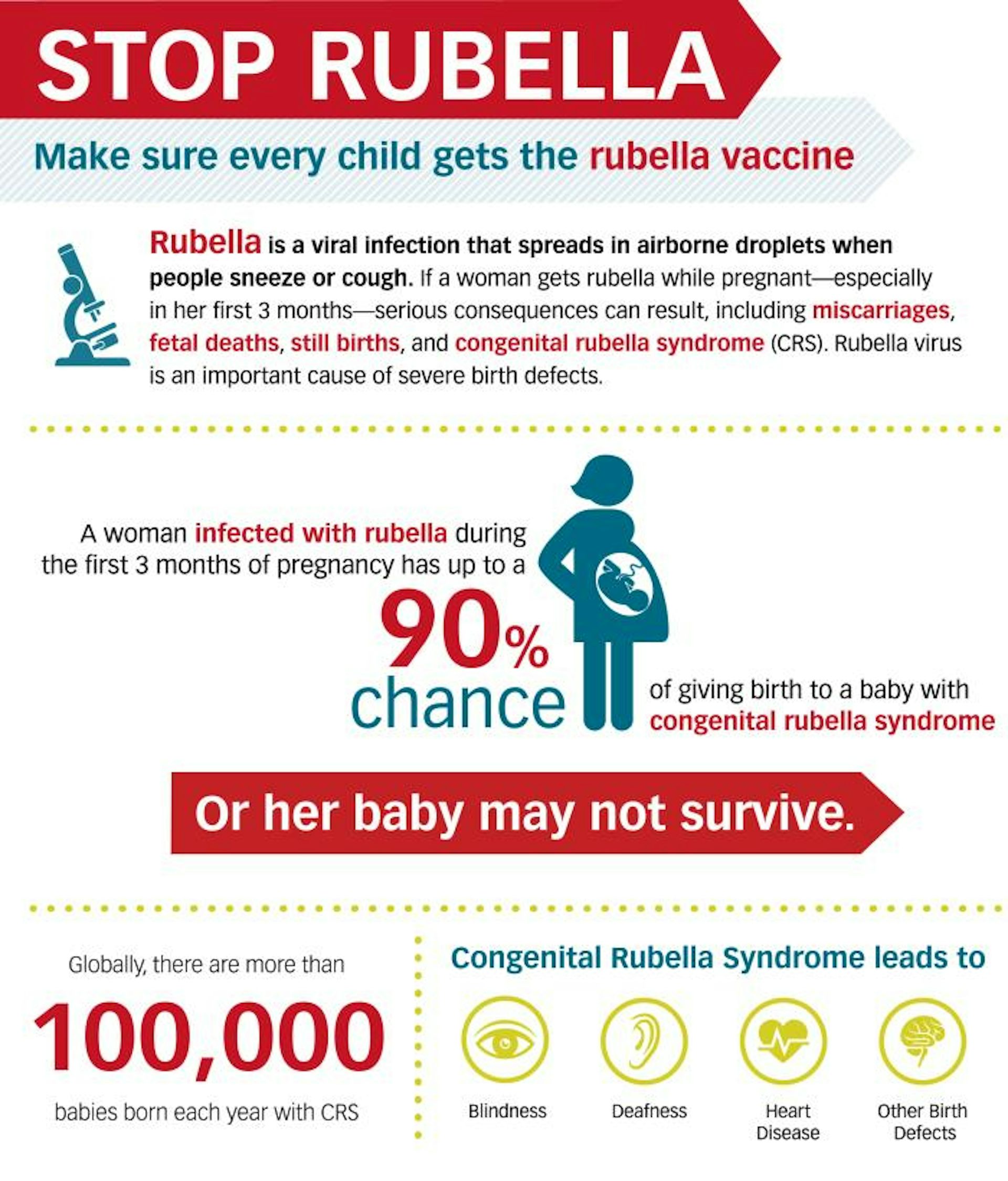 If you’re not immune, this is a good time to have the vaccine. Similar to the MMR booster, the VZV vaccine is a live-attenuated virus vaccine. A woman should have this vaccine at least four weeks before attempting to conceive, due to the theoretical concern for fetal exposure.
If you’re not immune, this is a good time to have the vaccine. Similar to the MMR booster, the VZV vaccine is a live-attenuated virus vaccine. A woman should have this vaccine at least four weeks before attempting to conceive, due to the theoretical concern for fetal exposure.
Human papillomavirus (HPV): This vaccine helps prevent new HPV infections and HPV-associated diseases, including cervical cancer. It is recommended for teens and people through age 26, but those ages 27 through 45 years may also benefit. Discuss this with your doctor. While the HPV vaccine is not recommended during pregnancy, inadvertently getting it during pregnancy is not associated with harm for you or your baby.
Additional vaccines to consider: Your doctor can tell you whether it’s especially important for you to consider the hepatitis A, hepatitis B, and pneumococcal vaccines based on health issues, lifestyle, or travel plans that could put you at higher risk.
Which vaccines should you have during pregnancy?
During every pregnancy, the ACOG recommends:
- An influenza vaccine during flu season. This can protect women from severe medical and obstetrical complications, and provide protection for babies during early infancy. It can be safely given any time during pregnancy.
- A tetanus, diphtheria, and pertussis (Tdap) vaccine, given during the third trimester. This protects against pertussis (whooping cough) in pregnant women who might pass it to their babies during delivery, and also protects babies during early infancy when pertussis can be life-threatening. Additionally, Tdap is recommended for anyone who has not received the vaccine and will be in close contact with infants less than a year old, such as grandparents or childcare providers.
Additional vaccines to consider: Hepatitis A, Hepatitis B, and pneumococcal vaccines are recommended if you have certain risk factors, or are midway through a vaccine series that was started before you conceived.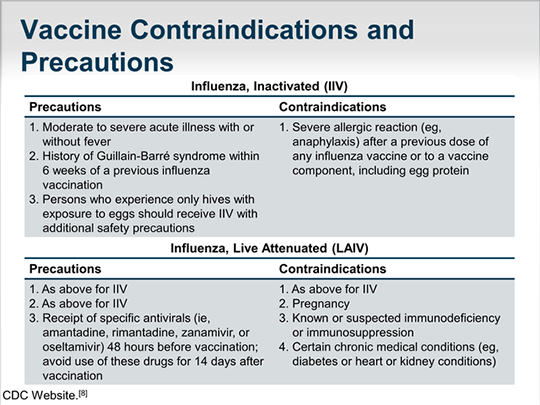 Ask your doctor about whether you would benefit from any of these vaccines.
Ask your doctor about whether you would benefit from any of these vaccines.
What about vaccines after a birth or if you’re breastfeeding?
If your doctor told you during your pregnancy that you did not have immunity to rubella, measles, or chickenpox, you should receive these vaccines to help protect yourself and your baby. There is no concern about breastfeeding.
If you haven’t had the HPV vaccine, you should start the series if
- you are 26 or younger
- you are over 26 and at risk for HPV exposure.
Finally, ask your doctor if you should consider having hepatitis A, hepatitis B, and pneumococcal vaccines. These are recommended for women with certain risk factors.
What are some myths about vaccines?
Social media and well-meaning friends may spread misconceptions about vaccine safety and efficacy. Below are the most common myths.
- The flu shot makes me sick.
 While some patients may feel achy or fatigued after the flu shot, this is a sign that your immune system is working in response to the vaccine. Because the flu vaccine is made from a killed virus, you can’t get the flu from the vaccine.
While some patients may feel achy or fatigued after the flu shot, this is a sign that your immune system is working in response to the vaccine. Because the flu vaccine is made from a killed virus, you can’t get the flu from the vaccine. - I’m young and healthy, so I never get the flu shot. Even healthy pregnant women can become severely ill and die from influenza infection.
- Vaccines cause autism. Many studies have been conducted reviewing mercury (thimerosal), vaccines, and autism. No study has ever shown a positive relationship between vaccines, mercury, and subsequent autism diagnosis.
- Vaccines pose a risk to my unborn baby. Vaccines recommended in pregnancy have proven to be safe in all trimesters. Since 2004 the CDC and ACOG have recommended vaccinations such as influenza during any trimester.
- Vaccines in the first trimester will cause miscarriage.
 Vaccines such as influenza have been given to millions of pregnant women over decades. No relationship has been shown between influenza vaccination and birth defects and miscarriage.
Vaccines such as influenza have been given to millions of pregnant women over decades. No relationship has been shown between influenza vaccination and birth defects and miscarriage. - I can get my Tdap after the birth. This will not effectively protect your newborn from pertussis. Vaccination during pregnancy gives newborns passive immunity, which protects them from pertussis until they are able to get their vaccination at 2 months.
Vaccination during pregnancy planning - health articles
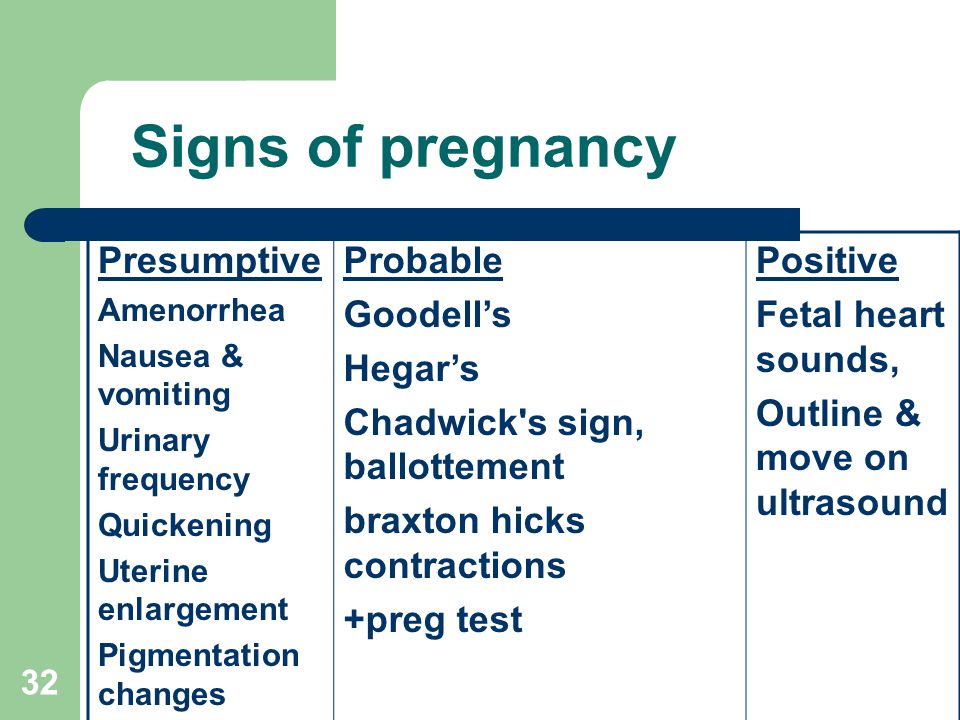
Pregnancy planning is an important stage in the life of any person. During this period, it is very important for a woman to pass a number of tests and undergo some examinations. Immunization is desirable. At the moment, it is carried out in order to prevent infection with measles, rubella and influenza. Even if a pregnant woman gets sick, the disease will be mild.
Vaccination against coronavirus is also important when planning pregnancy.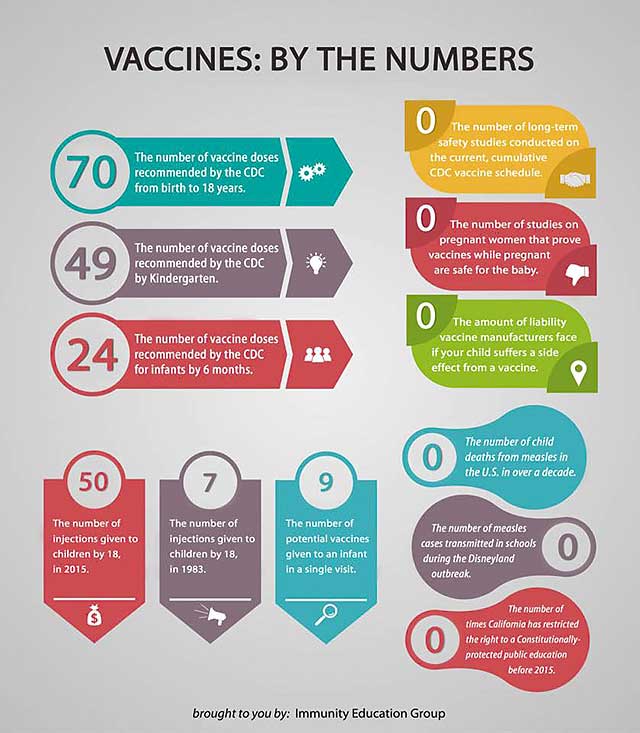 This is due to the fact that women who are expecting a baby are at risk for the severe course of the pathology and the development of its complications. nine0003
This is due to the fact that women who are expecting a baby are at risk for the severe course of the pathology and the development of its complications. nine0003
Consider all aspects of vaccination.
Is vaccination necessary during pregnancy?
We have already figured out what you need! Immunization is recommended by international organizations working in the field of health. Moreover, the vaccine can be delivered already during pregnancy (from the 22nd week). At the same time, there is no scientific evidence confirming that earlier dates are not recommended for immunization.
Can vaccination against COVID-19be combined at the stage of pregnancy planning with other vaccinations?
Yes! Drugs can be administered in one period. There must be 14 days between vaccinations. Therefore, a woman can quickly protect herself from influenza, whooping cough and a number of other diseases.
Should there be some time between vaccination and pregnancy planning (including with the use of assisted reproductive technologies (ART))?
Natural conception or entry into ART programs is not allowed between the introduction of the first and second component of two-component drugs.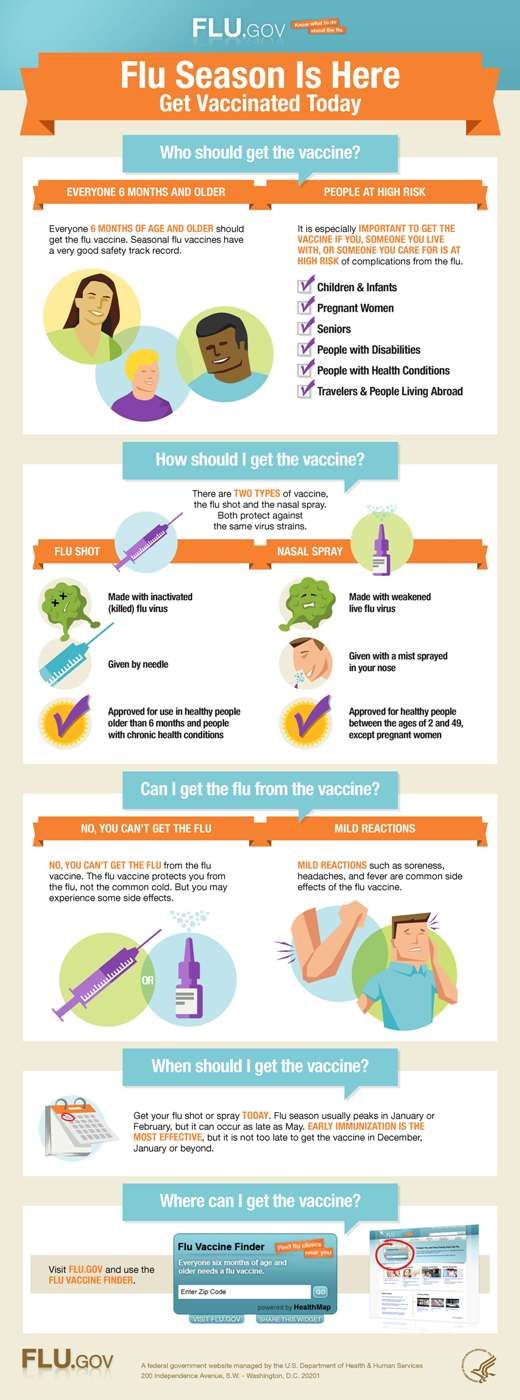 After the vaccination, 2-3 weeks should pass. This is due to the period of a possible acute immune response to the vaccine. In addition, a natural immune response should form. The date of entry into assisted reproductive technology programs is determined on an individual basis. It is advisable for a woman to consult a doctor. nine0003
After the vaccination, 2-3 weeks should pass. This is due to the period of a possible acute immune response to the vaccine. In addition, a natural immune response should form. The date of entry into assisted reproductive technology programs is determined on an individual basis. It is advisable for a woman to consult a doctor. nine0003
As for men, it is possible to donate sperm for IVF or start natural conception already after 3-5 days (including after the first vaccination when using two-component preparations). At the same time, it should be understood that the effect of vaccines on spermatogenesis has not yet been precisely established. If a man is worried about the quality of germ cells, it is recommended to consult a doctor.
If necessary, cryopreservation of oocytes or spermatozoa prior to vaccination can also be used. This procedure does not affect the quality of germ cells. At the same time, it allows you to quickly eliminate any existing doubts. nine0003
If the vaccine is not given in preparation for pregnancy, is it possible to administer the drug during pregnancy?
Relatively recently, the Ministry of Health changed the previously up-to-date instructions for the use of Sputnik V. The vaccine was allowed to be used for immunization of pregnant women. In this case, a consultation with a gynecologist is required. It will determine whether the expected benefit of the vaccine to the mother outweighs the potential risks to the baby. When is the best time to vaccinate? So far, the period has been set from the 22nd week of gestation. Perhaps it will change in the future, and it will be possible to vaccinate earlier. nine0003
The vaccine was allowed to be used for immunization of pregnant women. In this case, a consultation with a gynecologist is required. It will determine whether the expected benefit of the vaccine to the mother outweighs the potential risks to the baby. When is the best time to vaccinate? So far, the period has been set from the 22nd week of gestation. Perhaps it will change in the future, and it will be possible to vaccinate earlier. nine0003
Are there possible side effects after vaccination during pregnancy planning?
Some mistakenly believe that modern drugs can cause infertility. Such claims are not substantiated and are not supported by scientific evidence. Vaccination does not affect the planning of pregnancy and does not affect the fertility (ability to conceive) of men and women. It does not complicate the course of the process and does not contribute to the disruption of the menstrual cycle. nine0003
No relationship has been established between pregnancy loss and vaccinations.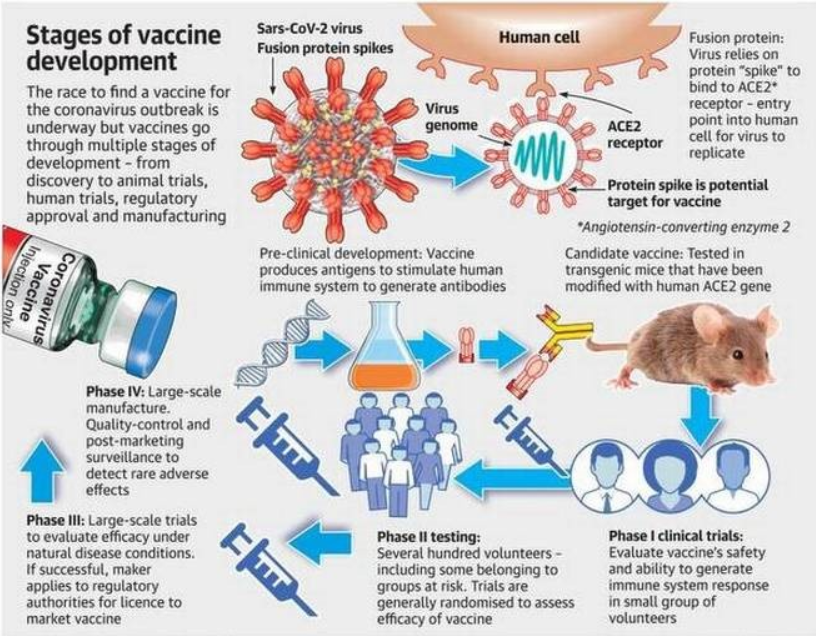 At the same time, the threat of miscarriage increases when infected with a coronavirus infection, especially in cases of a severe course of the disease.
At the same time, the threat of miscarriage increases when infected with a coronavirus infection, especially in cases of a severe course of the disease.
Important! It should be remembered that vaccination, both by itself and at the stage of pregnancy planning, can cause a deterioration in well-being. Typically, patients complain of a slight fever, aching joints, headache, redness of the mucous membranes of the eyes, and other minor symptoms of standard colds. nine0003
Benefits of contacting MEDSI
- Experienced professionals. Vaccination is carried out by paramedical personnel (nurses) with the necessary knowledge and skills
- Diagnostic options. Before vaccination, you can perform a rapid test for the coronavirus antigen (smear) or a PCR study to detect the virus RNA (smear), as well as a study of the level of IgG antibodies to the spike protein of the SARs CoV-2 virus
- Possibilities for the introduction of two drugs. Immunization can be carried out with Sputnik V, Sputnik Light and Kovivak vaccines
- Obligatory preliminary medical consultation.
 He will talk about the possibilities of planning pregnancy after vaccination, identify indications for vaccination and possible contraindications
He will talk about the possibilities of planning pregnancy after vaccination, identify indications for vaccination and possible contraindications - Immunization Preparation Program. It includes a doctor's examination before the administration of each vaccine component, a rapid test for COVID-19, vaccination (1-2 doses) and 2 telemedicine consultations in the SmartMed app
- Comfortable conditions for the procedure. Vaccination is carried out without queues and long waiting times on a convenient day. To undergo the procedure, each patient can choose the nearest clinic
- Transfer of vaccination data and their availability on the State Services portal. Our specialists provide data transfer to a special register to receive QR code
To clarify the conditions of vaccination or sign up for a vaccination, just call +7 (495) 7-800-500. Our specialist will answer all questions. Recording is also possible through the SmartMed application.
Planning a pregnancy - vaccinations - EMC
Vaccination of women in preparation for a planned pregnancy
Often women have a question whether it is necessary to vaccinate before and during pregnancy, against which infections and how to do it correctly.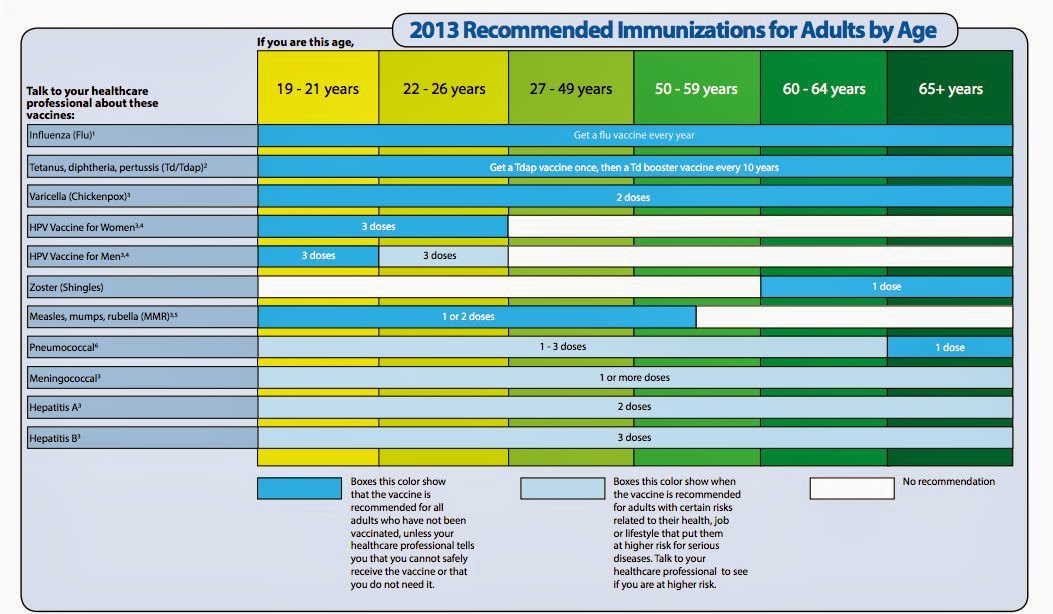
Vaccination in preparation for pregnancy is due to the need to create an immune barrier against infections. What gives the prevention of primary infection of the pregnant woman and the fetus, and the complications associated with this.
From the point of view of the immune system, pregnancy is a serious shock. During pregnancy, all organs and systems work differently, which also affects the immune system. Pregnancy is a condition that can lead to a significant decrease in immunity. nine0003
It is important to vaccinate before pregnancy against the following infections: rubella, viral hepatitis B, poliomyelitis, diphtheria, tetanus, influenza
Rubella
barrier. Among them, rubella is especially dangerous. The consequence of the disease of a pregnant woman who does not have immunity, with a 75–95% probability, is congenital malformations in the fetus. Congenital rubella is responsible for about 20% of malformations and occurs in more than 2 per 1000 live births. nine0003
nine0003 If the woman has not had rubella, the vaccine must be given at least 2 months before the planned pregnancy. You can check the presence of immunity to rubella by immunological methods.
All current rubella vaccines are 95-100% effective. Immunity after vaccination lasts more than 20 years. The vaccine contains a live virus, the vaccination course consists of only one vaccination, i.e. immunity is formed immediately. Another positive effect of vaccination is the transfer of antibodies against rubella from mother's milk to the unborn child. nine0003
In no case should the rubella vaccine be given during pregnancy due to the theoretical, but still, possibility of damage to the fetus by the vaccine virus.
NB! For at least 2 months. after vaccination against rubella, it is necessary to protect yourself!
Viral hepatitis B
Strictly speaking, vaccination against viral hepatitis B is necessary for everyone. The hepatitis B virus does not have the ability to damage the fetus, like the rubella virus.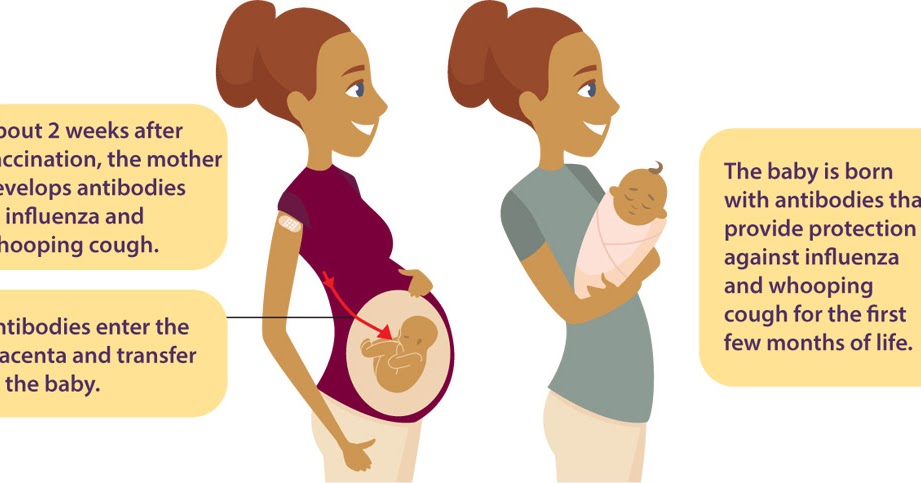
The hepatitis B virus is transmitted through blood and other bodily fluids. All pregnant women are subjected to injections, examinations, manipulations. Childbirth and potential transfusions of blood and blood products also pose an additional risk of possible infection with the hepatitis B virus.
The standard hepatitis B vaccination schedule is 0 – 1 – 6 months, i.e. selected day (0) - in a month (1) - in 6 months. (3) after the first vaccination. Ideally, it is better to start vaccination in such a way as to have time to do all three vaccinations before the start of pregnancy - i.e. for 6 months. nine0003
However, when preparing for a planned pregnancy in practice (unfortunately, rarely does anyone think about vaccinations six months before pregnancy), this scheme will most likely look like: the selected day (0) - in a month (1) - in 6 - 12 months. (3) after the first. In other words, two vaccinations 1 month apart. provide immunity lasting up to 1 year, the third vaccination (done after childbirth) forms immunity lasting more than 15 years (modern vaccines have been used only since 1986, so the full duration of immunity has not been clarified). nine0003
nine0003
The hepatitis B vaccine is a pure "Australian antigen", that is, only a part, or rather only one of the proteins of the virus. The effectiveness of vaccination in adults is on average 85-90%, adverse reactions are insignificant (a slight increase in temperature is possible in about 2% of those vaccinated and mild soreness at the injection site) in 5-10% of those who received the vaccine.
Poliomyelitis
The risk of contracting naturally circulating poliomyelitis both in Europe and in Russia is negligible - the last time a "wild" polio virus was seen in the central regions of the Russian Federation was 10-15 years ago. But there is a more than real risk of contracting a live vaccine virus, since children in the country are receiving OPV, a live virus vaccine, without exception, in order to eradicate polio. nine0003
In many countries, vaccination (booster) with inactivated polio vaccine (IPV) is recommended before pregnancy. One vaccination is enough to "remind" the immune system of the existence of the virus.
Diphtheria, tetanus
Diphtheria and tetanus vaccination is needed if the next vaccination is due or if you missed the previous vaccination. According to the calendar, vaccination against diphtheria and tetanus is done every 10 years after vaccination at 16 years old, that is, at 26 years old, 36 years old, etc. up to 60 years old. nine0% of adults do not remember and do not know about it. The vaccine is needed, first of all, for the unborn child, who needs to be protected from such a pathology as neonatal tetanus, an absolutely fatal infection. The child does not have its own antibodies to tetanus bacillus, and the mother's, transmitted with milk in the first days of feeding, will render the baby an invaluable service.
Influenza
Pregnant women whose 2nd - 3rd trimester coincides with an influenza epidemic should preferably be vaccinated against influenza 2 - 3 months before the epidemic. These recommendations are based on evidence of a higher susceptibility of pregnant women to severe influenza complications. In addition, vaccination is especially strongly recommended for pregnant women (as well as other adults and children) with chronic diseases. nine0003
In addition, vaccination is especially strongly recommended for pregnant women (as well as other adults and children) with chronic diseases. nine0003
It is best to get vaccinated against influenza before the planned pregnancy, if updated vaccines are available at that time (usually they appear in September), to protect in the current epidemic season. Modern inactivated influenza vaccines belonging to the classes of split (split-) and subunit drugs are not contraindicated and are even recommended for use during pregnancy.
Pre-pregnancy Immunization Schedule
| Months before planned pregnancy | Vaccination |
| 3 months | hepatitis B*(1), rubella |
| 2 months | hepatitis B(2), poliomyelitis (IPV) |
| 1 month | diphtheria-tetanus (ADS-M**), influenza*** |
| 1 month postpartum | hepatitis B (3) |
* - if it is not possible to start a hepatitis B vaccination course (see below) 6 months in advance.