How long is the third trimester of pregnancy
Third trimester | Pregnancy Birth and Baby
Third trimester | Pregnancy Birth and Baby beginning of content5-minute read
Listen
Once you reach the third trimester of pregnancy, you’re well over half way there. As you look forward to the birth of your baby, there is plenty to plan for and decisions to make. You might find you’re slowing down, or you might be filled with energy to clean, tidy and organise as you prepare for your baby’s arrival. This urge to clean is known as the ‘nesting’ instinct.
What is the third trimester?
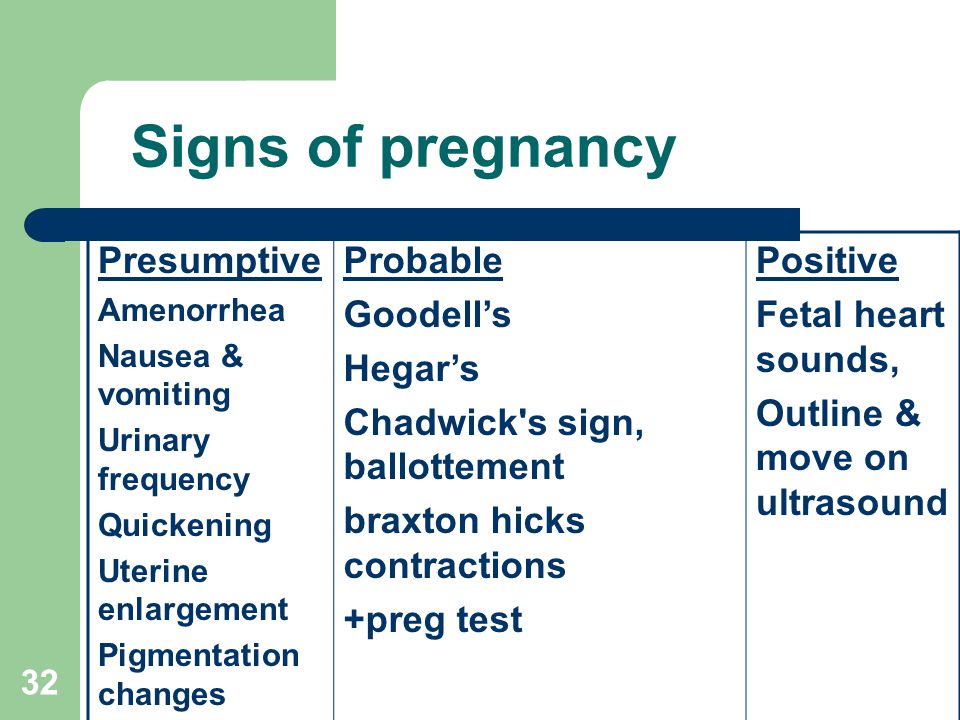
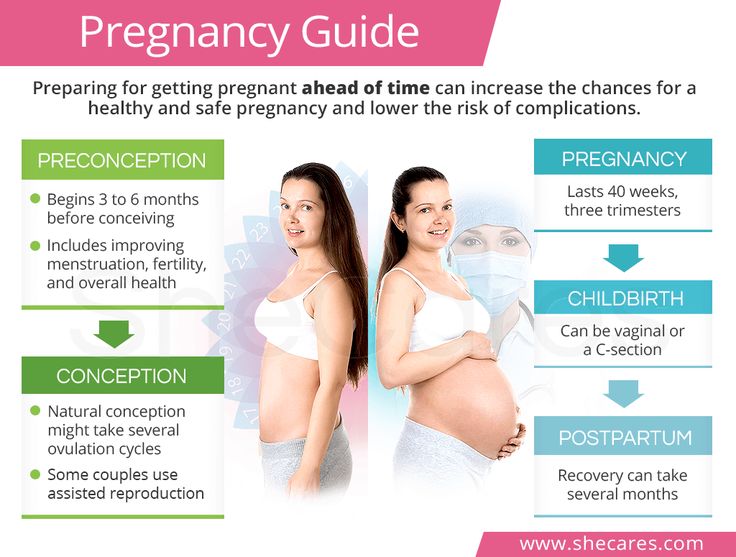
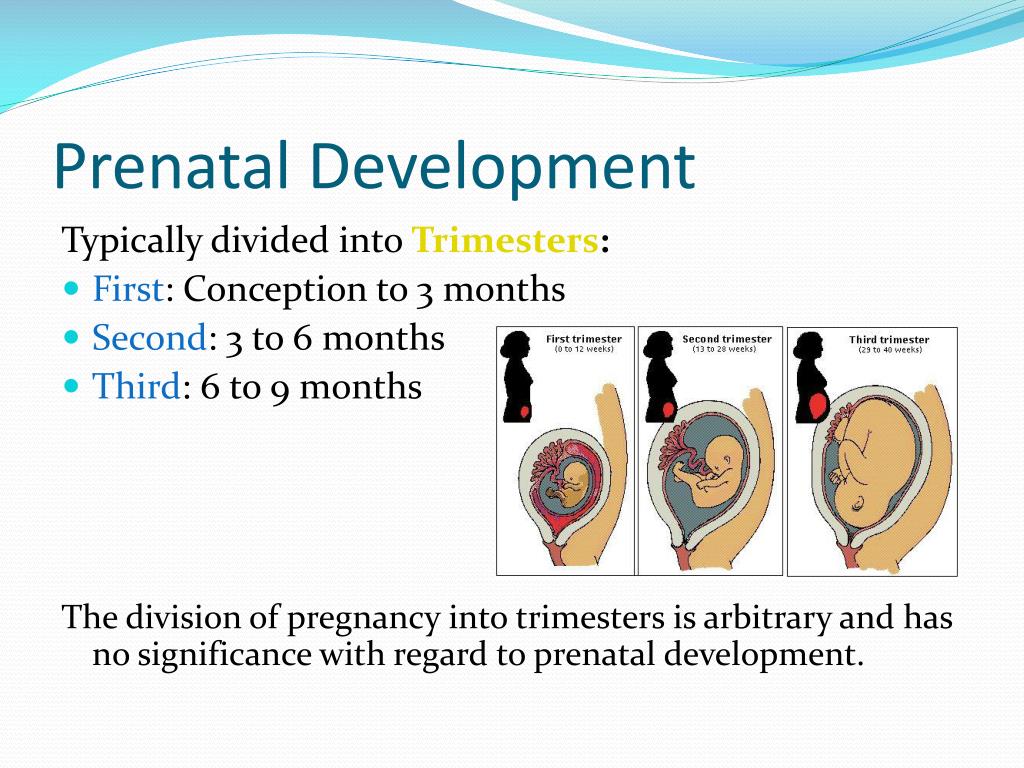
Pregnancy is divided into 3 blocks of 3 months each – the first, second and third trimesters. Reaching week 27 of your pregnancy means you’re now in the third and final trimester. While this trimester could end at week 40, in reality it ends whenever your baby is born.
A baby is considered to have been born full-term if it is born in weeks 37 to 42 of pregnancy. A baby born before week 37 is considered premature, and if your baby has not been born by week 42, labour may be induced.
What happens to your body?
As you get closer to the time your baby will be born, here are some things you’ll notice:
- Your skin and ligaments continue to stretch to accommodate your growing baby.
- You get tired easily, and sleeping becomes more difficult.
- You experience heartburn and/or breathlessness, as the baby grows in your abdomen.
While these are all part of a normal pregnancy, you can take steps to minimise discomfort. Speak with your doctor or midwife for suggestions, particularly if you are in pain.
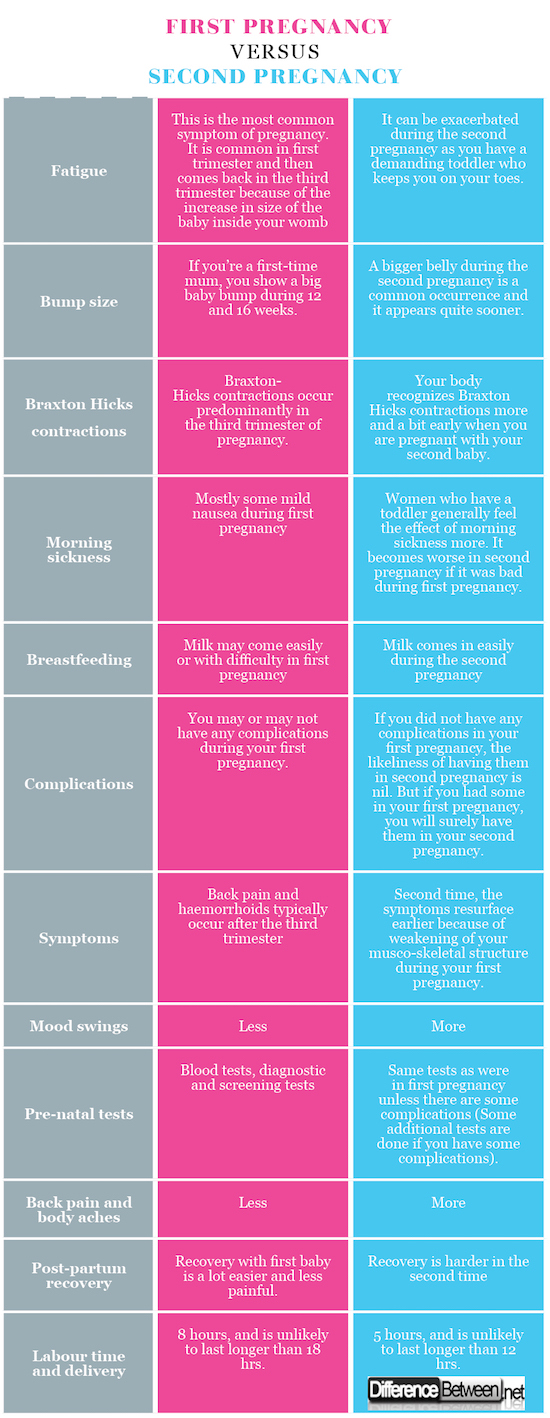
You may also experience Braxton-Hicks contractions, which are a tightening of the muscles of the uterus. They last around 30 seconds, are irregular and not painful. They are not labour contractions, and not a sign that labour has begun.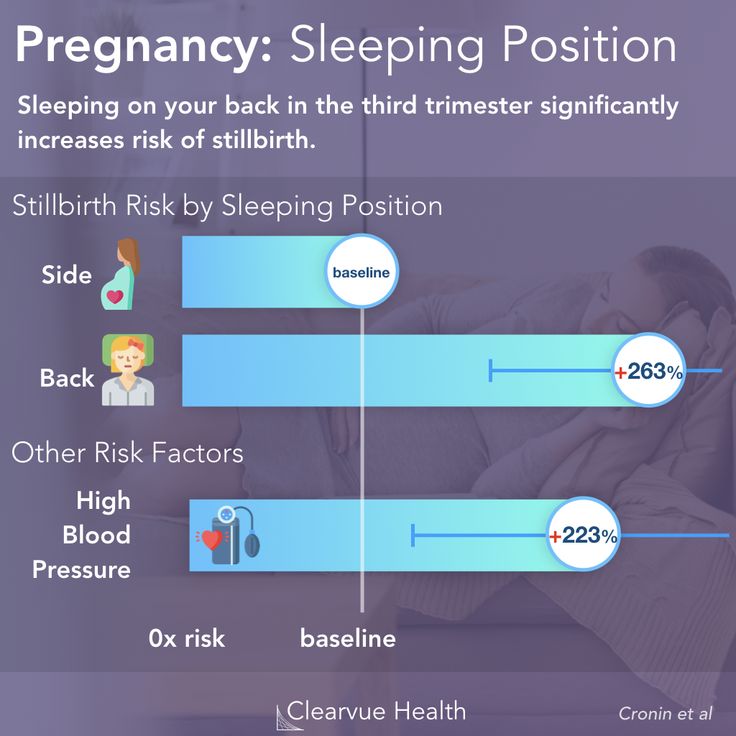
If this is your first baby, you may notice around 36 weeks that your baby has moved further down into your pelvis. This is often referred to as 'the baby has engaged or dropped'. You will notice more room near your ribs and breathing will become easier, but this also adds more pressure on your bladder (meaning more trips to the toilet).
In the last few weeks of this trimester your body begins to prepare for the coming labour. The cervix begins to soften, and many women notice a ‘show’. The ‘show’ is the release of the mucous plug that sits within the cervical canal during pregnancy, and is an early sign that your labour will soon begin.
Your emotions
During this last stage of pregnancy, you may be worried or anxious about labour and the birth, or about how you will manage as a parent.
Difficulty getting comfortable in bed and frequent bathroom visits can mean poor sleep, which is known to trigger irritability and low mood in some people.
Although most pregnant women see the third trimester as an exciting time and feel positive about the next stage, one in 5 will experience antenatal anxiety or depression.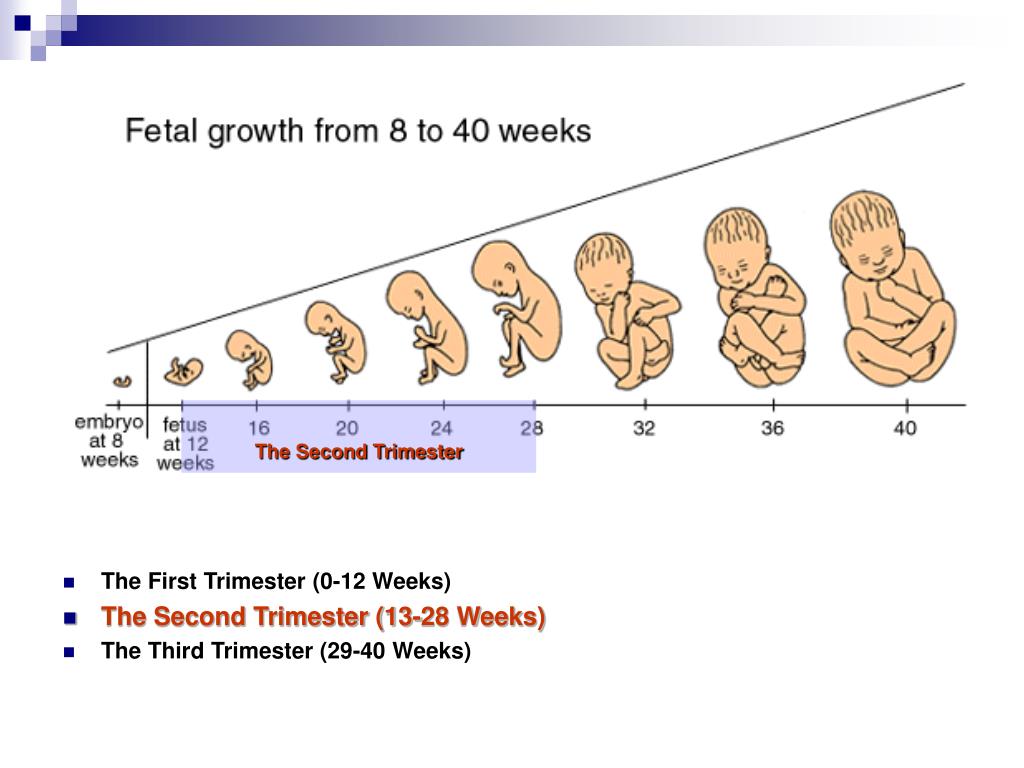 Seek help early if this is how you (or your partner) are feeling.
Seek help early if this is how you (or your partner) are feeling.
What happens to the baby?
By week 31, your baby’s lungs are more mature, but are yet to produce surfactant, a substance that helps with breathing once they are born.
By week 36, your baby is about 47cm long and weighs approximately 2.6kg. Your baby’s head may start to engage or sit lower into your pelvis at this time, getting ready for labour. Around one in 25 of all babies will be in the ‘breech position’, rather than the usual head-down position, at the start of labour. If this is your situation, your doctor or midwife will discuss with you what this means for your labour, what your options are and how your baby might be born.
By 40 weeks, your baby will be about 50cm, and weigh approximately 3.4kg. Developmentally, your baby is now ready to be born.
What to expect with your doctor or midwife?
Through the third trimester you will have frequent antenatal check-ups: about every 4 weeks until 36 weeks, then every 2 weeks after that.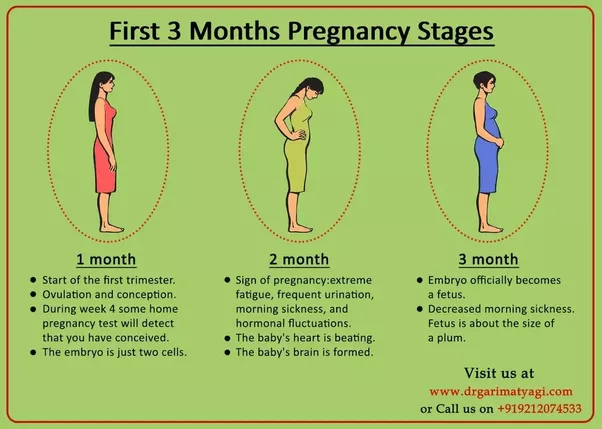
If you haven’t already had them, the following may be offered:
- gestational diabetes check
- strep (streptococcal) B check
- whooping cough (pertussis) vaccination
- flu (influenza) vaccination
How to stay healthy
To give your baby a healthy start, it’s important to eat healthy foods throughout pregnancy. Ensure your diet is varied and includes a range of fresh fruit and vegetables as well as sources of protein, iron and calcium. Don’t forget to drink plenty of water too.
Weight gain is a normal part of pregnancy and most women can expect to gain between 11 and 16kg.
A pregnancy weight gain calculator can be a handy tool to track your weight gain through the third trimester.
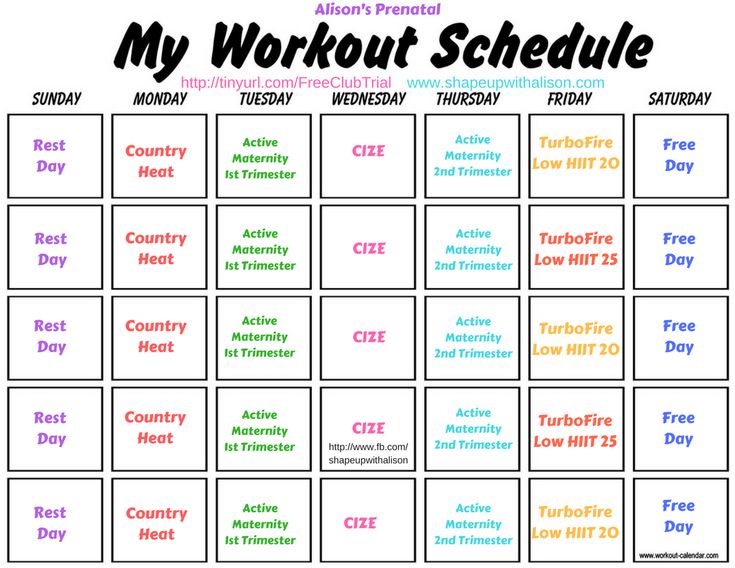
Try to stay active throughout pregnancy - even in your third trimester. While it's important to stick with safe, gentle exercise as you get closer to your due date, recommendations state that pregnant women without complications are encouraged to participate in regular exercise as part of a healthy lifestyle.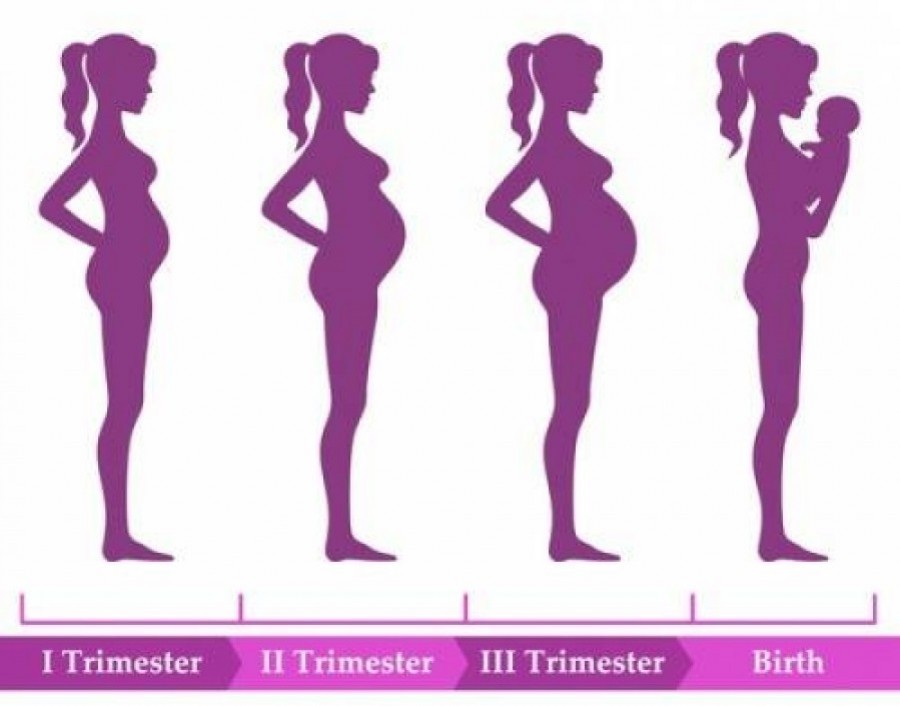
Things to consider
As you enter the third trimester don’t forget to:
- pack a hospital bag
- book a hospital/birthing centre tour
- arrange a properly-fitted car seat (to bring your baby home)
- consider what you will need when you bring your baby home – what will you buy, can you borrow from family or friends?
- if you have other children (or pets), plan for their care while you are in hospital
- consider shopping ahead – especially for non-perishable staples (tinned foods, bathroom products, etc.)
- cook double portions through your third trimester, and load your freezer for when things get busy once the baby is born
Sources:
NSW Health (Having a baby), Royal Women's Hospital (Pregnancy and birth), Raising Children Network (Pregnancy week-by-week), Women's and Children's Health Network (The first 3 months of pregnancy: the first trimester), Perinatal Anxiety and Depression Australia (During pregnancy), Healthy WA (Emotional health for parents during pregnancy and after the birth), Sports Medicine Australia (Exercise in pregnancy and the postpartum period), Mater Mother's Hospital (Labour and birth information)Learn more here about the development and quality assurance of healthdirect content.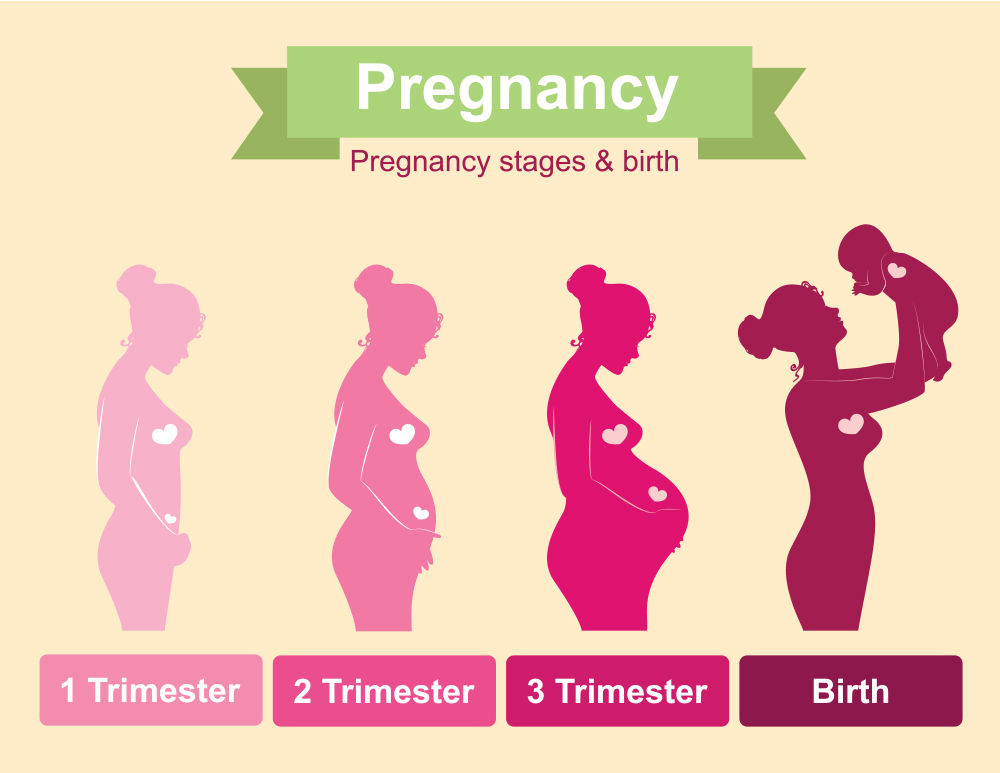
Last reviewed: May 2021
Back To Top
Related pages
- First trimester
- Second trimester
- Pregnancy week-by-week
Need more information?
Third trimester: pregnancy week by week | Raising Children Network
Pregnant? In our pregnancy week by week guide, you can find out what to expect and follow your baby's development during the third trimester.
Read more on raisingchildren.net.au website
Pregnancy changes video: third trimester | Raising Children Network
In this video parents and a midwife describe physical and emotional changes in the third trimester of pregnancy including discomfort and baby movement.
Read more on raisingchildren.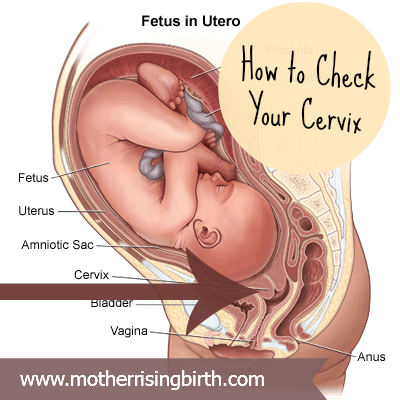 net.au website
net.au website
Third trimester: what men can expect | Raising Children Network
The third trimester is an exciting time, as baby’s birth gets closer. It’s a time for men to prepare for a birth support role and their first hours as dads.
Read more on raisingchildren.net.au website
Men, sex & third trimester of pregnancy | Raising Children Network
It’s usually fine to have sex in pregnancy, but in the third trimester it might feel different or awkward. Our Dads Guide describes how this can affect men.
Read more on raisingchildren.net.au website
Pregnancy at week 31
Feeling tired and emotional during the third trimester is very common, but it's important to discuss these feelings with your doctor or midwife.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 30
Your baby's reflexes are developing, and they may even be sucking their thumb or fingers. You might be tired and sore, but try to exercise and get enough sleep.
Read more on Pregnancy, Birth & Baby website
Is 'baby brain' real?
Researchers at Deakin University who investigated 'baby brain' found that cognitive function and memory are affected in the third trimester of pregnancy.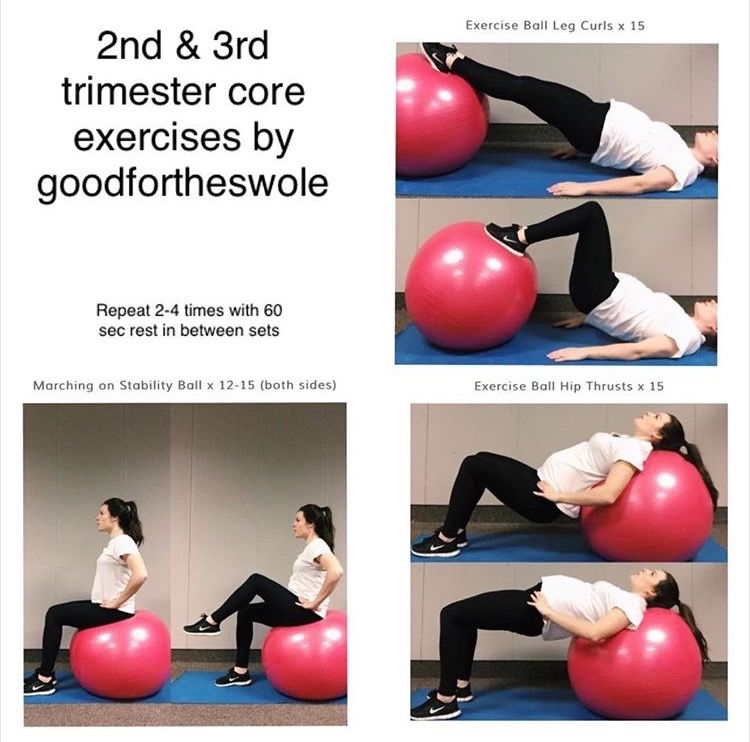
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 29
Your baby should weigh about 1kg by now and as your uterus pushes against your diaphragm and lungs, you might be feeling quite breathless.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 36
Your baby will by now be curled up and cramped inside your uterus and weigh about 2.5kg. Your bump may have moved down, putting pressure on your lower abdomen.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.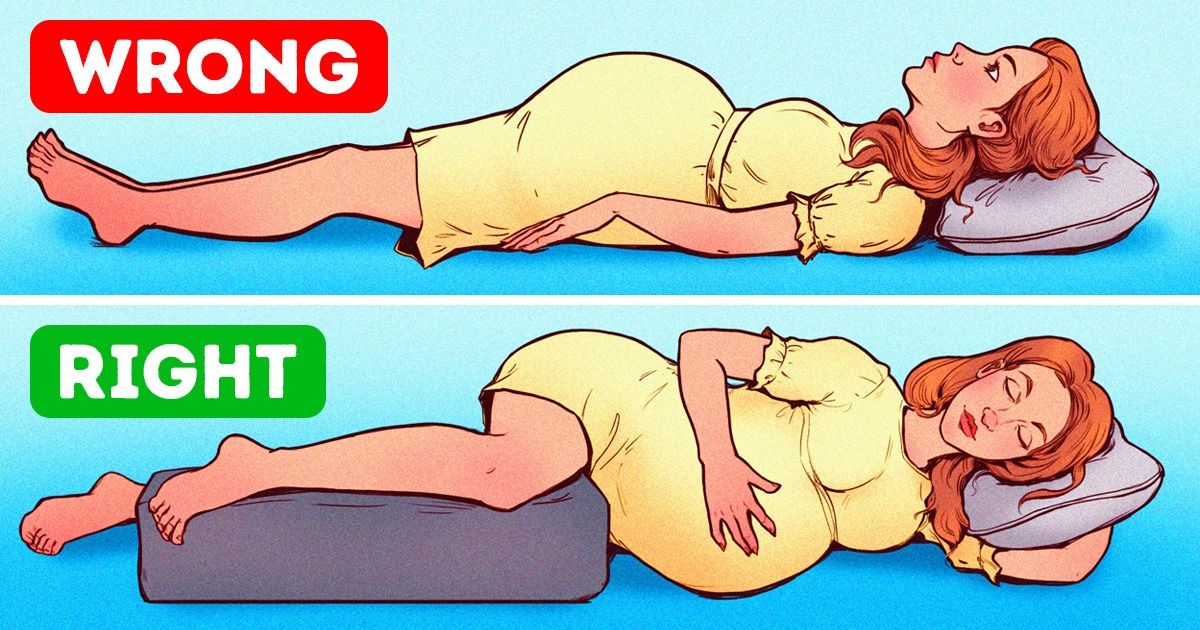
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What to Expect, Fetal Development
Written by Stephanie Watson
In this Article
- What Is the Third Trimester?
- New Fetal Development
- Third Trimester Changes in Your Body
- Red Flag Symptoms
- Third Trimester Tips for Twins
What Is the Third Trimester?
The third trimester is the last phase of your pregnancy.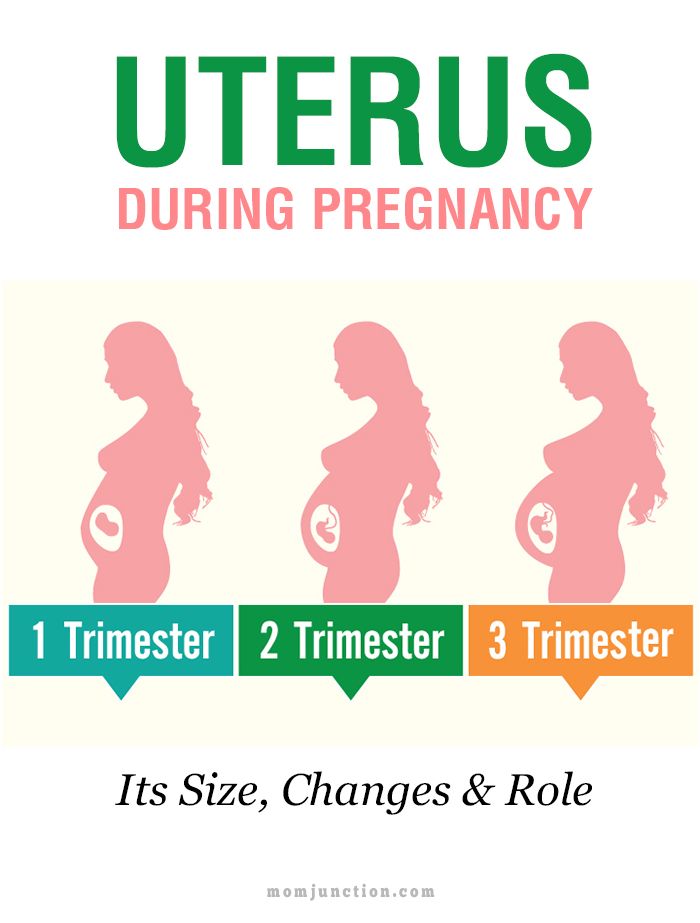 It lasts from weeks 29 to 40, or months 7, 8, and 9. During this trimester, your baby grows, develops, and starts to change position to get ready for birth.
It lasts from weeks 29 to 40, or months 7, 8, and 9. During this trimester, your baby grows, develops, and starts to change position to get ready for birth.
Now that you've reached the third trimester, you're in the home stretch of your pregnancy. You've only got a few more weeks to go, but this part of your pregnancy can be the most challenging.
New Fetal Development
In the third trimester, your baby keeps growing. By the end, a full-term baby usually is between 19 and 21 inches long and between 6 and 9 pounds.
Your baby begins to turn itself head-down to get ready for delivery. At week 36, the baby’s head should begin to move into your pelvic area, also called lightening. It will stay in this down-facing position for the last 2 weeks of your pregnancy.
Your baby develops in other important ways in the third trimester. During this phase, it’s able to:
- Open its eyes and see
- Hear
- Suck on its thumb
- Cry
- Smile
Your baby’s brain continues to develop. Its lungs and kidneys mature. It gains muscle tone and about 16% body fat. The bones at the top of its skull are soft to ease delivery. Most babies have blue eyes at this stage, and they’ll stay that color until a few days or weeks after they’re born. It also has nails on its toes and reaching to the ends of its fingers. If it’s a boy, the testes have descended into the scrotum.
Its lungs and kidneys mature. It gains muscle tone and about 16% body fat. The bones at the top of its skull are soft to ease delivery. Most babies have blue eyes at this stage, and they’ll stay that color until a few days or weeks after they’re born. It also has nails on its toes and reaching to the ends of its fingers. If it’s a boy, the testes have descended into the scrotum.
During the third trimester, the vernix caseosa, a protective coating, covers your fetus’ skin. Soft body hair called the lanugo falls out and is almost gone by the end of week 40.
Third Trimester Changes in Your Body
- Abdominal achiness. As your baby grows, it takes up more room in your abdomen. This can cause you to have some aches and discomfort. You may find it hard to get comfortable when you’re in bed at night trying to go to sleep. You may even feel like it’s harder to take deep breaths.
- Backache. The extra weight you've gained puts added pressure on your back, making it feel achy and sore.
 You might also feel discomfort in your pelvis and hips as your ligaments loosen to prepare for labor. To ease the pressure on your back, try to practice good posture. Sit up straight and use a chair that provides good back support. At night, sleep on your side with a pillow tucked between your legs. Wear low-heeled, comfortable shoes with good arch support. To ease back pain, use a heating pad. Ask your doctor whether it's OK for you to take acetaminophen.
You might also feel discomfort in your pelvis and hips as your ligaments loosen to prepare for labor. To ease the pressure on your back, try to practice good posture. Sit up straight and use a chair that provides good back support. At night, sleep on your side with a pillow tucked between your legs. Wear low-heeled, comfortable shoes with good arch support. To ease back pain, use a heating pad. Ask your doctor whether it's OK for you to take acetaminophen. - Bleeding. Some light bleeding toward the end of your pregnancy might be a sign that labor is starting. But spotting may sometimes be a sign of a serious problem, including placenta previa (the placenta grows low and covers the cervix), placental abruption (separation of the placenta from the uterine wall), or preterm labor. Call your doctor as soon as you notice any bleeding.
- Braxton-Hicks contractions. You might start to feel mild contractions, which are warm-ups to prepare your uterus for the real labor to come.
 Braxton-Hicks contractions often aren't as intense as real labor contractions, but they may feel a lot like labor and can eventually progress to it. One main difference is that real contractions gradually get closer and closer together -- and more intense. If you're red in the face and out of breath after your contractions, or they're coming regularly, call your doctor.
Braxton-Hicks contractions often aren't as intense as real labor contractions, but they may feel a lot like labor and can eventually progress to it. One main difference is that real contractions gradually get closer and closer together -- and more intense. If you're red in the face and out of breath after your contractions, or they're coming regularly, call your doctor. - Breast enlargement and leaking. By the end of your pregnancy, your breasts will have grown by as much as 2 pounds. Make sure you're wearing a supportive bra so your back doesn't suffer. Close to your due date, you may start to see a yellowish fluid leaking from your nipples. This substance, called colostrum, will nourish your baby in the first few days after birth.
- Vivid dreams. It’s common to have more vivid dreams or nightmares in your third trimester. This can disrupt your sleep. Your wild dreams are likely caused by changes in hormone levels from pregnancy.
- Clumsiness.
 You may feel clumsy or out of balance during the third trimester. You may drop things. Part of the reason is that you’ve gained weight in your belly area. That makes it harder to balance your body.
You may feel clumsy or out of balance during the third trimester. You may drop things. Part of the reason is that you’ve gained weight in your belly area. That makes it harder to balance your body. - Discharge. You might see more vaginal discharge during the third trimester. If the flow is heavy enough to soak through your panty liners, call your doctor. Close to your delivery date, you might see a thick, clear, or slightly blood-tinged discharge. This is your mucus plug, and it's a sign that your cervix has begun dilating in preparation for labor. If you experience a sudden rush of fluid, it may mean that your water has broken (although only about 8% of pregnant women have their water break before contractions begin). Call your doctor as soon as possible after your water breaks.
- Fatigue. You might have been feeling energetic in your second trimester, but are weary now. Carrying extra weight, waking up several times during the night to go to the bathroom, and dealing with the anxiety of preparing for a baby can all take a toll on your energy level.
 Eat healthy food and get regular exercise to give yourself a boost. When you feel tired, try to take a nap, or at least sit down and relax for a few minutes. You need to reserve all your strength now for when your baby arrives and you're really not getting any sleep.
Eat healthy food and get regular exercise to give yourself a boost. When you feel tired, try to take a nap, or at least sit down and relax for a few minutes. You need to reserve all your strength now for when your baby arrives and you're really not getting any sleep. - Frequent urination. Now that your baby is bigger, its head may be pressing down on your bladder. That extra pressure means you'll have to go to the bathroom more frequently -- including several times each night. You might also find that you're leaking urine when you cough, sneeze, laugh, or exercise. To relieve the pressure and prevent leakage, go to the bathroom whenever you feel the urge and urinate completely each time. Avoid drinking fluids right before bedtime to cut down on unwanted late-night bathroom visits. Wear a panty liner to absorb any leakage. Let your doctor know if you have any pain or burning with urination. These can be signs of a urinary tract infection.
- Heartburn and constipation.
 They're caused by extra production of the hormone progesterone, which relaxes certain muscles -- including the muscles in your esophagus that normally keep food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (like citrus fruits). For constipation, increase your fiber intake and drink extra fluids to keep things moving more smoothly. If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief.
They're caused by extra production of the hormone progesterone, which relaxes certain muscles -- including the muscles in your esophagus that normally keep food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (like citrus fruits). For constipation, increase your fiber intake and drink extra fluids to keep things moving more smoothly. If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief. - Hemorrhoids. Hemorrhoids are actually varicose veins -- swollen veins that form around the anus. These veins enlarge during pregnancy because extra blood is flowing through them and the weight of pregnancy increases the amount of pressure to the area. To relieve the itch and discomfort, try sitting in a warm tub or sitz bath.
 Ask your doctor whether you can also try an over-the-counter hemorrhoid ointment or stool softener.
Ask your doctor whether you can also try an over-the-counter hemorrhoid ointment or stool softener. - Sciatica. Nerve pain that shoots from your lower back to your buttocks and down your leg is more likely in the third trimester. Sciatica may be caused by hormone changes during pregnancy, or because your baby’s growing body presses against the sciatic nerve. Sciatica pain may come and go or be constant. Yoga, massage, or physical therapy are ways to relieve the pain, but it usually goes away after your baby is born.
- Shortness of breath. As your uterus expands, it rises up until it sits just under your rib cage, leaving less room for your lungs to expand. That added pressure on your lungs can make it more difficult to breathe. Exercising can help with shortness of breath. You can also try propping up your head and shoulders with pillows while you sleep.
- Spider and varicose veins. Your circulation has increased to send extra blood to your growing baby.
 That excess blood flow can cause tiny red veins, known as spider veins, to appear on your skin. Spider veins may get worse in your third trimester, but they should fade once your baby is born. Pressure on your legs from your growing baby may also cause some surface veins in your legs to become swollen and blue or purple. These are called varicose veins. They should improve within a few months after you deliver. Although there's no way to avoid varicose veins, you can prevent them from getting worse by:
That excess blood flow can cause tiny red veins, known as spider veins, to appear on your skin. Spider veins may get worse in your third trimester, but they should fade once your baby is born. Pressure on your legs from your growing baby may also cause some surface veins in your legs to become swollen and blue or purple. These are called varicose veins. They should improve within a few months after you deliver. Although there's no way to avoid varicose veins, you can prevent them from getting worse by:- Getting up and moving throughout the day
- Wearing support hose
- Propping up your legs whenever you have to sit for long periods.
- Stretch marks. You may develop stretch marks on your breasts, butt, tummy, or thighs. Stretch marks are a type of scar that happens when your skin stretches during pregnancy. Not everyone gets them. If you do, they may be red, purple, pink, or brown in color.
- Swelling. Your rings might be feeling tighter these days, and you may also notice that your ankles and face are looking bloated.
 Mild swelling is the result of excess fluid retention (edema). To reduce swelling, put your feet up on a stool or box whenever you sit for any length of time, and elevate your feet while you sleep. If you have sudden onset of swelling though, seek medical attention immediately as it may be a sign of preeclampsia, a dangerous pregnancy complication.
Mild swelling is the result of excess fluid retention (edema). To reduce swelling, put your feet up on a stool or box whenever you sit for any length of time, and elevate your feet while you sleep. If you have sudden onset of swelling though, seek medical attention immediately as it may be a sign of preeclampsia, a dangerous pregnancy complication. - Weight gain. Aim for a weight gain of 1/2 pound to 1 pound a week during your third trimester. By the end of your pregnancy, you should have put on a total of about 25 to 35 pounds (your doctor may have recommended that you gain more or less weight if you started out your pregnancy underweight or overweight). The extra pounds you've put on are made up of the baby's weight, plus the placenta, amniotic fluid, increased blood and fluid volume, and added breast tissue. If your baby seems to be too small or too big based on the size of your belly, your doctor will do an ultrasound to check the baby’s growth.
Red Flag Symptoms
Any of these symptoms could be a sign that something is wrong with your pregnancy.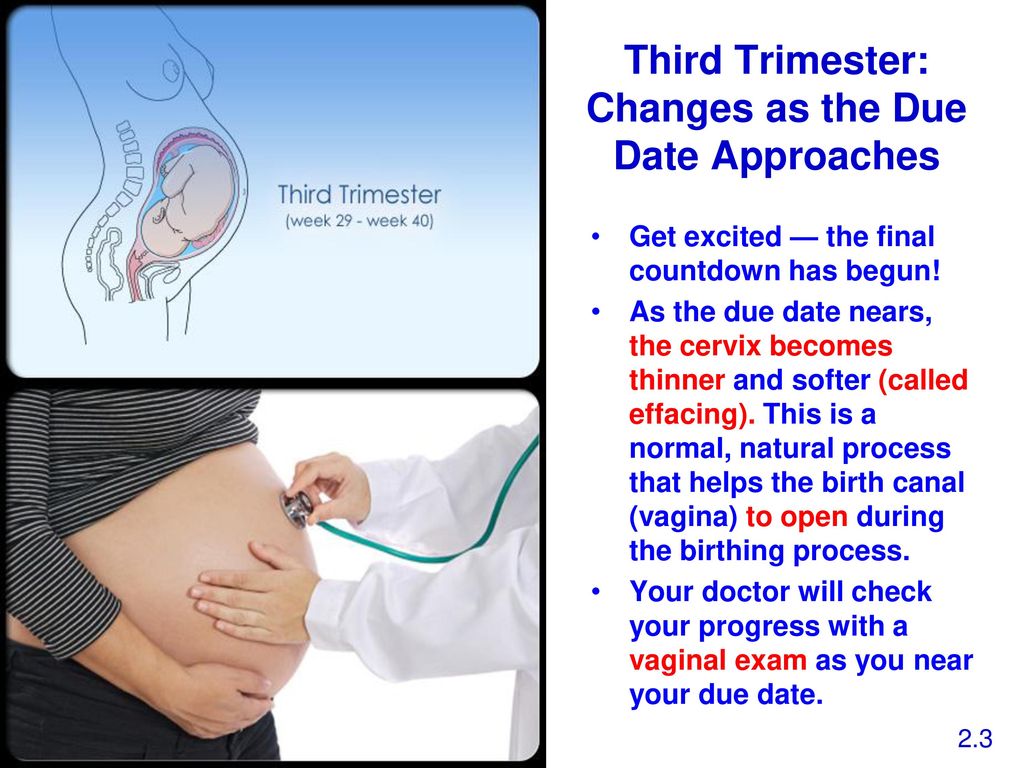 Don't wait for your regular prenatal visit to talk about it. Call your doctor right away if you experience:
Don't wait for your regular prenatal visit to talk about it. Call your doctor right away if you experience:
- Severe abdominal pain or cramps
- Severe nausea or vomiting
- Bleeding
- Severe dizziness
- Pain or burning during urination
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain
Third Trimester Tips for Twins
Expecting twins? You might want to add these things to your third trimester to-do list:
- Go stroller shopping. Side-by-side or tandem? Take a few double strollers for a test drive to see which type feels best to you. Look for one that's easy to open and maneuver.
- Get breastfeeding tips. Breastfeeding two babies is more of a challenge than one, but you can definitely do it. Ask your doctor ahead of time for tips.
- Check your iron. Ask your doctor if you need to take iron supplements.
 As a mom-to-be of twins, you're four times more likely to have iron-deficiency anemia.
As a mom-to-be of twins, you're four times more likely to have iron-deficiency anemia. - Know the signs of preeclampsia. Carrying twins doubles your risk of this serious condition. Tell your doctor right away if you have a headache, trouble seeing, or sudden weight gain.
- Find a support group. Start looking for groups of moms of multiples in your area. You may appreciate exchanging tips and getting support from other moms in the same boat.
- Create a schedule. Read up on how to get your twins on the same sleeping and eating schedule. Learning some tips now may save your sanity when you have two newborns.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Pregnancy by trimesters: 2nd and 3rd trimester
The first trimester is behind us with its anxiety, morning sickness, constant sleepiness and other problems. If you count by weeks, the II trimester starts from the 13th week and is considered the easiest and calmest. The future mother, both psychologically and physically, has already adapted to her status, but it seems that motherhood is not yet close. However, there is also a lot of research to be done.
If you count by weeks, the II trimester starts from the 13th week and is considered the easiest and calmest. The future mother, both psychologically and physically, has already adapted to her status, but it seems that motherhood is not yet close. However, there is also a lot of research to be done.
A full range of laboratory tests is available at DILA: Program 185 "Examination of a pregnant woman at 22-24 weeks of gestation", prenatal screening of the second trimester, prenatal non-invasive screening (NIPT, basic), as well as a number of other screening programs and mono-studies. All of them are aimed at determining the general state of health, the work of the main systems and organs of a pregnant woman in the second and third trimesters of pregnancy. Regular monitoring will allow early detection of various complications that may arise and provide the necessary treatment. Thus, the chances of a normal pregnancy and the birth of a healthy child are increased. nine0003
Second trimester examinations
The second (II) trimester of pregnancy includes the period between 13 and 26 weeks. It is during this time period, closer to the 16th week, that all organs and systems of the fetus are already finally laid down, but all the organs and systems of the fetus continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators of this period reflects not only the state of health of a pregnant woman and the features of the work of the main organs and systems, but also makes it possible to detect diseases and possible complications. nine0003
It is during this time period, closer to the 16th week, that all organs and systems of the fetus are already finally laid down, but all the organs and systems of the fetus continue to develop, the placenta is formed, and after the 23rd week the fetus is already considered fully viable and formed. Clinical laboratory diagnostics of a number of biochemical indicators of this period reflects not only the state of health of a pregnant woman and the features of the work of the main organs and systems, but also makes it possible to detect diseases and possible complications. nine0003
So, Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy" includes the following studies:
- Complete blood count. It is aimed at a basic assessment of the general state of health: the hematopoietic system, the presence of inflammatory, infectious (including viral), oncological diseases, as well as allergic processes in the body.
- Urinalysis. Allows you to assess the state of the urinary tract and some extrarenal diseases, to identify the presence of preeclampsia.
 nine0020
nine0020 - Glucose tolerance test, which makes it possible to evaluate carbohydrate metabolism disorders (including latent forms).
- HIV 1/1o/2 to detect HIV infection.
Complete blood count with leukocyte count and ESR (erythrocyte sedimentation rate) and urinalysis should preferably be performed once a month.
Clinical blood test makes it possible to study the qualitative and quantitative composition of blood by key indicators: erythrocytes and their specific indicators, leukocytes and their varieties in absolute and percentage terms, platelets. The detection of deviations in these markers may indicate the presence of pathological processes in the body of a pregnant woman. A decrease in the level of erythrocytes and hemoglobin in erythrocytes is a sign of anemia in pregnant women. This can lead to placental insufficiency - the main reason for miscarriage, the birth of small children and fetal death. nine0003
Changes in the leukocyte formula may indicate a wide range of changes in the body of pregnant women in the 2nd trimester. They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which requires a more extensive additional examination - both instrumental and laboratory. The content of platelets during physiological pregnancy may slightly decrease, but significant changes in this indicator, including developing thrombocytopenia, require special observation, since they may be indirect signs of a violation of the blood coagulation system, as well as DIC (disseminated intravascular coagulation syndrome), which are severe pregnancy complications. nine0003
They can act as laboratory signs of previously undiagnosed inflammatory and infectious processes, which requires a more extensive additional examination - both instrumental and laboratory. The content of platelets during physiological pregnancy may slightly decrease, but significant changes in this indicator, including developing thrombocytopenia, require special observation, since they may be indirect signs of a violation of the blood coagulation system, as well as DIC (disseminated intravascular coagulation syndrome), which are severe pregnancy complications. nine0003
Changes in erythrocyte sedimentation rate (ESR) can be observed in acute and chronic inflammatory pathologies, infectious diseases, as well as oncological and autoimmune processes. At the same time, in pregnant women, the erythrocyte sedimentation rate slightly increases in the norm.
General analysis of urine allows you to evaluate the general properties of urine, its physico-chemical properties, the presence of metabolic products, to detect the quantitative and qualitative content of certain organic compounds.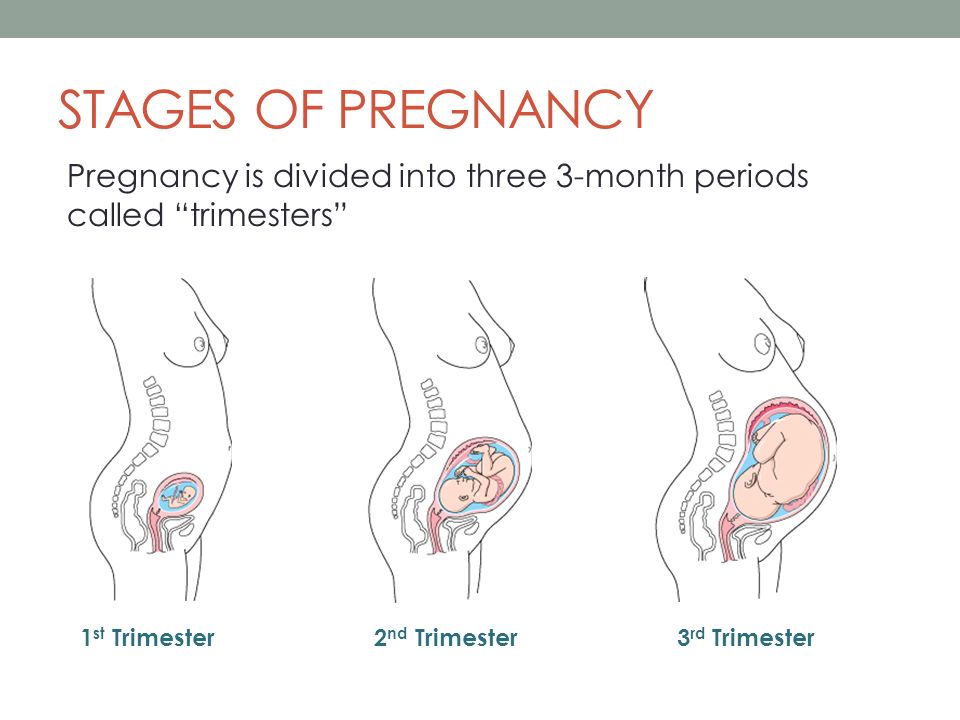 This study reflects the functional state of the kidneys, urinary tract, allows you to evaluate the overall metabolic processes, suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, "pregnancy diabetes". If protein is found in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks. nine0003
This study reflects the functional state of the kidneys, urinary tract, allows you to evaluate the overall metabolic processes, suggest the presence of infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, "pregnancy diabetes". If protein is found in the urine, this may be evidence of developing kidney pathology in pregnant women, as well as a sign of the development of a severe complication during pregnancy - preeclampsia for more than 20 weeks. nine0003
The glucose tolerance test detects gestational diabetes (“diabetes in pregnancy”). If this deviation is detected, a woman needs to control her sugar levels throughout pregnancy and after childbirth. Early detection of gestational diabetes is very important to prevent a number of undesirable consequences, including the birth of a large fetus and the risk of prenatal complications.
HIV testing . To reduce the risk of infection of the fetus, it is very important to detect the human immunodeficiency virus in a pregnant woman in a timely manner. The detection of HIV infection is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. Without preventive measures, the risks of transmission of HIV infection from mother to fetus are 20-40%, while the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur when the fetus passes through the natural birth canal. In addition, there is a high risk of infection during breastfeeding. nine0003
To reduce the risk of infection of the fetus, it is very important to detect the human immunodeficiency virus in a pregnant woman in a timely manner. The detection of HIV infection is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. Without preventive measures, the risks of transmission of HIV infection from mother to fetus are 20-40%, while the use of special preventive measures reduces the likelihood of transmission of infection to 1-2%. Most cases of infection occur when the fetus passes through the natural birth canal. In addition, there is a high risk of infection during breastfeeding. nine0003
We have only described the possibilities of Program 185 "Examination of a pregnant woman at 22-24 weeks of pregnancy", but there are a number of other important studies.
2nd trimester prenatal screening - "triple test", including the determination of the total unit of beta-hCG, AFP and unconjugated (free) estriol. It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain fetal chromosomal abnormalities:
It is carried out for the purpose of biochemical screening of a pregnant woman to assess the risks of certain fetal chromosomal abnormalities:
- Down syndrome. Violation is accompanied by characteristic features of appearance, mental retardation, defects of internal organs, short stature. nine0020
- Edwards syndrome. Most children with this syndrome die before the age of 3 months, only 5-10% survive to a year. The survivors are profoundly mentally retarded.
- Patau Syndrome. Accompanied by severe congenital malformations.
Also, prenatal screening of the second trimester makes it possible to assess the risk of malformations of the neural tube of the fetus.
The test is performed between 14 and 21 weeks, optimally between 16 and 18 weeks of pregnancy. Down, Edwards and Patau syndromes are the most common chromosomal disorders. The ability to detect these disorders in the early stages allows you to timely assess the genetic health of the fetus.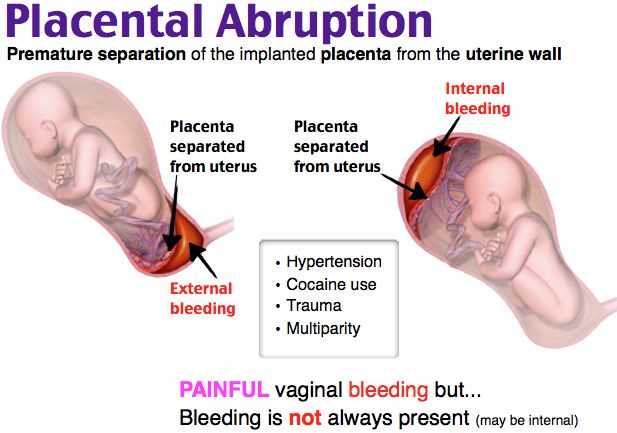 nine0003
nine0003
An alternative to biochemical prenatal screening is the NIPT test. It is more accurate than biochemical, and neither the course of pregnancy, nor the drugs taken, nor the woman's somatic diseases affect its results. The difference from biochemical screening is that NIPT is a direct method that allows you to examine the DNA of the fetus, while biochemistry is an indirect method. Biochemical screening has an accuracy of 70-80%, while NIPT has an accuracy of more than 99.9%. nine0003
Another important laboratory marker in the 2nd trimester is thyroid-stimulating hormone (TSH). This hormone is produced by the pituitary gland and is responsible for regulating the synthesis of the thyroid hormones thyroxine and triiodothyronine according to the “feedback system”, which allows maintaining a stable concentration of these hormones in the blood. Despite the fact that the thyroid hormone systems of a pregnant woman and the fetus do not depend on each other, her health and, accordingly, the course of the entire pregnancy depend on the normal functioning of the thyroid system of a woman. During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible. nine0003
During pregnancy, TSH blood levels often remain stable. TSH is important for the normal development of the fetus, in particular for the normal formation of the central nervous system. In iodine deficiency conditions, the development of compensatory hyperplasia of the thyroid gland of the fetus is possible. nine0003
In the second and third trimesters of pregnancy, it is important to assess the risk of one of the most serious pregnancy complications, preeclampsia. Placental growth factor (PLGF), a marker of preeclampsia, has angiogenic properties and is essential for the normal development of the placental vascular system. Normally, the concentration of PlGF gradually increases up to 30 weeks of pregnancy. In the case of preeclampsia, there is a decrease in PLGF. Timely detection of increased risk allows you to predict the optimal tactics of pregnancy and childbirth. nine0003
What tests should be done in the third trimester
The third trimester of pregnancy includes the period between 27 and 40 weeks.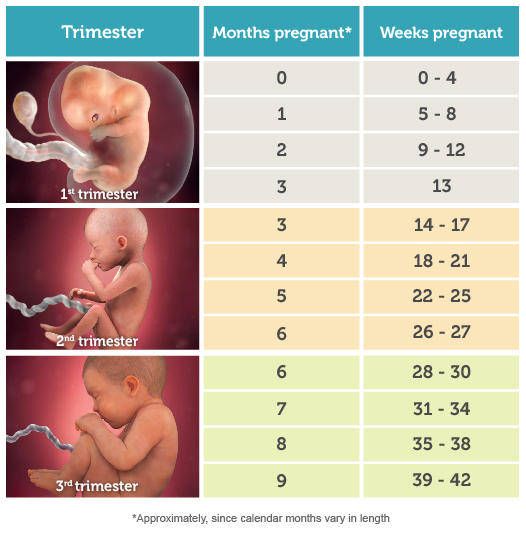 This period is characterized by the active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, and the maturation of the nervous system. Clinical laboratory diagnostics of the III trimester is aimed at assessing the functioning of the main organs and systems, in particular the liver, kidneys, blood coagulation system, endocrine system of a pregnant woman, as well as infection control during pregnancy. nine0003
This period is characterized by the active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, and the maturation of the nervous system. Clinical laboratory diagnostics of the III trimester is aimed at assessing the functioning of the main organs and systems, in particular the liver, kidneys, blood coagulation system, endocrine system of a pregnant woman, as well as infection control during pregnancy. nine0003
To check the state of health in the 3rd trimester, comprehensive examinations are available in DILA Program 186 "Examination of a pregnant woman at 28-29 weeks of gestation" and Program 187 "Examination of a pregnant woman at 32-35 weeks of gestation", as well as individual programs.
Risk of bleeding . In the third trimester of pregnancy, it is important to monitor the state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic coagulation pathway. The test results are Quick prothrombin time and international normalized ratio. These indicators make it possible to assess the state of the liver, the main pathways of the blood coagulation system and the functional state of its basic components. The determination of these markers has a high diagnostic value for predicting thrombosis during pregnancy, diagnosing DIC, a dangerous complication accompanied by massive blood loss. nine0003
The test results are Quick prothrombin time and international normalized ratio. These indicators make it possible to assess the state of the liver, the main pathways of the blood coagulation system and the functional state of its basic components. The determination of these markers has a high diagnostic value for predicting thrombosis during pregnancy, diagnosing DIC, a dangerous complication accompanied by massive blood loss. nine0003
Normally, the levels of prothrombin and fibrinogen in the III trimester of pregnancy slightly increase, but a significant increase in these indicators requires close monitoring and the appointment of the necessary treatment. The concentration of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, however, a sharp increase in the concentration of this protein may indicate a large number of blood clots, which is often associated with venous thromboembolism or DIC. nine0003
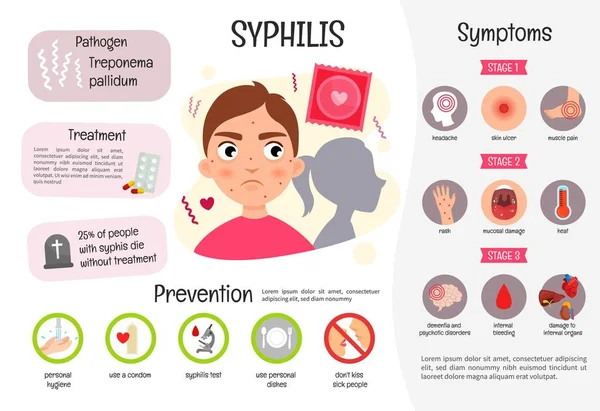
Infections . In the third trimester of pregnancy, it is also recommended to re-examine for:
- hepatitis B;
- hepatitis C;
- HIV infection;
- syphilis - antibodies to Treponema pallidum.

Because the incubation period for some infectious diseases varies greatly, negative test results taken early in pregnancy may change by the 3rd trimester or remain negative as well. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or a planned caesarean section. nine0003
Screening for group B streptococcus is now a mandatory test, essential at 36 +0 -37+ 6 weeks of pregnancy.
There is a group of infections that are very dangerous for pregnant women - these are TORCH infections. Their peculiarity lies in the fact that during the primary infection (if the woman has not yet been ill with them) during pregnancy, they can adversely affect all systems and organs of the fetus, especially its central nervous system. Infection with TORCH-group infections increases the likelihood of miscarriage, stillbirth and congenital malformations of the baby, up to disability. Program 134 "Extended screening for TORCH infections" from DILA allows you to assess the immune status (the presence of immune memory) to pathogens that are part of the TORCH complex group. Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period. nine0003
Screening will help to adequately assess the risks of developing intrauterine infections, receive recommendations regarding subsequent pregnancy management and lifestyle changes to reduce the likelihood of primary infection during this critical period. nine0003
Biochemical indicators (alanine aminotransferase, aspartate aminotransferase total bilirubin and direct bilirubin fraction, total protein in serum), which are part of Program 151 "Blood Biochemistry", allow assessing the functional state of the liver. A significant increase in the content of transaminases in the blood may indicate the presence of liver damage, hepatitis, the development of preeclampsia. A decrease in the level of total protein in the blood serum, along with the loss of protein in the urine and with an increase in blood pressure, can also be a sign of developing preeclampsia. To exclude gestational diabetes and the development of complications, in particular diabetic nephropathy, it is important to determine the level of glucose in the blood plasma. To assess the functional state of the kidneys will help determine the concentration of urea and creatinine, as well as assessing the glomerular filtration rate. Importantly, in pregnant women, the amount of creatinine is reduced by almost half due to an increase in blood volume, increased blood flow to the kidneys and, consequently, an increasing degree of filtration. Also, an increase in renal filtration leads to a decrease in the amount of urea in pregnant women. nine0003
To assess the functional state of the kidneys will help determine the concentration of urea and creatinine, as well as assessing the glomerular filtration rate. Importantly, in pregnant women, the amount of creatinine is reduced by almost half due to an increase in blood volume, increased blood flow to the kidneys and, consequently, an increasing degree of filtration. Also, an increase in renal filtration leads to a decrease in the amount of urea in pregnant women. nine0003
During the second and third trimesters of pregnancy, a woman still needs to carefully monitor her health and undergo laboratory diagnostics. Screening programs and individual studies from DILA will help the doctor evaluate the functioning of internal organs, timely identify bleeding disorders in a woman, diagnose dangerous infections, detect possible genetic abnormalities of the fetus, and identify the risk of preeclampsia in time.
Other news
0 0
Third trimester of pregnancy (weeks 28 to 40)
At 30 weeks pregnant, you are ready to go on maternity leave. In the case of twins, prenatal leave is from 28 weeks. Active work, physical and mental overload during this period can provoke premature birth.
In the case of twins, prenatal leave is from 28 weeks. Active work, physical and mental overload during this period can provoke premature birth.
It's time to put on the bandage - it will help your baby stay in the right position and you in good shape after childbirth.
The child still needs a lot of nutrients, vitamins, mineral salts. Use your vacation to relax, but don't lie around all day. We hope that hiking in the fresh air has become a habit for you. nine0003
Do not forget to keep track of the ratio of drunk and excreted liquids. Accumulating in the body, the fluid disrupts the functioning of the kidneys, increases the load on the heart, which causes an increase in blood pressure. As a result, the child suffers: he lacks nutrients, oxygen.
A sharp headache, flashing flies before the eyes, convulsions are signs of eclampsia, a severe complication of pregnancy that poses a threat to the life of the mother and child. Urgently call the ambulance. nine0003
At this time, the uterus becomes very sensitive to the pushes and movements of the child, its muscles periodically tighten. It's like she's doing gymnastics. If this rarely happens and you do not feel pain, then everything is in order and there is no cause for concern. But if the uterus tenses often, pain appears - call an ambulance. If spotting appears, amniotic fluid is pouring out, do not wait for contractions - immediately to the hospital!
It's like she's doing gymnastics. If this rarely happens and you do not feel pain, then everything is in order and there is no cause for concern. But if the uterus tenses often, pain appears - call an ambulance. If spotting appears, amniotic fluid is pouring out, do not wait for contractions - immediately to the hospital!
Sex life from 32-33 weeks is not recommended. nine0003
At 32 weeks, another scheduled ultrasound examination is scheduled to assess the correct functioning of the placenta, if necessary, the study of fetal heart sounds.
The last month is the most difficult. The load on the body has increased to the maximum. You are already tired of the long wait. Approximately two weeks before delivery, a mucous plug will come off the cervix, which is a lump, sometimes slightly stained with blood.
Do not forget to make up for the lack of calcium in the body - until the last day of intrauterine existence, the child intensively stores minerals. Eat fully and properly - the fetus eagerly takes everything valuable for the formation of the body. He needs protein now. Be sure to take a prenatal multivitamin. Rest during the day. Lie on your side, slightly raise your legs. nine0003
He needs protein now. Be sure to take a prenatal multivitamin. Rest during the day. Lie on your side, slightly raise your legs. nine0003
Many women suffer from constipation at this time. Only a rational diet will help. Eliminate grapes, fresh cabbage, peas and other legumes, fresh milk, muffins, sweets. Useful: curdled milk, fermented baked milk, kefir. Steamed dried fruits normalize bowel function well. Don't take laxatives. In the last trimester of pregnancy, they can provoke uterine contractions and cause premature birth.
Sometimes, if the fetus is very large, the navel turns outward. Don't be scared and don't try to push it back. After giving birth, everything will return to normal. nine0003
By the last weeks of pregnancy, the mammary glands are greatly enlarged. The appearance of colostrum is another harbinger of close childbirth. The bra should be tight, with wide straps, always cotton.
Be prepared for contractions to start at any moment. Trim your fingernails and toenails short, and shave your pubic hair.