How does a child get scabies
Scabies (for Parents) - Nemours KidsHealth
What Is Scabies?
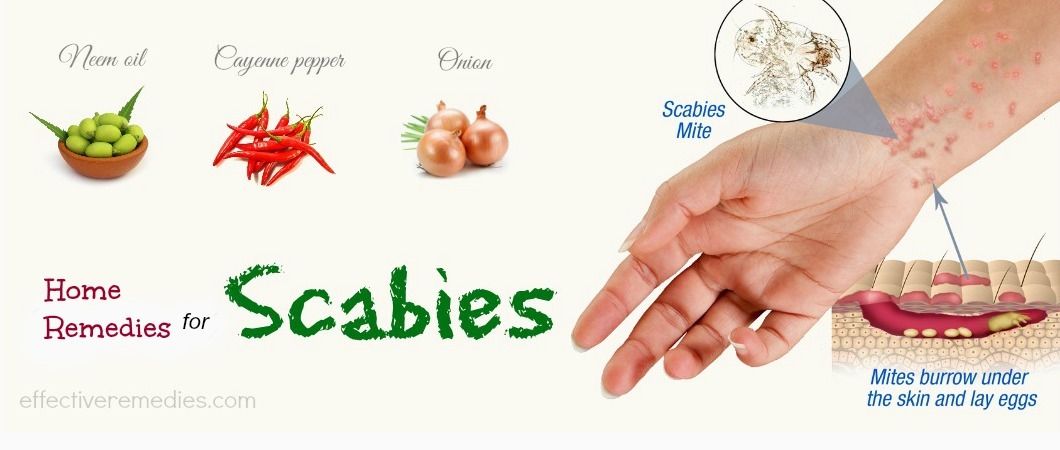
Scabies is a common skin problem caused by tiny mites called Sarcoptes scabiei. The mites burrow into the skin, leave their feces (poop). The female mites lay eggs in the tiny tunnels they create. This causes small itchy bumps and blisters. The itching and rash from scabies are due to a hypersensitive reaction to the mite, its feces, and its eggs.
What Are the Signs & Symptoms of Scabies?
The most common symptom of scabies is itching, which usually starts before any other signs. Other symptoms of scabies include:
- bumps or blisters
- burrow tracks
- thickened, scaly, scratched, and scabbed skin
- in young children, irritability and poor feeding
Scabies can show up on any part of the body but is most common on:
- the hands and feet (especially the webs of skin between the fingers and toes)
- the inner part of the wrists and the folds under the arms
- waistline and groin area
- head and scalp of infants (rare in older children and adults)
It usually takes about 3 weeks after infection for symptoms to show in someone who's never had scabies. People who have had scabies before might see symptoms in a few days.
Is Scabies Contagious?
Scabies is contagious. It spreads through close contact with someone who is infected. Direct physical contact — like holding hands — is the most common way people get scabies.
Mites can live for about 2–3 days in clothing, bedding, or dust. So people can get scabies by sharing clothing, towels, or bedding used by someone who has scabies.
Scabies spreads most easily in crowded places with a lot of close contact, such as childcare centers, college dorms, and nursing homes.
How Is Scabies Diagnosed?
Doctors usually diagnose scabies based on symptoms and how the rash looks. The doctor may scrape the skin to look for mites or eggs under a microscope.
How Is Scabies Treated?
Doctors treat scabies by prescribing a medicated cream or lotion to kill the mites. Apply the cream to skin all over the body (from the neck down), not just the area with the rash. In infants and young children, also put the cream on the face (avoiding the mouth and eyes), scalp, and ears. Trim your child's nails and also put medicine on the fingertips.
In infants and young children, also put the cream on the face (avoiding the mouth and eyes), scalp, and ears. Trim your child's nails and also put medicine on the fingertips.
Most treatments need to stay on the skin for 8–12 hours before they're washed off. You may want to apply the medicine before your child goes to bed, then wash it off in the morning.
If treatment is effective, there should be no new rashes or burrows after 24–48 hours. The treatment may need to be repeated in 1–2 weeks. It may take 2–6 weeks after successful treatment before the itching and rash are gone.
Sometimes doctors use an oral (taken by mouth) medicine instead of skin lotion to treat scabies in older children.
The doctor might recommend an antihistamine or steroid cream, like hydrocortisone, to help with itching.
Can Scabies Be Prevented?
Household members and close contacts of someone being treated for scabies should get treated at the same time, even if they have no symptoms. This will help prevent the spread of scabies.
This will help prevent the spread of scabies.
Wash clothing, sheets, and towels in hot water and dry on a hot setting. Put stuffed animals and any other items you can't wash in a sealed plastic bag for at least 3 days. Vacuum each room in the house, then throw away the vacuum cleaner bag.
What Else Should I Know?
Most kids can return to school the day after treatment is complete.
Scratching the itchy areas of skin can let bacteria get into the skin. The doctor will prescribe antibiotics if your child gets a skin infection. Talk to your doctor if you notice any signs of skin infection, such as redness, swelling, or pus.
Reviewed by: Mary L. Gavin, MD
Date reviewed: October 2019
Pediatric Scabies | Children's National Hospital
What is scabies?
Scabies is an infestation of mites (tiny insects) characterized by small red bumps and intense itching. This highly contagious infection often spreads from person to person while they are sleeping together in the same bed or have close personal contact.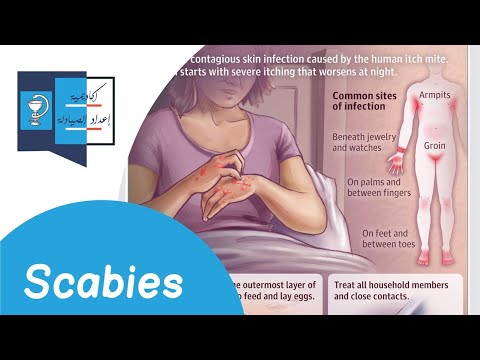
The itching is caused by the mites burrowing into the skin where they lay eggs that hatch a few days later. Scabies can affect people of all ages. Scabies occurs mostly in children and young adults.
What are the symptoms of scabies?
It may take between 4 to 6 weeks for a child to develop symptoms of scabies after coming in contact with an infected person.
In children younger than 2 years of age, the lesions caused by the mites tend to occur on the head, neck, palms, and soles. In older children, the lesions are usually between the fingers, on the hands or wrists, along the belt line, on the thighs or belly button, in the groin area, around the breasts, and in the armpits.
The following are the most common symptoms of scabies. However, each child may experience symptoms differently. Symptoms may include:
- Itching, usually severe
- Rash, with small pimples or red bumps
- Scaly or crusty skin (with advanced conditions)
How is scabies diagnosed?
In diagnosing scabies, the skin and skin crevices are examined by a physician.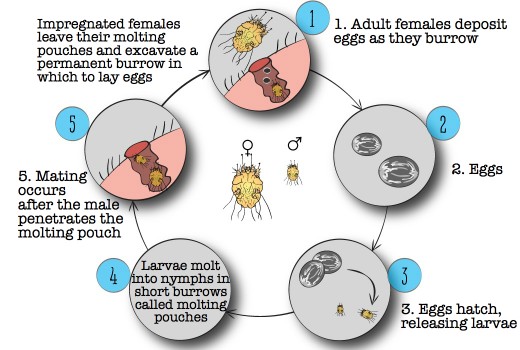 A sample of skin, obtained by scraping the skin, may be examined under a microscope to confirm the presence of mites.
A sample of skin, obtained by scraping the skin, may be examined under a microscope to confirm the presence of mites.
What is the treatment for scabies?
Scabies is treatable and usually all members in a family are treated at the same time. Specific treatment will be determined based on:
- The child's age, overall health, and medical history
- Extent of the infestation
- The child's tolerance for specific medications, procedures, or therapies
- Expectations for the course of the infestation
- Child or parent’s opinion or preference
Treatment may include:
- Applications of prescription creams and lotions, such as permethrin and lindane solutions
- Oral antihistamine medication (to help relieve itching)
- In some cases, topical ointments are recommended
In addition, it is important to wash all clothes and bedding in hot water and dry in a hot dryer in order to kill the mites. Clothing and other objects that cannot be washed (i.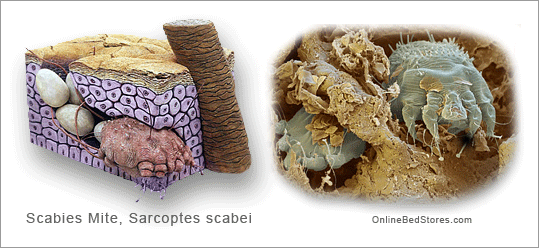 e., pillows, stuffed animals) should be placed in a plastic bag for at least one week.
e., pillows, stuffed animals) should be placed in a plastic bag for at least one week.
Also, the itching may continue for many weeks after the initial treatment of the scabies.
Children's Team Departments
Children's Team
Children's Team
Providers
Anna Kirkorian
Chief, DermatologyDermatologist
Colleen Cotton
DermatologistDepartments
Departments
Dermatology
The Division of Dermatology at Children's National Hospital continues to expand services as more families seek our expertise in the diagnosis and treatment of disorders of the skin, hair and nails.
Make an Appointment Find a ProviderInvest in future cures for some of life's most devastating diseases
$10 a month
One time donation
See other ways to give
Share your birthday with a child.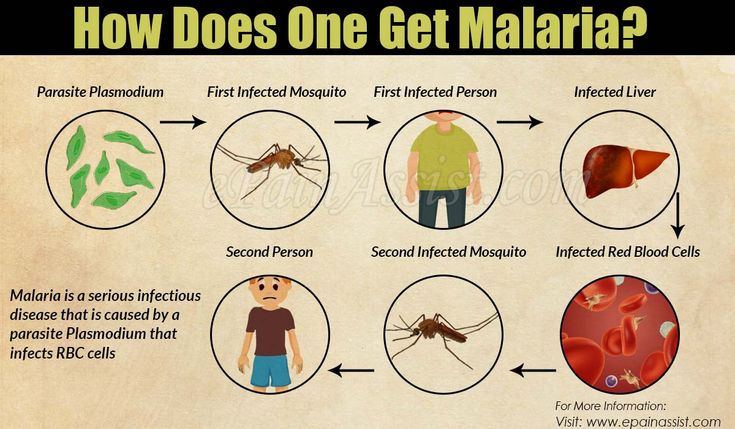 Celebrate your life, and give a chance to someone who desperately wants to have as many as you.
Celebrate your life, and give a chance to someone who desperately wants to have as many as you.
Make it happen
Xavion's Story
Sometimes a mom’s intuition is all it takes to get her child to the right physician. When 8-year-old Xavion Chisley developed a fungal infection on his toe, his mother, Nikki, immediately took him to see a dermatologist who removed his toenail to treat the infection. However, when Xavion’s toenail grew back, the infection had not diminished but actually appeared to be spreading to his foot.
Read More of Xavion's Story
Scabies in children - symptoms and treatment
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Video Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate safety of treatment
We have made children's medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Dermatology services
- Consultation of a pediatric dermatologist
Manipulations, procedures, operations
- Removal of papillomas in children
- Removal of warts in a child
- Removal of molluscum contagiosum in a child
- Phototherapy for the treatment of skin diseases
Frequent calls
- Treatment of atopic dermatitis in children
- Urticaria in children
- Seborrheic dermatitis in children
- Pink lichen in a child
- Ringworm in children
- eczema in a child
- herpes in a child
- Acne disease (acne) in adolescents
- molluscum contagiosum
- Treatment of childhood psoriasis
- Allergic dermatitis
- contact dermatitis
- pyoderma in a child
- Warts in a child
- Fungal infections in children
- Treatment of vitiligo in children
- Dermatoscopy
- Skin mapping
Online payment
Documents online
Online services
Scabies
Scabies- Healthcare issues »
- A
- B
- in
- g
- D 9005 and
- K
- L
- m
- H
- O
- P
- R
- T
- Ф
- 9003 900.
- 900 900 C
- 900 900 900 C
- 900 900 900 TU
- 9ATHER
- 9ATHER
- 9ATHER 900
- b
- s
- b
- e
- i
- i
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- U
- Ф
- x
- C
- h
- Sh
- С
- s
- 900 900 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/
- Scabies
N.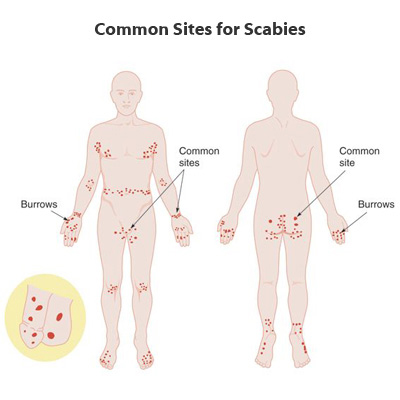 Lufanga
Lufanga
Baby suffering from Scabies in the United Republic of Tanzania.
© A photo
Basic facts
- An estimated 200 million people in the world are infected with scabies at any given time
- Up to 10% of children in under-resourced areas have scabies
- Human scabies is a parasitic infestation caused by Sarcoptes scabiei varhominis
- Scabies is distributed throughout the world, mainly in hot tropical countries and in areas with high population density
Human scabies is a parasitic infestation caused by Sarcoptes scabiei var hominis. The microscopic mite enters the skin and lays eggs, eventually triggering an immune response in the host that results in severe itching and a rash. Scabies can be exacerbated by bacterial infections leading to the development of skin ulcers, which in turn can lead to more severe complications such as sepsis, heart disease, and chronic kidney disease. In 2017, scabies and diseases caused by other ectoparasites were listed as neglected tropical diseases (NTDs) in response to requests from Member States and recommendations from the WHO Strategic and Technical Advisory Group on NTDs.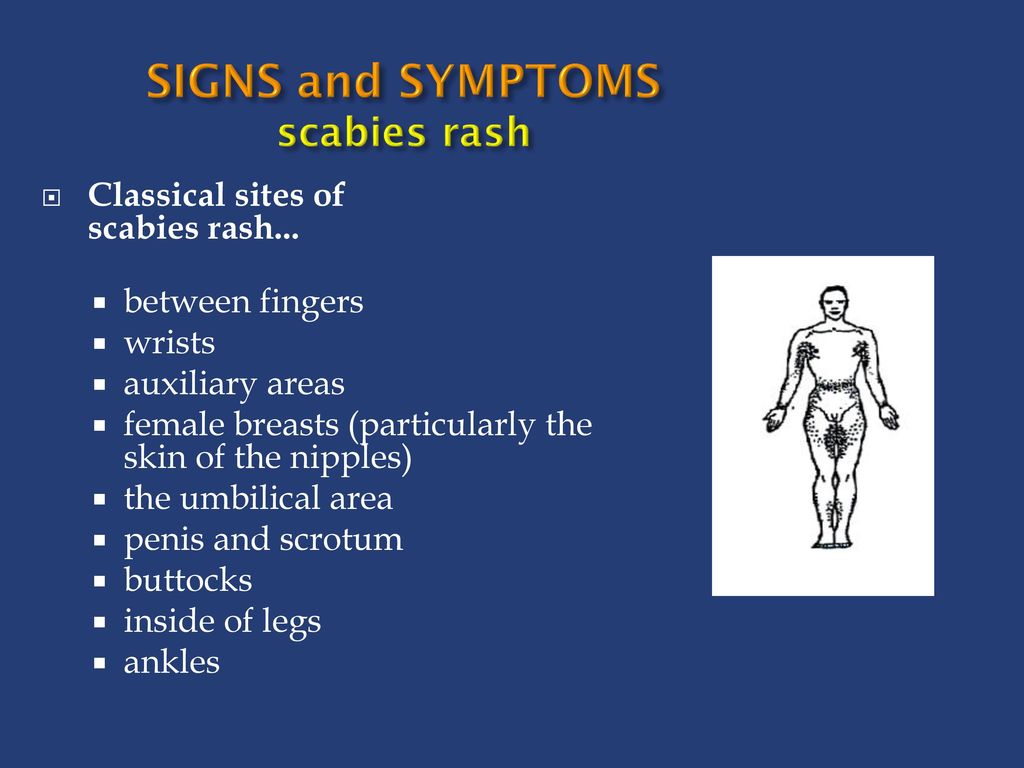
Magnitude of the problem
Scabies is one of the most common skin diseases and accounts for a significant proportion of skin diseases in developing countries. It is estimated that over 200 million people in the world are infected with scabies at any given time, but more work is needed to better estimate this burden. According to recent publications on scabies, prevalence rates range from 0.2% to 71%.
Scabies is endemic in many resource-limited tropical areas, where average prevalence rates in children are estimated to be 5-10%. Re-infections are widespread. The heavy burden of scabies and its complications comes at a high cost to health systems. Although isolated cases occur in high-income countries, outbreaks of scabies in health care settings and vulnerable communities result in significant economic costs to national health services.
Scabies is prevalent throughout the world, but the most vulnerable populations – young children and the elderly in under-resourced communities – are particularly susceptible to scabies infection and secondary complications. Infection rates are highest in countries with hot tropical climates, especially in communities where people live in conditions of overcrowding and poverty and access to treatment is limited.
Infection rates are highest in countries with hot tropical climates, especially in communities where people live in conditions of overcrowding and poverty and access to treatment is limited.
Symptoms
Scabies mites penetrate the top layer of the skin where adult females lay their eggs. After 3-4 days, larvae appear from the eggs, which develop into adult ticks in 1-2 weeks. After 4-6 weeks, the patient develops an allergic reaction to the proteins and feces of the mites in the scabies, which causes severe itching and a rash. Most people are infected with 10-15 mites.
Patients usually experience severe itching, and tick-like burrows and vesicles appear in the interdigital spaces, on the wrists, on the upper and lower extremities and in the lumbar region. In infants and young children, the rash may be more widespread and involve the palms, soles of the feet, ankles, and sometimes the scalp. Inflammatory scabies nodules can be found in adult men on the penis and scrotum, and in women in the mammary glands.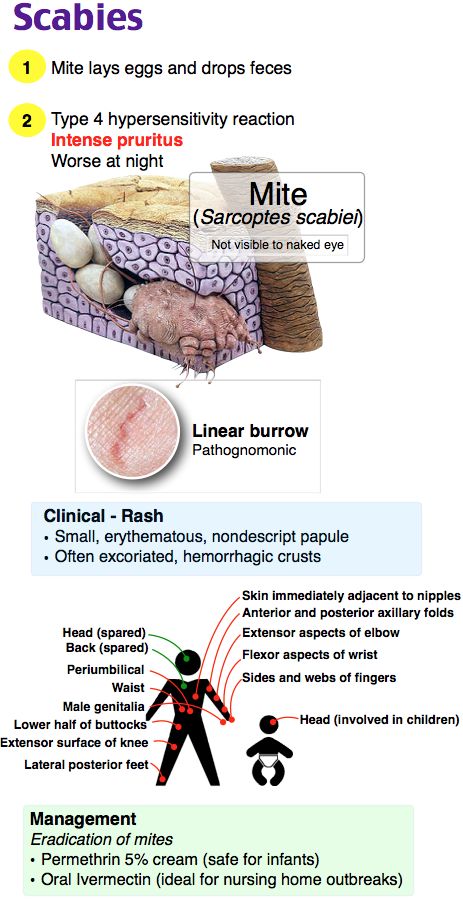 Due to the fact that symptoms develop some time after the initial infection, itch moves can be detected in people who have had close contact with an infected person who have not yet developed itching.
Due to the fact that symptoms develop some time after the initial infection, itch moves can be detected in people who have had close contact with an infected person who have not yet developed itching.
People with crusted scabies develop thick, scaly scabies on their skin that may spread more widely, including on the face.
Immunocompromised people, including people with HIV/AIDS, can develop a special form of the disease called crusted (Norwegian) scabies. Crusted scabies is a hyperinfection, in which the number of mites reaches several thousand and even millions. The mites spread widely and lead to crusting, but often do not cause significant itching. If left untreated, this disease is characterized by high mortality from secondary sepsis.
The effects of mites on the immune system, as well as the direct effects of scratching, can lead to bacterial infection of the skin, leading to the development of impetigo (skin ulcers), especially in tropical conditions. Impetigo may be complicated by deeper skin infections such as abscesses or severe invasive diseases, including sepsis. In tropical settings, skin infection associated with scabies is a common risk factor for kidney disease and possibly rheumatic heart disease. Signs of acute kidney injury can be found in up to 10% of scabies-infected children in under-resourced areas, and in many cases these symptoms persist for years after infection, leading to irreversible kidney damage.
In tropical settings, skin infection associated with scabies is a common risk factor for kidney disease and possibly rheumatic heart disease. Signs of acute kidney injury can be found in up to 10% of scabies-infected children in under-resourced areas, and in many cases these symptoms persist for years after infection, leading to irreversible kidney damage.
Transmission
Scabies is usually spread from person to person through close skin contact (eg, living together) with an infected person. The risk of transmission depends on the level of infection, with the highest risk coming from contact with individuals suffering from crusting scabies. The likelihood of transmission from contact with contaminated personal items (eg clothing and bedding) is low for common scabies, but high for crusted scabies. Given the asymptomatic period of infection, transmission may occur before symptoms appear in the initially infected person.
Treatment
Primary treatment of infected individuals includes the use of topical scabicides such as 5% permethrin, 0. 5% water-based malathion, 10-25% benzyl benzoate emulsion, or 5-10% Sulfuric ointment. Oral ivermectin is also highly effective and has been approved in several countries. The safety of ivermectin in pregnant women or children weighing less than 15 kg has not been established, so ivermectin should not be used in these populations until further safety data are available. With effective treatment within 1-2 weeks, pruritus usually increases, and persons undergoing treatment should be informed about this.
5% water-based malathion, 10-25% benzyl benzoate emulsion, or 5-10% Sulfuric ointment. Oral ivermectin is also highly effective and has been approved in several countries. The safety of ivermectin in pregnant women or children weighing less than 15 kg has not been established, so ivermectin should not be used in these populations until further safety data are available. With effective treatment within 1-2 weeks, pruritus usually increases, and persons undergoing treatment should be informed about this.
Since there may be no symptoms in the early stages of a new infection, and since scabies drugs do not kill parasite eggs, best results are achieved by treating all family members at the same time and re-treatment at the appropriate time for the drug chosen.
WHO activities
WHO is collaborating with Member States and partners to develop scabies control strategies and outbreak response plans. WHO recognizes that the burden of disease and the risk of long-term complications need to be better defined, and that scabies control strategies need to be linked to interventions to facilitate rapid and cost-effective implementation.