How to read panorama test results
Panorama Patient Information | Natera
Noninvasive prenatal testing (NIPT)
Panorama is a blood-based genetic, prenatal screening test of the pregnant person that screens for common chromosomal conditions that affect a baby’s health. Panorama uses SNP*-based technology to deliver highly accurate results and unique insights for both singleton and twin pregnancies
Panorama can be performed as early as nine weeks gestation. Most results will be returned to your doctor within 5-7 calendar days.
Panorama is a screening test, which means that this test does not make a final diagnosis. A high risk result means that your pregnancy has a higher chance of having a specific genetic condition. However, you cannot know for sure if your baby has that condition based upon the screening result alone. All medical decisions should be made after discussion with your healthcare provider regarding diagnostic testing during the pregnancy, like chorionic villus sampling (CVS) or amniocentesis, or testing the baby after birth.
*SNP, single nucleotide polymorphism
Personalized results
Panorama offers a personalized report, which indicates whether your baby has a high or low chance for certain genetic conditions. Your report could state the following:
Low Risk
A low risk result means that the chance that your baby has one of the conditions tested by Panorama is very unlikely but not zero — less than 1 in 10,000 for most conditions.1,3
High Risk
Panorama is a screening test, which means that this test does not make a final diagnosis. A high risk result means that your pregnancy has a higher chance of having a specific genetic condition. However, you cannot know for sure if your baby has that condition based on screening results alone.
If you receive a high risk Panorama result, speak with your healthcare provider (HCP) to discuss which next steps you could decide to do, such as genetic counseling, detailed ultrasound, and the option of diagnostic testing.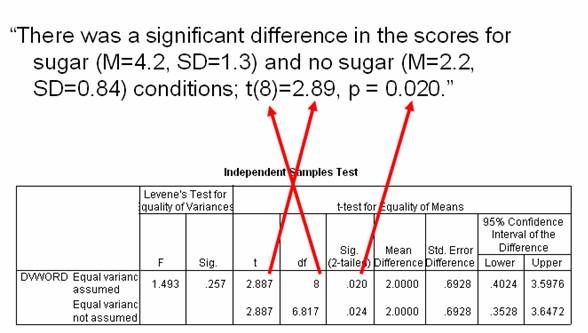
All medical decisions should be made after discussion with your HCP regarding diagnostic testing during the pregnancy, like chorionic villus sampling (CVS) or amniocentesis, or testing the baby after birth.
No Result
About 1 in 65 tests could receive a no result or other type of result.3 You should speak with your HCP about these result types and whether you should consider having a second blood draw to do the test again. There is also a small chance that Panorama will have a result relating to your genetics or your physical health.1
Complete Test Specifications for Singleton, Egg Donor, Gestational Carrier, and Monozygotic (Identical) Twins
Definition of performance terms
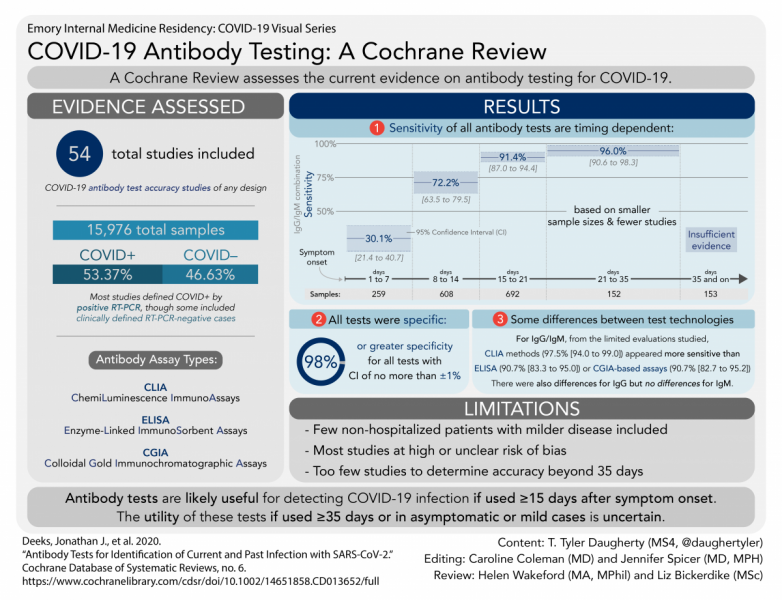
Sensitivity is the ability to correctly identify a truly high risk case as high risk. For example, in a group of Trisomy 21 cases, Panorama will correctly identify more than 99% of those cases.
Specificity is the ability to correctly identify an unaffected case as low risk.
Positive Predictive Value (PPV) is the likelihood the result says high risk and the fetus is actually affected. For example, when Panorama shows a high risk result for Trisomy 21, there is a 95% chance that the fetus is affected by Trisomy 21. In other words, 5% of the time, you could get a high risk result when the fetus is not affected by Trisomy 21.
Negative Predictive Value (NPV) is the likelihood the result says low risk and the fetus is truly not affected.
| Condition | Sensitivity (95% CI) | Specificity (95% CI) | PPV | NPV |
|---|---|---|---|---|
| Trisomy 21*3,5 | 99.0% (CI 97.1-100) | >99% (CI 99.93-99.99) | 95% | >99.99%‡ |
| Trisomy 18*3,5 | 94.1% (CI 82.9-100) | >99% (CI 99.96-100) | 91% | >99.99%‡ |
| Trisomy 13*3,5 | >99% (CI 73.5-100) | >99% (CI 99. 96-100) 96-100) | 68% | >99.99%‡ |
| Monosomy X**5-8 | 94.7% (CI 74.0-99.9) | >99% (CI 99.7-100) | 78% | >99.99%‡ |
| Triploidy**9,10 | >99% (CI 66.4-100) | >99% (CI 99.5-100) | 11% | >99.99%‡ |
| XXX, XXY, XYY**11 | 73.1% (CI 61.0-85.1) | 99.9% (CI 99.90-99.99) | 86.4% | 99.87%‡ |
| 22q11.2 deletion syndrome**12 | 83.3% (CI 51.6-97.9) | >99% (CI 99.91-99.98) | 53% | 99.9%||(CI 99.9-100) |
| 1p36 deletion syndrome**13,14 | >99% (CI 2.5-100) | >99% (CI 99.1-100) | 7-17%|| | 99.98-99.99%|| |
| Angelman syndrome**†13,14 | 95.5% (CI 77.2-99.9) | >99% (CI 99.1-100) | 10%§ | >99. 99% 99% |
| Cri-du-chat syndrome**13,14 | >99% (CI 85.8-100) | >99% (CI 99.1-100) | 2-5%|| | >99.99% |
| Prader-Willi syndrome**†13,14 | 93.8% (CI 69.8-99.8) | >99% (CI 99.1-100) | 5% | >99.99% |
| Female6,7,8 | >99.9% (CI 99.4-100) | >99.9% (CI 99.5-100) | ||
| Male6,7,8 | >99.9% (CI 99.5-100) | >99.9% (CI 99.4-100) |
Test Specifications for Dizygotic (Nonidentical) Twins
1| Condition | PPV | NPV |
|---|---|---|
| Trisomy 21 | 70% | >99.975% |
| Trisomy 18 | 50% | >99.999% |
| Trisomy 13 | 33% | >99.999% |
References
1Natera internal data on file
2Definitive Healthcare report to identify billing for NIPT based on US Clearinghouse for Medical Claims using CPT codes 81420, 81507, 81422.
3Dar et al. Am J Obstet Gynecol. 2022 Aug;227(2):259.e1-259.e14.
4ACOG Practice Bulletin 226. Obstet Gynecol. 2020 Oct;136(4):859-867.
5DiNonno et al. J Clin Med. 2019 Aug 26;8(9):1311.
6Nicolaides et al. Prenat Diagn. 2013 June;33(6):575-9.
7Pergament et al. Obstet Gynecol. 2014 Aug;124(2 Pt 1):210-8.
8Ryan et al. Fetal Diagn Ther. 2016;40(3):219-223.
9Nicolaides et al. Fetal Diagn Ther. 2014. 35;(3):212-7.
10Kantor et al. Prenat Diagn. 2022;42:994–999.
11Martin et al. 25th International Conference on Prenatal Diagnosis and Therapy Meeting; June 6-8, 2021.
12Dar et al. Am J Obstet Gynecol. 2022 Jul;227(1):79.e1-79.e11.
13Martin et al. Clin Genet. 2018 Feb;93(2):293-300.
14Wapner et al. Am J Obstet Gynecol. 2015 Mar;212(3):332.e1-9.
2015 Mar;212(3):332.e1-9.
Footnotes
* CA residents: If your clinician ordered screening through the California Prenatal Screening program using Natera's Vasistera™ NIPT, Panorama™ will only screen for supplemental conditions. If this is the case, trisomies 21, 18 and 13, and fetal sex (optional) will be screened using Vasistera™ NIPT and will be reported separately.
** Not available for egg-donor or gestational carrier pregnancies or in cases of dizygotic (nonidentical) twins. Triploidy and microdeletions except for 22q11.2 deletions are not available for monozygotic (identical) twins.
† This test has been validated on full region deletions of Prader-Willi syndrome/Angelman syndrome (PWS/AS) only and might be unable to detect smaller deletions. It has not been validated for other molecular mechanisms which could cause PWS/AS such as uniparental disomy (UPD) or methylation.
‡ Ongoing clinical follow-up is performed to ensure the NPV does not fall below the quoted value but follow up is not obtained for all low risk calls.
§ PPV for 22q11.2 deletion syndrome and Angelman syndrome in published studies was 53% and 10% respectively when no ultrasound anomalies were seen and was up to 100% when ultrasound anomalies were seen prior to testing.
|| Dependent upon fetal fraction (FF). For 22q11.2 deletion syndrome, only the paternal allele is evaluated at FF ≤ 6.5%. For 1p36 deletion syndrome and Cri-du-chat syndrome, only the paternal allele is evaluated at FF
How Can You Evaluate NIPT Performance?
Published Date
Last year, the American College of Obstetricians and Gynecologists (ACOG) updated its prenatal screening guidelines to recommend that all pregnant women should have access to noninvasive prenatal testing (NIPT), citing evidence that NIPT is the most accurate screening method for common aneuploidies. 1
1
Even in average risk pregnancies, NIPT utilization and the development of new NIPT technologies will likely continue to grow. As NIPT adoption increases, it is important that we have standards for evaluating NIPT performance across technologies to ensure that we are offering patients the best possible care through the highest-quality, most-reliable screens.
One key reporting variable for NIPT performance is positive predictive value (PPV). As PPV is applied as a tool to evaluate NIPT, it is becoming clear that PPV is a reliable metric of NIPT quality, and that it offers a means to evaluate NIPT performance across patient populations.2
What is PPV, and why is it important?
In the context of NIPT, PPV tells us how likely it is that someone with a positive NIPT test result truly has an affected pregnancy. In other words, PPV gives us an idea of the extent to which we can expect test results to match reality. For example, the Panorama NIPT has a PPV of 95% for trisomy 21, which means that if a patient tested with Panorama has a high-risk result for trisomy 21, there is approximately a 19 out of 20 chance that the baby has the chromosomal abnormality.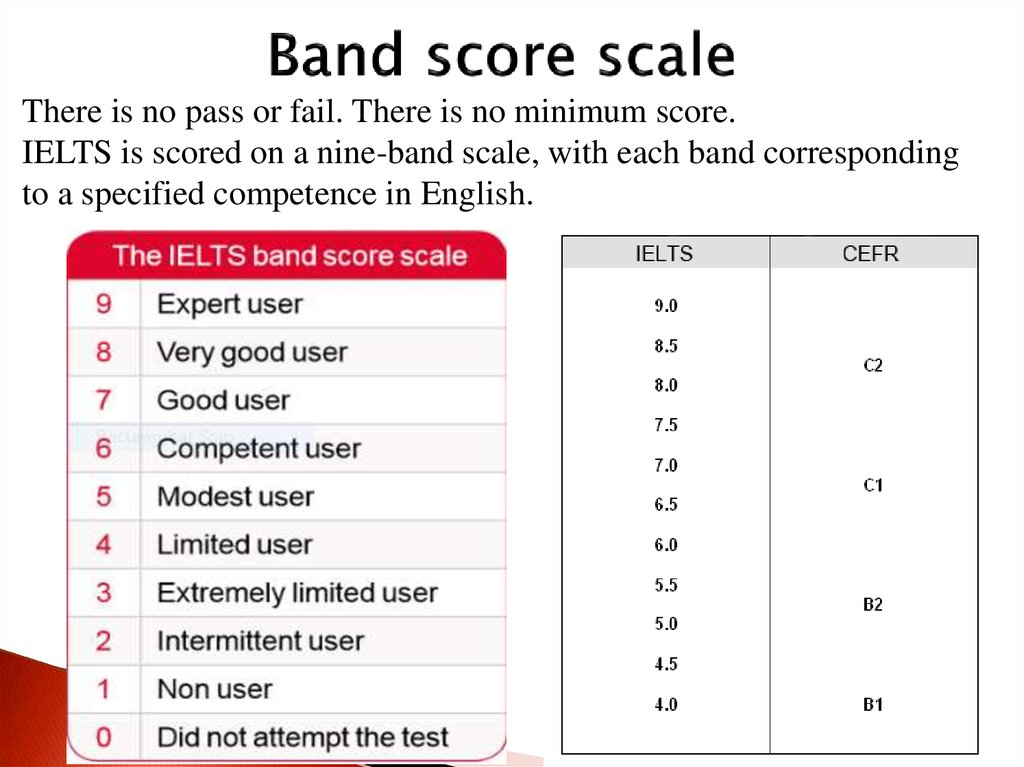 3
3
PPV can be calculated as true positives divided by the sum of true positives and false positives: true positives/(true positives + false positives)
A PPV calculation can be performed based on real-world data or analytical data, and the data type used affects the value and meaning of the calculated PPV. Panorama relies on clinical PPVs, rather than analytically determined PPV calculators or “personalized” PPVs, for several reasons, including that only clinical PPVs are derived from patient outcomes.
Clinical PPVs are based on clinical outcomes studies that occur in clinical practice. On the other hand, analytical PPV calculators extrapolate data from validation studies that could exclude important factors such as vanished twins or maternal chromosome abnormalities. Because these factors can alter a test’s specificity, if such factors are excluded, the PPVs could be overestimated.
Another advantage of clinical PPVs is that they can reflect the performance of complex algorithms for which simple analytical calculators cannot account. For example, the Panorama algorithm incorporates both maternal and gestational age into its aneuploidy risk assessment. Analytical PPV calculators cannot account for these factors, because they assume NIPT results are independent of prior risk. Therefore, it is inappropriate to use a Panorama result in a PPV calculator, because doing so would account for maternal age risk twice.
For example, the Panorama algorithm incorporates both maternal and gestational age into its aneuploidy risk assessment. Analytical PPV calculators cannot account for these factors, because they assume NIPT results are independent of prior risk. Therefore, it is inappropriate to use a Panorama result in a PPV calculator, because doing so would account for maternal age risk twice.
What do we know about NIPT PPVs?
The largest NIPT outcomes study to date provides some insight into the value of PPVs for assessing NIPT performance. The study cohort included more than 1 million patients, of which 13,231 (1.3%) were considered high-risk for common aneuploidies. The study analyzed the clinical performance of Panorama as part of a rigorous quality assurance program.2 Importantly, the results showed that PPV did not differ significantly for older versus younger populations, which is in contrast to the analytical PPVs of counting based tests.
Figure 1: Panorama trisomy 21 clinical PPVs are stable across age groups while “counting” NIPT analytical PPVs are much lower in younger women2–5
Figure 2: Panorama’s clinical PPVs for the common aneuploidies were comparable between average-risk and high-risk patients2
These high PPVs support broadening the use of SNP-based NIPT to younger women of average risk
Why is Panorama PPV stable at lower age groups?
Given the past concern that NIPT results would be significantly more reliable in older, higher risk women, resulting in a lower PPV in younger women, it is important to reflect on the observed stability of PPV in younger populations. Multiple potential explanations are possible.
Multiple potential explanations are possible.
For instance, Panorama’s SNP-based NIPT is associated with lower false positive rates than other NIPTs because Panorama can detect biological phenomena that are common causes of false positives in counting-based tests. These phenomena include vanishing twins and maternal chromosomal abnormalities.
Additionally, Panorama’s algorithm incorporates maternal age-based prior risk into its risk score. Younger women also could have lower false positive rates because of their lower risk of aneuploidy, and therefore lower risk of confined placental mosaicism, a known-source of NIPT false positives.1
PPV offers a way to evaluate NIPT technologies and establish performance standards
SNP-based NIPT has demonstrated consistent test performance in terms of sensitivity, specificity, and PPV. The newest data that show the stability of PPV across populations suggest that NIPT should be offered to all pregnant women, and that PPV can serve as a test quality assurance measure. We should therefore use clinical PPV to evaluate the performance of specific NIPT technologies and the value of NIPT for subpopulations of pregnant women.
We should therefore use clinical PPV to evaluate the performance of specific NIPT technologies and the value of NIPT for subpopulations of pregnant women.
Learn more about the only SNP-based NIPT, Panorama, here: https://www.natera.com/womens-health/panorama-nipt-prenatal-screening/
Natera is committed to helping women access Panorama and believes that the cost of your prenatal screening test bill should not be a barrier. If you have questions about what you might expect on your prenatal screening test bill, please contact the Natera billing phone number at 1-844-384-2996 (8 am-7 pm CT M-F) or visit the Natera billing page.
References
- Screening for Fetal Chromosomal Abnormalities. Obstetrics & Gynecology. 2020;136(4):859-867. doi:10.1097/AOG.0000000000004107
- DiNonno W, Demko Z, Martin K, et al. Quality Assurance of Non-Invasive Prenatal Screening (NIPS) for Fetal Aneuploidy Using Positive Predictive Values as Outcome Measures.
 Journal of Clinical Medicine. 2019;8(9):1311. doi:10.3390/jcm8091311
Journal of Clinical Medicine. 2019;8(9):1311. doi:10.3390/jcm8091311 - Myriad Women’s Health website accessed Oct 23 2019.
- Progenity Innatal Clinician Guide.
- Natera internal data on file.
Panorama, non-invasive prenatal test (extended panel
To conduct the study, it is necessary to provide the results of ultrasound diagnostics (ultrasound).
"Panorama", a non-invasive prenatal test (extended panel - diagnosis of aneuploidy + microdeletions) - is the most modern method for diagnosing fetal chromosomal pathologies, which is used in many countries around the world. Its advantages over other diagnostic methods are accuracy and safety. This test allows with an accuracy of 99.9% determine the chromosomal pathology of the fetus during pregnancy according to the most common syndromes. The method is based on the isolation of freely circulating fetal DNA in the mother's blood.
The advantage of the Panorama non-invasive prenatal test over invasive diagnostics is that the analysis requires only the collection of venous blood from the mother and is completely safe for mother and child. You receive accurate and complete information about the course of your pregnancy without risk.
Panorama non-invasive prenatal test, diagnosis of aneuploidy + microdeletion is performed for pregnant women from 9th week.
Chromosomes are carriers of hereditary information that are present in all cells of the human body. The human genome consists of 46 chromosomes or 23 pairs.
Aneuploidy is a phenomenon in which the number of chromosomes in a cell changes up or down from normal.
Microdeletions are the loss of small sections of chromosomes. Some microdeletions cause specific genetic syndromes and can have a significant impact on a child's physical health and mental capacity. The risk of microdeletions is observed in 1 case out of 1000 newborns. Microdeletions can lead to serious mental and physical impairments. All pregnancies are at the same risk of microdeletions regardless of the age of the mother.
Microdeletions can lead to serious mental and physical impairments. All pregnancies are at the same risk of microdeletions regardless of the age of the mother.
Non-invasive prenatal test "Panorama", diagnostics of aneuploidy + microdeletions reveals:
- all possible types of fetal aneuploidies: Down syndrome, Edwards syndrome, Patau syndrome;
- pathologies of sex chromosomes: Klinefelter's syndrome, X-chromosome trisomy, X-chromosome monosomy (Turner's syndrome), XXY syndrome;
- microdeletion syndromes: DiGeorge Syndrome, Angelman Syndrome, Cat's Cry Syndrome, Prader-Willi Syndrome.
Indications:
- increased risk of chromosomal abnormalities on biochemical screening;
- chromosomal pathology in previous pregnancies;
- the age of the pregnant woman is over 35;
- the threat of termination of pregnancy in the early stages;
- the desire of a pregnant woman.
Currently, the use of the Panorama test does not make sense in only a few cases:
- if you have a multiple pregnancy;
- if you have used someone else's egg or are a surrogate mother;
- if you have had a bone marrow transplant;
- reduction of one embryo from twins according to the results of an ultrasound examination.
Before taking the study, a doctor's consultation is required.
Interpretation of results
What results can I get after the non-invasive prenatal test "Panorama", diagnosis of aneuploidy + microdeletions?
Although most pregnancies end in the birth of healthy children, any woman is not immune from the fact that her child will be born with a chromosomal disease. The Panorama screening test allows you to assess such a risk and prepare for it in advance.
After receiving the test result, you will receive the following information:
Low risk
A low risk result indicates that it is unlikely that your child has the pathology listed in the report. However, it is worth noting that a low risk result does not guarantee a 100% healthy pregnancy, as an accurate diagnosis can only be achieved using invasive methods.
However, it is worth noting that a low risk result does not guarantee a 100% healthy pregnancy, as an accurate diagnosis can only be achieved using invasive methods.
High risk
A high risk score does not mean that the child is diagnosed with a pathology, rather, it means that the chance of having a chromosomal abnormality is higher than average. Your healthcare provider may refer you to a genetics specialist for professional advice, or you can check your Panorama test results using invasive diagnostic methods.
No result
In a small percentage of cases, the Panorama test is unable to detect genetic material in a blood sample. In this case, it is necessary to do a second blood sampling.
The Panorama test, along with other screening methods, may show a high risk result when your baby is healthy (false positive) or may not detect chromosomal abnormality (false negative). Therefore, it is very important to discuss the test results with your healthcare provider for further medical guidance.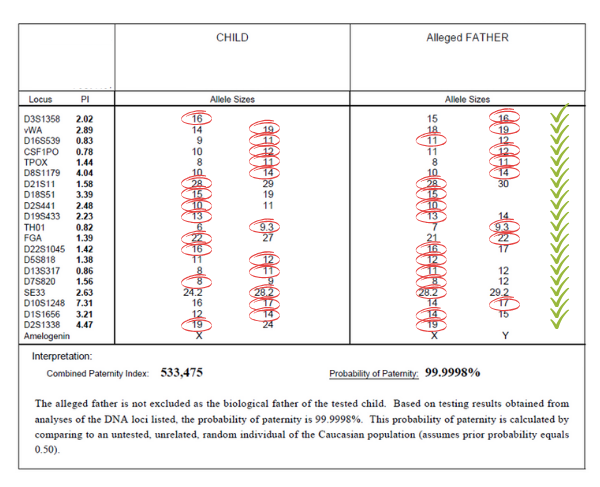
Simultaneously with the "Panorama" test, it is possible to determine the carriage of mutations in the mother, leading to frequent hereditary diseases.
Despite the high accuracy, this test is a screening research method. If a chromosomal abnormality is detected in the fetus, confirmation of the test results using invasive diagnostics is required.
The test is NOT taken on an empty stomach.
20 minutes before taking the biomaterial, you must eat a chocolate bar or drink orange juice.
Panorama test, Down syndrome, Edwards syndrome and Patau syndrome
The Panorama test is a non-invasive, prenatal, safe and accurate screening test for chromosomal diseases based on the study of fetal extracellular DNA in the mother's blood, which can be performed from the ninth week of pregnancy.
The Panorama test recognizes 99% of fetuses with Down syndrome, Edwards syndrome and Patau syndrome and 92% of fetuses with Turner syndrome.
Although the test is very accurate, Panorama is not a diagnostic test, so in the case of a positive Panorama test, an invasive examination is necessary to clarify the diagnosis (chorionic biopsy or amniotic fluid test). Loote Ultraheliskriining is collaborating with the Tallinn Genetics Center on invasive research.
The Panorama test is completely safe for both you and your fetus, and the test does not endanger the pregnancy in any way. The screening test is performed from your venous blood.
Panorama test is indicated for women at risk *:
- Pregnant age 35 years at the time of delivery
- Increased risk of chromosomal pathology on fetal ultrasound
- Screening test of the first or second semester of a pregnant woman found an increased risk of chromosomal diseases
- Down syndrome during a previous pregnancy
- Balanced Robertsonian translocation in parents due to increased risk of Down syndrome or Patau syndrome.
This test is also used:
- Hereditary X-linked diseases in the family (to determine the sex of the fetus).
- Test sensitivity >99%.
Benefits of Panorama over other non-invasive screening tests:
- High disease detection
- Low false positive rate
- Also indicates the risk of Patau syndrome and Turner syndrome
- Gives an opportunity to estimate the sex of the fetus
Panorama test not performed:
- If the child's NT (occipital translucency) is greater than 3.0 mm
- In case of multiple pregnancy
- In case of twin pregnancy, if one of the fetuses died
- In case of IVF pregnancy with donor egg
- If the pregnant woman had a bone marrow transplant before pregnancy
If the body mass index (BMI) of the pregnant woman is above 30 kg/m 2 , there is a danger that the blood test has so little fetal extracellular DNA that a scraping from the father's mucosa will be needed to ensure an accurate diagnosis. There is also a small chance that no result will come from your initial sample. In this case, we advise you to take a second venous blood test, in which case no additional fee is required.
There is also a small chance that no result will come from your initial sample. In this case, we advise you to take a second venous blood test, in which case no additional fee is required.
Since the Panorama test cannot assess fetal anatomy, neural tube pathology, risk of congenital heart disease, preeclampsia in pregnancy, fetal growth retardation and preterm birth, Loote Ultraheliskriining offers the OSCAR test as one part of the Panorama test, where the analysis maternal blood is done preferably at 10 weeks of gestation and ultrasound at 12 weeks of gestation. The results of the combined study, together with a detailed explanation of the test, will be received by the family immediately after the ultrasound examination.
In case of increased NT ( nuchal translucency ) > 3.5 mm and euploid chromosome set, Loote Ultraheliskriining cooperates with the Tallinn Genetics Center in carrying out a genetic test based on the APEX method ( adrenogenital prime5 extension 902 syndrome, Noonan syndrome, Smith-Lemli-Opitz syndrome, spinal muscular atrophy) and in performing FISH (fluorescence in situ hybridization) analysis to detect 22q11.