Delivering twins vaginally
Giving birth to twins | Pregnancy Birth and Baby
Twins are more likely to be born early, often before 38 weeks, so it's important to understand your birth options. Less than half of all twin pregnancies last beyond 37 weeks.
Because of the likelihood that your babies will be born early, there is a good chance one or both of them will spend some time in special care.
As twins are often born prematurely, it's a good idea to discuss birth options with your midwife or doctor early in your pregnancy.
You should also discuss where you would like to give birth. You will most likely be advised to give birth in a hospital because there's a higher chance of complications with a twin birth.
It's common for more medical staff to be involved in the birth of twins, such as a midwife, an obstetrician and two paediatricians - one for each baby.
While the process of labour is the same as when single babies are born, twin babies are more closely monitored. To do this, an electronic monitor and a scalp clip might be fitted on the first baby once your waters have broken. You will be given a drip in case it is needed later.
Vaginal birth
About one third of all twins are born vaginally and the process is similar to that of giving birth to a single baby. If you're planning a vaginal delivery, it's usually recommended that you have an epidural for pain relief. This is because, if there are problems, it's easier and quicker to assist the delivery when the mother already has good pain relief.
If the first twin is in a head down position (cephalic), it's usual to consider having a vaginal birth. However, there may be other medical reasons why this would not be possible. If you have had a previous caesarean section, it's usually not recommended you have a vaginal birth with twins.
If you have a vaginal birth, you may need an assisted birth, which is when a suction cup (ventouse) or forceps are used to help deliver the babies.
Once the first baby is born, the midwife or doctor will check the position of the second baby by feeling your abdomen and doing a vaginal examination. If the second baby is in a good position, the waters will be broken and this baby should be born soon after the first as the cervix is already fully dilated. If contractions stop after the first birth, hormones will be added to the drip to restart them.
If the second baby is in a good position, the waters will be broken and this baby should be born soon after the first as the cervix is already fully dilated. If contractions stop after the first birth, hormones will be added to the drip to restart them.
Caesarean section
You may choose to have an elective caesarean from the outset of your pregnancy, or your doctor may recommend a caesarean section later in the pregnancy as a result of potential complications. You’re nearly twice as likely to have a caesarean if you’re giving birth to twins than if you’re giving birth to a single baby.
The babies' position may determine whether they need to be delivered by caesarean section or not. If the presenting baby - the one that will be born first - is in a breech position (feet, knees or buttocks first), or if one twin is lying in a transverse position (with its body lying sideways), you will need to have a caesarean section.
Some conditions also mean you will need a caesarean section; for example if you have placenta praevia (a low-lying placenta) or if your twins share a placenta.
If you have previously had a very difficult delivery with a single baby, you may be advised to have a caesarean section with twins. Even if you plan a vaginal birth, you may end up having an emergency caesarean section.
This could be because:
- one or both babies become distressed
- the umbilical cord prolapses (falls into the birth canal ahead of the baby)
- your blood pressure is going up
- the labour is progressing too slowly
- assisted delivery doesn't work
In very rare cases, you may deliver one twin vaginally and then require a caesarean section to deliver the second twin if it becomes distressed.
After the birth
After the birth, your midwife will examine the placenta to determine what type of twins you have. Twins can either be fraternal or identical.
If your babies need special care
Depending on where you plan to give birth, you may need to go to another hospital with appropriate facilities if complications in your pregnancy indicate you're likely to have an early delivery. This may not be near to home, so make sure to check there are enough beds for both your babies in the neonatal unit.
This may not be near to home, so make sure to check there are enough beds for both your babies in the neonatal unit.
Ask if your chosen hospital has a transitional care unit or a special care nursery. These are places that allow mothers to care for their babies if they need special care but not intensive care. These hospitals are more likely to be able to keep you and your babies in the same place.
You might also want to ask if your hospital has cots that allow co-bedding (where your babies sleep in a single cot), if this is appropriate and if you want your babies to sleep together.
If you have one baby in the hospital and one at home, you will need to think about splitting your time between the two. When you visit your baby in hospital, ask if you can bring their twin and if co-bedding is allowed during visits.
If you want to breastfeed and only one twin can feed effectively, you may need to express milk to feed the twin who is having trouble feeding. You may then need to put the twin who can feed on the breast to encourage milk production in order to get enough milk to feed both babies.
Check if your hospital offers support from a community neonatal nurse, which would allow for you and your babies to leave hospital earlier, for example if your baby is still tube-fed.
When you go to clinics for follow-up appointments, it's a good idea to ask not to be booked into early morning appointments. Getting out of the house with two babies, particularly if one is unwell, can be difficult.
For more information and support, visit Twins Research Australia.
Learn more here about the development and quality assurance of healthdirect content.
Giving birth to twins or more
It's important to understand your birth options if you're expecting more than 1 baby.
Twins and triplets are more likely to be born early and need special care after birth than single babies.
Your birth choices with twins
It's a good idea to discuss your birth options with your midwife or consultant early on in your pregnancy.
You'll normally be advised to give birth in a hospital, as there's a higher chance of complications with twins.
There are usually more health professionals at a multiple birth – for example, there may be 2 midwives, an obstetrician and 2 paediatricians (1 for each baby).
For more information on who's who, read about the antenatal team.
The process of labour is more or less the same as for 1 baby, but your maternity team will usually advise you to have your babies electronically monitored because of the higher risk of complications.
This means attaching belts with sensors (1 for each twin) to your bump. You'll still be able to move around into different positions.
Once your waters have broken, your midwife may ask your permission to attach a clip attached to a wire to the first baby's head to get a more accurate measure of their heartbeat.
You'll be offered a drip in case it's needed later – for example, to restart contractions after your first baby is born.
Triplets or more babies are almost always delivered by a planned caesarean section.
Can you have a natural birth with twins?
Lots of women think they have to have a caesarean section with twins, but in fact, many twin births are vaginal
If you're planning a vaginal delivery, it's usually recommended that you have an epidural for pain relief, but you can discuss this with your midwife.
If there are any problems, it's easier for your antenatal team to deliver your babies quickly if you have already got an epidural in place.
Find out more about the signs and stages of labour
You're more likely to have a vaginal birth if the first twin is in a head-down position.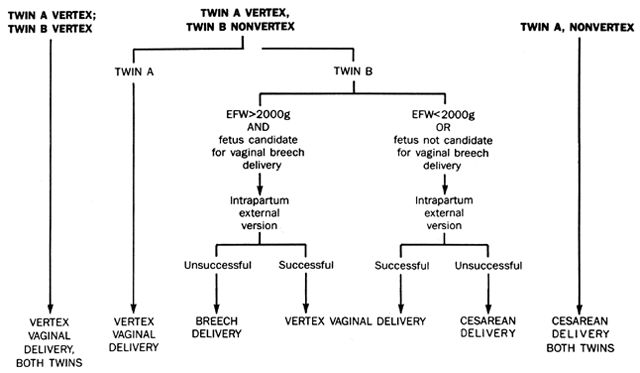
But there may be medical reasons why a vaginal birth is not recommended.
If you have had a caesarean section before, for example, it's not usually recommended that you have a vaginal birth with twins.
As with any vaginal birth, you may need an assisted birth. This is where forceps or vacuum delivery are used to help deliver your babies.
Once the first baby is born, your midwife or doctor can check the position of the second baby by feeling your tummy and doing a vaginal examination. They may also use an ultrasound scan.
If the second baby is in a good position, it should be born soon after the first, as your cervix is already fully dilated.
If your contractions stop after the first baby is born, the doctor or midwife may discuss giving you hormones via a drip to restart them.
Caesarean section and twins
In the UK, more than half of twins and almost all triplets are delivered by caesarean section is a common method used during twin and triplet births.
You may choose to have a planned caesarean, or your doctor may recommend a caesarean, if:
- the first baby is lying feet, knees or buttocks first (breech)
- 1 twin is lying sideways (transverse)
- you have a low-lying placenta
- your twins share a placenta
- you have had a difficult delivery with a single baby before
As with any pregnancy, if you plan a vaginal birth, you may still end up needing an emergency caesarean.
In a small number of cases, some women deliver 1 twin vaginally and then need a caesarean section to deliver the second twin.
Video: how can my twin or multiple births be managed?
In this video, a midwife explains what can happen when giving birth to more than 1 baby.
Media last reviewed: 1 November 2019
Media review due: 2 November 2022
Page last reviewed: 31 October 2022
Next review due: 31 October 2025
Vaginal delivery is safer than caesarean section for twin births vaginal delivery of twins is associated with a lower incidence of adverse outcomes for children than caesarean section.
 They believe that this method of delivery should be considered as a priority, especially if the first twin is in cephalic presentation. The findings are presented in the journal Obstetrics & Gynecology.
They believe that this method of delivery should be considered as a priority, especially if the first twin is in cephalic presentation. The findings are presented in the journal Obstetrics & Gynecology. In the course of the work, scientists analyzed data obtained in a large national observational cohort study, which was conducted in France from February 10, 2014 to March 1, 2015. Its participants were 5915 women who gave birth to twins after the 32nd week of gestation, and the first their twin was in head presentation. Of these, 1454 (24.6%) had a caesarean section planned (mean age 32.8±5.8 years), and 4461 (75.4%) had vaginal delivery (mean age 31.4±5.1 years). of the year). The former were distinguished by greater body weight, frequent caesarean section and complications during pregnancy in history. Ultimately, 61% of women delivered vaginally, including 25 (1.7%) women who were scheduled for caesarean section.
The primary clinical outcomes analyzed by the scientists were the incidence of neonatal death during childbirth and during the first 28 days of life, as well as their condition at the level of <4 points on the Apgar scale at the 5th minute of life, the development of neurological or respiratory complications after childbirth. Such outcomes were noted in 5.2% of children born during caesarean section and in 2.2% of newborns after vaginal delivery (relative risk (RR) 2.38; 95% confidence interval (CI) 1.86–3.05 ). To control for potential differences influencing OR found between women planning different methods of delivery, the authors conducted a comparative analysis of 2288 women in labor (1144 from each group). Cumulative neonatal morbidity and mortality among newborns whose mothers underwent caesarean section was 5.3%, and among infants born during vaginal delivery - 3.0% (RR 1.85; 95% CI 1.29–2.67). The most common cause of neonatal death in both groups was multiple malformations and genetic disorders.
Such outcomes were noted in 5.2% of children born during caesarean section and in 2.2% of newborns after vaginal delivery (relative risk (RR) 2.38; 95% confidence interval (CI) 1.86–3.05 ). To control for potential differences influencing OR found between women planning different methods of delivery, the authors conducted a comparative analysis of 2288 women in labor (1144 from each group). Cumulative neonatal morbidity and mortality among newborns whose mothers underwent caesarean section was 5.3%, and among infants born during vaginal delivery - 3.0% (RR 1.85; 95% CI 1.29–2.67). The most common cause of neonatal death in both groups was multiple malformations and genetic disorders.
In another subgroup that excluded women with complicated pregnancies, researchers analyzed outcomes in 564 (14.2%) women who had an elective caesarean section and 3410 (84.8%) women who had a vaginal delivery. When analyzing the gestational age of newborns, the researchers noted that an increased risk of adverse outcomes with caesarean section was observed only when children were born before reaching the 35th week of gestation. In the course of a thorough analysis of the history of childbirth of women who are not included in high-risk groups, the authors of the work did not reveal a statistically significant relationship between caesarean section and the likelihood of primary negative outcomes.
In the course of a thorough analysis of the history of childbirth of women who are not included in high-risk groups, the authors of the work did not reveal a statistically significant relationship between caesarean section and the likelihood of primary negative outcomes.
Based on the results obtained, according to scientists, two important conclusions can be drawn. First, when twins are born, one of which is in cephalic presentation, vaginal delivery is associated with a low risk of neonatal morbidity and mortality. Secondly, elective caesarean section is associated with a high risk of neonatal morbidity and mortality only among twins born before the 37th week of gestation, with the most common complication being the development of respiratory distress syndrome.
Author Dr. Thomas Schmitz noted that in multiple pregnancies, planned vaginal delivery at 32–37 weeks' gestation should be preferred over caesarean section. These results are consistent with the recommendations of experts from the American College of Obstetricians and Gynecologists (ACOG). He emphasized that reducing the prevalence of operative delivery is not only achievable for women in labor, but also safer for newborns. So, currently in the United States, 75% of twins are born by caesarean section. Reducing this figure to 50% will help almost 17,000 women a year avoid surgery, which may be unsafe both for themselves and for their children.
He emphasized that reducing the prevalence of operative delivery is not only achievable for women in labor, but also safer for newborns. So, currently in the United States, 75% of twins are born by caesarean section. Reducing this figure to 50% will help almost 17,000 women a year avoid surgery, which may be unsafe both for themselves and for their children.
Yuliya Kotikovich
Elective caesarean section for twin pregnancies
There is considerable variation in the prevalence of twins in different communities and families, and there has been an increase in the number of older mothers, as well as the use of infertility treatments and artificial insemination . Infants with twin pregnancies are at a higher risk of death during childbirth and in the immediate peripartum period than infants with single pregnancies. This occurs in some cases due to a higher risk of preterm birth. The second-born twin has an increased risk of adverse perinatal outcomes compared to the first-born twin.
The policy of planned vaginal delivery in women with twin pregnancies in hospital is associated with an emergency caesarean section rate of 30% to 40%. When the first twin is born vaginally (naturally), there is still a risk of an emergency caesarean section (surgery) to deliver the second twin. It is possible that some of the adverse effects can be avoided with timely delivery by caesarean section, but the risks of caesarean section for the mother in this (current, delivery) and subsequent pregnancies must be considered.
In this review, we included two randomized trials comparing planned caesarean section and planned vaginal birth in twin pregnant women, with a total of 2864 participants. For important outcomes, the evidence was rated as moderate (moderate) quality evidence.
Maternal mortality: there were no events reported in one of the trials and there were two deaths (one in each of the compared groups) in the other trial. There was no clear evidence of a difference in death or serious illness for both mothers and infants between women randomized to elective caesarean delivery or planned vaginal delivery.