How do you get cmv during pregnancy
Cytomegalovirus (CMV) during pregnancy | Pregnancy Birth and Baby
Cytomegalovirus (CMV) during pregnancy | Pregnancy Birth and Baby beginning of content8-minute read
Listen
Key facts
- CMV is a common virus that often doesn’t cause any symptoms, but it can cause health problems for your baby if you catch it for the first time when you’re pregnant.
- CMV is spread through body fluids. It can appear in urine and saliva for years after you’ve been infected.
- People who have young children or work in childcare centres are at higher risk of catching CMV.
- Most unborn babies who are infected with CMV won’t have any problems, but some have poor hearing and vision, developmental delay and intellectual disability.
- The best way to prevent CMV is by good hygiene, especially handwashing after contact with any body fluids.
What is CMV?
Cytomegalovirus (CMV) is a virus that is especially common in adolescents and children under 2 years of age. It often doesn’t cause any obvious symptoms, so you may not know you’ve been infected. About 1 in 2 people have had CMV by the time they become adults.
After you first become infected, CMV stays in your body and becomes inactive. It can become active again at times when your immune system is weaker than usual, such as when you’re pregnant.
It’s possible for an unborn baby to become infected with CMV. This can sometimes cause serious problems.
How does CMV spread?
CMV is transmitted from person to person through contact with body fluids, such as saliva, nasal mucus, urine, vaginal discharge, semen and breast milk. It can be spread by coughing and sneezing and by contact with objects that have body fluids on them. It’s also possible to get CMV from having sex, a blood transfusion or an organ transplant. Babies can become infected with CMV during breastfeeding.
It’s also possible to get CMV from having sex, a blood transfusion or an organ transplant. Babies can become infected with CMV during breastfeeding.
If a child has had CMV, the virus can continue to appear in their urine and saliva for years afterwards and can infect other people who haven’t had CMV. Some people get CMV while they’re pregnant. This can happen through contact with toys, tissues or nappies used by children who have had CMV. People with young children at home and people who work in childcare centres are at higher risk of catching CMV if they haven’t had it before.
How do I know if I have CMV?
CMV usually doesn't cause any noticeable symptoms. However, in some people, it can cause mild symptoms such as fever, swollen glands, tiredness, sore throat and a cough. Sometimes it can cause mild liver inflammation. These symptoms usually go away by themselves.
CMV can cause serious illness in people with a weak immune system, for example people with HIV or who are having chemotherapy for cancer.
Most people don’t know they have CMV infection, or if they have had it before. You might find out from a blood test that you’ve had it.
Could I give CMV to my baby?
If you have CMV when you’re pregnant, the virus can travel across the placenta and infect your baby. This is called congenital CMV.
This can happen if:
- it’s the first time you’ve been infected with CMV (this is called primary infection)
- you’ve had CMV before and the virus in your body becomes active again (this is called reactivation)
- you get infected with a different strain of CMV than you’ve had before
You are more likely to pass the virus on to your baby if you have a primary CMV infection during pregnancy. CMV can spread to your baby at any stage of pregnancy, but risk is higher in the first half of pregnancy.
How does CMV affect unborn babies?
Most babies born with CMV don’t have symptoms or health problems as a result of the virus, but some do. Your baby is more likely to be affected if it’s the first time you’ve been infected with CMV. Your doctor might see signs of congenital CMV on a pregnancy ultrasound.
Your baby is more likely to be affected if it’s the first time you’ve been infected with CMV. Your doctor might see signs of congenital CMV on a pregnancy ultrasound.
About 3 in 10 people who get CMV for the first time in pregnancy will pass it on to their baby. About 1 in 10 of these babies will be born with symptoms. In total, about 1 or 2 out of every 10 babies infected with CMV during pregnancy will have a long-term health problem.
If your baby is born with symptoms of congenital CMV, these may include:
- rash
- small head size
- enlarged liver and spleen
- pneumonia
- low platelet count
Congenital CMV also increases your baby’s risk of poor growth, miscarriage, stillbirth and death before 3 months of age.
If your baby is born without symptoms, there’s a chance they could develop health problems later. These may include:
- poor hearing – this is the most common problem
- poor vision
- intellectual impairment
- developmental delay
- cerebral palsy
- seizures
Babies who are born without any symptoms or hearing loss have a lower chance of problems.
Should I be tested for CMV?
There is a blood test for CMV, but in Australia it’s not routinely done in pregnancy. CMV testing in pregnancy is recommended for:
- people who develop symptoms of a viral infection suggestive of CMV
- people who come into frequent contact with young children (such as child care workers)
- people who know they have been exposed to someone with a new CMV infection
- people who have had a pregnancy ultrasound that shows signs of congenital CMV
You can check with your doctor if you need to test for CMV. If you have a test that shows that you have CMV, you may need further testing to see if your baby has CMV. It’s important to remember that even if your baby tests positive for CMV, this doesn’t always mean they will have health problems.
If you have CMV during pregnancy, your baby will need to be tested for CMV after birth. Babies who have an abnormal hearing test after birth may also be tested for CMV.
You can talk to your doctor about CMV testing if you have concerns.
If I get CMV during pregnancy, can my baby be treated?
Some treatments have been tried, but currently there’s no treatment that clearly lowers the risk of your baby getting CMV from you. It’s best to discuss this with your doctor.
Your baby will need to have hearing tests and eye checks for a few years to see if any problems develop.
Can I prevent getting CMV?
The best way to try to avoid infection with CMV is by practising good hygiene.
If you are pregnant, it is a good idea to:
- regularly and thoroughly wash your hands with soap and water, particularly when feeding and caring for children, changing nappies, wiping noses or handling anything with body fluids on it
- regularly clean surfaces and objects that may have body fluids on them
- wear gloves when changing nappies
- avoid contact with children’s saliva and don’t kiss them on the lips
- avoid sharing food, cups, utensils, or toothbrushes
There is no vaccine to prevent CMV infection.
If you have any concerns, you can discuss them with your doctor or midwife.
Sources:
NSW Health (Cytomegalovirus (CMV) and pregnancy fact sheet), Australasian Society for Infectious Diseases (Management of perinatal infections), Australian Government Department of Health (Cytomegalovirus), Sydney Children’s Hospitals Network (Cytomegalovirus), SA Health (Cytomegalovirus (CMV) infection - including symptoms treatment and prevention)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Guide to a healthy pregnancy
Need more information?
Cytomegalovirus (CMV)
Cytomegalovirus (CMV)
Read more on Queensland Health website
Cytomegalovirus (CMV) and pregnancy fact sheet - Fact sheets
Cytomegalovirus (CMV) and pregnancy factsheet
Read more on NSW Health website
Cytomegalovirus (CMV) infection | SA Health
Cytomegalovirus (CMV) infection in children and adults is usually without symptoms but the infection is thought to remain for life
Read more on SA Health website
Cytomegalovirus (CMV) | Sydney Children's Hospitals Network
What is cytomegalovirus (CMV)? Cytomegalovirus or CMV means "big cell virus" because cells grow big when infected
Read more on Sydney Children's Hospitals Network website
Cytomegalovirus (CMV) - Better Health Channel
If an unborn baby gets CMV from their mother, it can cause hearing loss and intellectual disability.
Read more on Better Health Channel website
Reduce your risk of CMV infection in pregnancy | Cerebral Palsy Alliance
Cytomegalovirus (CMV) is a common virus. When healthy people are infected they frequently have no symptoms.
Read more on Cerebral Palsy Alliance website
Cytomegalovirus | Australian Government Department of Health and Aged Care
Cytomegalovirus is the most common infectious cause and the second most common overall cause of congenital malformation in Australia. However, there is limited evidence to support universal testing of pregnant women for cytomegalovirus. As cytomegalovirus may be transmitted to the baby and can have
Read more on Department of Health and Aged Care website
Ways infectious diseases spread | SA Health
How infectious diseases spread including via air, personal contact, soiled objects, skin, mucous membranes, saliva, urine, blood, sexual contact, food and water
Read more on SA Health website
A guide to blood tests in pregnancy | Know Pathology Know Healthcare
The following guide outlines the different pathology tests available throughout each trimester, and the purpose of your prenatal blood tests.
Read more on Know Pathology Know Healthcare website
Having a small baby
It's normal for parents to worry about their baby's birth weight and growth. Here’s what you need to know if you have been told your baby is likely to be small (less than 2.5kg at birth).
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.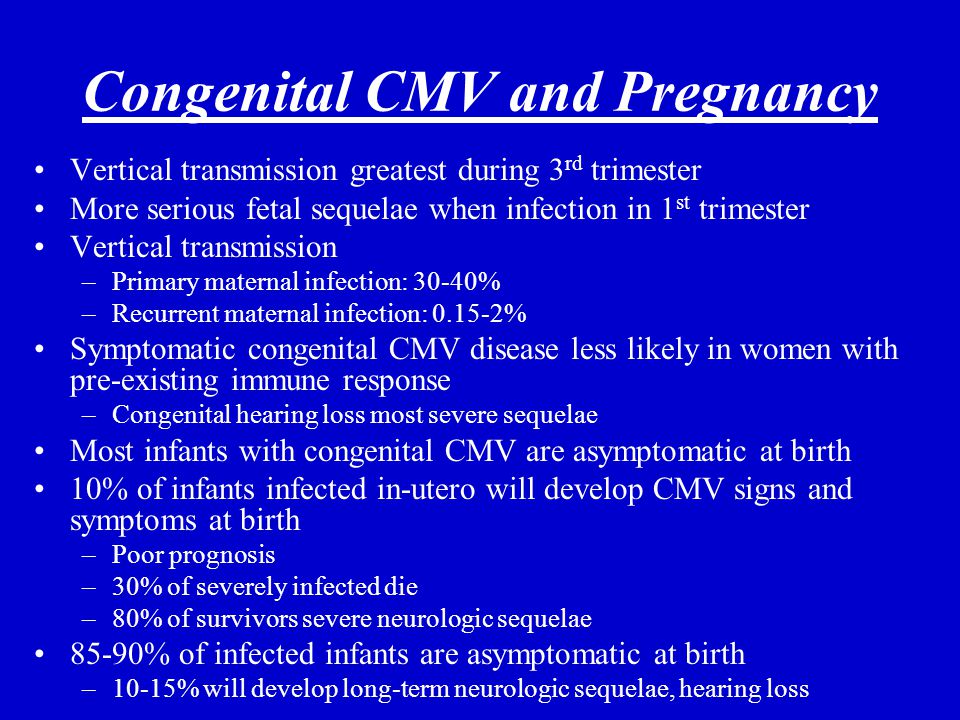
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
CMV Fact Sheet for Pregnant Women and Parents
Español (Spanish)
Most people have been infected with cytomegalovirus (CMV), but do not have symptoms. If a pregnant woman is infected with CMV, she can pass it to her developing baby. This is called congenital CMV, and it can cause birth defects and other health problems.
For pregnant women
You can pass CMV to your baby
If you are pregnant and have CMV, the virus in your blood can cross through your placenta and infect your developing baby. This is more likely to happen if you have a frst-time CMV infection while pregnant but can also happen if you have a subsequent infection during pregnancy.
You are not likely to be tested for CMV
It is not recommended that doctors routinely test pregnant women for CMV infection. This is because laboratory tests cannot predict which developing babies will become infected with CMV or have long-term health problems.
You may be able to reduce your risk
You may be able to lessen your risk of getting CMV by reducing contact with saliva and urine from babies and young children. The saliva and urine of children with CMV have high amounts of the virus. You can avoid getting a child’s saliva in your mouth by, for example, not sharing food, utensils, or cups with a child. Also, you should wash your hands after changing diapers. These cannot eliminate your risk of getting CMV, but may lessen the chances of getting it.
Also, you should wash your hands after changing diapers. These cannot eliminate your risk of getting CMV, but may lessen the chances of getting it.
For parents
About 1 out of every 200 babies is born with congenital CMV. About 1 out of 5 of these babies will have birth defects or other long-term health problems.
Babies with congenital CMV may show signs at birth
Some signs that a baby might have congenital CMV infection when they are born are:
- Small head size
- Seizures
- Rash
- Liver, spleen, and lung problems
Tests on a baby’s saliva, urine, or blood done within two to three weeks after birth can confirm if the baby has congenital CMV.
Early treatment may help
Babies who show signs of congenital CMV at birth may be treated with medicines called antivirals. Antivirals may decrease the severity of health problems and hearing loss but should be used with caution due to side effects.
Long-term health problems may occur
Babies with signs of congenital CMV at birth are more likely to have long-term health problems, such as:
- hearing loss
- intellectual disability
- vision loss
- seizures
- lack of coordination or weakness
Some babies with congenital CMV but without signs of disease at birth may still have or develop hearing loss. Hearing loss may be present at birth or may develop later in babies who passed their newborn hearing test. Sometimes, hearing loss worsens with age.
Hearing checks and therapies are recommended
Children with congenital CMV should have regular hearing checks. Children with hearing loss should receive services such as speech or occupational therapy. These services help ensure they develop language, social, and communication skills.
The earlier your child can get hearing checks and therapies, the more he or she can benefit from them.
Download the print version and share pdf icon[1 page]
Diagnosis and treatment of cytomegalovirus during pregnancy H-Clinic blog CMV treatment
Diagnosis and treatment of cytomegalovirus during pregnancy H-Clinic blog CMV treatment
04/15/2020
Cytomegalovirus (CMV) is one of the members of the herpes virus family (it also includes the causative agents of herpes simplex, chickenpox, Epstein-Barr virus). The first contact with the virus most often occurs in childhood, and most adults have antibodies to it. Like many viruses of this family, CMV has the ability to persist for life in the body's cellular reservoirs, usually without causing any symptoms, since the immune system does not allow the virus to multiply uncontrollably. However, cytomegalovirus during pregnancy can be reactivated from reservoir cells against the background of a physiological decrease in immune function in a pregnant woman. This can lead to serious fetal developmental disorders such as:
This can lead to serious fetal developmental disorders such as:
• lack of hearing;
• decreased vision or blindness;
• hepatitis and jaundice;
• microcephaly;
• decrease in the level of platelets;
• learning difficulties;
• epilepsy.
Cytomegalovirus in pregnant women is especially dangerous for the fetus if the woman has not previously been in contact with the virus, does not have immunity to it, and became infected with CMV during the current pregnancy or shortly before its onset.
This can be checked by testing for antibodies to the virus. During pregnancy, monitoring is carried out for the so-called TORCH complex (this is an analysis for infections that can be transmitted from mother to fetus during pregnancy and cause developmental disorders in the child: toxoplasma, rubella, cytomegalovirus and herpes). It is optimal to pass this analysis even before the onset of the planned pregnancy to assess possible risks.
Upon contact of the body with any pathogen (be it a bacterium, virus or helminth), at least two types of antibodies can be produced in the blood: antibodies of the IgM class and antibodies of the IgG class. The former are an "immediate" reaction of the human immune system to the entry of a foreign organism and usually indicate a recent infection. The second type of antibodies is aimed at the final suppression of the disease and the maintenance of immunity for a long time (sometimes for life).
Thus, if IgG antibodies are detected before pregnancy, and IgM antibodies give a negative result, this indicates that your body has previously encountered the virus, has a certain level of immune protection, and the risk of re-infection is very small. If the test for IgG is negative, then additional precautions are necessary. In the practice of monitoring a pregnant woman, PCR tests of blood and urine for CMV infection are also widely used. All women are shown mandatory screening for cytomegalovirus during pregnancy. The timing and order of the examination are determined by the doctor.
The timing and order of the examination are determined by the doctor.
How is CMV transmitted?
CMV is usually transmitted through close contact with a person who already has the virus in their body and sheds it into the environment. The virus can spread through saliva, blood, urine, seminal fluid, breastfeeding. CMV can only be transmitted from a person whose virus is in an "active" state and is excreted in bodily fluids. This happens, for example, if:
• a person contracted the virus for the first time: children often transmit the virus to each other through close contact in kindergarten;
• the virus "reactivated": began to multiply uncontrollably after a certain time after the initial infection. This occurs as a result of a significant weakening of the immune system;
• if reinfection (re-infection) has occurred: the person has become infected with another subtype of CMV.
Thus, the source of infection can most often be children, in whom, after the first contact with the infection, the virus actively multiplies in the body for some time, sometimes causing symptoms like acute respiratory infections, and sometimes completely asymptomatic. In the "risk zone" are pregnant women who work with children or already have children.
In the "risk zone" are pregnant women who work with children or already have children.
How to prevent infection?
It is impossible to completely prevent infection: a CMV vaccine has not yet been developed. But during pregnancy, you can reduce your risk by doing the following:
• Wash your hands regularly with warm water and soap, especially if you've changed your baby's diapers or work in day care;
• do not kiss small children on the lips or cheek: it is better to kiss them on the top of their head or just hug them;
• do not finish eating after the child, do not use the same utensils with him;
• Do not lick baby's pacifiers.
How to cure an infection?
In the event that a planned screening examination nevertheless revealed signs of infection or reactivation of an infection in a pregnant woman, further tactics of treatment and management of pregnancy are determined by the doctor together with the woman, taking into account the risks of infection of the fetus. Sometimes invasive diagnostic interventions (such as amniocentesis) may be required.
Sometimes invasive diagnostic interventions (such as amniocentesis) may be required.
The following drugs are registered in Russia for the treatment of cytomegalovirus infection: ganciclovir and valganciclovir. Foscarnet and cidofovir are also used abroad. All of these drugs have a direct antiviral effect. However, possible effects on the fetus limit the use of some of them during pregnancy. There are studies showing the efficacy and safety of hyperimmune globulin G (that is, a drug containing antibodies to the virus) in preventing transmission to the fetus. The choice of treatment tactics, therapy regimens is determined by the attending physician, based on a number of data: laboratory test results, gestational age, etc. As for drugs that indirectly affect the immune system (panavir, isoprinosine, viferon), their effectiveness in the prevention of congenital CMV infection has not been proven.
Diagnosis and treatment of cytomegalovirus during pregnancy is a complex task, which usually requires the simultaneous participation of an experienced obstetrician-gynecologist and an infectious disease specialist.
Author: infectious disease specialist at the H-Clinic Degtyareva Svetlana Yurievna .
Medical editor: Head of the University Clinic, Candidate of Medical Sciences, infectious disease specialist Konnov Danila Sergeevich .
You can also read about cytomegalovirus in our article CYTOMEGALOVIRUS TREATMENT .
Return to the list
Asked by - Irina, - question-answer from the specialists of the clinic "Mother and Child"
gestational age 23 weeks, age 31, first pregnancy. on the 9th week - October 20, an analysis was taken for cytomegalovirus-antibody Ig G detected - the number was not indicated, the avidity index was 50 (in decoding - primary infection, on Wednesday 3-5 months ago, if the avidity index was more than 50 percent, then in decoding these are highly avid bodies), from the 3rd week of pregnancy, the subfebrile temperature of 37.2 lasted more than 5 weeks, the throat hurt (plugs, white plaque), severe runny nose, pulling pains in the muscles of the legs, ached eyes. herpes popped up on the lip. at 11 weeks, the analysis for CMV was again passed, the result of Ig G 10me \ ml-immunocab (positive from 1 me \ lm), Ig M-not detected, two weeks later, the result of which cytomegalovirus-anti was tested for control Ig G bodies were detected, the avidity index was already 62%. I did not donate blood before pregnancy, I did it by PCR (scraping of the cervical canal epithelium) on June 24, DNA was not detected. Streptococcus genus was found in a normal throat culture molytic grade 3, at first they wanted to prescribe antibiotics but sent for a blood test, it wasn’t found there, she was treated with bioparox, nothing was found on the next smear. Then, on November 25, blood was donated - immunoglobulin M to CMV was not detected, avidity 62 percent, December 12 - avidity 74 percent, M-negative. On December 27, I was tested in another laboratory for CMV-Ig M-not detected, Ig G 100, avidity index for CMV-99 percent. From January 16, smears were taken - scraping of the epithelium of the cervical canal, DNA of the pathogen, the result of a PCR study - CMV - DNA was not detected, Herpes type 1 and 2 DNA was not detected, and in the blood by the Ifa method of January 27, CMV-Ig M-not detected, Ig G 140, Herpes simplex virus 1,2 type Ig M-not detected, Ig Gk HSV 1 type 100, HSV 2 type Ig G not detected, avidity to HSV-98.
herpes popped up on the lip. at 11 weeks, the analysis for CMV was again passed, the result of Ig G 10me \ ml-immunocab (positive from 1 me \ lm), Ig M-not detected, two weeks later, the result of which cytomegalovirus-anti was tested for control Ig G bodies were detected, the avidity index was already 62%. I did not donate blood before pregnancy, I did it by PCR (scraping of the cervical canal epithelium) on June 24, DNA was not detected. Streptococcus genus was found in a normal throat culture molytic grade 3, at first they wanted to prescribe antibiotics but sent for a blood test, it wasn’t found there, she was treated with bioparox, nothing was found on the next smear. Then, on November 25, blood was donated - immunoglobulin M to CMV was not detected, avidity 62 percent, December 12 - avidity 74 percent, M-negative. On December 27, I was tested in another laboratory for CMV-Ig M-not detected, Ig G 100, avidity index for CMV-99 percent. From January 16, smears were taken - scraping of the epithelium of the cervical canal, DNA of the pathogen, the result of a PCR study - CMV - DNA was not detected, Herpes type 1 and 2 DNA was not detected, and in the blood by the Ifa method of January 27, CMV-Ig M-not detected, Ig G 140, Herpes simplex virus 1,2 type Ig M-not detected, Ig Gk HSV 1 type 100, HSV 2 type Ig G not detected, avidity to HSV-98. 9%. tell me, please, they didn’t take blood from me by PCR for CMV, I just now asked the doctor, on the advice of a laboratory assistant, who said that CMV and herpes can be a cross reaction. If I now donate blood by PCR for CMV, then a positive result will indicate an acute process? and how long the M titers to CMV are in the blood, which indicate an acute process. I also know that a fourfold increase in G indicates an acute process, but I can’t compare the analysis from November and December, and the doctor does not answer anything. I’m going to do it at 24 weeks ultrasound, afp at 17 weeks below the norm - 0.6 mom, norm 20.9-59.9 I have 17.8 beta hcg and free estriol is normal.
9%. tell me, please, they didn’t take blood from me by PCR for CMV, I just now asked the doctor, on the advice of a laboratory assistant, who said that CMV and herpes can be a cross reaction. If I now donate blood by PCR for CMV, then a positive result will indicate an acute process? and how long the M titers to CMV are in the blood, which indicate an acute process. I also know that a fourfold increase in G indicates an acute process, but I can’t compare the analysis from November and December, and the doctor does not answer anything. I’m going to do it at 24 weeks ultrasound, afp at 17 weeks below the norm - 0.6 mom, norm 20.9-59.9 I have 17.8 beta hcg and free estriol is normal.
MD GROUP Clinical Hospital:
01/26/2021
Virus carriers are not yet sick. The vast majority of people do not even know that they are infected. Infection and real disease are by no means the same thing. IgM antibodies may indicate either a primary infection or an exacerbation of a chronic infection. The presence of specific. IgM increase shortly after the onset of the disease, reach a peak by 1-4 weeks, exist in the blood for 30-60 days after the initial infection with the virus, and then disappear. You have never had IgM during pregnancy, apparently there was no exacerbation of the infection, or there was no acute process, but it is possible that you had CMV infection immediately before pregnancy. IgG are determined a little later (not earlier than 2 weeks after the onset of the disease), their levels rise more slowly than IgM, but they also remain much longer (for some infections, throughout life). An increase in the level of IgG suggests that the body has already met with this infection. If you are pregnant and have positive IgG antibodies against cytomegalovirus, then the chance of transmitting the virus from you to the fetus is negligible if you did not become infected with CMV in the months preceding pregnancy. In your case, this is likely (clinical manifestations at the beginning of pregnancy, low-avid IgG antibodies).
The presence of specific. IgM increase shortly after the onset of the disease, reach a peak by 1-4 weeks, exist in the blood for 30-60 days after the initial infection with the virus, and then disappear. You have never had IgM during pregnancy, apparently there was no exacerbation of the infection, or there was no acute process, but it is possible that you had CMV infection immediately before pregnancy. IgG are determined a little later (not earlier than 2 weeks after the onset of the disease), their levels rise more slowly than IgM, but they also remain much longer (for some infections, throughout life). An increase in the level of IgG suggests that the body has already met with this infection. If you are pregnant and have positive IgG antibodies against cytomegalovirus, then the chance of transmitting the virus from you to the fetus is negligible if you did not become infected with CMV in the months preceding pregnancy. In your case, this is likely (clinical manifestations at the beginning of pregnancy, low-avid IgG antibodies).