How long does it take to make sperm
How Long Does It Take for Sperm to Regenerate? Tips for Production
How Long Does It Take for Sperm to Regenerate? Tips for ProductionMedically reviewed by Janet Brito, Ph.D., LCSW, CST — By Tim Jewell on September 19, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
How long does it take?
You produce sperm every day, but a full sperm regeneration cycle (spermatogenesis) takes about 64 days.
Spermatogenesis is the complete cycle of sperm production and maturation. It constantly supplies your body with sperm able to travel through the vagina to an unfertilized ovum in a woman’s ovaries to conceive.
Read on to learn more about how often your body replenishes your sperm, what happens in your body to make sperm production possible, how you can help keep your sperm healthy, and more.
What’s the rate of sperm production?
Your testicles are constantly producing new sperm in spermatogenesis. The full process takes about 64 days.
During spermatogenesis, your testicles make several million sperm per day — about 1,500 per second. By the end of a full sperm production cycle, you can regenerate up to 8 billion sperm.
This may seem like overkill, but you release anywhere from 20 to 300 million sperm cells in a single milliliter of semen. Your body maintains a surplus to ensure there’s a fresh supply for conception.
What’s the cycle for sperm production?
The sperm regeneration cycle includes:
1. The division of diploid sperm cells into haploid spermatids that can carry genetic data.
2. The maturation of sperm in your testicles, specifically in the seminiferous tubules. Hormones help spermatids through this process until they become spermatozoa. Sperm then remain in the testicles until they’re almost mature.
A mature sperm has a head containing genetic material and a tail to help the sperm travel through the female body for fertilization.
3. The movement of sperm into the epididymis, a tube connected to your testicles that stores sperm. The epididymis preserves sperm until ejaculation. This is also where sperm gain motility, or the ability to move. This enables them to travel when released in seminal fluid (semen) during ejaculation.
What does this mean for me?
Fertilization is most likely when you haven’t ejaculated in a while. Constant sperm regeneration fills the epididymis with fresh sperm. The longer they build up, the higher your sperm count in a single ejaculation.
If you and your partner are trying to conceive, waiting a few days between ejaculations can increase your chances of conception.
You can further increase your chances by abstaining from ejaculation the week before your partner ovulates. This will maximize your sperm count during your partner’s most fertile window.
On the other hand, more frequent ejaculations can lower your sperm count in a single ejaculation. This can help you avoid getting your partner pregnant, especially if you abstain from sex until after ovulation ends.
This can help you avoid getting your partner pregnant, especially if you abstain from sex until after ovulation ends.
How to improve sperm health
The healthier your sperm are, the more likely you are to be fertile and conceive.
Aside from quantity, or how many of them you produce, sperm health is measured by:
- Sperm movement (motility).Sperm need to travel through a woman’s cervix, uterus, and fallopian tubes before they get to the ovum for fertilization. Motility is measured by how many sperm are moving — if you’re fertile, at least 40 percent of your sperm are motile.
- Sperm shape (morphology). Spermshould have long tails and oval-shaped heads. A higher count of normal-shaped sperm means a higher chance of conceiving with your partner.
Try the following to help make sure that your sperm are being produced in high enough quantities, as well as with high motility and regular shapes:
- Exercise regularly.
 Researchers in one 2014 study analyzed 433 semen samples from 231 participants. They found that men who did outdoor activities or lifted weights for about 3.2 hours a week had sperm counts up to 42 percent higher than men who didn’t exercise at all.
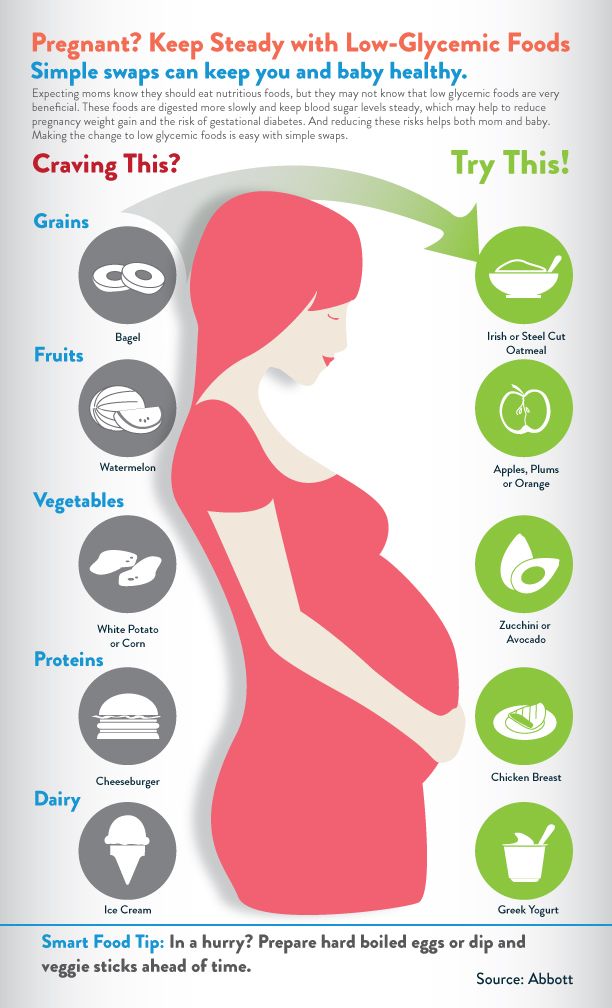
Researchers in one 2014 study analyzed 433 semen samples from 231 participants. They found that men who did outdoor activities or lifted weights for about 3.2 hours a week had sperm counts up to 42 percent higher than men who didn’t exercise at all. - Get enough vitamin C and D in your diet. A 2016 study of 200 men found that men who lost weight and took 1,000 milligrams (mg) of vitamin C supplements every other day saw an increase in sperm count and motility. This effect was more noticeable as the men lost weight. A 2015 study of 102 couples showed that female partners of men with normal levels of vitamin D in their blood samples experienced higher pregnancy rates than partners of men with vitamin D deficiency, despite no substantial differences in their sperm count or motility.
- Get enough lycopene. A 2014 study suggests that consuming 4 to 8 mg of lycopene daily can help increase sperm count and viability, or the amount of sperm living in a given sample of semen.
 Lycopene is an antioxidant found in many fruits and vegetables.
Lycopene is an antioxidant found in many fruits and vegetables. - Limit how much you smoke. A 2015 review of 33 studies dating back to 1982 found that smoking had a noticeable effect on semen quality and sperm function, especially in normally fertile men.
- Limit your alcohol intake. A 2014 study of 1,221 men found that the more the men drank, the more they produced irregularly shaped sperm. The researchers also noted a link between drinking and low testosterone, which can also affect fertility.
- Wear loose-fitting underwear and clothing. Your testicles hang away from your body so that they remain 35 to 37°C (95 to 98.6°F), which is cooler than your body temperature. This is the optimal environment for sperm production. Wearing tight underwear, jeans, or pants pushes your testicles against your body and raises their temperature, which can cause sperm to lose motility and viability.
How to increase you and your partner’s chance of conception
If you and your partner are trying to conceive, you may want to:
- Have sex two to three times a week to increase your chances of releasing many healthy sperm.

- Wait two to three days between sessions to make sure that you release the largest possible number of sperm in the highest possible volume of semen. For this to work, you’ll need to abstain from masturbation on “off” days.
- Use an ovulation predictor kit to test the levels of luteinizing hormone (LH) in your partner’s urine. LH levels go up right before ovulation. If your partner receives a positive result, have sex the day they took the test. Having sex for the next couple of days may also increase your chance of conceiving.
- Don’t use oil-based lubricants while you’re trying to conceive. They can have a negative effect on sperm health.
- See your doctor for a semen analysisif you’ve been trying to conceive for over six months. Your sperm health depends on many factors, including your age, diet, and overall sperm count. Your doctor can determine how healthy your sperm are and whether conception is possible, as well as advise you on next steps.
The bottom line
Your body produces fresh sperm every day, and your sperm supply gets replenished at least every 64 days. This ensures that a sufficient supply of sperm is available at any given time.
Sperm quality and quantity are affected by your diet and lifestyle. Eat well, stay active, and avoid unhealthy behaviors to keep your sperm as healthy as possible.
Last medically reviewed on September 19, 2018
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Dell’Amore C. (2010). How a man produces 1,500 sperm a second.
news.nationalgeographic.com/news/2010/03/100318-men-sperm-1500-stem-cells-second-male-birth-control/ - Durairajanayagam D, et al.
 (2014). Lycopene and male infertility. DOI:
(2014). Lycopene and male infertility. DOI:
10.4103/1008-682X.126384 - Durairajanayagam D, et al. (2015). Sperm biology from production to ejaculation. DOI:
10.1007/978-1-4939-2140-9_5 - Gaskins AJ, et al. (2014). Paternal physical and sedentary activities in relation to semen quality and reproductive outcomes among couples from a fertility center. DOI:
10.1093/humrep/deu212 - Harlev A, et al. (2015). Smoking and male infertility: An evidence-based review. DOI:
10.5534/wjmh.2015.33.3.143 - Jensen TK, et al. (2014). Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones: A cross-sectional study among 1221 young Danish men. DOI:
10.1136/bmjopen-2014-005462 - Kumar N, et al. (2015). Trends of male factor infertility, an important cause of infertility: A review of the literature. DOI:
10.4103/0974-1208.170370 - Leahy, M.
 & MacQueen, H. (2011). The science of sperm.
& MacQueen, H. (2011). The science of sperm.
open.edu/openlearn/body-mind/health/health-sciences/the-science-sperm - Mayo Clinic Staff. (2018). Healthy sperm: Improving your fertility.
mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/fertility/art-20047584?pg=2 - Mayo Clinic Staff. (2018). Low sperm count.
mayoclinic.org/diseases-conditions/low-sperm-count/symptoms-causes/syc-20374585 - Rafiee B, et al. (2016). Comparing the effectiveness of dietary vitamin C and exercise interventions on fertility parameters in normal obese men.
ncbi.nlm.nih.gov/pubmed/27085565 - Sabeti, P., et al. (2016). Etiologies of sperm oxidative stress.
ncbi.nlm.nih.gov/pmc/articles/PMC4918773/ - Sandhu RS, et al. (2014). In vitro effects of coital lubricants and synthetic and natural oils on sperm motility. DOI:
10.1016/j.fertnstert.2013.12.024 - Spermatogenesis.
 (2017).
(2017).
soc.ucsb.edu/sexinfo/article/spermatogenesis - Tartagni M, et al. (2015). Males with low serum levels of vitamin D have lower pregnancy rates when ovulation induction and timed intercourse are used as a treatment for infertile couples: Results from a pilot study. DOI:
10.1186/s12958-015-0126-9 - Trost L. (2018). Abnormal sperm morphology: What does it mean?
mayoclinic.org/diseases-conditions/male-infertility/expert-answers/sperm-morphology/faq-20057760
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Sep 19, 2018
Written By
Tim Jewell
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Janet Brito, PhD, LCSW, CST
Share this article
Medically reviewed by Janet Brito, Ph.D., LCSW, CST — By Tim Jewell on September 19, 2018
Read this next
How Long Can Sperm Survive After Ejaculation?
Medically reviewed by Justin Choi, MD
How long can sperm live outside the body? Which sperm and pregnancy myths are true and which are false? Many factors, including environment, your…
READ MORE
How Is Sperm Produced?
Medically reviewed by Stacy Sampson, D.
 O.
O.As the male reproductive cell, sperm is a key aspect of human fertility. In this article, you’ll find a brief overview of the male reproductive system…
READ MORE
How Long Does It Take to Get Pregnant?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Getting pregnant can take longer than expected. Many couples also struggle with infertility. Learn how long it typically takes to conceive after sex…
READ MORE
How Does Sperm Morphology Affect Fertility?
Medically reviewed by Daniel Murrell, M.D.
Find out how sperm morphology can affect fertility.
READ MORE
STI Prevention for Sexual Health
Medically reviewed by Sarah Taylor, MD, FAAD
Practicing safe sex is crucial to the prevention of sexually transmitted infections.
 Learn more.
Learn more. READ MORE
Ro Sperm Storage and Fertility Kit Review: What to Know
The Ro Sperm Kit analyzes your sperm health and even lets you store your sperm — but is it worth it?
READ MORE
All About Male Fertility Testing
Medically reviewed by Carolyn Kay, M.D.
We'll take a look at fertility testing for men and what may (or may not) be contributing to the challenge of having a child.
READ MORE
10 Ways to Boost Male Fertility and Increase Sperm Count
Medically reviewed by Jillian Kubala, MS, RD
Infertility is something many men experience. Here are 10 science-backed ways to increase sperm count and enhance overall fertility in men.
READ MORE
How Is Sperm Produced?
How Is Sperm Produced?Medically reviewed by Stacy Sampson, D. O. — By Scott Frothingham on June 13, 2018
O. — By Scott Frothingham on June 13, 2018
Overview
A man’s reproductive system is specifically designed to produce, store, and transport sperm. Unlike the female genitalia, the male reproductive organs are on both the interior and the exterior of the pelvic cavity. They include:
- the testes (testicles)
- the duct system: epididymis and vas deferens (sperm duct)
- the accessory glands: seminal vesicles and prostate gland
- the penis
Where is sperm produced?
Sperm production occurs in the testicles. Upon reaching puberty, a man will produce millions of sperm cells every day, each measuring about 0.002 inches (0.05 millimeters) long.
How is sperm produced?
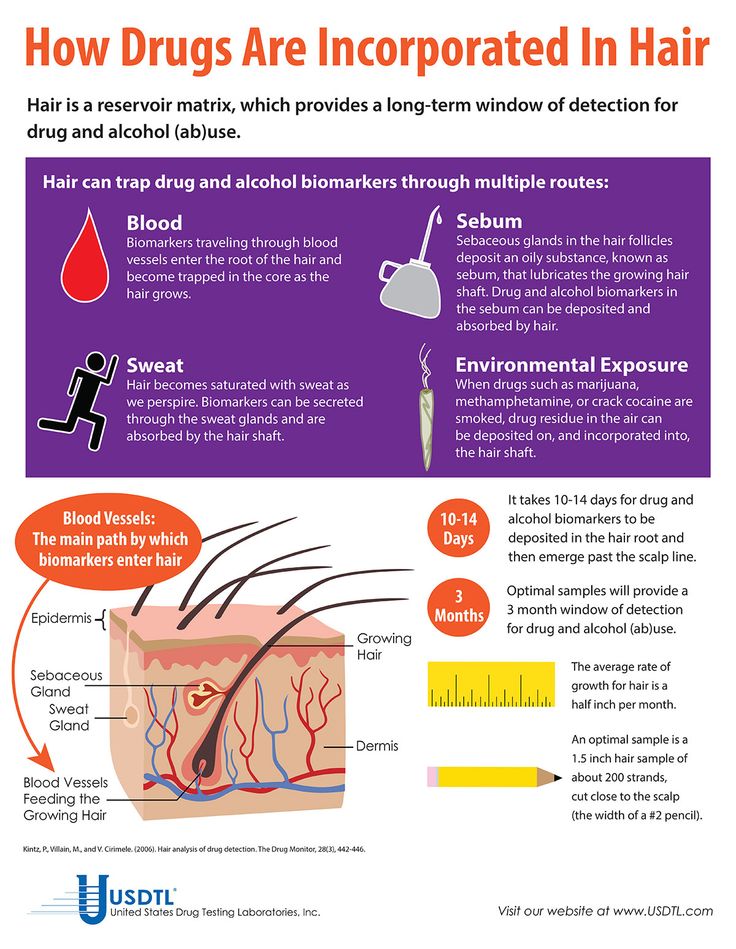
There is a system of tiny tubes in the testicles. These tubes, called the seminiferous tubules, house the germ cells that hormones — including testosterone, the male sex hormone — cause to turn into sperm. The germ cells divide and change until they resemble tadpoles with a head and short tail.
The tails push the sperm into a tube behind the testes called the epididymis. For about five weeks, the sperm travel through the epididymis, completing their development. Once out of the epididymis, the sperm move to the vas deferens.
When a man is stimulated for sexual activity, the sperm are mixed with seminal fluid — a whitish liquid produced by the seminal vesicles and the prostate gland — to form semen. As a result of the stimulation, the semen, which contains up to 500 million sperm, is pushed out of the penis (ejaculated) through the urethra.
How long does it take to produce new sperm?
The process of going from a germ cell to a mature sperm cell capable of egg fertilization takes around 2.5 months.
The takeaway
Sperm are produced in the testicles and develop to maturity while traveling from the seminiferous tubules through the epididymis into the vas deferens.
Last medically reviewed on June 13, 2018
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Hirsh IH. (n.d.). Structure of the male reproductive system.
merckmanuals.com/home/men-s-health-issues/biology-of-the-male-reproductive-system/structure-of-the-male-reproductive-system - Male reproductive system. (n.d.).
kidshealth.org/en/parents/male-reproductive.html - SEER Training: Anatomy of the testis. (2009).
training.seer.cancer.gov/testicular/anatomy/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Jun 13, 2018
Written By
Scott Frothingham
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Stacy Sampson, D.O.
Share this article
Medically reviewed by Stacy Sampson, D.O. — By Scott Frothingham on June 13, 2018
Read this next
How Long Does It Take for Sperm to Regenerate? What to Expect
Medically reviewed by Janet Brito, Ph.
 D., LCSW, CST
D., LCSW, CSTSpermatogenesis is the complete cycle of sperm production and maturation. It constantly supplies your body with sperm able to travel through the…
READ MORE
How Does Sperm Morphology Affect Fertility?
Medically reviewed by Daniel Murrell, M.D.
Find out how sperm morphology can affect fertility.
READ MORE
What Is Sperm Motility and How Does It Affect Fertility?
Medically reviewed by Steven O'Brien
Learn about the different types of sperm motility and whether Y ("boy") chromosomes actually swim faster than X ("girl") chromosomes.
READ MORE
How Long Can Sperm Survive After Ejaculation?
Medically reviewed by Justin Choi, MD
How long can sperm live outside the body? Which sperm and pregnancy myths are true and which are false? Many factors, including environment, your…
READ MORE
What Is a Normal Sperm Count?
Medically reviewed by Daniel Murrell, M.
 D.
D.Many factors can affect your sperm count. A semen analysis can help you determine if your sperm count is normal. If your sperm count is abnormal, work…
READ MORE
Ro Sperm Storage and Fertility Kit Review: What to Know
The Ro Sperm Kit analyzes your sperm health and even lets you store your sperm — but is it worth it?
READ MORE
All About Male Fertility Testing
Medically reviewed by Carolyn Kay, M.D.
We'll take a look at fertility testing for men and what may (or may not) be contributing to the challenge of having a child.
READ MORE
10 Ways to Boost Male Fertility and Increase Sperm Count
Medically reviewed by Jillian Kubala, MS, RD
Infertility is something many men experience. Here are 10 science-backed ways to increase sperm count and enhance overall fertility in men.
READ MORE
What Causes Low Sperm Count and How Is It Treated?
Medically reviewed by Kevin O. Hwang, MD, MPH
Low sperm count can be caused by a number of issues and create difficulty getting pregnant. Fortunately, several very effective treatments are…
READ MORE
What Is Azoospermia?
Medically reviewed by Kevin Martinez, M.D.
Azoospermia is the absence of sperm in your ejaculate. But depending on the type of azoospermia you have, it may be treatable — allowing you to have…
READ MORE
How quickly a man's seminal fluid is restored
Normally, a healthy man's sperm should contain many motile spermatozoa with the correct structure and intact genetic material. But what if a man's body is exposed to negative factors that worsen the quality of sperm? If, for example, the future father works with harmful substances or drank a course of antibiotics? In this case, you need to wait until the complete renewal of the sperm in the man occurs. How does this process go and how long does it take?0003 restores seminal fluid in men to conceive a healthy child ?
How does this process go and how long does it take?0003 restores seminal fluid in men to conceive a healthy child ?
How does sperm renewal take place?
The formation and formation of spermatozoa (spermatogenesis) occurs in the tubules of the testicles and includes several stages:
- First, spermatogonia divide. This is what progenitor cells are called - there are about a billion of them in the testicles.
- Some of the spermatogonia become first-order spermatocytes.
- Spermatocytes divide. One such cell forms two spermatocytes of the second order. Each of them contains a set of 23 unpaired chromosomes.
- Secondary spermatocytes are converted to form two spermatids.
- The next step is the transformation of the spermatid into a spermatozoon. This process is impossible without male sex hormones.
- Acrosome is forming. This is a membrane vesicle that contains hyaluronidase, an enzyme that dissolves the egg cell membrane during fertilization.
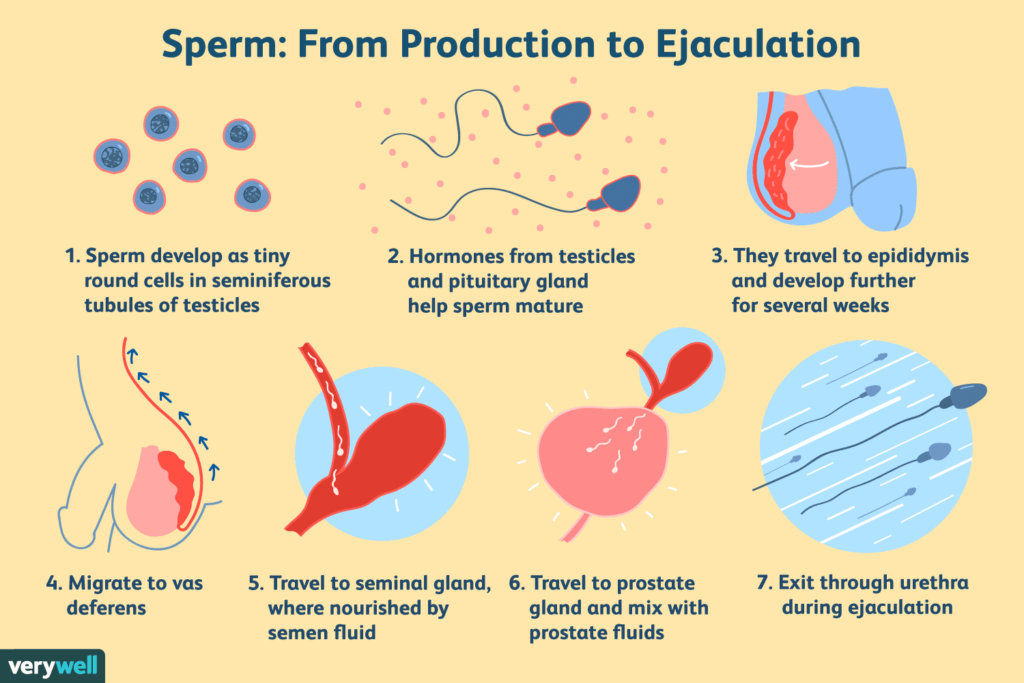
- The final stage is the maturation of spermatozoa in the seminal appendages. After that, they are ready for fertilization.
How fast is sperm completely restored?
It takes 68 to 78 days for complete recovery of sperm, that is, approximately 2.5 months. Of these, from 56 to 64 days are required for the transformation of spermatogonia into spermatozoa, and from 12 to 14 days the spermatozoa mature in the seminal appendages. This means that if a man has been exposed to factors that negatively affect spermatogenesis (taking antibiotics, overheating, etc.), then conception should be planned no earlier than 3 months after their elimination.
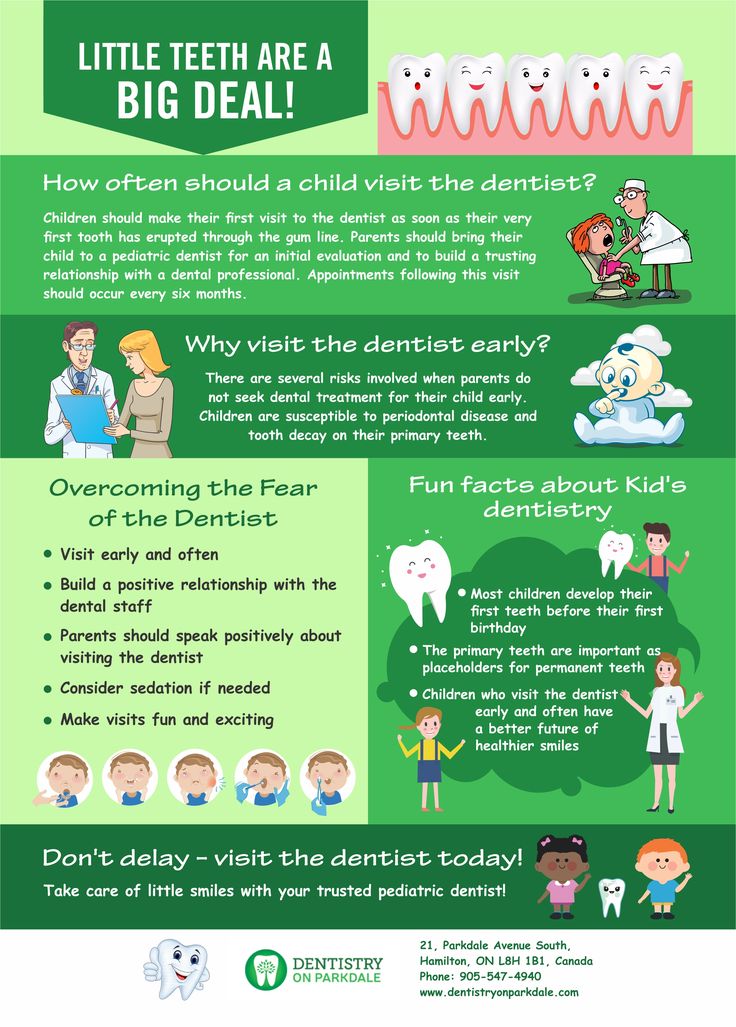
Also, when planning a conception, it is important to understand how much sperm is restored after intercourse. After ejaculation, new spermatozoa mature and come from the appendages in 72 hours (3 days). Therefore, the optimal frequency of having sex for a couple who are trying to conceive a child is 2 times a week. Otherwise, immature spermatozoa will get into the sperm, which have little chance of fertilizing the egg.
Otherwise, immature spermatozoa will get into the sperm, which have little chance of fertilizing the egg.
How is the frequency of sperm renewal related to the conception and bearing of a healthy child?
In addition to taking antibiotics and working with harmful substances, sperm maturation is negatively affected by:
- Diseases of the genitourinary system (prostatitis, STDs, varicocele).
- X-ray (for example, if a man took a picture of the sacrum).
- Unfavorable environmental situation: increased radioactive background, constant exposure to electromagnetic radiation, dusty or polluted air.
- Bad habits.
- Overheating: wearing tight underwear, regularly going to the sauna or using heated seats in the car, etc.
That is why knowing how long sperm is restored allows you to increase the chances of conception and minimize the risks that arise when an egg is fertilized by an inferior sperm: spontaneous abortion, fetal development pathologies, congenital genetic diseases. Since the “reserve” of spermatozoa is updated every three months, doctors recommend that men plan conception no earlier than 3 months after the end of exposure to harmful factors. And this time should be devoted to preparing for conception in order to ensure the maturation and full development of spermatozoa. How to do it?
Since the “reserve” of spermatozoa is updated every three months, doctors recommend that men plan conception no earlier than 3 months after the end of exposure to harmful factors. And this time should be devoted to preparing for conception in order to ensure the maturation and full development of spermatozoa. How to do it?
During this period, a man needs to take specialized complexes to improve the quality of sperm, and hence male fertility. For example, the drug Speroton (more about the product can be found here) increases the number of spermatozoa with the correct structure, increases their mobility, concentration and ejaculate volume. As a result, the chances of conception increase markedly.
It is also necessary to lead a healthy lifestyle:
- Walk more often in the fresh air, try to avoid traffic jams, being near smokers.
- Postpone heavy physical activity for this period, whether it is sports or scheduled repairs.
- Eat foods rich in protein and antioxidants.
 Give up alcohol for three months.
Give up alcohol for three months. - Be sure to get enough sleep, try to avoid stress and nervous tension.
IS NOT ADVERTISING. THE MATERIAL IS PREPARED WITH THE PARTICIPATION OF EXPERTS.
How long does it take for spermatozoa to mature? | "Gedeon Richter"
Valeria
Naberezhnye Chelny
Sperm is the smallest cell in the human body. It is necessary for the fertilization of the female egg. The spermatozoon has great mobility (due to the tail) and a high speed of movement. In half an hour, this "tadpole" is able to overcome about 10 centimeters.
Spermatozoa mature in the process of spermatogenesis. It occurs inside the seminiferous tubules, which make up most of the adult male testicle. The process of sperm formation is triggered by hormones during adolescence and can continue into old age. Thus, a healthy man, unlike a woman, retains fertility (the ability to conceive) even in old age. But the number of "nimble tadpoles" by this time is noticeably decreasing, as well as their quality.
How long does it take for spermatozoa to mature?
One gram of ovarian tissue produces up to 300 germ cells per second. However, before turning into a full-fledged spermatozoon, they go through several stages of development. First, the primary germ cells turn into spermatogonia, then into spermatids, and only then into spermatozoa. Thus, the total maturation time of spermatozoa capable of fertilization is about 72-74 days.
How many spermatozoa are there in semen?
The arithmetic is simple. During ejaculation, depending on the physiological characteristics, emotional state and duration of abstinence, the man releases from 2 to 10 milligrams of sperm. One milligram contains from 20 to 120 million germ cells. Normally, at least 60% of them are distinguished by the necessary activity. Accordingly, after unprotected intercourse, on average, from 12 million to 720 million spermatozoa will go on an “egg hunt”. The vast majority of them will die in the acidic environment of the vagina. Spermatozoa that manage to pass this milestone will be able to live in the genitals of women from 2 to 8 days, but only one, if he is lucky, will fertilize the egg.
Spermatozoa that manage to pass this milestone will be able to live in the genitals of women from 2 to 8 days, but only one, if he is lucky, will fertilize the egg.
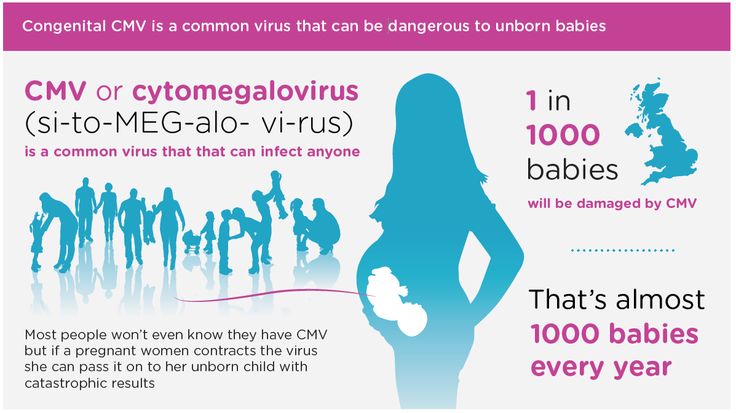
What factors affect sperm production?
If one milligram of semen contains less than 20 million spermatozoa, and the motility of more than half is questionable, we can talk about possible infertility. It is usually associated with disorders that occur during the maturation of spermatozoa, or problems with their excretion. They can be caused by malformations, injuries, diseases. So, for example, with cryptorchidism (undescended testicle into the scrotum), the process of spermatogenesis is disrupted in every 2-3 men. And with varicocele (expansion of the veins of the plexus of the spermatic cord), poor spermogram results, according to various sources, have from 2 to 9men out of 10. Childhood infections can also play an important role in the development of male infertility. Mumps, better known to many as "mumps", in adolescence often leads to damage to the testicles.