Hand foot and mouth when pregnant
Hand, Foot and Mouth Disease
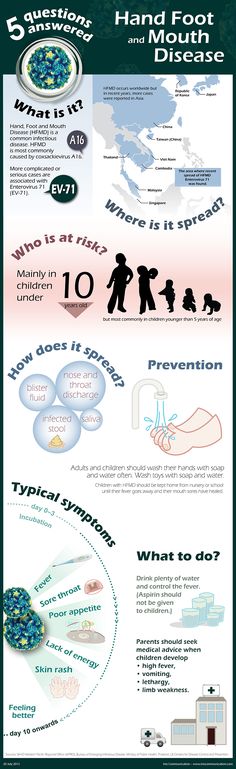
Hand Foot and Mouth Disease (HFMD) is a very common illness. It can be very scary for parents because it usually affects young children and often starts with a high fever and a rash. It could also be the name – Hand, Foot and Mouth Disease just sounds like something you really want to avoid!
What is Hand, Foot and Mouth?
Hand foot and Mouth disease (HFMD) is a common viral illness. It typically starts with a fever followed by a rash. The rash is most commonly on the chin, mouth and inside the mouth and also on the hands and feet. A rash can also be found in the diaper area. Kids can also experience high fevers and mouth pain that affects their ability to eat and drink.
HFMD usually peaks in summer and early fall and typically affects children who are five years and under. However older children and adults can get it too. One of the frustrating things for parents about HFMD is that it can be caused by different viruses—which means your child could get it again.
What are the symptoms of HFMD?
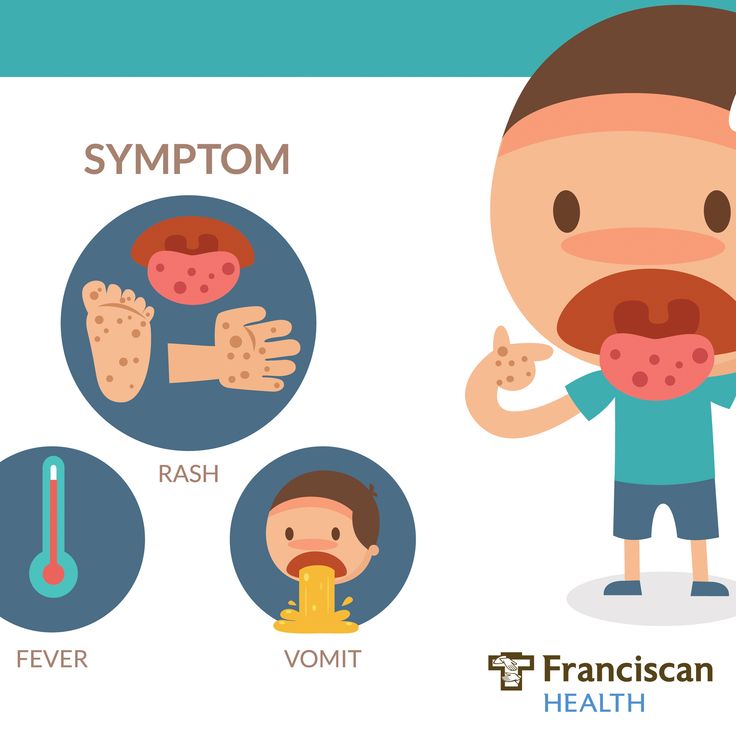
It usually starts with:
- A fever
- Decreased appetite
- Sore throat
- Tiredness or feeling of being unwell
One or two days after the fever starts, painful sores/small red spots can develop in the mouth that can blister and become painful.
A rash on the palms of the hands and soles of the feet may also develop over one or two days as flat, red spots, sometimes with blisters. It may also appear on the knees, elbows, buttocks or genital area.
Some people, especially young children, may get dehydrated if they are not able to swallow enough liquids because of painful mouth sores. You should seek medical care in these cases.
Not everyone will get all of these symptoms. Some people, especially adults, may become infected and show no symptoms at all, but they can still pass the virus to others.
How is HFMD diagnosed?
Health care providers can usually identify mouth sores caused by hand, foot, and mouth disease by considering:
- Patient age
- Patient symptoms
- Appearance of the rash and mouth sores
Who is most likely to get HFMD?
HFMD usually peaks in summer and early fall and typically affects children who are five years and under. However, older children and adults can get it too.
However, older children and adults can get it too.
Is HFMD Contagious?
Yes. The viruses that cause HFMD can be found in an infected person’s:
- Nose and throat secretions (such as saliva, sputum, or nasal mucus)
- Blister fluid
- Feces (poop)
You can get exposed to the viruses that cause HFMD through:
- Close personal contact, such as hugging an infected person
- The air when an infected person coughs or sneezes
- Contact with feces, such as changing diapers of an infected person, then touching your eyes, nose, or mouth before washing your hands
- Contact with contaminated objects and surfaces, like touching a doorknob that has viruses on it, then touching your eyes, mouth, or nose before washing your hands
It is also possible to get infected with the viruses that cause HFMD if you swallow However, this is not very common. This is more likely to happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has HFMD.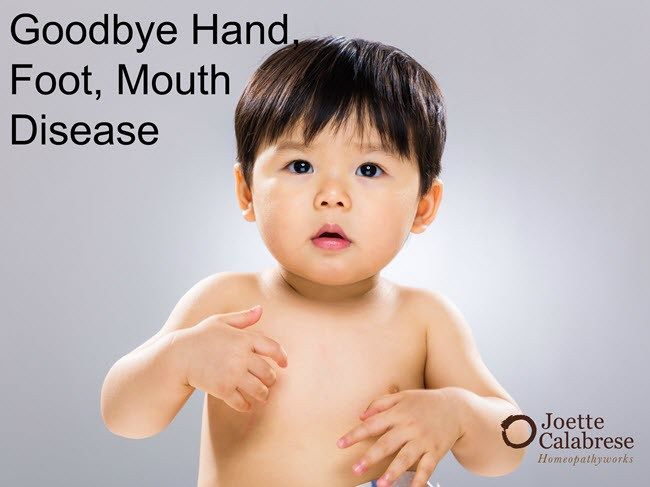
Generally, a person with HFMD is most contagious during the first week of illness. People can sometimes be contagious for days or weeks after symptoms go away. Some people, especially adults, may become infected and not develop any symptoms, but they can still spread the virus to others.
HFMD is not transmitted to or from pets or other animals.
How to stop the spread of HFMD?
Hand, food and mouth is easily passed on to people by a simple cough or sneeze. To reduce the risk spreading HFMD:
- Maintain good hygiene, such as frequent hand washing and teach your kids (try singing a song while washing hands to teach them the length of time to wash hands)
- Use a tissue to cough or sneeze
- Don’t share towels or household items, such as cutlery
- Wash soiled bedding and clothes in hot water
How soon can children return to school after HFMD?
Those with HFMD should stay home while they are sick. Talk with your healthcare provider if you are not sure when you should return to work or school. The same applies to children returning to daycare.
The same applies to children returning to daycare.
Is it dangerous to women who are pregnant?
Although there’s normally no risk to the pregnancy or baby, it’s best to avoid close contact with anyone who has hand, foot and mouth disease. If a pregnant woman is infected with HFMD shortly before delivery, there is a chance she can pass the virus to her baby. These babies usually have only mild illness, but in rare cases they may have severe infection.
HFMD is very common and pregnant woman are likely to be exposed at some point in her pregnancy to someone who is infected, especially in the summer and fall. But most pregnant women, like other adults, have immunity (protection) from previous exposures to these viruses. So if she does get infected she will likely not have symptoms or will only have mild illness. Pregnant women without immunity to HFMD viruses have a greater chance of getting infected and having symptoms.
There is no clear evidence that HFMD during pregnancy increases the risk of severe complications like miscarriage, stillbirth, or congenital defects.
How is it treated?
HFMD is a virus so antibiotics won’t help. We use Tylenol or Ibuprofen to help kids deal with the pain. There are also some different mouthwashes that have Benadryl and Maalox/Mylanta in them that can be used to help ease the pain for kids who develop mouth ulcers. Be sure to talk with your pediatrician before treating HFMD.
When can my child go back to school or daycare?
As long as your child is fever free, acting normally and doesn’t have draining blisters, she or he is fine to go back to school or daycare. It may take up to 7 days for all of the blisters to dry up.
What should I notice signs of HFMD in my child?
If your child is showing any symptoms of an hand, foot and mouth, please call Building Blocks Pediatrics at (660) 262-7415.
Other Recent Posts by WMMC:
Breastfeeding Myths Debunked
Pediatric Swimmer’s Ear
Recreational Water Illnesses
About Western Missouri Medical Center
Western Missouri Medical Center (WMMC) is a fully-accredited acute care county medical center located in Warrensburg, MO.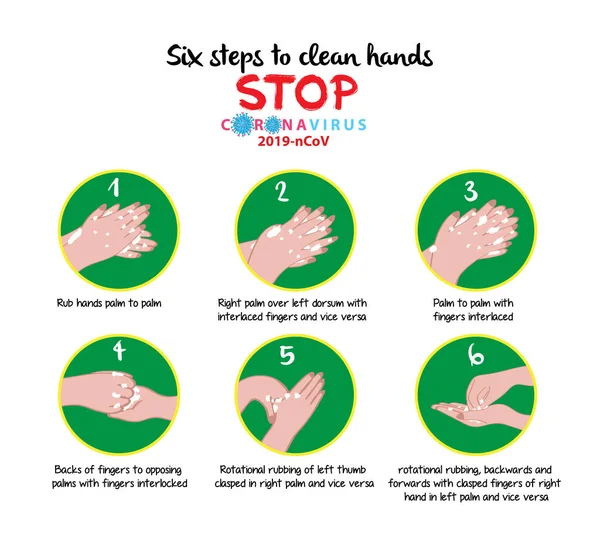 WMMC prides itself in emergency care, obstetrics, orthopedic and general surgery, family healthcare, internal medicine, outpatient clinics, ambulatory care, rehabilitation services and more. Inpatient services include medical, surgical, intensive, obstetrical, orthopedic, pediatric and skilled nursing care, as well as a wide range of therapeutic and diagnostic outpatient services. This institution is an equal opportunity provider and employer. Learn more at WMMC.com.
WMMC prides itself in emergency care, obstetrics, orthopedic and general surgery, family healthcare, internal medicine, outpatient clinics, ambulatory care, rehabilitation services and more. Inpatient services include medical, surgical, intensive, obstetrical, orthopedic, pediatric and skilled nursing care, as well as a wide range of therapeutic and diagnostic outpatient services. This institution is an equal opportunity provider and employer. Learn more at WMMC.com.
Hand, Foot, and Mouth Disease During Pregnancy: Is It Dangerous?
Hand, Foot, and Mouth Disease During Pregnancy: Is It Dangerous?Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Chaunie Brusie on December 10, 2018
Coxsackievirus during pregnancy
Even though I’m a nurse, coxsackievirus is new to me. But it’s in the same family as one virus I know well.
Different strains of coxsackievirus, also known as coxsackievirus A16, are usually the culprit behind hand, foot, and mouth disease (HFMD). That’s a virus most of us have heard of, if not already had the pleasure of dealing with.
That’s a virus most of us have heard of, if not already had the pleasure of dealing with.
Coxsackievirus is actually a type of virus in the enterovirus family. These are common during pregnancy.
Most of the time, the virus doesn’t pose serious danger to you or your baby. But there are a few things you need to know.
Symptoms
Coxsackievirus, in the form of HFMD, is most common in children under the age of 5. But it can occasionally affect adults. The virus is more common in certain parts of the world, such as Asia.
The symptoms of HFMD include:
- fever
- general feeling of sickness
- sore throat
- painful mouth sores or blisters
- skin rash developing on the elbows, feet, or genital areas
For adults, the virus may not give you any symptoms.
Risk factors
Having the coxsackievirus virus during pregnancy may pose a slight risk to your baby. But that’s only if the virus is able to pass through the placenta. The chance of that happening is very small.
The chance of that happening is very small.
Having the coxsackievirus slightly increases the risk of miscarriage or stillbirth, as is the case with any infection during pregnancy.
HFMD is more risky if the woman acquires the virus near the end of her pregnancy. An infection near delivery carries more risk of stillbirth, or HFMD in the newborn.
There has also been some evidence that the virus is linked to congenital heart defects and other anomalies in babies. But there’s conflicting data on whether or not the virus definitely causes those problems.
Confusing, I know. But the odds are having the virus doesn’t necessarily mean your baby will suffer later on. Which is good news, indeed.
Prevention
HFMD and other conditions caused by the coxsackievirus family are commonly seen in young children. That’s why it’s more likely that you’ll come into contact with the virus while caring for other kids.
If you have other children with HFMD and are pregnant, here are a few tips to help navigate caring for both of you.
- Wash hands often. Try to wash your hands after each contact with your child.
- Wear a face mask. Some doctors recommend a face mask if your child has a serious runny nose and cough. As any parent knows, that snot is going to get on you, no matter how often you wash your hands.
- Don’t pick blisters. It’s very important not to pick at your child’s blisters. Blister fluid can be contagious.
- Don’t share. Avoid sharing drinks, toothbrushes, or anything that comes into contact with saliva. The virus lives in saliva, so it may just mean a break from baby kisses for now.
- Stay hydrated. Dehydration is always a risk with infections during pregnancy. It can cause other complications like contractions or premature labor. Drink plenty of water, even if you don’t have any symptoms of the virus.
The takeaway
If you develop coxsackievirus during pregnancy, talk to your doctor. The chance of potential risks are small, but do your best to prevent being exposed with careful hand washing and avoid exposure.
The chance of potential risks are small, but do your best to prevent being exposed with careful hand washing and avoid exposure.
Take care of yourself first, and rest assured that you’re doing the best you can to take care of your baby in the process.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on December 10, 2018
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Hand, foot, and mouth disease. (2017).
cdc.gov/hand-foot-mouth/about/signs-symptoms.html - Hand, foot, and mouth disease. (2018).
kkh.com.sg/HealthPedia/Pages/ChildhoodIllnessesHFMD.aspx - Ornoy At, et al. (2006). Pregnancy outcome following infections by coxsackie, echo, measles, mumps, hepatitis, polio and encephalitis viruses.
sciencedirect.com/science/article/pii/S0890623806000207 - Yu W, et al. (2015). Coxsackie virus A16 infection of placenta with massive perivillous fibrin deposition leading to intrauterine fetal demise at 36 weeks gestation. DOI:
doi.org/10.2350/15-01-1603-CR.1
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 10, 2018
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Chaunie Brusie on December 10, 2018
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Chaunie Brusie on December 10, 2018
related stories
Medications You Should Avoid During Pregnancy
Can a Fever During Pregnancy Harm My Baby?
Using Tamiflu in Pregnancy: Is It Safe?
Headache During Pregnancy: What You Need to Know
Can You Take Benadryl While Pregnant?
Read this next
Medications You Should Avoid During Pregnancy
Medically reviewed by Zara Risoldi Cochrane, Pharm.D., M.S., FASCP
Some medicines are considered unsafe to take during pregnancy. They may be damaging to you or your developing baby. Discover some medicines to avoid…
READ MORE
Can a Fever During Pregnancy Harm My Baby?
Medically reviewed by Karen Gill, M.D.
A high fever during early pregnancy might be dangerous for your baby-to-be.
 Here’s why you should see a doctor for treatment.
Here’s why you should see a doctor for treatment.READ MORE
Using Tamiflu in Pregnancy: Is It Safe?
Medically reviewed by Dena Westphalen, Pharm.D.
Learn if, when, and why Tamiflu is a safe option to treat the flu during pregnancy.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
Can You Take Benadryl While Pregnant?
Medically reviewed by Carolyn Kay, M.D.
You're wary of taking medications while pregnant, but your allergy symptoms are unbearable. Fortunately, Benadryl during pregnancy is typically fine.

READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
How to behave in childbirth? Learning to give birth quickly and with problems
Childbirth is a natural process, laid down by nature. The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
Childbirth is the final and most important stage of pregnancy. How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions.
1. When is it time to go to the maternity hospital?
Childbirth is a natural result of hormonal changes that occur in your body during the final stages of pregnancy. The sagging belly and heaviness in its lower part and the lumbar region speak of the imminent denouement of the story. Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity.
The signal to call an ambulance should be sufficiently strong contractions that are repeated at regular intervals, the appearance of mucous secretions from the genital tract, slightly stained with blood, or the outflow of amniotic fluid.
2. First stage of childbirth: we breathe for two!
From the moment the contractions become regular, the first stage of labor begins, during which the strength, frequency and duration of uterine spasms increases and the cervix opens.
During spastic contraction of the uterine muscle fibers, the blood vessels that carry arterial blood to the placenta and fetus are compressed. The fetus begins to experience a lack of oxygen, and this involuntarily makes you breathe deeper. The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
In the first stage of labor, during each contraction, you need to breathe calmly and deeply, trying not to hold your breath while inhaling. At the same time, the air should fill the upper sections of the lungs, as if raising the chest. You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
3. Auto-training in the prenatal ward
To speed up the opening of the cervix, you need to walk more, but sitting is not recommended, while blood flow in the limbs is disturbed and venous blood stagnation occurs in the pelvis. From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby."
From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby."
4. To relieve pain
Acupressure of the lower back can help relieve pain. Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Monitor the frequency and duration of contractions and if they weaken or sharply increase, immediately inform your doctor. In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
If dilatation of the cervix causes reflex vomiting, rinse the mouth with water and then drink a few sips to replace the lost fluid. Do not drink a lot, this can provoke a recurrence of vomiting.
Do not drink a lot, this can provoke a recurrence of vomiting.
5. The maternity ward is not a place for tantrums
They say that difficult childbirth is a person's retribution for walking upright. Childbirth is actually a painful process, but the presence of reason allows us, representatives of the genus Homo sapiens, to control our emotions. Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome.
6. Second stage of labor - pushing and expulsion of the fetus
After the baby's head slips through the dilated cervix and finds itself on the bottom of the pelvis, the pushing period of labor begins. At this time, there is a desire to push, as it usually happens during a bowel movement, but at the same time many times stronger. At first, the attempts are controllable, they can be "breathed", but by the beginning of the third stage of labor, the expulsion of the fetus, they become unbearable.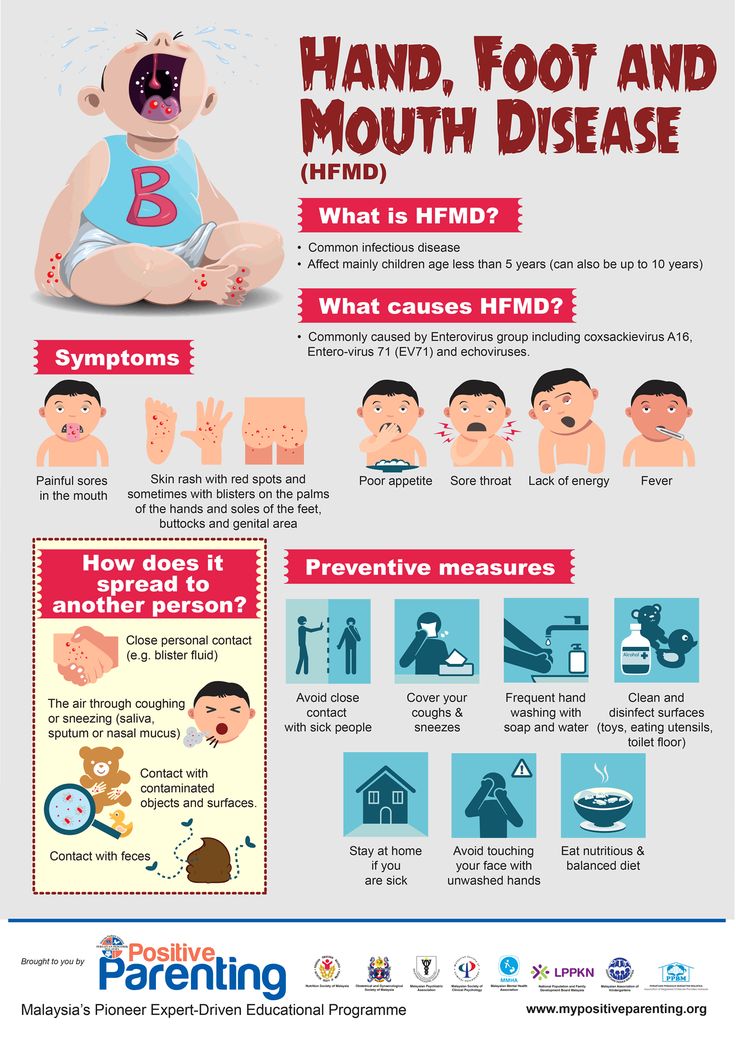
With the beginning of the straining period, you will be transferred to the delivery room. Having settled down on the delivery table, rest your feet on the special steps, firmly grasp the handrails and wait for the midwife's command.
While pushing, inhale deeply, close your mouth, clench your lips tightly, pull the handrails of the delivery table towards you and direct all the exhalation energy down, squeezing the fetus out of you. When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
7. Third stage of labor and final
Third stage of labor - afterbirth.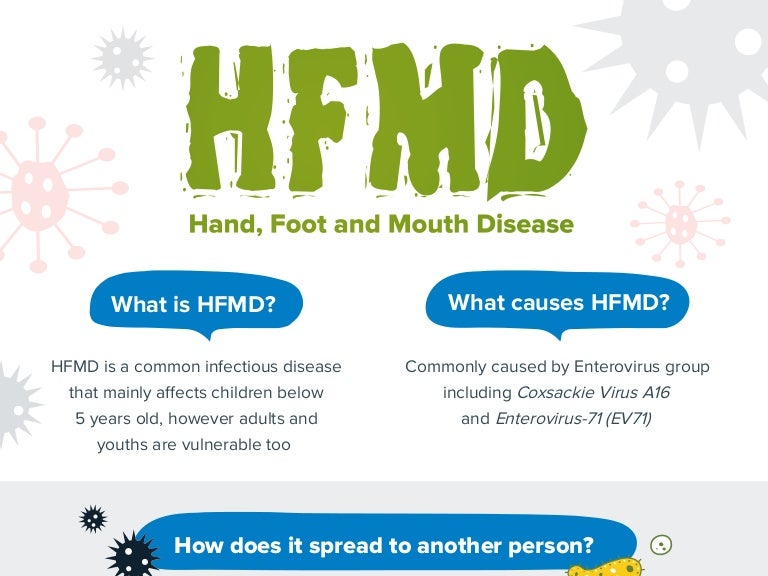 At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
About 10 minutes after your baby is born, your midwife will ask you to push again to deliver your afterbirth. The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures.
You will have to spend another couple of hours in the delivery room with an ice-filled bladder on your stomach. To quickly contract the uterus, you will be given injections of special drugs. When the threat of postpartum hemorrhage has passed, you will be transferred to the postpartum ward to the baby.
Childbirth completed. Ahead of the postpartum period, during which your body will recover after pregnancy.
More details on Medkrug. RU: http://www.medkrug.ru/article/show/kak_pravilno_vesti_sebja_v_rodah_uchimsja_rozhat_bystro_i_problem
RU: http://www.medkrug.ru/article/show/kak_pravilno_vesti_sebja_v_rodah_uchimsja_rozhat_bystro_i_problem
Source: http://www.medkrug.ru/
10 questions from pregnant women about ultrasonography
10 questions from pregnant women about ultrasonography
The moment when an expectant mother can see her unborn baby on ultrasound is exciting sometimes to tears. Also important are the quality of the examination and the personality of the doctor, who can both please and, if anything, reassure. Gynecologist Gunars Sergeants , who will soon celebrate his 70th birthday, has been working at Riga 1st Hospital since 1980 years. Thousands of grateful mothers and born babies! Today, an ultrasound specialist answers the questions that pregnant women ask most often.
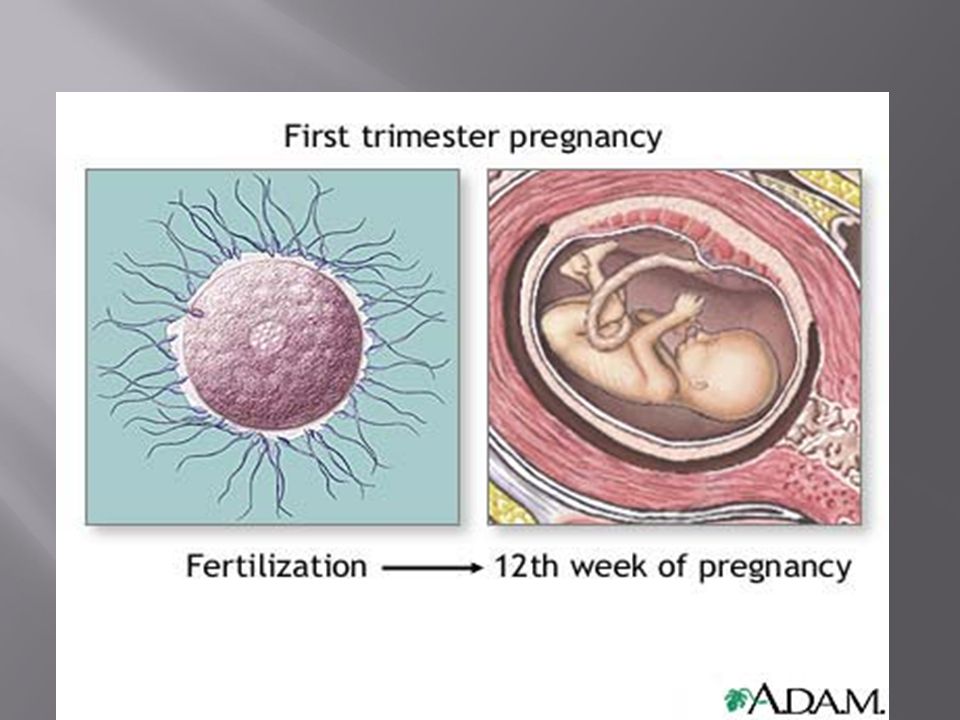
1. When should ultrasonography be done?
The very first sonography is usually performed between the fourth and sixth weeks of pregnancy, before the mother is registered.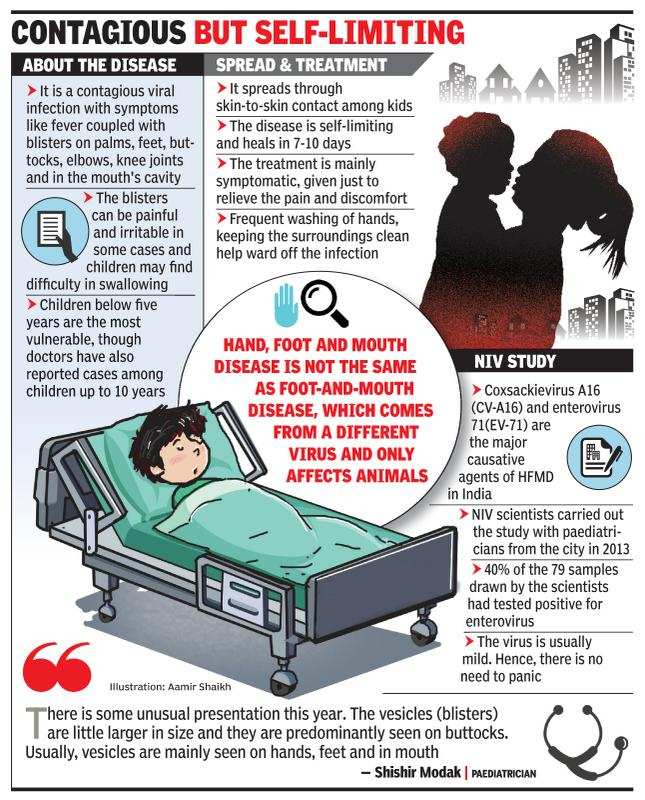 The task of the specialist during the examination is to establish whether the pregnancy has occurred, whether there is an ectopic pregnancy that should be terminated, whether the fetus has a heartbeat, or whether the pregnancy is multiple. The parameters of the child are also measured, which allow you to determine the week of pregnancy and the approximate date of birth.
The task of the specialist during the examination is to establish whether the pregnancy has occurred, whether there is an ectopic pregnancy that should be terminated, whether the fetus has a heartbeat, or whether the pregnancy is multiple. The parameters of the child are also measured, which allow you to determine the week of pregnancy and the approximate date of birth.
The next sonography, which is also called the first trimester screening, is carried out at 11-13 weeks, when the fetus is 45-85 mm in size and already looks like a human. The doctor will check if all the internal organs are in order, how the arms and legs look, how the heart beats and the umbilical circulation system works.
Third sonography (second trimester screening) performed at 20-22 weeks. The doctor can see if the fetus has any pathologies. If so, will they be treatable while still in the womb or immediately after birth. Unfortunately, sometimes halfway through the journey, you have to make a decision to terminate the pregnancy.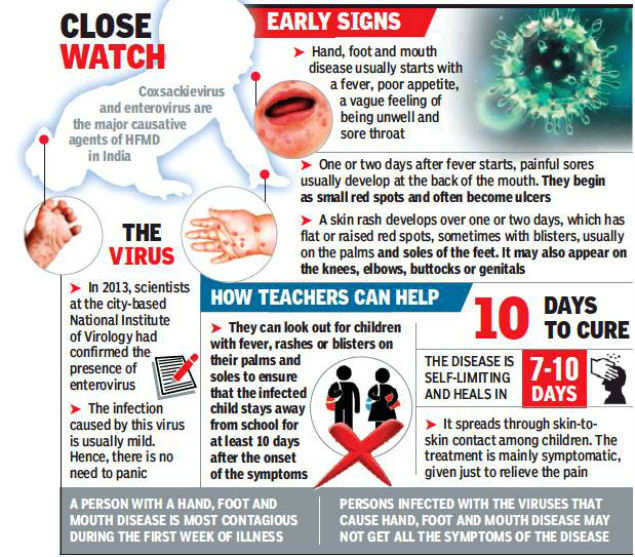
2. What is screening? Why does it need to be done multiple times?
Screening and sonography are practically the same thing. The only difference is in the names. But, during screening in the first trimester, in addition to ultrasound, a blood test is done within 24 hours and, taking into account the results of both procedures, it is determined whether the baby has a risk of being born with Down syndrome.
Tests are no longer taken during the second trimester screening. On ultrasound, the doctor examines not only the baby, but also measures the amniotic fluid, looks at the bottom of the uterus, its density, and checks for placental abruption. If a woman has previously had a delivery by caesarean section, then the old suture is also examined during screening.
3. Why is the state-paid planned ultrasound not carried out in the third trimester as well?
Ultrasound can be performed as many times as needed. If the doctor needs to make sure that everything is in order with the baby, additional ultrasonographic checks are prescribed in both the second and third trimester.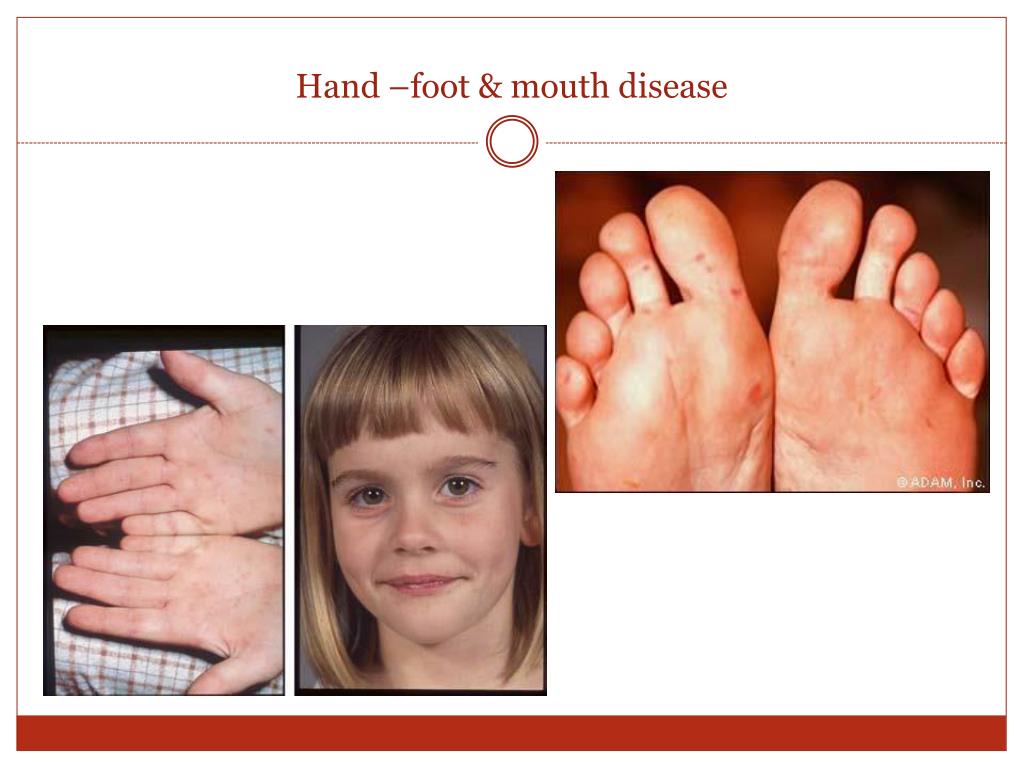 They are not prohibited, and, if necessary, the state pays for them. It is possible to carry out an ultrasound in the third trimester if the doctor wants to make sure that the baby is preparing for childbirth. If everything is in order with the child on the second ultrasound, then sonography is usually not prescribed in the third trimester.
They are not prohibited, and, if necessary, the state pays for them. It is possible to carry out an ultrasound in the third trimester if the doctor wants to make sure that the baby is preparing for childbirth. If everything is in order with the child on the second ultrasound, then sonography is usually not prescribed in the third trimester.
After the 36th week, sonography can determine the approximate weight at which the baby will be born. Pay attention to how the child moves. If it seemed to the mother that the activity of the child had decreased, this is a reason for an additional ultrasound. After the 40th week, the doctor looks at how the baby feels, whether he is ready to be born on his own or needs stimulation. There are many situations when a sonographic examination is necessary in the third trimester.
4. At what time can you accurately determine the sex of the child by ultrasound? Are there any mistakes?
The external sexual characteristics of the child begin to appear from the ninth week. But not so clearly to say for sure whether it is a boy or a girl. It can only be guesswork. In boys, the scrotum is not yet clearly visible, and a boy's penis can still be easily confused with a girl's clitoris. The sex of the child is determined after the 16th week of pregnancy. You can see the baby well, provided that the child does not spin and does not cover the “right place” with a pen or leg. The specialist is mistaken in rare cases.
But not so clearly to say for sure whether it is a boy or a girl. It can only be guesswork. In boys, the scrotum is not yet clearly visible, and a boy's penis can still be easily confused with a girl's clitoris. The sex of the child is determined after the 16th week of pregnancy. You can see the baby well, provided that the child does not spin and does not cover the “right place” with a pen or leg. The specialist is mistaken in rare cases.
5. Is it possible to determine with the help of ultrasound whether the child is developing correctly?
Possible. If the ultrasonography specialist during the screening sees that the development of the baby is normal, then there is no reason to doubt it. If the doctor suspects that the child has some kind of pathology, then additional examinations are carried out by a geneticist. Also, the doctor asks to do an ultrasound again - earlier than it should be. The ultrasound specialist and the attending physician talk to the pregnant woman about the possible pathology in the baby only when this possibility is really very high. The only thing that is difficult to determine one hundred percent is the specific date of birth. During sonography, the latest possible date of delivery is established, when the pregnant woman can already walk over. It is also difficult to determine the exact weight of the child. At a later date, the error can be 200 grams, because the baby is already "donkey" in the pelvic area and it is difficult to accurately measure it.
The only thing that is difficult to determine one hundred percent is the specific date of birth. During sonography, the latest possible date of delivery is established, when the pregnant woman can already walk over. It is also difficult to determine the exact weight of the child. At a later date, the error can be 200 grams, because the baby is already "donkey" in the pelvic area and it is difficult to accurately measure it.
6. What, unfortunately, cannot be seen on ultrasound?
Any disease or pathology that develops only after the birth of a child. It is impossible to see the child's joints and determine how strong the internal ligaments of the foot will be. In a sonographic image, it is almost impossible to see what is happening with the child's skin, whether he will have birthmarks or moles.
7. Can the procedure be performed in the presence of the child's father?
Yes, it is allowed. For a man, this is a wonderful opportunity to meet a baby and the moment when he can realize: I will become a father. The first sonography is carried out at a very early stage, when the baby is not yet visible, and it is performed vaginally, which not all men are ready to look at, and the expectant mother may not feel comfortable. The best time when future parents can come to the ultrasound together is 20-22 weeks of pregnancy. The image of the child is very clear, besides, it is possible to determine its gender, which gives parents great joy. However, there is a request to the accompanying persons - do not stay in the office during the entire time of the inspection. Let the doctor and the expectant mother talk in private.
The first sonography is carried out at a very early stage, when the baby is not yet visible, and it is performed vaginally, which not all men are ready to look at, and the expectant mother may not feel comfortable. The best time when future parents can come to the ultrasound together is 20-22 weeks of pregnancy. The image of the child is very clear, besides, it is possible to determine its gender, which gives parents great joy. However, there is a request to the accompanying persons - do not stay in the office during the entire time of the inspection. Let the doctor and the expectant mother talk in private.
8. What does the baby feel in the mother's belly during the ultrasound?
Most often, the baby sleeps during ultrasonography, which proves that the procedure does not interfere with him. To better examine the baby, it is desirable that he spin. Therefore, it happens that we ask the pregnant woman to move, walk around, turn from side to side so that the child wakes up.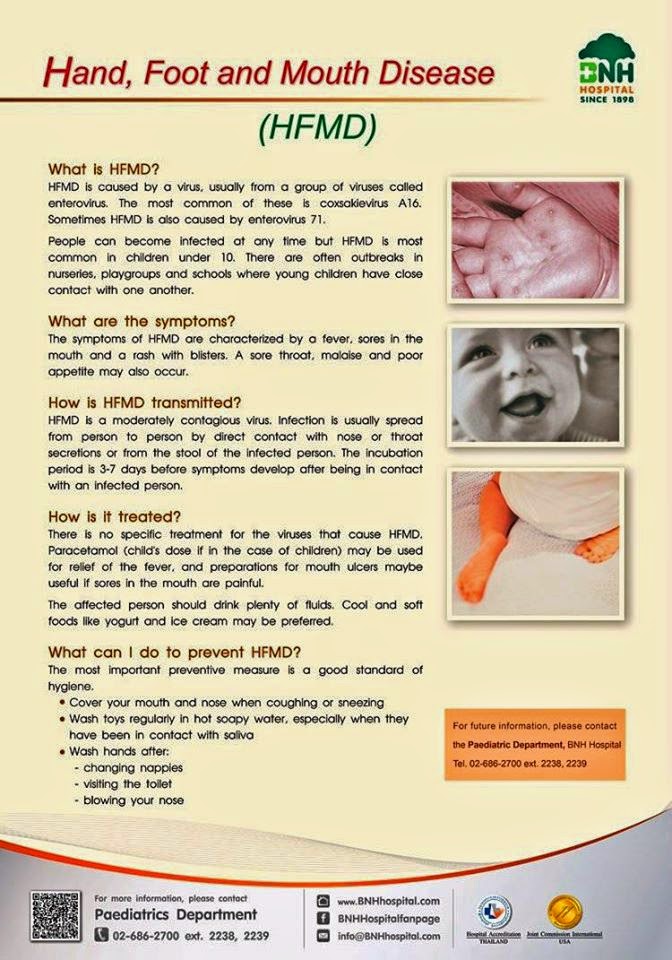
9. If ultrasonography is performed frequently, is it harmful to the child?
Sonography is not only accurate, but also safe. It is not true that he can somehow harm the child. A visit to an ultrasound specialist takes 40 minutes, but the process of examining a child lasts no more than 10 minutes. With such a duration of the ultrasound procedure, it is not harmful, even if it is done once a month. In addition, even at a monthly examination by a gynecologist, a pregnant woman is not looked at as carefully and for a long time as in an ultrasound room. The observing gynecologist, even if he uses an ultrasound machine, examines the most necessary things - whether the baby’s heart is working well, whether the size of the head corresponds to the size of the abdomen, whether fluid collects in the child’s head, whether the pregnant woman’s cervix opens.
One can say that sonography can supposedly warm up the amniotic fluid (there are such concerns) if the stomach is heated with the device for more than 40 minutes.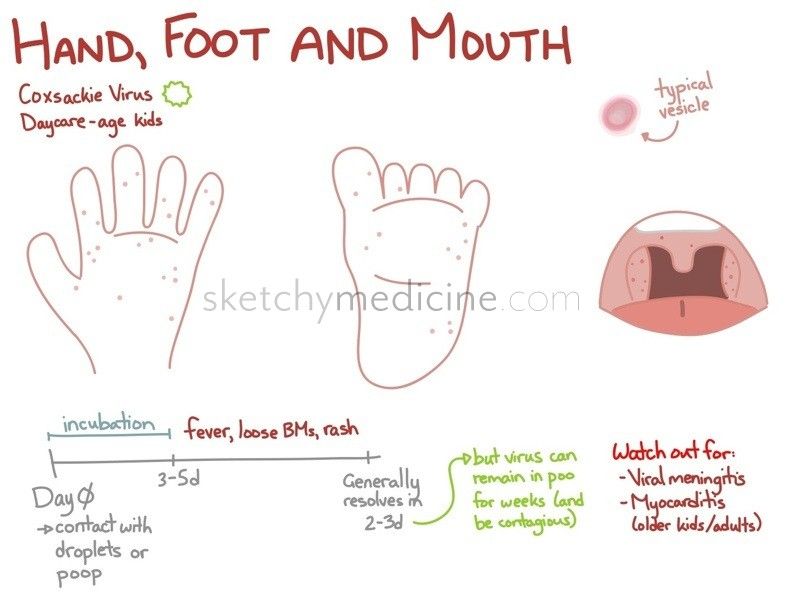 But neither at the visit to the gynecologist, nor at the ultrasound specialist, the examination is carried out for such a long time.
But neither at the visit to the gynecologist, nor at the ultrasound specialist, the examination is carried out for such a long time.
10. Ultrasound in 2D, 3D and 4D – a tribute to fashion or a necessity?
Most pregnant women are traditionally examined with a two-dimensional image (2D) The picture on the screen is flat, and everything that is in the stomach is visible on it. Everything solid is white, liquid is black. With the help of 2D sonography, the doctor can clearly see both the baby and his organs. 3D sonography does not allow you to see the internal organs so well. It is used in order to better consider the face of the expected child. 3D ultrasonography helps to view the baby's body not in a flat image, but in a three-dimensional one. Usually 3D is used if the mother wants to get a clear photo of the baby in the stomach, close to the real one. In turn, 4D allows you to “catch” the movements of the baby. The image is the same as in 3D, but it is very clearly visible how the baby moves his arms, legs, fingers, how he smiles, and sometimes you can even see how he pees.