Migraine and pregnancy first trimester
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to WorryMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women.)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger.
 Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom. - Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).
- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells. Examples include paints, perfumes, and your toddler’s explosive diaper.
- Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
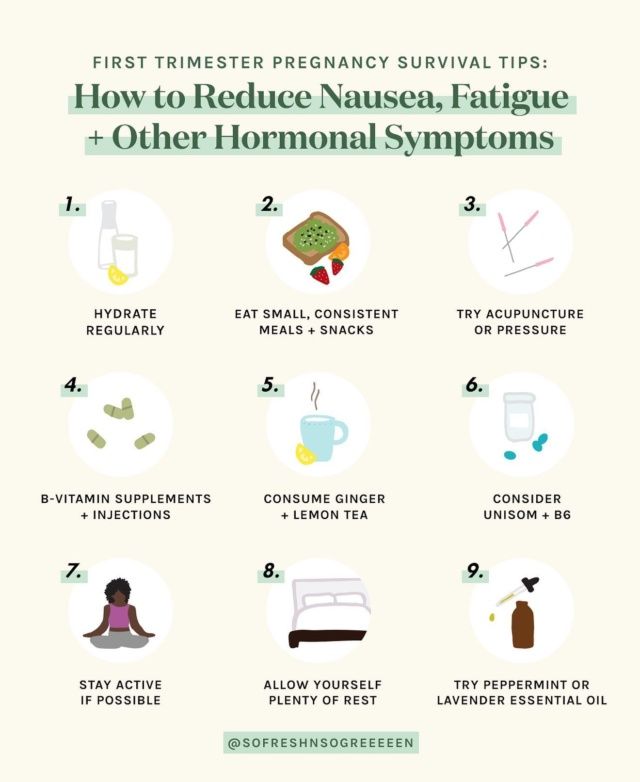
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers. Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
- Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
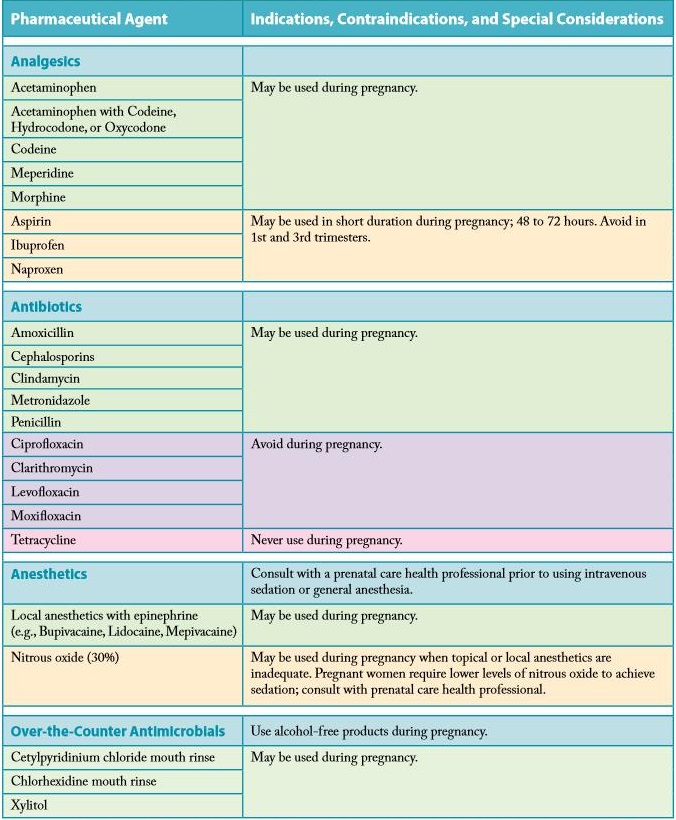
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol. It’s also sold under many other brand names.
- Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.
Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t. Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
- Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects. If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective. The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy. For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ.
 (2009).
(2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine. (2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens.org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant.
 (n.d.).
(n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them. (2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 6, 2020
Written By
Donna Christiano
Edited By
Jessica Jondle
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Copy Edited By
Christina Guzik, BA, MBA
Share this article
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.D.
Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks.
 Here are eight ways you can improve the quality of your sleep for migraine relief.
Here are eight ways you can improve the quality of your sleep for migraine relief.READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.
READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.

READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.

READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Pregnancy Plus: Migraine in pregnancy
BMJ. 2008 Jun 28; 336(7659): 1502–1504.
doi: 10.1136/bmj.39559.675891.AD
Pregnancy Plus
, professor ,1, associate professor,2 and , professor3
Author information Article notes Copyright and License information Disclaimer
The authors explore whether migraine affects pregnancy, how pregnancy alters migraine, and how to treat and prevent migraine in pregnancy
Migraine is common, with a one year prevalence of 12-15% in the Western world.1 The case described here (see the Scenario box) illustrates many of the problems that arise when a patient who has migraines becomes pregnant.
Scenario
A 32 year old woman with a history of episodic headache has recently become aware she is pregnant. She has had troublesome headaches from childhood. She has no other medical problems. Her sister and mother have migraines. She is a non-smoker. In the previous five years, her headaches have become more frequent, with five to seven attacks a month of disabling left or right sided, throbbing pain around the parietal and temporal region. The pain is aggravated by physical activity and any movement and associated with nausea and marked vomiting, prominent photophobia, and phonophobia. The attacks last two to three days. She had no aura symptoms. Neurological and general physical examinations were normal, and thus her diagnosis is migraine without aura.2
She has had minimal benefit from over the counter analgesics, including paracetamol (acetaminophen) with and without codeine; aspirin; metoclopramide; prochlorperazine; domperidone; and non-steroidal anti-inflammatory drugs (notably ibuprofen and naproxen). She was started on sumatriptan 20 mg nasal spray. This provided headache relief in about two hours, with some mild chest discomfort. She was also started on topiramate as a migraine preventive, which, at a dose of 50 mg twice daily, reduced her attack frequency to two a month. Breakthrough attacks were treated with sumatriptan. She had some mild paraesthesia with topiramate but no other side effects. This pregnancy, her first, was unplanned. She is currently at six weeks’ gestation by her last menstrual period.
She was started on sumatriptan 20 mg nasal spray. This provided headache relief in about two hours, with some mild chest discomfort. She was also started on topiramate as a migraine preventive, which, at a dose of 50 mg twice daily, reduced her attack frequency to two a month. Breakthrough attacks were treated with sumatriptan. She had some mild paraesthesia with topiramate but no other side effects. This pregnancy, her first, was unplanned. She is currently at six weeks’ gestation by her last menstrual period.
Migraine is defined by the International Headache Society as a disorder involving headache with particular features—notably, it is usually unilateral and often throbbing and is associated with nausea and sensitivity to light, sound, and head movement.1 More broadly the disorder can be regarded as a substantially inherited disorder in which physiological changes (both external, such as weather change, or internal, such as changes in sleep pattern) often trigger stereotypical attacks, with the features of migraine as defined above. 3 Migraine is three times more common in females than in males, and in females the highest prevalence rates are during the childbearing years, peaking (at 27%) at the age of 41. Migraine has not been proved to affect fertility or the course of a pregnancy,4 but pregnancy substantially alters migraine.
3 Migraine is three times more common in females than in males, and in females the highest prevalence rates are during the childbearing years, peaking (at 27%) at the age of 41. Migraine has not been proved to affect fertility or the course of a pregnancy,4 but pregnancy substantially alters migraine.
Migraine has long been mentioned as a possible predictor of complications in pregnancy,5 although because migraine is so common in females systemically establishing a link to complications in pregnancy has been a challenge. Several associations have been proposed, including miscarriage, pre-eclampsia, congenital anomalies, and low birth weight, but these associations remain clouded by a lack of well controlled studies.
Pregnancy will usually reduce the frequency and severity of migraine attacks. This is especially true for women with migraine without aura. A minority of women have their first migraine attack during pregnancy or in the postpartum period. 15 Migraine attacks often increase in frequency in the first trimester but can be expected to decrease later in pregnancy. However, although attacks are usually less frequent in the second and third trimesters, new onset aura may appear at that time.16
15 Migraine attacks often increase in frequency in the first trimester but can be expected to decrease later in pregnancy. However, although attacks are usually less frequent in the second and third trimesters, new onset aura may appear at that time.16
A recent large prospective study using the International Headache Society’s definition criteria showed that by the third trimester of pregnancy 89% of women had either no attacks or fewer attacks.17 A prospective study of 49 women with migraine reported an 11%, 53%, and 79% reduction in attacks in the first, second, and third trimesters respectively.18 An older retrospective study of 1300 women reported a 67% cessation of migraine in pregnancy,19 and a smaller study of 18 patients found a 41% reduction in the overall frequency of headache.20 Taken together, these studies show that pregnancy is a time of substantial reduction in migraine attacks.
Importantly, pregnancy can alter migraine aura and may trigger attacks of aura without headache. This often leads to a search for intracranial disease—in particular, arteriovenous malformations and intracranial venous sinus thrombosis. Clinically, however, these attacks are typical of aura, with the slow emergence of symptoms, and although cerebral ischaemia is often considered, it is seldom the cause. This change in migraine pattern during late pregnancy is well recognised and usually easy to manage, with excellent prognosis.15
This often leads to a search for intracranial disease—in particular, arteriovenous malformations and intracranial venous sinus thrombosis. Clinically, however, these attacks are typical of aura, with the slow emergence of symptoms, and although cerebral ischaemia is often considered, it is seldom the cause. This change in migraine pattern during late pregnancy is well recognised and usually easy to manage, with excellent prognosis.15
Although the relative hormonal stability in pregnancy is generally considered to be the basis for the improvement in headache, the detailed physiological mechanisms are not understood.4
The two main areas of concern are treating an acute migraine and preventing attacks. When planning pregnancy, women should find it useful to discuss the treatment options that exist for the acute attack (table 1). It should be noted that ergotamine is specifically contraindicated in pregnancy. Paracetamol (acetaminophen) is a safe treatment for acute migraine in pregnancy, but it may provide no benefit.
Table 1
Safety profiles in pregnancy and breast feeding for drugs commonly used for treating acute attacks of migraine23 24
| Drug | Fetal risk | Breast feeding | ||
|---|---|---|---|---|
| FDA | TERIS | |||
| Paracetamol (acetaminophen) | B | None | Caution | |
| Dihydroergotamine | X | Minimal | Contraindicated | |
| Ergotamine | X | Undetermined | Contraindicated | |
| 5-HT1 agonists | C | Undetermined | Probably compatible | |
| Aspirin | C* | Minimal | Compatible | |
| Caffeine | B | None | Compatible | |
| Ibuprofen | B* | Minimal | Compatible | |
| Naproxen | B* | Undetermined | Compatible | |
| Codeine | C** | Unlikely | Compatible | |
| Pethidine (meperidine) | B** | Unlikely | Compatible | |
| Morphine | B** | Unlikely | Compatible | |
| Prednisolone | C* | None or minimal | Compatible | |
| Prochlorperazine | C | None | Concern | |
Open in a separate window
FDA=US Food and Drug Administration.
TERIS= Teratogen Information System (a consensus of expert opinion and literature that assesses teratogenic risk from drug exposure).
FDA ratings: A=controlled studies show no risk; B=no evidence of risk in humans; C=risk cannot be ruled out—use if benefit justifies potential risk; D=positive evidence of risk—use if benefits outweigh risk; X=contraindicated in pregnancy—risk outweighs any possible benefit). *Rating D if used in third trimester. ** = rating D if used when pregnancy is prolonged or at term.
The FDA categories provide therapeutic guidance.
The data are still accumulating, but current evidence suggests that sumatriptan does not carry a risk to either the fetus or the mother.1214 The best data for sumatriptan can be found on the sumatriptan and naratriptan pregnancy registry, where the most recent data have been reported in February 2008. The authors report 516 cases of exposure to sumatriptan and 46 cases of exposure to naratriptan in pregnancy, with a reported 4. 4% (95% confidence interval 2.7% to 7.0%) rate of birth defects for exposure in the first trimester, which is in line with the prevalence of birth defects in women with migraine (3.4%; 2.1% to 4.6%).11
4% (95% confidence interval 2.7% to 7.0%) rate of birth defects for exposure in the first trimester, which is in line with the prevalence of birth defects in women with migraine (3.4%; 2.1% to 4.6%).11
For many patients, the first trimester will be well advanced by the time the pregnancy is confirmed. The most important thing the pregnant woman who experiences migraine can do in the first trimester is to see her physician and establish a treatment plan. Preventive agents not recommended during pregnancy should be stopped, so a plan should be drawn up for treating any migraine attacks that occur. The nausea and vomiting that often accompany migraine may be exacerbated by pregnancy associated nausea, which places the woman at risk for dehydration. We believe that opioids and antiemetics are often the treatment of choice for acute migraine during pregnancy whereas that is not the case outside pregnancy. Prochlorperazine (both the oral and the suppository form) is safe and effective for both nausea and headache.
No particular problems arise for women with migraine around the time of the birth. Postpartum headache is common, occurring in about 34% of women.18 It is most common during days 3 to 6 postpartum and is associated with a personal history or family history of migraine. Postpartum headache, although usually less severe than patients’ typical migraine, is usually bifrontal, prolonged, and associated with photophobia, nausea, and anorexia.2122
No direct data exist to establish that any particular triggers are worse than others in the postpartum period. In the absence of a specific contraindication such as coronary or cerebrovascular disease, sumatriptan by injection is an ideal way to deal with disabling migraine in this period, even for breastfeeding women. Preventive agents can be reintroduced during breast feeding. Table 2 lists the current options for prevention and the level of recommendation as classified by the US Food and Drug Administration and TERIS (the Teratogen Information System).
Table 2
Safety profiles in pregnancy and breast feeding for drugs commonly used for preventing migraine23 24
| Drug | Fetal risk | Breast feeding | ||
|---|---|---|---|---|
| FDA | TERIS | |||
| β blockers | ||||
| Atenolol | D | Undetermined | Caution | |
| Metoprolol | C** | Undetermined | Compatible | |
| Nadolol | C** | Undetermined | Compatible | |
| Propranolol | C** | Undetermined | Compatible | |
| Timolol | C** | Undetermined | Compatible | |
| Neuromodulators | ||||
| Gabapentin | C | Undetermined | Probably compatible | |
| Topiramate | C | Undetermined | Caution | |
| Semisodium valproate | D | Moderate | Compatible | |
| Serotonin antagonists | ||||
| Pizotifen | NA | Safety not established | Caution | |
| Methysergide | X | Safety not established | Contraindicated | |
| Calcium channel blockers | ||||
| Flunarizine | NA | Safety not established | Contraindicated | |
| Tricylics | ||||
| Amitriptyline | C | Unlikely | Concern | |
| Imipramine | C | Unllikely | Concern | |
| Nortriptyline | C | Undetermined | Concern | |
Open in a separate window
FDA=US Food and Drug Administration.
NA= not applicable.
TERIS=Teratogen Information System (a consensus of expert opinion and literature that assesses teratogenic risk from drug exposure).
FDA ratings: A=controlled studies show no risk; B=no evidence of risk in humans; C=risk cannot be ruled out—use if benefit justifies potential risk; D=positive evidence of risk—use if benefits outweigh risk; X=contraindicated in pregnancy—risk outweighs any possible benefit. ** = rating D if used when pregnancy is prolonged or at term.
The FDA categories provide therapeutic guidance.
Migraine prevention is more difficult when a patient is pregnant. Preventive agents are associated with the possibility of complications during pregnancy, so they should ideally be stopped in women planning to conceive (table 2). Propranolol is both effective and safe. Unfortunately, the neuromodulators, valproate (semisodium), topiramate, and gabapentin, are not established as safe; valproate is a known teratogen.2324
Methods
We searched the literature from PubMed using the terms “migraine” and “pregnancy” and reviewed our own database of references from meetings of the International Headache Society and the American Headache Society over the past 20 years.
This is one of a series of occasional articles about how to manage a pre-existing medical condition during pregnancy.
Contributors: PJG wrote the first draft. SDS and JG reviewed the manuscript and made substantial contributions to the content. PJG acts as guarantor.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Patient consent not needed (patient hypothetical).
1. Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American migraine study II. Headache 2001;41:646-57. [PubMed] [Google Scholar]
2. Headache Classification Committee of the International Headache Society. The international classification of headache disorders. 2nd ed. Cephalalgia 2004;24(suppl 1):1-160. [Google Scholar]
3. 3Lance JW, Goadsby PJ. Mechanism and management of headache 7th ed. New York: Elsevier, 2005
4. Olesen J, Tfelt-Hansen P, Ramadan N, Goadsby PJ, Welch KMA. The headaches Philadelphia: Lippincott, Williams & Wilkins, 2005
The headaches Philadelphia: Lippincott, Williams & Wilkins, 2005
5. Philipp EE. Obstetrics in general practice. Minor disorders of pregnancy. BMJ 1964;i:749-52. [PMC free article] [PubMed]
6. Hughes G. Hughes syndrome: the antiphospholipid syndrome—a clinical overview. Clin Rev Allergy Immunol 2007;32:3-12. [PubMed] [Google Scholar]
7. Mitsikostas DD, Sfikakis PP, Goadsby PJ. A meta-analysis for headache in systemic lupus erythematosus: the evidence and the myth. Brain 2004;127:1200-9. [PubMed] [Google Scholar]
8. Adeney KL, Williams MA. Migraine headaches and preeclampsia: an epidemiologic review. Headache 2006;46:794-803. [PubMed] [Google Scholar]
9. Sanchez SE, Qiu C, Williams MA, Lam N, Sorensen TK. Headaches and migraines are associated with an increased risk of preeclampsia in Peruvian women. Am J Hypertens 2008;21:360-4. [PubMed] [Google Scholar]
10. Diener HC, Kurth T, Dodick D. Patent foramen ovale and migraine. Curr Pain Headache Rep 2007;11:236-40. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
11. Wainscott G, Sullivan FM, Volans GN, Wilkinson M. The outcome of pregnancy in women suffering from migraine. Postgrad Med J 1978;54:98-102. [PMC free article] [PubMed] [Google Scholar]
12. Kallen B, Lygner PE. Delivery outcome in women who used drugs for migraine during pregnancy with special reference to sumatriptan. Headache 2001;41:351-6. [PubMed] [Google Scholar]
13. Olesen C, Steffensen FH, Sorensen HT, Nielsen GL, Olsen J. Pregnancy outcome following prescription for sumatriptan. Headache 2000;40:20-4. [PubMed] [Google Scholar]
14. Evans EW, Lorber KC. Use of 5-HT1 agonists in pregnancy. Ann Pharmacother 2008;42:543-9. [PubMed] [Google Scholar]
15. Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 1992;12:221-8. [PubMed] [Google Scholar]
16. Silberstein SD, Lipton RB, Goadsby PJ. Headache in clinical practice 2nd ed. London: Martin Dunitz, 2002
17. Melhado EM, Maciel JA Jr, Guerreiro CA. Headache during gestation: evaluation of 1101 women. Can J Neurol Sci 2007;34:187-92. [PubMed] [Google Scholar]
Headache during gestation: evaluation of 1101 women. Can J Neurol Sci 2007;34:187-92. [PubMed] [Google Scholar]
18. Sances G, Granella F, Nappi RE, Fignon A, Ghiotto N, Polatti F, et al. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia 2003;23:197-205. [PubMed] [Google Scholar]
19. Granella F, Sances G, Zanferrari C, Costa A, Martignoni E, Manzoni GC. Migraine without aura and reproductive life events: a clinical epidemiological study in 1300 women. Headache 1993;33:385-9. [PubMed] [Google Scholar]
20. Marcus DA, Scharff L, Turk D. Longitudinal prospective study of headache during pregnancy and postpartum. Headache 1999;39:625-32. [PubMed] [Google Scholar]
21. Goadsby PJ, Lipton RB, Ferrari MD. Migraine—current understanding and treatment. New Engl J Med 2002;346:257-70. [PubMed] [Google Scholar]
22. Stein G, Morton J, Marsh A, Collins W, Branch C, Desaga U, et al. Headaches after childbirth. Acta Neurol Scand 1984;69:74-9. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
23. Briggs GG, Freeman RK, Yaffe SJ. Drugs in pregnancy and lactation. 7th ed. Philadelphia: Lippincott Williams & Wilkins, 2005
24. Friedman JM, Polifka JE. Teratogenic effects of drugs Baltimore: Johns Hopkins Press, 2000
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations. This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make seizures less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods.
 Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted.
 However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Follow our Instagram to read the latest materials on the diagnosis and treatment of headaches!
cluster headache. Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Migraine during pregnancy - Juno
Migraine during pregnancy - Junohome
Articles
Migraine during pregnancy
How to recognize an attack and deal with it properly - read on. We will tell you how dangerous migraines are and how to get rid of them safely during pregnancy.
Contents of the article
Features and manifestations of migraine during pregnancy
If a woman was worried about migraines before pregnancy, then during the bearing of a child, the attacks are more likely to stop, or become milder and rarer. Improvements come from the 2nd trimester and are due to the fact that fluctuations in estrogen levels stop. In the early stages, the likelihood of migraine is higher. In the 1st trimester, ailments often occur, including headaches. But it's not always a migraine.
In the early stages, the likelihood of migraine is higher. In the 1st trimester, ailments often occur, including headaches. But it's not always a migraine.
Migraine symptoms in pregnant women are similar to those that occur in other people. Approximately the picture looks like this:
- Harbingers. They are not characteristic for everyone and may be absent. They occur 1-3 days before an attack, manifest as irritability, depression, or, conversely, a surge of activity.
- Headache. Very intense, more often covers the temporal or frontal region, has a pulsating, arching character. It can be localized in one half of the head, but sometimes it spreads to the entire head. The pain lasts from 2-3 hours to several days, it is difficult to remove.
- Aura. It also doesn't happen to everyone. The phenomenon accompanies headache and lasts 10-40 minutes. Patients note flashes of light, spots, flies before the eyes, sometimes numbness of the extremities worries.
 With an aura, it is almost impossible to do something around the house or work.
With an aura, it is almost impossible to do something around the house or work.
Even after the pain passes, the expectant mother experiences depression, fatigue, irritability. Unpleasant sensations continue for about a day.
Why do pregnant women get migraines
The exact cause of the disease has not been established. However, experts single out hormonal changes in the body and an increased load on the body during pregnancy among the provoking factors.
General risk factors:
- sudden change in weather - especially for weather-sensitive women;
- stress and depression have a bad effect on blood vessels and the nervous system;
- violation of the diet - long intervals between meals, overeating, abuse of citrus fruits, smoked products and chocolate;
- overwork - physical fatigue at home and at work, sleep disturbances;
- irritants - unpleasant odors, stuffiness, excessive light or noise;
- fluid deficiency - dehydration due to insufficient water intake;
- concomitant pathologies, for example, hypertension.

The condition of pregnant women is adversely affected by weight gain, hypothermia and overheating. This can also provoke migraine attacks, especially if they have happened before.
Are seizures dangerous for the fetus
By itself, migraine during pregnancy is not critical. If the seizures are not caused by more serious problems - hypertension, eclampsia, then a woman is highly likely to give birth to a healthy child at term. Migraine does not increase the risk of preterm birth or developmental anomalies in the fetus.
But despite the safety for the baby, migraines are debilitating for a pregnant woman. This affects general well-being - worsens sleep, nutrition, causes stress, decreased activity. Therefore, too frequent seizures can result in problems with the nervous system, fetal hypoxia. It is important to help yourself in time.
Treatment of migraine during pregnancy
Tablets should be taken only as a last resort. In the early stages, strong drugs are prohibited. First, try to cope with non-drug methods:
In the early stages, strong drugs are prohibited. First, try to cope with non-drug methods:
- Drink sweet tea or cola. Caffeine in small doses is harmless and can help relieve headaches.
- Take a walk in the fresh air, do simple exercises. This contributes to the outflow of blood from the vessels of the brain and the elimination of pain.
- Apply a warm or cool compress to the head. It can be a towel moistened with water or a heating pad.
- Take a cool shower (but not too cold). The procedure is useful as a prevention of varicose veins and migraines.
- Relax and sleep in a quiet, dark room.
- Do not hold back the urge to vomit - it can relieve an attack of pain.
- Rub essential oils of lemon, orange, lemon balm into whiskey - just a little is enough. Too much oil can make headaches worse. If you have previously noticed such a reaction of your body to odors, you should not apply this method now.
- Drink freshly squeezed juice or clean water.
 Replenishing fluids often helps get rid of a migraine.
Replenishing fluids often helps get rid of a migraine.
If the above measures do not help, and the seizures are disturbing enough, you need to consult a doctor. The specialist will prescribe treatment, for example, prescribe pills that will help to cope with pain. The safest drug is paracetamol. It can be taken on its own. The doctor may prescribe magnesium for treatment - it has a beneficial effect on blood vessels.
In some cases, ibuprofen and aspirin are acceptable (only in the 2nd trimester). Opioid analgesics and triptans are strictly prohibited. If a migraine is growing or has appeared for the first time, an aura has joined, pressure rises, you should definitely consult a doctor in the near future.
Prophylaxis
Dealing with migraines during pregnancy is not always easy. It is better to follow some rules that will help reduce the risk of seizures:
- Stick to a sleep and rest routine.
- Control sweets and fatty foods.

- Try to walk every day, do light exercises.
- Massage or self-massage the head and collar area. Movements should be light: it is better if the specialist shows what they should be.
Even if an attack has already happened, try not to abruptly get involved in worries and affairs after it. Remember that you are responsible not only for yourself, but also for the child. Do not be shy to turn to your loved ones for help and do not be heroic. Be healthy!
Other articles
10.10.2022
eighth week of pregnancy
So, the 8th obstetric week of pregnancy refers to the 1st trimester, which is especially important for the development of the unborn child, since it is at the period of 8-9 weeks of pregnancy that the laying and development of your baby's organs and systems occurs.