Frequent urination after c section
What Can Cause Bladder Problems after a C-Section?
It was recently announced that c-sections have doubled since 2000 because of the fear of labour pain, sexual dysfunction and the fear of incontinence related to vaginal delivery.
It is common knowledge that women who have a natural childbirth have a higher chance of developing incontinence later in life, it has therefore become very common for pregnant women who have experienced leakage before childbirth to be concerned. Chair of FIGO’s Safe Motherhood Committee, asserted: “worldwide there is an alarming increase in caesarean section rates". However, experts are becoming more adamant that women should not choose this option just to avoid incontinence.”
Did you have a C-Section delivery? Post a question on our forum and share your experience.
Experts are worried that women are not aware of the potential complications of having a caesarean section and that glossing over the risks and side effects are common. Maternal death and disability rates are higher with c-sections and it is known to increase conditions such as asthma. Surprisingly, research has even shown that susceptibility of incontinence is genetic to some degree, and a substantial number of women who choose c-sections over natural birth do end up leaking.
Those who choose c-sections should remember that any kind of childbirth causes tears and strains on the body, and as researcher Goldberg explains: “things tend to equalize due to wear and tear and gravity”. As your baby grows in pregnancy, your uterus becomes heavier and your supporting structures are therefore become stretched and weakened. Hormones during pregnancy also contribute to the loosening of ligaments and muscles. A study in 2011 found that c-sections only drastically lower the risk of bladder problems if a woman delivers all of her children that way. This study found that 55% of women who had vaginal birth experienced incontinence, and 59% of women who had one vaginal birth and one caesarean had incontinence. Glazener explains, “unless women are resolved to have all their deliveries by the abdominal route, caesarean section doesn’t necessarily protect from incontinence”.
Glazener explains, “unless women are resolved to have all their deliveries by the abdominal route, caesarean section doesn’t necessarily protect from incontinence”.
However, unique to c-sections is the scar. During a c-section an incision is made meaning a scar will form as part of the healing process. A temporary scab can form too close to the edges of the incision and as a result, the body creates scar tissue from collagen which can extend into deeper layers below the skin. These collagen fibres in scar tissue are formed in a single linear direction which can cause a variety of problems including bladder problems as the scar can attached to the front wall of your bladder causing urge incontinence and frequent urination. Physical therapist Kristen Maike explains “as everything shrinks back down after the birth, the scar begins tugging on the bladder. This makes it feel like you have to pee”. A 40 year old Doctor and mother, Ellen, is one of many women who experienced the side effects of a c-section scar. After the operation, her left leg was not responding well to the brain due to nerves being trapped – the scar was shutting off the muscles to her left leg and anterior pelvic muscles causing incontinence. Neurokinetic Therapy was used to reprogram her neurological system and restore muscular control and coordination. She was eventually able to regain leg movement and her incontinence cleared.
After the operation, her left leg was not responding well to the brain due to nerves being trapped – the scar was shutting off the muscles to her left leg and anterior pelvic muscles causing incontinence. Neurokinetic Therapy was used to reprogram her neurological system and restore muscular control and coordination. She was eventually able to regain leg movement and her incontinence cleared.
When is a C-Section Urgently Needed?
A C-Section consists of delivering the baby through a cut made in the abdomen and womb. It can be necessary for the following reasons:
- Your labour isn’t progressing as expected
- Your baby is in a bottom-down, or breech, position
- Your baby is in a sideways position or keeps changing position
- Yours or your baby’s health is at risk
- Your baby is too large for vaginal birth
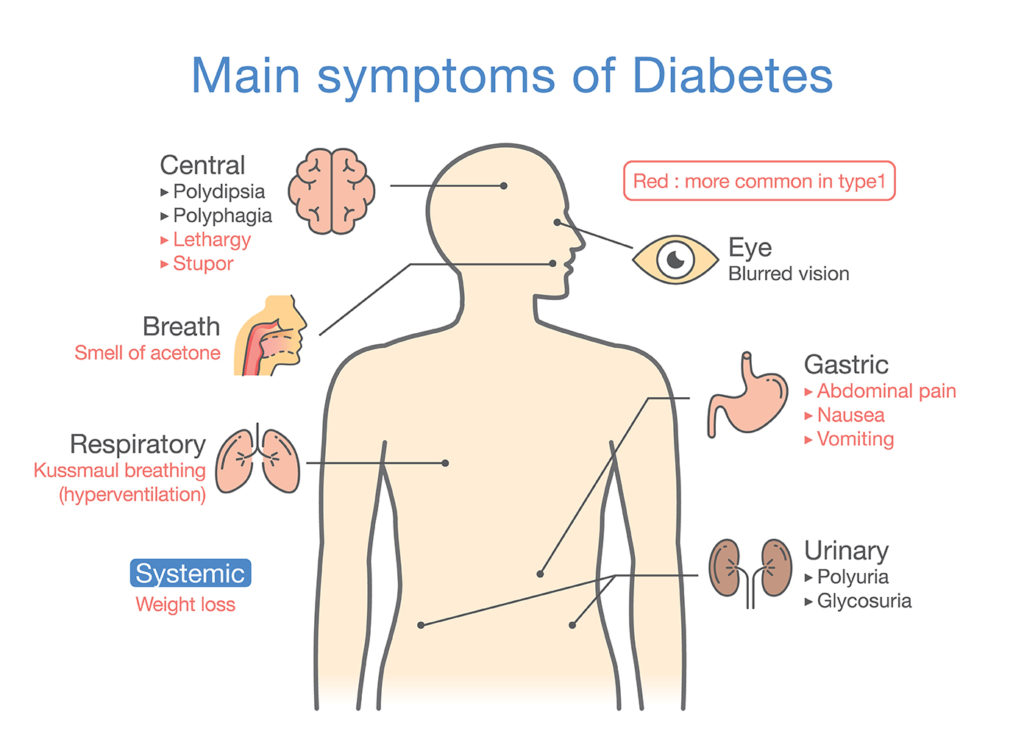
- You have a serious medical condition, such as Diabetes or heart disease
- You are expecting twins
Who is More at Risk of Incontinence after a C-Section?
Women with gestational diabetes and women who smoke often are at risk of developing incontinence after a c-section.
Are you currently pregnant and experiencing leaks? Read about managing incontinence during pregnancy.
Most women see improvements or completely cure their incontinence after a c-section with the help of pelvic floor exercises. Expert Maike asserts, “it’s worth checking with your Doctor or a pelvic floor physical therapist to ensure you are doing these exercises correctly”. You can read about how to do pelvic floor exercises here. Incontinence requires the ideal protective products to manage leaks. For light incontinence, we recommend small shaped pads and pull up pants. If your incontinence is heavy to severe, we recommend using pull ups, all in ones or large pads. Here are some of our product recommendations:
Here are some of our product recommendations:
Ideal For: Moderate to Severe Incontinence
Prices Online:Incontinence Supermarket: £6.49 to £12.60 (Packs of 20, 22, 24, 26) Allanda: £6.49 to £12.59 (Packs of 20, 22, 24, 26)
TENA PantsIdeal For:
Moderate to Heavy Incontinence
Prices Online:Incontinence Supermarket: £4.89 to £13.95 (Packs of 8, 9, 10, 12, 14, 15, 18) Allanda: £7.20 to £13.95 (Packs of 8, 9, 10, 12, 14, 15, 18)
Attends Contours Ideal For:Light to Heavy Incontinence
Prices Online:Incontinence Supermarket: £6. 20 to £9.40 (Packs of 21, 28, 35, 42) Allanda: £6.20 to £9.40 (Packs of 21, 28, 35, 42)
20 to £9.40 (Packs of 21, 28, 35, 42) Allanda: £6.20 to £9.40 (Packs of 21, 28, 35, 42)
The Connection Between C-Sections and Urinary Incontinence
Posted on
by Michelle Stepp
Finding out you’re pregnant can be a time that is full of excitement and joy! However, sometimes there may be some topics of concern that may come up along your journey. You might have a pre-existing health condition or a problem arises and your doctor may feel that having a traditional vaginal birth may be too risky. Some serious thoughts and conversations might lie ahead and the topic of delivering your child via c-section could be the safest choice.
What is a C-Section and When is it Needed?
What is a c-section?
Cesarean birth, which is often referred to as a c-section, is a surgical procedure performed by a doctor to deliver a newborn through an incision that is made in the abdomen and uterus. It may be a safer option rather than vaginal birth if the goal is to protect the newborn’s health or if the mother has a medical condition that can affect the pregnancy. A c-section can be either scheduled to coincide with the planned due date or it can be an emergency if the mother or baby’s health is in immediate danger.
It may be a safer option rather than vaginal birth if the goal is to protect the newborn’s health or if the mother has a medical condition that can affect the pregnancy. A c-section can be either scheduled to coincide with the planned due date or it can be an emergency if the mother or baby’s health is in immediate danger.
What are some medical reasons a c-section may be needed?
A c-section may be the best course of action to take due to potential complications that can make vaginal birth unsafe for the mother and/or her baby. A c-section can be necessary for any of the following reasons:
- The baby is too large for a vaginal birth. A very large baby sometimes simply cannot fit through the vaginal opening without causing significant damage.
- The baby is either sideways or breech (feet first instead of head first) in the womb. The position of the baby in this way can be dangerous as there is a risk that oxygen supply through the umbilical cord could be cut off if the baby gets stuck during delivery.
- The mother has a medical condition such as high blood pressure or diabetes. High blood pressure can be risky during pregnancy due to the stress that is put on the heart. When there is a high amount of sugar in the blood, as with diabetes, nerves and blood vessels can be damaged. Both of these medical conditions can make a c-section more favorable for the safety of the mother and her baby.
- If the mother has had a previous c-section, she is at a greater risk for complications during childbirth. There can be scar tissue buildup after each c-section making another incision more difficult and risk damage to the bladder or bowel.
- The mother might have an infection that could potentially be passed on to the baby during vaginal birth. As a safety precaution, a c-section would be a better choice in this case.
- When there are multiple babies in the womb, a c-section is a wise decision so that no harm is done to either the babies or the mother.
Can a C-Section Cause Incontinence?
Childbirth in itself causes strain and tears on a woman’s body. The uterus starts getting heavier as the infant grows and the surrounding structures begin to stretch and weaken. Some women think that having a c-section will prevent them from side effects of vaginal birth like urinary incontinence or fecal incontinence. However, studies have shown that having a c-section doesn’t protect women from suffering from urinary or fecal incontinence. Bladder issues after a c-section are quite common.
The uterus starts getting heavier as the infant grows and the surrounding structures begin to stretch and weaken. Some women think that having a c-section will prevent them from side effects of vaginal birth like urinary incontinence or fecal incontinence. However, studies have shown that having a c-section doesn’t protect women from suffering from urinary or fecal incontinence. Bladder issues after a c-section are quite common.
After the abdominal incision is made during a c-section, scar tissue is formed from collagen during the healing process. The collagen fibers of this scar tissue can extend deep into the layers below the skin and create bladder problems. Bladder issues after a c-section such as urinary incontinence can result when this scar tissue attaches to the wall of the bladder. After a woman gives birth, things begin to reduce back down in size, this scar tissue pulls on the bladder making her feel as though she needs to urinate more urgently (urge incontinence) or more often (overactive bladder).
How Long Does Urinary Incontinence from a C-Section Last?
Urinary incontinence from a c-section can take up to six months, or even longer for some women, to get their bladder functioning like normal again. There are several things that a woman can do to help the process along and get it back faster. In the interim, considering the use of incontinence products such as pads, liners, and protective underwear can help women get through the more difficult times.
How You Can Improve Urinary Incontinence Symptoms from a C-Section
Some of the ways a woman can treat urinary incontinence from a c-section to help her bladder get back to its normal function are:
Kegel Exercises
Strengthening the pelvic floor muscles after delivery is an important part of regaining bladder control. The stronger and more elastic these muscles are, the less stress or urge incontinence is experienced. Starting kegel exercises right after childbirth can greatly reduce urinary incontinence symptoms and get you on the path for normal bladder function sooner rather than later.
A Pessary Ring
A pessary ring is a small, soft, silicone vaginal ring that is inserted into the vagina. Women who can benefit from a pessary ring are those that have urinary incontinence that seems to be persistent. The pessary ring is placed inside the vagina to act as a “speed bump” for the urethra and left there throughout the day. Some women prefer to use a pessary ring only when they engage in activities, while others put it in place in the morning and remove it in the evening. This device can be very helpful for women experiencing bladder issues after a c-section.
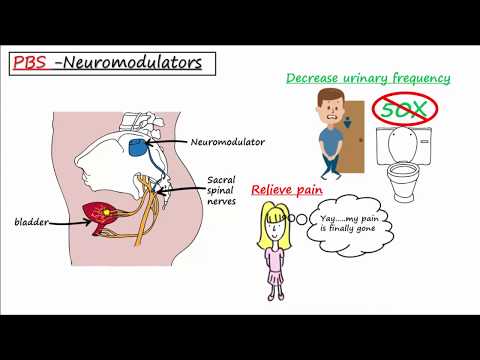
Electrical Stimulation Therapy
By sending mild electrical currents to the muscles in the pelvic floor that are involved in urination, these muscles then contract. By repeating this electrical stimulation pulse, the pelvic floor muscles begin to strengthen, producing a similar effect to what kegel exercises do. A doctor can perform this therapy or the patient can be given a unit to use in the privacy of their own home to help relieve their urinary incontinence symptoms.
Sling Surgery
One of the most common surgeries for urinary incontinence is sling surgery. In this minimally invasive procedure, the surgeon inserts a U- shaped, mesh sling that permanently lifts and supports the urethra like a hammock. This procedure is quick and important to note that it is also permanent, so women that choose this option should not consider any more pregnancies.
Lifestyle Changes
There are many lifestyle changes that can also help women with urinary incontinence to regain bladder control. Many of these might be good to try before choosing some of the more permanent options.
- Remain at a healthy weight. Carrying around extra pounds can put pressure on the bladder and lead to urinary incontinence.
- Maintain a healthy diet. Alcohol, caffeine, and spicy foods tend to aggravate the bladder causing it to contract more often, making urine harder to control.
- Stay hydrated. Try to drink the recommended 8 ounces of water each day.
 Avoiding water as a way to control the number of times you need to use the restroom can result in a urinary tract infection or dehydration. Both are not good for a healthy bladder.
Avoiding water as a way to control the number of times you need to use the restroom can result in a urinary tract infection or dehydration. Both are not good for a healthy bladder. - Stop smoking. Nicotine causes bladder muscles to spasm and women who smoke also often have a chronic cough. Frequent coughing episodes lead to urinary incontinence because of the pressure continuously put on the bladder.
- Pads, liners, and other incontinence products can help absorb leaks and help with urinary incontinence. There are so many options available to women that are concerned about discreetness and living a dignified lifestyle.
As you can see, there is a connection between c-sections and urinary incontinence but you don’t have to let your bladder control your life. There are many options available to treat bladder issues after a c-section such as urinary incontinence, even if you feel that you have exhausted all other avenues.
For questions about any of the incontinence products we carry to help with urinary or fecal incontinence, give us a call. One of our Personally Delivered Product Experts is happy to help.
One of our Personally Delivered Product Experts is happy to help.
Popular Incontinence Products for Women
Posted in Incontinence ResourcesTagged c-section incontinence, incontinence after c-section, incontinence after giving birth
Problems with urination after childbirth: pain, cramps, burning
PreviousNext
- Problems with urination after childbirth
- How to speed up the recovery of bladder functions
- It is recommended to consult a doctor
Contents:
During the postpartum period, many women have difficulty urinating. Lack of urge or, conversely, too frequent urge, pain, leakage when coughing or laughing is a consequence of stretching the muscles of the pelvic floor and reducing the tone of the bladder.
Problems with urination after childbirth
After giving birth, a woman may not feel like going to the toilet at all, even when her bladder is already full.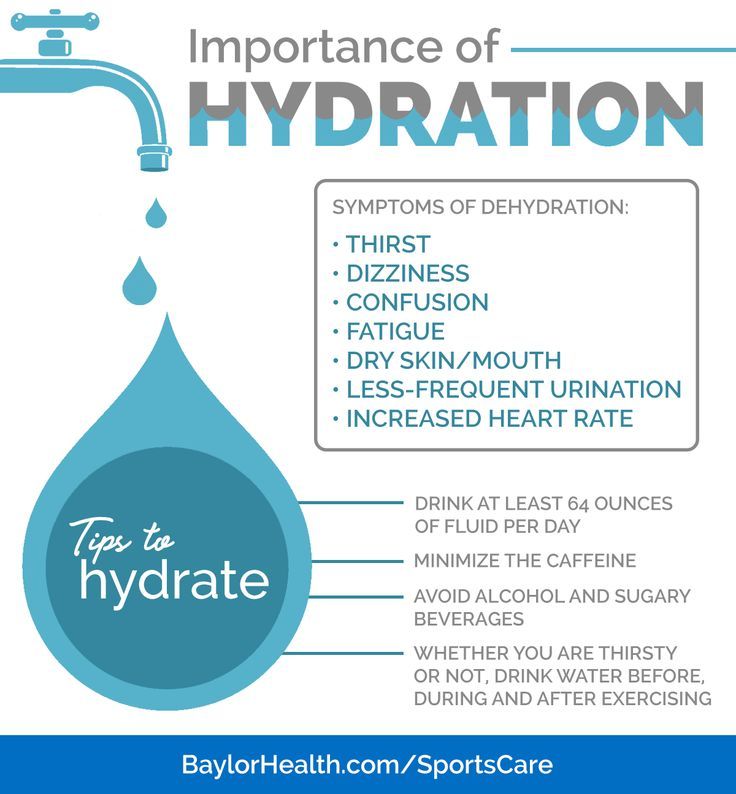
This is due to the fact that the pressure of the uterus on the bladder disappears, the tone of the bladder decreases, it increases in size, swells and begins to accumulate a lot of fluid. His sensitivity may decrease due to the use of painkillers in childbirth, muscle spasms, or fear of pain.
This problem does not require special treatment: gradually the tone of the bladder increases, the swelling subsides, and urination returns to normal. It’s just worth at first regularly reminding yourself that you need to visit the toilet.
Frequent and profuse urination in the first days after childbirth indicates the removal of excess fluid from the body. If you often want to go to the toilet, and the amount of urine is scanty, it is better to consult a doctor, as this may be a sign of the onset of inflammation of the bladder or urethra.
Most often, burning and pain are explained by the ingress of urine on abrasions that appeared during childbirth, and unhealed sutures. To reduce discomfort, you can urinate while standing in the shower with your legs wide apart so that the stream of urine does not touch the external genitalia.
To reduce discomfort, you can urinate while standing in the shower with your legs wide apart so that the stream of urine does not touch the external genitalia.
If painful urination does not go away after healing of abrasions and stitches (usually on the second or third day) or the bladder itself hurts, this may be a symptom of urethritis or cystitis.
After natural childbirth, the pelvic floor muscles stretch and lose elasticity, relieving pressure on the bladder and urethra. As a result, the bladder loses its ability to close completely, so when laughing or coughing, a few drops of urine may be released. Many women are embarrassed by this delicate problem, but in fact, it can be dealt with with the help of sanitary pads and Kegel exercises.
How to speed up recovery of bladder function
If you find it difficult to get up, use the vessel, but not cold, but preheated. Urination can be caused reflexively - the sound of flowing water. If you couldn’t go to the toilet on your own, inform the nurse who will put the catheter.
-
Bladder exercise: do not reduce fluid intake, especially if breastfeeding.
-
Force the bladder to work: in the first days after childbirth, go to the toilet every two hours, even if you do not feel the urge.
-
Walk more: this stimulates the normal functioning of the intestines and bladder.
-
Do special pelvic floor exercises called Kegel exercises.
In a lying or sitting position, tighten the muscles of the vagina and anus as if you are holding back urination, stay in this position for a few seconds, and then completely relax the muscles. When doing the exercises, do not strain your stomach and buttocks and do not move your legs together. Kegel exercises are recommended to be done at least 3 times a day, and preferably more often. In one approach, it is optimal to perform 8-10 muscle contractions.
-
Refuse to use drinks and foods that irritate the bladder - coffee, hot spices, pickles, smoked meats.

It may take from several days to one and a half months to restore the normal functioning of the bladder. If during this time the incontinence does not go away, you need to inform the gynecologist about this at the scheduled examination, which usually happens six weeks after the birth.
It is recommended to see a doctor if:
-
after healing of tears or incisions in the perineum, you still experience pain or burning in the urethra or in the bladder area;
-
frequent urge to urinate, but scant amount of urine;
-
urine cloudy and with a sharp, unpleasant odor;
-
body temperature is increased, even slightly.
These symptoms may be a sign of the development of a urinary tract infection, which, if not properly treated, will cause pyelonephritis. Treatment today can be successfully combined with breastfeeding, so do not be afraid to seek medical help if your bladder does not work like clockwork after childbirth.
| Authors: | Huggies experts |
References:
-
Caring for your Bladder During and after Delivery. University of Michigan Health System.
-
Chaunie Brusie. Postpartum Incontinence Causes and Treatment. Verywell Family. Updated on August 04, 2019.
-
After birth—bladder assessment. Mater Mothers' Hospital.
-
Urinary Incontinence and Pregnancy. WebMD.
-
10 truths: leaking urine in pregnancy and after birth. NCT UK.
Read us on Yandex Zen
PreviousNext
Urinary incontinence and other health issues after childbirth - Useful articles
There are two types of incontinence: in one case it is associated with an irresistible urge (as they say, "did not reach the toilet"), in the other case, involuntary urination occurs when intra-abdominal pressure increases during exercise , laughing, coughing, sneezing, etc.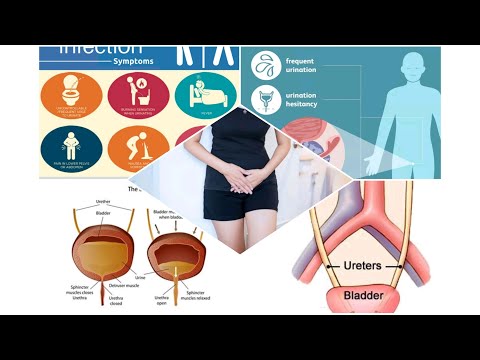 There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
The problem in most cases is not solved by itself, causing physical and psychological inconvenience and suffering (the need to walk around with pads and diapers) and reducing the quality of life, including intimate life. They are embarrassed to talk about it, and compared to how many people are prone to this problem, only a few seek help. Often they simply do not know who exactly to turn to - they go to a gynecologist, and to a therapist, and to a neuropathologist, while this should be done comprehensively and always with the participation of a urologist.
Therapeutic exercise for incontinence
In women after childbirth, disorders of vascular circulation and nervous regulation in the pelvic area are not uncommon. If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
1. Slow contractions: tighten the muscles as if to stop urination, slowly count to three. To relax.
2. Contractions: tense and relax these same muscles as quickly as possible.
3. Push-ups: tense the perineum and abdominal muscles.
Special therapeutic exercises also help to strengthen the muscles of the small pelvis.
1. I.P. lying on your back. We exhale, draw in the stomach, pull the knees to the chest.
2. I.P. Same. Alternately raise straight legs and make circular movements out and in with full amplitude.
3. From the same position, on exhalation, we pull the chest to the bent knees and clasp them with our hands.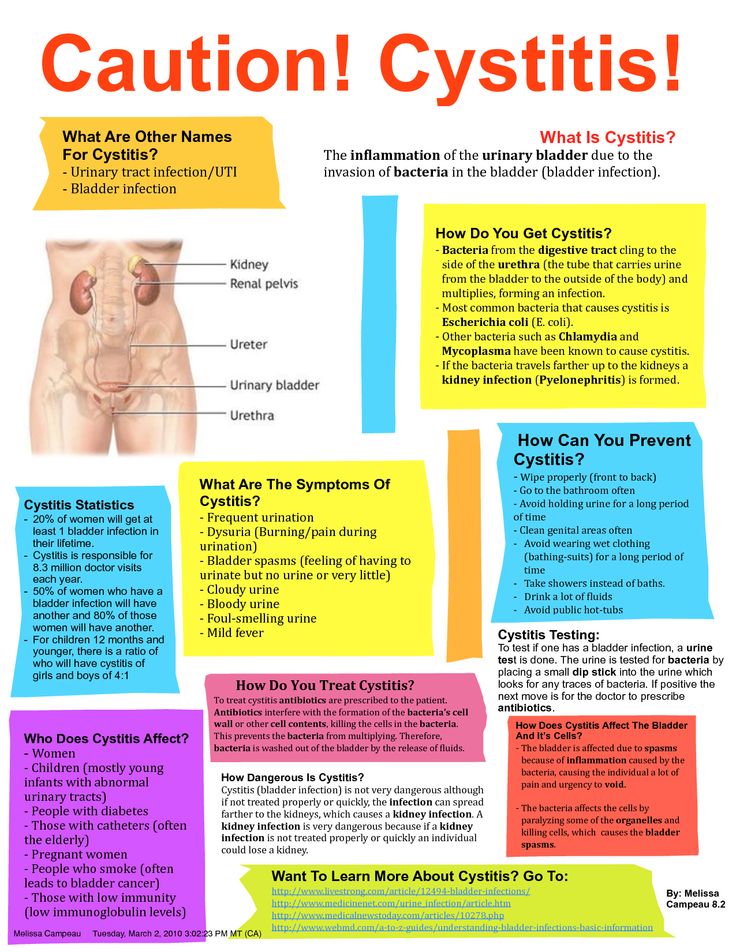
4. Now we raise the upper part of the body and sit down, wrapping our arms around our knees.
5. At the expense of 1-2-3, raise the upper body and one leg, to which we reach with the same hand. We go down to count 4.
6. Knees bent. At the expense of 1-2-3, we raise the pelvis, squeeze the buttocks, retract the anus. On the count of 4, lower the pelvis and relax.
7. From the same position, we lay bent knees to the right and left of the body.
8. I.P. standing, with support. On the inhale we rise on our toes, on the exhale we squat, holding on to the chair.
9. In the same position, holding on to the support, we roll from toes to heels and back.
10. I.P. On knees. Sit on your heels, stretch your arms up.
11. From the same position, alternately straighten the legs and pull them back. Shoulders-back-leg at the same time form one straight line.
12. Standing on all fours, alternately pull opposite arm and leg: straighten on the count of times, hold 2-3, return to the starting position on the count of 4. Be careful not to arch your back.
Be careful not to arch your back.
13. From the same starting position on count 1 stretch one leg back, on count 2-3 take it to the side parallel to the floor, bending at the knee, on count 4 return to the starting position.
14. I.P. hands on the belt, one foot is on the chair. We lean forward and reach for the raised leg, bending it at the knee as much as possible.
There is no need to despair: although treatment is not an easy process due to the large number of components involved in the formation of this syndrome, it is very effective. In all cases, it begins with conservative methods: medicines, physiotherapy and, of course, the therapeutic exercises we have already mentioned. Refrain from activities that increase intra-abdominal pressure. If conservative treatment does not help, low-traumatic surgical methods come to the rescue in the form of imposing various types of loops.
Problems in the perineum
During childbirth, injuries to the soft tissues of the perineum are possible. Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Sometimes an episiotomy is done for the benefit of the baby and mother. Healing is very fast due to tissue matching and a powerful hormonal explosion. The main task of the mother, if she has stitches, is to keep them clean. This, of course, is hygiene (washing twice a day, from front to back, you can use a decoction of chamomile or a weak solution of potassium permanganate) and ensuring oxygen access. Associated with the latter is the ban on underwear and pads, which causes violent protest among women in maternity hospitals.
One should not underestimate such an important moment as the normalization of the stool on the third day after childbirth. Defecation does not provoke the divergence of the sutures, on the contrary, this stool retention can lead to trouble, so try to achieve a soft and spontaneous stool by the third day, and upon returning from the hospital, consult a doctor to make sure that the sutures are healing correctly, without divergence and suppuration.
Uterus and vagina
Some women who have recently given birth complain of vaginal gaping, even asking to "sew it up so that it was like before." Bringing the vaginal ring back to normal is really very important, but this process takes some time. During childbirth, the vagina stretches to let the baby through. Closing occurs within six months, which can be accelerated, for example, by the already mentioned Kegel exercise or the mixing-breeding of the legs.
Immediately after delivery, the uterus should empty well, so turn over, give a vertical load. This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
The return of the tone of the soft tissues of the perineum will also be helped by sexual intercourse, which improves tissue nutrition. Please note: they are allowed when the placental site has been restored in the uterine cavity and there is no longer a risk of inflammation. If you feel pain during intercourse, do not hesitate to tell the doctor about it - he will find out the reason and advise the appropriate position.
Hemorrhoids
Another problem after the birth of a baby is hemorrhoids - a frequent manifestation of varicose veins.