Birth canal diagram
birth | Definition, Stages, Complications, & Facts
birth
See all media
- Key People:
- Virginia Apgar Hugh Chamberlen, the Elder Sir James Young Simpson, 1st Baronet Walter Channing Gertie F. Marx
- Related Topics:
- multiple birth presentation natural childbirth labour dilatation
See all related content →
Summary
Read a brief summary of this topic
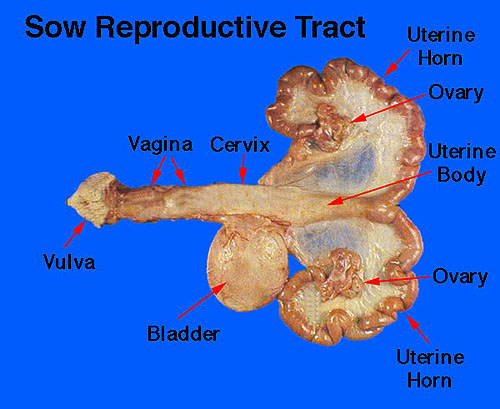
birth, also called childbirth or parturition, process of bringing forth a child from the uterus, or womb. The prior development of the child in the uterus is described in the article human embryology. The process and series of changes that take place in a woman’s organs and tissues as a result of the developing fetus are discussed in the article pregnancy.
Initiation of labour
Despite decades of research, the events leading to the initiation of labour in humans remain unclear. It is suspected that biochemical substances produced by the fetus induce labour. In addition, the timing of the production of these substances and their interaction with placental and maternal biochemical factors appear to influence this process. Among the most studied of these biochemical substances are fetal hormones such as oxytocin and placental inflammatory molecules. Increased placental and maternal production of inflammatory molecules in late pregnancy has been strongly linked to the initiation of labour. Hormonelike substances called prostaglandins, which are produced by the placenta in response to various biochemical signals, can induce inflammation and are present in increased levels during labour. Several factors that increase the production of prostaglandins include oxytocin, which stimulates the force and frequency of uterine contractions, and a fetal lung protein called surfactant protein A (SP-A). Surfactant production in the fetal lung does not begin until the last stages of gestation, when the fetus prepares for air breathing; this transition may act as an important labour switch.
Surfactant production in the fetal lung does not begin until the last stages of gestation, when the fetus prepares for air breathing; this transition may act as an important labour switch.
The stages of labour
First stage: dilatation
Early in labour, uterine contractions, or labour pains, occur at intervals of 20 to 30 minutes and last about 40 seconds. They are then accompanied by slight pain, which usually is felt in the small of the back.
As labour progresses, those contractions become more intense and progressively increase in frequency until, at the end of the first stage, when dilatation is complete, they recur about every three minutes and are quite severe. With each contraction a twofold effect is produced to facilitate the dilatation, or opening, of the cervix. Because the uterus is a muscular organ containing a fluid-filled sac called the amnion (or “bag of waters”) that more or less surrounds the child, contraction of the musculature of its walls should diminish its cavity and compress its contents. Because its contents are quite incompressible, however, they are forced in the direction of least resistance, which is in the direction of the isthmus, or upper opening of the neck of the uterus, and are driven, like a wedge, farther and farther into this opening. In addition to forcing the uterine contents in the direction of the cervix, shortening of the muscle fibres that are attached to the neck of the uterus tends to pull those tissues upward and away from the opening and thus adds to its enlargement. By this combined action each contraction of the uterus not only forces the amnion and fetus downward against the dilating neck of the uterus but also pulls the resisting walls of the latter upward over the advancing amnion, presenting part of the child.
Because its contents are quite incompressible, however, they are forced in the direction of least resistance, which is in the direction of the isthmus, or upper opening of the neck of the uterus, and are driven, like a wedge, farther and farther into this opening. In addition to forcing the uterine contents in the direction of the cervix, shortening of the muscle fibres that are attached to the neck of the uterus tends to pull those tissues upward and away from the opening and thus adds to its enlargement. By this combined action each contraction of the uterus not only forces the amnion and fetus downward against the dilating neck of the uterus but also pulls the resisting walls of the latter upward over the advancing amnion, presenting part of the child.
Britannica Quiz
About to Pop: How Many Babies?
How many babies does a fox typically have? What about a tiger? Test your knowledge of animal reproductive rates.
In spite of this seemingly efficacious mechanism, the duration of the first stage of labour is rather prolonged, especially in women who are in labour for the first time. In such women the average time required for the completion of the stage of dilatation is between 13 and 14 hours, while in women who have previously given birth to children the average is 8 to 9 hours. Not only does a previous labour tend to shorten this stage, but the tendency often increases with succeeding pregnancies, with the result that a woman who has given birth to three or four children may have a first stage of one hour or less in her next labour.
In such women the average time required for the completion of the stage of dilatation is between 13 and 14 hours, while in women who have previously given birth to children the average is 8 to 9 hours. Not only does a previous labour tend to shorten this stage, but the tendency often increases with succeeding pregnancies, with the result that a woman who has given birth to three or four children may have a first stage of one hour or less in her next labour.
The first stage of labour is notably prolonged in women who become pregnant for the first time after age 35, because the cervix dilates less readily. A similar delay is to be anticipated in cases in which the cervix is extensively scarred as a result of previous labours, amputation, deep cauterization, or any other surgical procedure on the cervix. Even a woman who has borne several children and whose cervix, accordingly, should dilate readily may have a prolonged first stage if the uterine contractions are weak and infrequent or if the child lies in an inconvenient position for delivery and, as a direct consequence, cannot be forced into the mother’s pelvis.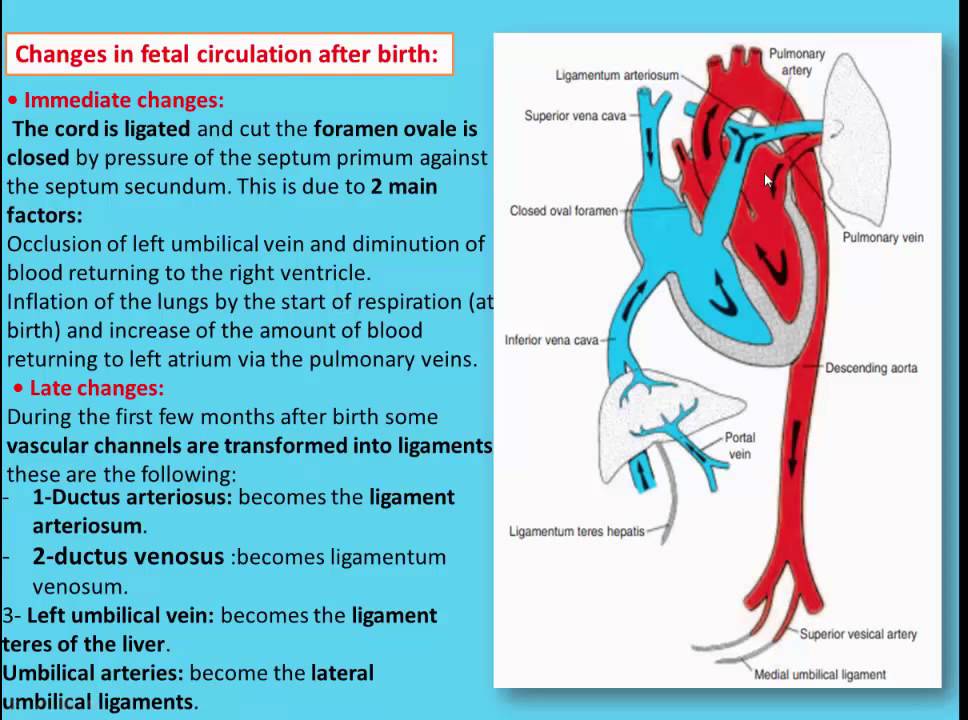
Get a Britannica Premium subscription and gain access to exclusive content. Subscribe Now
On the other hand, the early rupturing of the amnion often increases the strength and frequency of the labour pains and thereby shortens the stage of dilatation; occasionally, premature loss of the amniotic fluid leads to molding of the uterus about the child and thereby delays dilatation by preventing the child’s normal descent into the pelvis. Just as an abnormal position of the child and molding of the uterus may prevent the normal descent of the child, an abnormally large child or an abnormally small pelvis may interfere with the descent of the child and prolong the first stage of labour.
Second stage: expulsion
About the time that the cervix becomes fully dilated, the amnion breaks, and the force of the involuntary uterine contractions may be augmented by voluntary bearing-down efforts of the mother. With each labour pain, she can take a deep breath and then contract her abdominal muscles.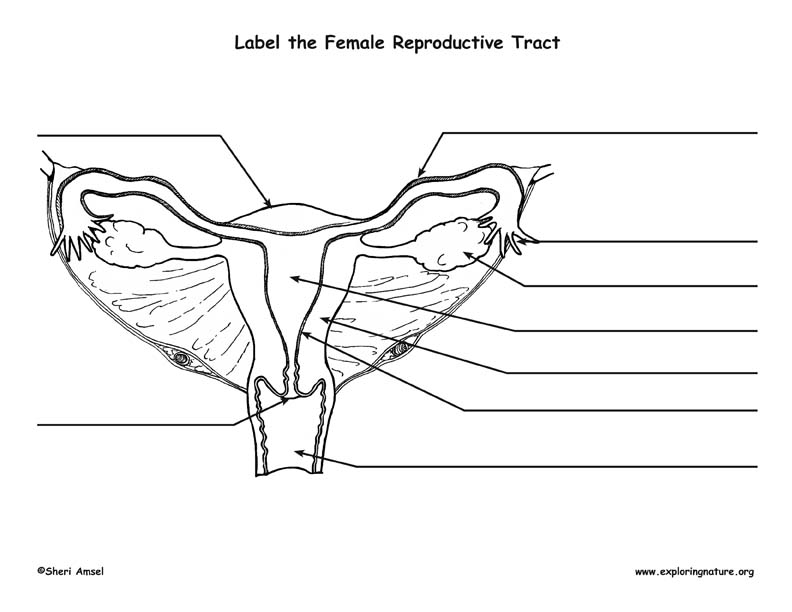 The increased intra-abdominal pressure thus produced may equal or exceed the force of the uterine contractions. These bearing-down efforts may double the effectiveness of the uterine contractions.
The increased intra-abdominal pressure thus produced may equal or exceed the force of the uterine contractions. These bearing-down efforts may double the effectiveness of the uterine contractions.
As the child descends into and passes through the birth canal, the sensation of pain is often increased. This condition is especially true in the terminal phase of the stage of expulsion, when the child’s head distends and dilates the maternal tissues as it is being born.
Your baby in the birth canal: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/002060.htm
To use the sharing features on this page, please enable JavaScript.
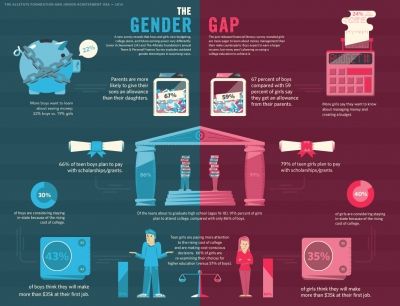
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
FETAL LIE
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between his head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
Engagement
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
Descent
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
Flexion
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
Extension
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
Expulsion
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal
- Childbirth
- Emergency Childbirth
- Emergency Childbirth
- Delivery presentations
- C-section - series
- Breech - series
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Important to know - Health of a Petersburger
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm. This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because for a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
In the process of one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.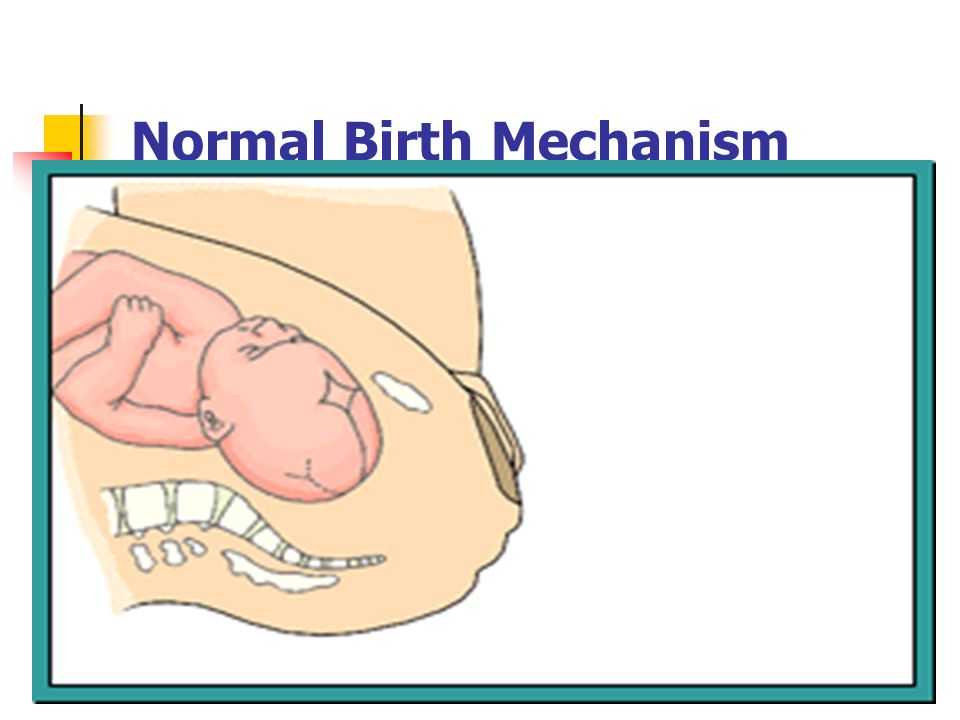
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, the uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).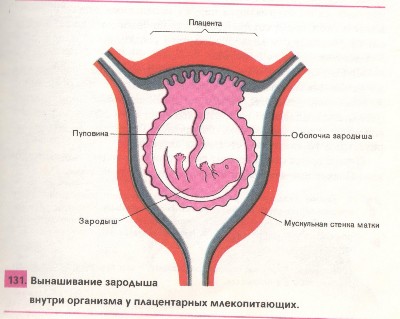
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).
Three periods of physiological labor - the natural end of a nine-month wait. Most likely, during the birth process itself, the woman in labor will not care what the period or phase of childbirth is now, but it is still desirable to know about them, at least for greater certainty before going to the hospital.
Sanitation of the birth canal in pregnant women before childbirth and its effect on the course of the postpartum period | Tyutyunnik V.L., Kan N.E., Lomova N.A., Veresova A.A.
The article is devoted to sanitation of the birth canal in pregnant women before childbirth and its influence on the course of the postpartum period
Introduction
The issues of prevention and treatment of mixed genital infections are of particular importance due to their high frequency, diagnostic difficulties and the absence of pathognomonic clinical manifestations. However, the species composition and spectrum of pathogens are extremely wide. In 60–70% of cases, the etiological factor of inflammatory diseases of the female genital organs are associations of pathogens: Trichomonas vaginalis, Chlamidia spp., Ureaplasma spp., Staphylococcus spp., Streptococcus spp., Bacillus spp. , Shigella spp., Corynebacterium spp., Diphteroides spp., Micrococcus flavus, Gardnerella vaginalis, Mobiluncus, Peptostreptococcus, Prevotella, Bacteroides, Fusobacterium, Candida albicans [1–3].
However, the species composition and spectrum of pathogens are extremely wide. In 60–70% of cases, the etiological factor of inflammatory diseases of the female genital organs are associations of pathogens: Trichomonas vaginalis, Chlamidia spp., Ureaplasma spp., Staphylococcus spp., Streptococcus spp., Bacillus spp. , Shigella spp., Corynebacterium spp., Diphteroides spp., Micrococcus flavus, Gardnerella vaginalis, Mobiluncus, Peptostreptococcus, Prevotella, Bacteroides, Fusobacterium, Candida albicans [1–3].
Modern laboratory identification of pathogens is not always effective enough to select the optimal etiotropic therapy due to the technologies used, the characteristics of the microorganisms themselves.
The microflora of the vagina is variable under the influence of exogenous and endogenous factors. Microcenosis is affected by physiological and hormonal changes (puberty, menopause, pregnancy), phases of the menstrual cycle, menstrual dysfunction. Of great importance are the degree of sexual activity, the use of antibacterial drugs, hormone therapy, and surgical interventions [2, 4, 5].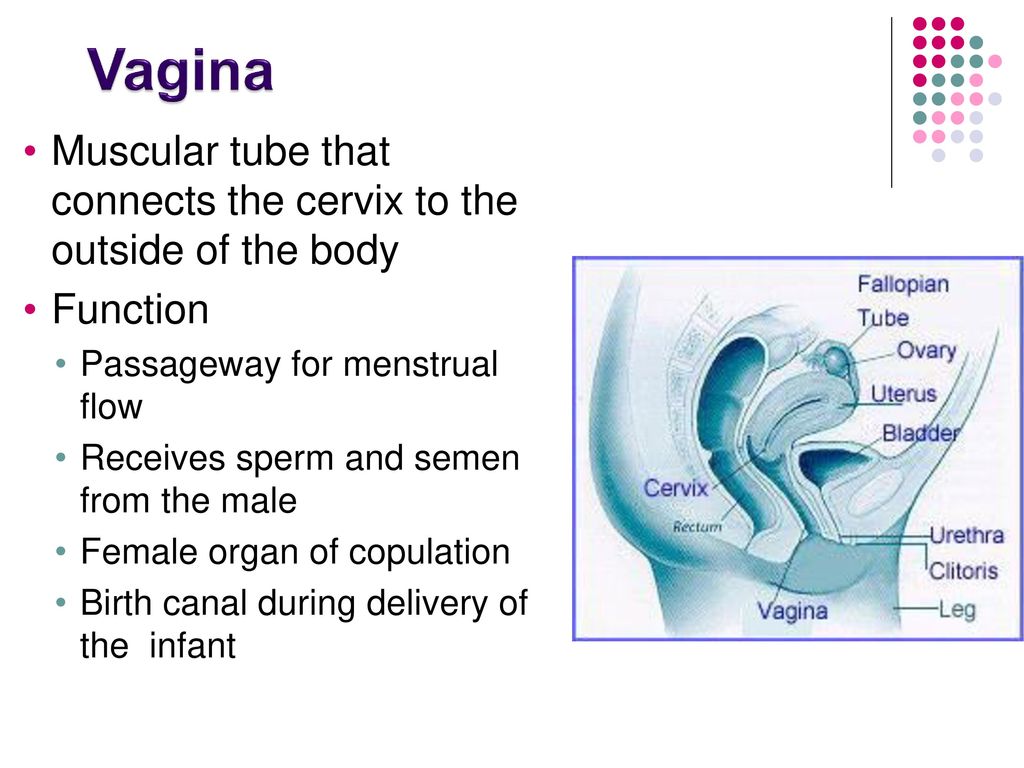
Any variant of violation of the microcenosis of the vagina must be considered as a dysbiosis of the vaginal microflora. In this case, lactobacilli are eliminated with colonization of the vagina by strict anaerobes (Prevotella/Porphyromonas spp., Peptostreptococcus spp., Fusobacteium spp., Mobiluncus spp.), gardnerella and fungi of the genus Candida. Sometimes, with the absolute predominance of conditionally pathogenic microorganisms, lactobacilli are also present in a low titer, more often lactobacilli of anaerobic origin that do not produce hydrogen peroxide [6].
With mixed infections, there is the greatest risk of developing complications associated with them. These include severe inflammatory diseases of the uterine appendages with the development of a pronounced adhesive process and tubal-peritoneal infertility, postpartum and postoperative complications [6, 7].
Vulvovaginal infections are a big problem. Their frequency reaches 60–85% in patients of gynecological hospitals [1, 7, 8].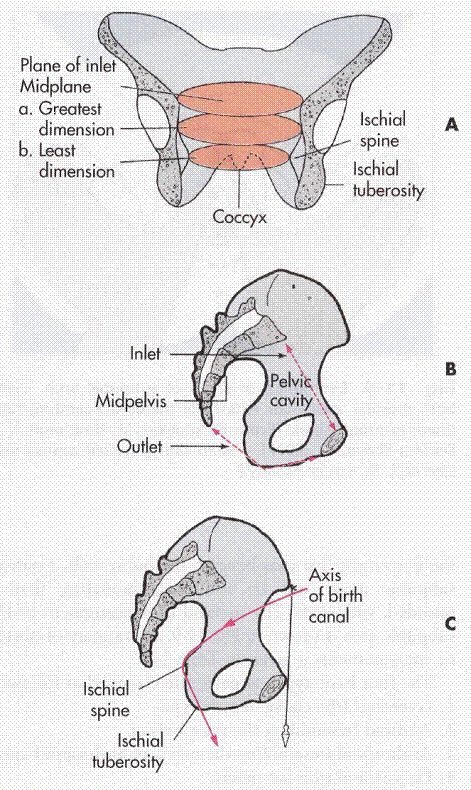
Currently, numerous clinical, microbiological and pathogenetic studies on vulvovaginitis are being carried out, new drugs and methods of treatment are being offered, but the prevalence of this pathology in women of reproductive age remains high. Moreover, such forms as bacterial vaginosis (BV), vulvovaginal candidiasis, trichomonas vaginitis account for 90% of all cases [8, 9].
The presence of genital infections during pregnancy poses a risk to the mother and fetus. The likelihood of premature termination of pregnancy, the risk of antenatal and intranatal infection, and the development of pyoinflammatory complications in the postpartum period increase [3, 5, 10]. Timely diagnosis and rational etiotropic therapy during pregnancy are urgent tasks.
Of particular interest is the choice of a drug that can have a sanitizing effect on the lower sections of the birth canal immediately before childbirth, without adversely affecting the fetus. Of great importance is the presence in the doctor's arsenal of a drug with a sufficiently wide spectrum of action, capable of suppressing all types of pathogenic microorganisms.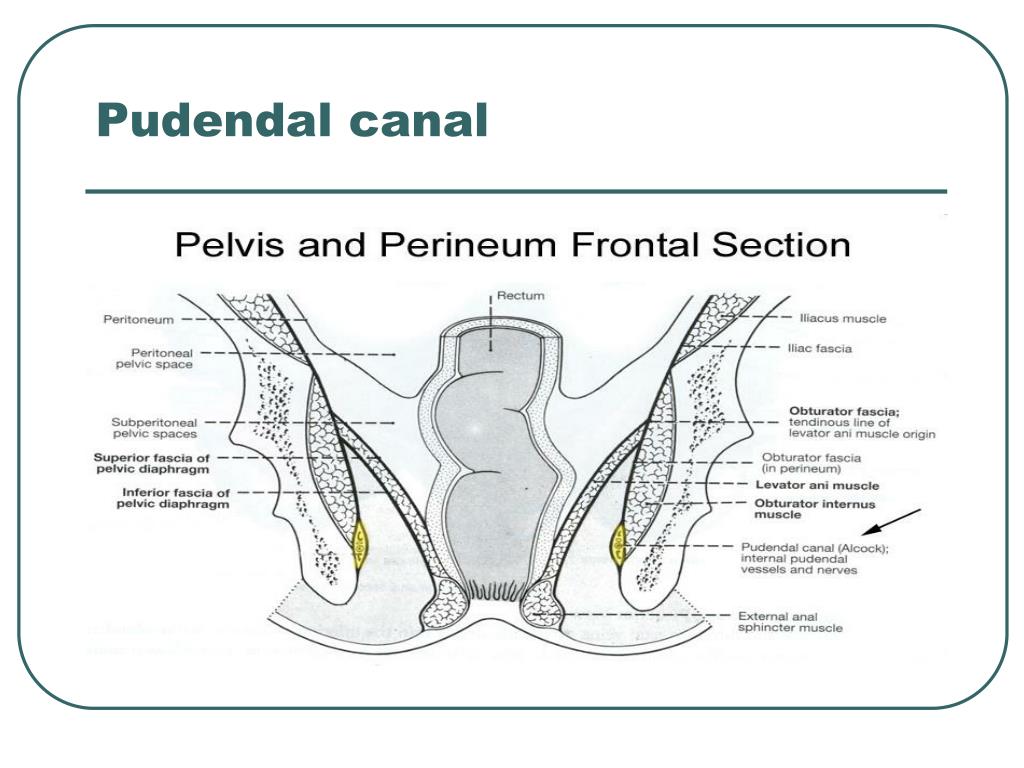 The drug Betadine (international non-proprietary name - povidone-iodine) is a broad-spectrum antiseptic and disinfectant that kills bacteria, viruses, fungi, protozoa, with the exception of tubercle bacillus.
The drug Betadine (international non-proprietary name - povidone-iodine) is a broad-spectrum antiseptic and disinfectant that kills bacteria, viruses, fungi, protozoa, with the exception of tubercle bacillus.
Betadine is a complex water-soluble compound of iodine and polyvinylpyrrolidone (a non-toxic inert synthetic polymer that acts as a carrier, has a large molecular weight and therefore does not penetrate biological barriers well). The antiseptic and disinfectant properties of betadine are due to the presence of iodine in the preparation. In combination with polyvinylpyrrolidone, iodine loses its ability to cause tissue burning, but retains high bactericidal activity, which allows expanding the scope of iodine in obstetric and gynecological practice [11].
Iodine belongs to the group of halogen antiseptics, its spectrum of action extends to gram-positive and gram-negative bacteria, fungi, viruses and protozoa. The bactericidal effect of iodine is explained by its strong oxidizing properties, it actively interacts with the amino acids of proteins, as a result of which the quaternary structure of the protein changes, its catalytic and enzymatic activity is lost.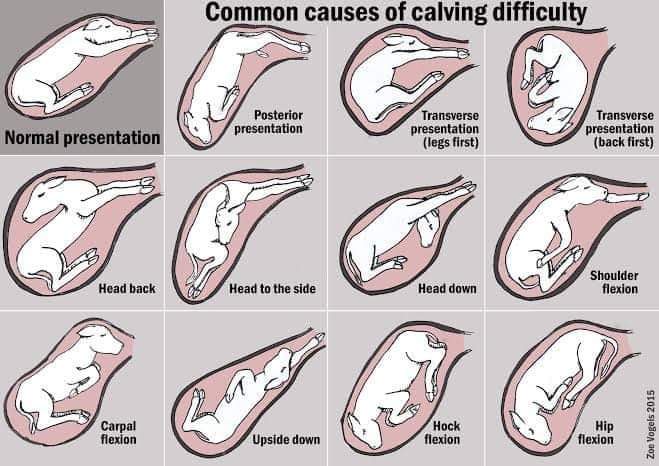 Basically, iodine disrupts the structures of bacterial transmembrane proteins and enzymes that do not have membrane protection [12].
Basically, iodine disrupts the structures of bacterial transmembrane proteins and enzymes that do not have membrane protection [12].
After insertion into the vagina, the Betadine suppository quickly dissolves and envelops the vaginal mucosa, forming a thin layer on its surface. Upon contact of the drug with the mucous membrane, iodine, slowly released from the complex with polyvinylpyrrolidone, has a long-term antiseptic and disinfectant effect. Betadine molecules are quite large, they are hardly absorbed into the blood, so the drug acts mainly locally, without any toxic effects [12, 13].
In addition, Betadine is more effective than other antiseptics in suppressing the reproduction of microorganisms, even in high dilution (up to 1/256).
Betadine suppositories are indicated for the treatment of acute and chronic vaginitis, BV, candidiasis, Trichomonas vaginalis infection, vaginal infections after antibiotic or steroid therapy, and for the prevention of infectious complications before surgical or diagnostic interventions in the vagina.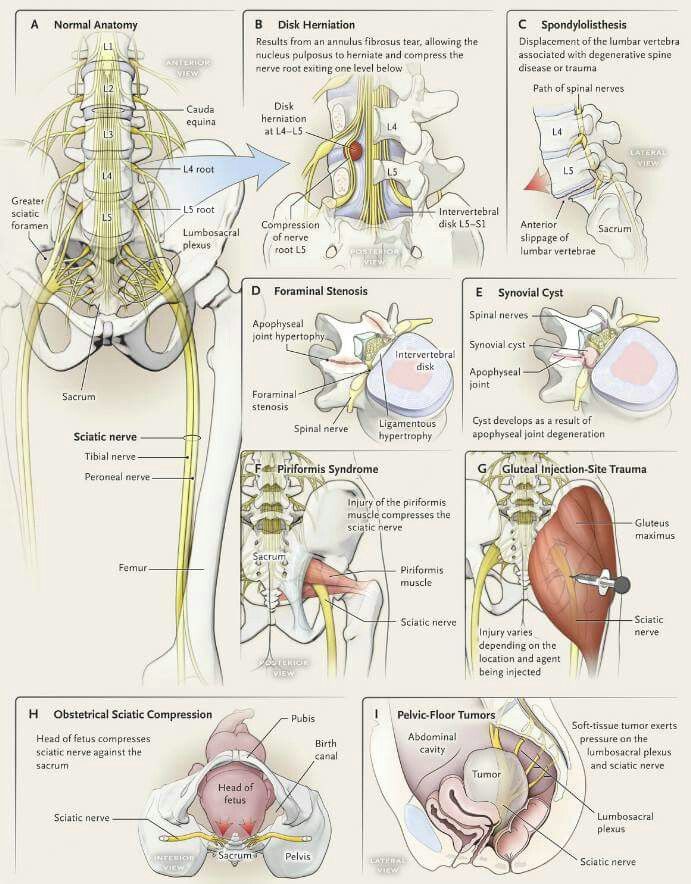
Candles Betadine can not be used in case of hypersensitivity to iodine and other components of the drug, dysfunction or adenoma of the thyroid gland, Dühring's herpetiform dermatitis, simultaneously with the use of radioactive iodine and in children during the neonatal period.
In addition, Betadine is also available in the form of a 10% solution for local and external use of 30, 120 and 1000 ml. 1 ml of the solution contains 0.1 g of povidone-iodine and excipients (glycerin, nonoxynol-9, anhydrous citric acid, disodium hydrogen phosphate, sodium hydroxide 10% solution (m / o) to establish pH, purified water).
Betadine solution can be used to disinfect the birth canal (without dilution), as well as to treat the palpebral fissure and umbilical wound in newborns. Used for the prevention of conjunctivitis in newborns, Betadine solution is effective both at a concentration of 2.5% [14] and at a concentration of 1.25% [15]. Treatment of the skin of newborns with a 0.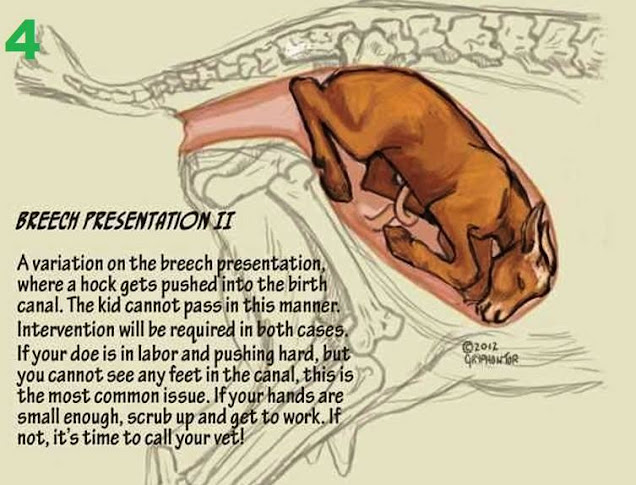 1% solution of Betadine completely eliminates the possibility of developing a nosocomial infection (including that associated with MRSA) [16]. The Betadine solution has a good clinical effect, not inferior to the action of a number of antibacterial drugs, and can be considered a necessary and reliable tool for the prevention and treatment of purulent-septic complications in gynecological practice [17].
1% solution of Betadine completely eliminates the possibility of developing a nosocomial infection (including that associated with MRSA) [16]. The Betadine solution has a good clinical effect, not inferior to the action of a number of antibacterial drugs, and can be considered a necessary and reliable tool for the prevention and treatment of purulent-septic complications in gynecological practice [17].
We have conducted a study aimed at evaluating the clinical efficacy of Betadine in the treatment of bacterial vaginosis, mixed urogenital infection and the prevention of purulent-inflammatory complications of childbirth.
Material and methods
We examined 42 pregnant women at a gestational age of 34-36 weeks, aged 18 to 42 years, with clinical signs of BV. The diagnosis was established by microscopy of vaginal smears, bacteriological examination of cervical mucus, determination of the number of lactobacilli, examination for sexually transmitted infections, polymerase chain reaction (PCR) methods.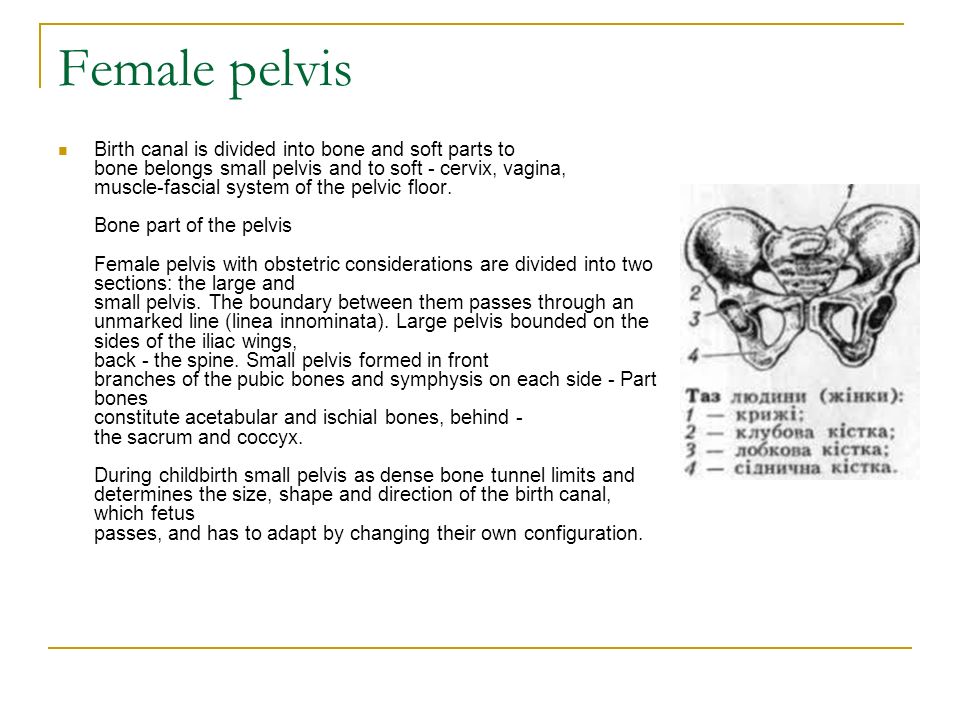
The main symptom in BV was profuse discharge from the genital tract of white or gray color (92%), sometimes foamy (21%), often with an unpleasant odor (64%). When viewed in the mirrors, the discharge was evenly distributed along the walls of the vagina and the vaginal part of the cervix and was easily removed from the mucous membrane with a gauze swab.
Complaints of itching were much less common (38%). In 19% of women with BV, there were no complaints. The latter were diagnosed on the basis of microscopy of vaginal smears and the results of bacteriological examination of cervical mucus.
Thus, depending on the presence of complaints, BV is divided into 2 variants: asymptomatic and with clinical manifestations;
- in the first case, there is an absence of clinical manifestations along with positive results of laboratory tests;
- in the second case, there are abundant, liquid, white or grayish discharges, with an unpleasant odor. Characterized by frequent combination with pathological processes of the cervix (pseudo-erosion, leukoplakia, endocervicitis, endometriosis) and recurrent course.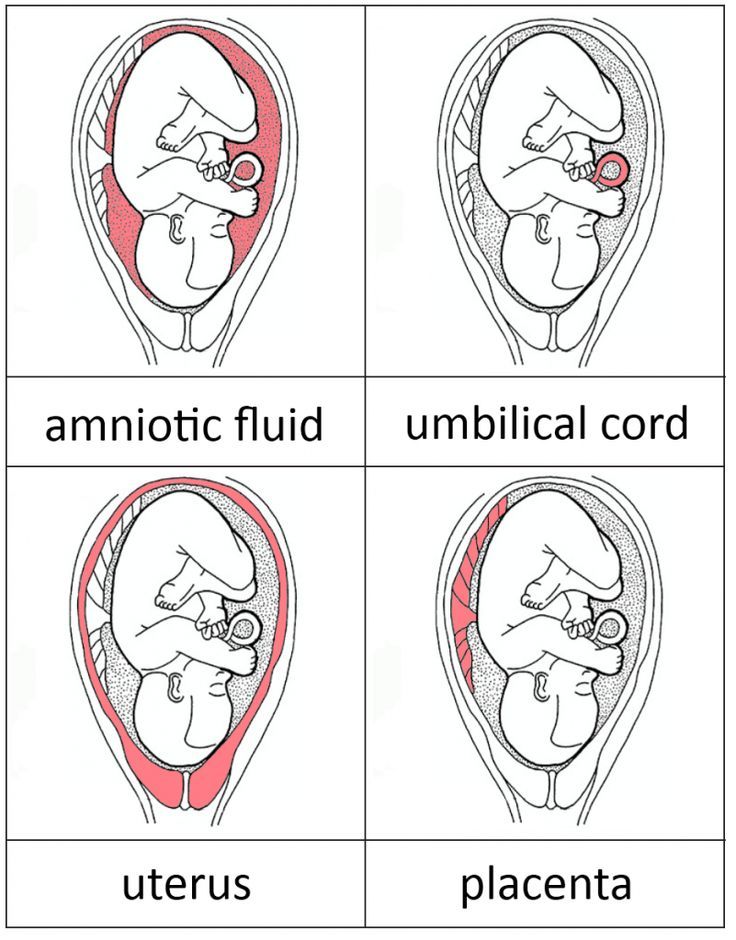
4 screening diagnostic tests (the so-called "Amsel criteria") are commonly used to diagnose BV:
1. Pathological nature of vaginal discharge.
2. pH of the vaginal discharge >4.5. The alkaline environment of the vaginal contents is the result of the elimination of lactobacilli (or a sharp decrease in their content). If cervical mucus, blood or semen enters the vaginal discharge, a false positive result may be observed. To perform pH measurements, you can use universal indicator paper with a reference scale or various modifications of pH meters.
3. Positive amine test. The vaginal contents often have a rotten fish odor due to the production of diamines during the decarboxylation of amino acids by anaerobes. Salts of these substances in an alkaline environment are converted into volatile amines.
4. Identification of "key cells" by microscopic examination of wet, unstained preparations of vaginal discharge. “Key cells” are mature epithelial cells with microorganisms adhered to them (gardnerella, mobiluncus, gram-positive cocci).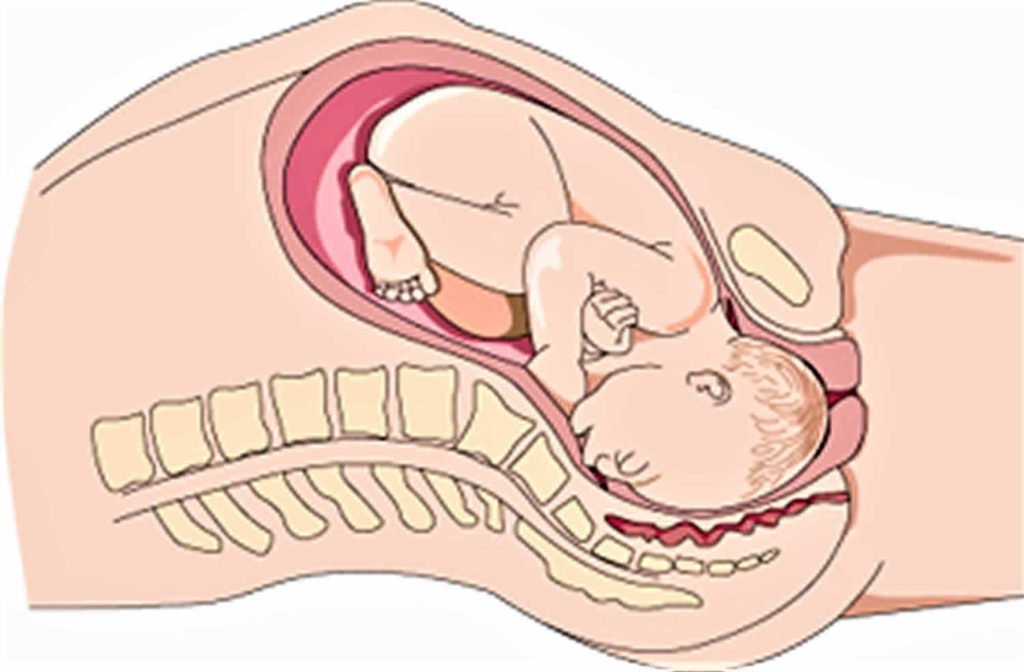 False positive results can be obtained by identifying epithelial cells with lactobacilli adhering to them; in this case, microscopy of Gram-stained vaginal smears should be performed.
False positive results can be obtained by identifying epithelial cells with lactobacilli adhering to them; in this case, microscopy of Gram-stained vaginal smears should be performed.
Diagnostically significant is the presence of at least 3 positive signs out of 4.
The culture method has a high sensitivity and specificity in the diagnosis of BV. Its high information content is due to qualitative and quantitative indicators of the composition of the microbiocenosis of the vagina. Accordingly, with BV, a decrease in the number of lactobacilli and an increase in the content of opportunistic flora are observed. Disadvantages of the method: relative high cost and duration of execution.
The method of molecular diagnostics by real-time quantitative PCR allows to estimate the total bacterial mass, the number of lactobacilli and bacteria that are BV markers in the vaginal discharge, and is widely used by modern diagnostic laboratories. However, the expediency of detecting a large number of microorganisms associated with BV by this method has not been proven.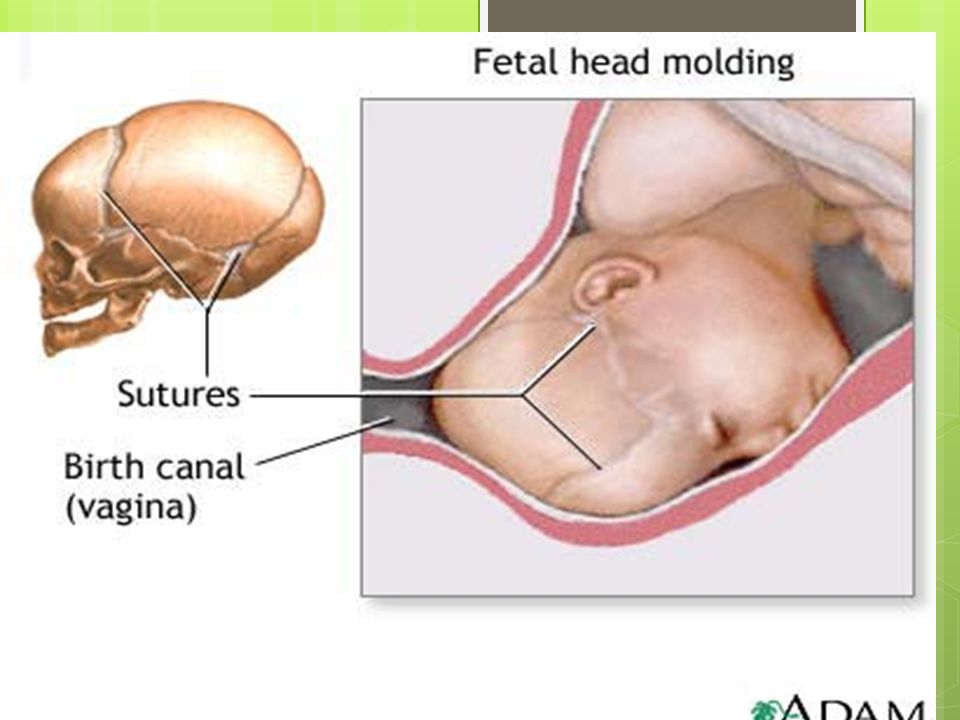
BV treatment was carried out in 2 stages:
1. Selective decontamination (selective elimination of pathogens), for which antimicrobial drugs were prescribed to reduce the number of anaerobic microorganisms.
2. Restoration of normal or as close to normal microbiocenosis of the vagina with the help of eubiotics. Microbiocenosis - microorganisms and their metabolic products, which are normally located on the mucous membranes of the vagina.
Treatment of BV in the present observation was carried out to all patients by prescribing Betadine 1 suppository per day in the vagina for 14 days. The effectiveness of therapy was assessed on the basis of clinical data and laboratory results.
Results
Before treatment, microscopy of a vaginal smear, the number of leukocytes ranged from 11 to 32 per field of view. Against this background, 90,065 Candida albicans were detected in bacterial cultures in 37% of women, Staphylococcus epidermidis at a concentration of 106 CFU in 19%, Enterococcus faecalis in 17%, and Staphylococcus saprophyticus (104 CFU) in 23%. In 67% of observations, key cells (gardnerella) were detected in large numbers, conditionally pathogenic strains of ureaplasma were determined in 11%, and mycoplasmas detected by PCR methods were detected in 6% of cases.
In 67% of observations, key cells (gardnerella) were detected in large numbers, conditionally pathogenic strains of ureaplasma were determined in 11%, and mycoplasmas detected by PCR methods were detected in 6% of cases.
After the treatment, during the first and second control examinations by PCR, we did not reveal opportunistic pathogens.
After therapy, no patient complained at the second visit. Analysis of laboratory data showed that after 1 week. after therapy, Staphylococcus epidermidis was detected only in 2 patients, and at the second control visit, opportunistic flora was absent in all women, an increase in the titer of lactobacilli was noted.
After a course of treatment with Betadine, eubiotic therapy was performed, against which the vaginal biocenosis returned to normal, the titer of lactobacilli was within the normal range during a second study.
After 4 weeks after therapy, in 96% of patients, the landscape of the vaginal smear returned to normal: the number of leukocytes was 4–8 in the field of view. In bacterial crops after treatment, opportunistic flora was not detected.
In bacterial crops after treatment, opportunistic flora was not detected.
Regardless of the treatment regimen (with or without the use of eubiotics), in a control study in 69% of women, the titer of lactobacilli was within the normal range.
After 1 month after therapy, only 5% of women complained of moderate discharge from the genital tract, not accompanied by itching and unpleasant odor. In addition, in the course of therapy with Betadine, the patients in the vast majority of cases did not notice any adverse reactions associated with the use of suppositories, in the form of unpleasant sensations in the vulva and vagina (burning, itching, swelling, etc.).
Subsequently, we analyzed the outcomes of pregnancy and the postpartum period in 39 out of 42 patients included in the study.
An analysis of the course of the postpartum period showed the absence of significantly significant purulent-inflammatory complications in all patients who underwent sanitation of the birth canal with Betadine over an average of 4–6 weeks.