What is the symptoms of jaundice
Infant jaundice - Symptoms and causes
Overview
Infant jaundice is yellow discoloration of a newborn baby's skin and eyes. Infant jaundice occurs because the baby's blood contains an excess of bilirubin (bil-ih-ROO-bin), a yellow pigment of red blood cells.
Infant jaundice is a common condition, particularly in babies born before 38 weeks' gestation (preterm babies) and some breast-fed babies. Infant jaundice usually occurs because a baby's liver isn't mature enough to get rid of bilirubin in the bloodstream. In some babies, an underlying disease may cause infant jaundice.
Most infants born between 35 weeks' gestation and full term need no treatment for jaundice. Rarely, an unusually high blood level of bilirubin can place a newborn at risk of brain damage, particularly in the presence of certain risk factors for severe jaundice.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Yellowing of the skin and the whites of the eyes — the main sign of infant jaundice — usually appears between the second and fourth day after birth.
To check for infant jaundice, press gently on your baby's forehead or nose. If the skin looks yellow where you pressed, it's likely your baby has mild jaundice. If your baby doesn't have jaundice, the skin color should simply look slightly lighter than its normal color for a moment.
Examine your baby in good lighting conditions, preferably in natural daylight.
When to see a doctor
Most hospitals have a policy of examining babies for jaundice before discharge. The American Academy of Pediatrics recommends that newborns be examined for jaundice during routine medical checks and at least every eight to 12 hours while in the hospital.
Your baby should be examined for jaundice between the third and seventh day after birth, when bilirubin levels usually peak. If your baby is discharged earlier than 72 hours after birth, make a follow-up appointment to look for jaundice within two days of discharge.
The following signs or symptoms may indicate severe jaundice or complications from excess bilirubin.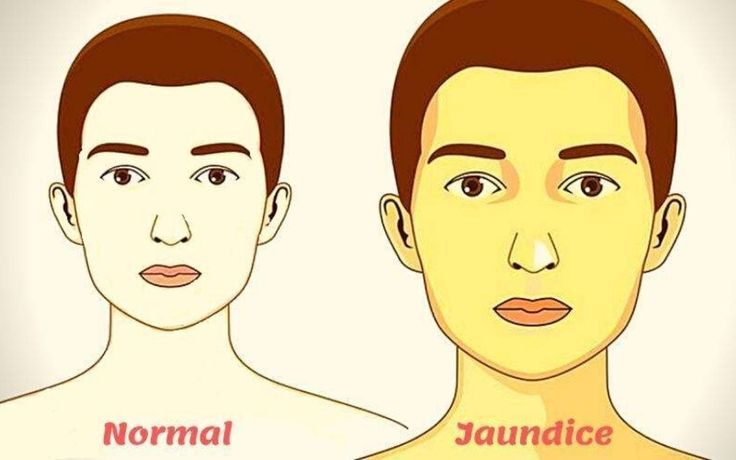 Call your doctor if:
Call your doctor if:
- Your baby's skin becomes more yellow
- The skin on your baby's the abdomen, arms or legs looks yellow
- The whites of your baby's eyes look yellow
- Your baby seems listless or sick or is difficult to awaken
- Your baby isn't gaining weight or is feeding poorly
- Your baby makes high-pitched cries
- Your baby develops any other signs or symptoms that concern you
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Excess bilirubin (hyperbilirubinemia) is the main cause of jaundice. Bilirubin, which is responsible for the yellow color of jaundice, is a normal part of the pigment released from the breakdown of "used" red blood cells.
Newborns produce more bilirubin than adults do because of greater production and faster breakdown of red blood cells in the first few days of life. Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. A newborn's immature liver often can't remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life.
Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. A newborn's immature liver often can't remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life.
Other causes
An underlying disorder may cause infant jaundice. In these cases, jaundice often appears much earlier or much later than does the more common form of infant jaundice. Diseases or conditions that can cause jaundice include:
- Internal bleeding (hemorrhage)
- An infection in your baby's blood (sepsis)
- Other viral or bacterial infections
- An incompatibility between the mother's blood and the baby's blood
- A liver malfunction
- Biliary atresia, a condition in which the baby's bile ducts are blocked or scarred
- An enzyme deficiency
- An abnormality of your baby's red blood cells that causes them to break down rapidly
Risk factors
Major risk factors for jaundice, particularly severe jaundice that can cause complications, include:
- Premature birth.
 A baby born before 38 weeks of gestation may not be able to process bilirubin as quickly as full-term babies do. Premature babies also may feed less and have fewer bowel movements, resulting in less bilirubin eliminated through stool.
A baby born before 38 weeks of gestation may not be able to process bilirubin as quickly as full-term babies do. Premature babies also may feed less and have fewer bowel movements, resulting in less bilirubin eliminated through stool. - Significant bruising during birth. Newborns who become bruised during delivery gets bruises from the delivery may have higher levels of bilirubin from the breakdown of more red blood cells.
- Blood type. If the mother's blood type is different from her baby's, the baby may have received antibodies through the placenta that cause abnormally rapid breakdown of red blood cells.
- Breast-feeding. Breast-fed babies, particularly those who have difficulty nursing or getting enough nutrition from breast-feeding, are at higher risk of jaundice. Dehydration or a low caloric intake may contribute to the onset of jaundice. However, because of the benefits of breast-feeding, experts still recommend it.
 It's important to make sure your baby gets enough to eat and is adequately hydrated.
It's important to make sure your baby gets enough to eat and is adequately hydrated. - Race. Studies show that babies of East Asian ancestry have an increased risk of developing jaundice.
Complications
High levels of bilirubin that cause severe jaundice can result in serious complications if not treated.
Acute bilirubin encephalopathy
Bilirubin is toxic to cells of the brain. If a baby has severe jaundice, there's a risk of bilirubin passing into the brain, a condition called acute bilirubin encephalopathy. Prompt treatment may prevent significant lasting damage.
Signs of acute bilirubin encephalopathy in a baby with jaundice include:
- Listlessness
- Difficulty waking
- High-pitched crying
- Poor sucking or feeding
- Backward arching of the neck and body
- Fever
Kernicterus
Kernicterus is the syndrome that occurs if acute bilirubin encephalopathy causes permanent damage to the brain.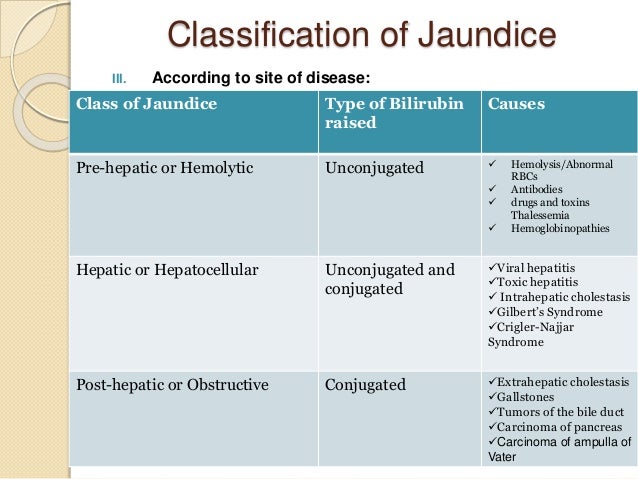 Kernicterus may result in:
Kernicterus may result in:
- Involuntary and uncontrolled movements (athetoid cerebral palsy)
- Permanent upward gaze
- Hearing loss
- Improper development of tooth enamel
Prevention
The best preventive of infant jaundice is adequate feeding. Breast-fed infants should have eight to 12 feedings a day for the first several days of life. Formula-fed infants usually should have 1 to 2 ounces (about 30 to 60 milliliters) of formula every two to three hours for the first week.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Jaundice: Causes, symptoms, and treatments
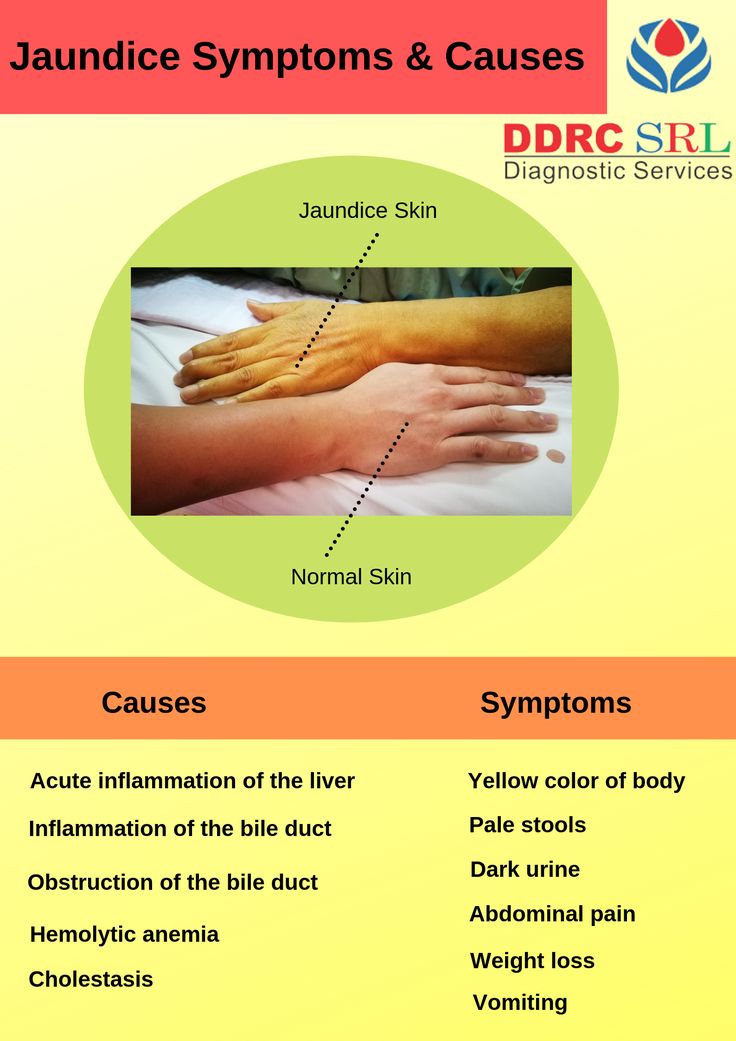
Jaundice is a condition in which a yellowish tinge appears on the skin, mucous membranes, and the whites of the eye. Body fluids may also change color.
Jaundice frequently indicates a problem with the liver or bile ducts. When the liver is not working properly, it can cause a waste material called bilirubin to build up in the blood.
With moderate bilirubin levels, a person’s skin, eyes, and mucous membranes can turn yellow. As it progresses, the color can also change from yellow to green. The green color occurs due to biliverdin, the green pigment present in bile.
Jaundice can develop in people of all ages and is normally the result of an underlying condition. Newborns and older adults have the highest likelihood of developing jaundice.
This article discusses what causes jaundice, how healthcare professionals diagnose and treat the condition, and how a person can help to prevent it from occurring. It also explores the symptoms a person can expect.
According to the American Family Physician (AAFP), jaundice is the yellowing of the skin, mucous membranes, and the whites of the eyes that occurs when the body does not process bilirubin as it should.
Bilirubin levels increase as the red blood cells naturally break down. Typically, the liver filters this waste material out of the bloodstream and turns it into a new form called conjugated bilirubin. The new form then exits the body in a person’s stool.
The new form then exits the body in a person’s stool.
If there is too much bilirubin for the liver to process, it can build up in the body. This is known as hyperbilirubinemia, and it causes the yellow color in the skin and eyes.
Jaundice typically occurs due to an underlying disorder that either causes the production of too much bilirubin or prevents the liver from eliminating it.
Some possible underlying conditions and causes of jaundice include:
- side effects of certain medications
- gallstone disease
- excessive alcohol consumption
- gallbladder or pancreatic cancer
- cirrhosis, which is a disease that causes scar tissue to replace healthy tissue in the liver
- hepatitis or other liver infections
- hemolytic anemia
Treatment will depend on the underlying cause of jaundice.
Jaundice can lead to itching, or pruritis. A 2021 article notes that a person can have warm baths containing oatmeal and take antihistamines for mild pruritis.
A healthcare professional may prescribe medications for those experiencing moderate to severe pruritis, such as cholestyramine or colestipol.
As jaundice may sometimes indicate damage to the liver, a liver transplant may be necessary in some cases, depending on the severity of the injury.
Jaundice is related to liver function.
People can help take care of their liver with several lifestyle changes, such as:
- eating a balanced diet
- exercising regularly
- limiting alcohol consumption
- avoiding toxins from chemicals and other sources, both inhaled and touched
- managing medications carefully
A 2021 article also suggests:
- avoiding herbal medications without consulting a healthcare professional first
- avoiding smoking, alcohol, and intravenous drugs
- avoiding taking more than the recommended dose of prescribed medications
- getting the recommended vaccinations before traveling
- practicing safe sex, such as using barrier methods of contraception
Common symptoms of jaundice include:
- a yellow tinge to the skin, mucous membranes, and the whites of the eyes
- pale stools
- dark urine
- itchiness
In infants, the yellowish tinge can start at the head and spread down the body to the toes.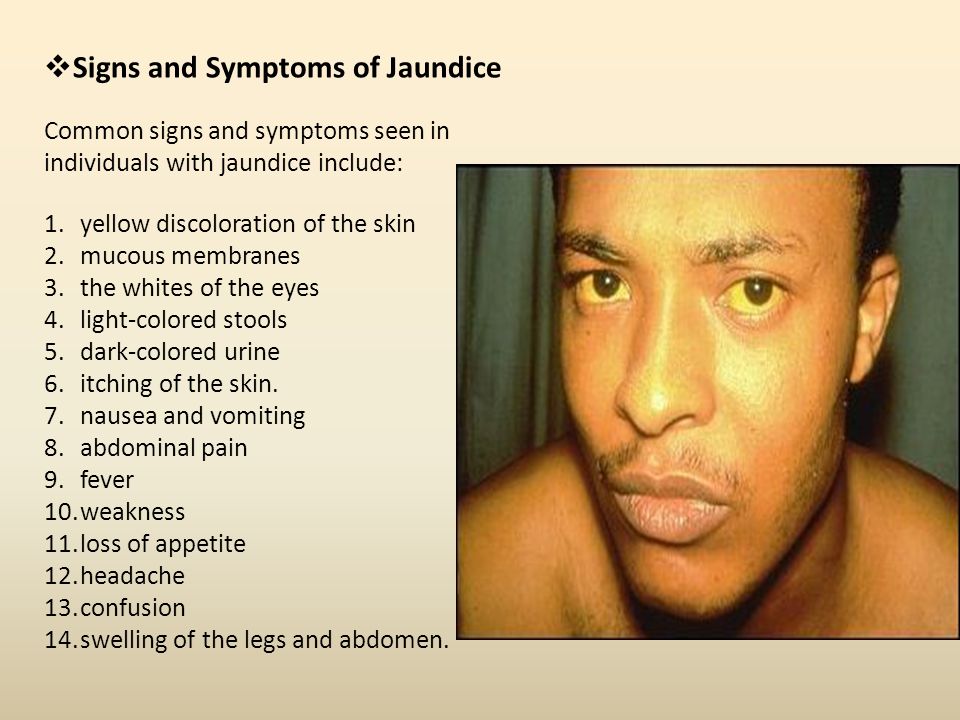
The United Kingdom’s National Health Service (NHS) notes that jaundice may be less apparent on Black and Brown skin. It is more obvious in the whites of the eyes.
Accompanying symptoms of jaundice may include:
- fatigue
- abdominal pain
- weight loss
- vomiting
- fever
High levels of bilirubin can be toxic and lead to a rare type of brain damage called kernicterus in infants.
The underlying conditions causing jaundice can also lead to their own complications.
Three main types of jaundice include:
- Prehepatic: This occurs before the liver processes the waste and results in higher unconjugated bilirubin levels.
- Hepatic: This occurs in the liver and results in both higher conjugated and unconjugated bilirubin levels.
- Posthepatic: This occurs after the liver has processed the waste and results in higher conjugated bilirubin levels.
Jaundice is a common health issue in newborn children.
The Centers for Disease Control and Prevention (CDC) note that approximately 60% of newborns develop jaundice, and signs appear within 48 hours of birth. A doctor or nurse should examine the baby when they are between 3–5 days old. This is because the bilirubin levels are usually at their highest during this time.
Red blood cells in the body of an infant are frequently broken down and replaced. This causes the production of more bilirubin. In addition, the livers of infants are less developed and are therefore less effective at filtering bilirubin from the body.
Symptoms will usually resolve without treatment in mild cases. However, infants with extremely high bilirubin levels will require treatment with either a blood transfusion or phototherapy.
In these cases, jaundice treatment in newborns is vital to help prevent kernicterus.
Causes of jaundice in newborns
Although jaundice in babies is common and often resolves without treatment, some underlying medical conditions can cause jaundice.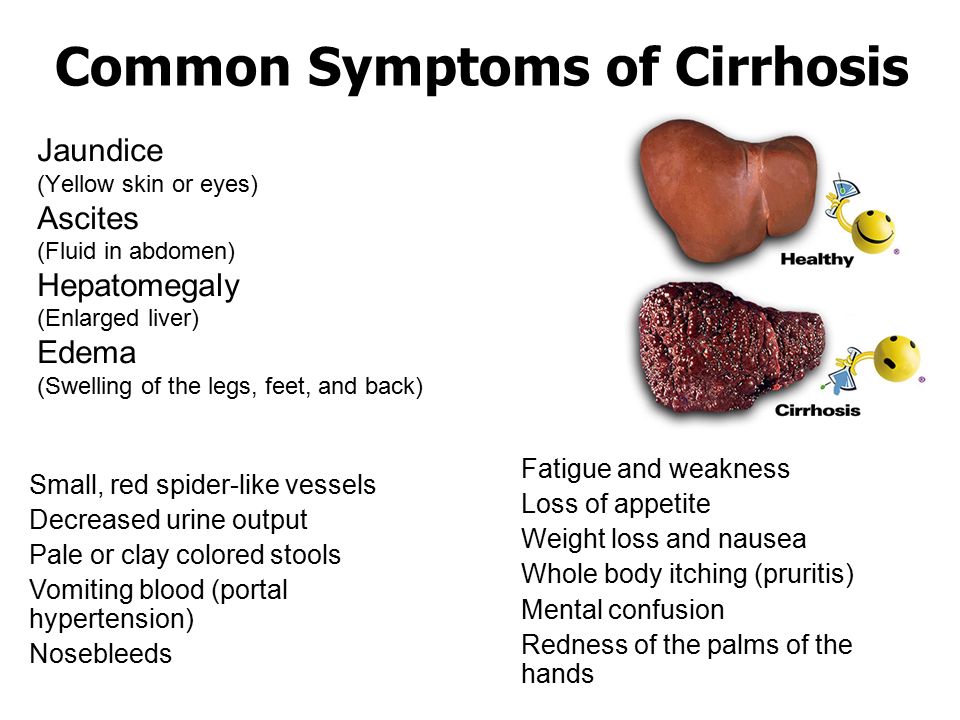 These include:
These include:
- underactive thyroid gland
- blood group incompatibility, when the blood of both the pregnant person and infant become mixed in the womb or during birth
- rhesus disease, a condition in which the pregnant person’s antibodies destroy the infant’s blood cells
- urinary tract infection
- a blockage in the bile ducts and gallbladder
- Crigler-Najjar syndrome, a condition that affects the enzymes that process bilirubin
Breastfeeding or chestfeeding can also increase the chance of jaundice in newborns. However, there is no need for a person to stop feeding the baby this way. In these cases, the symptoms of jaundice resolve in a few weeks.
According to a 2021 article, normal bilirubin levels are less than 1 milligram per deciliter (mg/dl).
A person has jaundice if these levels reach approximately 3 mg/dl.
A 2021 article notes that doctors may diagnose jaundice in infants if the bilirubin levels increase to 5 mg/dl per day or more than 0. 2 mg/dl per hour.
2 mg/dl per hour.
These ranges may differ between laboratories. How far above the normal range a person’s levels will help a doctor determine the best course of treatment.
Doctors will most likely start with the person’s history and a physical exam to diagnose jaundice. They may later also order lab tests.
During an examination, they will pay close attention to the abdomen, liver, and skin.
The doctor may often include lab tests to help determine the underlying cause of jaundice. These include:
- Bilirubin tests: A high level of unconjugated bilirubin compared to levels of conjugated bilirubin suggest hemolytic jaundice.
- Full blood count (FBC) or complete blood count (CBC): This measures levels of red blood cells, white blood cells, and platelets.
- Hepatitis A, B, and C tests: This tests for a range of liver infections.
The doctor will also examine the structure of the liver if they suspect an obstruction. In these cases, they will use imaging tests, including MRI, CT, and ultrasound scans.
In these cases, they will use imaging tests, including MRI, CT, and ultrasound scans.
In addition, they may carry out an endoscopic retrograde cholangiopancreatography (ERCP). This is a procedure combining endoscopy and X-ray imaging.
The AAFP states that a healthcare professional may perform a liver biopsy. A liver biopsy can check for inflammation, cirrhosis, cancer, and fatty liver. This test involves inserting a needle into the liver to obtain a tissue sample. A healthcare professional will then examine the sample under the microscope.
Jaundice is the yellowing of the skin, mucous membranes, and whites of the eyes. It is a symptom of an underlying condition or health concern that involves the liver.
It occurs when the liver cannot keep up with the demand to process waste in the blood or when the liver becomes damaged. Several conditions can cause liver issues and result in jaundice.
Treatment for jaundice typically involves treating the underlying condition.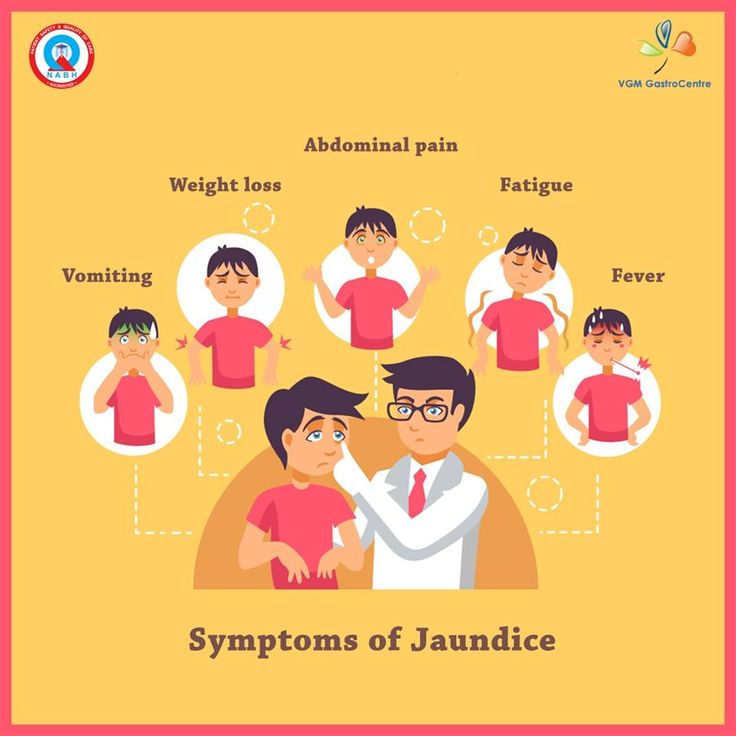
Read the article in Spanish.
Jaundice in adults - causes, examination and treatment | Symptoms
Alcoholic liver disease
Signs: Slowly developing jaundice. History of heavy alcohol consumption. The appearance in men of female characteristics (loss of muscle tissue, smoothness of the skin, enlargement of the mammary glands, reduction of the testicles and growth of female pubic hair). Sometimes dropsy of the abdomen due to accumulation of fluid (ascites).
Blockade of the bile duct by gallstone, tumor of the pancreas or bile ducts
Signs: Dark urine and light in color, soft, voluminous, oily and unusually foul-smelling stools. Usually there is pain in the upper right side or in the center of the abdominal cavity. If the cause is a tumor, weight loss and sometimes chronic abdominal pain.
Cholestasis during pregnancy
Signs: Severe itching. Later appearance of jaundice and dark urine. Usually develops in late pregnancy.
Usually develops in late pregnancy.
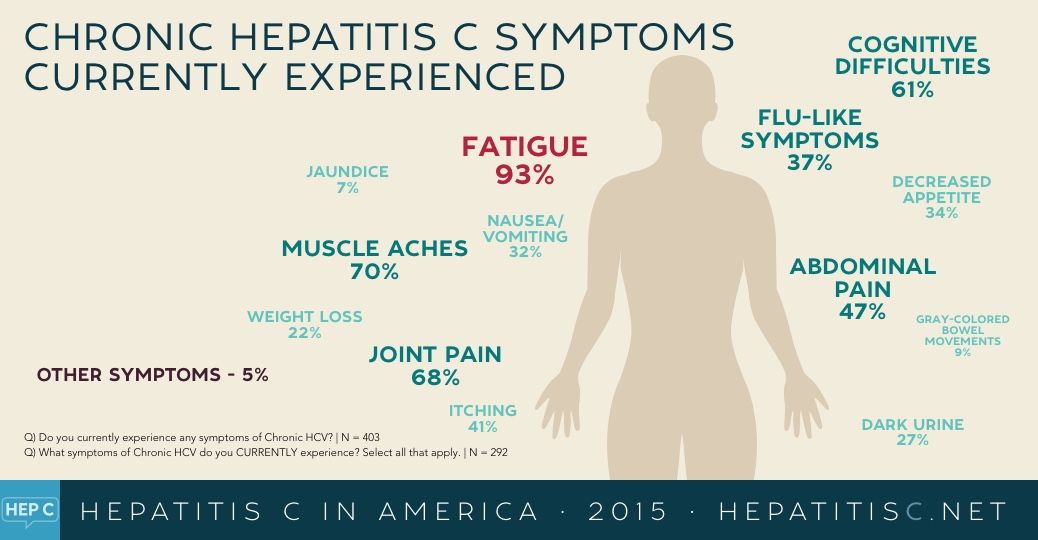
Hepatitis (viral)
Signs: Symptoms that are observed before the development of jaundice (nausea, vomiting, loss of appetite, fatigue, constant pain in the upper right side of the abdomen, fever, sometimes joint pain).
Primary biliary cholangitis (an autoimmune disease that causes damage to the small bile ducts inside the liver)
Signs: Symptoms that often occur before jaundice develops (fatigue, itching, dry mouth and dry eyes). Sometimes discomfort in the upper right side of the abdomen, blackening of the skin, and small yellow deposits of fat in the skin (xanthomas) or eyelids (xanthelasma).
Primary sclerosing cholangitis (scarring and destruction of small and large bile ducts)
Signs: Symptoms that occur before the development of jaundice (worse symptoms of fatigue, itching, pain in the upper right side of the abdomen). Sometimes light-colored, soft, voluminous, oily, and unusually foul-smelling stools. Often in people with inflammatory bowel disease.
Often in people with inflammatory bowel disease.
RBC destruction (hemolysis)
Signs: Symptoms of anemia (pallor, weakness and fatigue). Sometimes use of drugs that cause hemolysis, or a family member with a red blood cell disorder.
Wilson's disease (causes accumulation of copper in the liver)
Signs: Trembling, difficulty speaking and swallowing, involuntary movements, loss of coordination, and personality changes. Golden or greenish-golden ring on the border of the cornea of the eyes (Kaiser-Fleischer rings).
Surgical complications (scarring of the bile ducts due to surgery, reduced blood flow to the liver due to blood loss or other complications of major surgery)
Signs: Develops soon after surgery, especially after major surgery.
Medicines
Signs: Use of a substance that can cause jaundice.
types, causes, symptoms, diagnosis, treatment in children and adults
Jaundice is a syndrome in which the skin, mucous membranes and whites of the eyes turn yellow.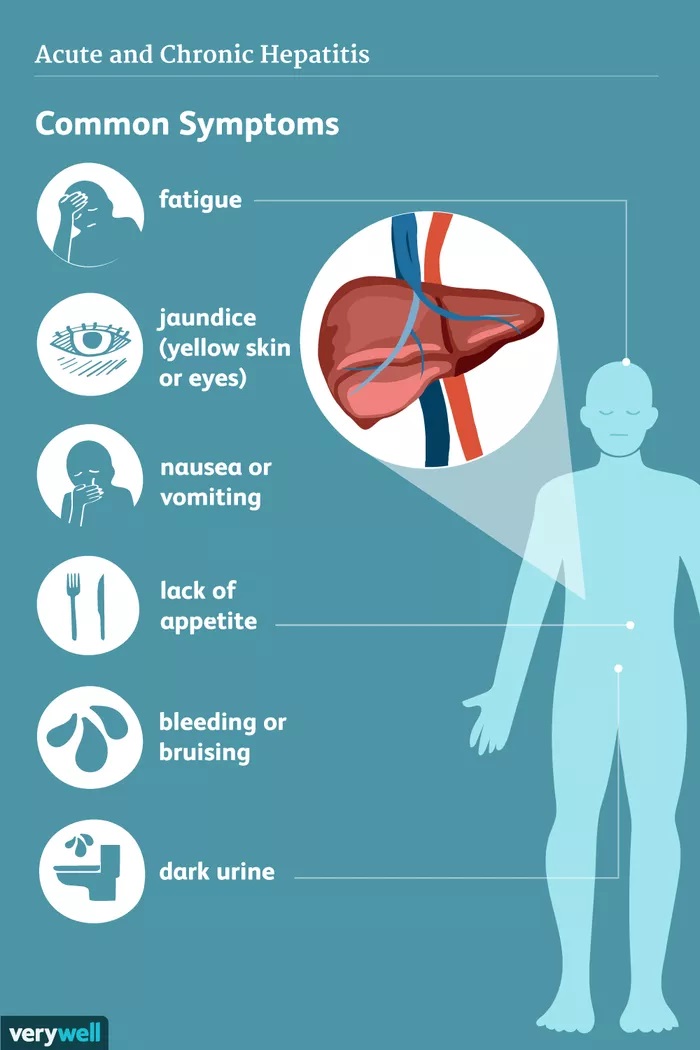 This is not an independent disease, but only a manifestation of some kind of pathology. The reasons for the development of jaundice can be completely different.
This is not an independent disease, but only a manifestation of some kind of pathology. The reasons for the development of jaundice can be completely different.
What causes jaundice?
Jaundice occurs when there is too much bilirubin in the blood. It can be increased due to many factors: disorders in the liver, disorders of the outflow of bile (bile itself contains bilirubin) from the gallbladder and bile ducts, disorders of the blood, in which too many red blood cells containing bilirubin break down.
Bilirubin is a yellow substance formed from the breakdown of red blood cells that carry oxygen throughout the body. When red blood cells die, the liver filters their breakdown products from the bloodstream. But with pathologies (diseases of the liver itself and biliary tract, increased destruction of red blood cells), the liver may not keep up with this process, bilirubin accumulates, and the skin, sclera of the eyes and mucous membranes become yellow.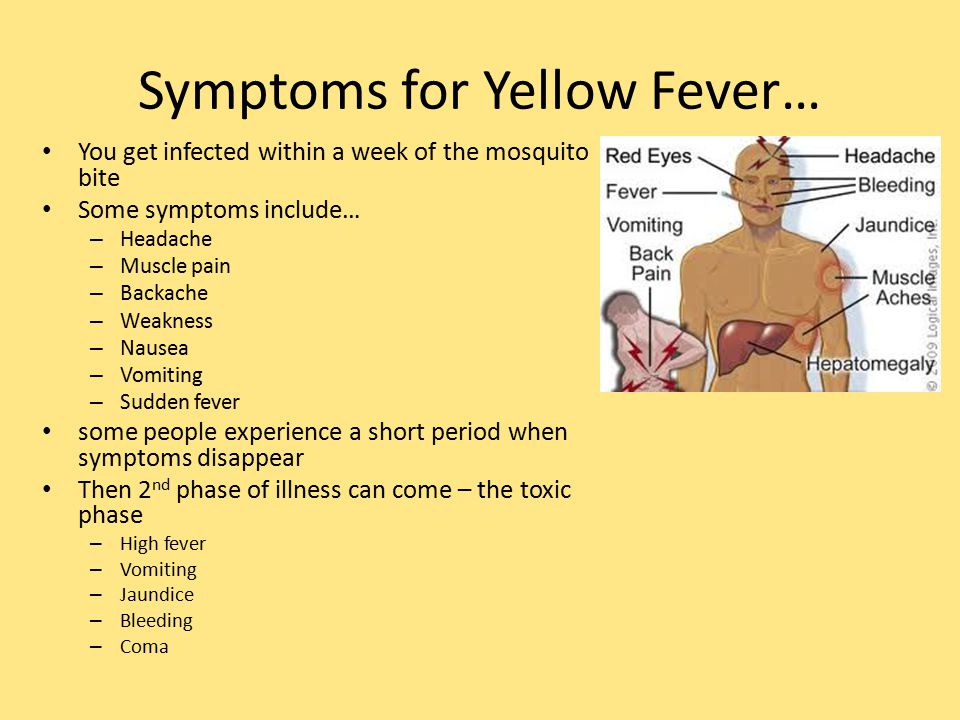
Get tested for bilirubin at CITILAB
- Total bilirubin
- Bilirubin direct (conjugated)
Types of jaundice
There are several types of jaundice, and depending on this, the mechanism of damage differs.
There are three types of jaundice:
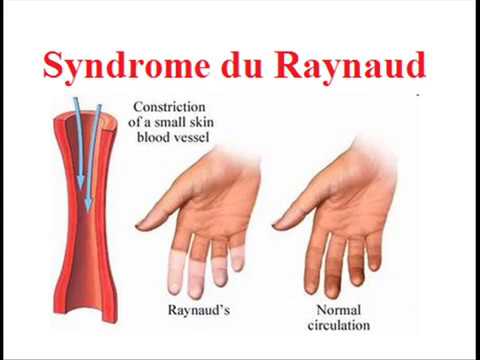
- Prehepatic (hemolytic) jaundice. Appears when too many red blood cells break down. This process is called hemolysis. When too many red blood cells break down at once, a large amount of bilirubin is released that the liver cannot handle. This happens, for example, with hereditary types of anemia, when a person's erythrocytes (red blood cells) have a special shape and are prone to more rapid destruction.
- Hepatic (parenchymal) jaundice. This type is associated with damage to the liver, from which the filtering ability of the organ suffers, and too much bilirubin enters the bloodstream. This is possible with liver infections, hepatitis, cirrhosis.
- Subhepatic (mechanical) jaundice. This type of jaundice occurs due to blockage of the bile ducts that connect the liver, gallbladder, and intestines.
The bile ducts are a series of tubes that look like blood vessels but are responsible for transporting bile from the liver to the gallbladder. If the obstruction does not allow the liver to remove excess bilirubin, serious malfunctions occur in its work, which in turn provoke jaundice. This happens due to gallstones, enlarged lymph nodes or tumors.
Symptoms of jaundice
From the name of the syndrome it is clear what constitutes the main symptom. With jaundice, the whites of the eyes, skin and other tissues of the human body turn yellow. Interestingly, the shade of yellow can suggest the type of jaundice. With hemolytic jaundice, the skin becomes pale and acquires a light yellow, lemon tint. With hepatic - orange. With mechanical jaundice, the skin darkens, becomes earthy, greenish in color.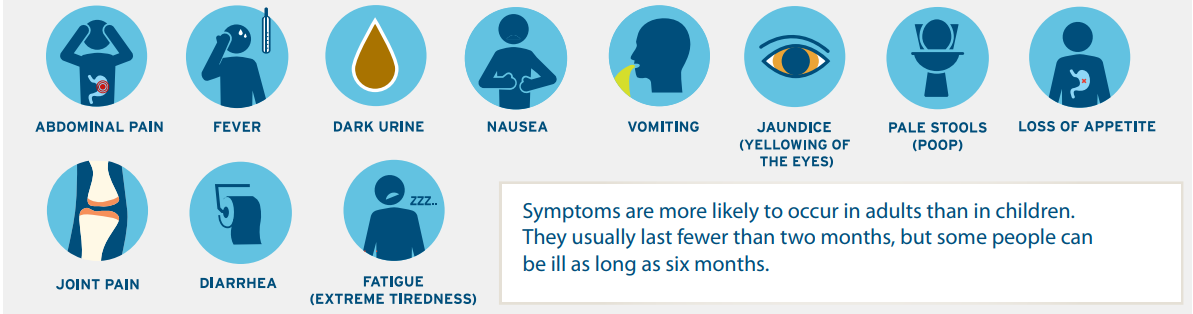
Jaundice due to acute illness is usually accompanied by fever, chills, abdominal pain, flu-like symptoms, dark urine, and light-colored stools.
If jaundice develops as a result of a chronic pathology, there may be symptoms such as weight loss or pruritus. Jaundice caused by cancer of the pancreas or biliary tract may be accompanied by abdominal pain.
Jaundice in children
A common occurrence is neonatal jaundice. As in adults, childhood jaundice is associated with elevated levels of bilirubin in the blood, but in the vast majority of cases it does not pose a serious threat to life or health.
Jaundice is one of the most common syndromes faced by newborns. According to statistics, almost 60% of full-term children and 80% of those born prematurely (before the 37th week of pregnancy) have jaundice of varying degrees at birth. At the same time, 60-70% of this number are faced with a physiological, and not a pathological, form of jaundice. And only one in 20 babies has bilirubin in the blood so high that it needs treatment.
And only one in 20 babies has bilirubin in the blood so high that it needs treatment.
Symptoms of neonatal jaundice usually develop 2 to 3 days after birth and resolve without treatment by 2 weeks. Most hospitals screen children for jaundice before discharge. Despite the fact that jaundice in newborns usually goes away without medical attention, at the first symptoms it is necessary to show the baby to the doctor so that the specialist can determine the cause of the yellow sclera or yellow skin and give individual recommendations.
Jaundice is common in newborns because infants' red blood cells break down faster. In addition, a newborn's liver is not fully developed, so it does not remove bilirubin from the blood as efficiently as it does in an adult. Plus - the low content of bacteria in the intestines of newborns also affects the exchange of bilirubin, increasing its content in the blood. Usually, by the end of the second week of a baby's life, his liver begins to cope with the amount of bilirubin, and the indicator returns to normal.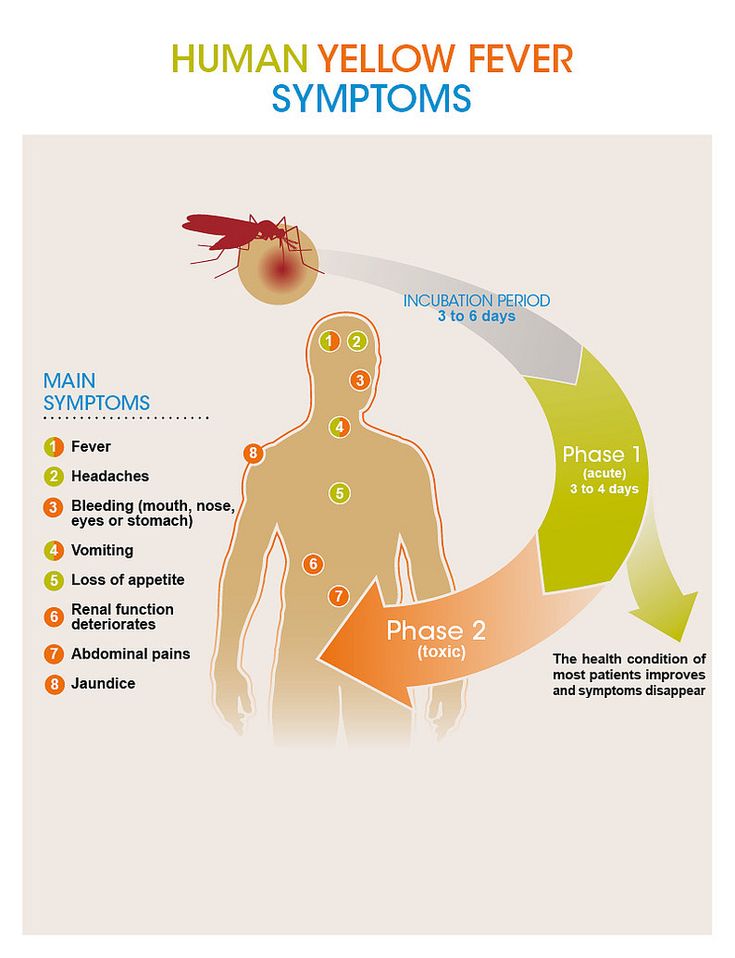
Treatment is usually only recommended if tests show a very high level of bilirubin in the child's blood. In especially high amounts, bilirubin has a neurotoxic effect - that is, it can harm the baby's brain. The extent of the damage depends on the duration of the jaundice and the degree to which the bilirubin is elevated.
Phototherapy is often used to lower the baby's bilirubin levels. Light from a special lamp falls on the skin and converts bilirubin into a form that is more easily broken down by the liver. In rare and severe cases, exchange transfusion is used: the baby's blood is removed using a catheter and replaced with blood from a suitable donor. Most babies respond well to treatment and are discharged from the hospital within a few days.
Jaundice in adults
Jaundice in adults is less common than in children and can occur for many reasons, including:
- Hepatitis. This is an inflammatory disease of the liver, often caused by a virus.
 Hepatitis can be acute (completely curable) or chronic. Other causes of hepatitis: drugs, drugs, alcohol, autoimmune diseases. Such damage to the liver eventually leads to jaundice.
Hepatitis can be acute (completely curable) or chronic. Other causes of hepatitis: drugs, drugs, alcohol, autoimmune diseases. Such damage to the liver eventually leads to jaundice. - Blocked bile ducts. These thin tubes carry bile from the liver and gallbladder to the small intestine. Gallstones and tumors can block the ducts.
- Pancreatic cancer: This is the 10th most common cancer in men and 9th in women.
- Blood disorders that cause rapid breakdown of red blood cells.
Gilbert's syndrome
Separately, it is worth highlighting Gilbert's syndrome, a common hereditary disease, also known as constitutional liver dysfunction and familial non-hemolytic jaundice. It does not require treatment, and many doctors do not consider it a disease and consider it as a variant of the norm and an individual feature. Gilbert's syndrome occurs in 1-5% of the population, depending on the region. It is associated with a defect in the gene that is responsible for the production of a liver enzyme.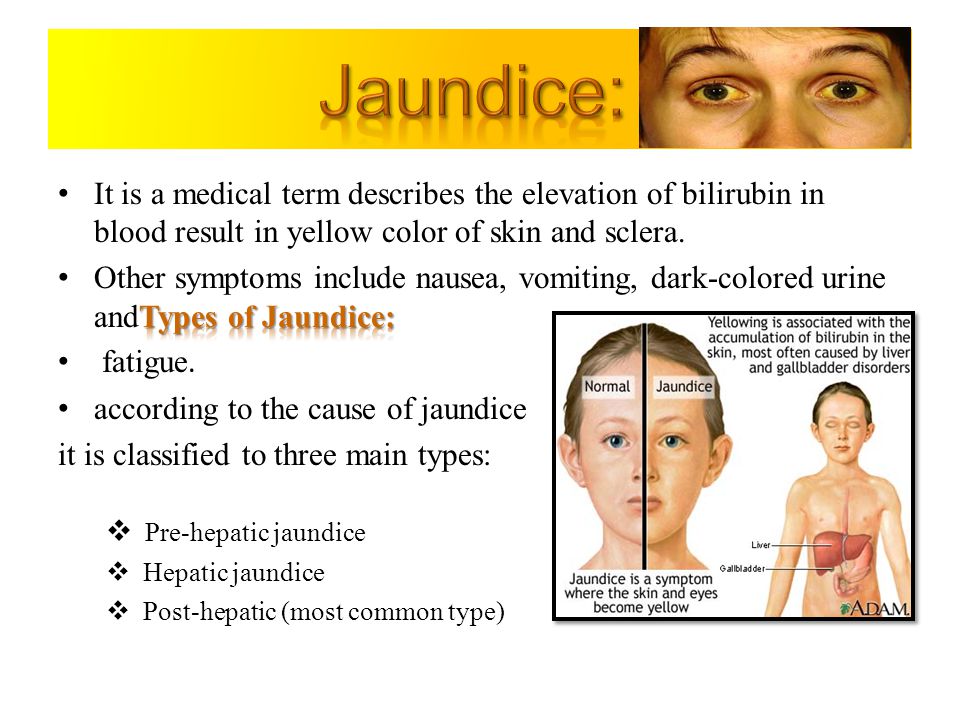 This enzyme binds indirect bilirubin.
This enzyme binds indirect bilirubin.
In a third of carriers of Gilbert's syndrome, the pathology does not manifest itself throughout life. It is often asymptomatic and is only detected by a blood test for bilirubin. However, more pronounced symptoms are also possible: pain in the right hypochondrium, metallic taste in the mouth, flatulence, vomiting, general weakness and fatigue, loss of appetite, insomnia. The symptoms are varied, and often patients with Gilbert's syndrome experience low mood, irritability, and anxiety.
There is usually no specific treatment for Gilbert's syndrome. The patient needs to limit the amount of fatty foods in the diet, adhere to a healthy lifestyle and visit a gastroenterologist - he is the one who diagnoses and treats this disease.
Diagnosis and treatment of jaundice
A preliminary diagnosis can be made already by skin color, but we repeat that jaundice is not a disease, but a syndrome. Therefore, all further diagnostics after the initial examination will be aimed at identifying the cause of the symptoms.
Therefore, all further diagnostics after the initial examination will be aimed at identifying the cause of the symptoms.
In case of yellowing of the skin or sclera, the following tests should be taken:
- complete blood count;
- urinalysis;
- biochemical blood test, including a blood test for total bilirubin and direct bilirubin;
- urinalysis for total bilirubin and direct bilirubin;
- blood for antibodies to viral hepatitis.
The next step is hardware diagnostics. Ultrasound of the liver and biliary tract is often required. An MRI or tomography may also be ordered by a doctor.
Treatment is selected individually, depending on the causes that caused jaundice, the condition of the internal organs and the results of the studies. Jaundice has many types and manifestations, and its treatment is also varied.
Different types of jaundice are dealt with by different specialists: therapists, infectious disease specialists, hematologists, oncologists.