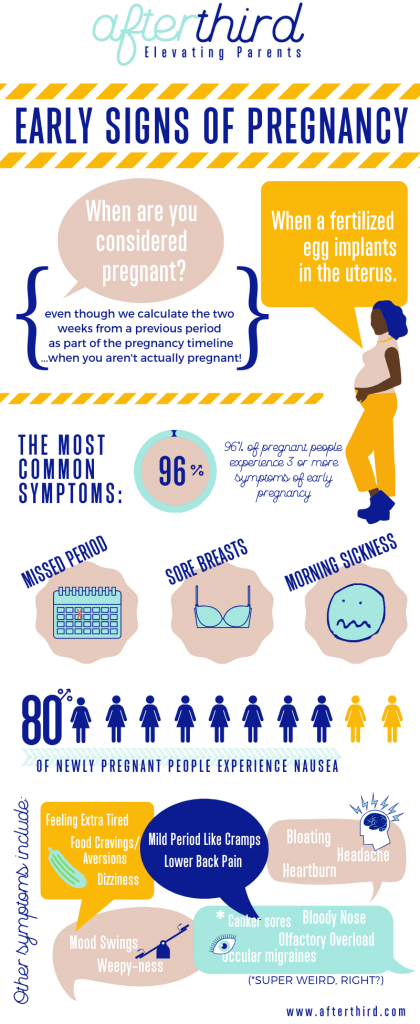
Partial molar pregnancy symptoms
Molar pregnancy - Symptoms and causes
Overview
A molar pregnancy — also known as hydatidiform mole — is a rare complication of pregnancy characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta.
There are two types of molar pregnancy, complete molar pregnancy and partial molar pregnancy. In a complete molar pregnancy, the placental tissue is abnormal and swollen and appears to form fluid-filled cysts. There's also no formation of fetal tissue. In a partial molar pregnancy, there may be normal placental tissue along with abnormally forming placental tissue. There may also be formation of a fetus, but the fetus is not able to survive, and is usually miscarried early in the pregnancy.
A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.
Products & Services
- Book: Your Guide to Miscarriage and Pregnancy Loss
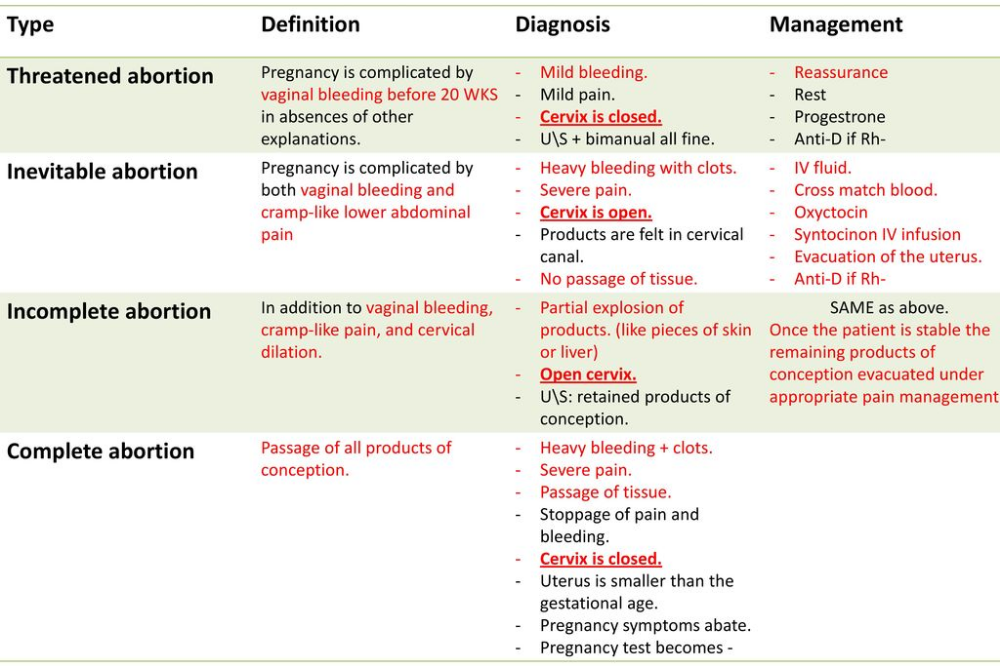
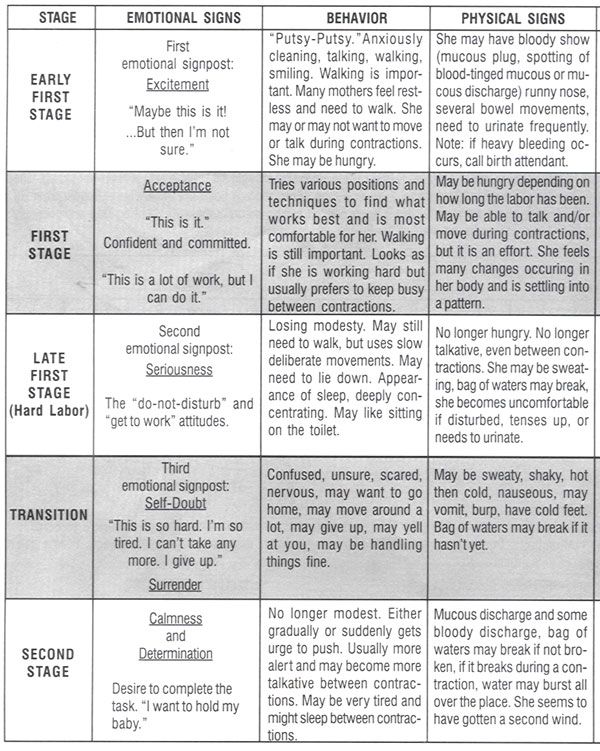
Symptoms
Molar pregnancy
Molar pregnancy
During a molar pregnancy, the placental tissue develops abnormally, and can appear as a mass of cysts. The embryo either doesn't form or is malformed and can't survive.
A molar pregnancy may seem like a normal pregnancy at first, but most molar pregnancies cause specific signs and symptoms, including:
- Dark brown to bright red vaginal bleeding during the first trimester
- Severe nausea and vomiting
- Sometimes vaginal passage of grapelike cysts
- Pelvic pressure or pain
If you experience any signs or symptoms of a molar pregnancy, consult your doctor or pregnancy care provider. He or she may detect other signs of a molar pregnancy, such as:
- Rapid uterine growth — the uterus is too large for the stage of pregnancy
- High blood pressure
- Preeclampsia — a condition that causes high blood pressure and protein in the urine after 20 weeks of pregnancy
- Ovarian cysts
- Anemia
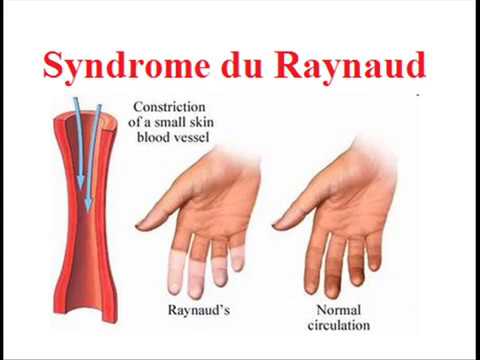
- Overactive thyroid (hyperthyroidism)
Request an Appointment at Mayo Clinic
Causes
A molar pregnancy is caused by an abnormally fertilized egg. Human cells normally contain 23 pairs of chromosomes. One chromosome in each pair comes from the father, the other from the mother.
Human cells normally contain 23 pairs of chromosomes. One chromosome in each pair comes from the father, the other from the mother.
In a complete molar pregnancy, an empty egg is fertilized by one or two sperm, and all of the genetic material is from the father. In this situation, the chromosomes from the mother's egg are lost or inactivated and the father's chromosomes are duplicated.
In a partial or incomplete molar pregnancy, the mother's chromosomes remain but the father provides two sets of chromosomes. As a result, the embryo has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father's genetic material.
Risk factors
Approximately 1 in every 1,000 pregnancies is diagnosed as a molar pregnancy. Various factors are associated with molar pregnancy, including:
- Maternal age. A molar pregnancy is more likely in women older than age 35 or younger than age 20.
- Previous molar pregnancy.
 If you've had one molar pregnancy, you're more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 women.
If you've had one molar pregnancy, you're more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 women.
Complications
After a molar pregnancy has been removed, molar tissue may remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). This occurs in about 15% to 20% of complete molar pregnancies, and up to 5% of partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, an invasive hydatidiform mole penetrates deep into the middle layer of the uterine wall, which causes vaginal bleeding.
Persistent GTN can nearly always be successfully treated, most often with chemotherapy. Another treatment option is removal of the uterus (hysterectomy).
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. A complete molar pregnancy is more likely to have this complication than a partial molar pregnancy.
Prevention
If you've had a molar pregnancy, talk to your doctor or pregnancy care provider before conceiving again. He or she may recommend waiting for six months to one year before trying to become pregnant. The risk of recurrence is low, but higher than the risk for women with no previous history of molar pregnancy.
During any subsequent pregnancies, your care provider may do early ultrasounds to monitor your condition and offer reassurance of normal development. Your provider may also discuss prenatal genetic testing, which can be used to diagnose a molar pregnancy.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Molar pregnancy information and support
What is a molar pregnancy?
A molar pregnancy can be a traumatic experience. Try to remember that molar pregnancies are not caused by anything you (or the baby’s father) did or didn’t do. There is support available if you need it.
Try to remember that molar pregnancies are not caused by anything you (or the baby’s father) did or didn’t do. There is support available if you need it.
“Two of the most important things are to not blame yourselves and not to give up hope. Talk about your feelings and emotions with your partner and try to contact others in your local area who have experienced what you are going through. You are never alone.”
Sue
There are two main types of molar pregnancy. Sadly, neither type of pregnancy can survive.
Complete mole
Complete moles usually happen when a single sperm fertilises an ‘empty’ egg which has none of the mother’s genetic material inside. Because of this, a fetus does not develop.
Partial mole
Partial moles happen when two sperm fertilise a normal egg. In a partial mole, there are usually some early signs of a fetus, but this won’t develop into a baby.
What causes a molar pregnancy?
We don’t know exactly what causes a molar pregnancy, but there are some things that increase the risk. Again, try to remember that molar pregnancies are not caused by anything you (or the baby’s father) did or didn’t do.
Again, try to remember that molar pregnancies are not caused by anything you (or the baby’s father) did or didn’t do.
Age
Molar pregnancies are more common in teenage women and women over 45.
Ethnicity
Molar pregnancies are about twice as common in women of Asian origin.
Previous molar pregnancy
If you've had a molar pregnancy before, your chance of having another one is about 1 in 80, compared with 1 in 600 for women who haven't had one before. If you've had 2 or more molar pregnancies, your risk of having another is around 1 in 5.
A low intake of carotene (a form of vitamin A) and folic acid
Women who don't get enough of these vitamins have a higher rate of complete molar pregnancy.
However, you should not take any supplements that include vitamin A. Having large amounts of vitamin A can harm your unborn baby. The best thing you can do to make sure you are getting all the vitamins and minerals you need is to eat a healthy, balanced diet. Find out more about tips for a pre-pregnancy diet.
Find out more about tips for a pre-pregnancy diet.
Folic acid is a vitamin (B9). It is found in certain foods and it can also be taken as tablets. The best thing to do is take folic acid tablets for two to three months before you get pregnant and for the first 12 weeks of pregnancy. This gives the most protection to your future baby against neural tube defects, such as spina bifida.
Find out more about folic acid in pregnancy.
What are the symptoms of a molar pregnancy?
There are often no symptoms of a molar pregnancy. It may only be diagnosed during a routine ultrasound scan at 8-14 weeks or during tests are done after a miscarriage.
Some women with a molar pregnancy have:
- vaginal bleeding or a dark discharge from the vagina in early pregnancy (usually in the first trimester) – this may contain small, grape-like lumps
- severe morning sickness
- an unusually swollen tummy.
Some of these symptoms are quite common in pregnancy and aren't necessarily a sign that anything is wrong with your baby.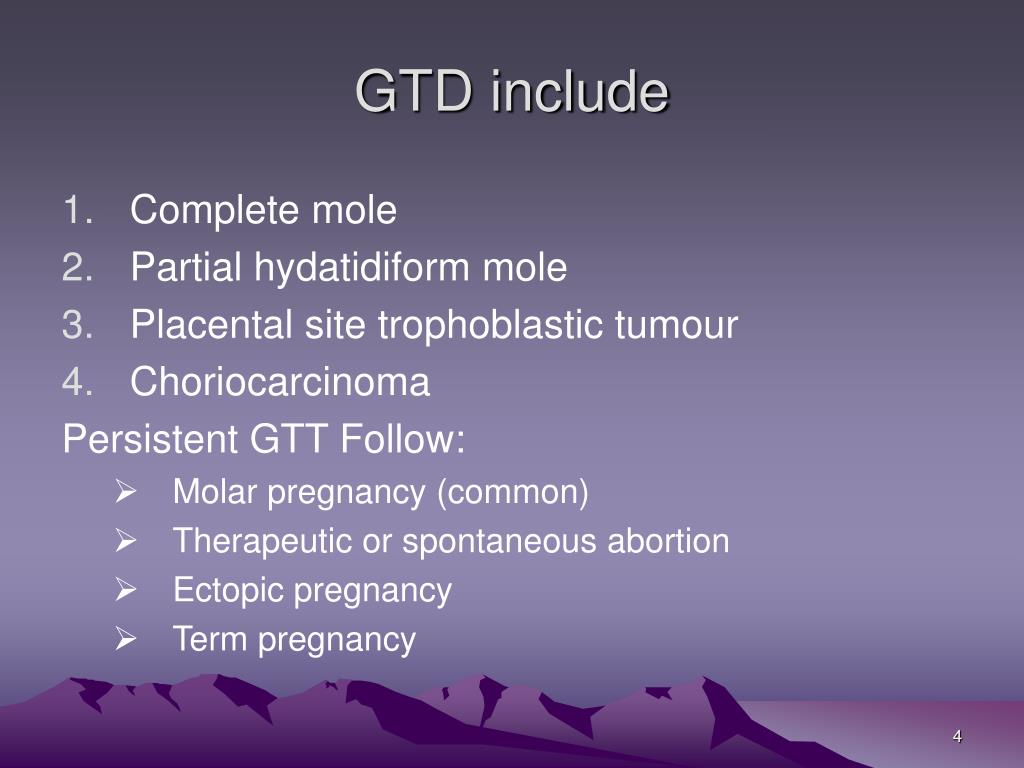 Try not worry, but contact a health professional and get checked out just in case.
Try not worry, but contact a health professional and get checked out just in case.
Less common symptoms include:
- high blood pressure
- symptoms of an overactive thyroid gland (such as tiredness, weakness, twitching or trembling)
- stomach pain (because of large ovarian cysts).
When should I get help?
Contact your midwife or GP if you think you have any of these symptoms.
You will be referred to an early pregnancy unit for an ultrasound scan. If you’ve had a molar pregnancy before and you think you are having another, you can contact the early pregnancy unit yourself without contacting your midwife first.
As well as a scan, you will also have a blood test, which measures the amount of a pregnancy hormone called human chorionic gonadotrophin (hCG). This is usually much higher in molar pregnancies than in healthy pregnancies.
Doctors may also discover a molar pregnancy after a woman has a miscarriage if the tissues are looked at under a microscope.
What is the treatment for a molar pregnancy?
Unfortunately, a molar pregnancy will not survive and will need to be removed. You will likely need surgery to remove the pregnancy. Most women are successfully treated with suction removal and can go home later the same day.
What follow-up will I have?
In the UK, all women who have had a molar pregnancy are asked if their details can be registered with a specialist centre. This is so your treatment is provided by doctors who are experts in this field. These centres are in hospitals in London, Sheffield and Dundee.
After registering with a specialist centre, you will have follow-up appointments for at least 6 months. Your specialist centre will ask you to have regular blood or urine tests done at your local GP surgery. These are done to check if your hCG levels are going back to normal.
Does a molar pregnancy have any complications?
Very rarely, a molar pregnancy can lead to gestational trophoblastic neoplasia (GTN). GTN is a rare form of cancer. This sounds frightening, but it has a cure rate of over 99%.
GTN is a rare form of cancer. This sounds frightening, but it has a cure rate of over 99%.
GTN happens when some of the molar pregnancy tissue is still in the uterus. It is usually diagnosed if your hCG levels do not return to normal or if you have persistent or irregular bleeding after a pregnancy.
What happens if I have GTN?
You will usually need to have further treatment from the specialist centre you are registered with. This may involve a second operation to remove any tissue from your womb or chemotherapy.
Treatment is continued until 6 weeks after your hCG level has returned to normal. In very rare cases, some women may need to have a hysterectomy (removal of the womb).
If you have chemotherapy for GTN, your periods will usually restart 2 to 6 months after the end of chemotherapy. Your fertility (ability to get pregnant) is usually not affected.
Your specialist centre will talk to you about the treatment you need and any side effects.
Will I still be able to have a baby in the future?
Yes, you have every chance of getting pregnant again and having a healthy baby.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) The risk of having another molar pregnancy is small (about 1 in 80).
The risk of having another molar pregnancy is small (about 1 in 80).
It’s best not to try getting pregnant again until all your follow-up treatment has finished. For most women, this will take about 6 months.
If you have GTN, you will need to wait for 12 months after you have finished chemotherapy treatment. This is because GTN can sometimes come back. This is rare and happens to around 3% of women.
Contraception
You should use barrier methods of contraception such as condoms or diaphragm until your hCG levels are normal. You should not have an intrauterine contraceptive device fitted until your hCG levels have returned to normal. This is because it can cause a puncture in the uterus after a molar pregnancy.
Once your hCG levels are normal, you may use all types of hormonal contraception including the combined contraceptive pill, progestogen only pill, progestogen injection and progestogen implant.
Talk to your healthcare team about what contraception will be best for you.
How you may feel about a molar pregnancy
It can take time to recover emotionally and physically from a molar pregnancy. Waiting to find out if everything is okay after a lot of tests can be very stressful.
Try to remember that most women who have had a molar pregnancy go on to have healthy pregnancies and babies in the future.
You may find it helpful to:
- talk to your partner, family or friends about how you feel
- ask your care team what support is available – they may refer you to a counsellor who specialises in support for people affected by molar pregnancy
- talk to a Tommy’s midwife free of charge from 9-5 Monday to Friday on our helpline: 0800 0147 800 or email [email protected]
- visit Molar pregnancy Support and Information, MyMolarPregnancy.com or Babycentre’s ectopic and molar pregnancy support group.
How to diagnose a molar pregnancy - advice from an obstetrician
Molar pregnancy (molar pregnancy) is a rare complication of pregnancy and a type of gestational trophoblastic disease, when the fertilization of an egg by a sperm cell does not occur correctly and creates abnormal cells or accumulations of water-filled sacs inside the uterus. This pathology is rare, and according to statistics, for every 590 pregnancies, there is about 1 case of a molar pregnancy. Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist.
This pathology is rare, and according to statistics, for every 590 pregnancies, there is about 1 case of a molar pregnancy. Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist.
Quick navigation
Causes
Molar pregnancy is caused by an imbalance in the genetic material (chromosomes) during pregnancy. This usually occurs when an egg that contains no genetic information is fertilized by a sperm (complete molar pregnancy) or when a normal egg is fertilized by two sperm (partial molar pregnancy).
Mole risk factors
All pregnant women are at risk of developing a molar pregnancy, but this risk is very small.
Age. Researchers have found that certain types of molar pregnancies are more common in certain age groups. Complete molar pregnancies are more common in mothers over 45 years of age. The risk is moderately increased in young adolescents. Age does not affect the risk of partial molar pregnancies.
Complete molar pregnancies are more common in mothers over 45 years of age. The risk is moderately increased in young adolescents. Age does not affect the risk of partial molar pregnancies.
Previous molar pregnancy. If a woman has already had one molar pregnancy, she has a 1 in 100 chance of having a recurrence. If a woman has had two or more molar pregnancies, the risk of another pregnancy with this condition is higher, about 15 to 20 out of 100.
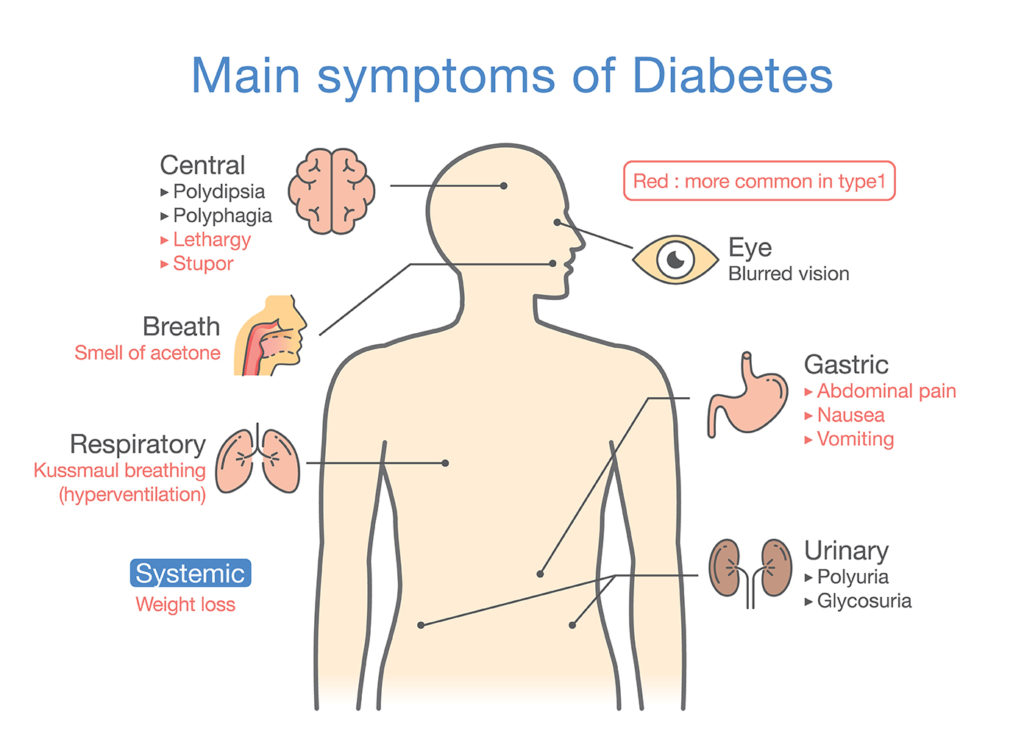
Symptoms of molar pregnancy
Vaginal bleeding
Vaginal bleeding is the most common symptom of molar pregnancy. Bleeding can occur during normal pregnancy and is not always serious, but the woman should immediately inform the gynecologist or midwife about it. Women with a mole are more likely to develop blood clots or a watery brown vaginal discharge. In some pregnant women, pieces of molar tissue come out, which can look a bit like small bunches of grapes. Bleeding caused by a mole usually starts between 6 and 12 weeks of gestation.
The following symptoms are rare. This is because most hydatidiform moles are detected and corrected during routine ultrasound examinations performed in early pregnancy. In some women with a complete hydatidiform mole, the abdomen may expand more rapidly than in a normal pregnancy. In women with partial hydatidiform mole, the uterus and abdomen may be smaller than expected for this stage of pregnancy.
Nausea is common in normal pregnancies, but may be more severe and more frequent with mole. This is called hyperemesis.
Anemia means that the patient has few red blood cells in her body. If a woman is losing blood due to vaginal bleeding, her red blood cell count may decrease. Due to anemia, the patient may feel constant fatigue and shortness of breath.
Pre-eclampsia is a complication that can occasionally occur during the last 3 months of a normal pregnancy. The main symptoms are high blood pressure and protein in the urine. In rare cases, with a hydatidiform mole, preeclampsia can be obtained much earlier.
An overactive thyroid is a rare symptom of molar pregnancy. The medical term for this is hyperthyroidism.
Molar pregnancy stages
staging is a system doctors use to describe the size of a tumor and whether it has spread. Gynecologists usually remove abnormal molar tissue during pregnancy from the uterus. If the levels of a hormone called hCG return to normal shortly after the mole is removed, then the doctor does not need to stage the mole. In most women, the hCG level practically disappears within 4-6 weeks after the removal of the hydatidiform mole. Once the molar tissue has left the uterus, it cannot produce hCG. Thus, in addition to subsequent blood and urine tests to check for molar tissue return, the woman will not need additional tests.
If the hCG level remains high or rises, this may be a sign that abnormal cells are still present in the uterus. The cells may spread to deeper layers of the uterus or other parts of the body. Gynecologists call this persistent trophoblastic disease. In this case, the woman will need additional tests to determine the stage of the tumor.
Gynecologists call this persistent trophoblastic disease. In this case, the woman will need additional tests to determine the stage of the tumor.
Survival of hydatidiform mole
Almost all women with hydatidiform mole recover. Doctors remove all of the abnormal molar tissue with surgery, and most women don't need further treatment. In a small number of patients, some abnormal cells remain and may spread to deeper layers of the uterus or other parts of the body. This is called persistent trophoblastic disease. Chemotherapy can usually completely rid a woman of all abnormal cells.
Molar Pregnancy Diagnosis
When a woman is pregnant, the placenta produces the hormone human chorionic gonadotropin (hCG), which helps the baby develop. The placenta releases hCG into the bloodstream, and the body gets rid of the rest in the urine. HCG is produced during molar pregnancy, but is at a much higher level than normal. Thus, routine blood tests during pregnancy may reveal a mole.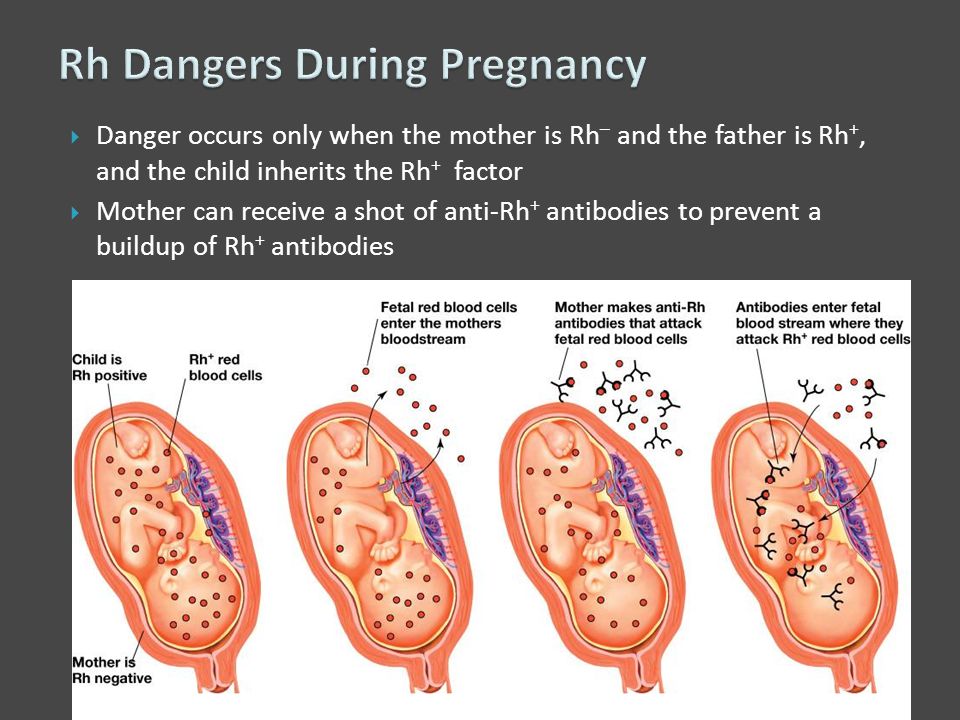
Women usually have a routine ultrasound at 12 weeks pregnant. Molar pregnancies may show a characteristic "blizzard appearance" on scans. An ultrasound scan is a good way to diagnose complete molar pregnancies, but it is not as good at detecting partial molar pregnancies. A partial molar pregnancy can still be detected by a blood test.
Diagnosis after a miscarriage or abortion
A doctor will usually examine the tissues of the placenta and fetus if a woman has had a miscarriage in the hospital or an abortion. These checks may reveal abnormal mole cells. If positive, the woman will need treatment to remove molar tissue from the uterus.
Treatments for hydatidiform mole
There are various surgical options for removing a molar pregnancy.
Mole surgery
Most women have a minor operation under general anesthesia to remove molar tissue from the uterus. The operation is called dilation and suction evacuation. The surgeon uses a thin tube to gently suck out the molar tissue. Sometimes they may also use a sharp instrument to cut tissue from the uterine lining. This is called expansion and scraping. This treatment removes all of the molar tissue for most women.
Sometimes they may also use a sharp instrument to cut tissue from the uterine lining. This is called expansion and scraping. This treatment removes all of the molar tissue for most women.
Removal of the uterus (hysterectomy)
The surgeon may suggest removal of the uterus (hysterectomy) instead of removing just the molar tissue.
Drug treatment to remove molar tissue
Some women with partial mole are given drug treatment to make the uterus contract and get rid of the abnormal cells.
Author: Belyakov Nikolai Grigorievich
Specialization: Pediatrician
Where does the reception: Clinic General Medical Center (GMC), St. Petersburg
Share:
The best specialists in St. Petersburg with a rating of 4.5+
Veromei Dominika Tadeushevna
Specialization: Therapist, Gynecologist, Obstetrician-gynecologist
Medical experience: since 20105
Where does the appointment: Dr. Pel's Clinic
Pel's Clinic Andreeva Oksana Sergeevna
Specialization: Ultrasound doctor, Gynecologist, Obstetrician-gynecologist
Medical experience: since 1998
Where does the appointment: Dr. Pel's Clinic
Evgeniya Kaminskaya
Specialization: Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 1994
Where he meets: Clinic of Dr. Pel, IEM Medical Center, Medical College
Golotina Maria Vladimirovna
Specialization: Ultrasound doctor, Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 2008
Where does the appointment: Dr. Pel's Clinic
Literature:
- Beskova T.K., Kalinin A.V. Study of the immune status in patients with hydatidiform mole // Journal "A and G" 1981. No. 9.
- Davydova M.A., Kalelyushnik N.
 L., Osipov R.A. Progressive form of hydatidiform drift//Kazan medical journal 1979 (1).
L., Osipov R.A. Progressive form of hydatidiform drift//Kazan medical journal 1979 (1). - Kalinin A.V. Clinical and morphological features of hydatidiform mole and its prognosis // Abstract of the discussion for the degree of candidate of medical sciences. 1982.
- I. Persianinov L.S., Demidov V.N. Ultrasonic diagnostics in obstetrics. — M.: Medicine. - 1980. —- 335 S.
- Kosenko IA, Bakinovskaya IE Ultrasound diagnosis of trophoblastic tumors of the uterus. Minsk: Medicine, 2005.-75p.
Latest diagnostic articles
Radiation therapy
Radiation therapy is a treatment that uses radiation to kill cancer cells. This therapy is most often prescribed by oncologists for the treatment of oncological diseases.
Read more
Is MRI harmful to health
When making an MRI appointment, the patient sometimes has questions about the safety of the examination: “Is there any harm from MRI for the body, what is the danger of magnetic resonance imaging, and how often can MRI be done.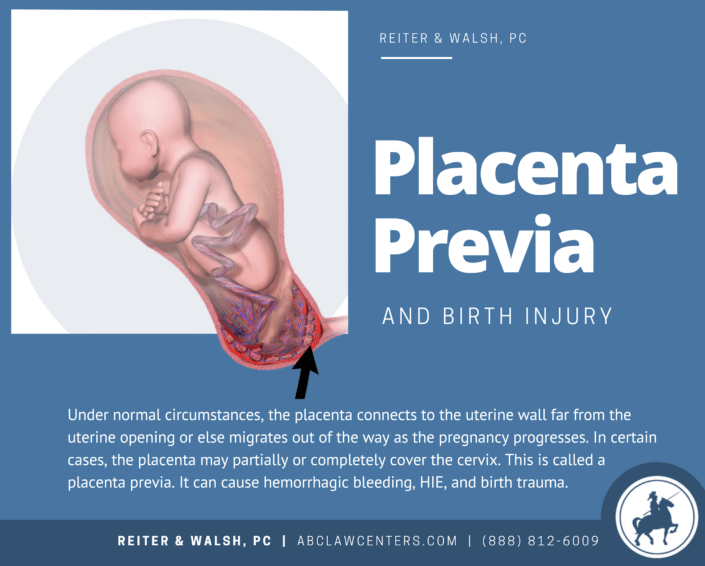 Let's figure it out.
Let's figure it out.
Read more
Principles of operation of MRI, ultrasound, CT, X-ray and PET
In modern medicine, thanks to advances in technology, there is a wide range of diagnostic equipment that helps doctors in the early detection of diseases and pathological disorders. In this article we will talk about the principles of operation of MRI, ultrasound, CT,
Read more
MRI during pregnancy
Since every day MRI technology provides doctors of St. Petersburg medical centers with an increasing range of diagnostic capabilities, it is being actively used in pediatrics, prenatal diagnostics in pregnant women and oncology. As soon as a woman finds out that she will become a mother, she immediately has the question of what procedures she can do and which are contraindicated. Almost all pregnant women know that they are strictly forbidden to take x-rays and can undergo ultrasound.
Read more
Mole - causes, signs, treatments and consequences
Bubble skid during pregnancy - the transformation of the chorionic villi into vesicles with liquid, accompanied by the growth of the epithelium.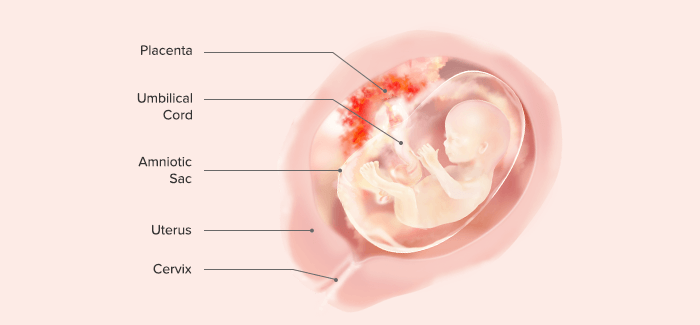 Pathology leads to intrauterine death of the fetus. The main manifestations are pronounced early toxicosis, bleeding. To detect abnormalities, it is necessary to do a vaginal examination, ultrasound.
Pathology leads to intrauterine death of the fetus. The main manifestations are pronounced early toxicosis, bleeding. To detect abnormalities, it is necessary to do a vaginal examination, ultrasound.
Classification of neoplasms
Bubble skid or molar pregnancy - this is how a rare anomaly of the fetal egg is called in gynecology. They are detected in 0.02-0.8% of pregnant women. It develops due to disturbances in the development and growth of the outer layer of the embryo. Pathology refers to gestational trophoblastic diseases. The ICD-10 code is O01.
The US National Institutes of Health identifies 2 options for the development of pathology. Benign tumors include partial and complete hydatidiform drift. To malignant - an invasive or destructive form of neoplasm. These are chorionic carcinoma, trophoblastic tumor of the placental bed, epithelioid trophoblastic tumor. Classification by histological structure - syncytial or cytotrophoblastic type, mixed form.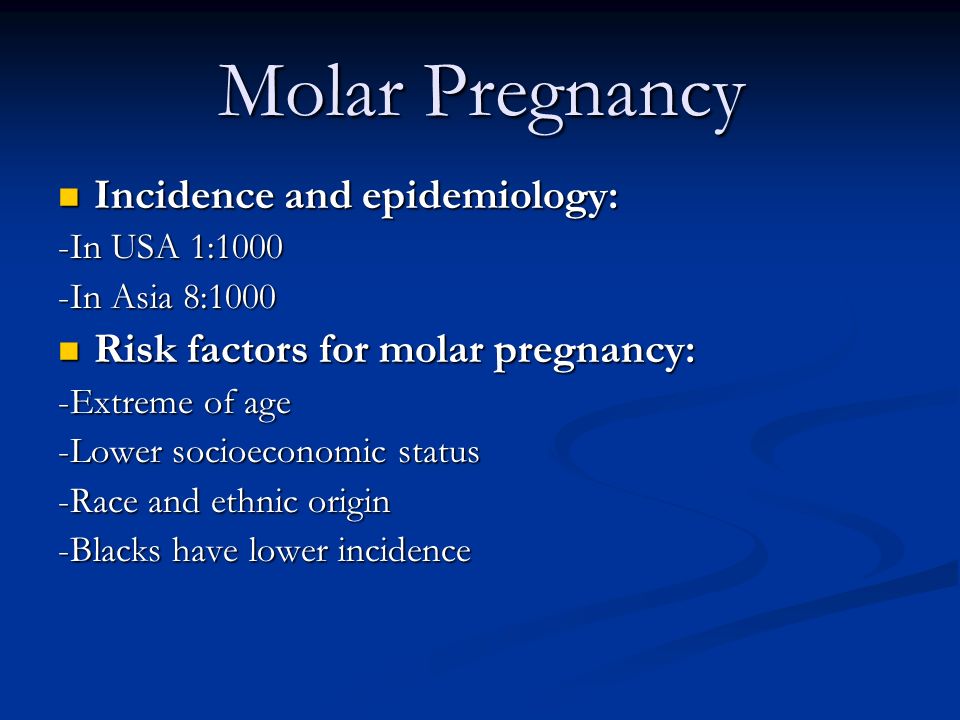
In molar pregnancy, instead of a normal embryo, multiple bubble cysts of different sizes are formed. A fertilized egg looks like a bunch of grapes.
With the full form of the pathology, there are no maternal chromosomes in the fertilized egg. Embryo, fertilized bladder and placenta are not formed. The fetus dies due to the degeneration of the chorionic villi. After the death of the fetus, the neoplasm grows, the uterus rapidly increases in size.
Partial hydatidiform mole forms after 12 weeks of gestation. Pathology occurs if a fertilized egg contains 2 sets of father's chromosomes and one set of maternal chromosomes. This occurs when one egg and two sperm fuse, or when the father's chromosomes are duplicated. The placental structure has a cystic structure.
The invasive form is characterized by the germination of chorionic villi into the deep layers of the myometrium, tissue destruction. The pathological process can be limited to the uterus, spread to other genital organs. Metastases can spread to the lungs and other distant organs.
Metastases can spread to the lungs and other distant organs.
Important! Malignant trophoblast tumors may occur during childbearing, after childbirth, abortion, ectopic pregnancy. But most often they are a complication of molar pregnancy.
Causes of pathology
Bubble drift is a chromosomal pathology. Occurs with the loss of maternal genes, duplication of a set of paternal genes, fertilization by two sperm at the same time.
The exact reasons for the development of molar pregnancy are not fully understood. A supporter of the viral degeneration of the trophoblast believes that the virus starts the process of mutation at the initial stage of embryo formation, a tumor is formed.
According to the immunological theory, in women with a metabolic predisposition to the development of neoplasms, immunity is reduced. During pregnancy, the body perceives the fetus as a transplant, a woman's immune system responds, and a molar pregnancy develops.
Risk factors:
- the presence of a molar pregnancy in history - after two cases, the risk increases by 11-25%;
- abortions - the probability of pathology increases by 3 times;
- age up to 15 and over 40 years - in early and late pregnancy, the risk of developing gestational trophoblastic disease increases by 7.5 times;
- late onset of menstruation;
- ectopic pregnancy in the fallopian tube;
- multiple births;
- immunodeficiency states;
- thyrotoxicosis;
- lack of animal fats in the diet, lack of vitamin A;
- marriages between close relatives.
Molar pregnancy should not be confused with non-vesical mole. Non-vesical mole or anembryony is a form of missed pregnancy. After fertilization and fixation, the egg does not develop into an embryo, an empty fetal egg remains. The cause of the disease can be genetic and chromosomal disorders, chronic endometritis, malformations of the uterus, diseases of the coagulation system.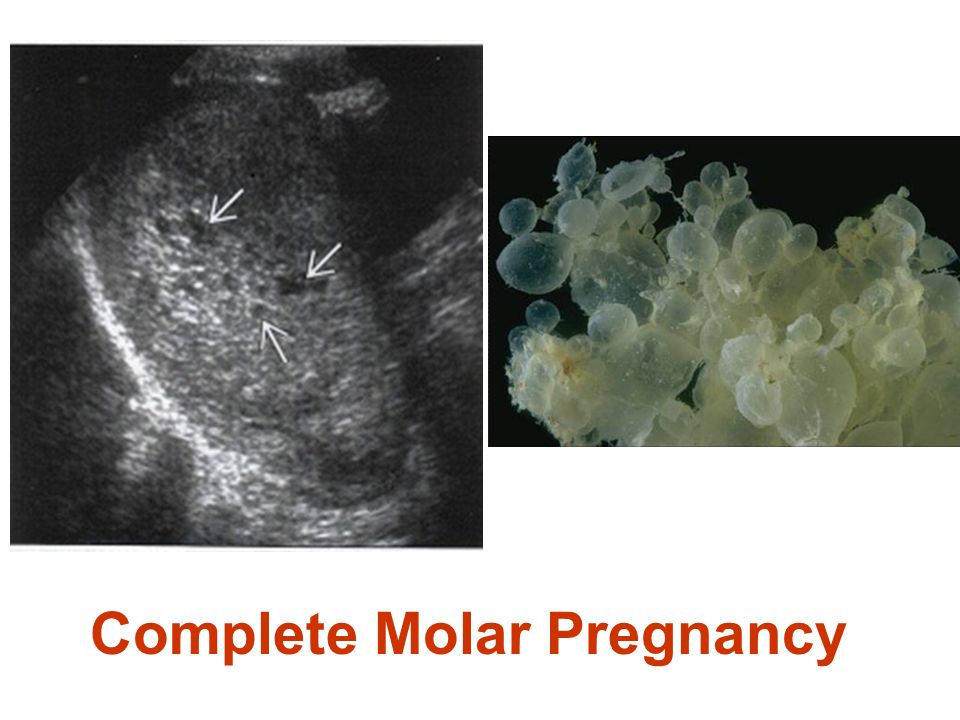
Pathogenesis of pathology
With a significant accumulation of fluid in the villi, the nutrition of the trophoblast vessels is disrupted. The structure that covers the vesicles is proliferating - characterized by rapid cell growth. When introduced into the muscular layer of the uterus, the vessels and muscle elements are destroyed.
The integumentary epithelium of the cysts can destroy the wall of the uterus, when penetrating into the abdominal cavity, internal bleeding occurs. This form of vesicles is called destructing, in terms of growth it is similar to tumors.
Stages of gestational trophoblastic neoplasms
When trophoblastic pathology is detected, additional studies are carried out to determine the degree of spread of the process to other tissues and organs. The choice of treatment methods depends on the stage of the disease, the age and general condition of the patient.
Stages of trophoblast disease:
- Bubble drift.
 The pathological process does not go beyond the uterus. If tumor cells are present in the muscle layer of the reproductive organ, the invasive form of the disease is diagnosed.
The pathological process does not go beyond the uterus. If tumor cells are present in the muscle layer of the reproductive organ, the invasive form of the disease is diagnosed. - Gestational trophoblastic disease of the placenta bed. Places of localization of malignant formation - the area of attachment of the placenta, the muscular layer of the uterus.
- Non-metastatic gestational trophoblastic tumor. The neoplasm grows into the uterus, but does not go beyond the organ. Pathology occurs after an abortion, childbirth, removal of a bubble formation.
- Metastatic trophoblastic tumor. A favorable outcome is possible if the pregnancy was no more than four months ago, the level of beta-hCG is low, metastases do not penetrate the brain and liver, and chemotherapy has not yet been performed.
Clinical manifestations
The first signs of pathology appear before the 18th week of pregnancy. The main vesical symptoms include scanty and irregular uterine bleeding. observed in 90% of patients. The bloody discharge contains particles that look like bunches of grapes. With abundant secretions, anemia develops - weakness, fatigue, palpitations, a feeling of lack of air, pale skin worries.
observed in 90% of patients. The bloody discharge contains particles that look like bunches of grapes. With abundant secretions, anemia develops - weakness, fatigue, palpitations, a feeling of lack of air, pale skin worries.
If any uncharacteristic discharge occurs during pregnancy, it is urgent to contact a gynecologist.
Signs of cystic mole:
- the size of the uterus exceeds the estimated gestational age;
- signs of severe toxicosis - vomiting, weakness, dizziness, swelling, weight loss, pain in the lower abdomen;
- symptoms of preeclampsia, eclampsia appear already in the first trimester;
- sometimes neoplasms can be felt through the anterior wall of the peritoneum;
- acute pain in the abdomen and loss of consciousness - symptoms of perforation of the uterine wall;
- the fetal heartbeat is not audible and is not recorded by hardware methods, the fetus does not move;
- biological and immunological pregnancy tests are positive.
Cysts with bubble drift reach a size of 25 mm. They are filled with a blue-white or yellowish liquid. Composition - globulins, amino acids, albumins, human chorionic gonadotropin. There are no vessels in the vesicles, or single capillaries are present.
Important! With the development of complications, bleeding intensifies, vomiting becomes indomitable. Concerns about tachycardia, respiratory failure, hand tremor. Often women complain of a feeling of fullness inside the abdomen.
Diagnostics
Bubble pregnancy is diagnosed based on the history and assessment of symptoms, ultrasound findings, and hCG hormone levels. Pathological abnormalities are visible on the micropreparation.
Diagnosis of hydatidiform mole:
| Diagnostic method | Diagnostic criteria |
| Bubble skid on ultrasound | The size of the uterus with cystic drift differs from the norm for the expected gestational age. With a full variety of pathology, ultrasound does not show the presence of an embryo and amniotic fluid. With partial - the size of the fetal bladder is increased, the fetus has a developmental delay, one or more pathological inclusions are present in the placenta. In the uterine cavity there are tissues with a fine-grained structure, in the appendages - thecalutein cysts. |
| Fetal phonocardiography | Heartbeat is not audible |
| Laboratory tests | The level of hCG with complete mole is above 100 thousand mIU / ml, with incomplete - below 100 thousand mIU / ml. In addition, the indicators of oncomarkers were increased, the level of ACE was reduced. |
| Characteristics of secretions | Bloody, vesicles are present. |
| Gynecological examination results | Visually visible bubbles on the uterus, which are called a snowstorm. The consistency of the reproductive organ is dense, but elastic, there are areas of excessive softening, the size does not correspond to the duration of pregnancy. |
| Additional symptoms | Before 20 weeks, signs of preeclampsia appear. Blood pressure rises, protein is detected in the urine. |
Additionally, studies are carried out to exclude multiple pregnancy, polyhydramnios, spontaneous miscarriage, uterine fibroids. Assign EchoGSS, hysteroscopy, diagnostic laparoscopy. If metastatic screening is suspected, it is necessary to make an x-ray of the chest and abdominal organs, a CT scan of the brain.
Pay attention! Timing of detection of partial mole - 9-34 weeks, complete - 11-25 weeks.
Treatment
Bubble drift is treated only surgically.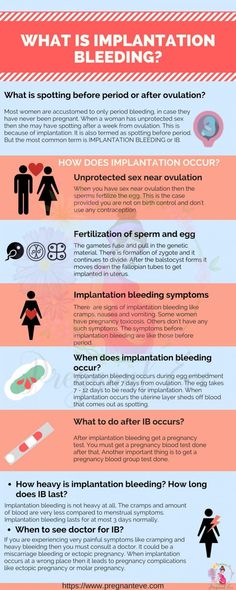 The formation is removed, a control curettage is carried out, drugs are prescribed to reduce the uterus. Since the neoplasm can be malignant, the biomaterial after removal of the tumor is sent for histology, karyotyping.
The formation is removed, a control curettage is carried out, drugs are prescribed to reduce the uterus. Since the neoplasm can be malignant, the biomaterial after removal of the tumor is sent for histology, karyotyping.
If it is necessary to preserve reproductive functions, removal is carried out using vacuum aspiration. If a woman does not plan to become pregnant in the future, life-threatening bleeding develops, an operation is performed to remove the uterus - a hysterectomy.
It is necessary to monitor the level of hCG every week after removal of the hydatidiform mole. Analyzes are prescribed until three negative results are obtained in a row. Then, during the year, monitoring is carried out once a month. Additionally, once every 2 weeks, an ultrasound of the pelvic organs, an x-ray of the lungs are done.
Important! If hCG levels do not decrease, metastases are detected, chemotherapy is prescribed. With normal indicators after a molar pregnancy, a woman is registered with an oncogynecologist for 2 years.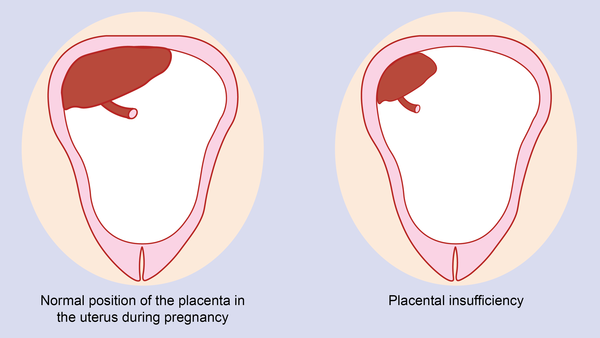
Complications
With cystic drift, the embryo dies at the initial stage of development, or the fetus dies at an early stage. It is impossible to avoid this, since the placenta is not formed correctly, severe hypoxia and nutritional deficiencies develop.
Other complications:
- re-development of cystic drift, but with proper treatment, the probability of recurrence is not more than 1%;
- preeclampsia - manifested by severe edema, high blood pressure, convulsions;
- persistent arterial hypertension;
- thyrotoxicosis - increased levels of thyroid hormones;
- intrauterine infections;
- torsion of thecalyutein cyst is a life-threatening condition;
- thrombosis and inflammation of the venous vessels of the uterus;
- sepsis;
- large thecalutein cysts in the ovaries - formed early in pregnancy if the corpus luteum does not produce enough progesterone;
- degeneration of cystic drift into chorioncarcinoma - transformation occurs in 20% of cases, is characterized by metastasis to the liver, brain, lungs, often leads to death;
- rarely - pulmonary embolism.

With partial hydatidiform mole, hydrocephalus, syndactyly, and other malformations are detected in the fetus.
According to the reviews and observations of doctors, menstruation after a cystic drift may begin on time, but 14% of women develop secondary amenorrhea. Infertility is diagnosed in 30%, and the risk of developing pathologies in the fetus during subsequent pregnancies increases.
If hydatidiform mole occurs during multiple pregnancies, in rare cases one embryo may develop normally while the other is dead or unformed. A woman can endure and give birth to a healthy child with a probability of 30-50%. Contact our doctors at any time of the day - they will remotely answer all your questions and give recommendations.
Pregnancy after hydatidiform mole
When removing a hydatidiform drift, sparing methods and techniques are used, which allows preserving fertility. But with oncology, the detection of metastases, the prognosis is less favorable.
Important! In 80% of cases, after a mole, spontaneous remission occurs, additional therapy is not required.
FAQ
Is it possible to keep a pregnancy with a hydatidiform mole?
+
No, hydatidiform mole often causes spontaneous miscarriage. With a complete partial drift, the embryo dies at the stage of fertilization of the egg, with a partial one - up to 20 weeks. In rare cases, exceptions are observed in multiple pregnancies, when one of the embryos survives.
How to recognize a molar pregnancy?
+
The main symptoms of cystic drift include bloody uterine discharge. With bubble pregnancy, the size of the uterus exceeds the norm, which is manifested in a noticeable increase in the volume of the abdomen. Additional signs include pronounced early toxicosis with frequent vomiting, weakness, dizziness.
Is it possible to get pregnant immediately after a hydatidiform mole?
+
Conception can occur after the restoration of the monthly cycle if the dominant follicle matures.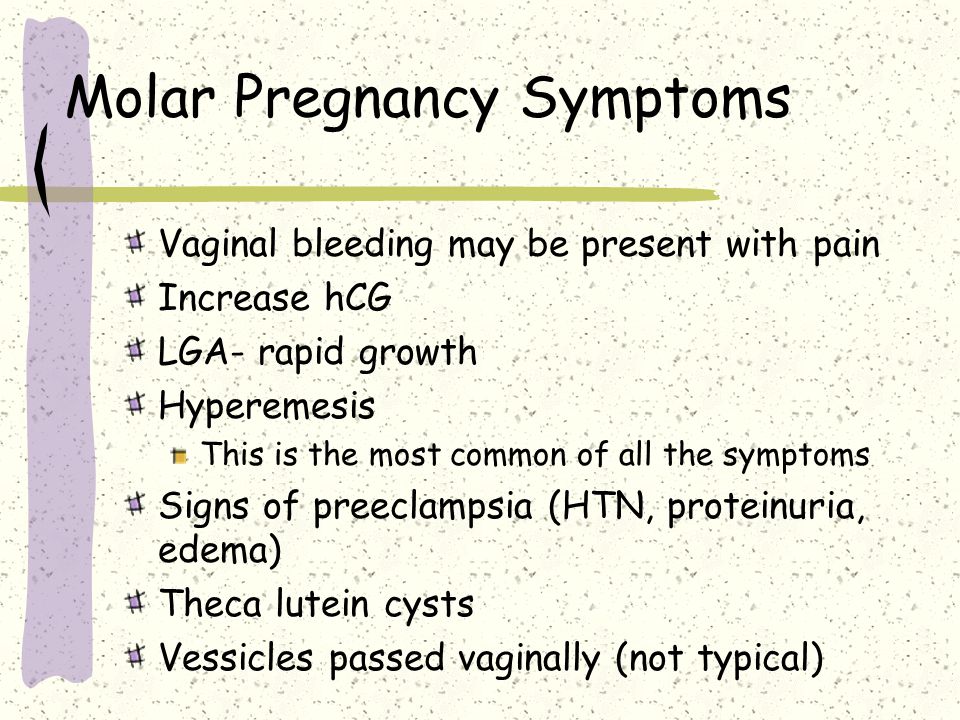 But after removal of the hydatidiform drift, it is necessary to use contraceptives for at least a year, until the level of hCG reaches normal levels.
But after removal of the hydatidiform drift, it is necessary to use contraceptives for at least a year, until the level of hCG reaches normal levels.
How to avoid recurrence of hydatidiform mole?
+
Since the exact causes of hydatidiform drift have not been established, the main and simple method of prevention is regular visits to the doctor for 1-1.5 years. To avoid conception, restore hormonal balance, the doctor will select hormonal contraceptives. With a negative Rh factor, immunoglobulin therapy is performed. Additionally, you need to take vitamin A - a deficiency of this substance is a risk factor for the development of gestational trophoblastic disease.
Expert opinion
After elimination of the hydatidiform drift without the use of chemotherapy, conception can be planned only after a year. After chemotherapy - after 24 months. First you need to check the level of hCG.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience.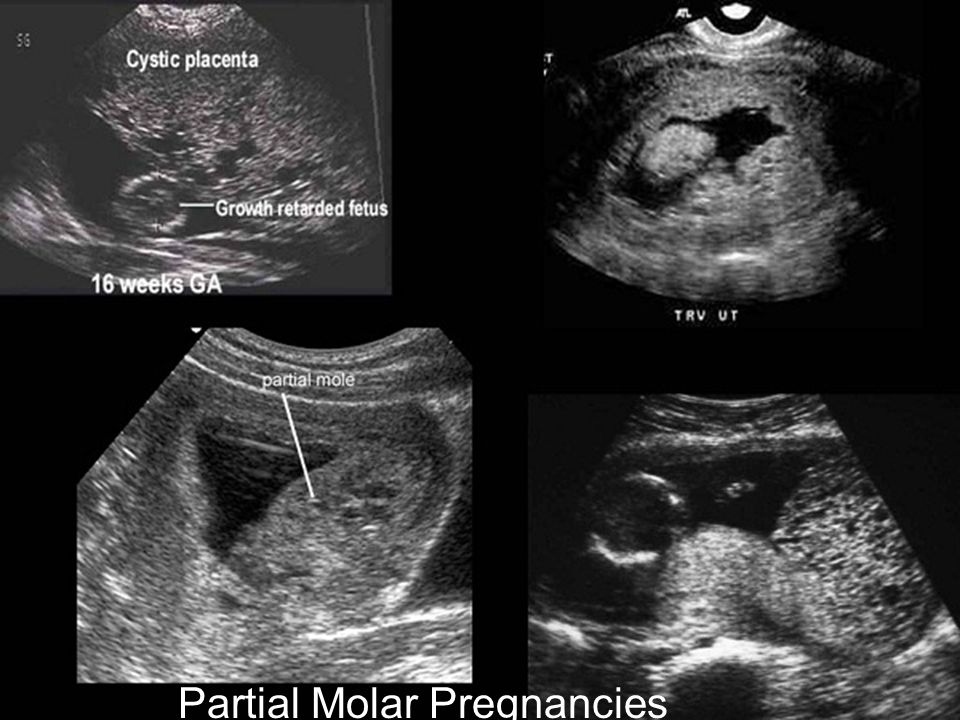
 With a full form, they are increased by 2 or more times, with a partial form, they are reduced or correspond to the gestational age.
With a full form, they are increased by 2 or more times, with a partial form, they are reduced or correspond to the gestational age.