First aid children
First Aid Guide for Parents & Caregivers
Log in | Register
Safety & Prevention
Safety & Prevention
Listen
Español
Text Size
General Tips
- Know how to get help.
- Make sure the area is safe for you and the child.
- When possible, personal protective equipment (such as gloves) should be used.
- Position the child appropriately if her airway needs to be opened or CPR (cardiopulmonary resuscitation) is needed.
- DO NOT MOVE A CHILD WHO MAY HAVE A NECK OR BACK INJURY (from a fall, motor vehicle crash, or other injury or if the child says his neck or back hurts) unless he is in danger.
- Look for anything (such as emergency medical identification jewelry or paperwork) that may give you information about health problems.
Stings, Bites & Allergies
- Stinging Insects: Remove the stinger as soon as possible with a scraping motion using a firm item (such as the edge of a credit card). Put a cold compress on the bite to relieve the pain. If trouble breathing; fainting; swelling of lips, face, or throat; or hives over the entire body occurs, call 911 or your local emergency number right away. For hives in a small area, nausea, or vomiting, call the pediatrician. For spider bites, call the pediatrician or Poison Help (1-800-222-1222). Have the pediatrician check any bites that become red, warm, swollen, or painful.
- Animal or Human Bites: Wash the wound well with soap and water. Call the pediatrician. The child may need a tetanus or rabies shot or antibiotics.
- Ticks: Use tweezers or your fingers to grasp as close as possible to the head of the tick and briskly pull the tick away from where it is attached. Call the pediatrician if the child develops symptoms such as a rash or fever.

- Snake Bites: Take the child to an emergency department if you are unsure of the type of snake or if you are concerned that the snake may be poisonous. Keep the child at rest. Do not apply ice. Loosely splint the injured area and keep it at rest, positioned at or slightly below the level of the heart. Identify the snake if you can do so safely. If you are not able to identify the snake but are able to kill it safely, take it with you to the emergency department for identification.
- Allergy: Swelling, problems breathing, and paleness may be signs of severe allergy. Call 911 or your local emergency number right away. Some people may have emergency medicine for these times. If possible, ask about emergency medicine they may have and help them administer it if necessary.
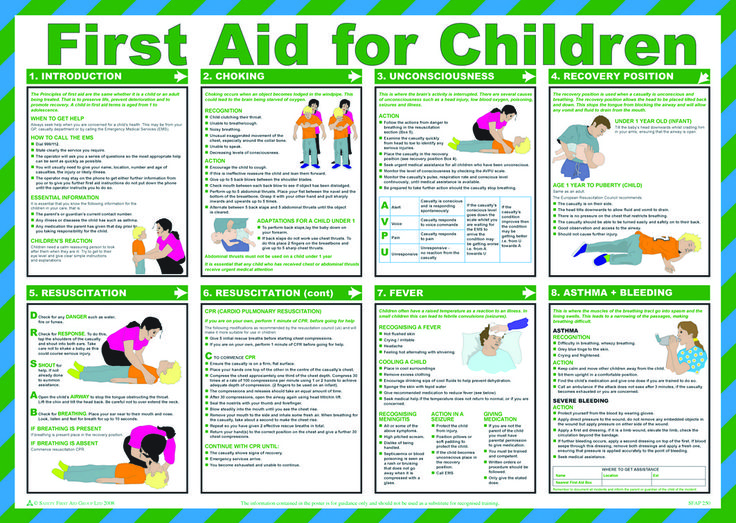
Fever
Fever in children is usually caused by infection. It also can be caused by chemicals, poisons, medicines, an environment that is too hot, or an extreme level of overactivity.
Take the child's temperature to see if he has a fever. Most pediatricians consider any thermometer reading 100.4°F (38°C) or higher as a fever. However, the way the child looks and acts is more important than how high the child's temperature is.
Call the pediatrician right away if the child has a fever and:
- Appears very ill, is unusually drowsy, or is very fussy
- Has other symptoms such as a stiff neck, a severe headache, severe sore throat, severe ear pain, an unexplained rash, repeated vomiting or diarrhea, or difficulty breathing
- Has a condition causing immune suppression (such as sickle cell disease, cancer, or chronic steroid use)
- Has had a first seizure but is no longer seizing
- Is younger than 3 months (12 weeks) and has a temperature of 100.4°F (38°C) or higher
- Has been in a very hot place, such as an overheated car
To make the child more comfortable, dress him in light clothing, give him cool liquids to drink, and keep him calm. The pediatrician may recommend fever medicines. Do NOT use aspirin to treat a child's fever. Aspirin has been linked with Reye syndrome, a serious disease that affects the liver and brain.
The pediatrician may recommend fever medicines. Do NOT use aspirin to treat a child's fever. Aspirin has been linked with Reye syndrome, a serious disease that affects the liver and brain.
Skin Wounds
Make sure the child is up to date for tetanus vaccination. Any open wound may need a tetanus booster even when the child is currently immunized. If the child has an open wound, ask the pediatrician if the child needs a tetanus booster.
- Bruises: Apply cool compresses. Call the pediatrician if the child has a crush injury, large bruises, continued pain, or swelling. The pediatrician may recommend acetaminophen for pain.
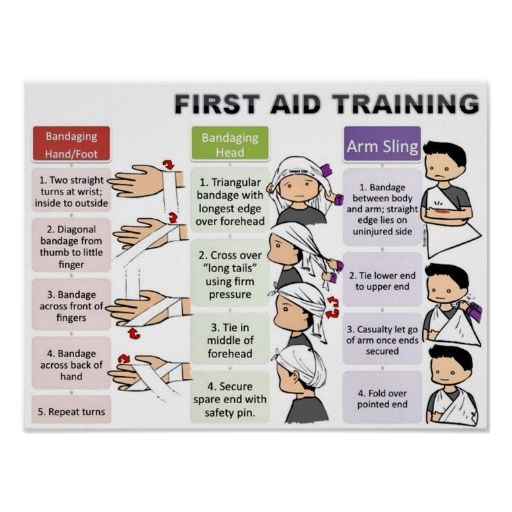
- Cuts: Rinse small cuts with water until clean. Use direct pressure with a clean cloth to stop bleeding and hold in place for 1 to 2 minutes. If the cut is not deep, apply an antibiotic ointment; then cover the cut with a clean bandage. Call the pediatrician or seek emergency care for large or deep cuts, or if the wound is wide open.
 For major bleeding, call for help (911 or your local emergency number). Continue direct pressure with a clean cloth until help arrives.
For major bleeding, call for help (911 or your local emergency number). Continue direct pressure with a clean cloth until help arrives. - Scrapes: Rinse with clean, running tap water for at least 5 minutes to remove dirt and germs. Do not use detergents, alcohol, or peroxide. Apply an antibiotic ointment and a bandage that will not stick to the wound.
- Splinters: Remove small splinters with tweezers; then wash until clean. If you cannot remove the splinter completely, call the pediatrician.
- Puncture Wounds: Do not remove large objects (such as a knife or stick) from a wound. Call for help (911 or your local emergency number). Such objects must be removed by a doctor. Call the pediatrician for all puncture wounds. The child may need a tetanus booster.
- Bleeding: Apply pressure with gauze over the bleeding area for 1 to 2 minutes. If still bleeding, add more gauze and apply pressure for another 5 minutes.
 You can also wrap an elastic bandage firmly over gauze and apply pressure. If bleeding continues, call for help (911 or your local emergency number).
You can also wrap an elastic bandage firmly over gauze and apply pressure. If bleeding continues, call for help (911 or your local emergency number).
Eye Injuries
If anything is splashed in the eye, flush gently with water for at least 15 minutes. Call Poison Help (1-800-222-1222) or the pediatrician for further advice. Any injured or painful eye should be seen by a doctor. Do NOT touch or rub an injured eye. Do NOT apply medicine. Do NOT remove objects stuck in the eye. Cover the painful or injured eye with a paper cup or eye shield until you can get medical help.
Fractures & Sprains
If an injured area is painful, swollen, or deformed, or if motion causes pain, wrap it in a towel or soft cloth and make a splint with cardboard or other firm material to hold the arm or leg in place. Do not try to straighten. Apply ice or a cool compress wrapped in thin cloth for not more than 20 minutes. Call the pediatrician or seek emergency care. If there is a break in the skin near the fracture or if you can see the bone, cover the area with a clean bandage, make a splint as described above, and seek emergency care.
If the foot or hand below the injured part is cold or discolored (blue or pale), seek emergency care right away.
Burns & Scalds
- General Treatment: First, stop the burning process by removing the child from contact with hot water or a hot object (for example, hot iron). If clothing is burning, smother flames. Remove clothing unless it is firmly stuck to the skin. Run cool water over burned skin until the pain stops. Do not apply ice, butter, grease, medicine, or ointment.
- Burns with Blisters: Do not break the blisters. Ask the pediatrician how to cover the burn. For burns on the face, hands, feet, or genitals, seek emergency care.
- Large or Deep Burns: Call 911 or your local emergency number. After stopping and cooling the burn, keep the child warm with a clean sheet covered with a blanket until help arrives.
- Electrical Burns: Disconnect electrical power. If the child is still in contact with an electrical source, do NOT touch the child with bare hands.
 Pull the child away from the power source with an object that does not conduct electricity (such as a wooden broom handle) only after the power is turned off. ALL electrical burns need to be seen by a doctor.
Pull the child away from the power source with an object that does not conduct electricity (such as a wooden broom handle) only after the power is turned off. ALL electrical burns need to be seen by a doctor.
Nosebleeds
Keep the child in a sitting position with the head tilted slightly forward. Apply firm, steady pressure to both nostrils by squeezing them between your thumb and index finger for 5 minutes. If bleeding continues or is very heavy, call the pediatrician or seek emergency care.
Teeth
- Baby Teeth: If knocked out or broken, apply clean gauze to control bleeding and call the pediatric or family dentist.
- Permanent Teeth: If knocked out, handle the tooth by the top and not the root (the part that would be in the gum). If dirty, rinse gently without scrubbing or touching the root. Do not use any cleansers. Use cold running water or milk. Place the tooth in egg white or coconut water or, if those are unavailable, milk, saline solution (1 teaspoon of table salt added to 8 ounces of water), or water, and transport the tooth with the child when seeking emergency care.
 If the tooth is broken, save the pieces in milk. Stop bleeding using gauze or a cotton ball in the tooth socket and have the child bite down. Call and go directly to the pediatric or family dentist or an emergency department.
If the tooth is broken, save the pieces in milk. Stop bleeding using gauze or a cotton ball in the tooth socket and have the child bite down. Call and go directly to the pediatric or family dentist or an emergency department.
Convulsions, Seizures
If the child is breathing, lay her on her side to prevent choking. Call 911 or your local emergency number for a prolonged seizure (more than 5 minutes).
Make sure the child is safe from objects that could injure her. Be sure to protect her head. Do not put anything in the child's mouth. Loosen any tight clothing. Start rescue breathing if the child is blue or not breathing.
Head Injuries
DO NOT MOVE A CHILD WHO MAY HAVE A SERIOUS HEAD, NECK, OR BACK INJURY. This may cause further harm.
Call 911 or your local emergency number right away if the child:
- Loses consciousness
- Has a seizure (convulsion)
- Experiences clumsiness or inability to move any body part
- Has oozing of blood or watery fluid from ears or nose
- Has abnormal speech or behavior
Call the pediatrician for a child with a head injury and any of the following symptoms:
- Drowsiness
- Difficulty being awakened
- Persistent headache or vomiting
For any questions about less serious injuries, call the pediatrician.
Poisons
If the child has been exposed to or ingested a poison, call Poison Help at 1-800-222-1222. A poison expert is available 24 hours a day, 7 days a week.
- Swallowed Poisons: Any nonfood substance is a potential poison. Do not give anything by mouth or induce vomiting. Call Poison Help right away. Do not delay calling, but try to have the substance label or name available when you call.
- Fumes, Gases, or Smoke: Get the child into fresh air and call 911, the fire department, or your local emergency number. If the child is not breathing, start CPR and continue until help arrives.
- Skin Exposure: If acids, lye, pesticides, chemicals, poisonous plants, or any potentially poisonous substance comes in contact with a child's skin, eyes, or hair, brush off any residual material while wearing rubber gloves, if possible. Remove contaminated clothing. Wash skin, eyes, or hair with a large amount of water or mild soap and water.
 Do not scrub. Call Poison Help for further advice.
Do not scrub. Call Poison Help for further advice.
If a child is unconscious, becoming drowsy, having convulsions, or having trouble breathing, call 911 or your local emergency number. Bring the poisonous substance (safely contained) with you to the hospital.
Fainting
Check the child's airway and breathing. If necessary, call 911 and begin rescue breathing and CPR.
If vomiting has occurred, turn the child onto one side to prevent choking. Elevate the feet above the level of the heart (about 12 inches).
Learn & Practice CPR
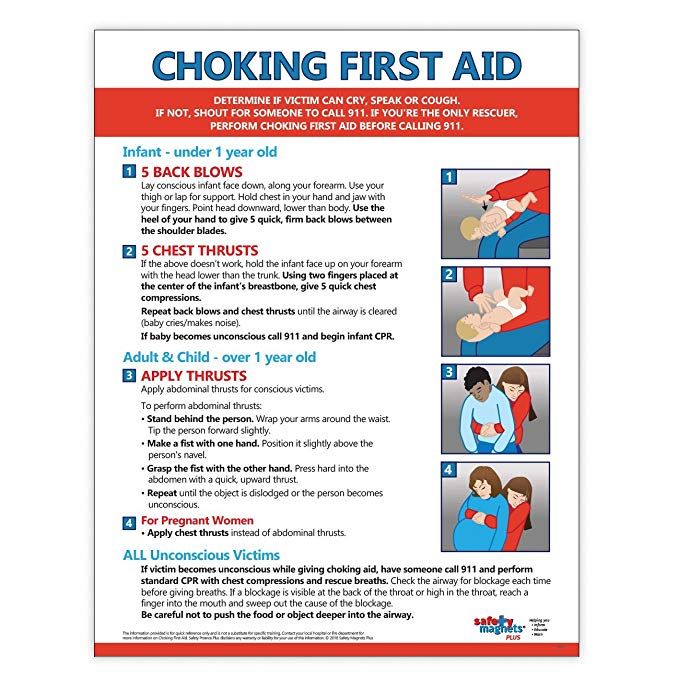
If alone with a child who is choking:
- SHOUT FOR HELP.
- START RESCUE EFFORTS.
- CALL 911 OR YOUR LOCAL EMERGENCY NUMBER.
Start first aid for choking If:
- The child cannot breathe at all (the chest is not moving up and down).
- The child cannot cough or talk or looks blue.
- The child is found unconscious/unresponsive.
Do not start first aid for choking if:
- The child can breathe, cry, or talk.
- The child can cough, sputter, or move air at all. The child's normal reflexes are working to clear the airway.
For Infants Younger than 1 Year:
- Infant Choking: If the infant is choking and is unable to breathe, cough, cry, or speak, follow these steps. Have someone call 911.
- GIVE 5 BACK BLOWS (SLAPS).
- ALTERNATING WITH
- GIVE 5 CHEST COMPRESSIONS.
- Alternate back blows (slaps) and chest compressions until the object is dislodged or the infant becomes unconscious/unresponsive. If the infant becomes unconscious/unresponsive, begin CPR.
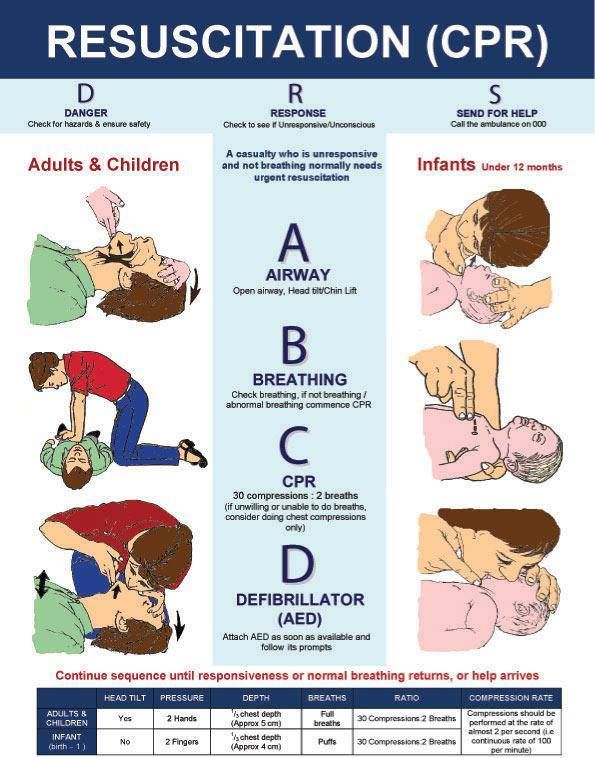
- Infant CPR: To be used when the child is UNCONSCIOUS/UNRESPONSIVE or when breathing stops. Place child on flat, hard surface.
- START CHEST COMPRESSIONS.
- Place 2 fingers of 1 hand on the breastbone just below the nippleline.
- Compress chest at least 1/3 the depth of the chest, or about 4cm (1.5inches).
- After each compression, allow chest to return to normal position.
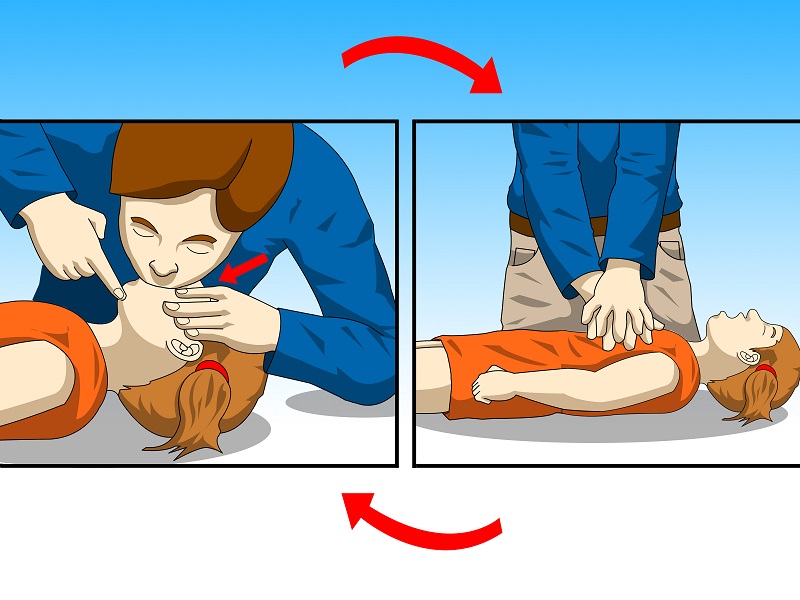 Compress chest at rate of at least 100 times per minute.
Compress chest at rate of at least 100 times per minute. - Do 30 compressions.
- OPEN AIRWAY.
- Open airway (head tilt–chin lift).
- If you see a foreign body, sweep it out with your finger. Do NOT do blind finger sweeps.
- START RESCUE BREATHING.
- Take a normal breath.
- Cover infant's mouth and nose with your mouth.
- Give 2 breaths, each for 1 second. Each breath should make the chest rise.
- RESUME CHEST COMPRESSIONS.
- Continue with cycles of 30 compressions to 2 breaths.
- After 5 cycles of compressions and breaths (about 2minutes) and if no one has called 911 or your local emergency number, call it yourself.
For Children 1 to 8 Years of Age:
Child choking (Heimlich Maneuver): Have someone call 911. If the child is choking and is unable to breathe, cough, cry, or speak, follow these steps.
- Perform Heimlich maneuver.
- Place hand, made into a fist, and cover with other hand just above the navel.
 Place well below the bottom tip of the breastbone and rib cage.
Place well below the bottom tip of the breastbone and rib cage. - Give each thrust with enough force to produce an artificial cough designed to relieve airway obstruction.
- Perform Heimlich maneuver until the object is expelled or the child becomes unconscious/unresponsive.
- If the child becomes UNCONSCIOUS/UNRESPONSIVE, begin CPR.
Child CPR: To be used when the infant is UNCONSCIOUS/UNRESPONSIVE or when breathing stops. Place infant on flat, hard surface.
- START CHEST COMPRESSIONS.
- Place the heel of 1 or 2 hands over the lower half of the sternum.
- Compress chest at least 1/3 the depth of the chest, or about 5 cm (2 inches).
- After each compression, allow chest to return to normal position. Compress chest at rate of at least 100 to 120 times per minute.
- Do 30 compressions.
- OPEN AIRWAY.
- Open airway (head tilt–chin lift).
- If you see a foreign body, sweep it out with your finger.
 Do NOT do blind finger sweeps.
Do NOT do blind finger sweeps. - START RESCUE BREATHING.
- Take a normal breath.
- Pinch the child's nose closed, and cover child's mouth with your mouth.
- Give 2 breaths, each for 1 second. Each breath should make the chest rise.
- RESUME CHEST COMPRESSIONS.
- Continue with cycles of 30 compressions to 2breaths until the object is expelled.
- After 5 cycles of compressions and breaths (about 2 minutes) and if no one has called 911 or your local emergency number, call it yourself.
If at any time an object is coughed up or the infant/child starts to breathe, stop rescue breaths and call 911 or your local emergency number.
Ask your pediatrician for information on choking/CPR instructions for children older than 8 years and for information on an approved first aid or CPR course in your community.
Additional Information from HealthyChildren.org:
10 Things for Parents to Know Before Heading to the ER
Cuts, Scrapes & Scar Management: Parent FAQs
When to Call Emergency Medical Services (EMS)
Dental Emergencies: What Parents Need to Know
- Last Updated
- 1/5/2017
- Source
- First Aid (Copyright © 2016 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
How to Perform Child & Baby First Aid
Your browser's Javascript functionality is turned off. Please turn it on so that you can experience the full capabilities of this site.
-
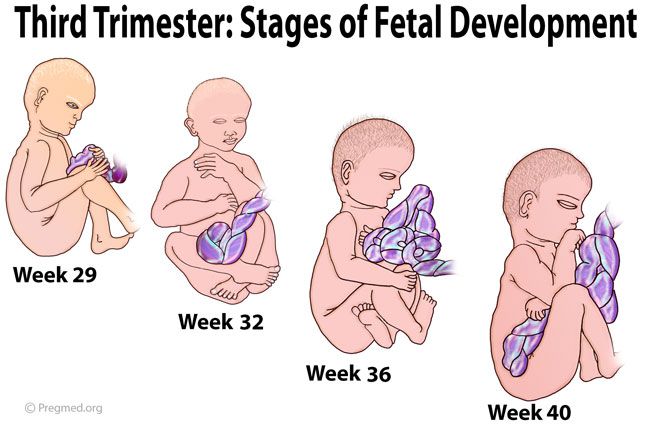
When a child or baby is experiencing an emergency, it's important to provide care and seek help as quickly as possible. But because their bodies are still forming, more delicate, and more compact than an adult's, delivering child or baby first aid is different than administering care to an adult. In order to help you provide the right type of care, we've created a step-by-step guide that you can print up and place on your refrigerator, in your car, in your child's nursery, in your bag or at your desk.
Before Giving Child or Baby First Aid1
Check the scene for safety, form an initial impression, obtain consent from the parent or guardian, and use personal protective equipment (PPE)
Giving First Aid1
If the child or baby appears unresponsive, check the child or baby for responsiveness (shout-tap-shout)
- For a child, shout to get the child’s attention, using the child’s name if you know it.
 If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition - For a baby, shout to get the baby’s attention, using the baby’s name if you know it. If the baby does not respond, tap the bottom of the baby’s foot and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
- CHECK for no more than 10 seconds
2
If the child or baby does not respond, responds but is not fully awake, is not breathing or is only gasping, or has life-threatening bleeding or another obvious life-threatening condition, immediately call 9-1-1 and give care based on the condition found and your level of training
- If the child or baby does not respond and is not breathing or only gasping, immediately begin CPR, starting with compressions.
 Continue giving sets of 30 chest compressions and 2 breaths until:
Continue giving sets of 30 chest compressions and 2 breaths until:
- You notice an obvious sign of life
- An AED is ready to use
- Another trained responder is available to take over compressions
- EMS personnel arrive and begin their care
- You are alone and too tired to continue
- The scene becomes unsafe
- You have performed approximately 2 minutes of CPR (5 sets of 30:2), you are alone and caring for baby, and you need to call 9-1-1
3
If the child or baby is responsive or responds to stimulation and is fully awake and does not appear to have a life-threatening condition:
- Interview the child, parent or guardian
- Do a focused check based on what the child, parent or guardian told you, how the child or baby is acting and what you see
- Call 9-1-1 if needed, and give care based on the condition found and your level of training
Of course, the key to providing care when it's needed most is to prepare for the unexpected.
 Find out how to get First Aid certified in first aid, CPR and AED use from the American Red Cross, or take a refresher course and renew your current first aid certificate.
Find out how to get First Aid certified in first aid, CPR and AED use from the American Red Cross, or take a refresher course and renew your current first aid certificate. - For a child, shout to get the child’s attention, using the child’s name if you know it.
Basic First Aid for Children (for the public)
Parents cannot always be with their child and protect him from any danger, but it is in our power to teach children to help themselves in a dangerous situation. No matter how small and defenseless they may seem to us, it's time to teach them some first aid rules.
No matter how old your child is, teach him what to do in an emergency so he can save his life.
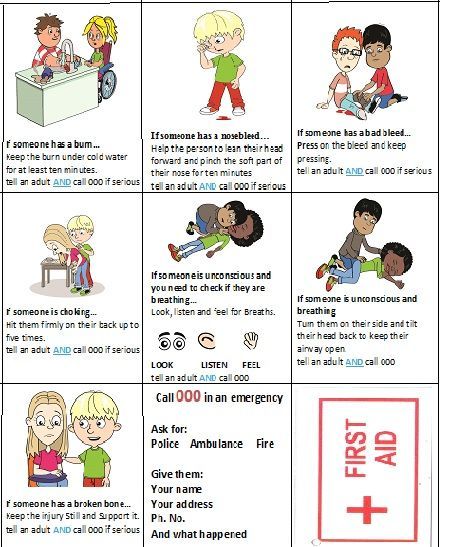
Teach them the main emergency numbers
It is important to teach children the emergency numbers, but it is even more important to teach them when to call them and what information to give. Put the EMERCOM phone on the speed dial list on your home phone (and mark it with a bright color, for example, using nail polish), and also do some exercises with the children.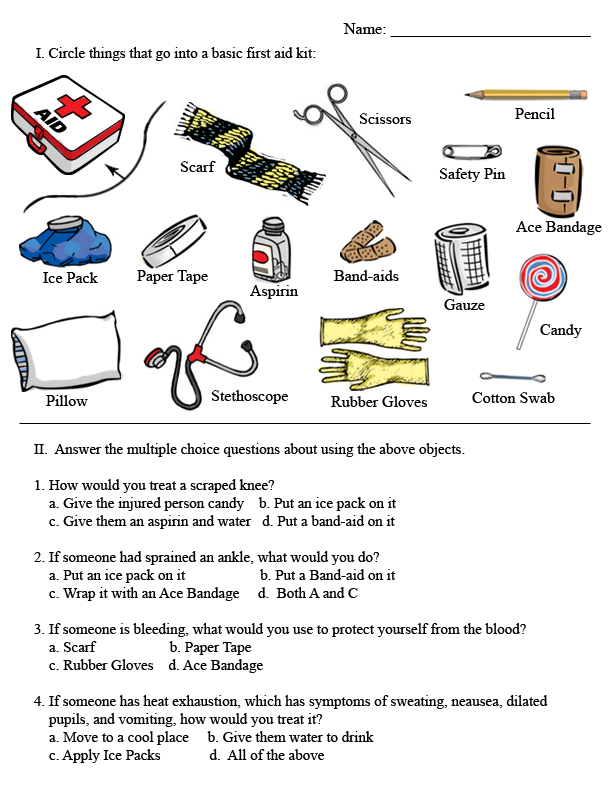 Have them "call" the various emergency services and tell them what happened. We recommend training once every six months so that the skill becomes automatic: unfortunately, many children and adults in a critical situation cannot get help in time, as they get lost and sometimes even forget their own address. nine0003
Have them "call" the various emergency services and tell them what happened. We recommend training once every six months so that the skill becomes automatic: unfortunately, many children and adults in a critical situation cannot get help in time, as they get lost and sometimes even forget their own address. nine0003
Teach how to stop bleeding
Most bleeding can be stopped by simply pressing or pulling hard on the pulse area. Teach the children that if he or someone nearby bleeds heavily, it is worth pulling a part of the body below the wound with a T-shirt or scarf, and also be sure to attach a piece of paper to the bandage indicating the time when the bandage was applied. And, of course, seek help immediately.
Teach CPR
If your child is 10 years old or older, he or she should already be strong enough to carry out an effective breathing action. If you don't know how to do artificial respiration yourself, maybe it's time to learn?
Teach what to do with a burn
The most important thing children should do about burns is that the first thing to do is to put the affected area under cold water, preferably running water.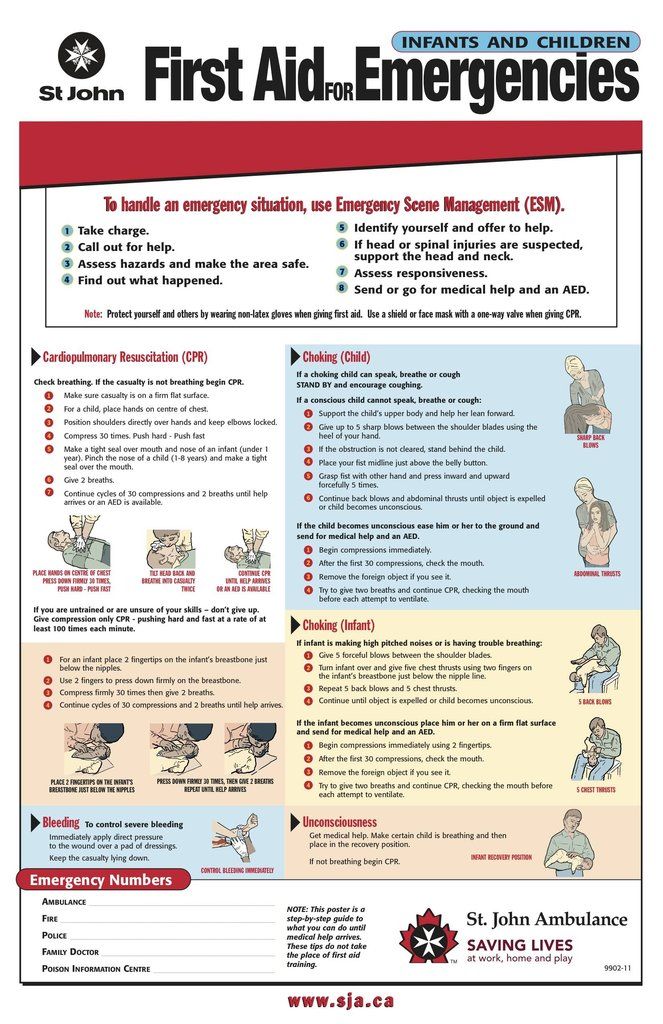 And in no case do not smear the burn with oil, cream or similar products that can increase the temperature of the skin. Cold water or ice - and adults for help! nine0003
And in no case do not smear the burn with oil, cream or similar products that can increase the temperature of the skin. Cold water or ice - and adults for help! nine0003
Teach what to do with eye injuries
The first rule: no matter what happens to the eyes, in no case should you rub them. It is best to close your eyes as tightly as possible: the accumulated tears will help to “wash out” any foreign object that has got into the eye. If this does not help, then you need to keep the injured eye closed and run for help.
Teach you what to do for a bee sting
Gently run your finger over the sting: bees usually leave a sting filled with venom. It must be urgently removed and immediately seek help. If your child is allergic to insect stings, teach them to take medicine, seek help from adults, and be sure to tell them about the allergy.
Teach what to do in case of sunstroke
If a person has been in the sun for a long time on a hot day and his breathing has noticeably quickened, his temperature has risen, and his skin has become very dry and hot, this means that sunstroke has occurred. Explain to the child that he needs help to move to a place where the direct rays of the sun do not fall, give him a drink of water and put a cloth moistened with cold water on his forehead. nine0003
Explain to the child that he needs help to move to a place where the direct rays of the sun do not fall, give him a drink of water and put a cloth moistened with cold water on his forehead. nine0003
Teach what to do if an animal bites
While playing with stray animals on the street, one wrong gesture and the child may not get off with an unfriendly hiss. Explain to your child that if he was bitten by a dog or cat, it is necessary to wash the wound with hydrogen peroxide, lubricate the edges with iodine and be sure to seek help from parents or immediately to the hospital.
Learn what to do when injured
During active play at home and outdoors, a dislocation, strain or even fracture can occur. It is necessary to immobilize the limb and, if possible, apply cold, and then be sure to call the parents. nine0003
Teach what to do with an abrasion
Even while walking, a child can get an abrasion.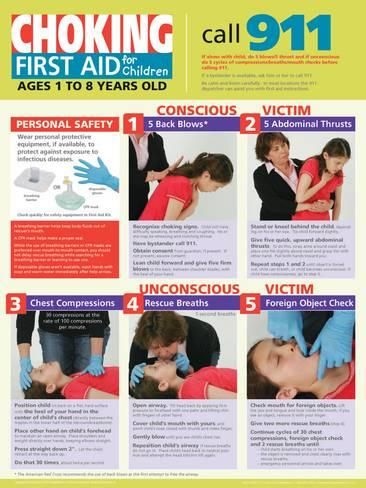 In this situation, it is necessary to moisten the napkin with water and rinse the wound with blotting movements. Treat the abrasion with hydrogen peroxide, grease the edges of the wound with brilliant green. Seal with bactericidal plaster.
In this situation, it is necessary to moisten the napkin with water and rinse the wound with blotting movements. Treat the abrasion with hydrogen peroxide, grease the edges of the wound with brilliant green. Seal with bactericidal plaster.
Teach how to deal with nosebleeds
A child may develop nosebleeds under various circumstances. At the sight of blood, fear overcomes adults, to say nothing of a child. It is important to explain to the baby that you need to raise your head to stop the bleeding. Then put a napkin soaked in cold water on the bridge of the nose. Remove frozen blood with a cotton swab dipped in hydrogen peroxide. nine0003
Learn what to do if you have frostbite
In winter, you also want to go for a walk, play snowballs and build a snowman. Having played, the children do not notice how they get frostbite. Awareness comes when the fingers no longer “obey”. Therefore, it is necessary to know the first actions in such a situation. It is necessary to warm the frostbitten part of the body, but only in warm, not hot water. Moisten with a blotting motion with any alcohol-containing solution. Put on a bandage and drink hot tea. nine0003
It is necessary to warm the frostbitten part of the body, but only in warm, not hot water. Moisten with a blotting motion with any alcohol-containing solution. Put on a bandage and drink hot tea. nine0003
Teach what to do if there is a splinter in the finger
For adults, a splinter in the finger is a common trifle. But the child may not cope and drive the splinter even deeper or bring an infection into the wound. In this case, accuracy is key. Tell them that you need to treat the tweezers with hydrogen peroxide and carefully remove the splinter (you need to pull the splinter out exactly at the angle at which it entered the wound).
These simple rules above are designed to make it as easy as possible for your baby to understand what to do at critical moments. Someday they can save a person's life and health. Teach your child these accessible things so that he knows how to behave competently in emergencies. But remember, if in an emergency you are not sure of the correctness and safety of your actions, then it is better not to do this. nine0003
nine0003
Emergency numbers for mobile and stationary phones
112 - Salvation Services
101 - Fire Guard 9000 9000 102 - Police 9000 9000 9000 103 - Sleeping Assistance 104 - GAS SERVICE 121, 123 - "CHILD IN DANGER" All mothers know for sure: something always happens to children! Either they fall into a puddle, or they stick their fingers into the socket. In order to be prepared for any emergency situations, we will describe all the necessary actions for the parent before the arrival of the ambulance team. After all, the main thing in this matter is not to harm, but to help. nine0003 The situation arises when the child is under the open sun for a long time without a hat. Due to a rush of blood to the brain, the following symptoms appear: In order to provide first aid, it is necessary to transfer the victim to the shade, open or remove clothes from him and lay him down in such a way that the head is higher than the body. The face, neck and chest of the child should be wiped with cold water. Also, for cooling, you need to put a cold wet towel on your forehead. Bring down the temperature with children's antipyretics. Give as much to drink as possible. nine0003 Damage to tissues under the influence of cold can occur not only in severe frosts, but even at a temperature of 0 - +3 degrees. This situation often occurs if the child walked in wet clothes or in strong winds. To provide first aid, it is necessary to maintain minus temperature on the surface of the damaged skin area. To do this, a heat-insulating bandage is applied, which includes 4 layers: bandage + cotton wool + oilcloth (or plastic bag) + scarf. The child must be given a warm drink, covered with a blanket on top. Attention! In no case should you rub the skin in the place of frostbite with snow or mittens. This will damage the skin and may result in infection. Also, you can not warm the frostbitten area with warm (and even more hot!) Water - serious consequences can occur. According to statistics, burns are considered the most common injuries in childhood. In the event of a burn, it is necessary to irrigate the affected area with cold water. These manipulations continue for 10-15 minutes. You should never treat a burn with iodine, potassium permanganate, oil. No "pissing" on damaged skin, no applying potatoes and other unthinkable methods! With an extensive burn, every second is important - we wrap the child in a clean, freshly ironed sheet, give him warm tea and take him to the clinic as soon as possible. nine0003 When receiving an electrical injury, the child must be immediately removed from the source of electricity. In case of respiratory arrest, a cardiac massage should be performed. To do this, press your hands on your chest 30 times, then exhale air into your mouth 2 times. Actions should be repeated until the ambulance arrives. nine0003 Even if a child who has received an electric shock does not complain about his health, he must be shown to a doctor in any case. The negative impact of current on the body may not appear immediately. Bruises are called damage to body tissues without violating the integrity of the skin. The main symptom of a bruise is a bruise or hematoma. After an injury, the child feels pain, swelling may occur. The main action of parents with bruises is to apply cold to the damaged area. Attention! With a strong blow, it is imperative to show the child to the doctor to exclude serious dislocations and fractures. In most cases, when sprained or torn, the ankle joint suffers. After the child twisted his foot, he feels a sharp pain. At this time, swelling appears on the outer surface of the joint. In case of sprain and rupture of the ligaments, it is necessary to apply cold to the damaged joint and fix it with an eight-shaped bandage. In order for the twisted leg not to cause a bone crack, it is recommended to show the child to the doctor. nine0003 This is one of the most dangerous injuries, requiring not only knowledge about immediate care, but also about subsequent rehabilitation. In the case of an open fracture, the first action of the parent is to stop the bleeding with a sterile bandage (we will discuss bleeding in more detail below). If the ends of the bones and fragments were found, in no case try to immerse them deep into the wound. Broken limbs must be immobilized with a splint made from improvised materials. These can be boards, sticks, pieces of cardboard, etc. In case of a broken arm, you can bandage it to the body. The broken leg can be gently bandaged to the uninjured leg. It is necessary to move the victim very carefully, without exposing additional injury. nine0003 If the spine is fractured, the child must be moved in a prone position. Sitting position is not allowed. Transportation takes place on a shield or a stretcher with a solid frame. If a fracture of the pelvic bones is suspected, the victim should be placed on a stretcher, placing a roller under his bent knees. Any, even the smallest, wounds are open gates for infection. Often, infection occurs as a result of improper care. nine0003 If a wound occurs, clean the damaged skin from dirt (we make movements from the edges of the wound to its outer part), cover with a sterile bandage. When providing assistance, do not examine the wound with your fingers, do not wash it with any liquids. When treating with brilliant green or iodine, make sure that the product does not get on the wound itself, only on its edges. If the applied bandage is saturated with blood, do not try to remove it, it is better to apply another additional layer of bandage on top. nine0003 The tactics of stopping bleeding depends on its type. So, with venous or capillary bleeding, the injured limb of the child should be raised and a pressure bandage applied to the wound. With arterial - a tourniquet will be required. In order to properly apply the tourniquet, it should be fixed on a soft lining (any fabric will do). It is necessary to record the time of applying the tourniquet and ensure that the duration of pulling in summer does not exceed 40 minutes, in winter - 20. To control the situation, do not cover the tourniquet with clothing. The main task of parents when a child receives a skull injury is to create complete rest. In the case of an open wound, a tight sterile bandage is applied. If vomiting occurs, care must be taken to ensure that the child does not choke on vomit. It is better to carry the victim to the doctor in your arms. nine0003 Attention! In case of any traumatic brain injury, the child must be shown to a pediatric neurologist without fail. Underestimating the severity of what happened can lead to serious consequences: headaches, memory impairment, fatigue, etc.0 9
First aid for childhood injuries
Sun or heat stroke

Frostbite
 nine0003
nine0003 Burn
Electric shock
 However, it should be understood that at this moment the victim himself becomes a current conductor, and he can only be touched with rubber gloves or standing on a rubber surface. Also, electrical wires can be thrown away from the child with a dry branch.
However, it should be understood that at this moment the victim himself becomes a current conductor, and he can only be touched with rubber gloves or standing on a rubber surface. Also, electrical wires can be thrown away from the child with a dry branch. Bruise
 Any frozen product from the freezer, pre-wrapped in a handkerchief or thin towel, will do. After 2-3 days, a warm heating pad is applied to the site of injury. In case of a bruise in the joint area, it is necessary to immobilize it. nine0003
Any frozen product from the freezer, pre-wrapped in a handkerchief or thin towel, will do. After 2-3 days, a warm heating pad is applied to the site of injury. In case of a bruise in the joint area, it is necessary to immobilize it. nine0003 Sprain or rupture of ligaments
Fracture
 Open fractures are considered the most dangerous, since there is a high risk of infection through damaged tissues.
Open fractures are considered the most dangerous, since there is a high risk of infection through damaged tissues. 
Wound
Bleeding
 When applying, it is necessary to monitor the bleeding: as soon as it has stopped, the tourniquet pressure must be left at this level. You don't need to! nine0003
When applying, it is necessary to monitor the bleeding: as soon as it has stopped, the tourniquet pressure must be left at this level. You don't need to! nine0003 Traumatic brain injury