2Nd trimester discharge
The Second Trimester of Pregnancy: Pain, Bleeding, and Discharge
Pain, bleeding, and discharge
Some pain or discomfort is normal during the second trimester of pregnancy. Spotting and very small amounts of blood may also be harmless. However, there are certain types of pain, bleeding, and vaginal discharge that you shouldn’t ignore.
Learn how to tell the difference between normal pregnancy problems and serious medical concerns.
Emergency medical symptoms during the second trimester
There are a number of situations during pregnancy that demand medical attention. If you experience the symptoms below, don’t hesitate to call your doctor or seek emergency care.
When to seek emergency medical attention
Always seek emergency care if you are experiencing the symptoms of a miscarriage. Symptoms of a miscarriage include:
- enough vaginal bleeding to soak more than one menstrual pad
- severe pain in the abdomen or pelvic region
- clots or clumps of tissue (typically gray or pink in color) passed from the vagina
If you pass clots or clumps from the vagina, try to save the tissue in a jar or plastic bag to give to the doctor for analysis. They may then determine the cause of the problem.
There are three types of miscarriage.
If a miscarriage has been threatened, there was bleeding before 20 weeks of pregnancy with no cervical dilation and no expulsion of any of the fetal parts.
If a miscarriage has been completed, there was complete expulsion of fetal parts from your body.
If a miscarriage has happened incompletely, there was partial expulsion of the fetal parts before 20 weeks. In the case of incomplete miscarriages, the next step may be to allow the remaining products of pregnancy to pass naturally or perform a dilation and curettage.
Note: If you have miscarried before and notice bleeding or cramping, you should seek emergency medical attention.
Always seek emergency care if you are experiencing the symptoms of an ectopic pregnancy (a pregnancy outside the uterus). Symptoms of an ectopic pregnancy include:
- cramps and colicky (spasmodic) pain with associated tenderness
- pain that starts on one side and spreads across the belly
- pain that worsens with taking a bowel movement or coughing
- light bleeding or spotting that is brown in color, is either constant or intermittent, and precedes the pain by weeks
- one of the above symptoms combined with nausea and vomiting, pain in the shoulder, weakness or lightheadedness, or rectal pressure
- rapid and weak pulse, clamminess, fainting, and sharp pain (these symptoms may arise if the ectopic pregnancy is in the fallopian tube and the tube ruptures, causing septic shock)
When to call your doctor
Emergency care isn’t always necessary. However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
- cramps and pain in the center of the abdomen with vaginal bleeding
- severe pain or pain that lasts for more than a day (even without bleeding)
- bleeding that is as heavy as a period
- spotting or staining that lasts for three days or longer
Pain
Although you may not experience an emergency, there will probably be times during your pregnancy when you’re uncomfortable or in pain. Many women have pain during the second trimester even when nothing is medically wrong.
Abdominal pain, back pain, headaches, leg cramps, and hand pain don’t always signal a problem. Learning to identify and relieve these normal discomforts will help you throughout your pregnancy.
Abdominal pain
Abdominal pain can either be a normal symptom of pregnancy or a sign of something serious, like preterm labor or ectopic pregnancy. It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
When you feel pain in your abdomen during the second trimester, it’s usually related to the tension on the ligaments and muscles in the pelvis. These get stretched as the uterus expands to hold the growing baby.
If you move quickly, you can “pull” a ligament or muscle. This may feel like a painful pang in your pelvis or a cramp down your side that can last for several minutes. This kind of pain isn’t harmful to you or your baby.
Sometimes abdominal pain is related to past pregnancies or surgeries. If you’ve had surgery for infertility or other types of abdominal surgery, you may experience pain from the pulling of the remnants of scar tissue (adhesions).
Pregnant women can also have the same types of abdominal infections that other women develop. Infections that can cause abdominal pain include:
- cholecystitis (inflamed gallbladder)
- appendicitis (inflamed appendix)
- hepatitis (inflamed liver)
- pyelonephritis (kidney infection)
- pneumonia (lung infection)
Sometimes these diseases are harder to diagnose during pregnancy because the location of pain characteristic to each has been shifted.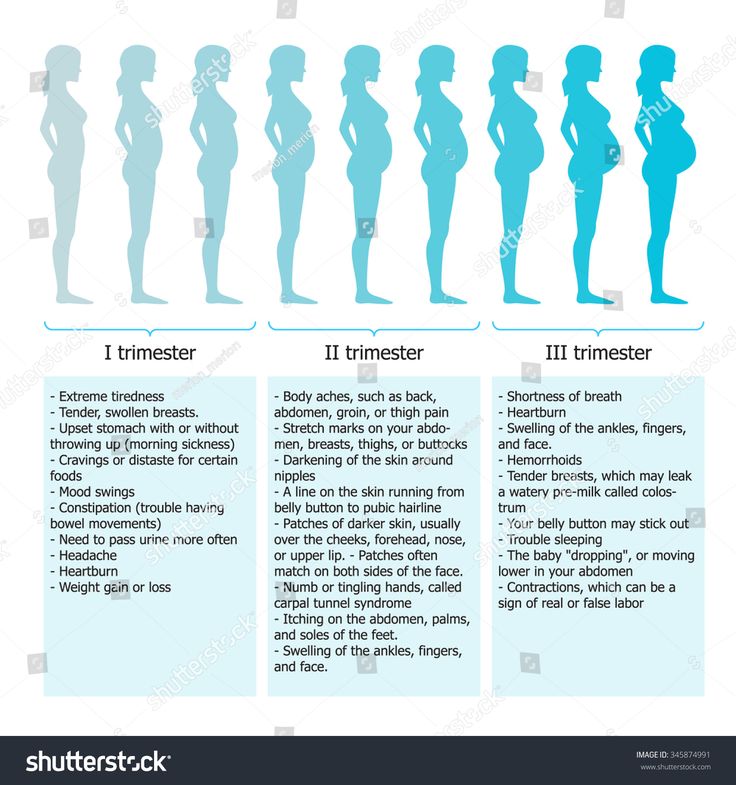 This happens when the growing uterus pushes nearby organs out of its way.
This happens when the growing uterus pushes nearby organs out of its way.
If you’re experiencing serious pain that doesn’t feel like it’s in your uterus, show or tell your doctor exactly where the pain is located. If you have one of the above infections, you may need antibiotics or surgery to fix the problem.
Warning: If you’re experiencing regular or painful contractions in the pelvis or abdomen, call a doctor immediately. These may be a sign of preterm labor.
Back pain
Back pain is very common during pregnancy. Pregnancy hormones cause the joints in the pelvis to become soft and lax in preparation for childbirth. As your uterus gets bigger in the second trimester, your center of gravity changes.
You begin to carry yourself differently to accommodate the weight. In addition, your abdominal muscles may separate as the uterus presses up against them, weakening the abdominal wall. All of these factors can contribute to back pain, strain, and discomfort.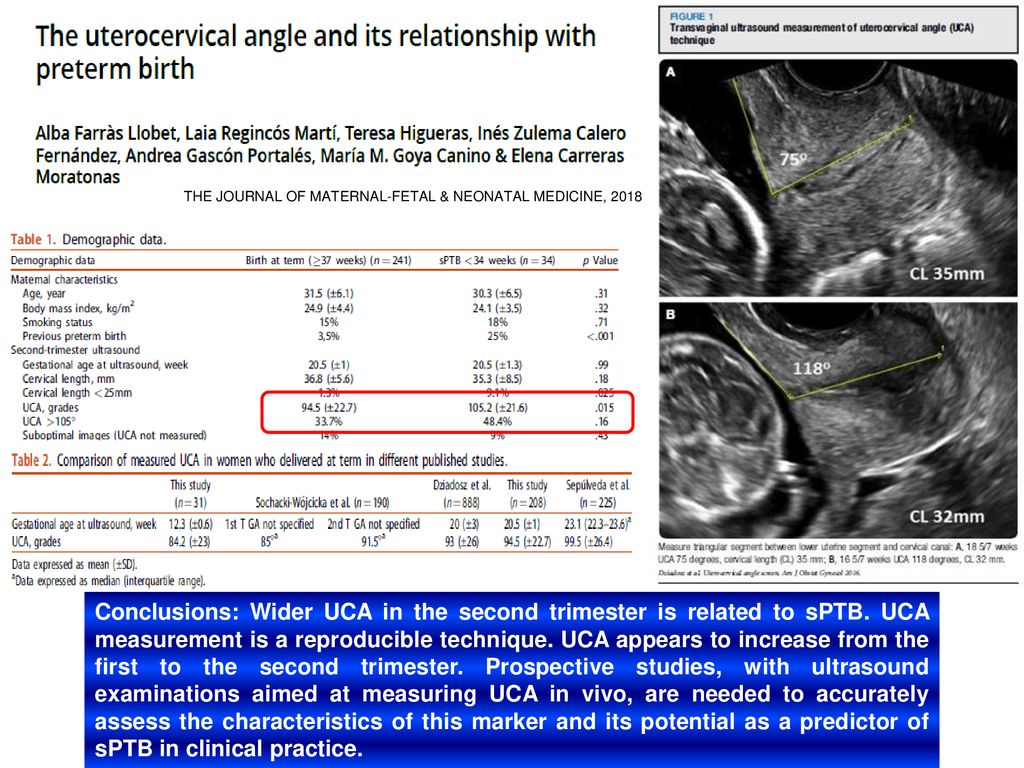
Here’s how you can improve back pain:
- Practice good posture while standing (shoulders back, pelvis in) and sitting (elevate feet slightly and try to avoid crossing your legs).
- Get up every once in a while when you’re sitting for long periods.
- Lift heavy objects by bending at the knees, rather than the waist.
- Try not to reach for things over your head.
- Sleep on your left side, bending at your hips and knees, and place a pillow between your legs to reduce pressure on your back.
- Strengthen your stomach muscles. One of the keys to a strong back is a strong abdomen.
- Talk to your doctor. You may need to use a back brace or some other form of support to relieve the pressure on your back.
Warning: If you’re experiencing lower back pain accompanied by painful urination, you may have a bladder or kidney infection. Low, dull, consistent back pain may be a sign of preterm labor. Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Headaches
Many women experience frequent headaches during pregnancy. You still may be experiencing headaches that started during the first trimester, or they may be just beginning now.
Hormonal changes, tension, fatigue, hunger, and stress are all culprits. Try to relax, stay rested, and eat regularly. You can also try to relieve headaches in the following ways:
- If you have a sinus headache, apply warm compresses to aches in the sinus areas of your head. These include both sides of the nose, the middle of the forehead, and the temples.
- If the headache is due to tension, try applying cold compresses to aches along the back of your neck.
- Learn relaxation exercises, like closing your eyes and imagining yourself in a peaceful place. Reducing stress is a key component of a healthy pregnancy.
 Consider calling a counselor or a therapist if needed.
Consider calling a counselor or a therapist if needed.
Speak with a physician before you begin using pain relievers. This is important even if you took over-the-counter medications for pain before you were pregnant.
Common headache medicines include ibuprofen (Motrin), aspirin (Bufferin), acetaminophen (Tylenol), and naproxen sodium (Aleve).
Acetaminophen is probably the safest option during pregnancy, but don’t take pills during pregnancy unless your doctor has specifically told you to do so.
Warning: Call your doctor if the headache is particularly severe or lasts for more than a few hours. Also note whether your headache comes with a fever, swelling in the face and hands, dizziness, nausea, or changes in vision. These may be signs of preeclampsia or another serious complication.
Leg cramps
Although no one knows exactly what causes them, leg cramps are common in the second and third trimester. Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
It may be that the uterus is pressing on the nerves that go to the legs. Regardless of the cause, you may wake up in the middle of the night with bothersome cramps.
You can avoid or get rid of cramps by:
- exercising your calves
- staying hydrated
- alternating between sitting and standing
- wearing support hose
- wearing comfortable, supportive shoes
- flexing the ankle and toes upward with a straightened knee to stop the cramping
- massaging or applying a warm compress to the leg that is cramping
- talking to your doctor about reducing the amount of phosphorous in your diet by cutting down on foods like milk or meat
- making sure you get enough calcium (by eating fortified cereal or spinach) and magnesium (by eating beans or semisweet chocolate)
Warning: Tell your doctor if the cramps feel particularly painful, fail to go away, cause swelling, feel warm to the touch, or change the skin color of your leg (to white, red, or blue). You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
Pain and numbness in the hand
Numbness and pain in the thumb, index finger, middle finger, and half of the ring finger can be a sign of carpal tunnel syndrome.
Usually this condition is diagnosed in people who regularly perform repetitive tasks such as typing or piano playing, but it’s also common in pregnant women.
During pregnancy, the tunnel that surrounds the nerve to these fingers can become swollen, causing tingling, numbness, and pain. In the evening, after your arm has been dangling by your side all day, your symptoms may worsen due to gravity.
Shaking out your arm when you experience the carpal tunnel symptoms may help. Alternatively, you may want to talk to your doctor about splinting your wrist or taking vitamin B-6.
Numbness and tingling in the hand can also be caused by poor posture. If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
Practice standing up straight with your head and spine erect. A supportive bra and proper bed rest are also important.
Bleeding
Bleeding can be a scary symptom during pregnancy. In some cases, bleeding can be harmless. It can happen when pregnancy hormones cause you to develop more sensitive, expanded blood vessels.
In other cases, bleeding can indicate a serious problem with the pregnancy. If you experience any bleeding, call a doctor for advice.
Vaginal bleeding
Light bleeding or spotting (which can be brown, pink, or red) during the second and third trimester isn’t usually cause for concern. It typically occurs as a result of interference with the cervix during sex or a vaginal exam.
Pink mucus or brownish discharge may both occur during the second trimester. It’s caused by small amounts of blood leaving your body with normal discharge.
Vaginal bleeding that’s like a period, however, can be a worrisome sign that needs immediate medical attention. Clots of blood or clumps of tissue in the blood may be symptoms of a miscarriage.
For this reason, you should never be the judge of what is normal or abnormal bleeding. Instead, call your doctor.
If the bleeding is heavy or if it’s accompanied by pain, call your doctor immediately. If it’s spotty, you can make the call sometime that day. Serious bleeding is most commonly caused by placenta previa, premature labor, or late miscarriage.
Rectal bleeding and hemorrhoids
Rectal bleeding isn’t as worrisome as vaginal bleeding and is generally a sign of either hemorrhoids or anal fissure. Rectal bleeding could also be a sign of something more serious. You should speak with your doctor if you’re experiencing this symptom.
Rectal bleeding may mean you have hemorrhoids, either external or, less commonly, internal. Hemorrhoids occur in up to half of all pregnant women.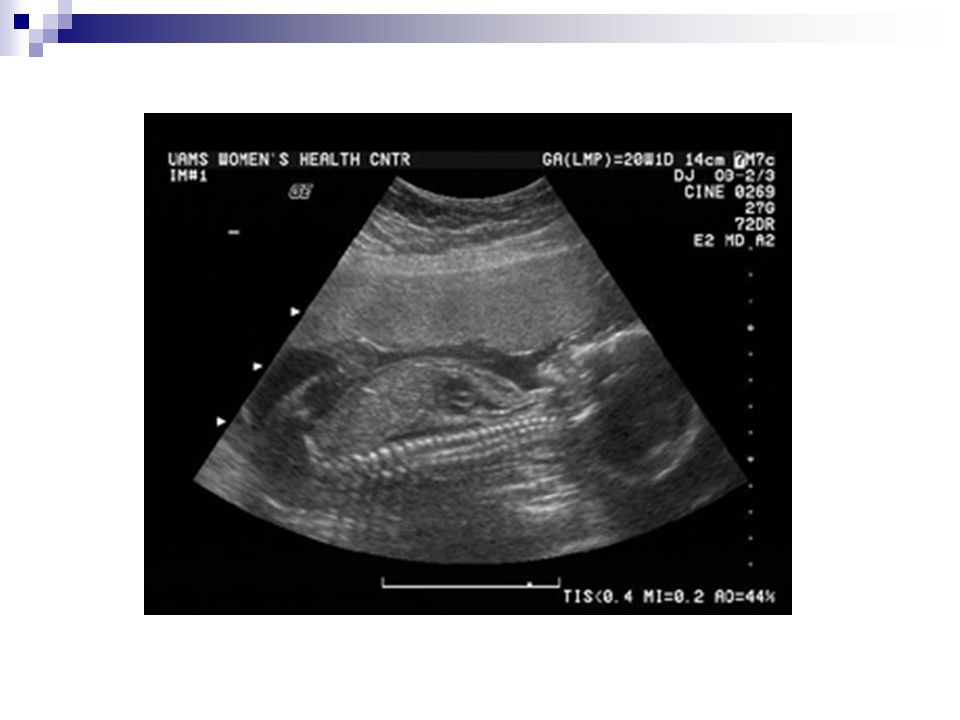 They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
Hemorrhoids are caused by progesterone acting on the walls of the rectal veins, causing them to relax and expand. As you advance in your pregnancy and the uterus presses on these veins, blood flow slows down and the veins dilate even more.
Squeezing and constipation can make hemorrhoids worse. Laughing, coughing, straining, and going to the bathroom may cause hemorrhoids to bleed.
If rectal bleeding isn’t caused by hemorrhoids, it may be caused by an anal fissure — a crack in the skin that lines the anal canal. Anal fissures are usually caused by constipation. Fissures are very painful, particularly during the strain of taking a bowel movement.
Hemorrhoids and anal fissures can cause brown, pink, or red bloodstains to appear on your underwear or toilet paper. If the bleeding is heavy or continuous, call a doctor for advice.
If you’re diagnosed with hemorrhoids or an anal fissure, you should do the following:
- Try to avoid constipation by remaining well hydrated and eating a diet high in fiber.
- Try to alleviate pressure on the veins in the rectum by sleeping on your side, not standing or sitting for long periods of time, and not taking too long or straining when going to the bathroom.
- Take warm sitz baths up to two times a day. Sitz baths are basins that fit on your toilet and are filled with warm water in which you can soak your anus.
- Soothe the hemorrhoids with ice packs or witch hazel, and only use topical medications if your doctor prescribes them. Your doctor may also prescribe stool softeners or a laxative.
- Practice good hygiene by wiping thoroughly after bowel movements (from front to back) and keeping yourself clean.
- Use only white, unscented toilet paper.
- Perform Kegel exercises to improve the circulation to the area.
Warning: Massive rectal bleeding can be a serious problem. It can be caused by ectopic pregnancies or serious internal problems. Seek medical care immediately if you’re bleeding heavily from the anus.
Nosebleeds and nasal congestion
Like many of the complaints of pregnancy, nasal stuffiness and nosebleeds are believed to be due in large part to estrogen and progesterone. These hormones cause increased blood flow and swelling of the blood vessels in the mucus membranes.
Particularly in cold, dry weather, this can mean that you feel more congested than normal. You may also experience nosebleeds more often than you did before getting pregnant.
You may want to try the following to ease your nasal symptoms:
- Use a humidifier to help with the dryness that can make symptoms worse.
- Blow your nose gently by closing one nostril while you blow through the other.
- Curb nosebleeds by leaning forward and applying gentle pressure to the nose. Try squeezing it with the thumb and forefinger for five minutes. Repeat if necessary.
- Call your doctor if the bleeding doesn’t stop, or is heavy or frequent.
- Seek emergency medical care if nasal congestion makes it hard to breathe.
The same changes in hormones and blood vessels that cause nasal bleeding can cause sensitive gums. If you experience bleeding when flossing or brushing your teeth, try using a softer toothbrush.
Visit a dentist if you bleed a lot or have a lot of pain when flossing or brushing your teeth. Serious dental problems can be a sign of other health concerns that can complicate pregnancy.
Discharge
Many women experience different types of discharge during the second trimester. Pay attention to the color, smell, amount, and frequency of vaginal or anal discharge. Some types of discharge may indicate an infection that needs medical attention or treatment.
Vaginal discharge
As the pregnancy progresses, you may notice increasing vaginal discharge. Typically, it looks like egg whites and is milky and a bit odorous. It may remind you of premenstrual discharge, only a bit heavier and more frequent.
This discharge is totally normal and is just another change your body goes through in response to the pregnancy hormones and the increased blood flow to the area. You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
Though the kind of discharge described above is normal, there are some types of discharge that may mean you have an infection.
Vulvovaginal candidiasis, or yeast infection, is very common during pregnancy. Signs include a thick, cottage cheese-like discharge accompanied by itching, redness, and burning, as well as painful intercourse and urination.
Sexually transmitted infections (STIs) may also occur during pregnancy, and because many of them can affect the fetus, it’s important that they be treated.
You may have a condition that requires treatment if any of the following is true:
- The discharge looks like pus.
- The discharge is yellow, green, or has a foul odor.
- You notice a burning sensation when you urinate.
- Your labia are red, swollen, or itchy.
Unlike signs of infection, clear or pinkish watery discharge may be a sign of premature rupture of the amniotic sac.
Rupture of the sac may cause a trickle of watery discharge or a rush of lots of watery fluid from the vagina. This is commonly known as having the water break before labor begins.
Warning: If you experience a steady trickle or a rush of watery discharge during the second trimester, call a doctor immediately. It may be a sign of premature labor or a tear in the amniotic sac.
Rectal discharge
In addition to bleeding from the rectum, some women may experience anal discharge during pregnancy. Rectal discharge may be caused by STIs, bowel and gastrointestinal problems, or physical wounds in the rectum. If you’re experiencing rectal discharge, consult a doctor.
Gonorrhea, chlamydia, and other infections that can be transmitted through sexual contact can cause an infection in the anus. These infections can cause lesions or sores that bleed.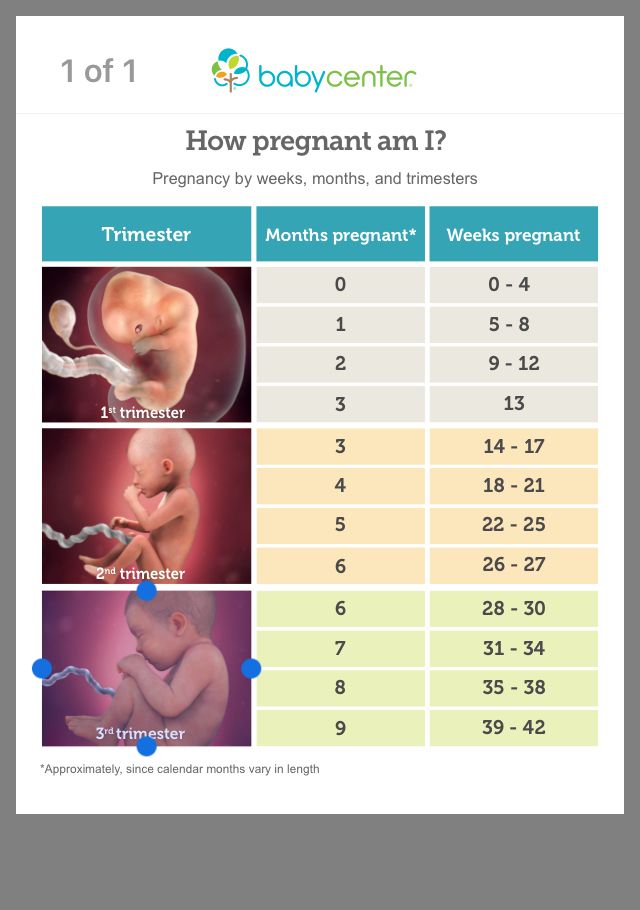 In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
It may be painful to wipe or go to the bathroom. If you have these symptoms, discuss them with a doctor. Left untreated, they may cause serious problems for the baby. Most STIs can be treated with antibiotics.
Some pregnant women may experience anal discharge due to bowel problems or gastrointestinal disorders. These may result in mucus or watery discharge from the anus.
Certain gastrointestinal problems or food poisoning may also cause frequent diarrhea or fecal matter with unusual colors or textures. Tell your doctor about any unusual characteristics of your bowel movements. Some conditions require immediate treatment.
Finally, if you have a hemorrhoid or anal fissure that has become infected, you may notice unusual rectal discharge. Infected wounds may cause brown, yellow, green, or white discharge.
Such a wound may or may not have a foul smell. Infected sores are often very painful and require medical attention. Consult a doctor for treatment if you experience anal discharge of this nature.
Consult a doctor for treatment if you experience anal discharge of this nature.
Nipple discharge
Many women experience discharge from one or both nipples during the second trimester of pregnancy. Breast tenderness and changes in nipple color are also common during pregnancy.
Discharge is most common in women who have previously given birth. Nipple discharge is often clear, milky, or yellowish in color.
Discharge from the nipples is normally not a sign of a problem, unless the following symptoms are present:
- The nipple changes in size or becomes inverted.
- The nipple is dry, cracked, or painful.
- The nipple has a rash or new bumps.
- The discharge is foul-smelling, bloody, green, or brown.
If you aren’t sure whether your nipple discharge is normal, call a doctor to discuss your symptoms.
The Second Trimester of Pregnancy: Pain, Bleeding, and Discharge
Pain, bleeding, and discharge
Some pain or discomfort is normal during the second trimester of pregnancy.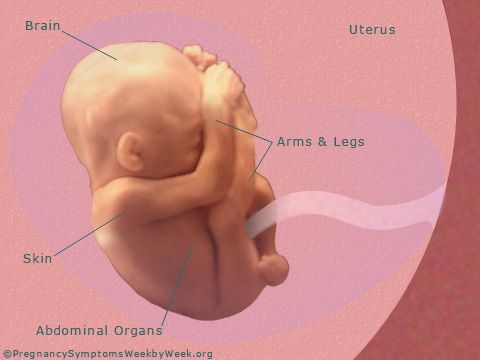 Spotting and very small amounts of blood may also be harmless. However, there are certain types of pain, bleeding, and vaginal discharge that you shouldn’t ignore.
Spotting and very small amounts of blood may also be harmless. However, there are certain types of pain, bleeding, and vaginal discharge that you shouldn’t ignore.
Learn how to tell the difference between normal pregnancy problems and serious medical concerns.
Emergency medical symptoms during the second trimester
There are a number of situations during pregnancy that demand medical attention. If you experience the symptoms below, don’t hesitate to call your doctor or seek emergency care.
When to seek emergency medical attention
Always seek emergency care if you are experiencing the symptoms of a miscarriage. Symptoms of a miscarriage include:
- enough vaginal bleeding to soak more than one menstrual pad
- severe pain in the abdomen or pelvic region
- clots or clumps of tissue (typically gray or pink in color) passed from the vagina
If you pass clots or clumps from the vagina, try to save the tissue in a jar or plastic bag to give to the doctor for analysis.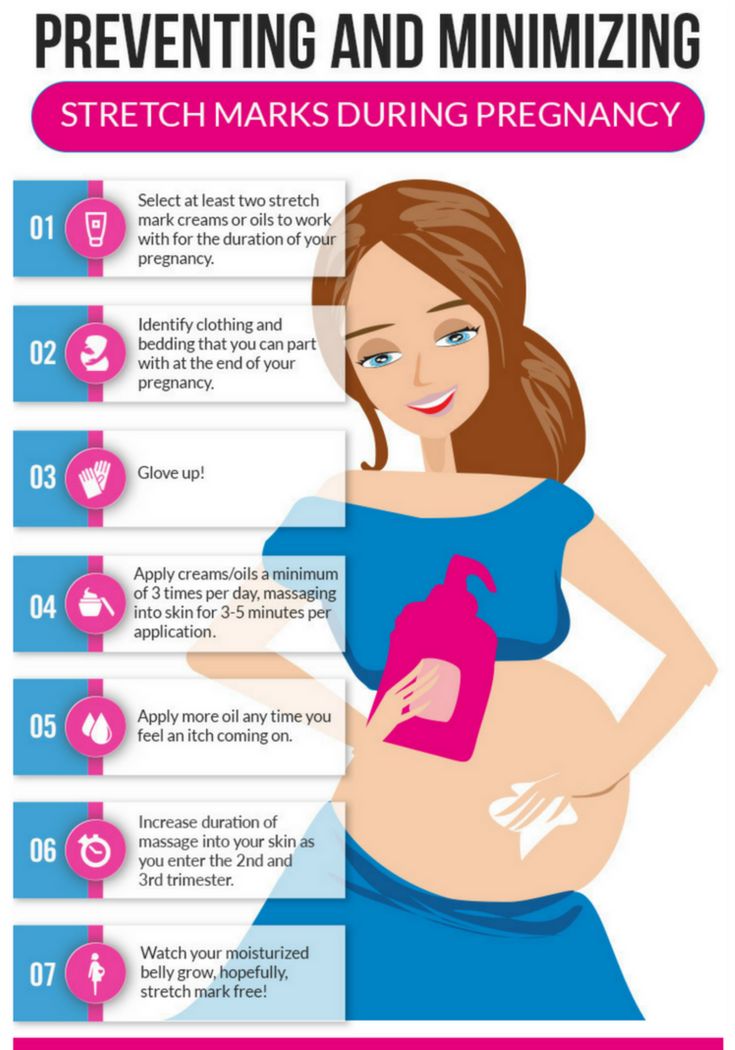 They may then determine the cause of the problem.
They may then determine the cause of the problem.
There are three types of miscarriage.
If a miscarriage has been threatened, there was bleeding before 20 weeks of pregnancy with no cervical dilation and no expulsion of any of the fetal parts.
If a miscarriage has been completed, there was complete expulsion of fetal parts from your body.
If a miscarriage has happened incompletely, there was partial expulsion of the fetal parts before 20 weeks. In the case of incomplete miscarriages, the next step may be to allow the remaining products of pregnancy to pass naturally or perform a dilation and curettage.
Note: If you have miscarried before and notice bleeding or cramping, you should seek emergency medical attention.
Always seek emergency care if you are experiencing the symptoms of an ectopic pregnancy (a pregnancy outside the uterus). Symptoms of an ectopic pregnancy include:
- cramps and colicky (spasmodic) pain with associated tenderness
- pain that starts on one side and spreads across the belly
- pain that worsens with taking a bowel movement or coughing
- light bleeding or spotting that is brown in color, is either constant or intermittent, and precedes the pain by weeks
- one of the above symptoms combined with nausea and vomiting, pain in the shoulder, weakness or lightheadedness, or rectal pressure
- rapid and weak pulse, clamminess, fainting, and sharp pain (these symptoms may arise if the ectopic pregnancy is in the fallopian tube and the tube ruptures, causing septic shock)
When to call your doctor
Emergency care isn’t always necessary. However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
However, some signs require a doctor’s evaluation. Always call your doctor for advice if you’re experiencing signs of miscarriage. Early signs of miscarriage include:
- cramps and pain in the center of the abdomen with vaginal bleeding
- severe pain or pain that lasts for more than a day (even without bleeding)
- bleeding that is as heavy as a period
- spotting or staining that lasts for three days or longer
Pain
Although you may not experience an emergency, there will probably be times during your pregnancy when you’re uncomfortable or in pain. Many women have pain during the second trimester even when nothing is medically wrong.
Abdominal pain, back pain, headaches, leg cramps, and hand pain don’t always signal a problem. Learning to identify and relieve these normal discomforts will help you throughout your pregnancy.
Abdominal pain
Abdominal pain can either be a normal symptom of pregnancy or a sign of something serious, like preterm labor or ectopic pregnancy.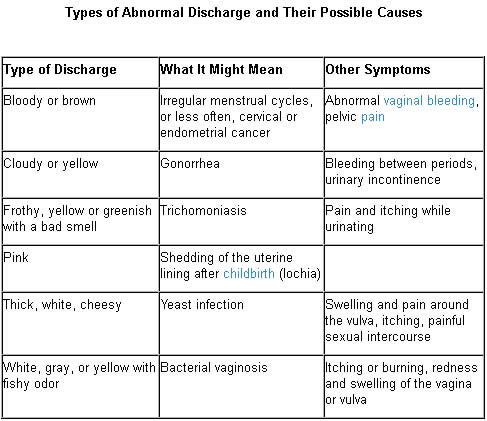 It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
It’s important to tell your doctor when you feel any type of abdominal pain, because of the potential for a serious complication.
When you feel pain in your abdomen during the second trimester, it’s usually related to the tension on the ligaments and muscles in the pelvis. These get stretched as the uterus expands to hold the growing baby.
If you move quickly, you can “pull” a ligament or muscle. This may feel like a painful pang in your pelvis or a cramp down your side that can last for several minutes. This kind of pain isn’t harmful to you or your baby.
Sometimes abdominal pain is related to past pregnancies or surgeries. If you’ve had surgery for infertility or other types of abdominal surgery, you may experience pain from the pulling of the remnants of scar tissue (adhesions).
Pregnant women can also have the same types of abdominal infections that other women develop. Infections that can cause abdominal pain include:
- cholecystitis (inflamed gallbladder)
- appendicitis (inflamed appendix)
- hepatitis (inflamed liver)
- pyelonephritis (kidney infection)
- pneumonia (lung infection)
Sometimes these diseases are harder to diagnose during pregnancy because the location of pain characteristic to each has been shifted.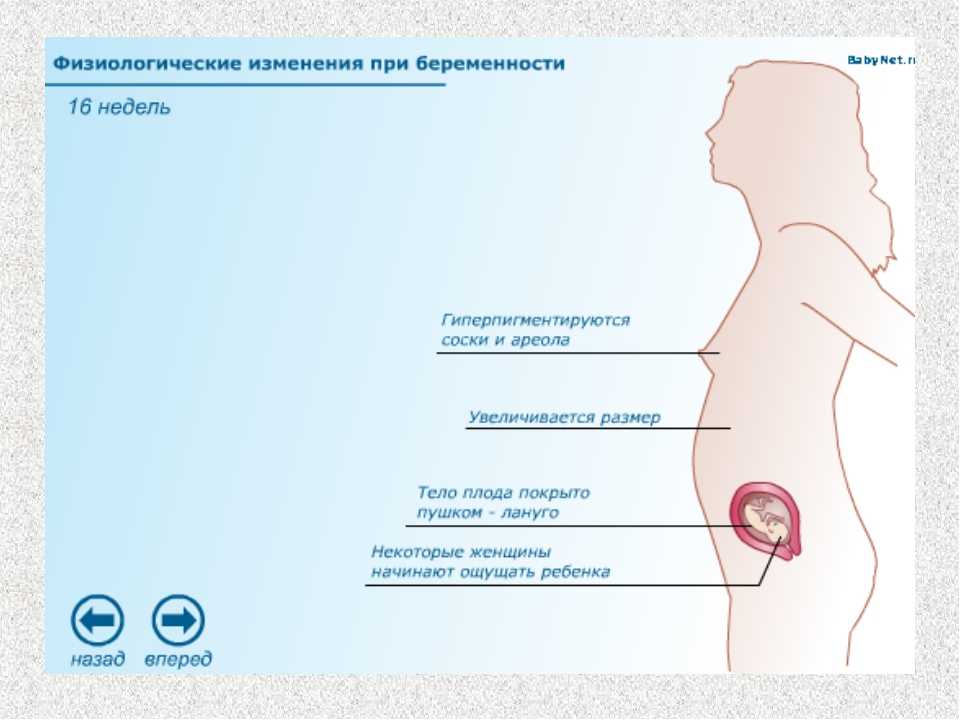 This happens when the growing uterus pushes nearby organs out of its way.
This happens when the growing uterus pushes nearby organs out of its way.
If you’re experiencing serious pain that doesn’t feel like it’s in your uterus, show or tell your doctor exactly where the pain is located. If you have one of the above infections, you may need antibiotics or surgery to fix the problem.
Warning: If you’re experiencing regular or painful contractions in the pelvis or abdomen, call a doctor immediately. These may be a sign of preterm labor.
Back pain
Back pain is very common during pregnancy. Pregnancy hormones cause the joints in the pelvis to become soft and lax in preparation for childbirth. As your uterus gets bigger in the second trimester, your center of gravity changes.
You begin to carry yourself differently to accommodate the weight. In addition, your abdominal muscles may separate as the uterus presses up against them, weakening the abdominal wall. All of these factors can contribute to back pain, strain, and discomfort.
Here’s how you can improve back pain:
- Practice good posture while standing (shoulders back, pelvis in) and sitting (elevate feet slightly and try to avoid crossing your legs).
- Get up every once in a while when you’re sitting for long periods.
- Lift heavy objects by bending at the knees, rather than the waist.
- Try not to reach for things over your head.
- Sleep on your left side, bending at your hips and knees, and place a pillow between your legs to reduce pressure on your back.
- Strengthen your stomach muscles. One of the keys to a strong back is a strong abdomen.
- Talk to your doctor. You may need to use a back brace or some other form of support to relieve the pressure on your back.
Warning: If you’re experiencing lower back pain accompanied by painful urination, you may have a bladder or kidney infection. Low, dull, consistent back pain may be a sign of preterm labor. Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Severe back pain coupled with vaginal bleeding or discharge may also indicate a serious problem. Call your doctor immediately if you experience any of these symptoms.
Headaches
Many women experience frequent headaches during pregnancy. You still may be experiencing headaches that started during the first trimester, or they may be just beginning now.
Hormonal changes, tension, fatigue, hunger, and stress are all culprits. Try to relax, stay rested, and eat regularly. You can also try to relieve headaches in the following ways:
- If you have a sinus headache, apply warm compresses to aches in the sinus areas of your head. These include both sides of the nose, the middle of the forehead, and the temples.
- If the headache is due to tension, try applying cold compresses to aches along the back of your neck.
- Learn relaxation exercises, like closing your eyes and imagining yourself in a peaceful place. Reducing stress is a key component of a healthy pregnancy.
 Consider calling a counselor or a therapist if needed.
Consider calling a counselor or a therapist if needed.
Speak with a physician before you begin using pain relievers. This is important even if you took over-the-counter medications for pain before you were pregnant.
Common headache medicines include ibuprofen (Motrin), aspirin (Bufferin), acetaminophen (Tylenol), and naproxen sodium (Aleve).
Acetaminophen is probably the safest option during pregnancy, but don’t take pills during pregnancy unless your doctor has specifically told you to do so.
Warning: Call your doctor if the headache is particularly severe or lasts for more than a few hours. Also note whether your headache comes with a fever, swelling in the face and hands, dizziness, nausea, or changes in vision. These may be signs of preeclampsia or another serious complication.
Leg cramps
Although no one knows exactly what causes them, leg cramps are common in the second and third trimester. Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
Possible causes may be that you don’t consume enough calcium, have too much phosphorous in your diet, or are tired.
It may be that the uterus is pressing on the nerves that go to the legs. Regardless of the cause, you may wake up in the middle of the night with bothersome cramps.
You can avoid or get rid of cramps by:
- exercising your calves
- staying hydrated
- alternating between sitting and standing
- wearing support hose
- wearing comfortable, supportive shoes
- flexing the ankle and toes upward with a straightened knee to stop the cramping
- massaging or applying a warm compress to the leg that is cramping
- talking to your doctor about reducing the amount of phosphorous in your diet by cutting down on foods like milk or meat
- making sure you get enough calcium (by eating fortified cereal or spinach) and magnesium (by eating beans or semisweet chocolate)
Warning: Tell your doctor if the cramps feel particularly painful, fail to go away, cause swelling, feel warm to the touch, or change the skin color of your leg (to white, red, or blue). You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
You may have a blood clot in a leg vein that needs to be treated. This is known as deep vein thrombosis, and without treatment it can be deadly. Consult a doctor immediately.
Pain and numbness in the hand
Numbness and pain in the thumb, index finger, middle finger, and half of the ring finger can be a sign of carpal tunnel syndrome.
Usually this condition is diagnosed in people who regularly perform repetitive tasks such as typing or piano playing, but it’s also common in pregnant women.
During pregnancy, the tunnel that surrounds the nerve to these fingers can become swollen, causing tingling, numbness, and pain. In the evening, after your arm has been dangling by your side all day, your symptoms may worsen due to gravity.
Shaking out your arm when you experience the carpal tunnel symptoms may help. Alternatively, you may want to talk to your doctor about splinting your wrist or taking vitamin B-6.
Numbness and tingling in the hand can also be caused by poor posture.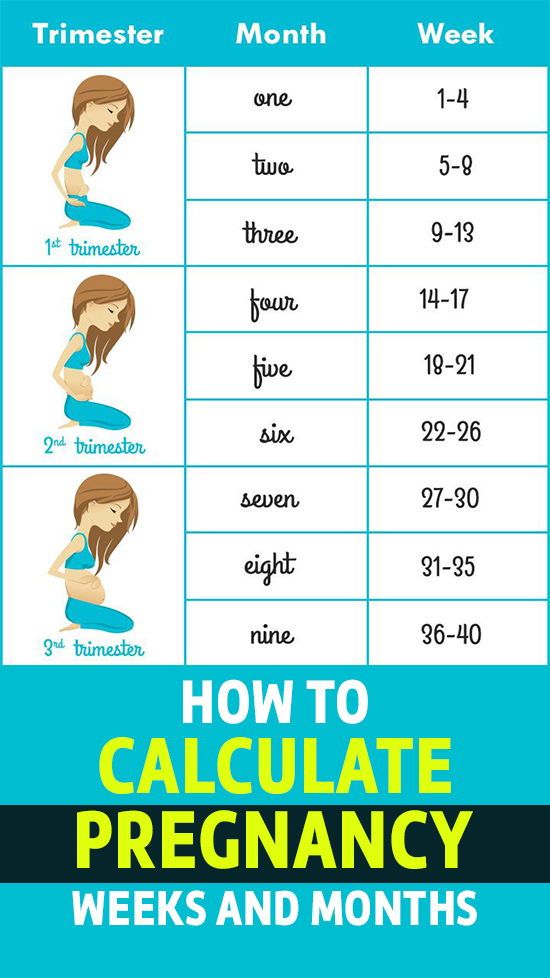 If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
If your shoulders droop and your head is thrust forward, you put pressure on the nerves under your arms, causing tingling.
Practice standing up straight with your head and spine erect. A supportive bra and proper bed rest are also important.
Bleeding
Bleeding can be a scary symptom during pregnancy. In some cases, bleeding can be harmless. It can happen when pregnancy hormones cause you to develop more sensitive, expanded blood vessels.
In other cases, bleeding can indicate a serious problem with the pregnancy. If you experience any bleeding, call a doctor for advice.
Vaginal bleeding
Light bleeding or spotting (which can be brown, pink, or red) during the second and third trimester isn’t usually cause for concern. It typically occurs as a result of interference with the cervix during sex or a vaginal exam.
Pink mucus or brownish discharge may both occur during the second trimester. It’s caused by small amounts of blood leaving your body with normal discharge.
Vaginal bleeding that’s like a period, however, can be a worrisome sign that needs immediate medical attention. Clots of blood or clumps of tissue in the blood may be symptoms of a miscarriage.
For this reason, you should never be the judge of what is normal or abnormal bleeding. Instead, call your doctor.
If the bleeding is heavy or if it’s accompanied by pain, call your doctor immediately. If it’s spotty, you can make the call sometime that day. Serious bleeding is most commonly caused by placenta previa, premature labor, or late miscarriage.
Rectal bleeding and hemorrhoids
Rectal bleeding isn’t as worrisome as vaginal bleeding and is generally a sign of either hemorrhoids or anal fissure. Rectal bleeding could also be a sign of something more serious. You should speak with your doctor if you’re experiencing this symptom.
Rectal bleeding may mean you have hemorrhoids, either external or, less commonly, internal. Hemorrhoids occur in up to half of all pregnant women.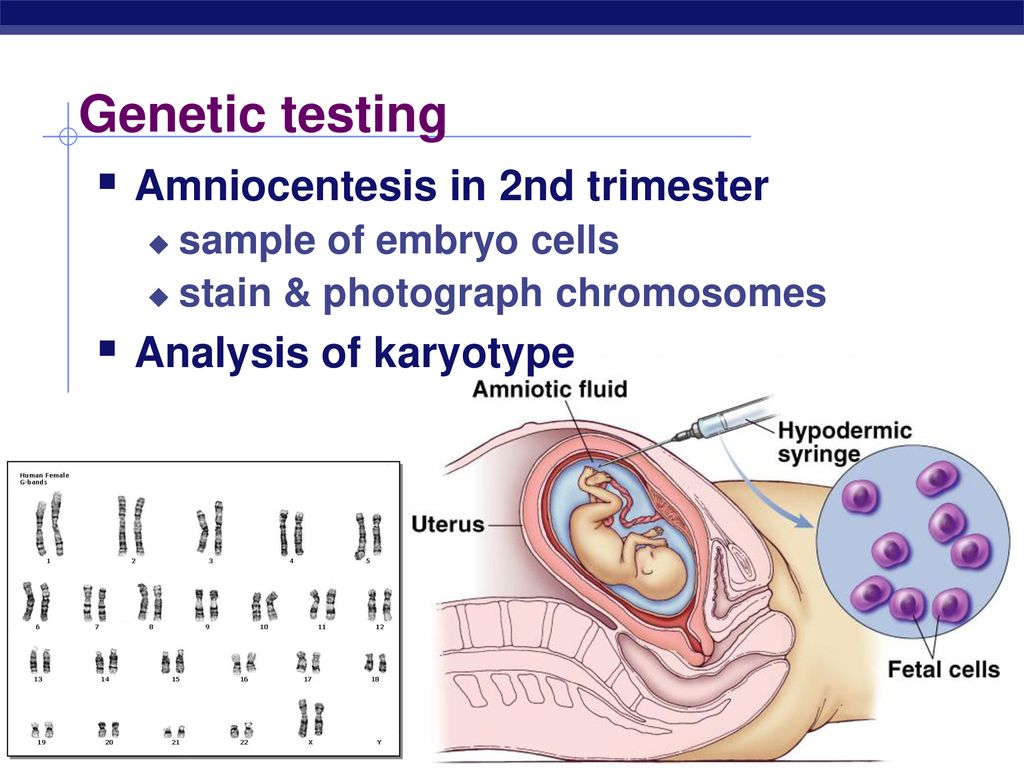 They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
They are varicose veins of the rectum and can cause pain, itching, and bleeding, often made worse by constipation.
Hemorrhoids are caused by progesterone acting on the walls of the rectal veins, causing them to relax and expand. As you advance in your pregnancy and the uterus presses on these veins, blood flow slows down and the veins dilate even more.
Squeezing and constipation can make hemorrhoids worse. Laughing, coughing, straining, and going to the bathroom may cause hemorrhoids to bleed.
If rectal bleeding isn’t caused by hemorrhoids, it may be caused by an anal fissure — a crack in the skin that lines the anal canal. Anal fissures are usually caused by constipation. Fissures are very painful, particularly during the strain of taking a bowel movement.
Hemorrhoids and anal fissures can cause brown, pink, or red bloodstains to appear on your underwear or toilet paper. If the bleeding is heavy or continuous, call a doctor for advice.
If you’re diagnosed with hemorrhoids or an anal fissure, you should do the following:
- Try to avoid constipation by remaining well hydrated and eating a diet high in fiber.

- Try to alleviate pressure on the veins in the rectum by sleeping on your side, not standing or sitting for long periods of time, and not taking too long or straining when going to the bathroom.
- Take warm sitz baths up to two times a day. Sitz baths are basins that fit on your toilet and are filled with warm water in which you can soak your anus.
- Soothe the hemorrhoids with ice packs or witch hazel, and only use topical medications if your doctor prescribes them. Your doctor may also prescribe stool softeners or a laxative.
- Practice good hygiene by wiping thoroughly after bowel movements (from front to back) and keeping yourself clean.
- Use only white, unscented toilet paper.
- Perform Kegel exercises to improve the circulation to the area.
Warning: Massive rectal bleeding can be a serious problem. It can be caused by ectopic pregnancies or serious internal problems. Seek medical care immediately if you’re bleeding heavily from the anus.
Nosebleeds and nasal congestion
Like many of the complaints of pregnancy, nasal stuffiness and nosebleeds are believed to be due in large part to estrogen and progesterone. These hormones cause increased blood flow and swelling of the blood vessels in the mucus membranes.
Particularly in cold, dry weather, this can mean that you feel more congested than normal. You may also experience nosebleeds more often than you did before getting pregnant.
You may want to try the following to ease your nasal symptoms:
- Use a humidifier to help with the dryness that can make symptoms worse.
- Blow your nose gently by closing one nostril while you blow through the other.
- Curb nosebleeds by leaning forward and applying gentle pressure to the nose. Try squeezing it with the thumb and forefinger for five minutes. Repeat if necessary.
- Call your doctor if the bleeding doesn’t stop, or is heavy or frequent.
- Seek emergency medical care if nasal congestion makes it hard to breathe.

The same changes in hormones and blood vessels that cause nasal bleeding can cause sensitive gums. If you experience bleeding when flossing or brushing your teeth, try using a softer toothbrush.
Visit a dentist if you bleed a lot or have a lot of pain when flossing or brushing your teeth. Serious dental problems can be a sign of other health concerns that can complicate pregnancy.
Discharge
Many women experience different types of discharge during the second trimester. Pay attention to the color, smell, amount, and frequency of vaginal or anal discharge. Some types of discharge may indicate an infection that needs medical attention or treatment.
Vaginal discharge
As the pregnancy progresses, you may notice increasing vaginal discharge. Typically, it looks like egg whites and is milky and a bit odorous. It may remind you of premenstrual discharge, only a bit heavier and more frequent.
This discharge is totally normal and is just another change your body goes through in response to the pregnancy hormones and the increased blood flow to the area. You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
You can wear panty liners or change your underwear more often than usual if you find the discharge bothersome.
Though the kind of discharge described above is normal, there are some types of discharge that may mean you have an infection.
Vulvovaginal candidiasis, or yeast infection, is very common during pregnancy. Signs include a thick, cottage cheese-like discharge accompanied by itching, redness, and burning, as well as painful intercourse and urination.
Sexually transmitted infections (STIs) may also occur during pregnancy, and because many of them can affect the fetus, it’s important that they be treated.
You may have a condition that requires treatment if any of the following is true:
- The discharge looks like pus.
- The discharge is yellow, green, or has a foul odor.
- You notice a burning sensation when you urinate.
- Your labia are red, swollen, or itchy.

Unlike signs of infection, clear or pinkish watery discharge may be a sign of premature rupture of the amniotic sac.
Rupture of the sac may cause a trickle of watery discharge or a rush of lots of watery fluid from the vagina. This is commonly known as having the water break before labor begins.
Warning: If you experience a steady trickle or a rush of watery discharge during the second trimester, call a doctor immediately. It may be a sign of premature labor or a tear in the amniotic sac.
Rectal discharge
In addition to bleeding from the rectum, some women may experience anal discharge during pregnancy. Rectal discharge may be caused by STIs, bowel and gastrointestinal problems, or physical wounds in the rectum. If you’re experiencing rectal discharge, consult a doctor.
Gonorrhea, chlamydia, and other infections that can be transmitted through sexual contact can cause an infection in the anus. These infections can cause lesions or sores that bleed.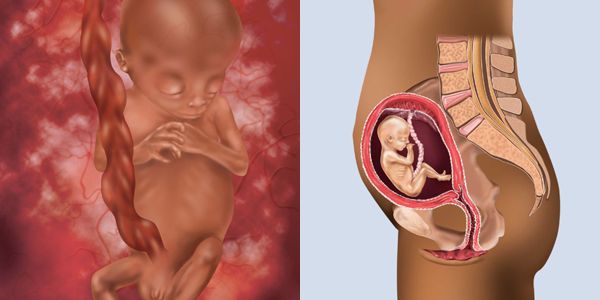 In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
In addition, they may lead to discharge that’s foul-smelling, green or yellow, and thick.
It may be painful to wipe or go to the bathroom. If you have these symptoms, discuss them with a doctor. Left untreated, they may cause serious problems for the baby. Most STIs can be treated with antibiotics.
Some pregnant women may experience anal discharge due to bowel problems or gastrointestinal disorders. These may result in mucus or watery discharge from the anus.
Certain gastrointestinal problems or food poisoning may also cause frequent diarrhea or fecal matter with unusual colors or textures. Tell your doctor about any unusual characteristics of your bowel movements. Some conditions require immediate treatment.
Finally, if you have a hemorrhoid or anal fissure that has become infected, you may notice unusual rectal discharge. Infected wounds may cause brown, yellow, green, or white discharge.
Such a wound may or may not have a foul smell. Infected sores are often very painful and require medical attention.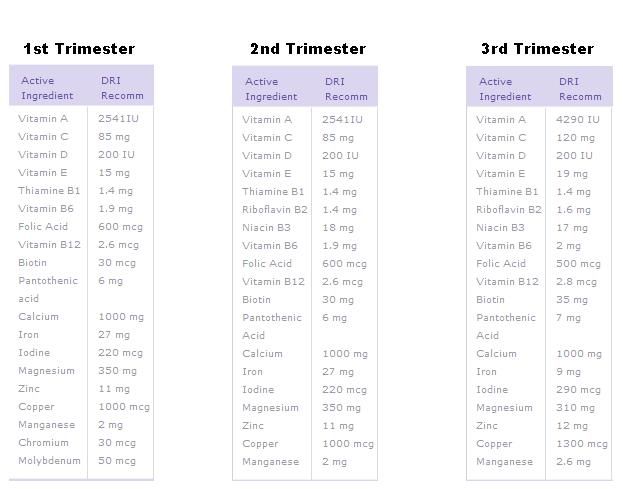 Consult a doctor for treatment if you experience anal discharge of this nature.
Consult a doctor for treatment if you experience anal discharge of this nature.
Nipple discharge
Many women experience discharge from one or both nipples during the second trimester of pregnancy. Breast tenderness and changes in nipple color are also common during pregnancy.
Discharge is most common in women who have previously given birth. Nipple discharge is often clear, milky, or yellowish in color.
Discharge from the nipples is normally not a sign of a problem, unless the following symptoms are present:
- The nipple changes in size or becomes inverted.
- The nipple is dry, cracked, or painful.
- The nipple has a rash or new bumps.
- The discharge is foul-smelling, bloody, green, or brown.
If you aren’t sure whether your nipple discharge is normal, call a doctor to discuss your symptoms.
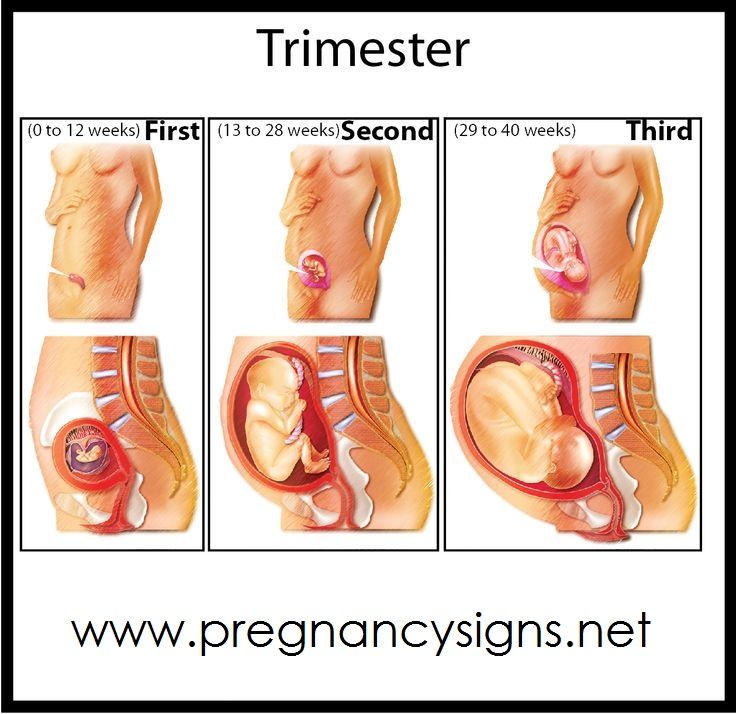
which week it starts, what can and cannot be done for pregnant women, nutrition and tests
Published: 06/27/2017
Reading time: 7 min.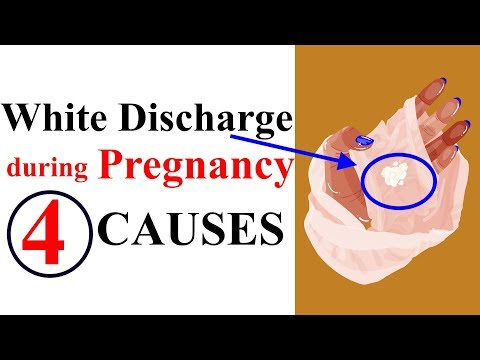
Number of reads: 26898
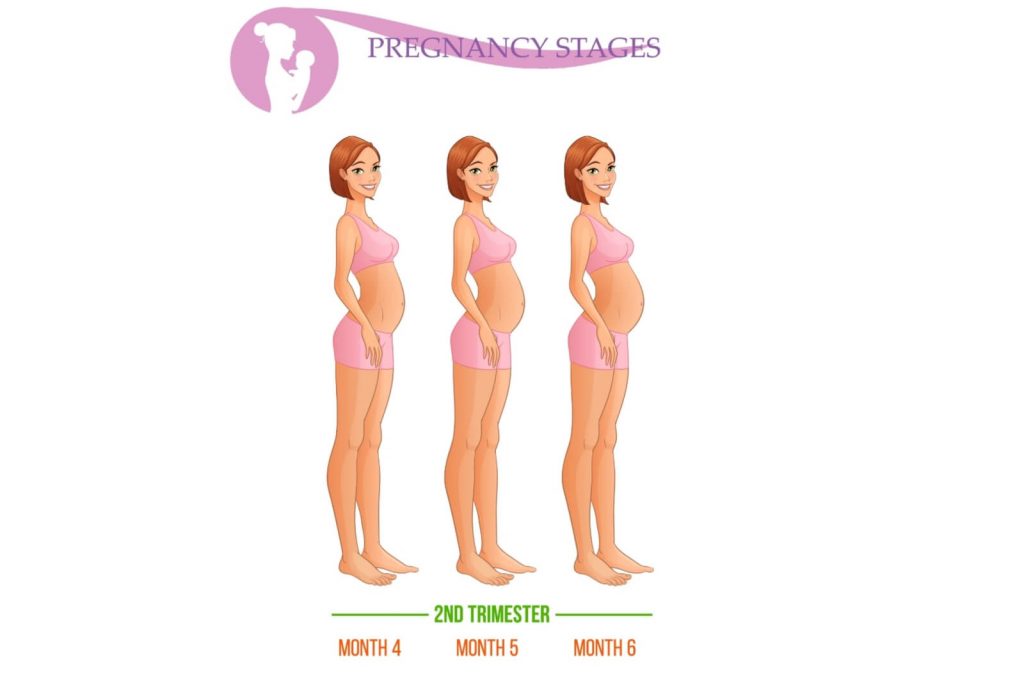
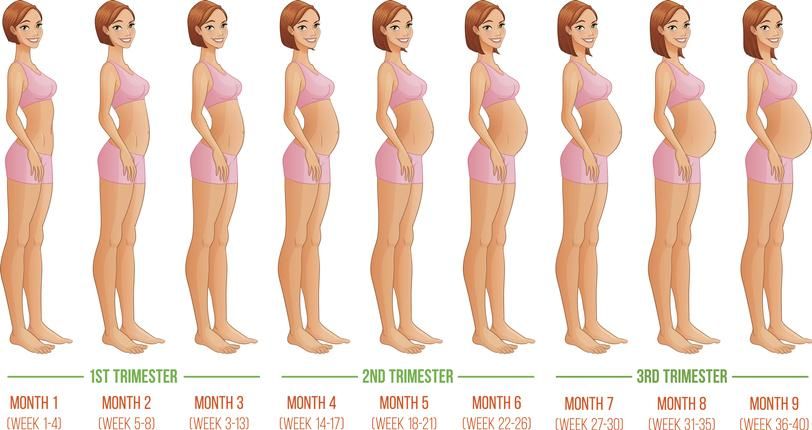
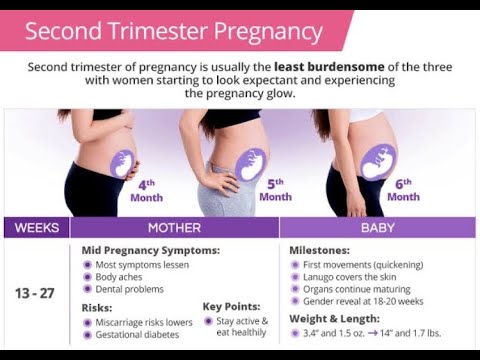
The second trimester of pregnancy is considered the "golden mean". It lasts from the 15th to the 26th week. At this time, the expectant mother, as a rule, no longer suffers from toxicosis, and the appearance of a large tummy is still far away. In the second trimester of pregnancy, appetite usually improves, mood improves. The woman literally blossoms and receives a lot of compliments. nine0003
Features of the course and signs of pregnancy in the second trimester
In the second trimester of pregnancy, certain physiological processes occur in a woman's body. Due to the increased level of estrogen, the production of melanin increases. Therefore, the expectant mother may darken the nipples and areolas. A dark line often appears on the skin of the abdomen. This is the median line, which doctors call Linea nigra. But do not be afraid, after childbirth, hyperpigmentation disappears.
During this period, the woman's body begins to actively prepare the mammary glands for feeding the baby. Under the influence of hormones, blood circulation increases in them, they begin to grow, sometimes increasing by 1-2 sizes. nine0003
Under the influence of hormones, blood circulation increases in them, they begin to grow, sometimes increasing by 1-2 sizes. nine0003
In the fourth month (approximately the 16th week), some pregnant women, for medical reasons, undergo an invasive amniocentesis procedure - the removal of amniotic fluid. Their analysis will help to identify various genetic pathologies in the early stages.
At the fifth month of pregnancy (at the 19th week), significant changes begin to occur in the body. In a woman, due to an increase in cardiac output, the pulse quickens, the volume of circulating blood increases by about 0.5 liters, and the level of hemoglobin may fall. nine0003
From the 21st week, when the child's musculoskeletal system begins to actively develop, the need for vitamins and minerals increases dramatically. It is during this period that the expectant mother needs to take care of their sufficient intake into the body. All reserves will go to the baby, and a woman, due to a shortage, may experience calf cramps, become brittle teeth, drop the level of iron in the blood, and as a result, develop anemia.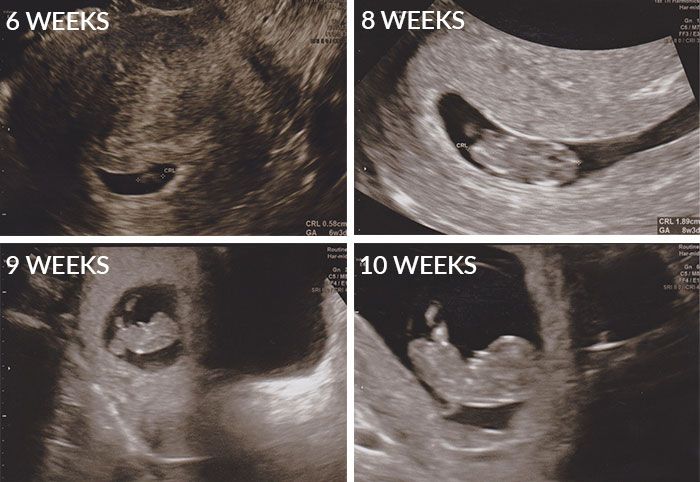
Between the 24th and 28th weeks, a complex blood test is performed, which can be used to determine glucose tolerance. It allows you to detect gestational diabetes in pregnant women. This condition is temporary and disappears after the birth of the child, but during pregnancy it can adversely affect the fetus. nine0003
At 25-26 weeks placental lactogen, a special peptide hormone, stimulates the production of the first colostrum. The mammary glands continue to grow. It's time to start preparing them for lactation. To do this, wash the chest with warm water and lightly rub the skin with a hard towel. But this is done carefully, since excessive massage can provoke an undesirable uterine tone.
Weekly development of the fetus in the second trimester of pregnancy
In this trimester, the baby is actively developing and gaining weight. This is a little man, whose systems and organs are almost completely formed and gradually begin to work. nine0003
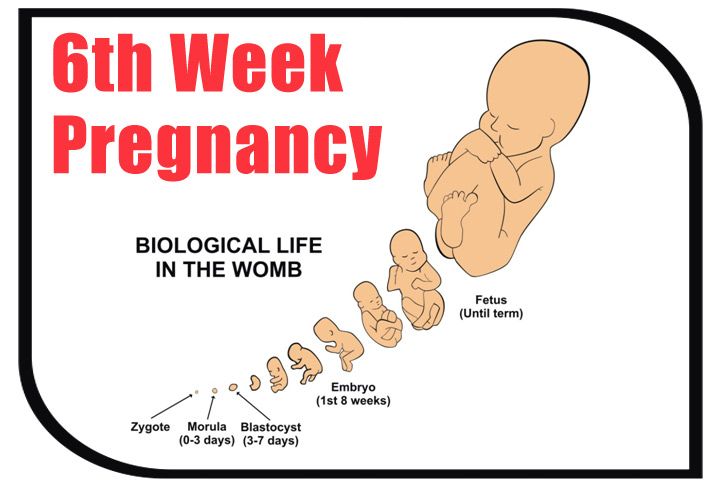
At the 15th week of pregnancy, the weight of the fetus is about 70 g, and its length is only 10 cm. But the baby can already grimace, as his facial muscles and nerves are functioning. He begins to move actively. The liver produces bile and the pancreas produces insulin. The skin, although formed, is still very thin. Blood vessels are easily visible through them. The fetus has a clearly auscultated heartbeat. Hair and eyebrows grow, milk teeth are laid. At the 16th week, the baby moves freely in the amniotic waters. nine0003
But the baby can already grimace, as his facial muscles and nerves are functioning. He begins to move actively. The liver produces bile and the pancreas produces insulin. The skin, although formed, is still very thin. Blood vessels are easily visible through them. The fetus has a clearly auscultated heartbeat. Hair and eyebrows grow, milk teeth are laid. At the 16th week, the baby moves freely in the amniotic waters. nine0003
At 17 weeks, the fetus weighs about 140 g and is 13 cm long. In the fourth month of pregnancy, the mother begins to feel her baby's movements. The thin skin of the baby is covered with soft fluffy hairs. During this period, the immune system is formed.
At 18 weeks, the fetus weighs about 190 g and is 14 cm long. He can already hear sounds coming from the outside world well, because the hearing aid is fully developed. At this stage, permanent teeth begin to form. The child moves, often changing the position of the body, crosses the legs and sucks his thumb. Reacts to bright light. nine0003
Reacts to bright light. nine0003
At 19 weeks, the baby begins to take an active interest in his little world. He touches the walls of the fetal bladder, face, pulls the umbilical cord. The baby can already react to loud sounds. The stress experienced by the mother responds with increased activity. His skin is covered with caseous grease - a viscous white substance that performs protective functions. By this time, the nerve cells of the brain responsible for the sense organs were fully formed. And now the improvement of these systems begins. nine0003
At the 20th week, the fetus is 16 cm long and weighs 300 g. The baby can already distinguish between day and night, so his activity may increase or decrease depending on the time of day. He is well versed in his little world. The twins at this time can already find each other and even hold hands.
At the 21st week, the fetus can weigh about 360 g, its length is about 27 cm. From this moment, the child begins to grow actively, gaining weight.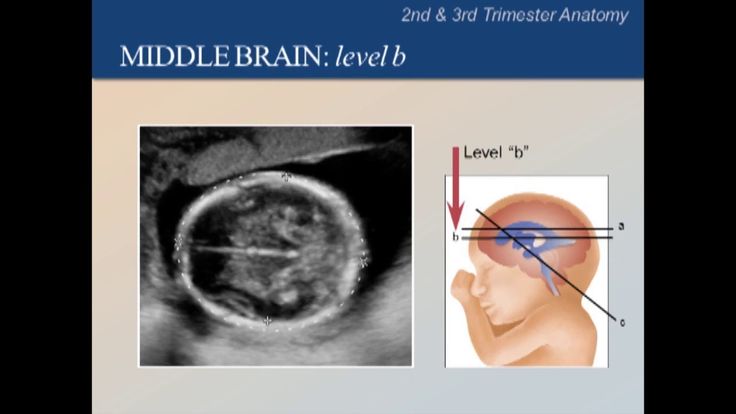 That is why mom needs an urgent intake of calcium and iron-containing drugs, and even better - vitamin-mineral complexes (if she did not start doing this in the first trimester). At this time, the intestines of the child are fully formed and a small amount of carbohydrates contained in the amniotic waters begins to be absorbed in it. Blood cells are produced in the bone marrow, and their synthesis in the spleen and liver gradually decreases. The reproductive system is actively developing. nine0003
That is why mom needs an urgent intake of calcium and iron-containing drugs, and even better - vitamin-mineral complexes (if she did not start doing this in the first trimester). At this time, the intestines of the child are fully formed and a small amount of carbohydrates contained in the amniotic waters begins to be absorbed in it. Blood cells are produced in the bone marrow, and their synthesis in the spleen and liver gradually decreases. The reproductive system is actively developing. nine0003
By the 23–24th week, all organs and systems are practically formed in the child. Its weight reaches 500-600 g. Surfactant begins to be produced in the alveoli - a mixture of substances that prevents the lungs from sticking together. However, it is still not enough for the baby to breathe on its own. Therefore, a child born prematurely must be placed in a special apparatus - an incubator - where there are systems that will help him survive. During this period, the fetus already completely fills the uterine cavity and begins to stretch it. The bottom of the uterus is at the level of the navel at a height of 24 cm from the articulation of the pubic bone. The baby has a fully developed inner ear, so he can determine what position his body is in and change it by actively moving in the amniotic fluid. The skin of the baby becomes less transparent, pigment begins to be produced in it. At this time, unique fingerprints are formed. nine0003
The bottom of the uterus is at the level of the navel at a height of 24 cm from the articulation of the pubic bone. The baby has a fully developed inner ear, so he can determine what position his body is in and change it by actively moving in the amniotic fluid. The skin of the baby becomes less transparent, pigment begins to be produced in it. At this time, unique fingerprints are formed. nine0003
At the 25th week, the weight of the fetus can reach 750 g. The adrenal glands and the pituitary gland begin to function, producing hormones. There is an improvement in the structures of the brain. During the 20-28th week, the child doubles its height.
Pain in the second trimester of pregnancy
After the 20th week, during the movement of the baby, short-term Braxton-Hicks contractions may occur, which last no more than 1-2 minutes. Such false contractions cause pain in the lower abdomen. Many pregnant women begin to worry about this. However, this condition does not pose a threat to the health of the baby or the expectant mother. So nature prepares the uterus for labor, trying to teach her to contract and relax. nine0003
So nature prepares the uterus for labor, trying to teach her to contract and relax. nine0003
During the second trimester of pregnancy, pulling pains may appear in the lumbar region. This usually occurs at 25-26 weeks and is due to the fact that the uterus increases significantly in size. Due to the increased load on the muscles and ligaments, periodic pulling pains in the back occur. Wearing flat shoes and frequent resting in a lying position can alleviate this condition.
In addition, pain in the lower abdomen during the second trimester of pregnancy can occur when the uterus begins to press on the bladder, there is frequent and sometimes painful urination. nine0003
In any case, any discomfort should be reported to the doctor.
Second trimester discharge
Many pregnant women complain of second trimester discharge. Most often this is due to the development of thrush, which is caused by yeast-like fungi of the genus Candida albicans. They are present in the body of every person, but are activated due to a decrease in immunity.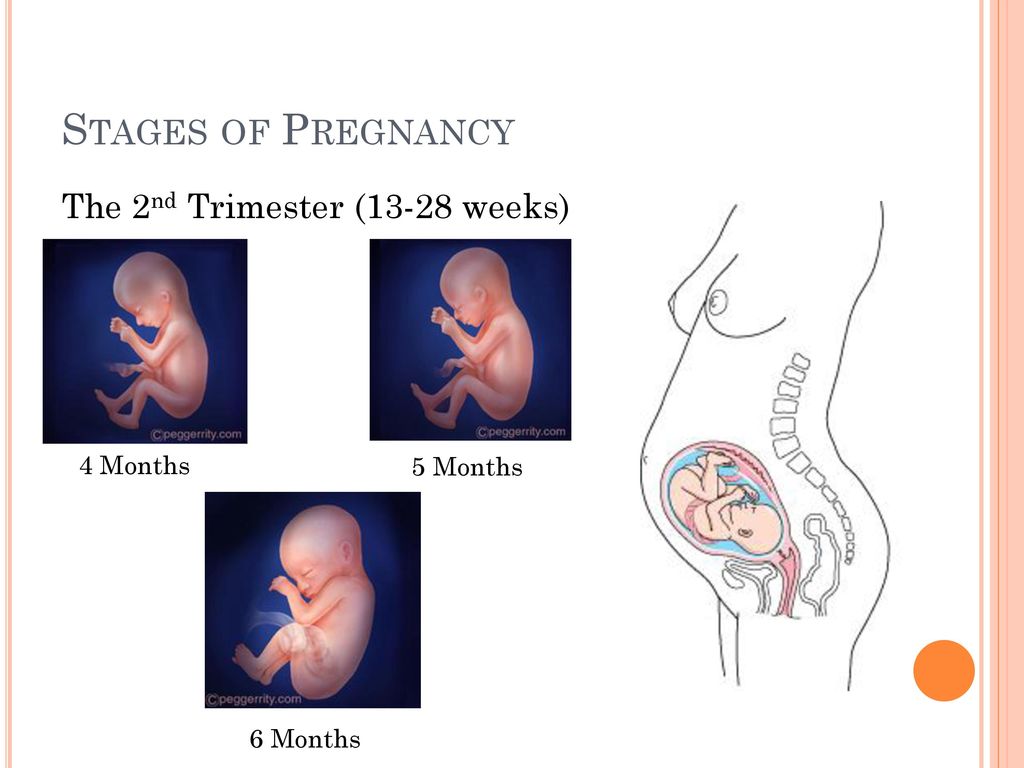 And during pregnancy, it significantly weakens.
And during pregnancy, it significantly weakens.
However, other, more dangerous microorganisms can cause discharge. Therefore, in any case, with prolonged and abundant discharge, it is necessary to consult a doctor and immediately begin treatment. nine0003
Bleeding causes the greatest concern, as it can be a sign of placental abruption or a consequence of trauma, high blood pressure and other conditions dangerous for a pregnant woman. In this case, immediate medical attention is required.
Vitamins and minerals in the second trimester of pregnancy
All pregnant women know that their diet should be rich in nutrients. This is necessary for the full growth and development of the fetus, as well as for the normal functioning of the endocrine system and the absorption of proteins. nine0003
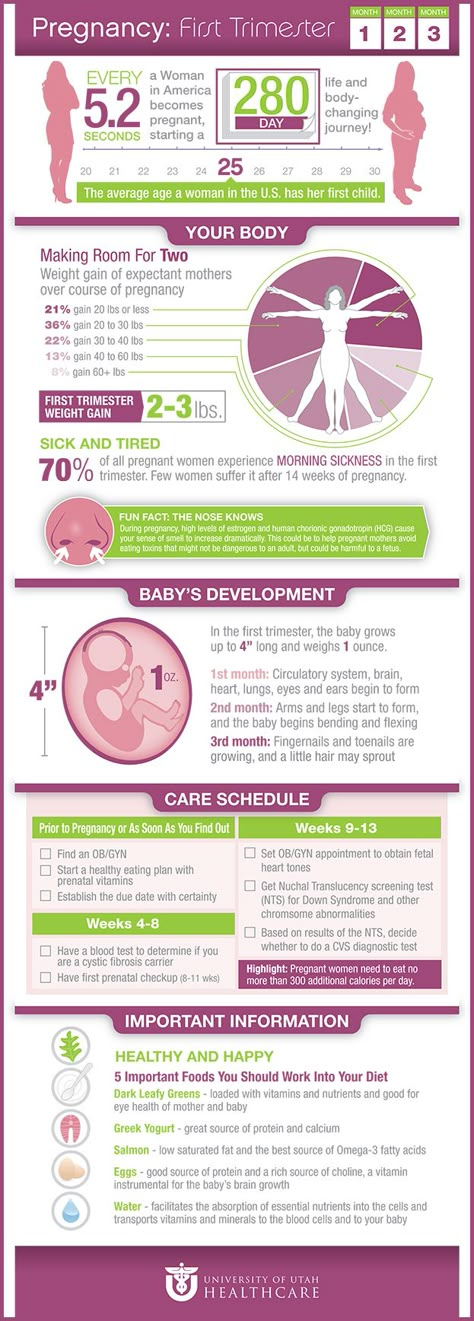
The baby receives vitamins and minerals from the mother. If her diet is poor, reserves from her own body are spent on the needs of the child. And this has a very negative impact not only on the course of pregnancy, but also on the health of the expectant mother.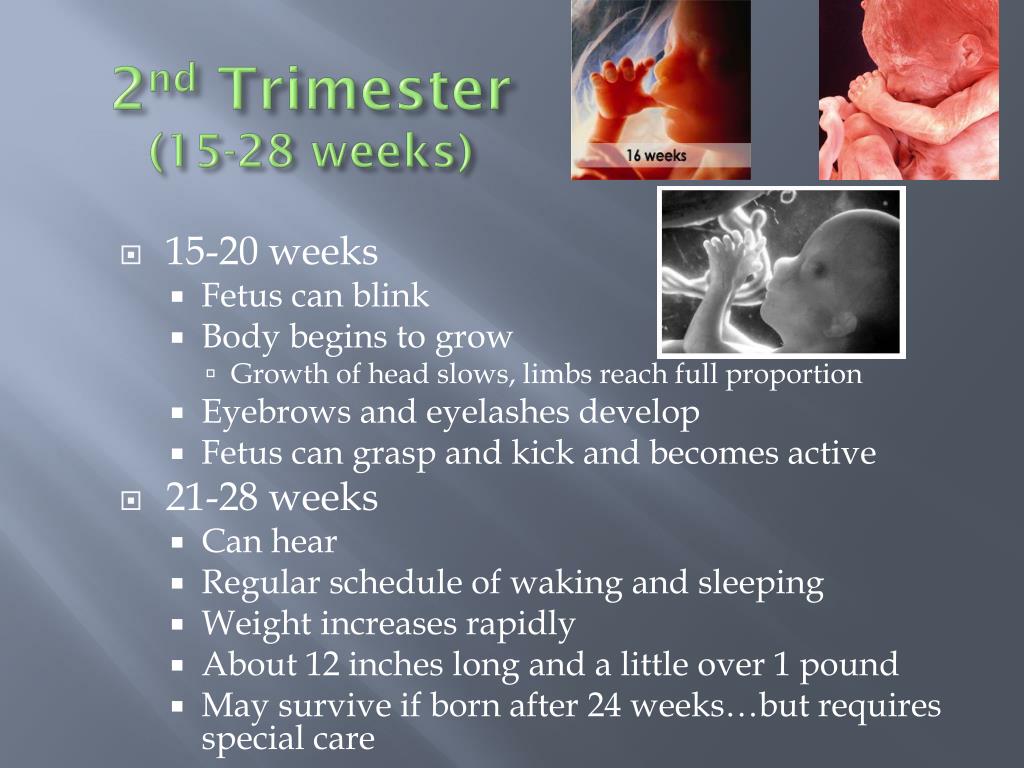 So, during pregnancy, the body's need for calcium increases one and a half times, twice for iron and folic acid, and 30% for zinc, iodine, and B vitamins. Consider the features of these substances.
So, during pregnancy, the body's need for calcium increases one and a half times, twice for iron and folic acid, and 30% for zinc, iodine, and B vitamins. Consider the features of these substances.
- Vitamin A. Required for vision and proper development of the skin and mucous membranes in a child. nine0074
- Vitamin B with or B 9 (folic acid). Participates in the formation of the placenta, new blood vessels, the synthesis of nucleic acids and hematopoiesis. Contributes to the proper development of the brain. The expectant mother also needs this vitamin. With its help, the restoration and renewal of cells in her body occurs.
- Vitamin B 6 . Participates in the synthesis of proteins - the main "building material" of cells. It is also necessary for hematopoiesis, contributes to the proper development of the nervous system and brain. It is also needed by a pregnant woman, as it reduces the manifestations of toxicosis and relieves irritability.
 nine0074
nine0074 - Vitamin C. Strengthens the immune system and blood vessel walls. Participates in the formation of the membranes of the fetus.
- Vitamin D . Helps the body absorb calcium needed for the development of bones and teeth.
- Vitamin E. Improves metabolic processes. Takes part in tissue respiration. Is an antioxidant.
- Iron. Participates in the supply of oxygen to all organs of the fetus. nine0074
- Calcium. Necessary for the formation of the musculoskeletal system and the nervous system.
- Zinc. Stimulates hematopoiesis and puberty. Affects the growth and weight of the fetus.
- Magnesium. Needed for fetal development, involved in bone formation.
- Copper. Takes part in the synthesis of blood cells, joints, cartilage, connective tissue.
- Iodine . Necessary for the proper formation of the central nervous system and skeleton.
 Responsible for the mental development of the child. Participates in the production of hormones that affect protein synthesis. nine0074
Responsible for the mental development of the child. Participates in the production of hormones that affect protein synthesis. nine0074
Pregnant women should be aware that no vitamin diet is able to cover the daily requirement of nutrients. Therefore, vitamins in the second trimester of pregnancy must be taken in the form of vitamin-mineral complexes, which the doctor will definitely prescribe, based on the general condition of the woman.
Sex in the second trimester of pregnancy
You can have sex in the absence of contraindications for almost the entire period, and the second trimester of pregnancy is no exception. It does not make sense to completely refuse intimacy with a beloved man. Reasonable restrictions on sex in the second trimester of pregnancy must be observed, but strict prohibitions can only be for those women who have certain contraindications, and above all the threat of miscarriage. At later dates, there may be some problems associated with the size of the abdomen. nine0003
nine0003
Today, doctors say that sex during pregnancy is not only not harmful, but also useful. Intimacy improves mood. As a result of sexual intercourse, blood circulation in the genitals improves. This means that the baby receives more nutrients for its development.
What questions might a future mother worry about
Do I need special care for my breasts?
During the second trimester, some women begin to produce colostrum. Therefore, breast care should be regular: washing with warm water and wiping with a hard towel. But here you can not overdo it. In addition, it is necessary to choose the right bra so that the enlarged breasts do not lose their shape and do not cause discomfort. nine0003
What if the nipple is flat or inverted?
If it is not developed, the baby will not be able to breastfeed on his own and will have to be bottle fed. Therefore, the nipples need to be slightly straightened with the help of special exercises, which should be started from the second trimester.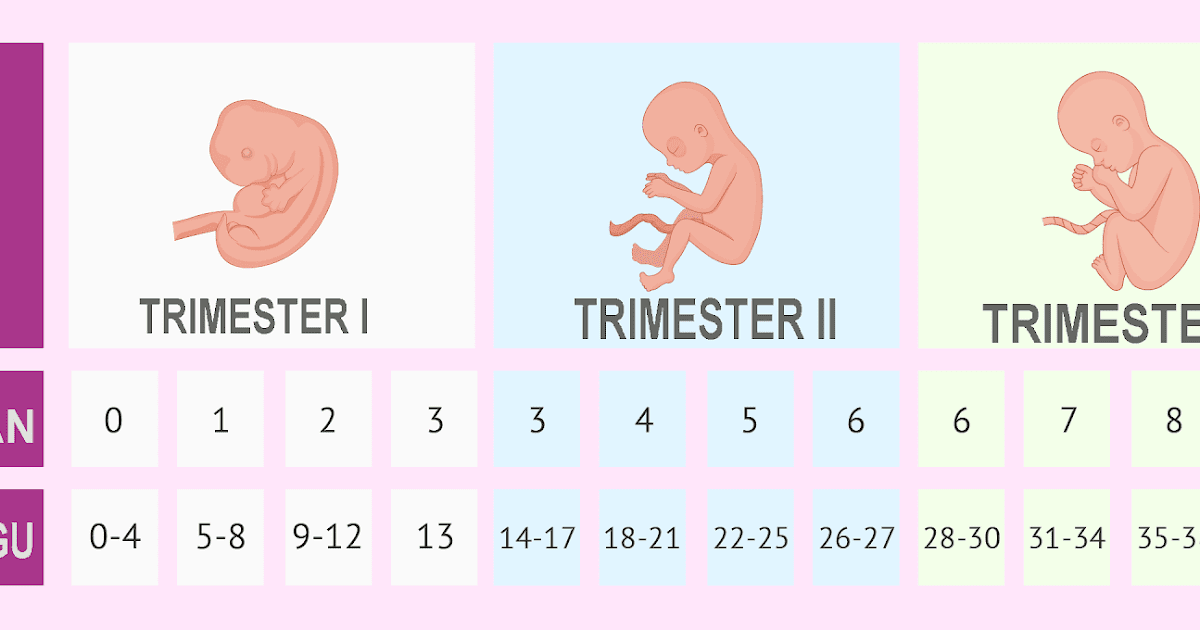 After washing the breast, the nipple should be gently grasped with the thumb and forefinger, gently pulled out and scrolled. However, such exercises should be done only in the absence of a threat of miscarriage. Otherwise, you can bring the uterus into tone. nine0003
After washing the breast, the nipple should be gently grasped with the thumb and forefinger, gently pulled out and scrolled. However, such exercises should be done only in the absence of a threat of miscarriage. Otherwise, you can bring the uterus into tone. nine0003
How to prevent stretch marks?
The appearance of stretch marks depends on the density of the skin. It is on delicate and thin skin that they will appear first. But now there is a huge variety of special creams and lotions for pregnant women on the market, which can slightly increase the elasticity of the skin and reduce the appearance of stretch marks.
What are the features of personal hygiene during pregnancy?
There are practically none. The main thing is to take a shower every day to remove sweat from the skin. After all, the skin performs not only protective functions, but also participates in respiration and metabolism, removing harmful substances from the body. During pregnancy, it is not recommended to visit the bathhouse and sauna frequently, and especially to abuse the steam room. The temperature should be comfortable. Otherwise, blood pressure may rise, and, as a result, there is a threat of miscarriage or premature birth. And it is best to avoid such procedures altogether during this delicate period. nine0003
The temperature should be comfortable. Otherwise, blood pressure may rise, and, as a result, there is a threat of miscarriage or premature birth. And it is best to avoid such procedures altogether during this delicate period. nine0003
Expectant mothers have a lot of questions, especially those who are expecting their first child. It is simply impossible to foresee everything, and situations are different. Therefore, it is best to consult on all issues of interest with a doctor.
Rate article
(Number of votes: 6, average 4.2)
Go back
2nd trimester of pregnancy: what happens to the fetus
2nd trimester of pregnancy: what happens to the fetus - Private maternity hospital Ekaterininskaya Clinics Most women enjoy the 2nd trimester of pregnancy more than the first, with the disappearance of morning sickness, breast tenderness and fatigue. But be prepared for some other symptoms to appear!
But be prepared for some other symptoms to appear!
- Pain. As a result of stretching of the tissues of the body, you may experience pain in the sides and under the abdomen. Weight gain can cause back pain and leg cramps. The doctor will advise you on simple exercises for such cases. nine0074
- Stuffy nose. Increased hormone levels can lead to nasal congestion and nosebleeds.
- Soft gums. Your gums tend to bleed, so oral hygiene requires special attention and careful brushing.
- Skin itching. The skin of the abdomen may itch as a result of stretching associated with the growth of the child. Try to use a moisturizer daily to avoid stretch marks. nine0074
- Varicose veins and hemorrhoids. During pregnancy, you will be more susceptible to varicose veins and hemorrhoids. Try not to stand or sit for too long, and avoid crossing your legs while sitting. If discomfort or pain occurs in the anus, the doctor may prescribe a remedy for hemorrhoids.
- Vaginal discharge. A white, thin vaginal discharge called leucorrhea is normal during this period of pregnancy. These secretions help keep the vagina healthy. If you find discharge of a different type or color, contact your doctor for advice. nine0074
- Impaired skin pigmentation. Pregnancy hormones may contribute to the appearance of dark spots on the face and abdomen. The sun can exacerbate the appearance of spots, so use sunscreen when you go outside. Sun exposure without skin protection is contraindicated!
- Shortness of breath. As your lungs allow more oxygen to meet your baby's needs, you may experience shortness of breath or a faster rate of breathing.
- Increased appetite. As your child grows, you may feel hungry all the time, but there is no need to "eat for two". If you need to snack, choose healthy foods like fruit or yogurt.
2nd trimester milestones
- You may feel your baby move for the first time around 18-20 weeks of pregnancy.
 This phenomenon is called "revival" and is initially felt as a flutter in the abdomen.
This phenomenon is called "revival" and is initially felt as a flutter in the abdomen. - As your baby grows, your belly will grow. nine0074
2nd trimester baby development
End of 2nd trimester:
- Your baby moves and responds to touch and sound.
- Eyelids begin to open, eyebrows and eyelashes are visible.
- The skin is covered with fine, downy hairs and a creamy white substance called primordial lubrication.
- Swallowing and sucking reflexes develop.
- Hair began to grow on the head.
- Fingerprint lines have formed on the fingers. nine0074
- Baby measures about 23 cm from head to lower torso.
Mobile application of the clinic
You can make an appointment with a doctor, get tests
and much more...
Fill out the form to make an appointment or order a call back
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.