Easing contraction pain
Dealing With Pain During Childbirth (for Parents)
Learning all you can about labor and delivery is one of the best ways to help you manage the pain of childbirth when the time comes.
Pain During Labor and Delivery
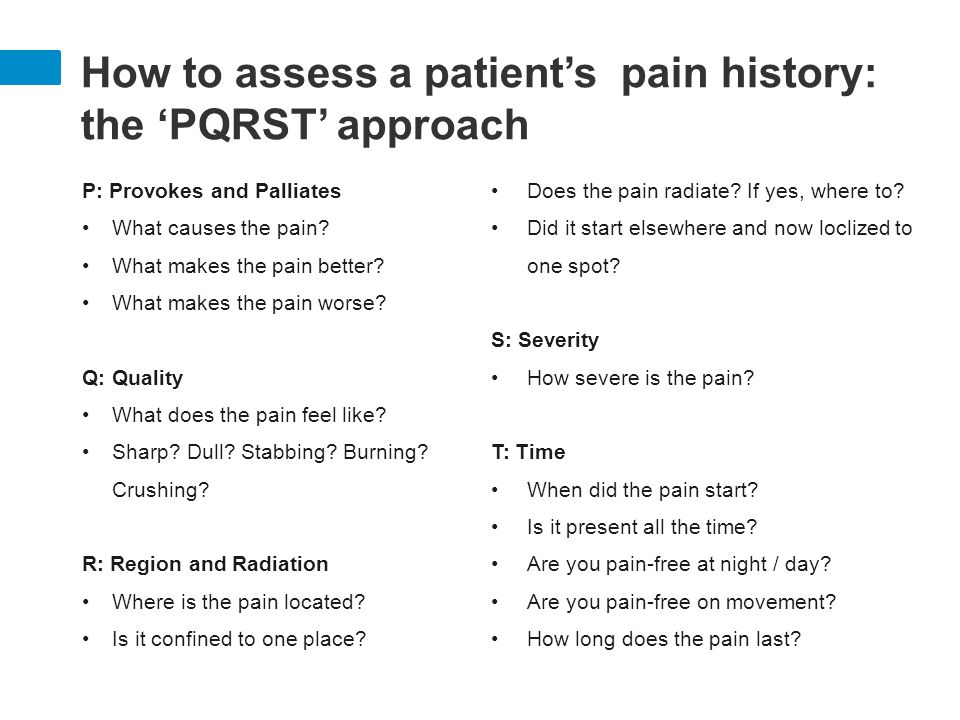
Pain during labor is caused by contractions of the muscles of the uterus and by pressure on the cervix. This pain can be felt as strong cramping in the abdomen, groin, and back, as well as an achy feeling. Some women experience pain in their sides or thighs as well.
Other causes of pain during labor include pressure on the bladder and bowels by the baby's head and the stretching of the birth canal and vagina.
Pain during labor is different for every woman. It varies widely from woman to woman and even from pregnancy to pregnancy.
It's often not the pain of each contraction on its own that women find the hardest, but the fact that the contractions keep coming — and that as labor progresses, there is less and less time between contractions to relax.
Preparing Yourself
To help with pain during labor, here are some things you can start doing before or during your pregnancy:
Regular and reasonable exercise (that your doctor says is OK) can help strengthen your muscles and prepare your body for the stress of labor. Exercise also can increase your endurance, which will come in handy if you have a long labor. The important thing to remember with any exercise is not to overdo it — and this is especially true if you're pregnant. Talk to your doctor about what he or she considers to be a safe exercise plan for you.
If you and your partner attend childbirth classes, you'll learn different techniques for handling pain, from visualization to stretches designed to strengthen the muscles that support your uterus. The two most common childbirth philosophies in the United States are the Lamaze technique and the Bradley method.
The Lamaze technique is the most widely used method in the United States. The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
The Bradley method (also called Husband-Coached Birth) emphasizes a natural approach to birth and the active participation of the baby's father as birth coach. A major goal of this method is the avoidance of medicines unless absolutely necessary. The Bradley method also focuses on good nutrition and exercise during pregnancy and relaxation and deep-breathing techniques as a method of coping with labor. Although the Bradley method advocates a medicine-free birth experience, the classes do discuss unexpected complications or situations, like emergency cesarean sections.
Medicine-free ways to handle pain during labor include:
- hypnosis
- yoga
- meditation
- walking
- massage or counterpressure
- changing position
- taking a bath or shower
- listening to music
- distracting yourself by counting or performing an activity that keeps your mind otherwise occupied
Pain Medicines
A variety of pain medicines can be used during labor and delivery, depending on the situation. Many women rely on such medicines, and it can be a huge relief when pain is quickly eased and energy can be focused on getting through the contractions. Talk to your health care provider about the risks and benefits of each type of medicine.
Analgesics. Analgesics ease pain, but don't numb it completely. They don’t affect sensation or muscle movement. They can be given many ways. If they are given intravenously (through an IV into a vein) or through a shot into a muscle, they can affect the whole body. These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
Regional anesthesia. This is what most women think of when they consider pain medicine during labor. By blocking the feeling from specific regions of the body, these methods can be used for pain relief in both vaginal and cesarean section deliveries.
Epidurals, a form of local anesthesia, relieve most of the pain from the entire body below the belly button, including the vaginal walls, during labor and delivery. An epidural involves medicine given by an anesthesiologist through a thin, tube-like catheter that's inserted in the woman's lower back. The amount of medicine can be increased or decreased according to a woman's needs. Very little medicine reaches the baby, so usually there are no effects on the baby from this method of pain relief.
Epidurals do have some drawbacks — they can cause a woman's blood pressure to drop and can make it difficult to pee. They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
Tranquilizers. These drugs don't relieve pain, but they may help to calm and relax women who are very anxious. Sometimes they are used along with analgesics. These drugs can have effects on both the mother and baby, and are not often used. They also can make it difficult for women to remember the details of the birth. Discuss the risks of tranquilizers with your doctor.
Natural Childbirth
Some women choose to give birth using no medicine at all, relying instead on relaxation techniques and controlled breathing for pain. If you'd like to experience childbirth without pain medicine, discuss this with your health care provider.
Things to Consider
Here are some things to think about when considering pain control during labor:
- Medicines can relieve much of your pain, but probably won't relieve all of it.
- Labor may hurt more than you expected. Some women who had said they want no pain medicine whatsoever end up changing their minds when they're actually in labor.
- Some medicines can affect your baby, making the baby drowsy or causing changes in the heart rate.
Talking to Your Health Care Provider
You'll want to review your pain control options with the person who'll be delivering your baby. Find out what's available, how effective they're likely to be, and when it's best not to use some medicines.
If you want to use pain-control methods other than medicine, make sure your health care provider and the hospital staff know. You might want to also consider writing a birth plan that makes your preferences clear.
Remember, many women make decisions about pain relief that they abandon — often for very good reason — at the last minute. Your ability to endure the pain of childbirth has nothing to do with your worth as a mother. By preparing and educating yourself, you can be ready to decide what pain management works best for you.
Ouch! Managing Labor Pains
We’ve all seen those movie scenes when a woman in a wheelchair is being rushed through the hospital doors after her water breaks. Cut to the mother-to-be screaming at the top of her lungs while pushing the baby out. Then, the money shot of the new parents staring adoringly at their newborn. But in real life, childbirth can take a lot longer than a few minutes of edited screen time, and there are a variety of ways to manage the pain that comes with bringing a baby into the world.
Erica Vu, certified nurse midwife at UC San Diego Health, talks about the stages of labor, the pain associated with the process and the interventions — both medicated and non-medicated — that are available.
How does a pregnant woman know when she is in labor?
Labor is very mysterious and one can never exactly know when it will start. Most women start to have various labor signs a few hours or weeks even before labor officially begins. These may include:
- Increased vaginal discharge — brown, pink or increased mucous discharge in general is a good sign the cervix is starting to ripen and the mucous plug, the sealed entrance to the uterus, is released.
- Many women notice more pelvis pressure as the baby’s head descends in her pelvis. Some call this “lightening” and it can happen weeks before or just as labor is starting.
- Some women start to have more nausea and loose stools or even diarrhea as the body is preparing for labor.
- The most common sign of labor is the increase in cramping associated with abdomen tightening or Braxton hicks. These early contractions usually start in the lower abdomen/pubic area and radiate towards the lower back. The frequency and duration of these start to increase and become more regular and rhythmic. At times, these contractions can start and increase rapidly, but for most, this can take several hours or even several days. We time the contractions from the start of one to the start of the next contraction. When they are still irregular and more than five minutes apart, most women are still in the cervical ripening/very early labor stage. These irregular contractions may even slow down or stop to give the mom’s a break.
 When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
What are the stages of labor and the pain associated with each stage?
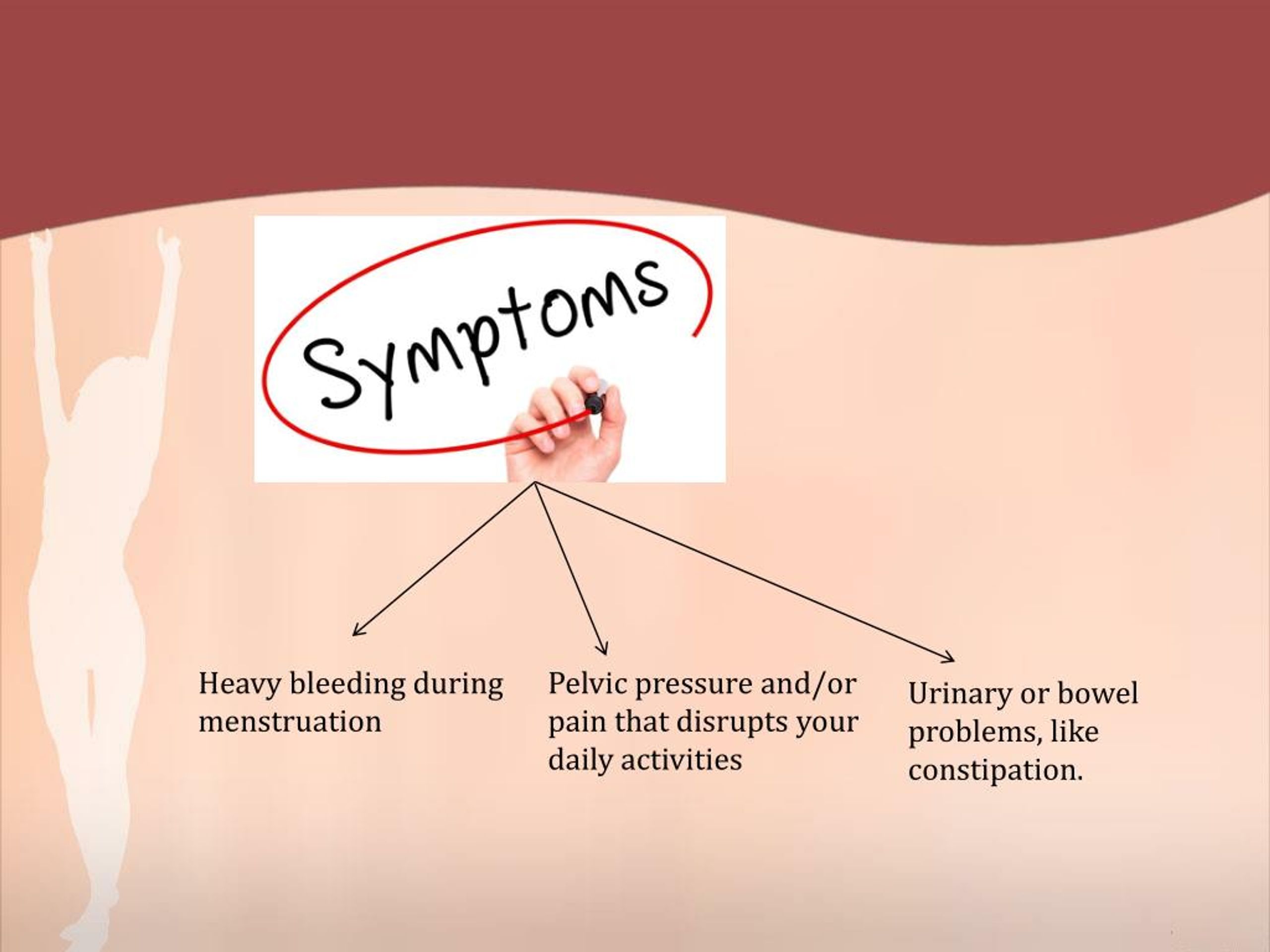
The first stage of labor is cervical dilation, or the opening of the cervix, from 0 to 10 centimeters. Early labor is when the cervix starts to dilate from closed to five centimeters with regular contractions. Early labor contractions tend to be a bit shorter in duration (60 seconds or less) and more menstrual like-cramping in the lower abdomen and back. Early labor can take several hours or even a day or more.
When the contractions intensify, include the upper abdomen and are around two to three minutes apart, active labor is most likely starting, which is the stage from 6 to 10 centimeters. Active labor contractions are a lot stronger, longer (one to two minutes in duration) and almost always necessitate more focus, breathing and position changes/labor support. Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Once women get to 10 centimeters, the second stage of labor starts and pushing begins until the baby is delivered. This can take minutes to hours depending on the baby’s position, maternal effort and anesthesia interventions.
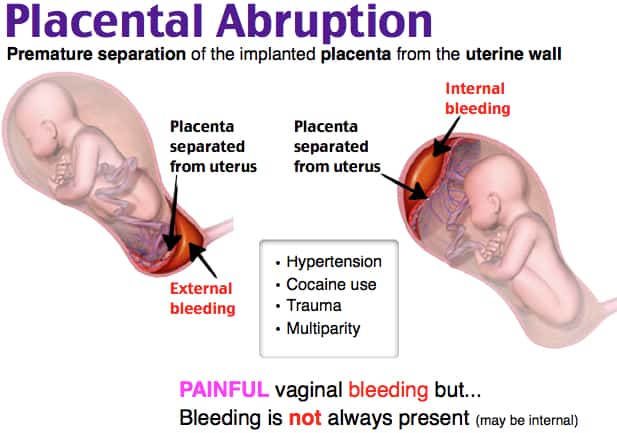
The third stage of labor is when the baby is out and the placenta is delivered.
What type of non-medicated interventions does UC San Diego Health provide for labor pain?
Still of Katherine Heigl and Seth Rogen from Universal Picture's Knocked Up.
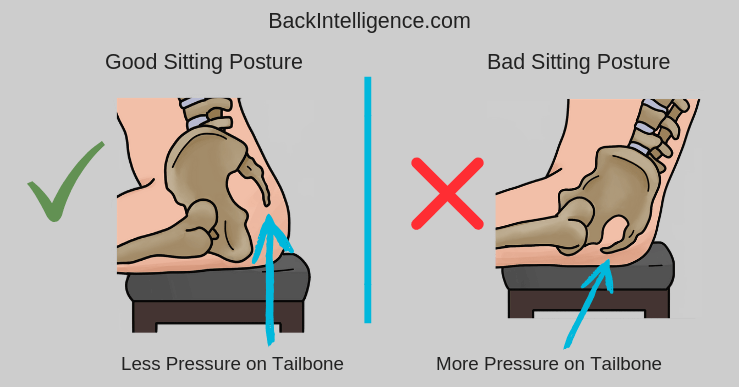
Multiple position changes: Walking, lunges, squats, birthing balls, birthing stools and using Rebozos (a fabric shawl originally from Mexico that when placed appropriately can help to lift lower abdomen weight off the pubic bone, squeeze hips with back labor or help during the pushing stage by pulling on the fabric in different positions both sitting, squatting or standing). All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
Doulas: Women can hire private doulas or ask for one of our volunteer Hearts & Hands Program. Doulas are beneficial in so many ways, but specifically they give continuous non-medical labor support, including help with breathing techniques, counter pressure, position changes and massage and can be an advocate for your preference of labor process and birth.
Hydrotherapy (Labor tubs): Buoyancy can help with freedom of movement during contractions. Warm water helps to relax between contractions, eases body aches, including back aces, improves circulation and is a safe and effective form of pain relief.
Showers: Warm water helps with relaxation and decreases maternal tension during the peak of the contractions.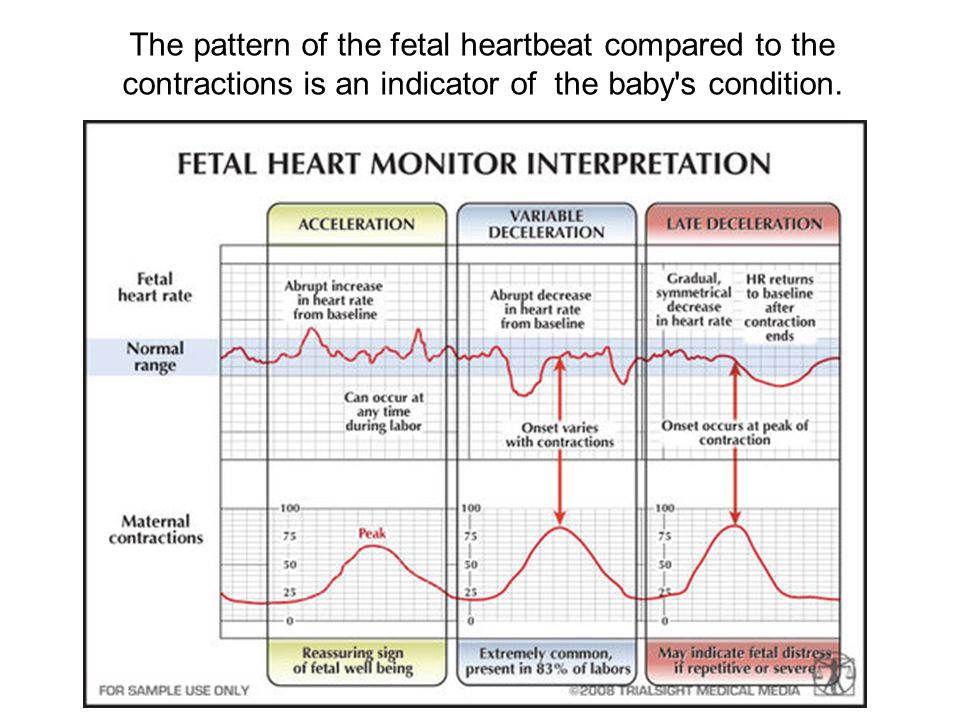 Partners are invited to join to help with support.
Partners are invited to join to help with support.
Waterproof Wireless Monitors: These allow laboring women to be in the shower for pain relief while still allowing the benefits of hydrotherapy and close monitoring of the baby. The wireless monitors also allow women to change positions easily and walk freely about in their rooms or down the hallways if they so desire.
What type of medicated interventions does UC San Diego Health provide for labor pain?
Nitrous Oxide: Nitrous is a gas women breathe in through a mask during contractions. Women are still aware of the contractions, but the nitrous helps to decrease anxiety during them. Some women may experience nausea or dizziness initially but that usually resolves in a few minutes. This intervention allows freedom of movement, such as standing or sitting on a birthing ball, to help the baby descend down the birthing canal. Women can use nitrous as the only form of pain relief or it can also be used as a bridge to other forms of pain relief as labor progresses. It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
Intravenous Pain Relief: Narcotics or opioids help to relax the mind and body during the peak of the contractions. These help to decrease the sensations of pain, and depending on the stage of labor, may even allow the woman to rest and sleep a bit. It does cross over to the baby through the placenta but in time, just like the mother, it wears off and has little side effects. Some women feel initial dizziness and nausea as well but that often resolves with time. We often combine the narcotic with an anti-emetic (anti-nausea) medication to help but also to prolong the duration of the pain relief. There are different types of narcotics used for different stages of labor to decrease side effects in the newborn in case of a quick delivery.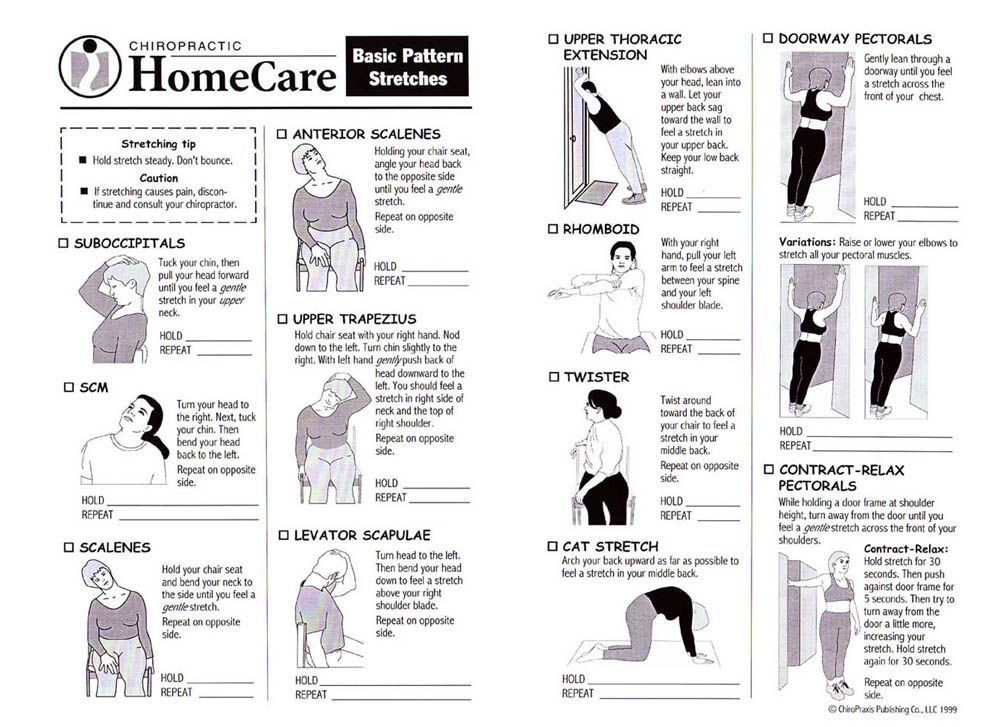
Regional Anesthesia (Epidurals): This is a pain relief method that decreases pain sensations from the abdomen and below by placing a small tube into in an area surrounding the spinal cord in the lower back and is connected to a pump. The medicine is continuously infusing during the course of labor while women remain awake and alert. Most women do not feel the majority of the pain sensations of contractions, but some will feel the pressure of the baby descending in the pelvis, which helps women to push when ready. Women are not allowed to walk with epidurals but are able to change positions in bed.
Learn more about labor pain management options at UC San Diego Health.
About UC San Diego Health Midwives
To learn more about the featured medical specialties, please visit:
- Pregnancy and Birth Care
Cramping pains in the abdomen - causes
Cramping pains in the abdomen - unpleasant acute, sudden pain in various parts of the abdomen, which can be associated with a large number of diseases, not only of the gastrointestinal tract, but also of other organ systems.
Most often, this condition is associated with spasms in the biliary system, stomach, and intestines.
"Symptoms of anxiety": if the cramping pain in the abdomen is of high intensity, accompanied by fever, chills, nausea, vomiting, severe bloating in the abdomen, constipation or diarrhea, blood in the stool, tension in the anterior abdominal wall, sharp pain when lightly touching the abdomen or pushing the bed - you should immediately consult a doctor, as an examination of the abdomen, blood tests, ultrasound examination (ultrasound) of the abdominal cavity and, possibly, other studies to rule out acute surgical and other serious pathology. nine0005
Causes of cramping pain in the right side of the abdomen:
- acute appendicitis
-
diseases of the stomach and duodenum (acute erosive gastroduodenitis, peptic ulcer, stomach cancer)
-
diseases of the liver and biliary system (acute cholecystitis, cholelithiasis and biliary colic, biliary dyskinesia with spasm of the gallbladder and bile duct sphincters, abscess, liver cancer)
-
bowel diseases (acute infectious enterocolitis, intestinal obstruction, strangulated hernia of the anterior abdominal wall, Crohn's disease, ulcerative colitis, diverticulitis, intestinal cancer)
-
damage to the vessels of the abdominal cavity (dissecting aortic aneurysm, thrombosis and embolism of intestinal vessels, hepatic veins, portal vein, thrombosis of the right renal artery)
-
diseases of the urinary system (urolithiasis and renal colic, cancer of the right kidney)
-
diseases of the genital organs (acute right-sided adnexitis, ovarian cyst, ectopic pregnancy, dysmenorrhea, acute prostatitis)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
-
diseases of the chest organs (lower lobe right-sided pneumonia, pleurisy, pneumothorax, acute myocardial infarction, pulmonary embolism)
-
diseases of the endocrine system (diabetic ketoacidosis)
-
rare diseases (acute intermittent porphyria, lead colic, periodic illness)
Causes of cramping pain in the left side of the abdomen:
- diseases of the pancreas (acute pancreatitis, cancer)
-
diseases of the stomach (acute erosive gastritis, peptic ulcer, stomach cancer)
-
bowel diseases (acute infectious enterocolitis, intestinal obstruction, strangulated hernia of the anterior abdominal wall, Crohn's disease, ulcerative colitis, diverticulitis, intestinal cancer, Makelia-Dvorkin-Biehl syndrome (splenic flexure syndrome of the large intestine with severe accumulation of gases)
-
diseases of the spleen (splenomegaly in blood diseases, infectious diseases, cirrhosis of the liver; cysts, tumors, abscess, rupture, perisplenitis, impaired blood supply - spleen infarction)
-
damage to the vessels of the abdominal cavity (dissecting aneurysm of the aorta, thrombosis and embolism of the intestinal vessels, thrombosis of the splenic vein, left renal artery)
-
diseases of the urinary system (urolithiasis and renal colic, cancer of the left kidney)
-
diseases of the genital organs (acute left-sided adnexitis, ovarian cyst, ectopic pregnancy, dysmenorrhea, acute prostatitis)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
Causes of epigastric cramping pain:
- acute appendicitis (at the beginning of the disease)
-
diseases of the stomach (acute gastritis, gastric ulcer, cancer)
-
hiatal hernia (strangulation)
nine0019 -
diseases of the biliary system (acute cholecystitis, cholelithiasis and biliary colic, biliary dyskinesia with gallbladder spasm)
-
bowel diseases (irritable bowel syndrome)
-
abdominal vascular disease (dissecting aortic aneurysm, thrombosis and embolism)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
-
heart disease (acute myocardial infarction)
diseases of the pancreas (acute pancreatitis, cysts, cancer)
In our center we are engaged in determining the cause of cramping pain in the abdomen, conducting an examination and differential diagnosis of this condition.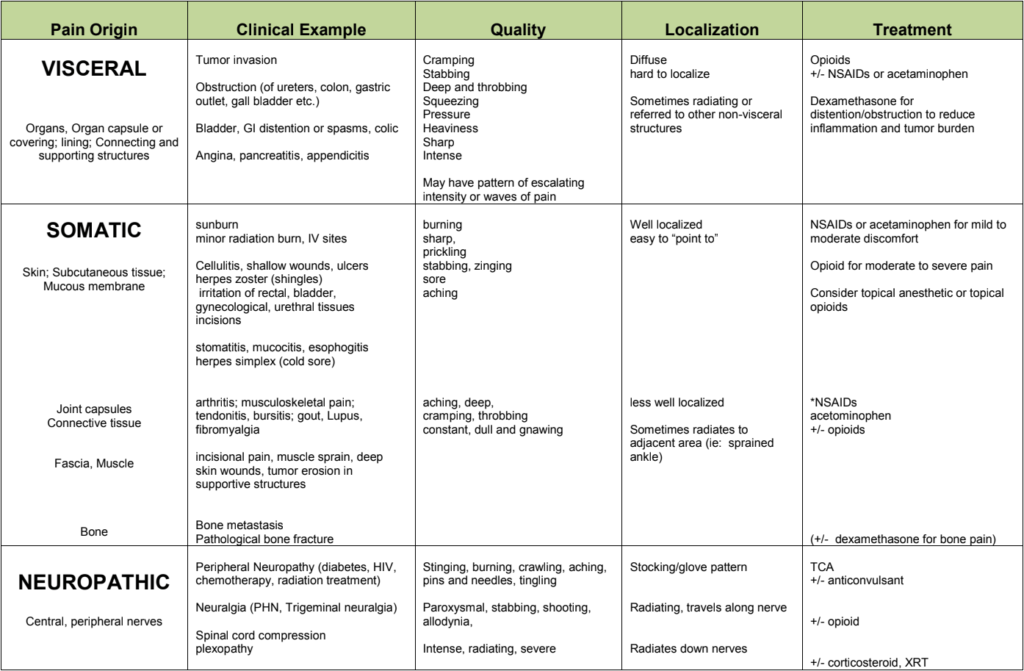 Experienced medical specialists (gastroenterologist, surgeon, neurologist, endocrinologist, psychotherapist), as well as the opportunity to be examined using expert-class equipment (ultrasound, videogastroduodenoscopy, colonoscopy) will help to deal with this problem. nine0005
Experienced medical specialists (gastroenterologist, surgeon, neurologist, endocrinologist, psychotherapist), as well as the opportunity to be examined using expert-class equipment (ultrasound, videogastroduodenoscopy, colonoscopy) will help to deal with this problem. nine0005
Intestinal spasm. What is Intestinal Spasm?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Intestinal spasm is a symptom of a wide variety of digestive tract diseases, characterized by high-intensity visceral pain associated with significant contraction of the intestinal wall. The main symptom of intestinal colic is cramping pain, usually combined with other symptoms of the underlying disease. To determine the cause of this condition, various laboratory, x-ray, ultrasound and instrumental research methods may be required.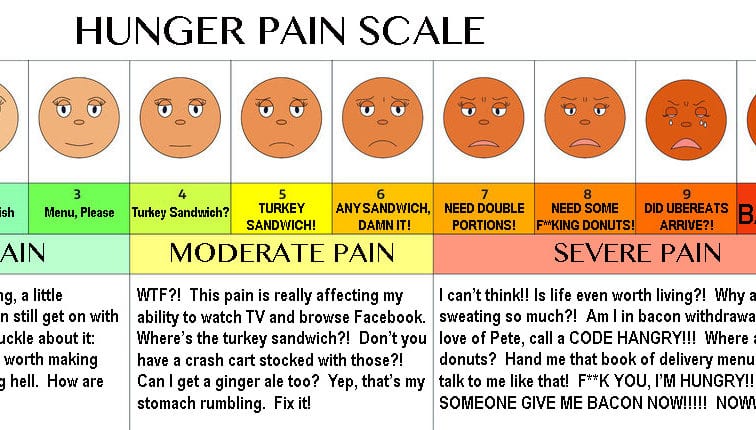 Treatment of intestinal spasm is conservative: sedatives, antispasmodics, heat on the abdomen, antidiarrheals and a special diet. nine0005
Treatment of intestinal spasm is conservative: sedatives, antispasmodics, heat on the abdomen, antidiarrheals and a special diet. nine0005
- Causes of intestinal spasm
- Symptoms of intestinal spasm
- Diagnosis of intestinal spasm
- Treatment of intestinal spasm
- Prognosis and prevention of intestinal spasm
- Treatment prices
General
Intestinal spasm is not an independent nosological unit, but only serves as a sign of serious malfunctions in the gastrointestinal tract. Most often, this functional disorder of the intestine occurs in infancy, but adults often also complain of spasmodic pain in the abdomen. Leading specialists of the country in the field of gastroenterology have been arguing for many years whether to consider such functional disorders (gastroesophageal reflux, functional diarrhea, intestinal spasm, etc.) as simply a symptom of trouble in the digestive tract, or as a premorbid condition, which in the future can be transformed into an organic pathology. There is currently no consensus on the status of functional disorders, but patients should take intestinal colic seriously. Finding out the cause of this condition means preventing the development of serious diseases of the gastrointestinal tract. nine0005
There is currently no consensus on the status of functional disorders, but patients should take intestinal colic seriously. Finding out the cause of this condition means preventing the development of serious diseases of the gastrointestinal tract. nine0005
Intestinal spasm
Causes of intestinal spasm
Cramping pain, characteristic of intestinal spasm, may occur due to violations of various mechanisms of intestinal motility. The main links of pathogenesis in intestinal spasm: overstretching of the intestinal wall, irritation of nerve endings, impaired tone of the smooth muscles of the intestine with a disorder in the mechanisms of its contraction, the occurrence of pathological peristalsis (antiperistalsis, weakening or strengthening of peristaltic waves, the disappearance of peristalsis in some parts of the intestine), the occurrence of an obstacle to promote the food bolus. nine0005
Intestinal spasm can occur against the background of digestive disorders - acute and chronic gastritis, gastric and duodenal ulcers, hepatitis, pancreatitis, etc.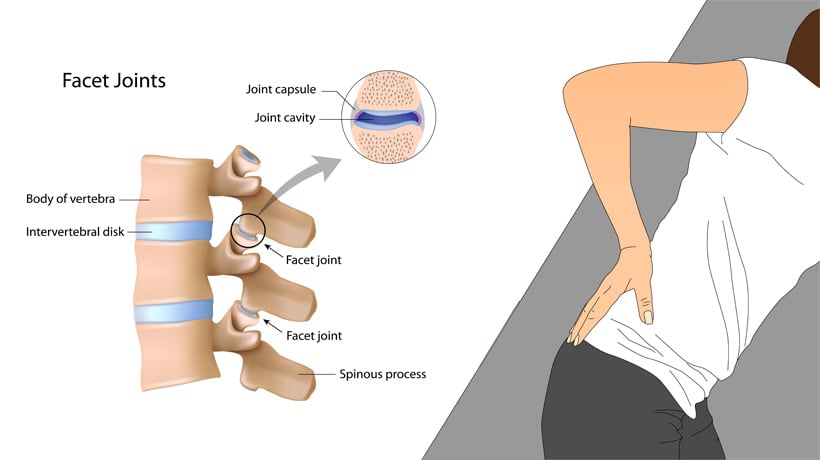 In case of violations of the digestion of food in the stomach and the initial sections of the intestine, the unprocessed food bolus enters the intestine and causes excessive irritation of its receptors, muscle spasm . Another common cause of intestinal spasm is nutritional errors - the mechanism for the development of colic is the same as with digestive disorders, but irritation of the intestinal wall occurs with too cold, spicy, fried, dry, stale food, yeast dough products, etc. nine0005
In case of violations of the digestion of food in the stomach and the initial sections of the intestine, the unprocessed food bolus enters the intestine and causes excessive irritation of its receptors, muscle spasm . Another common cause of intestinal spasm is nutritional errors - the mechanism for the development of colic is the same as with digestive disorders, but irritation of the intestinal wall occurs with too cold, spicy, fried, dry, stale food, yeast dough products, etc. nine0005
Intestinal colic can also develop with intoxication - with generalized viral infections (flu, SARS), poisoning with industrial and vegetable poisons, salts of heavy metals. In these cases, intestinal spasm occurs due to the effects of poisons and toxins on the neuromuscular apparatus of the intestine. Intestinal infections can also be the cause of this pathology: the multiplication of bacteria in the intestinal lumen has a complex effect, causing irritation of nerve endings, excessive exudation with overstretching of the intestinal wall, and peristalsis disorders. nine0005
nine0005
In asthenic people with a labile psyche, prone to strong feelings, often during stressful situations there are cramping pains in the abdomen associated with intestinal spasm. With emotional shocks, there is a violation of the autonomic regulation of intestinal motility.
Intestinal spasm is also characteristic of helminthiases: worms parasitizing in the digestive tube are able to gather into balls and conglomerates that block the lumen of the intestinal tube. In addition, the helminths themselves and their metabolic products irritate the nerve endings in the mucous membrane. nine0005
With intestinal obstruction, spastic contractions of its muscles are also possible. Spasm most often occurs against the background of obturation of the intestine by a tumor, a foreign body, coprolites and gallstones, balls of helminths, bezoars. There are frequent cases of the development of intestinal colic and with adhesive intestinal obstruction that has arisen against the background of inflammatory diseases of the abdominal cavity and small pelvis, surgical interventions, and radiation.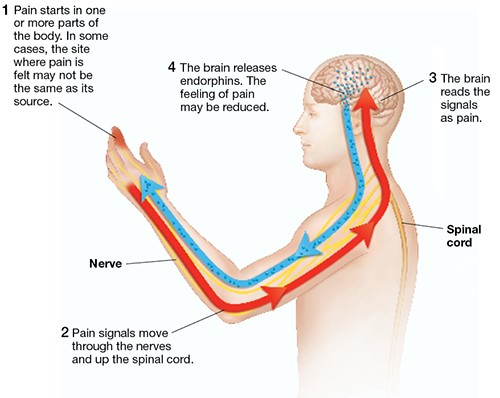 The intestine tries to overcome the obstruction by gradually increasing peristalsis, which eventually leads to spasm. nine0005
The intestine tries to overcome the obstruction by gradually increasing peristalsis, which eventually leads to spasm. nine0005
Depending on the cause and localization of the pathological process, separate types of intestinal spasm are distinguished. The appendicular type develops in the presence of an inflammatory process in the appendix. Usually, some time after appendicular colic, an appendicitis clinic appears. The rectal type is associated with spasm of the rectum and is manifested by frequent strong urge to defecate. The lead type of intestinal spasm accompanies lead poisoning, which is characterized by high fever, tension of the anterior abdominal wall, gray plaque on the gums, and bleeding from the oral cavity. The vascular type is associated with intestinal hypoperfusion against the background of a hypertensive crisis, atherosclerosis, thrombosis of the mesenteric veins, compression of the vessels by a tumor or adhesions. nine0005
Symptoms of intestinal spasm
The only symptom of intestinal spasm is intense cramping pain in the abdomen. Depending on the background of which disease an intestinal spasm occurred, other symptoms may also be recorded.
Depending on the background of which disease an intestinal spasm occurred, other symptoms may also be recorded.
With gastritis, intestinal spasm is accompanied by pain in the epigastrium, nausea, vomiting, dyspeptic symptoms, loss of appetite and weight loss. With peptic ulcer of the stomach and duodenum, the pain becomes more intense, occurs on an empty stomach and at night. Intestinal spasm in liver pathology is combined with pain in the right side and hepatic colic, vomiting of bile, yellowness of the skin and mucous membranes, skin itching. In diseases of the pancreas, intestinal spasm joins girdle pain in the abdomen, indomitable vomiting, flatulence and diarrhea. nine0005
Intestinal infections usually manifest with fever, nausea and vomiting, and then, against the background of diarrhea, intestinal spasm also joins the symptoms. At the same time, pathological impurities (mucus, blood) are visualized in the feces. The clinic of helminthiases often develops gradually, and intestinal spasms may be the only clinical signs for a long time. In addition, the patient complains of weakness, lethargy, decreased performance, skin rashes and itching in the anus. With intestinal obstruction in the early stages, the patient is disturbed by severe intestinal spasms, the intensity of which gradually decreases. Colic occurs against the background of the absence of discharge of gases and feces, repeated indomitable vomiting. The abdomen swells, peristalsis disappears. If you do not help the patient during the day, irreversible changes occur in the intestinal wall. nine0005
In addition, the patient complains of weakness, lethargy, decreased performance, skin rashes and itching in the anus. With intestinal obstruction in the early stages, the patient is disturbed by severe intestinal spasms, the intensity of which gradually decreases. Colic occurs against the background of the absence of discharge of gases and feces, repeated indomitable vomiting. The abdomen swells, peristalsis disappears. If you do not help the patient during the day, irreversible changes occur in the intestinal wall. nine0005
Diagnosis of intestinal spasm
Most often, when an intestinal spasm occurs, the patient seeks the advice of a gastroenterologist or therapist. These specialists carefully study the anamnesis, accompanying complaints and, if necessary, prescribe a consultation with the surgeon.
To identify the underlying disease that could lead to the development of intestinal spasm, a number of laboratory and instrumental studies are carried out. A general blood test can reveal anemia, inflammatory changes in the leukoformula. A general urine test will indicate a catastrophe in the small pelvis (pelvioperitonitis), metabolic disorders of bile acids and glucose. A biochemical blood test is an indicator of the state of the liver, pancreas, and kidneys. To exclude intestinal pathology, a coprogram and a fecal occult blood test are examined. nine0005
A general blood test can reveal anemia, inflammatory changes in the leukoformula. A general urine test will indicate a catastrophe in the small pelvis (pelvioperitonitis), metabolic disorders of bile acids and glucose. A biochemical blood test is an indicator of the state of the liver, pancreas, and kidneys. To exclude intestinal pathology, a coprogram and a fecal occult blood test are examined. nine0005
To detect organic pathology of the internal organs, it may be necessary to perform ultrasound, plain radiography (including contrast), computed tomography or MSCT of the abdominal organs.
Quite often, to establish the exact causes of intestinal spasm, consultation with an endoscopist is required. Esophagogastroduodenoscopy, colonoscopy and sigmoidoscopy allow visualizing changes in the mucous membrane of different parts of the intestine and identifying the exact cause of the pathological condition. nine0005
Treatment of intestinal spasm
Prior to the arrival of ambulance workers, one should not independently stop intestinal spasm with painkillers and antispasmodics, a warm heating pad, enemas.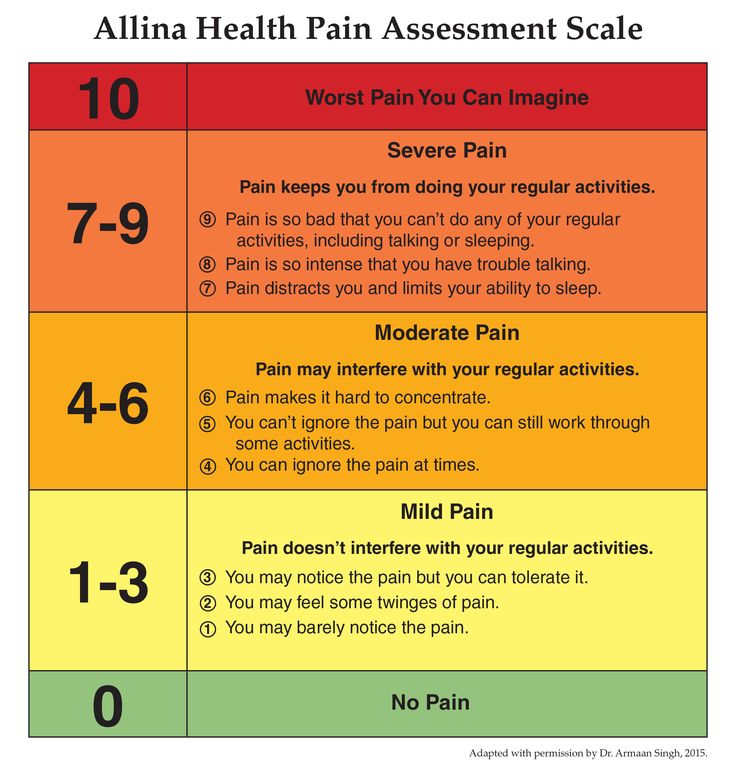 Only a doctor will be able to correctly assess the identified symptoms and exclude such serious diseases as acute appendicitis, peritonitis, intestinal obstruction. Self-treatment of intestinal spasms can lead to lubrication of symptoms, diagnostic errors and delay in therapeutic measures. nine0005
Only a doctor will be able to correctly assess the identified symptoms and exclude such serious diseases as acute appendicitis, peritonitis, intestinal obstruction. Self-treatment of intestinal spasms can lead to lubrication of symptoms, diagnostic errors and delay in therapeutic measures. nine0005
After acute surgical pathology has been excluded, pathogenetic treatment is prescribed. If intestinal spasm has developed against the background of emotional stress, or the appearance of this symptom has led to increased patient nervousness, sedatives are prescribed. Drotaverine and belladonna preparations relax the smooth muscles of the internal organs, eliminating intestinal spasm. A warm heating pad on the abdomen has a similar effect. With increased gas formation, a diet is prescribed (therapeutic fasting for 12 hours, then foods that lead to increased gas formation are excluded), enemas to remove feces and gases. If intestinal spasm occurs against the background of diarrhea, it is recommended to take smectite and other antidiarrheal agents.