How to help with contractions pain
Dealing With Pain During Childbirth (for Parents)
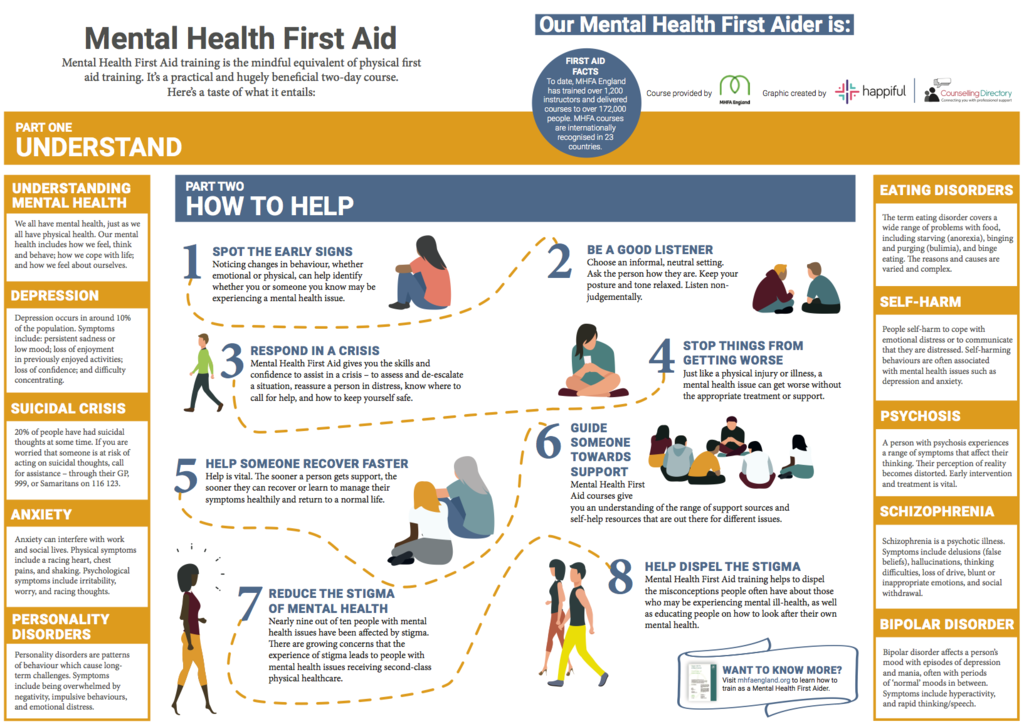
Learning all you can about labor and delivery is one of the best ways to help you manage the pain of childbirth when the time comes.
Pain During Labor and Delivery
Pain during labor is caused by contractions of the muscles of the uterus and by pressure on the cervix. This pain can be felt as strong cramping in the abdomen, groin, and back, as well as an achy feeling. Some women experience pain in their sides or thighs as well.
Other causes of pain during labor include pressure on the bladder and bowels by the baby's head and the stretching of the birth canal and vagina.
Pain during labor is different for every woman. It varies widely from woman to woman and even from pregnancy to pregnancy.
It's often not the pain of each contraction on its own that women find the hardest, but the fact that the contractions keep coming — and that as labor progresses, there is less and less time between contractions to relax.
Preparing Yourself
To help with pain during labor, here are some things you can start doing before or during your pregnancy:
Regular and reasonable exercise (that your doctor says is OK) can help strengthen your muscles and prepare your body for the stress of labor. Exercise also can increase your endurance, which will come in handy if you have a long labor. The important thing to remember with any exercise is not to overdo it — and this is especially true if you're pregnant. Talk to your doctor about what he or she considers to be a safe exercise plan for you.
If you and your partner attend childbirth classes, you'll learn different techniques for handling pain, from visualization to stretches designed to strengthen the muscles that support your uterus. The two most common childbirth philosophies in the United States are the Lamaze technique and the Bradley method.
The Lamaze technique is the most widely used method in the United States. The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
The Bradley method (also called Husband-Coached Birth) emphasizes a natural approach to birth and the active participation of the baby's father as birth coach. A major goal of this method is the avoidance of medicines unless absolutely necessary. The Bradley method also focuses on good nutrition and exercise during pregnancy and relaxation and deep-breathing techniques as a method of coping with labor. Although the Bradley method advocates a medicine-free birth experience, the classes do discuss unexpected complications or situations, like emergency cesarean sections.
Medicine-free ways to handle pain during labor include:
- hypnosis
- yoga
- meditation
- walking
- massage or counterpressure
- changing position
- taking a bath or shower
- listening to music
- distracting yourself by counting or performing an activity that keeps your mind otherwise occupied
Pain Medicines
A variety of pain medicines can be used during labor and delivery, depending on the situation. Many women rely on such medicines, and it can be a huge relief when pain is quickly eased and energy can be focused on getting through the contractions. Talk to your health care provider about the risks and benefits of each type of medicine.
Analgesics. Analgesics ease pain, but don't numb it completely. They don’t affect sensation or muscle movement. They can be given many ways. If they are given intravenously (through an IV into a vein) or through a shot into a muscle, they can affect the whole body.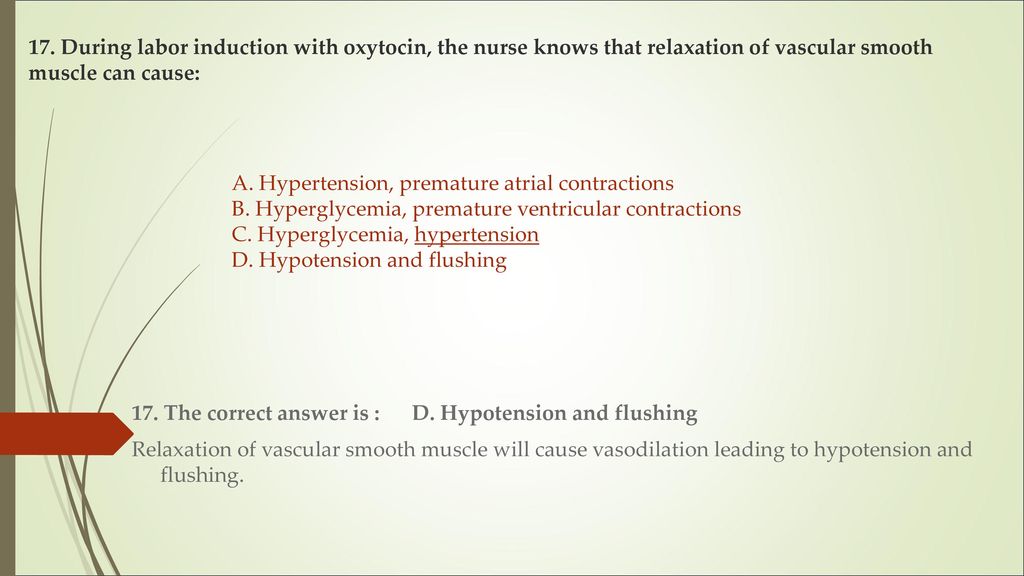 These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
Regional anesthesia. This is what most women think of when they consider pain medicine during labor. By blocking the feeling from specific regions of the body, these methods can be used for pain relief in both vaginal and cesarean section deliveries.
Epidurals, a form of local anesthesia, relieve most of the pain from the entire body below the belly button, including the vaginal walls, during labor and delivery. An epidural involves medicine given by an anesthesiologist through a thin, tube-like catheter that's inserted in the woman's lower back. The amount of medicine can be increased or decreased according to a woman's needs. Very little medicine reaches the baby, so usually there are no effects on the baby from this method of pain relief.
Epidurals do have some drawbacks — they can cause a woman's blood pressure to drop and can make it difficult to pee.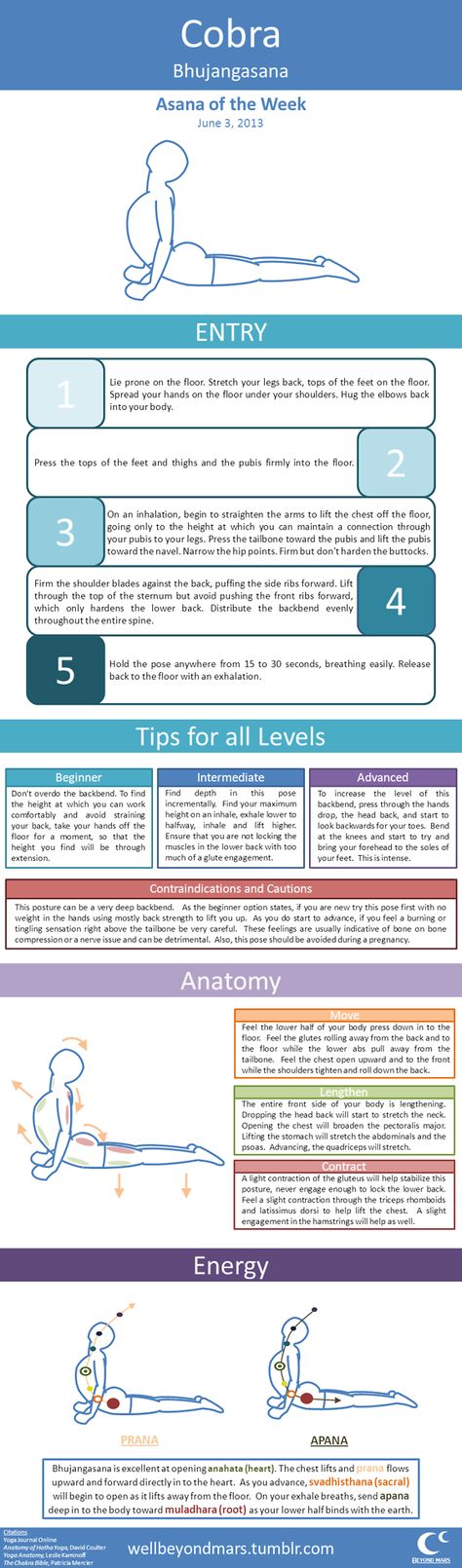 They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
Tranquilizers. These drugs don't relieve pain, but they may help to calm and relax women who are very anxious. Sometimes they are used along with analgesics. These drugs can have effects on both the mother and baby, and are not often used. They also can make it difficult for women to remember the details of the birth. Discuss the risks of tranquilizers with your doctor.
Natural Childbirth
Some women choose to give birth using no medicine at all, relying instead on relaxation techniques and controlled breathing for pain. If you'd like to experience childbirth without pain medicine, discuss this with your health care provider.
Things to Consider
Here are some things to think about when considering pain control during labor:
- Medicines can relieve much of your pain, but probably won't relieve all of it.

- Labor may hurt more than you expected. Some women who had said they want no pain medicine whatsoever end up changing their minds when they're actually in labor.
- Some medicines can affect your baby, making the baby drowsy or causing changes in the heart rate.
Talking to Your Health Care Provider
You'll want to review your pain control options with the person who'll be delivering your baby. Find out what's available, how effective they're likely to be, and when it's best not to use some medicines.
If you want to use pain-control methods other than medicine, make sure your health care provider and the hospital staff know. You might want to also consider writing a birth plan that makes your preferences clear.
Remember, many women make decisions about pain relief that they abandon — often for very good reason — at the last minute. Your ability to endure the pain of childbirth has nothing to do with your worth as a mother. By preparing and educating yourself, you can be ready to decide what pain management works best for you.
Ouch! Managing Labor Pains
We’ve all seen those movie scenes when a woman in a wheelchair is being rushed through the hospital doors after her water breaks. Cut to the mother-to-be screaming at the top of her lungs while pushing the baby out. Then, the money shot of the new parents staring adoringly at their newborn. But in real life, childbirth can take a lot longer than a few minutes of edited screen time, and there are a variety of ways to manage the pain that comes with bringing a baby into the world.
Erica Vu, certified nurse midwife at UC San Diego Health, talks about the stages of labor, the pain associated with the process and the interventions — both medicated and non-medicated — that are available.
How does a pregnant woman know when she is in labor?
Labor is very mysterious and one can never exactly know when it will start. Most women start to have various labor signs a few hours or weeks even before labor officially begins. These may include:
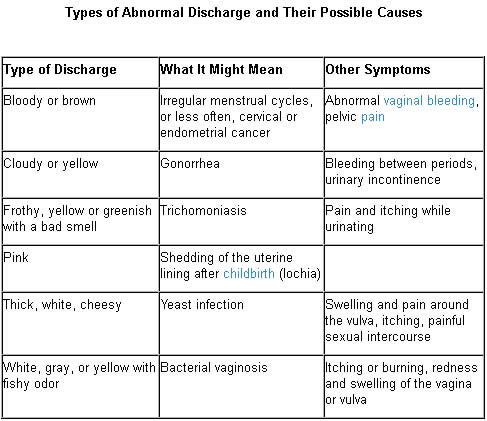
- Increased vaginal discharge — brown, pink or increased mucous discharge in general is a good sign the cervix is starting to ripen and the mucous plug, the sealed entrance to the uterus, is released.
- Many women notice more pelvis pressure as the baby’s head descends in her pelvis. Some call this “lightening” and it can happen weeks before or just as labor is starting.
- Some women start to have more nausea and loose stools or even diarrhea as the body is preparing for labor.
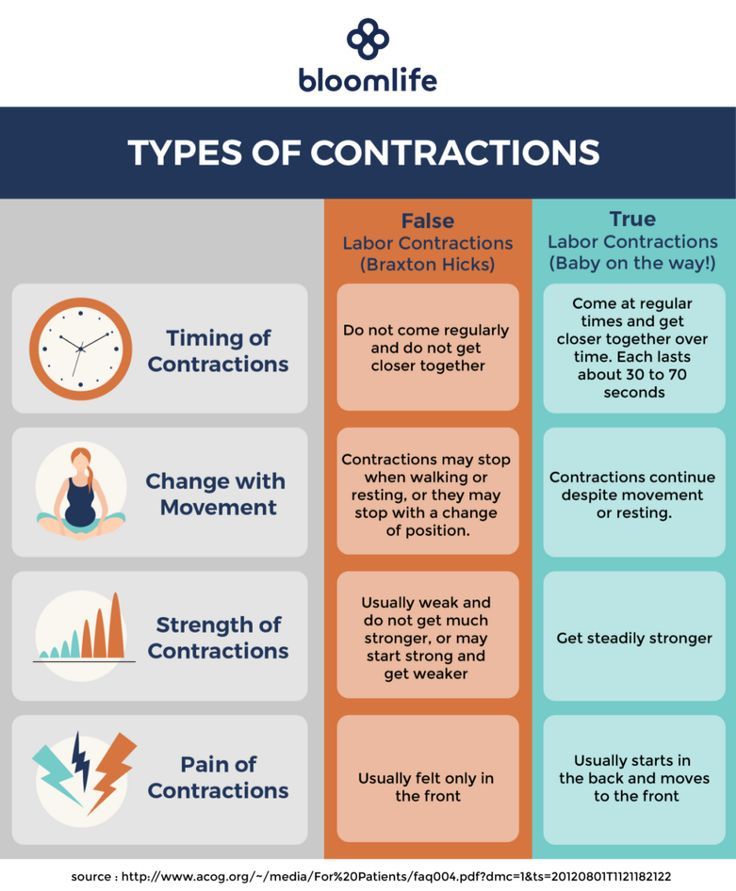
- The most common sign of labor is the increase in cramping associated with abdomen tightening or Braxton hicks. These early contractions usually start in the lower abdomen/pubic area and radiate towards the lower back. The frequency and duration of these start to increase and become more regular and rhythmic. At times, these contractions can start and increase rapidly, but for most, this can take several hours or even several days. We time the contractions from the start of one to the start of the next contraction. When they are still irregular and more than five minutes apart, most women are still in the cervical ripening/very early labor stage. These irregular contractions may even slow down or stop to give the mom’s a break.
 When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
What are the stages of labor and the pain associated with each stage?
The first stage of labor is cervical dilation, or the opening of the cervix, from 0 to 10 centimeters. Early labor is when the cervix starts to dilate from closed to five centimeters with regular contractions. Early labor contractions tend to be a bit shorter in duration (60 seconds or less) and more menstrual like-cramping in the lower abdomen and back. Early labor can take several hours or even a day or more.
When the contractions intensify, include the upper abdomen and are around two to three minutes apart, active labor is most likely starting, which is the stage from 6 to 10 centimeters. Active labor contractions are a lot stronger, longer (one to two minutes in duration) and almost always necessitate more focus, breathing and position changes/labor support. Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Once women get to 10 centimeters, the second stage of labor starts and pushing begins until the baby is delivered. This can take minutes to hours depending on the baby’s position, maternal effort and anesthesia interventions.
The third stage of labor is when the baby is out and the placenta is delivered.
What type of non-medicated interventions does UC San Diego Health provide for labor pain?
Still of Katherine Heigl and Seth Rogen from Universal Picture's Knocked Up.
Multiple position changes: Walking, lunges, squats, birthing balls, birthing stools and using Rebozos (a fabric shawl originally from Mexico that when placed appropriately can help to lift lower abdomen weight off the pubic bone, squeeze hips with back labor or help during the pushing stage by pulling on the fabric in different positions both sitting, squatting or standing). All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
Doulas: Women can hire private doulas or ask for one of our volunteer Hearts & Hands Program. Doulas are beneficial in so many ways, but specifically they give continuous non-medical labor support, including help with breathing techniques, counter pressure, position changes and massage and can be an advocate for your preference of labor process and birth.
Hydrotherapy (Labor tubs): Buoyancy can help with freedom of movement during contractions. Warm water helps to relax between contractions, eases body aches, including back aces, improves circulation and is a safe and effective form of pain relief.
Showers: Warm water helps with relaxation and decreases maternal tension during the peak of the contractions. Partners are invited to join to help with support.
Partners are invited to join to help with support.
Waterproof Wireless Monitors: These allow laboring women to be in the shower for pain relief while still allowing the benefits of hydrotherapy and close monitoring of the baby. The wireless monitors also allow women to change positions easily and walk freely about in their rooms or down the hallways if they so desire.
What type of medicated interventions does UC San Diego Health provide for labor pain?
Nitrous Oxide: Nitrous is a gas women breathe in through a mask during contractions. Women are still aware of the contractions, but the nitrous helps to decrease anxiety during them. Some women may experience nausea or dizziness initially but that usually resolves in a few minutes. This intervention allows freedom of movement, such as standing or sitting on a birthing ball, to help the baby descend down the birthing canal. Women can use nitrous as the only form of pain relief or it can also be used as a bridge to other forms of pain relief as labor progresses.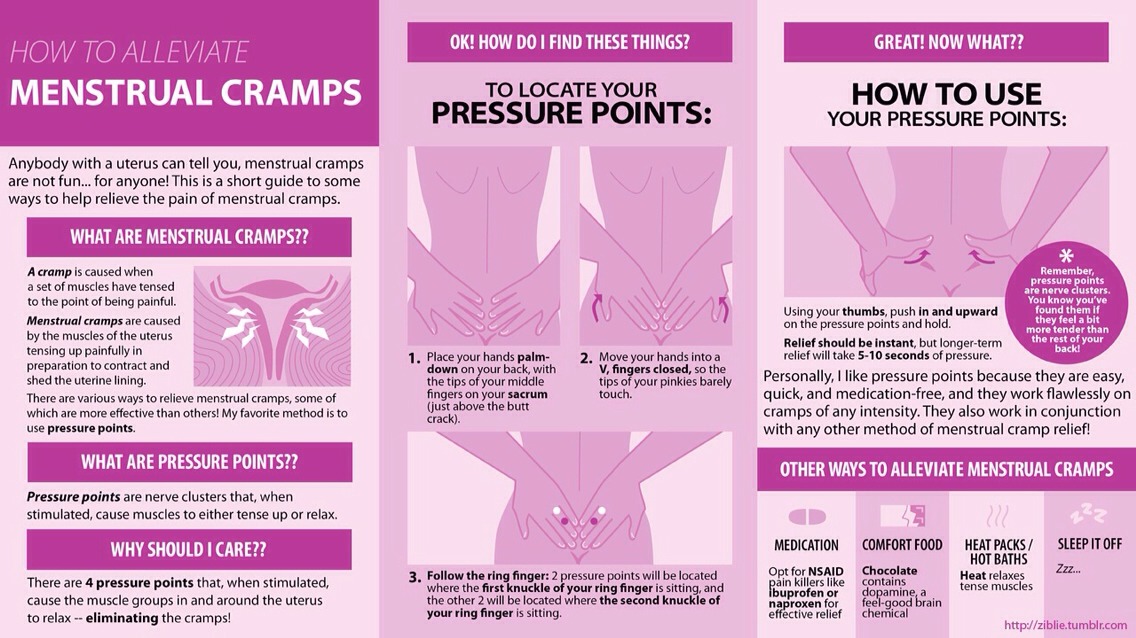 It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
Intravenous Pain Relief: Narcotics or opioids help to relax the mind and body during the peak of the contractions. These help to decrease the sensations of pain, and depending on the stage of labor, may even allow the woman to rest and sleep a bit. It does cross over to the baby through the placenta but in time, just like the mother, it wears off and has little side effects. Some women feel initial dizziness and nausea as well but that often resolves with time. We often combine the narcotic with an anti-emetic (anti-nausea) medication to help but also to prolong the duration of the pain relief. There are different types of narcotics used for different stages of labor to decrease side effects in the newborn in case of a quick delivery.
Regional Anesthesia (Epidurals): This is a pain relief method that decreases pain sensations from the abdomen and below by placing a small tube into in an area surrounding the spinal cord in the lower back and is connected to a pump. The medicine is continuously infusing during the course of labor while women remain awake and alert. Most women do not feel the majority of the pain sensations of contractions, but some will feel the pressure of the baby descending in the pelvis, which helps women to push when ready. Women are not allowed to walk with epidurals but are able to change positions in bed.
Learn more about labor pain management options at UC San Diego Health.
About UC San Diego Health Midwives
To learn more about the featured medical specialties, please visit:
- Pregnancy and Birth Care
How to behave in childbirth? Learning to give birth quickly and with problems
Childbirth is a natural process, laid down by nature. The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
Childbirth is the final and most important stage of pregnancy. How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions. nine0003
1. When is it time to go to the maternity hospital?
Childbirth is a natural result of hormonal changes that occur in your body during the final stages of pregnancy. The sagging belly and heaviness in its lower part and the lumbar region speak of the imminent denouement of the story. Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity. nine0003
nine0003
The signal to call an ambulance should be sufficiently strong contractions that are repeated at regular intervals, the appearance of mucous secretions from the genital tract, slightly stained with blood, or the outflow of amniotic fluid.
2. First stage of childbirth: we breathe for two!
From the moment the contractions become regular, the first stage of labor begins, during which the strength, frequency and duration of uterine spasms increases and the cervix opens. nine0003
During spastic contraction of the uterine muscle fibers, the blood vessels that carry arterial blood to the placenta and fetus are compressed. The fetus begins to experience a lack of oxygen, and this involuntarily makes you breathe deeper. The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
In the first stage of labor, during each contraction, you need to breathe calmly and deeply, trying not to hold your breath while inhaling. At the same time, the air should fill the upper sections of the lungs, as if raising the chest. You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly. nine0003
3. Auto-training in the prenatal ward
To speed up the opening of the cervix, you need to walk more, but sitting is not recommended, while blood flow in the limbs is disturbed and venous blood stagnation occurs in the pelvis. From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby."
4. To relieve pain
Acupressure of the lower back can help relieve pain.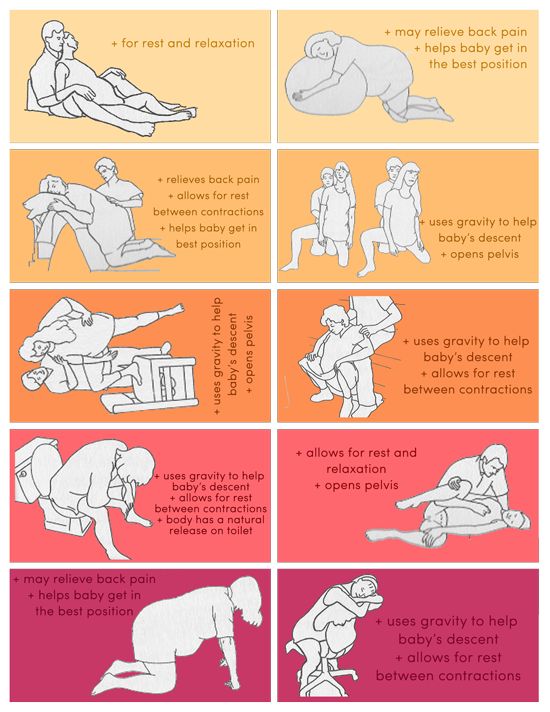 Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Monitor the frequency and duration of contractions and if they weaken or sharply increase, immediately inform your doctor. In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities. nine0003
If dilatation of the cervix causes reflex vomiting, rinse the mouth with water and then drink a few sips to replace the lost fluid. Do not drink a lot, this can provoke a recurrence of vomiting.
5. The maternity ward is not a place for tantrums
They say that difficult childbirth is a person's retribution for walking upright. Childbirth is actually a painful process, but the presence of reason allows us, representatives of the genus Homo sapiens, to control our emotions. Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome. nine0003
Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome. nine0003
6. Second stage of labor - pushing and expulsion of the fetus
After the baby's head slips through the dilated cervix and finds itself on the bottom of the pelvis, the pushing period of labor begins. At this time, there is a desire to push, as it usually happens during a bowel movement, but at the same time many times stronger. At first, the attempts are controllable, they can be "breathed", but by the beginning of the third stage of labor, the expulsion of the fetus, they become unbearable.
With the beginning of the straining period, you will be transferred to the delivery room. Having settled down on the delivery table, rest your feet on the special steps, firmly grasp the handrails and wait for the midwife's command.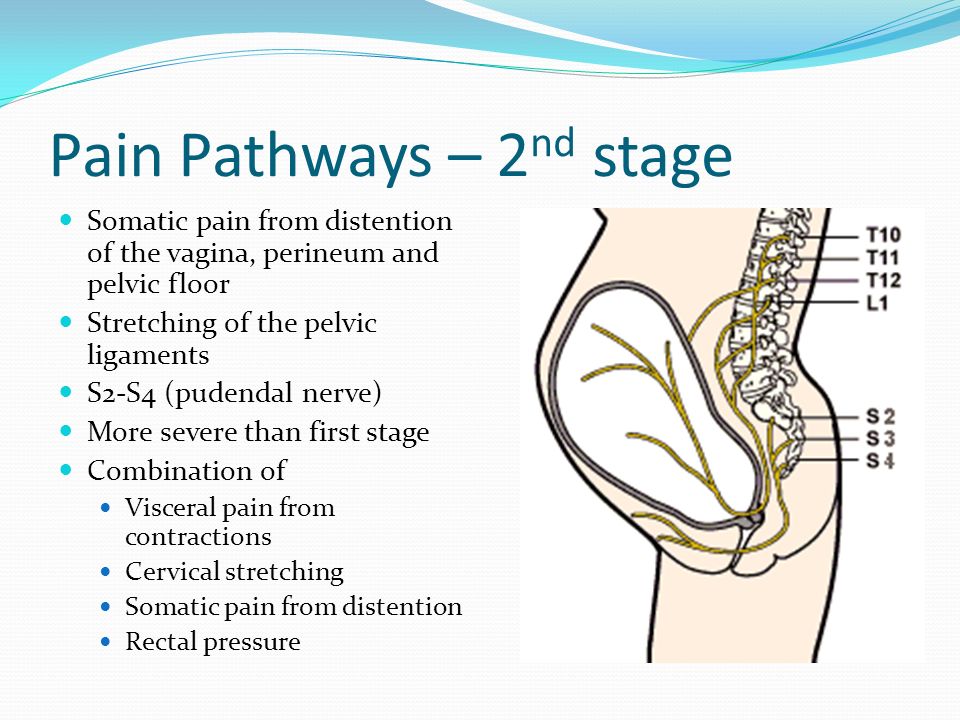 nine0003
nine0003
While pushing, inhale deeply, close your mouth, clench your lips tightly, pull the handrails of the delivery table towards you and direct all the exhalation energy down, squeezing the fetus out of you. When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over. nine0003
7. Third stage of labor and final
Third stage of labor - afterbirth. At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
About 10 minutes after your baby is born, your midwife will ask you to push again to deliver your afterbirth.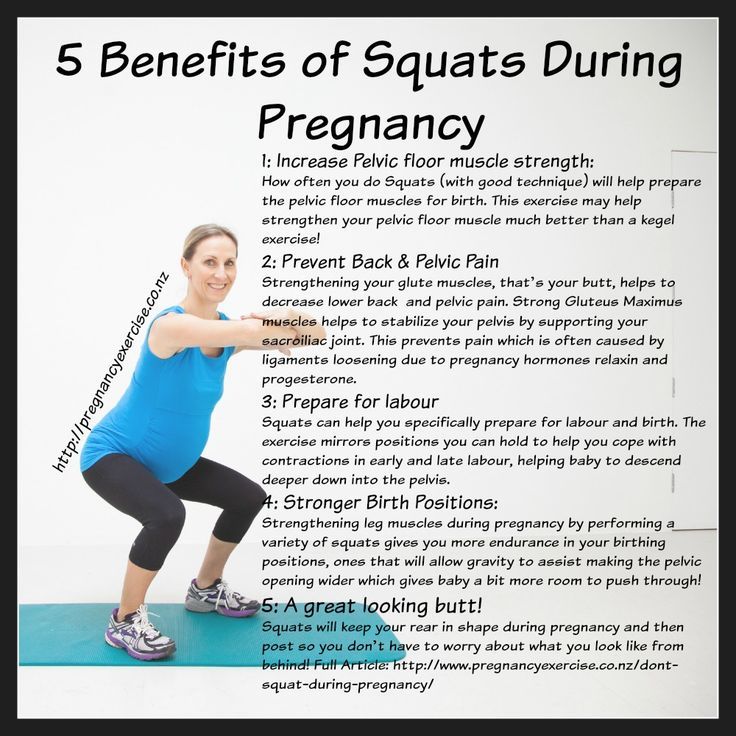 The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures. nine0003
The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures. nine0003
You will have to spend another couple of hours in the delivery room with an ice-filled bladder on your stomach. To quickly contract the uterus, you will be given injections of special drugs. When the threat of postpartum hemorrhage has passed, you will be transferred to the postpartum ward to the baby.
Childbirth completed. Ahead of the postpartum period, during which your body will recover after pregnancy.
More details on Medkrug.RU: http://www.medkrug.ru/article/show/kak_pravilno_vesti_sebja_v_rodah_uchimsja_rozhat_bystro_i_problem
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now, on the contrary, obstetricians recommend that the expectant mother move .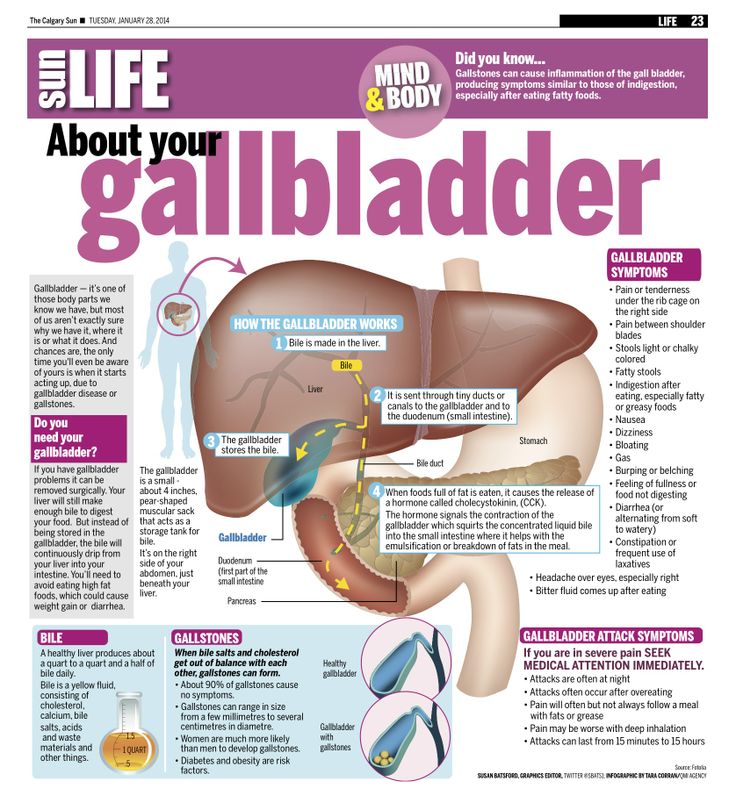 For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements. nine0003
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease.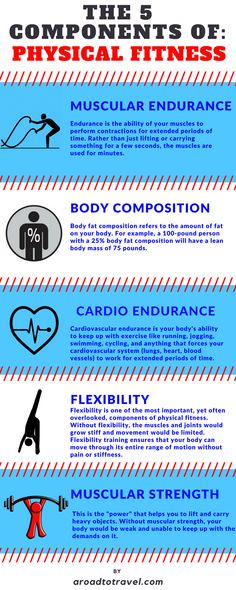 Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions. nine0003
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals. And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation. nine0003
And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation. nine0003
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
Hanging on a rope or wall bar
When the contractions become very strong and painful, you can take postures in which the stomach is, as it were, in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow. In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain. nine0003
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If a woman in childbirth wants not to move, but, on the contrary, to lie down, then, of course, she can lie down. In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control. nine0003
We use everything we have
In any roadblock, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest.