Serum hcg pregnancy test
HCG blood test - quantitative Information | Mount Sinai
Serial beta HCG; Repeat quantitative beta HCG; Human chorionic gonadotropin blood test - quantitative; Beta-HCG blood test - quantitative; Pregnancy test - blood - quantitative
A quantitative human chorionic gonadotropin (HCG) test measures the specific level of HCG in the blood. HCG is a hormone produced in the body during pregnancy.
Other HCG tests include:
- HCG urine test
- HCG blood test -- qualitative
Blood is drawn from a vein (venipuncture), usually from the inside of the elbow or the back of the hand. A needle is inserted into the vein, and the blood is collected in an air-tight vial or a syringe. Preparation may vary depending on the specific test.
How the Test is Performed
A blood sample is needed. This is most often taken from a vein. The procedure is called a venipuncture.
How to Prepare for the Test
No special preparation is needed.
How the Test will Feel
When the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging sensation. Afterward, there may be some throbbing.
Why the Test is Performed
HCG appears in the blood and urine of pregnant women as early as 10 days after conception. Quantitative HCG measurement helps determine the exact age of the fetus. It can also assist in the diagnosis of abnormal pregnancies, such as ectopic pregnancies, molar pregnancies, and possible miscarriages. It is also used as part of a screening test for Down syndrome.
Quantitative HCG measurement helps determine the exact age of the fetus. It can also assist in the diagnosis of abnormal pregnancies, such as ectopic pregnancies, molar pregnancies, and possible miscarriages. It is also used as part of a screening test for Down syndrome.
This test is also done to diagnose abnormal conditions not related to pregnancy that can raise HCG level.
Normal Results
Results are given in milli-international units per milliliter (mUI/mL).
Normal levels are found in:
- Non-pregnant women: less than 5 mIU/mL
- Healthy men: less than 2 mIU/mL
In pregnancy, HCG level rises rapidly during the first trimester and then declines slightly.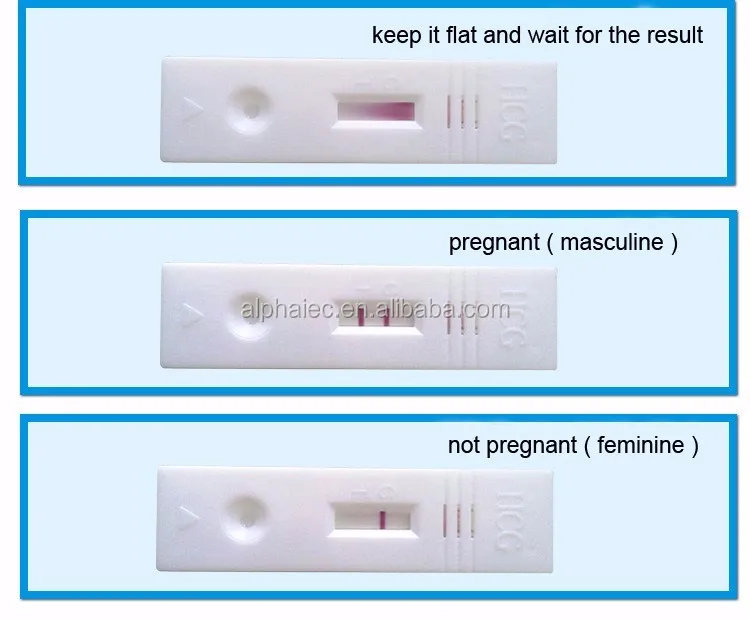 The expected HCG ranges in pregnant women are based on the length of the pregnancy.
The expected HCG ranges in pregnant women are based on the length of the pregnancy.
- 3 weeks: 5 - 72 mIU/mL
- 4 weeks: 10 -708 mIU/mL
- 5 weeks: 217 - 8,245 mIU/mL
- 6 weeks: 152 - 32,177 mIU/mL
- 7 weeks: 4,059 - 153,767 mIU/mL
- 8 weeks: 31,366 - 149,094 mIU/mL
- 9 weeks: 59,109 - 135,901 mIU/mL
- 10 weeks: 44,186 - 170,409 mIU/mL
- 12 weeks: 27,107 - 201,165 mIU/mL
- 14 weeks: 24,302 - 93,646 mIU/mL
- 15 weeks: 12,540 - 69,747 mIU/mL
- 16 weeks: 8,904 - 55,332 mIU/mL
- 17 weeks: 8,240 - 51,793 mIU/mL
- 18 weeks: 9,649 - 55,271 mIU/mL
Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test result.
What Abnormal Results Mean
Higher than normal level may indicate:
- More than one fetus, for example, twins or triplets
- Choriocarcinoma of the uterus
- Hydatidiform mole of the uterus
- Ovarian cancer
- Testicular cancer (in men)
During pregnancy, lower than normal levels based on the gestational age may indicate:
- Fetal death
- Incomplete miscarriage
- Threatened spontaneous abortion (miscarriage)
- Ectopic pregnancy
Risks
Risks of having blood drawn are slight, but may include:
- Excessive bleeding
- Fainting or feeling lightheaded
- Blood accumulating under the skin (hematoma)
- Infection (a slight risk any time the skin is broken)
Jain S, Pincus MR, Bluth MH, McPherson RA, Bowne WB, Lee P. Diagnosis and management of cancer using serological and other body fluid markers. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St Louis, MO: Elsevier; 2017:chap 74.
Diagnosis and management of cancer using serological and other body fluid markers. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St Louis, MO: Elsevier; 2017:chap 74.
Jeelani R, Bluth MH. Reproductive function and pregnancy. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St Louis, MO: Elsevier; 2017:chap 25.
University of Iowa Diagnostic Laboratories. Test directory: HCG - serum, quantitative. www.healthcare.uiowa.edu/path_handbook/rhandbook/test446.html. Updated February 10, 2022. Accessed March 11, 2022.
Yarbrough ML, Stout M, Gronowski AM. Pregnancy and its disorders. In: Rifai N, ed. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 6th ed. St Louis, MO: Elsevier; 2018:chap 69.
Last reviewed on: 12/3/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 03/11/2022.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 03/11/2022.
HCG blood test - quantitative
Medical Tests
Definition
A quantitative human chorionic gonadotropin (HCG) test measures the specific level of HCG in the blood. HCG is a hormone produced in the body during pregnancy.
Other HCG tests include:
- HCG urine test
- HCG blood test -- qualitative
Alternative Names
Serial beta HCG; Repeat quantitative beta HCG; Human chorionic gonadotropin blood test - quantitative; Beta-HCG blood test - quantitative; Pregnancy test - blood - quantitative
How the Test is Performed
A blood sample is needed. This is most often taken from a vein. The procedure is called a venipuncture.
How to Prepare for the Test
No special preparation is needed.
How the Test will Feel
When the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging sensation. Afterward, there may be some throbbing.
Why the Test is Performed
HCG appears in the blood and urine of pregnant women as early as 10 days after conception. Quantitative HCG measurement helps determine the exact age of the fetus. It can also assist in the diagnosis of abnormal pregnancies, such as ectopic pregnancies, molar pregnancies, and possible miscarriages. It is also used as part of a screening test for Down syndrome.
This test is also done to diagnose abnormal conditions not related to pregnancy that can raise HCG level.
Normal Results
Results are given in milli-international units per milliliter (mUI/mL).
Normal levels are found in:
- Non-pregnant women: less than 5 mIU/mL
- Healthy men: less than 2 mIU/mL
In pregnancy, HCG level rises rapidly during the first trimester and then declines slightly. The expected HCG ranges in pregnant women are based on the length of the pregnancy.
- 3 weeks: 5 - 72 mIU/mL
- 4 weeks: 10 -708 mIU/mL
- 5 weeks: 217 - 8,245 mIU/mL
- 6 weeks: 152 - 32,177 mIU/mL
- 7 weeks: 4,059 - 153,767 mIU/mL
- 8 weeks: 31,366 - 149,094 mIU/mL
- 9 weeks: 59,109 - 135,901 mIU/mL
- 10 weeks: 44,186 - 170,409 mIU/mL
- 12 weeks: 27,107 - 201,165 mIU/mL
- 14 weeks: 24,302 - 93,646 mIU/mL
- 15 weeks: 12,540 - 69,747 mIU/mL
- 16 weeks: 8,904 - 55,332 mIU/mL
- 17 weeks: 8,240 - 51,793 mIU/mL
- 18 weeks: 9,649 - 55,271 mIU/mL
Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test result.
What Abnormal Results Mean
Higher than normal level may indicate:
- More than one fetus, for example, twins or triplets
- Choriocarcinoma of the uterus
- Hydatidiform mole of the uterus
- Ovarian cancer
- Testicular cancer (in men)
During pregnancy, lower than normal levels based on the gestational age may indicate:
- Fetal death
- Incomplete miscarriage
- Threatened spontaneous abortion (miscarriage)
- Ectopic pregnancy
Risks
Risks of having blood drawn are slight, but may include:
- Excessive bleeding
- Fainting or feeling lightheaded
- Blood accumulating under the skin (hematoma)
- Infection (a slight risk any time the skin is broken)
References
Jain S, Pincus MR, Bluth MH, McPherson RA, Bowne WB, Lee P. Diagnosis and management of cancer using serological and other body fluid markers. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St Louis, MO: Elsevier; 2017:chap 74.
Jeelani R, Bluth MH. Reproductive function and pregnancy. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 23rd ed. St Louis, MO: Elsevier; 2017:chap 25.
University of Iowa Diagnostic Laboratories. Test directory: HCG - pregnancy, serum, quantitative. www.healthcare.uiowa.edu/path_handbook/rhandbook/test1549.html. Updated December 14, 2017. Accessed February 18, 2019.
Yarbrough ML, Stout M, Gronowski AM. Pregnancy and its disorders. In: Rifai N, ed. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. 6th ed. St Louis, MO: Elsevier; 2018:chap 69.
St Louis, MO: Elsevier; 2018:chap 69.
Review Date: 09/25/2018
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.
hCG, human chorionic gonadotropin, indications for the appointment, rules for preparing for the test, interpretation of the results and norm indicators.

I confirm More
- INVITRO
- Library
- Laboratory...
- HCG, Chorionic...
Miscarriage
Pregnancy
5317 July 29
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0025 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0025 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
We remind you that independent interpretation of the results is unacceptable, the information below is for reference only.
Human chorionic gonadotropin (hCG, β-hCG, beta-hCG, Human Chorionic Gonadotropin): indications for the appointment, rules for preparing for the test, interpretation of the results and normal indicators. nine0031
Chorionic gonadotropin is a hormone produced by the outer shell of the embryo, and is normally determined in the blood and urine of a woman only when pregnancy occurs.
Chorionic gonadotropin consists of two subunits - alpha and beta. The beta subunit (β-hCG) used for the immunometric determination of the hormone is unique. To monitor the course of pregnancy, the determination of the beta subunit of hCG is used. The level of beta-hCG in the blood as early as 6-8 days after conception makes it possible to diagnose pregnancy (the concentration of β-hCG in the urine reaches the diagnostic level 1-2 days later than in the blood serum). nine0003
The beta subunit (β-hCG) used for the immunometric determination of the hormone is unique. To monitor the course of pregnancy, the determination of the beta subunit of hCG is used. The level of beta-hCG in the blood as early as 6-8 days after conception makes it possible to diagnose pregnancy (the concentration of β-hCG in the urine reaches the diagnostic level 1-2 days later than in the blood serum). nine0003
HCG has a multifaceted effect on the body of a pregnant woman: it affects the development of the embryo and fetus, stimulates the synthesis of estrogens and androgens by ovarian cells, promotes the functional activity of the chorion and placenta, and ensures the successful course of pregnancy.
The introduction of hCG into the body of non-pregnant women stimulates ovulation and the synthesis of sex hormones necessary for conception. In men, this hormone enhances the formation of seminal fluid, activates the production of gonadosteroids. nine0003
nine0003
In early pregnancy and up to the 2nd trimester, β-hCG supports the production of hormones necessary to maintain pregnancy, and in male fetuses it stimulates cells responsible for the formation and development of the male reproductive system.
Human chorionic gonadotropin (hCG, beta-hCG, b-hCG, Human Chorionic)
Synonyms: Beta-hCG general. Human Chorionic Gonadotropin; hCG; Pregnancy Quantitative hCG; Beta hCG; Total beta hCG. Brief description of the analyte Human chorionic gonadotropin ...
Up to 1 business day
Available with home visit
RUB 685
Add to cart
Indications for determining the level of hCG in women
- Absence of menstruation (amenorrhea).
- Exclusion/confirmation of pregnancy, including ectopic (ectopic). nine0006
- Diagnosis of the state of the fetus at different stages of pregnancy.
- Assessment of the state of the placenta at different stages of pregnancy.
- Dynamic monitoring of fetal development during pregnancy, including in the diagnosis of malformations.
- Suspicion of the presence of neoplastic diseases of the reproductive system, such as hydatidiform mole (a rare pathology of the fetal egg, in which instead of developing the embryo, chorionic villi grow), chorionepithelioma (a malignant tumor that develops from the epithelium of the villi of the fetal egg). nine0006
- Performing artificial termination of pregnancy.
Indications for determining the level of hCG in men:
The presence of suspicion of tumors of the testicles.
Deadline for this test is 1 working day, excluding the day of taking the biomaterial.
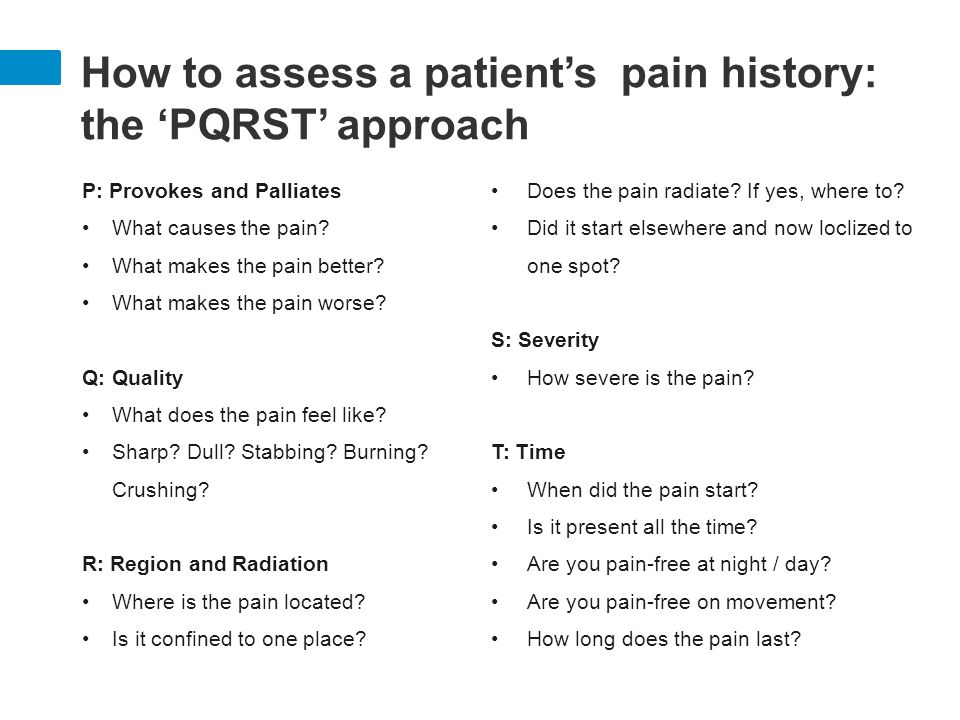
Rules for preparing for a blood test to determine the level of hCG
non-specific: it is enough to refrain from smoking and drinking alcohol on the eve of the procedure, limit stress and intense physical activity for a week; blood donation is carried out on an empty stomach. nine0003
The determination of hCG in the blood is possible already on the 6-8th day after conception. The use of urinary test systems (rapid pregnancy tests) will be informative starting from the 7th day after the fertilization of the egg. To confirm the result, it is recommended to re-determine the level of the hormone a few days after the first analysis.
You can take a blood test for hCG (thyroid stimulating hormone, thyrotropin, Thyroid StimulatingHormone, TSH) at the nearest INVITRO medical office. The list of offices where biomaterial is accepted for laboratory testing is presented in the "Addresses" section. nine0003
Reasons leading to high levels of β-hCG
- Multiple pregnancy.

- Incorrect timing of pregnancy.
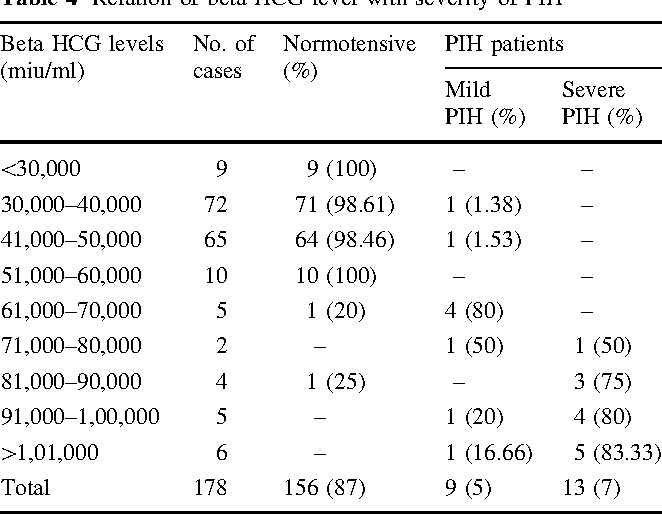
- Pathological pregnancy: the appearance of edema, increased blood pressure, loss of protein in the urine (preeclampsia), convulsions (eclampsia), toxicosis.
- The presence of a pregnant woman with chronic diseases (for example, diabetes mellitus). nine0006
- Multiple fetal malformations (in such a situation, the determination of the level of β-hCG is used together with other indicators, the so-called "triple test". This study is used as a screening, and not for diagnosis.).
Reasons for fixing a decrease in the level of β-hCG
- Incorrectly established terms of pregnancy.
- Ectopic pregnancy.
- Frozen pregnancy. nine0006
- Threat of miscarriage.
- Fetal or placental disorders (including placental insufficiency).
- Intrauterine fetal death (in this case, it is informative to determine the level of the hormone in the first and second trimesters).

During abortion, the level of β-hCG is also monitored, the dynamics of growth / fall of which can be used to judge the completeness of the manipulation.
Determining the level of hCG, in addition to establishing the fact of pregnancy in the early stages, is part of the screening examination of pregnant women in the first trimester, along with ultrasound. nine0003
1st trimester prenatal screening for trisomies, PRISCA-1 (1st trimester biochemical screening - 1st trimester “double test”, risk calculation using PRISCA software)
Synonyms: Prenatal Screening Markers for Down Syndrome; PRISCA-1. Brief description of the study "Prenatal screening for trisomies of the 1st trimester of pregnancy, PRISCA-1)" Test run...
Up to 1 business day
Available with home visit
2 040 RUB
Add to cart
Screening ultrasound of the 1st trimester of pregnancy (11-13 weeks 6 days)
Examination necessary to monitor the growth and development of the fetus in the first trimester of pregnancy.
RUB 2,790 Sign up nine0003
In gynecological practice, human chorionic gonadotropin is used to treat infertility, stimulate ovulation, and synthesize sex steroids. In urology, it is used in the treatment of cryptorchidism (undescended testicles) and infertility associated with impaired spermatogenesis.
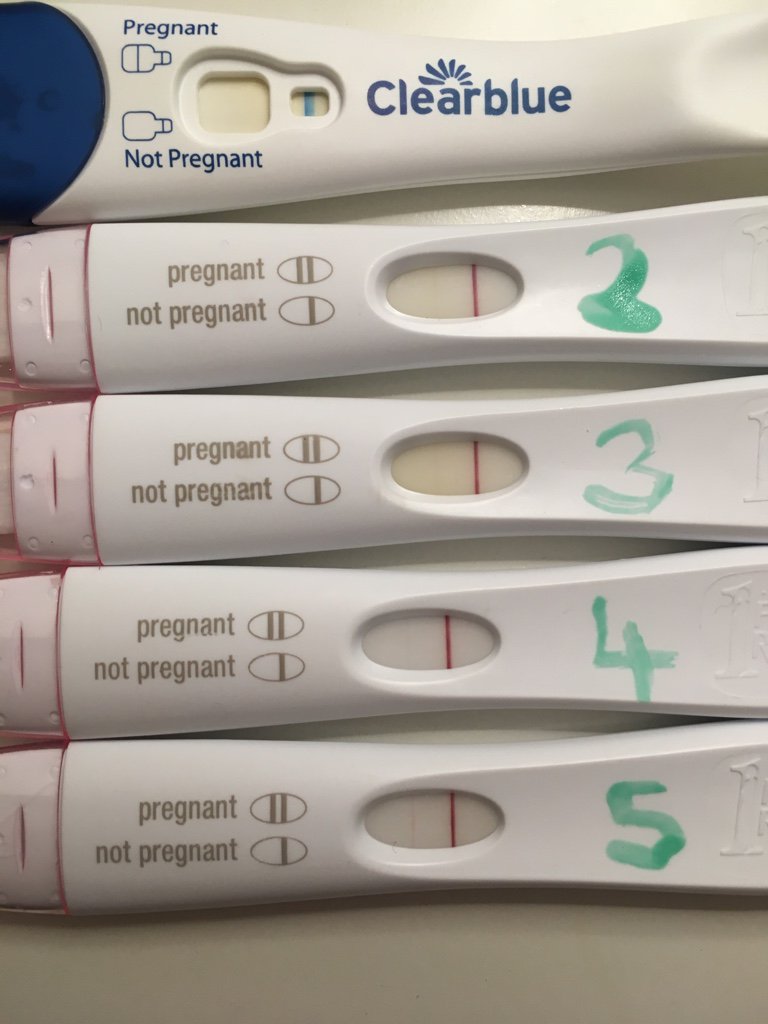
Quantitatively, β-hCG is determined in the blood, for a qualitative determination, special test systems (pregnancy tests) are used, and in this case, urine serves as a biomaterial.
Quantitative determination of the level of hCG allows you to monitor the course of pregnancy in dynamics. To do this, obstetrician-gynecologists have developed tables for increasing the level of hCG, depending on the duration of pregnancy in weeks. The sensitivity of the determination is in the range of 1.2-1125000 mU/ml. nine0025
Reference values of hCG levels in dynamics by gestational age
| Pregnancy (weeks from conception) | HCG level (mU / ml) |
| 2 | 25–300 |
| 3 | 1500–5000 | nine0195
| four | 10000–30000 |
| five | 20000–100000 |
| 6–11 | 20000–>225000 |
| 12 | 19000–135000 |
| 13 | 18000–110000 | nine0195
| fourteen | 14000–80000 |
| 15 | 12000–68000 |
| sixteen | 10000–58000 |
| 17–18 | 8000–57000 |
| nineteen | 7000–49000 | nine0195
| 20–28 | 1600–49000 |
| Men and non-pregnant women | 0–<5 mU/ml |
Values ranging from 5 to 25 mU / ml do not allow unambiguous confirmation or denial of pregnancy, therefore, a second study is required after two days.
Since the hormone is produced by the placenta, during normal pregnancy, with placental pathology (for example, with fetoplacental insufficiency - a violation of the development of the fetus and placenta), with multiple pregnancies, the values of β-hCG will differ. With a normal pregnancy until the fifth week, the level of the hormone rises exponentially: every two days its concentration doubles, reaching a peak by the 11th week of gestation. Accordingly, in a multiple pregnancy, the level of β-hCG will be even higher than in a single pregnancy. nine0003
If the indicator deviates from the norm, additional ultrasound of the pelvic organs (uterus, appendages) is required.
US examination of pelvic organs (uterus, adnexa)
Ultrasound scanning of the organs of the female reproductive system to assess the shape and size, as well as exclude pathology.
RUB 2,390 Sign up nine0003
However, with a normal hCG value, additional examinations may also be needed:
- Ultrasound diagnosis of pregnancy (required to confirm pregnancy, clarify the term).

Ultrasound diagnosis of pregnancy
Examination to confirm pregnancy and determine the place of attachment of the ovum (to exclude ectopic pregnancy).
RUB 2,290 Sign up nine0003
- Screening ultrasound of the 1st trimester of pregnancy (11-13 weeks 6 days) - to assess the characteristics and confirm the normal development of the fetus.
Screening ultrasound of the 1st trimester of pregnancy (11-13 weeks 6 days)
Examination necessary to monitor the growth and development of the fetus in the first trimester of pregnancy.
RUB 2,790 Sign up nine0003
- Screening ultrasound of the 1st trimester of multiple pregnancy (11-13 weeks 6 days) - to confirm the presence of several fetuses, determine their characteristics; It is necessary for planning the subsequent actions of the doctor and the management of pregnancy.

Screening ultrasound of the 1st trimester of multiple pregnancy (11-13 weeks 6 days)
A study that allows you to evaluate the growth and development of fetuses, their position in the uterus, and make a plan for further pregnancy management. nine0003
RUB 3,840 Sign up
- Fetal ultrasound according to indications (before the 20th week) - performed in case of suspected ectopic pregnancy.
Fetal ultrasound according to indications (before the 20th week)
Additional ultrasound, which is prescribed in the presence of concomitant pathologies to monitor the condition of the fetus.
RUB 2,540 Sign up nine0003
- Lab tests to be performed in the first trimester are collected in the Pregnancy: 1st trimester (1-13 weeks) profile.

For professional assistance in interpreting the results, contact
obstetrician-gynecologist
.
Sources:
- www.invitro.ru
- Clinical guidelines "Ectopic (ectopic) pregnancy". Developed by: Russian Society of Obstetricians-Gynecologists, Association of Obstetric Anesthesiologists-Resuscitators. – 2021.
- Clinical guidelines "Premature birth". Developed by: Russian Society of Obstetricians-Gynecologists, Association of Obstetric Anesthesiologists-Resuscitators. – 2020.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0025 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
PSA (prostate specific antigen) test
10018 may 13 nine0003
-
Human papillomavirus
14272 04 May
-
Alkaline phosphatase
5128 16 April
Similar articles
Hypogonadism
ECO
Menopause
Climax
nine0020 Estradiol Estradiol: indications for prescription, rules for preparing for the test, interpretation of the results and norm indicators.
More
ECO
Blood transfusion
Pregnancy
nine0020 Rh-affiliation (Rh-factor, Rh)Rh-affiliation: indications for the appointment, rules for preparing for the test, interpretation of the results and indicators of the norm.
More
Infertility
Varicocele
nine0002 ECOSpermogram in INVITRO
Sperm analysis is an integral part of infertility diagnostics and monitoring of diseases of the male genital area. The analysis of the ejaculate includes the determination of the quantitative and qualitative morphological composition of spermatozoa using visual counting in the Goryaev chamber and special staining.
The analysis of the ejaculate includes the determination of the quantitative and qualitative morphological composition of spermatozoa using visual counting in the Goryaev chamber and special staining.
More
nine0002 ECOThrombophilia
Stroke
Obesity
COVID-19
Nephrotic syndrome
Pregnancy
Thrombosis propensity in pregnancy - minimal panel
Thrombosis propensity in pregnancy: indications for prescribing, rules for preparing for the test, interpretation of the results and normal indicators.
More
Pregnancy
Abnormalities of the kidneys
Anencephaly
Alpha-fetoprotein (AFP, alfa-Fetoprotein)
Alpha-fetoprotein: indications for prescribing, rules for preparing for the analysis, interpretation of the results and norm indicators.
More nine0003
No results found
Try editing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from the list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Try changing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data nine0003
Subscribe
Beta-subunit of human chorionic gonadotropin (beta-hCG)
Beta-subunit of human chorionic gonadotropin is one of the subunits of a specific hormone molecule - chorionic gonadotropin, which is formed in the shell of the human embryo. The analysis is carried out for the purpose of early diagnosis of pregnancy, detection of its complications and diagnosis of diseases associated with impaired hCG secretion. nine0003
The analysis is carried out for the purpose of early diagnosis of pregnancy, detection of its complications and diagnosis of diseases associated with impaired hCG secretion. nine0003
Synonyms Russian
Beta subunit of hCG.
Synonyms English
Human Chorionic Gonadotropin, hCG, b-HCG, Quantitative hCG; Beta hCG, Total hCG, Total beta hCG.
Test method
Electrochemiluminescent immunoassay (ECLIA).
Detection range: 0.1 - 1,000,000 IU/l.
Units
IU/l (international unit per litre).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for an examination?
- Do not smoke for 30 minutes before the test.
General information about the study
Human chorionic gonadotropin (hCG) is a hormone produced in the fetal membrane of the human embryo. It is an important indicator of the development of pregnancy and its deviations. It is produced by the cells of the chorion (the shell of the embryo) immediately after it is attached to the wall of the uterus (this happens only a few days after fertilization). The embryo at this stage of pregnancy is a microscopic vesicle filled with fluid, the walls of which are made up of rapidly multiplying cells. From one part of these cells, the unborn child (embryoblast) develops, while from the cells outside the embryo, a trophoblast is formed - that part of the fetal egg, with which it is attached to the wall of the uterus. Later, the chorion is formed from the trophoblast. nine0003
It is an important indicator of the development of pregnancy and its deviations. It is produced by the cells of the chorion (the shell of the embryo) immediately after it is attached to the wall of the uterus (this happens only a few days after fertilization). The embryo at this stage of pregnancy is a microscopic vesicle filled with fluid, the walls of which are made up of rapidly multiplying cells. From one part of these cells, the unborn child (embryoblast) develops, while from the cells outside the embryo, a trophoblast is formed - that part of the fetal egg, with which it is attached to the wall of the uterus. Later, the chorion is formed from the trophoblast. nine0003
Chorion performs the function of nourishing the embryo, being an intermediary between the body of the mother and the child. In addition, it produces chorionic gonadotropin, which, on the one hand, affects the formation of the child, on the other hand, it specifically affects the mother's body, ensuring a successful pregnancy. The appearance of this hormone in the body of a future mother at the initial stage of pregnancy explains the importance of the test for early diagnosis of pregnancy.
The appearance of this hormone in the body of a future mother at the initial stage of pregnancy explains the importance of the test for early diagnosis of pregnancy.
Chorionic gonadotropin stimulates the secretory function of the corpus luteum of the ovaries, which should produce the hormone progesterone, which maintains the normal state of the inner lining of the uterine wall - the endometrium. The endometrium provides reliable attachment of the fetal egg to the mother's body and its nutrition with all the necessary substances. nine0003
Due to a sufficient amount of human chorionic gonadotropin, the corpus luteum, which normally exists for only about 2 weeks during each menstrual cycle, does not undergo resorption after successful conception and remains functionally active throughout the entire period of pregnancy. Moreover, it is in pregnant women under the influence of chorionic gonadotropin that it produces very large amounts of progesterone. In addition, CG stimulates the production of estrogens and weak androgens by ovarian cells and promotes the development of the functional activity of the chorion itself, and later the placenta, which is formed as a result of the maturation and growth of the chorionic tissue, improving its own nutrition and increasing the number of chorionic villi. nine0003
nine0003
Thus, the role of human chorionic gonadotropin lies in the specific and multifaceted effect on the body of a woman and the fetus in order to ensure a successful pregnancy. Based on the analysis for chorionic gonadotropin, the presence of chorionic tissue in the woman's body is determined, and hence pregnancy.
According to its chemical structure, chorionic gonadotropin is a combination of protein and complex carbohydrates, consisting of two parts (subunits): alpha and beta. The alpha subunit of chorionic gonadotropin is completely identical to the alpha subunits of the luteinizing, follicle-stimulating and thyroid-stimulating hormones of the pituitary gland, which perform functions that are largely similar to the function of chorionic gonadotropin, but not during pregnancy. The beta subunit of chorionic gonadotropin is unique, which, on the one hand, determines the specificity of its action, and, on the other hand, allows it to be identified in biological media. In this regard, this test is called "beta-subunit of human chorionic gonadotropin (beta-hCG)". nine0003
nine0003
Knowing the level of beta-hCG in the blood, it is possible to diagnose pregnancy already on the 6-8th day after conception (in the urine, the concentration of beta-hCG reaches the diagnostic level 1-2 days later). Normally, during pregnancy between the 2nd and 5th weeks, the amount of beta-hCG doubles every 1.5 days. With multiple pregnancy, it increases in proportion to the number of fetuses. The maximum level of hCG reaches the 10-11th week, and then gradually decreases. This is due to the fact that from the beginning of the 2nd third of pregnancy, the placenta is able to independently produce enough estrogens and progesterone, with the participation of which the endometrium functions normally, regardless of the secretion of hormones in the ovarian corpus luteum. At the same time, the concentration of CG in the blood of a pregnant woman gradually decreases, and the corpus luteum can function without the effects of CG. During this period, the role of the hormone is to stimulate the production of testosterone in the fetus, which is necessary for the normal development of the external genital organs of the embryo. nine0003
nine0003
Thus, during pregnancy, the level of beta-hCG in the blood first increases and then decreases. According to this indicator, one can judge the successful course of pregnancy and identify violations of the development of the fetus. The test for hCG in the blood is the most reliable method for determining pregnancy in the early stages. HCG appears in the body of a woman from 6-8 days after fertilization. A common rapid pregnancy test that every woman can use at home is also based on measuring hCG in the urine. nine0003
Below normal hormone levels at various stages of fetal development suggest ectopic pregnancy, fetal growth retardation, threatened miscarriage, non-progressive pregnancy, or placental insufficiency. The reason for the increased content of beta-hCG may be toxicosis, diabetes mellitus, or an incorrectly set gestational age. A high level of the hormone after a mini-abortion indicates a progressing pregnancy.
Determining the level of hCG is included in the triple test study, the results of which can be used to judge some anomalies in the development of the fetus, but an accurate diagnosis cannot be made. The study only allows you to classify a woman as a risk group for this pathology. In this case, further investigation is necessary. In non-pregnant women, CG is normally absent, but it can be secreted by some abnormal chorion-derived tissues (hydatidiform mole, chorionepithelioma) and some other tumors. nine0003
The study only allows you to classify a woman as a risk group for this pathology. In this case, further investigation is necessary. In non-pregnant women, CG is normally absent, but it can be secreted by some abnormal chorion-derived tissues (hydatidiform mole, chorionepithelioma) and some other tumors. nine0003
What is research used for?
- For the diagnosis of pregnancy, including multiple, ectopic and non-developing.
- To monitor the progress of pregnancy.
- To detect fetal growth retardation, threatened miscarriage, placental insufficiency.
- For the diagnosis of amenorrhea.
- To monitor the effectiveness of induced abortion.
- As part of a comprehensive examination to identify fetal malformations. nine0006
- For the diagnosis of CG-producing tumors.
When is the test ordered?
- If pregnancy is suspected, in particular multiple pregnancy.
- When monitoring the progress of pregnancy.

- When there is an assumption about a complication during pregnancy: fetal growth retardation, the threat of spontaneous abortion, non-developing or ectopic pregnancy, chronic placental insufficiency. nine0066 Confirm successful induced abortion if necessary.
- With a comprehensive examination to identify fetal malformations.
- When finding out the reason for the absence of menstruation (amenorrhea).
- When is the diagnosis of tumors producing hCG.
What do the results mean?
Reference values
| Floor | nine0191 Reference values | |
|
Female | Not pregnant | Less than 5 IU/L |
| 3 weeks | 5. | |
| 4 weeks | 9.5 - 750 IU/L | |
| 5 weeks | 217 - 7138 IU/L | |
| 6 weeks | 158 - 31795 IU/l | |
| 7 weeks | 3697 - 163563 IU/L | |
| 8 weeks | 32065 - 149571 IU/l | |
| 9 weeks | 63803 - 151410 IU/L | |
| 10 weeks | nine0191 ||
| 11-12 weeks | 27832 - 210612 IU/L | |
| 13-14 weeks | 13950 - 62530 IU/L | |
| 15 weeks | 12039 - 70971 IU/L | |
| 16 weeks | 9040 - 56451 IU/L | |
| 17 weeks | 8175 - 55868 IU/L | |
| 18 weeks | 8099 - 58176 IU/L | |
| Male |
| Less than 5 IU/L nine0192 |
Causes of high beta-hCG levels
In the absence of pregnancy, the result of the beta-hCG test should be negative. The detection of beta-hCG suggests that at least 5-6 days have passed since fertilization. Between the 2nd and 5th weeks of pregnancy, during its normal course, the level of beta-hCG doubles every 1.5 days and soon reaches its maximum. Then it starts to slowly decline. The results of the analysis are compared with the normal values for each gestational age. For a correct interpretation of the results, it is necessary to know exactly when the conception occurred. nine0003
The detection of beta-hCG suggests that at least 5-6 days have passed since fertilization. Between the 2nd and 5th weeks of pregnancy, during its normal course, the level of beta-hCG doubles every 1.5 days and soon reaches its maximum. Then it starts to slowly decline. The results of the analysis are compared with the normal values for each gestational age. For a correct interpretation of the results, it is necessary to know exactly when the conception occurred. nine0003
In pregnant women:
- multiple pregnancies (the rate increases in proportion to the number of fetuses),
- toxicosis,
- prolonged pregnancy,
- maternal diabetes,
- fetal malformations,
- taking synthetic hormones.
Not pregnant:
- hCG-producing tumors,
- surgical abortion (first 4-5 days after the procedure),
- taking hCG preparations.
Causes of low beta-hCG levels (during pregnancy):
- ectopic or non-developing pregnancy,
- fetal growth retardation,
- threatened miscarriage,
- chronic placental insufficiency,
- fetal death (in the 2nd-3rd trimester of pregnancy).
What can influence the result?
- When diagnosing pregnancy, taking the test too early - when less than 5 days have passed since conception - can lead to a false negative result. nine0006
Also recommended
- Alpha-fetoprotein (alpha-FP)
- Antiphospholipid antibodies IgG
- Antiphospholipid antibodies IgM
- Placental lactogen
- Free estriol
- Pregnancy - Prenatal screening for trisomies of the first trimester of pregnancy (Down syndrome), PRISCA
- Pregnancy-associated plasma protein A (PAPP-A)
- Pregnancy - Prenatal screening for trisomies of the second trimester of pregnancy, PRISCA
- Antibodies to steroid-producing cells of the placenta
Who orders the examination?
General practitioner, obstetrician-gynecologist, oncologist.
Literature
- Handbook of Clinical Laboratory Testing During Pregnancy, edited by Ann M.
 Gronowski. Springer-Verlag LLC, New York, 2004
Gronowski. Springer-Verlag LLC, New York, 2004 - Prenatal Diagnosis in Obstetric Practice. M. J. J. Whittle, Blackwell Publishers 1995 nine0066 Endocrinology of Pregnancy. Fuller W. Bazer, Humana Press 1998
- Blood Biochemistry. N J Russell, G M Powell, J G Jones, P J, Winterburn and J M Basford, Croom Helm, London and Canberra, 1982
- Blood Chemistry and CBC analysis-Clinical Laboratory Testing from a Functional Perspective. Rychard Weatherby N.D and Scott Fergusson, N.D., Bear Mounting Publishing, 2002.
- Tietz Clinical Guide to Laboratory Tests. Alan H. B. Wu, Saunders/Elsevier, 2006
- Laboratory and Diagnostic Tests. Joyce LeFever Kee - Pearson, Prentice Hall, 8th edition 2010
- District Laboratory Practice in Tropical Countries. Monica Cheesbrough, Cambridge University Press, second edition, 2005.
- Clinical Chemistry. A Laboratory Perspective. Wendy L. Arneson, Jean M. Brickell, F.A. Davis Company, 2007
- Clinical Chemistry.

 8 - 71.2 IU/L
8 - 71.2 IU/L