Placenta accreta discovered after delivery
Placenta Accreta Myths - Brigham and Women's Hospital
Placenta accreta is an uncommon and complex condition. Accreta patients, along with their friends and family, may receive inconsistent information about the condition and its consequences.
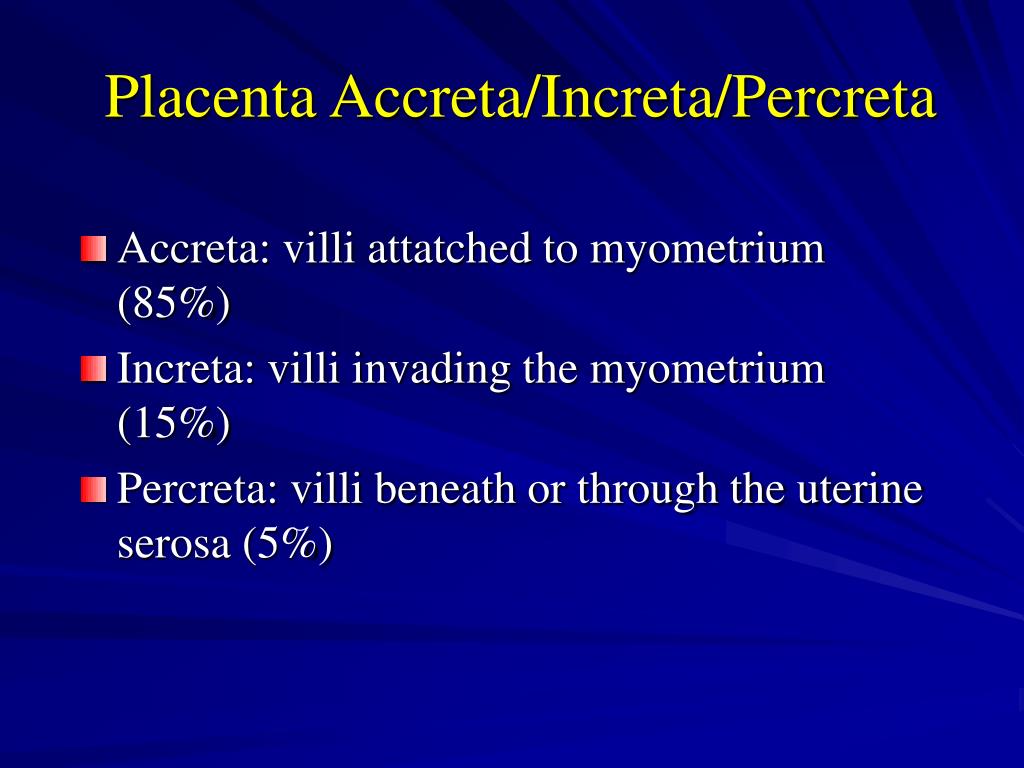
To begin with, it is important to understand the meaning of the terms accreta, increta and percreta. The terms can be confusing so before we turn to the myths, here are the definitions:
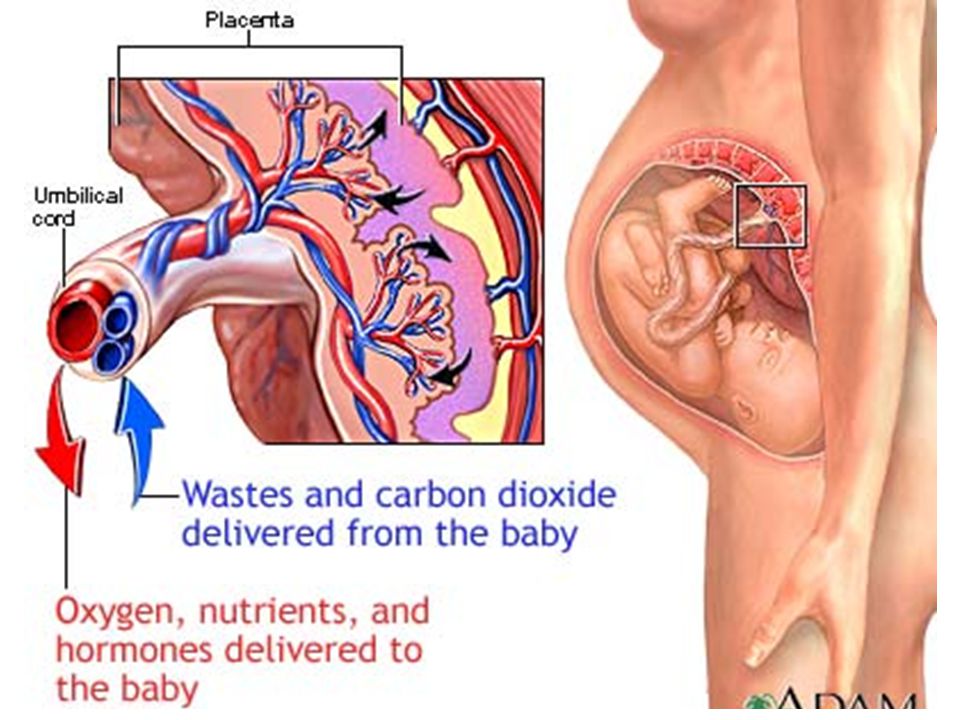
- Placenta accreta occurs when the placenta—the organ that provides nutrients and other support to a developing fetus—attaches too deeply to the uterine wall. This is a serious condition that can cause complications for the baby and mother, especially during the delivery.
- Placenta increta is a condition where the placenta attaches more firmly to the uterus and becomes embedded in the organ's muscle wall.
- Placenta percreta is a condition where placenta attaches itself and grows through the uterus and potentially to the nearby organs.
The following are commonly believed myths submitted by women who have experienced placenta accreta first-hand. The surgical obstetrics specialists at Brigham and Women’s Hospital have addressed each of these points based on current medical information and practice.
Myth: Women with placenta accreta always hemorrhage at the time of delivery.
Fact: Women with accreta are certainly at high risk for bleeding and hemorrhage, which is why expert care is needed. However, accreta can occur in a wide range of circumstances and not every woman will hemorrhage.
The likelihood of a hemorrhage depends on the individual conditions of your placenta. During pregnancy, bleeding and hemorrhage is more related to placenta previa (placenta covering the cervix) than to the accreta. With a previa, large blood vessels around the cervix may bleed in response to contractions, or bleed on their own, though most women with a previa do not hemorrhage. An accreta that develops without previa would be less likely to bleed.
An accreta that develops without previa would be less likely to bleed.
The risk also may be related to how the placenta is treated at the time of delivery. When delivering a baby from a uterus with an accreta, particular care is given to where the incision is made. Many women with accreta will have an up-and-down incision so as to deliver the baby without disturbing the accreta. If the accreta is low in the uterus, which is usually the case, this incision allows a safe delivery above this area.
Once the baby is delivered and the accreta is confirmed, trying to remove it can also create severe bleeding. Therefore, it is usually left in place and a hysterectomy is performed to avoid a major hemorrhage. In some cases the placenta may be removed or left behind without a hysterectomy, but only with special precautions to avoid hemorrhage. This is not a common practice.
In some cases, a hemorrhage is highly likely or even inevitable, but this is not true for all women with accreta.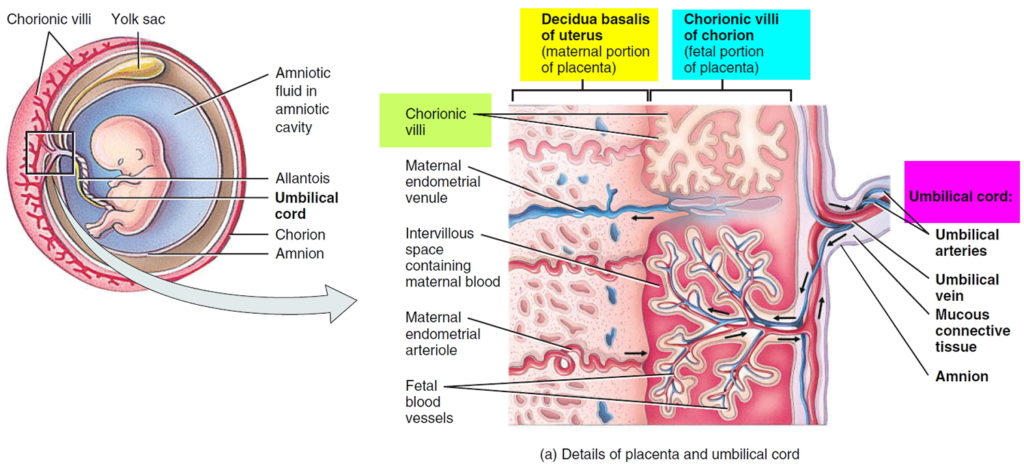 No matter the hemorrhage risk, it’s important that well-trained obstetricians who understand your specific needs and risks manage your baby’s delivery.
No matter the hemorrhage risk, it’s important that well-trained obstetricians who understand your specific needs and risks manage your baby’s delivery.
Myth: All women diagnosed with accreta must have a hysterectomy after delivery.
Fact: A hysterectomy is a highly effective treatment for minimizing hemorrhage, but is not always necessary. In general, large accretas, incretas and percretas are most safely managed with a hysterectomy. However, small or “focal” accretas can sometimes be removed without a hysterectomy. In other cases, patients and their doctors may agree that leaving some or all of the accreta in the uterus (rather than removing the uterus) is a reasonable option. These decisions are complicated and require extensive discussion with an experienced obstetrician.
Myth: Women with accreta will not bleed because the accreta holds the uterus and placenta together.
Fact: There are different reasons why women bleed before giving birth. The most serious cause is placental abruption, a condition where the placenta separates from the uterus early and bleeding occurs behind the placenta. It’s possible, although rare, for a woman with accreta to experience an abruption.
The most serious cause is placental abruption, a condition where the placenta separates from the uterus early and bleeding occurs behind the placenta. It’s possible, although rare, for a woman with accreta to experience an abruption.
The more common cause for bleeding in accreta patients is placenta previa. In this case, the placenta is sitting in an abnormally low position, and this causes the blood vessels connecting the uterus and placenta to bleed. Patients with accreta often also have placenta previa. The previa may bleed even though the placenta is tightly attached to the uterus.
Myth: If a woman with placenta accreta does not experience bleeding, this means it’s safe to carry the baby to term. In other words, “no bleeding, no problems.”
Fact: The majority of women with placenta accreta need to deliver weeks before their due dates, even if there has been no bleeding. This is often the best option for a controlled delivery, where all risks can be managed safely.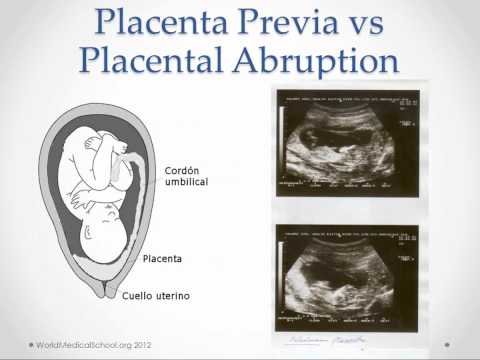 If a woman experiences heavy bleeding, an earlier delivery may be especially important.
If a woman experiences heavy bleeding, an earlier delivery may be especially important.
Delivery with accreta requires a very complex surgery, often with a multidisciplinary team of surgeons. Therefore, it is best to deliver your baby as soon as it is safe to do so, both in terms of the baby’s health and the mother’s wellbeing. Typically, this occurs at week 34 of gestation (6 weeks before the due date) and no later than week 36-37 of gestation. However, this depends on your specific conditions. For example, a patient who appears to have a percreta may be delivered earlier than a patient with no signs of this. On the other hand a patient with a small (“focal”) accreta and no previa may be delivered at 37 weeks or later.
Myth: All accreta patients must be under general anesthesia for either part or all of the delivery and hysterectomy.
Fact: The anesthesia required for delivery depends entirely on your individual circumstances.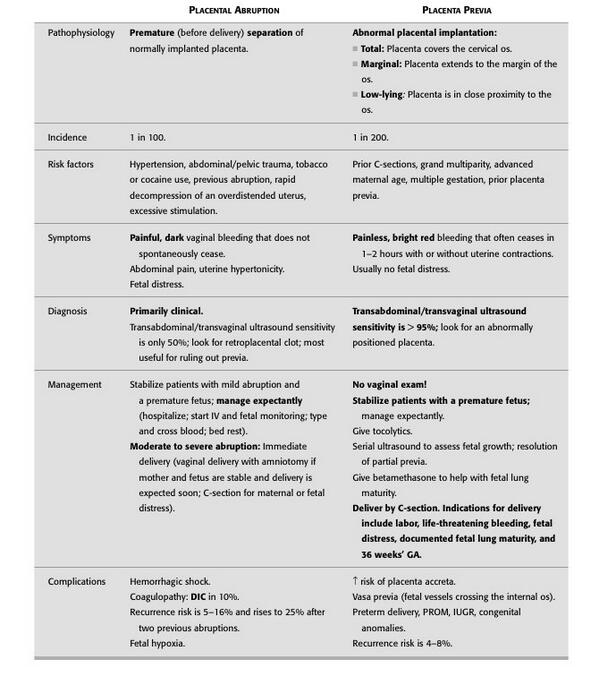 For women who require a long, complicated surgery, or who hemorrhage, general anesthesia may be necessary for safety and comfort. However, an epidural anesthetic will often be used at the beginning of the surgery to allow the patient to be awake for the baby’s delivery. Often the entire surgery can be performed with the epidural instead of general anesthesia.
For women who require a long, complicated surgery, or who hemorrhage, general anesthesia may be necessary for safety and comfort. However, an epidural anesthetic will often be used at the beginning of the surgery to allow the patient to be awake for the baby’s delivery. Often the entire surgery can be performed with the epidural instead of general anesthesia.
Myth: A vaginal delivery is not possible with accreta.
Fact: Many, if not most women with accreta also have placenta previa, have had a previous cesarean section, or both. A placenta previa always requires a cesarean section because the placenta is covering the cervix. Similarly, it is usually safest for women with accreta who have had a previous cesarean section to deliver their baby via cesarean again. This is especially true if the placenta is attached to the scar from the previous cesarean. Women who labor after a prior cesarean section are at risk for uterine rupture.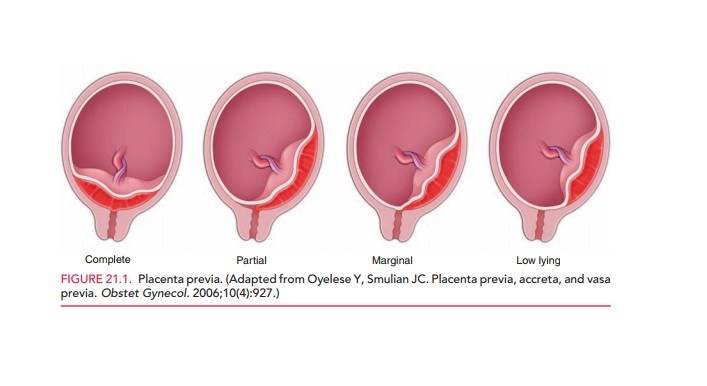 The safety of labor with a placenta invading a cesarean section scar has never been evaluated, and the risk of rupture and major hemorrhage may be higher in this situation.
The safety of labor with a placenta invading a cesarean section scar has never been evaluated, and the risk of rupture and major hemorrhage may be higher in this situation.
If you do not have a placenta previa, you may be able to deliver vaginally. However, this delivery may be complicated and is at a higher risk for hemorrhage. It is important to talk to an obstetrician with experience in this area before deciding on a vaginal versus cesarean delivery.
Myth: Placenta accreta and retained placenta always occur simultaneously.
Fact: Most women with placenta accreta will have a retained placenta (a piece of the placenta that stays in the uterus after delivery). This occurs because the accreta has grown deeply into the uterus and will not separate.
Many women without accreta experience a retained placenta. In fact, many women experience a placenta that is slow to separate from the uterus (usually after a vaginal delivery) or a placenta that won’t deliver and needs to be removed by hand.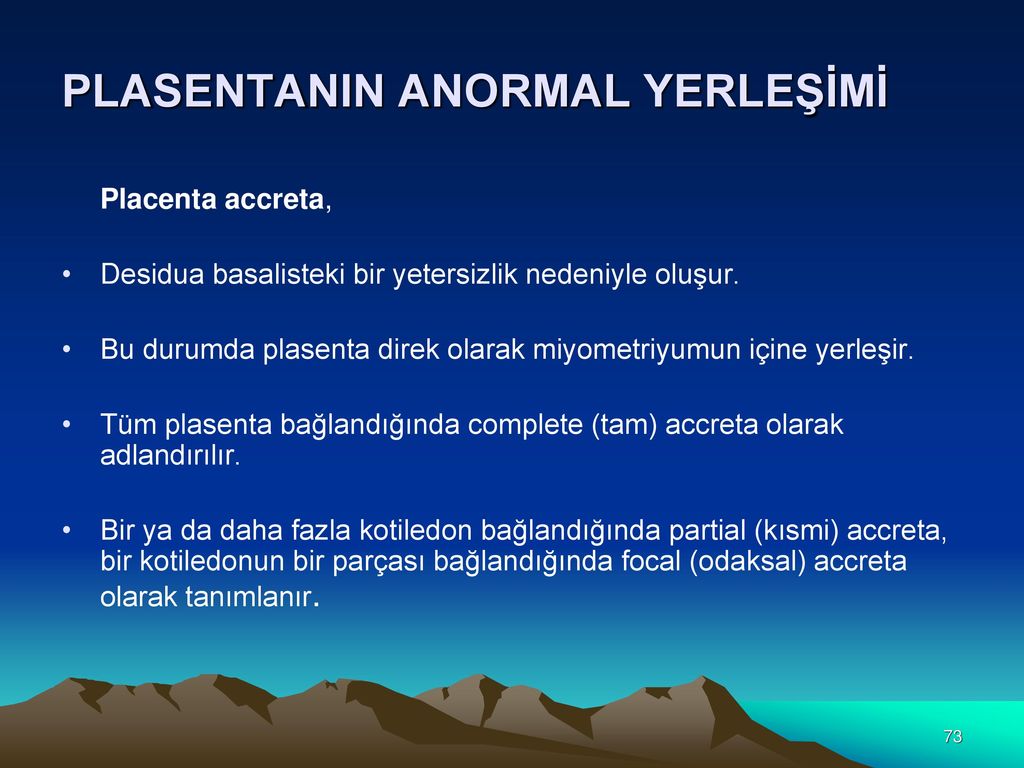 Retained placenta and accreta do not always go together.
Retained placenta and accreta do not always go together.
Myth: It is impossible to have accreta if I have never had a cesarean section before.
Fact: While a previous cesarean section is one of the strongest risk factors for accreta, there are other circumstances that can lead to accreta even without a previous cesarean. These include other types of surgery on the uterus (such as removal of fibroids or scar tissue), placenta previa, older maternal age and in vitro fertilization (IVF). Fortunately, the vast majority of patients with any of these risk factors will never experience an accreta. However, women who have placenta previa or more than one risk factor should be carefully checked for accreta.
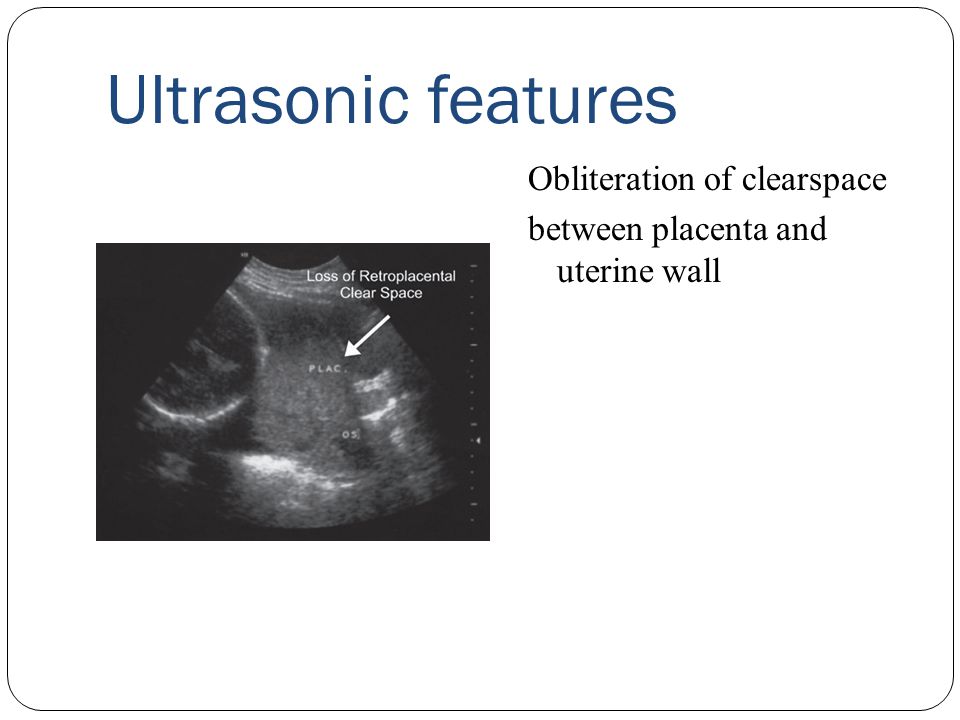
Myth: An accreta can always be detected on an ultrasound or MRI image before delivery.
Fact: An ultrasound or MRI image can usually detect an accreta, but not always. For example, an ultrasound or MRI may detect increased vascularity (or blood flow) beyond the parameters ordinarily seen.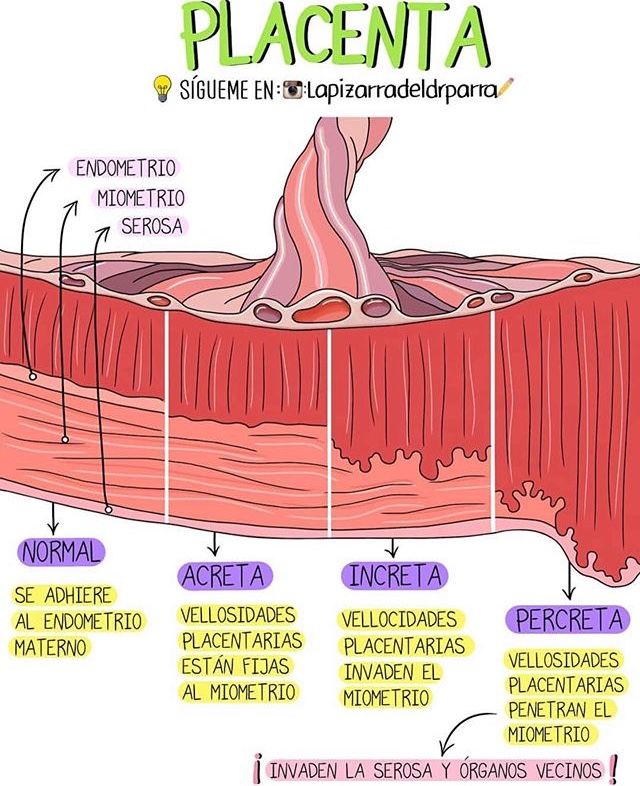 That could be evidence of a possible accreta. A pregnant uterus, however, always has extra blood flow to some degree. This makes interpreting ultrasound and MRI images particularly challenging. Having images reviewed by a radiologist and obstetrician that are experienced in identifying accreta cases is important, although even then there can be some uncertainty in diagnosis. Currently, researchers are trying to develop blood tests that will help make accreta diagnoses more accurate. For now, women at high risk for accreta should deliver with a team of experienced doctors prepared to manage an accreta and possible hemorrhage, even if accreta was not detected on the ultrasound or MRI.
That could be evidence of a possible accreta. A pregnant uterus, however, always has extra blood flow to some degree. This makes interpreting ultrasound and MRI images particularly challenging. Having images reviewed by a radiologist and obstetrician that are experienced in identifying accreta cases is important, although even then there can be some uncertainty in diagnosis. Currently, researchers are trying to develop blood tests that will help make accreta diagnoses more accurate. For now, women at high risk for accreta should deliver with a team of experienced doctors prepared to manage an accreta and possible hemorrhage, even if accreta was not detected on the ultrasound or MRI.
Myth: Women are not able to breastfeed after a cesarean and hysterectomy.
Fact: This is not the case. Some women who have a very complicated surgery and recovery will not be able to breastfeed, and their babies will develop healthfully with formula or donated breast milk.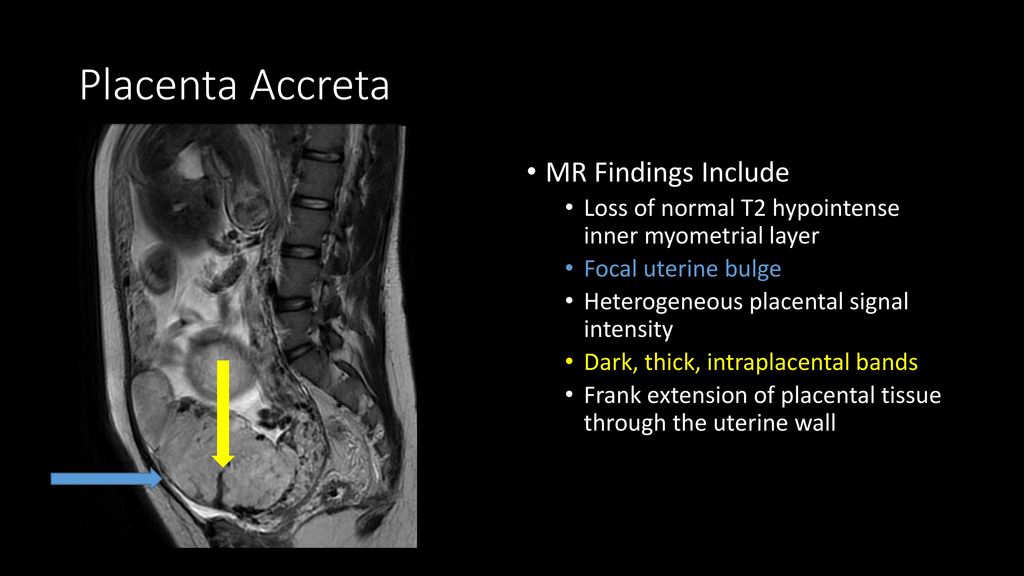 However, even after a hysterectomy or hemorrhage a mother can try to breastfeed. It is possible that the breast milk may take longer to come in given the complexity of the surgery, but women who wish to breastfeed should be supported in doing so.
However, even after a hysterectomy or hemorrhage a mother can try to breastfeed. It is possible that the breast milk may take longer to come in given the complexity of the surgery, but women who wish to breastfeed should be supported in doing so.
At Brigham and Women’s Hospital, patients are encouraged to breastfeed after a hemorrhage or hysterectomy if they feel up to it, and some have started pumping even while in intensive care.
The BWH Program for Surgical Obstetrics
- Established in 2008, our team has cared for hundreds of women with uterine and placental disorders, including placenta accreta.
- We offer accreta consultation and delivery planning, and focus on individualized care based on each patient’s particular circumstances.
- Our hospital offers 24-hour maternal fetal medicine, high-risk anesthesia, blood bank and interventional radiology coverage. Additionally, access to cell salvage, autologous blood transfusion, and a hybrid operating room are available.
In addition to delivery planning and management, we accept transfers of complicated postpartum patients and provide inter-pregnancy care, including management of retained accretas.
Consults
- Schedule a consultation with a Brigham and Women’s Obstetrician Specializing in Placenta Accreta.
- For patients with placenta accreta who have questions or are seeking another opinion contact the Mass General Brigham Online Specialty Consultations.
Psychiatric Services
Psychiatrists are available to provide immediate and ongoing support to women and couples facing stressful and high risk pregnancies. Close coordination between maternal-fetal specialists and the psychiatry team allows women to either initiate or transfer their psychiatric care to this program if needed. Learn more about this service.
Hope for Accreta
- Hope for Accreta offers information and support for women with placenta accreta.
- Find a local chapter to meet with other women in your area.

- Thank you to Sophia Watson and the women of the Hope for Accreta Foundation, who contributed myths and feedback for this site.
This information was made possible with a donation from the Hess Foundation.
Types, Risks, Causes & Treatment
Overview
Placenta accreta is a pregnancy complication that occurs when the placenta embeds too deep in the uterine wall.What is placenta accreta?
Placenta accreta is a condition where the placenta (the food and oxygen source for a fetus) grows too deeply into the wall of your uterus. In a typical pregnancy, the placenta easily detaches from the wall of your uterus after your baby is born. In placenta accreta, the placenta has grown into your uterine wall and doesn’t separate easily following delivery. In severe cases, it can lead to life-threatening vaginal bleeding. It may require a blood transfusion and hysterectomy (removal of your uterus). Pregnancy care providers diagnose placenta accreta during pregnancy or during delivery. Treatment usually involves an early Cesarean delivery (C-section) followed by a hysterectomy to minimize the risk of severe complications.
Treatment usually involves an early Cesarean delivery (C-section) followed by a hysterectomy to minimize the risk of severe complications.
What are the different types of placenta accreta?
There are three types of placenta accreta. Providers determine the type based on how deeply the placenta is attached to your uterus.
- Placenta accreta: The placenta firmly attaches to the wall of your uterus. It doesn’t pass through the wall of the uterus or impact the muscles of the uterus. This is the most common type.
- Placenta increta: In this type, the placenta is more deeply embedded in the wall of your uterus. It still doesn’t pass through the uterine wall but is firmly attached to the muscle of the uterus. Placenta increta accounts for about 15% of cases.
- Placenta percreta: The most severe of the types, placenta percreta happens when the placenta passes through the wall of your uterus. The placenta might grow through your uterus and impact other organs, such as your bladder or intestines.
 It accounts for about 5% of cases.
It accounts for about 5% of cases.
Who’s at risk for placenta accreta?
You’re at higher risk for placenta accreta if you:
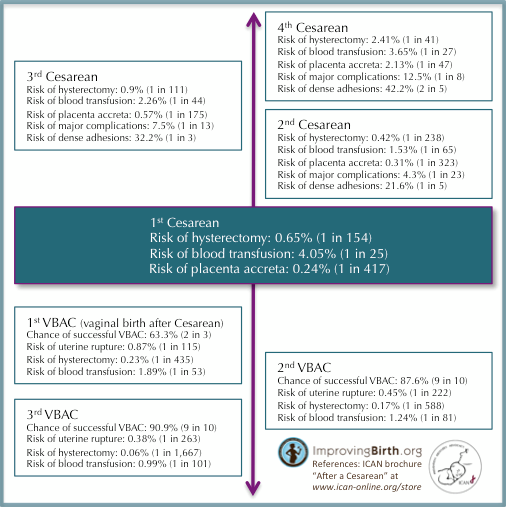
- Have had previous Cesarean deliveries.
- Have a placenta in an abnormal location in your uterus.
- Have had previous surgeries on your uterus.
- Have had more than one pregnancy.
- Are pregnant via IVF.
Does placenta accreta harm the fetus?
Placenta accreta doesn’t directly harm the fetus. Placenta accreta often leads to preterm birth. Preterm birth carries risks such as respiratory problems or trouble gaining weight. Babies born before 37 weeks of pregnancy have a higher risk of being admitted to a neonatal intensive care unit (NICU) for specialized treatment.
What are the risks of placenta accreta to the birthing person?
- Premature delivery.
- Damage to your uterus and surrounding organs.
- Loss of fertility due to hysterectomy.
- Excessive bleeding that requires a blood transfusion.

- Blood clotting issues.
- Lung or kidney failure.
- Death.
How common is placenta accreta?
Placenta accreta may affect up to 1 in 533 pregnancies. The occurrence of placenta accreta has increased over the last several decades, mostly due to the increased rate of C-sections.
Symptoms and Causes
What causes placenta accreta?
Abnormalities with the lining of your uterus cause placenta accreta. Your uterine lining can become damaged or scarred from prior uterine surgeries. It can also happen to people who haven’t had any uterine surgery.
The risk factors for placenta accreta are:
- Multiple C-sections: People who’ve had multiple C-sections have a higher risk of developing placenta accreta. This results from scarring of your uterus from the procedures. The more cesarean sections a woman has over time, the higher her risk of placenta accreta. Multiple cesareans are present in over 60% of cases.
- History of uterine surgeries: If you’ve had a uterine fibroid (a noncancerous growth or tumor of the uterine muscle) removed, the scarring could lead to placenta accreta. Surgeries such as curettage (removing tissue from your uterus) or endometrial ablation can also lead to scarring.
- Placenta previa: This condition occurs when the placenta blocks your cervix. In people with placenta previa and a history of prior C-section deliveries, the risk for placenta accreta increases with the number of C-sections they’ve had.
What are the symptoms of placenta accreta?
There are usually no symptoms of placenta accreta. In some cases, you may experience bleeding in the third trimester of pregnancy (weeks 28 to 40) or pelvic pain (from the placenta pressing on your bladder or other organs).
Diagnosis and Tests
How is placenta accreta diagnosed?
A prenatal ultrasound can diagnose placenta accreta during pregnancy. Magnetic resonance imaging (MRI) can be helpful in some cases to show how deeply the placenta has penetrated your uterine wall.
Magnetic resonance imaging (MRI) can be helpful in some cases to show how deeply the placenta has penetrated your uterine wall.
In other cases, pregnancy care providers discover placenta accreta after your baby is born. Ideally, uterine contractions expel the placenta within 30 minutes of delivery. When this doesn’t occur, your provider may suspect placenta accreta.
How important is an early diagnosis of placenta accreta?
An early diagnosis of placenta accreta is essential because it can allow multiple healthcare providers to become involved in your pregnancy and delivery care. For example, a neonatologist may be involved in your newborn’s care, or a perinatologist may be involved in yours. Your provider will monitor you closely to ensure the best results for you and your baby.
Having the right people involved could prevent the removal of your uterus (hysterectomy) or life-threatening blood loss. In some cases, providers can’t avoid a hysterectomy and blood transfusion despite an early diagnosis; however, risks for other complications decrease with early diagnosis.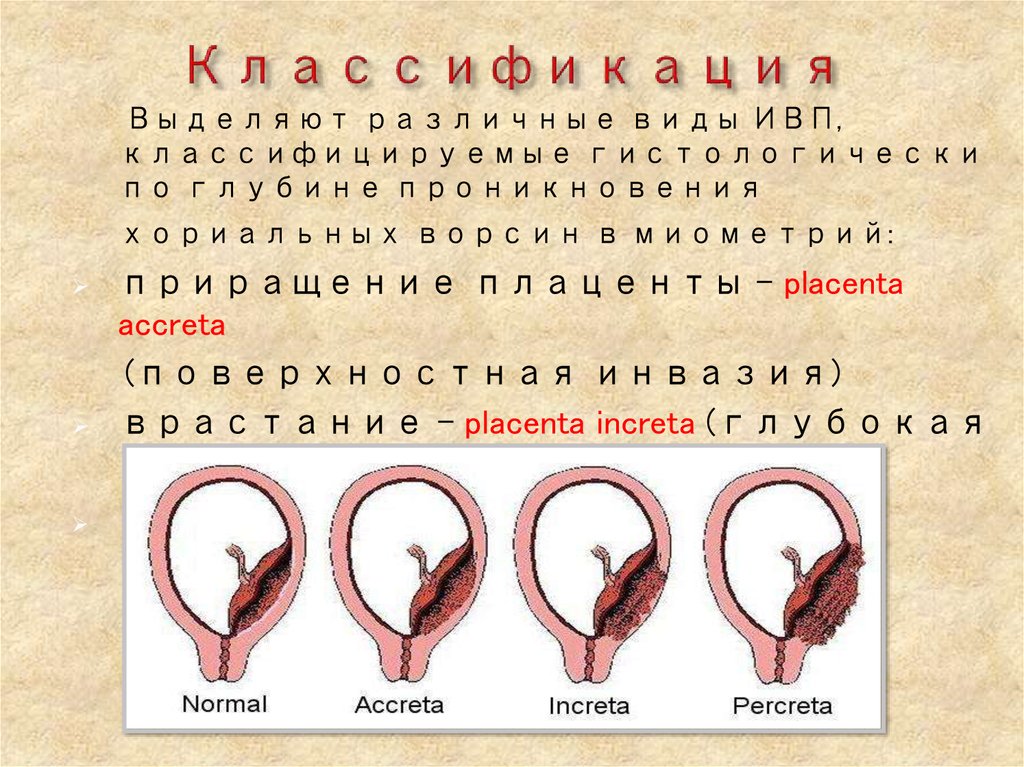
Management and Treatment
How is placenta accreta treated?
Treatment of placenta accreta can vary. If your provider diagnoses it before delivery, they’ll monitor you closely for the rest of your pregnancy. You may be hospitalized or put on bed rest to prevent preterm labor. Your provider will schedule a C-section to deliver your baby, usually around between 34 and 37 weeks. This is done to decrease the risk of bleeding from contractions or labor. If you wish to have future pregnancies, your healthcare provider can try to save your uterus.
However, in severe cases where the placenta is deeply or firmly attached or invading into other organs, a hysterectomy (removal of the uterus) may be the safest option. A Cesarean hysterectomy is when your uterus is removed at the time of a C-section delivery. In this case, your provider will deliver your baby, your uterus and the placenta at the same time. Removing your uterus with the placenta still attached minimizes the risk of excessive bleeding (hemorrhaging).
Some healthcare providers will leave small parts of the placenta inside your uterus because the placenta dissolves over time. This also carries risks like severe vaginal bleeding, infection and blood clots. It may still be difficult to get pregnant in the future.
How early do you deliver with placenta accreta?
Most healthcare providers will recommend a C-section between 34 and 37 weeks gestation if there are no complications. This prevents you from having contractions or going into labor, as these can cause significant bleeding. Your healthcare provider may give you corticosteroids to help develop the fetus's lungs.
Prevention
Can I prevent placenta accreta?
You can’t prevent placenta accreta. The risk of placenta accreta increases if you’ve had multiple C-sections or a placental disorder like placenta previa. Talk to your provider about your chances of developing placenta accreta based on your health history.
Outlook / Prognosis
What is the outlook for people with placenta accreta?
The outlook is generally good when pregnancy care providers diagnose placenta accreta during pregnancy. However, there will be complications associated with preterm labor and a possible hysterectomy. If your obstetrician removes your uterus, you’ll lose the ability to become pregnant again. This condition can also lead to massive blood loss, injury to the bowel or bladder and even death.
However, there will be complications associated with preterm labor and a possible hysterectomy. If your obstetrician removes your uterus, you’ll lose the ability to become pregnant again. This condition can also lead to massive blood loss, injury to the bowel or bladder and even death.
Can I have another baby after placenta accreta?
It depends on if you had a hysterectomy. Talk to your healthcare provider if you wish to become pregnant in the future. They may be able to prevent a hysterectomy to preserve your fertility.
What is the survival rate of placenta accreta?
The survival rate of placenta accreta is generally good. In most cases, this means you’ll have a hysterectomy to prevent postpartum hemorrhaging or other severe complications.
Living With
When should I call my healthcare provider?
Placenta accreta is a high-risk pregnancy condition. Your healthcare provider will monitor you closely and let you know what to expect for the rest of your pregnancy, delivery and recovery.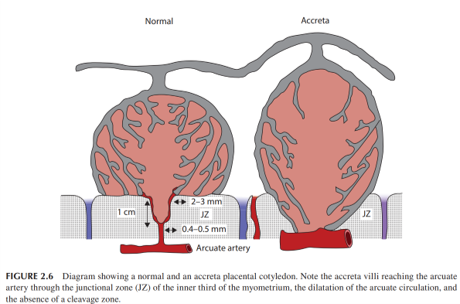 Contact them if you have questions about your diagnosis — they’re there to help you.
Contact them if you have questions about your diagnosis — they’re there to help you.
If at any point you begin bleeding heavily (soaking through a pad in less than an hour) or have pelvic pain, call 911.
What questions should I ask my obstetrician?
If you have placenta accreta, it’s normal to have questions. Some common questions to ask are:
- Will I have to give birth early?
- How is this condition treated?
- Do I need to be on bedrest or modify my daily activities?
- How do I know when to go to the hospital?
- Is a vaginal delivery possible?
- Will I be able to have a baby in the future?
- Will I need a hysterectomy?
Frequently Asked Questions
Does placenta accreta cause a hysterectomy?
Your healthcare provider makes every attempt to save your uterus; however, the risks of doing so may be too high. Most people with severe placenta accreta lose their uterus due to the life-threatening bleeding that can occur.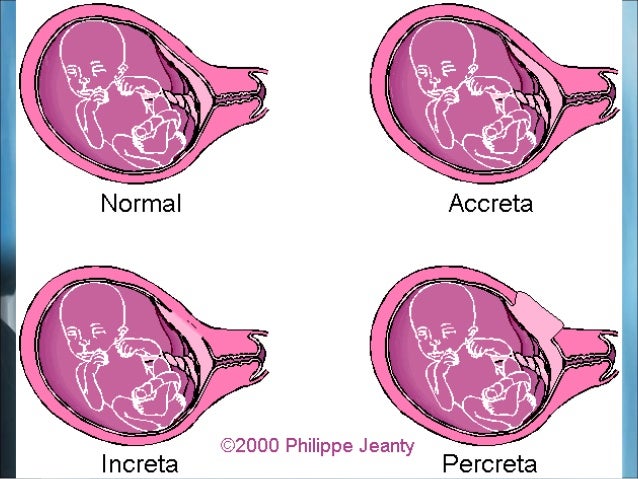 Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
A note from Cleveland Clinic
Placenta accreta is a potentially life-threatening condition that doesn’t typically cause symptoms during pregnancy. However, an early diagnosis via ultrasound and close monitoring can help lower your risk for complications from placenta accreta. In some cases, placenta accreta isn’t discovered until after your baby is delivered. Talk to your healthcare provider about what you can expect if you have placenta accreta. They’re there to keep you and your baby safe and healthy.
combined approach in operative delivery
Conditions such as placenta previa, placenta accreta can lead to catastrophic consequences for both the mother and the fetus, especially in full-term pregnancy. Obstetric bleeding due to placenta previa is one of the leading causes of maternal death [1—3].
The problem of diagnosing true placenta accreta and the development of methods for treating patients with this pathology are extremely relevant, since, on the one hand, such a pathology is associated with a high risk to a woman's life due to profuse bleeding during placental separation, often leading to hysterectomy, with the other is that its prevalence increased significantly with an increase in the number of caesarean sections [4-7]. nine0003
nine0003
One of the main factors predisposing to placenta accreta is its localization in the lower uterus and the presence of a scar after caesarean section. The risk of villus infiltration of the entire thickness of the myometrium increases with a history of several abdominal deliveries [8—10], and the situation may be complicated by the involvement of the posterior bladder wall in the pathological process.
The purpose of this work is to present a combined approach for surgical delivery of 2 patients with placental accreta in the area of the uterine scar after myomectomy, including the intraoperative use of two autonomous Zhukovsky balloon catheters (vaginal and uterine) [11], bilateral ligation of the uterine vessels, the imposition of supraplacental serous muscle hemostatic suture. nine0003
Clinical observation No. 1
Multi-pregnant, primiparous N ., 43 years old, was admitted to the maternity hospital of the budgetary health care institution of the Omsk region "Regional Clinical Hospital" 08. 11.16 with a diagnosis of pregnancy 39 weeks. Head presentation. Scars on the uterus after a small caesarean section and three myomectomy. Suspicion of placenta accreta. Isthmic-cervical insufficiency (ICI), corrected with an obstetric pessary. Gestational diabetes. Arterial hypertension is moderate. Burdened obstetric and gynecological history. nine0003
11.16 with a diagnosis of pregnancy 39 weeks. Head presentation. Scars on the uterus after a small caesarean section and three myomectomy. Suspicion of placenta accreta. Isthmic-cervical insufficiency (ICI), corrected with an obstetric pessary. Gestational diabetes. Arterial hypertension is moderate. Burdened obstetric and gynecological history. nine0003
Anthropometric data of a woman: height 164 cm, body weight 71 kg.
History had 3 myomectomy for large subserous uterine fibroids: in 2005 — laparotomy, enucleation of the node 10 cm in the left uterine angle, histological examination: cellular leiomyoma; in 2010 — laparotomy, enucleation of a 6 cm node in the left uterine angle, histological examination: leiomyoma; in 2012 — laparotomy, enucleation of a 6 cm node in the left uterine angle, histological examination: leiomyoma. nine0003
This pregnancy is the fifth, the first birth was coming. Previous pregnancies: 1) 2004 - non-developing pregnancy at 6-7 weeks of pregnancy, vacuum aspiration of the ovum; 2) 2006 - termination of pregnancy for medical reasons (congenital malformations of the fetus), small caesarean section at 20 weeks; 3) 2009 - non-developing pregnancy at 6-7 weeks, vacuum aspiration of the ovum; 4) 2012 - spontaneous abortion at 5-6 weeks of pregnancy.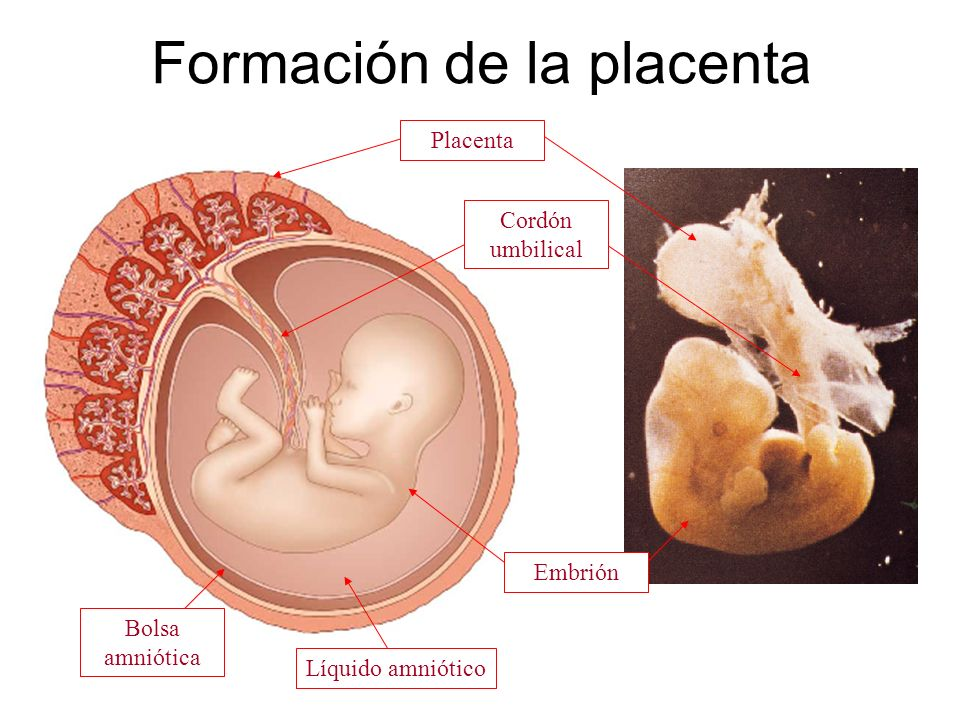
Course and complications of real pregnancy. nine0018 Registered in the antenatal clinic from the 11th week; threat of interruption - at 9 weeks, inpatient treatment. In order to correct ICI, an obstetric pessary Dr. Arabin was installed at 15–16 weeks, and she received progesterone (Utrogestan 200 mg) until 36 weeks of pregnancy. At 17 weeks there was a threat of abortion, received inpatient treatment. An increase in blood pressure (BP) up to 130/90 mm Hg was noted; the total weight gain during pregnancy was 10 kg.
At the time of receipt of complaints did not show. The general condition is satisfactory. Vision is clear. There is no headache. Skin of normal color. The abdomen is enlarged due to the pregnant uterus, palpation is soft, painless. The area of postoperative scars on the uterus is painless on palpation. The uterus is normal. The position of the fetus is longitudinal, the head is located above the entrance to the small pelvis. The fetal heartbeat is muffled, rhythmic, up to 140 beats per minute.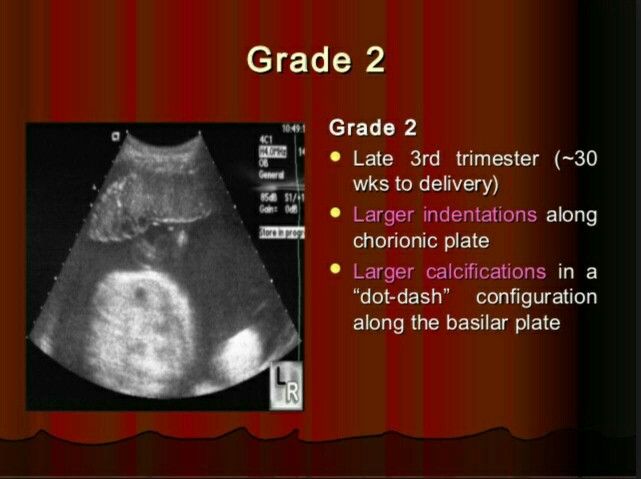 The waters are whole. There are no edema. Physiological functions are normal. Vaginal examination: nulliparous vagina, cervix - in an obstetric pessary, located in the center, up to 2.0 cm long, moderately softened, the cervical canal passes the tip of the examining finger; the fetal bladder is intact; the head is located above the entrance to the small pelvis; the basin is capacious, the cape is not achievable. nine0003
The waters are whole. There are no edema. Physiological functions are normal. Vaginal examination: nulliparous vagina, cervix - in an obstetric pessary, located in the center, up to 2.0 cm long, moderately softened, the cervical canal passes the tip of the examining finger; the fetal bladder is intact; the head is located above the entrance to the small pelvis; the basin is capacious, the cape is not achievable. nine0003
Ultrasound was performed on the SonoScape-8000Pro. There is a live fetus in the uterine cavity, head presentation, longitudinal position, I position, anterior view. Fetometric indicators of the fetus corresponded to 38.5 weeks of pregnancy. Congenital malformations were not found, the weight of the fetus was 3362 g. The placenta was located on the back wall, 10 cm higher than the internal os. The thickness of the placenta was 43 mm, III degree of maturity, structure with calcifications. The amniotic fluid index is 11.2 cm. There is no hypertonicity. The wall of the uterus in the area of placentation is thickened due to the expanded vascular network. nine0003
nine0003
At this stage, taking into account the scars on the uterus after a small caesarean section and three myomectomy, in a 43-year-old primiparous woman with a highly burdened obstetric and gynecological history, it was decided to deliver the pregnant woman by caesarean section in a planned manner.
On the same day, the patient was examined by an anesthesiologist-resuscitator, regional spinal anesthesia was recommended for caesarean section. Given the high risk of bleeding, intraoperative reinfusion of autologous erythrocytes using the Cell Saver is recommended. nine0003
On November 9, 2016 (10:50–12:10) under conditions of regional spinal anesthesia, in the presence of a perfusionist, a caesarean section was performed. The anterior abdominal wall was opened in layers from the womb to the navel. Upon opening the peritoneum, it was found that the size of the uterus corresponds to a full-term pregnancy, in the fundus of the uterus and on the left corner of the uterus - cicatricial changes in the wall after myomectomy, no myomatous nodes were detected.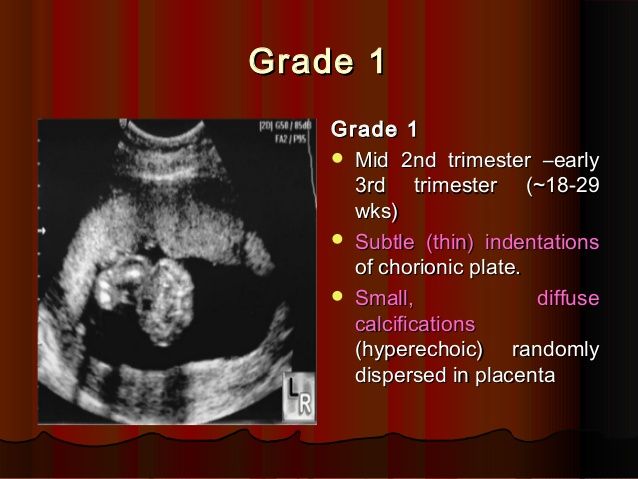 The uterine cavity was opened with a transverse incision in the region of the lower segment according to Gusakov. Light amniotic fluid was poured out in the amount of 500 ml. At the 5th minute, a live full-term boy weighing 3076 g, 51 cm tall, without visible malformations, with an Apgar score of 7 and 8 points, was removed. nine0003
The uterine cavity was opened with a transverse incision in the region of the lower segment according to Gusakov. Light amniotic fluid was poured out in the amount of 500 ml. At the 5th minute, a live full-term boy weighing 3076 g, 51 cm tall, without visible malformations, with an Apgar score of 7 and 8 points, was removed. nine0003
In order to reduce blood loss, bilateral ligation of the uterine vessels was performed. There were no signs of placental separation. External methods of separation of the placenta were without effect. It was decided to perform manual separation of the placenta. When examining the uterine cavity, the placenta was located along the posterior wall of the uterus with the transition to the bottom. When trying to separate the placenta by sawing movements of the right hand in the left uterine angle, in the area of the postoperative scar, placenta ingrowth was revealed throughout (10×10 cm). Resection of the left uterine angle with ingrown placenta was performed (Fig.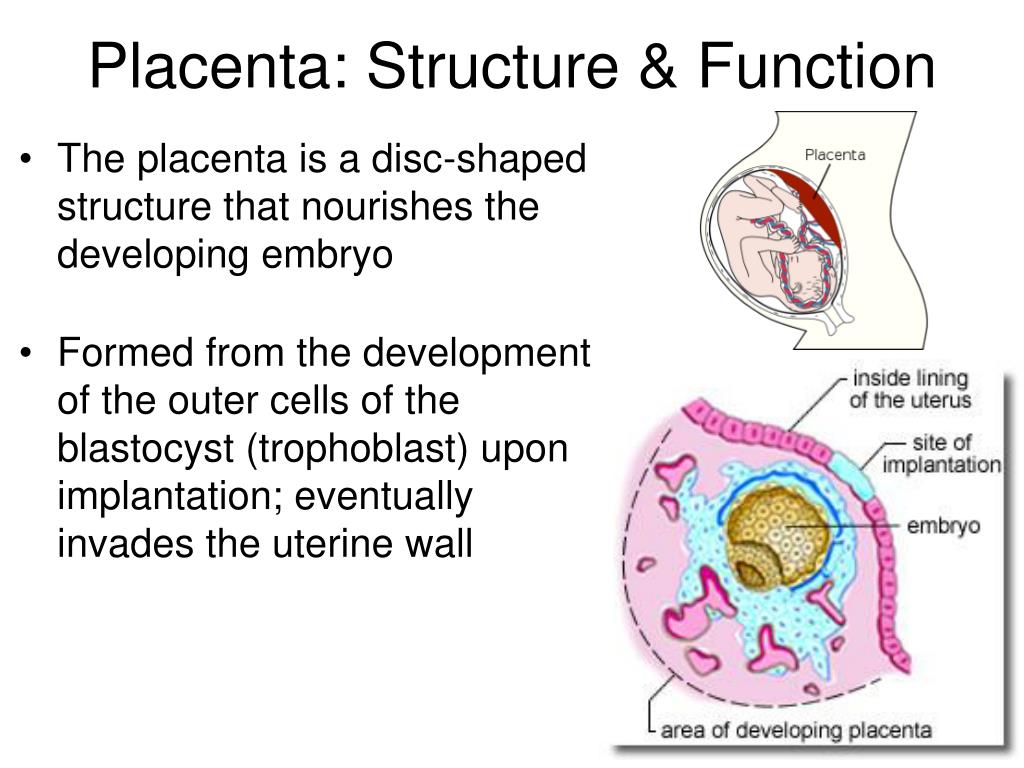 1). Rice. 1. Placenta together with the resected area of the uterine wall. a - placenta; b — resected area of the uterus with an ingrown placenta. The resected area of the uterus is sutured with separate eight-shaped sutures. A revision of the uterine cavity was made, blood clots were removed. To stop the bleeding of the area of the surgical wound on the uterus, a local hemostatic Hemoblock was used. Method of application: gauze wipes were externally sterilely moistened with a solution and applied to a bleeding, previously drained wound surface for 3 minutes. nine0003
1). Rice. 1. Placenta together with the resected area of the uterine wall. a - placenta; b — resected area of the uterus with an ingrown placenta. The resected area of the uterus is sutured with separate eight-shaped sutures. A revision of the uterine cavity was made, blood clots were removed. To stop the bleeding of the area of the surgical wound on the uterus, a local hemostatic Hemoblock was used. Method of application: gauze wipes were externally sterilely moistened with a solution and applied to a bleeding, previously drained wound surface for 3 minutes. nine0003
A supraplacental serous-muscular hemostatic suture was placed on the posterior wall of the uterus. The uterine cavity was dried with napkins. Separate Vicryl sutures were placed at the corners of the wound on the uterus. A modified balloon uterine catheter was placed through the hysterotomy incision using a guidewire, passing it through the cervical canal. The wound on the uterus is sutured with separate eight-shaped sutures.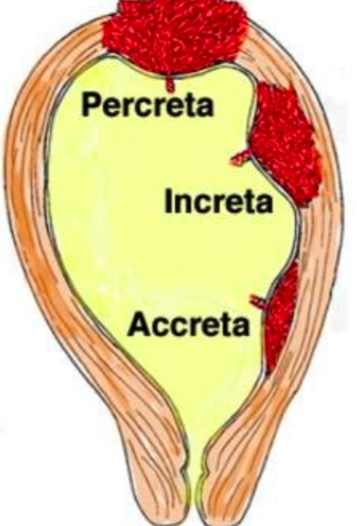 The modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought to the uterine balloon intravaginally through the conductor, filling it with 150 ml of isotonic sodium chloride solution. The duration of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1500 ml, urine output was 100 ml. Reinfusion of blood with Cell Saver 600 ml. nine0003
The modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought to the uterine balloon intravaginally through the conductor, filling it with 150 ml of isotonic sodium chloride solution. The duration of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1500 ml, urine output was 100 ml. Reinfusion of blood with Cell Saver 600 ml. nine0003
The postoperative period was uneventful, antibacterial, uterotonic therapy was carried out. The woman was discharged in a satisfactory condition with the child on the 6th day.
Histological examination of the excised area of the uterine wall with the placenta - deep ingrowth of the chorionic villi into the myometrium.
Clinical observation No. 2
Primiparous, primiparous M ., 32 years old, was admitted to the maternity hospital of the budgetary health care institution of the Omsk region "Regional Clinical Hospital" on 11/15/16 with a diagnosis of pregnancy 37 weeks.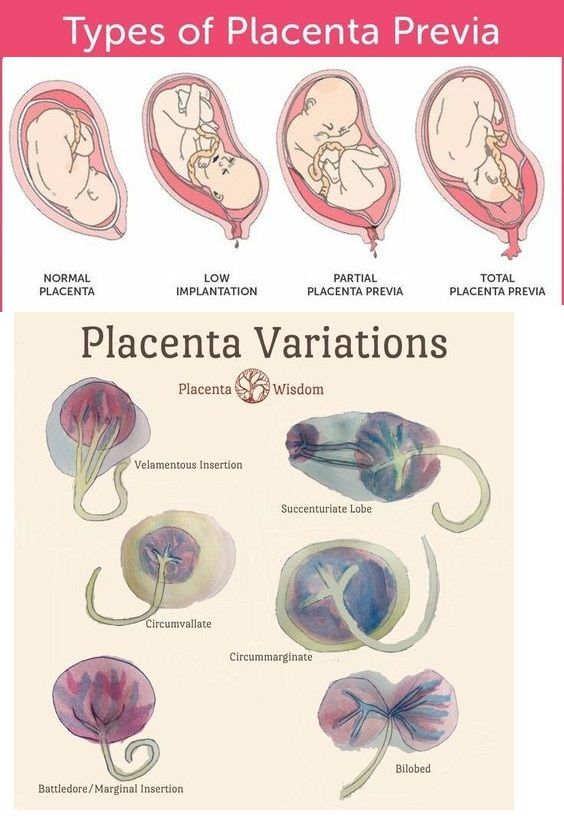 Head presentation. Scars on the uterus after myomectomy. Multiple uterine fibroids of large sizes. Isthmic-cervical insufficiency corrected with an obstetric pessary. Chronic pyelonephritis without exacerbation. Nephroptosis on the right. nine0003
Head presentation. Scars on the uterus after myomectomy. Multiple uterine fibroids of large sizes. Isthmic-cervical insufficiency corrected with an obstetric pessary. Chronic pyelonephritis without exacerbation. Nephroptosis on the right. nine0003
Anthropometric data of a woman: height 162 cm, body weight 80 kg.
History of two myomectomy for large subserous uterine fibroids: 2013 — laparotomy, enucleation of the node 8 cm in the right uterine angle, histological examination — cellular leiomyoma; 2016 (July) - laparotomy, enucleation of a 10 cm node in the left uterine angle, histological examination - leiomyoma.
The course and complications of this pregnancy: registered in the antenatal clinic since 10 weeks; in order to correct CCI at 17 weeks, an obstetric pessary Dr. Arabin was installed, she received progesterone (Utrogestan 400 mg) up to 36 weeks; the total weight gain during pregnancy was 8 kg. nine0003
At the time of receipt of complaints did not show.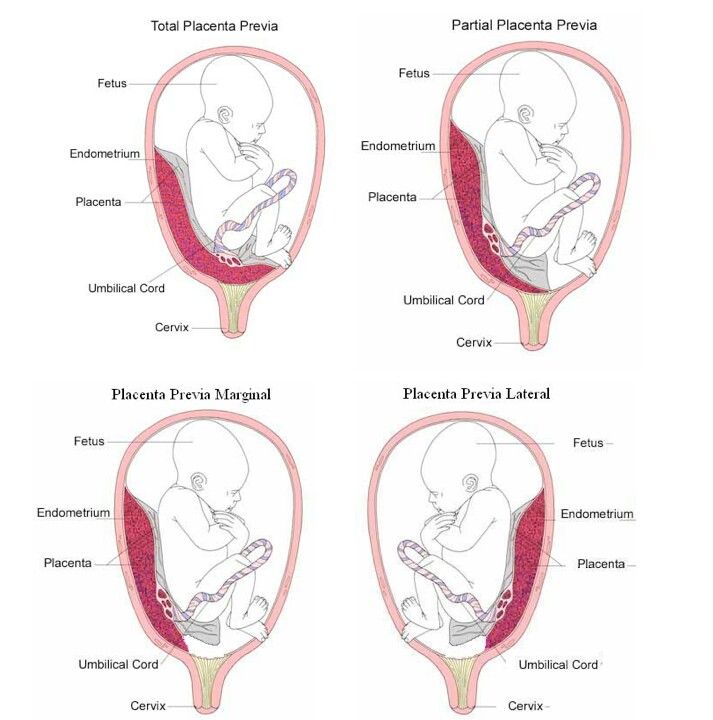 The general condition is satisfactory. Vision is clear. There is no headache. Skin of normal color. The abdomen is enlarged due to the pregnant uterus, on palpation it is soft, painless. The area of the postoperative scar on the uterus is painless on palpation. The uterus is normal. The position of the fetus is longitudinal, the head is located above the entrance to the small pelvis. The fetal heartbeat is muffled, rhythmic, up to 150 beats per minute. The waters are whole. There are no edema. Physiological functions are normal. Vaginal examination: nulliparous vagina, cervix - in an obstetric pessary, in the center, up to 1.5 cm long, moderately softened, the cervical canal passes the tip of the examining finger; the fetal bladder is intact; the head is located above the entrance to the small pelvis; the basin is capacious, the cape is not achievable. nine0003
The general condition is satisfactory. Vision is clear. There is no headache. Skin of normal color. The abdomen is enlarged due to the pregnant uterus, on palpation it is soft, painless. The area of the postoperative scar on the uterus is painless on palpation. The uterus is normal. The position of the fetus is longitudinal, the head is located above the entrance to the small pelvis. The fetal heartbeat is muffled, rhythmic, up to 150 beats per minute. The waters are whole. There are no edema. Physiological functions are normal. Vaginal examination: nulliparous vagina, cervix - in an obstetric pessary, in the center, up to 1.5 cm long, moderately softened, the cervical canal passes the tip of the examining finger; the fetal bladder is intact; the head is located above the entrance to the small pelvis; the basin is capacious, the cape is not achievable. nine0003
Ultrasound was performed on the SonoScape-8000Pro. There is a live fetus in the uterine cavity, head presentation, longitudinal position, I position, anterior view. Fetometric indicators of the fetus correspond to 37 weeks. Congenital malformations were not found, the weight of the fetus was 2914. The placenta was located along the back wall with a transition to the bottom, 9 cm higher than the internal os. The thickness of the placenta is 37 mm, III degree of maturity. The amniotic fluid index is 21.7 cm. There is no hypertonicity. In the lower segment, along the posterior wall, a myomatous node of size 69 is determined.×64×63 mm. In the bottom of the uterus, two myoma nodes are determined in the placentation zone, 38 × 15 × 31 and 45 × 42 × 43 mm in size, with color Doppler mapping (DDC) - avascular.
Fetometric indicators of the fetus correspond to 37 weeks. Congenital malformations were not found, the weight of the fetus was 2914. The placenta was located along the back wall with a transition to the bottom, 9 cm higher than the internal os. The thickness of the placenta is 37 mm, III degree of maturity. The amniotic fluid index is 21.7 cm. There is no hypertonicity. In the lower segment, along the posterior wall, a myomatous node of size 69 is determined.×64×63 mm. In the bottom of the uterus, two myoma nodes are determined in the placentation zone, 38 × 15 × 31 and 45 × 42 × 43 mm in size, with color Doppler mapping (DDC) - avascular.
At this stage, taking into account the scars on the uterus after two myomectomy, including 07/05/16, multiple large uterine myoma, it was decided to deliver the pregnant woman ahead of schedule by caesarean section in a planned manner.
Examined by an anesthesiologist-resuscitator, regional spinal anesthesia was recommended for caesarean section. Given the high risk of bleeding, intraoperative reinfusion of autologous erythrocytes using the Cell Saver is recommended. nine0003
Given the high risk of bleeding, intraoperative reinfusion of autologous erythrocytes using the Cell Saver is recommended. nine0003
On November 18, 2016 (9:15–10:50 a.m.), a caesarean section was performed under conditions of regional spinal anesthesia in the presence of a perfusionist. The anterior abdominal wall was opened in layers from the womb to the navel. After opening the peritoneum, the uterine cavity was opened with a transverse incision in the region of the lower segment according to Gusakov. Light amniotic fluid was poured out in the amount of 400 ml. At the 5th minute, a live full-term boy weighing 2743 g, 49 cm tall, without visible malformations, with an Apgar score of 7 and 7 points, was removed. nine0003
The uterus was brought out into the wound, the following was found (Fig. 2): 2. Subserous uterine fibroids, hernial protrusion in the scar on the uterus after myomectomy. a - retrocervical interstitial-subserous myomatous node; b - hernial protrusion; c — interstitial-subserous myoma node in the bottom area. along the posterior wall in the lower segment - an interstitial-subserous myomatous node with a diameter of 9 cm, in the bottom area - an interstitial-subserous myomatous node with a diameter of 6 cm. hernia), severe varicose veins of the uterine appendages. In order to reduce blood loss, bilateral ligation of the uterine vessels was performed with an unseparated placenta. nine0003
along the posterior wall in the lower segment - an interstitial-subserous myomatous node with a diameter of 9 cm, in the bottom area - an interstitial-subserous myomatous node with a diameter of 6 cm. hernia), severe varicose veins of the uterine appendages. In order to reduce blood loss, bilateral ligation of the uterine vessels was performed with an unseparated placenta. nine0003
The placenta was removed by pulling on the umbilical cord, the placenta is located on the back wall. The bed of hernial protrusion was examined: a site of ingrowth of placental tissue was found; there is no bleeding. A transverse incision was made on the uterus, myomectomy of the posterior cervical node was performed. The bed was sutured with eight-shaped sutures, the wound was sutured with a two-row vicryl suture. To stop bleeding in the area of the surgical wound on the uterus, a local hemostatic Hemoblock was used (Fig. 3). Rice. 3. The use of hemoblock after myomectomy with hernial protrusion. a - hernial protrusion; b — local hemostatic Hemoblock. Acute hernia repair was performed. The scar tissue with areas of placenta ingrowth was excised and removed (Fig. 4). Rice. 4. Excision of the site of placenta ingrowth. The bed was sutured with eight-shaped sutures, the wound was sutured with a two-row vicryl suture. Similarly produced myomectomy interstitial-subserous myomatous nodes in the fundus of the uterus. nine0003
Acute hernia repair was performed. The scar tissue with areas of placenta ingrowth was excised and removed (Fig. 4). Rice. 4. Excision of the site of placenta ingrowth. The bed was sutured with eight-shaped sutures, the wound was sutured with a two-row vicryl suture. Similarly produced myomectomy interstitial-subserous myomatous nodes in the fundus of the uterus. nine0003
The uterine cavity was inspected, blood clots were removed. To stop the bleeding of the area of the surgical wound on the uterus, a local hemostatic Hemoblock was used. A supraplacental serous-muscular hemostatic suture was placed on the posterior wall. The uterine cavity was dried with napkins. Separate Vicryl sutures were placed at the corners of the wound on the uterus. For the purpose of controlled tamponade of the uterus, a modified balloon uterine catheter was installed through a hysterotomy incision with the introduction of a conductor through the cervical canal. The wound on the uterus is sutured with separate eight-shaped sutures. The modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought to the uterine balloon intravaginally through the conductor, filling it with 120 ml of isotonic sodium chloride solution. The duration of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1100 ml, urine output was 150 ml. Reinfusion of blood with the Cell Saver device - 500 ml. nine0003
The modified balloon uterine catheter was filled with isotonic sodium chloride solution after suturing the wound on the uterus, then the vaginal module was brought to the uterine balloon intravaginally through the conductor, filling it with 120 ml of isotonic sodium chloride solution. The duration of the vaginal and uterine catheters was 14 hours. Intraoperative blood loss was 1100 ml, urine output was 150 ml. Reinfusion of blood with the Cell Saver device - 500 ml. nine0003
The postoperative period was uneventful, antibacterial, uterotonic therapy was carried out. The mother was discharged in a satisfactory condition with the child on the 6th day.
Histological conclusion: excised area of the uterine wall with placenta - deep ingrowth of chorionic villi into the myometrium.
Thus, the above examples show that the use of a combined approach in the surgical delivery of patients with placenta accreta in the area of the uterine scar after myomectomy, including the intraoperative use of two autonomous Zhukovsky balloon catheters (vaginal and uterine), bilateral ligation of the uterine vessels, the imposition of supraplacental serous muscle hemostatic suture, allows you to perform organ-preserving operations and preserve the reproductive function of patients.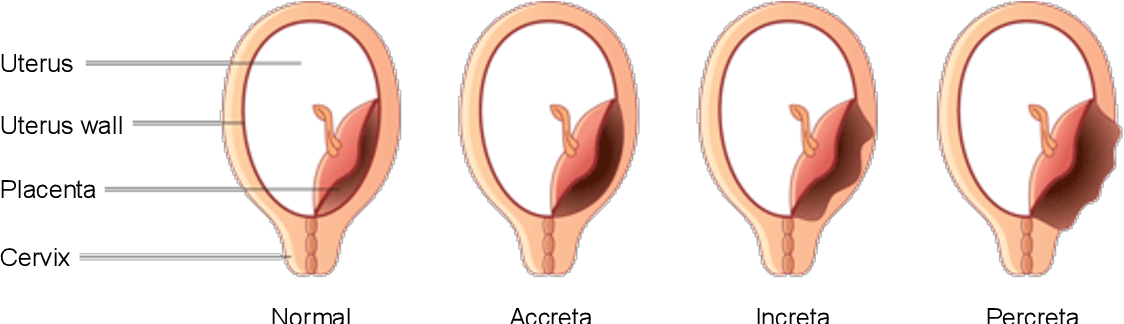 nine0003
nine0003
The authors declare no conflict of interest.
*e-mail: [email protected];
ORCID: http://orcid.org/0000-0002-0357-7097
True placenta accreta (placenta accreta). Conservative therapy » Obstetrics and Gynecology
An observation of successful conservative treatment of 2 patients with true placenta ingrowth is given. Both patients had placenta previa and a scar on the uterus after caesarean section. Placenta ingrowth was diagnosed during pregnancy with echography and magnetic resonance imaging. Taking into account the diagnosis, it was decided to perform a bottom caesarean section with subsequent embolization of the uterine arteries. The placenta was left in situ. In the postoperative period, delayed re-embolization of the uterine arteries was performed. After partial expulsion of the placenta, the remnants of the placental tissue were removed by curettage and hysteroscopy. During dynamic observation, the patients had a complete restoration of menstrual function.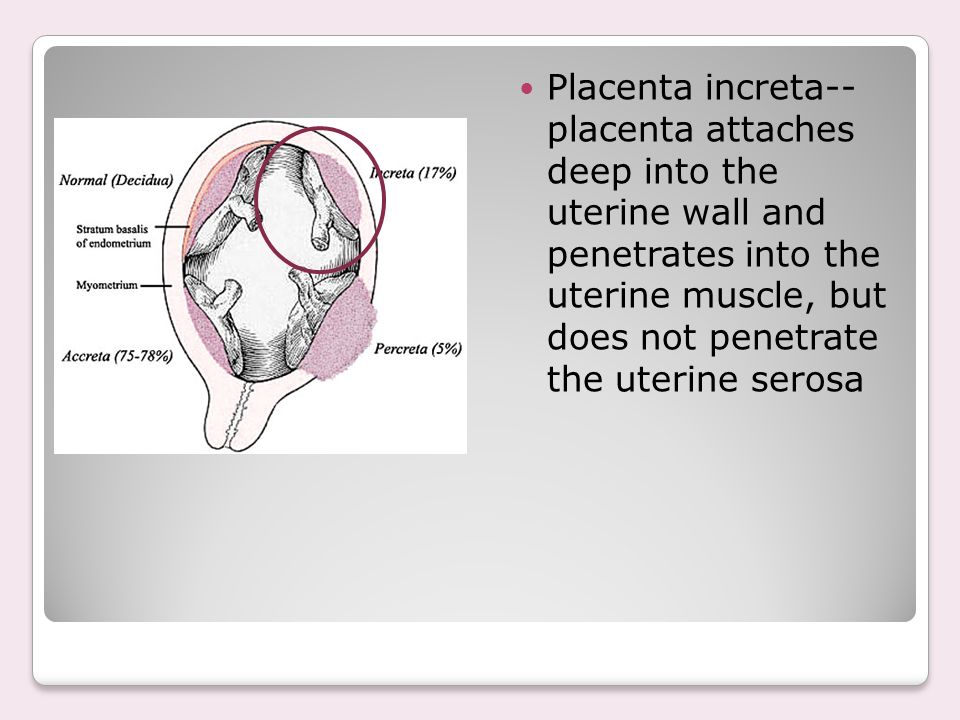 nine0003
nine0003
The problem of diagnosing true placenta ingrowth (IIP) and the development of methods for treating patients with this pathology are extremely relevant, since, on the one hand, such a pathology is associated with a high risk to the life of a woman due to profuse bleeding during placental separation, on the other - Its prevalence has increased significantly with an increase in the number of caesarean sections.
There are different types of IVP, classified histologically according to the depth of penetration of chorionic villi into the myometrium: placenta accreta - placenta accreta (superficial invasion),
ingrowth - placenta increta (deep invasion) and germination - placenta percreta. Placenta increment is such an attachment to the wall of the uterus, when there is no spongy layer of the decidua between the muscle layer and the villi of the chorion and the villi reach the muscle layer of the uterus and even penetrate into it. The most rare and severe form is
placenta percreta, which is found in 5–7% of all variants of IVP.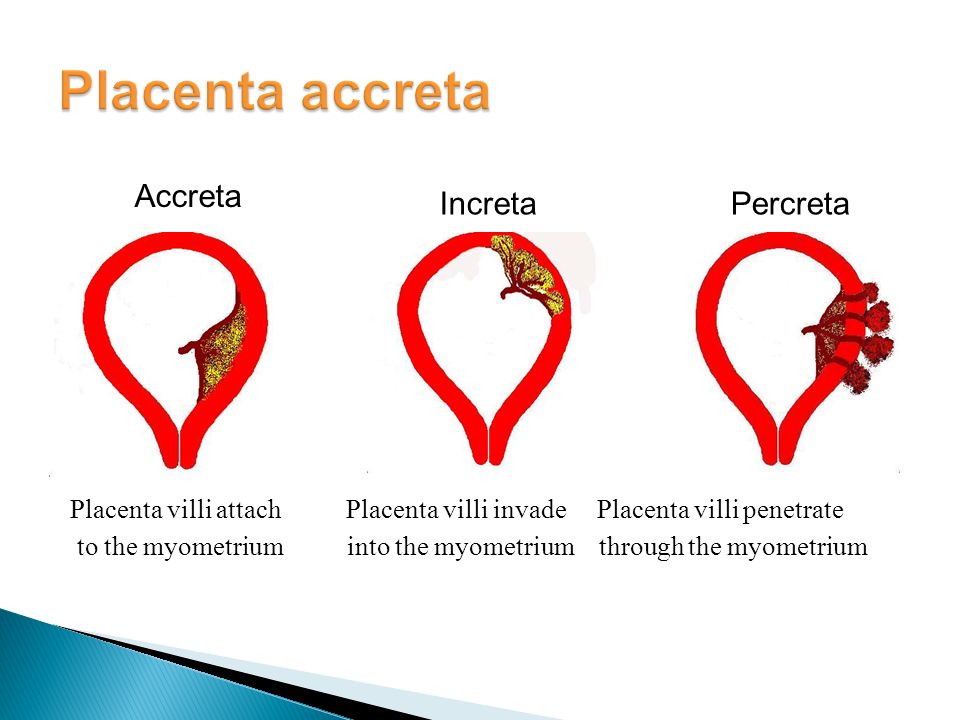 In Russia and abroad,
In Russia and abroad,
placenta percreta is interpreted as villi infiltration of the entire thickness of the myometrium,0091 serous membrane and damage to neighboring organs [18].
ITI occurs with a frequency of 1 in 2500-7000 births [16-18] and varies from 1:540 births in Thailand,
1:1000 births in South Africa to 1:93,000 births in the USA [9, 18]. Over the past 50 years,
10-fold increase in the number of patients with IVP has been noted [13, 18, 21, 22]. Many authors have noted a correlation
between an increase in the number of placenta accreta and an increase in the number of caesarean sections [4, 5, 14,
17–19, 20].
The increase in the prevalence of IVP is influenced not only by the frequency, but also by the type of suturing per incision
uterus for caesarean section [17]. Traditional was a 2-row suture on the lower uterine segment. But since 1990, a single-row suture has gained clinical approval, which has reduced operative time and maternal morbidity.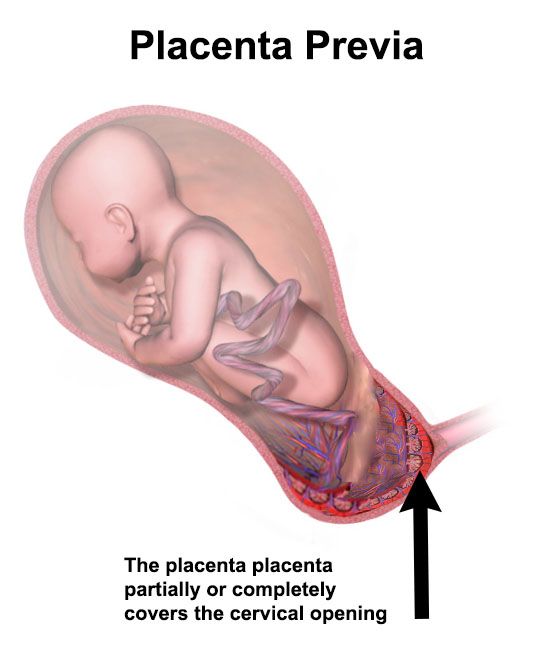 However, it can be assumed that a change in the surgical technique entails an increase in the risk of uterine rupture and the number of patients with placenta ingrowth.
However, it can be assumed that a change in the surgical technique entails an increase in the risk of uterine rupture and the number of patients with placenta ingrowth.
Placenta accreta is known to be associated with massive blood loss (up to 3000–5500 ml)
at the time of placental separation. The risk of uncontrolled bleeding increases with involvement of
posterior bladder wall. Complications in an attempt to separate the placenta and subsequent
hysterectomy are disseminated intravascular coagulation syndrome, damage to the ureters and bladder, infectious complications, fistula formation.
In the past, placenta accreta was diagnosed at the time of delivery and histological examination of the
removed uterus, with disastrous consequences for patients. Currently, ultrasound, color Doppler and magnetic resonance imaging data provide invaluable assistance in the diagnosis of this pathology. nine0003
For a long time, the prevailing opinion in obstetrics was that the treatment for
placenta accreta consisted of hysterectomy after caesarean section without attempting to remove the placenta [1, 2, 6, 9, 23].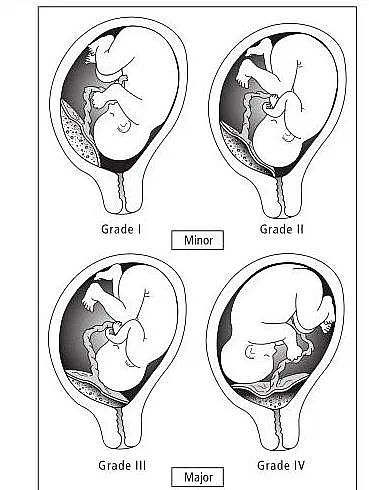 Since 1996, placenta accreta has become the leading indication for hysterectomy, overtaking previously leading uterine ruptures and refractory bleeding [6].
Since 1996, placenta accreta has become the leading indication for hysterectomy, overtaking previously leading uterine ruptures and refractory bleeding [6].
Over the past decade, the approach to treating patients with placenta accreta has changed: the old dogma against leaving even a part of the placenta in the uterus has given way to more conservative methods. nine0003
For the first time, a conservative method was described in 1986 [3] and consisted of leaving the placenta in the uterus during caesarean section and intravenous administration of 50 mg of methotrexate. Placental expulsion occurred 11 days later. In the literature, one can find various forms of alternative treatment for placenta accreta, represented by local resection of the placental bed and the use of methotrexate after leaving the placenta in situ [11, 12]. Many works are devoted to the study of methods for the diagnosis and conservative treatment of placenta ingrowth. The authors proposed an organ-preserving technique based on various options for metroplasty [8, 9, 15].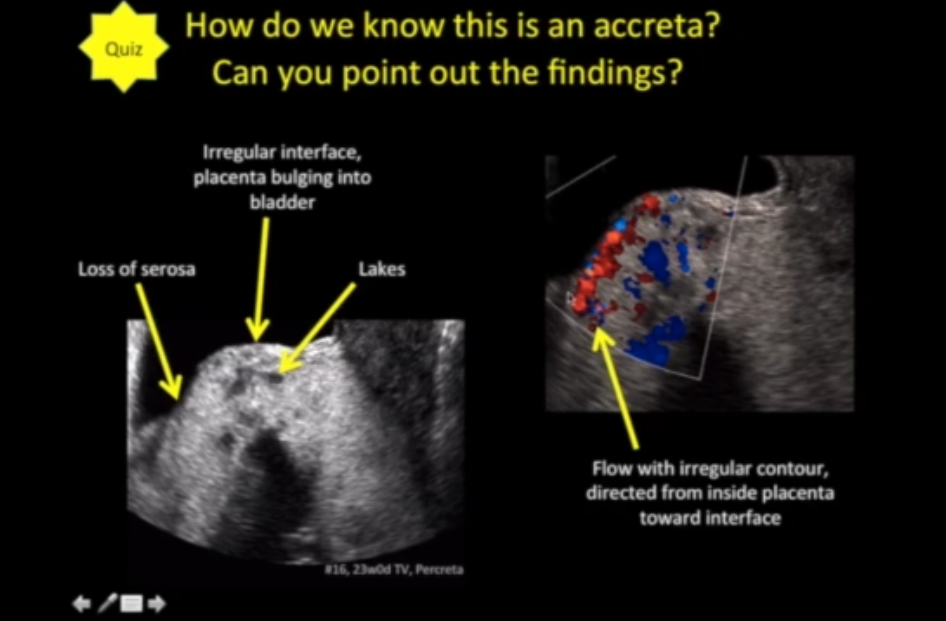
Conservative treatment includes caesarean section, placement of placenta in situ. Additionally,
is used for uterine artery embolization, parenteral methotrexate, or both [4, 18–20].
An important point in the surgical tactics for IVP is an incision on the uterus. It is best to avoid damage to placental tissue. The authors proposed a classic corporal and high transverse incision. In recent years, a transverse incision in the fundus of the uterus has become increasingly popular, minimizing blood loss, providing atraumatic fetal extraction and good visualization of the inner surface of the lower uterine segment [7, 10, 18]. nine0003
In most cases, it is impossible to do without surgical intervention, including
delayed (from 2 to 6 weeks) hysterectomy and manual removal of the placenta [11]. A decrease in the volume of blood transfusions and a decrease in the frequency of hysterectomy with a conservative approach have been noted
[8]. Conservative treatment reduces intraoperative blood loss by 2 times (from 2989 to 1411
ml). Secondary surgical intervention with conservative tactics is required in ⅓ of patients.
Secondary surgical intervention with conservative tactics is required in ⅓ of patients.
A conservative approach is appropriate in situations of intraoperative finding of placenta accreta,
especially if the obstetrician is not confident enough in the method of extirpation of the uterus or there is no technical possibility of adequate and competent treatment of massive blood loss.
We present an observation of successful conservative treatment of 2 patients with IVP, which was carried out at the Center for Family Planning and Reproduction (CPSR) in 2009.
Observation 1. According to the anamnestic data, menstruation from the age of 14 for 5 days, after 30 days, moderate, painless, regular. Somatically healthy. Past gynecological diseases: chronic adnexitis, cervical ectopia, genital herpes, genital chlamydia. Pregnancy fourth, artificial abortions two, childbirth second. The first birth was operative, by caesarean section in the lower uterine segment due to a clinically narrow pelvis, the child died. Objectively: the uterus is enlarged, corresponding to 31 weeks of pregnancy, in normotonus. The position of the fetus is longitudinal, the head of the fetus is high above the entrance to the small pelvis. The area of the scar on the uterus is painless. nine0003 Ultrasound examination revealed placenta previa. The placenta was located along the anterior, lateral wall, overlapping the internal os, and passed to the posterior wall of the uterus. There were multiple hypoechoic inclusions in the placental tissue, the myometrium of the anterior wall of the uterus was absent for 6 cm, hypervascularization of the border of the serous membrane of the uterus with the bladder was noted. Magnetic resonance imaging was performed to clarify the prevalence of placental invasion. The anterior wall of the uterus in the lower segment was evenly thinned (muscle fibers were practically not visualized, in the middle segment the wall thickness was 7–8 mm), in the projection of the serous membrane there were multiple convoluted vascular structures up to 2–3 cm in diameter, evidence of ingrowth into the urinary tract. bubble was gone. The asymmetry of the neck was determined due to the thickening of the posterior lip: posterior - 25 mm, anterior - 9mm. The posterior lip of a heterogeneous structure due to multiple convoluted vessels, which extended to the isthmus of the posterior wall, were determined in the lumen of the cervical canal and continued into the placenta. Diagnosis at admission: pregnancy 31 weeks. Scar on the uterus after caesarean section. Complete placenta previa. Ingrown placenta. Postnatal death of a child in anamnesis. It was decided to prolong the pregnancy under close control of vaginal discharge. On the 6th day on magnetic resonance imaging: the uterus is enlarged in size, in the cavity of its placenta, overlapping the internal os, with the presence of a large number of vessels in the underlying sections of the uterine wall (Fig. 1, see insert). The level of human chorionic gonadotropin (hCG) decreased from 12807 IU/ml on the 1st day to 1284 IU/ml on the 18th day. The patient was discharged on the 18th day, the placenta remained in the uterus. nine0003 On the 23rd day, ultrasound revealed severe vascularization of the placenta in the region of the lower uterine segment, for which repeated embolization of the uterine arteries was performed and 50 mg of methotrexate was administered. On the 66th day, the patient was hospitalized due to pain in the lower abdomen and bleeding. When magnetic resonance imaging was determined decreased in size of the uterus with smooth contours, without significant deformation of the walls. In the uterine cavity, there is a heterogeneous liquid content, as well as a significantly reduced placenta of a heterogeneous structure (Fig. On the 69th day there was a partial expulsion of the placenta, the remains of the placental tissue were removed with Placental tissue was histologically determined in a state of necrosis with a large number of petrificates and foci of leukocyte infiltration. At the control magnetic resonance imaging on the 76th day: the body of the uterus decreased The patient is regularly followed up at the Center for Psychiatry. Her condition is satisfactory. Observation 2. According to the anamnestic data, menstruation from the age of 14 for 3 days, after 28 days, moderate, painless, regular. Somatically healthy. Fourth pregnancy, non-developing Objectively: the uterus is enlarged according to full-term pregnancy, in normotonus. On palpation, the scar area is painless. The position of the fetus is longitudinal, the head of the fetus is high above the entrance to the small pelvis. nine0003 An ultrasound examination at the Center for Psychiatric Surgery confirmed presentation and diagnosed placenta accreta. Diagnosis at admission: pregnancy 34-35 weeks. Uterine scar after 2 caesarean sections. Complete placenta previa. True placenta accreta. nine0003 The patient was delivered at 36–37 weeks as planned. After catheterization of the femoral arteries and the installation of conductors in the uterine arteries under epidural anesthesia, a median laparotomy and a longitudinal incision in the bottom of the uterus were performed. A live full-term boy weighing 3570 g, 52 cm long, with an Apgar score of 7/8 points was retrieved. Uterine artery embolization was performed. The placenta was left in situ, the incision on the uterus was sutured. Intraoperative blood loss was 700 ml. In the postoperative period, antibacterial, uterine contraction therapy was performed. On the 6th day with magnetic resonance imaging: the uterus is enlarged. In the uterine cavity, the placenta is visualized, covering the internal os. The patient was discharged on the 14th day. The level of hCG at discharge is 910 IU / ml. On the 42nd day, due to revascularization of the placental tissue, repeated embolization of the uterine arteries was performed. On the 52nd day, the patient developed cramping pains, increased blood discharge. Ultrasound showed a shortening of the cervix, blood flow was detected in the placental tissue along the anterior wall of the uterus. There was a partial expulsion of the placenta, the remnants of the placental tissue were removed by hand. The blood loss was 1500 ml. With magnetic resonance imaging at 59On the 1st day, a decrease in the size of the uterus was noted. A significant amount of hemorrhagic contents was determined in the uterine cavity, the presence of placental tissue in the fundus On the 63rd day, hysteroscopy and resection of placental tissue were performed. Histologically, the tissue of the placenta and membranes in a state of necrosis, decidual plate with focal leukocyte infiltration. Control magnetic resonance imaging on the 81st day (Fig. 3, see inset) revealed a uterus measuring 65×73×65 mm. The uterine cavity up to 36 mm wide due to heterogeneous liquid content and gas bubbles, there was a hernial protrusion of the anterior wall in the lower third with local thinning of the myometrium up to 4 mm. nine0003 Currently, the patient's condition is satisfactory. There was a restoration of menstrual function. Thus, the above examples confirm the literature data on the possibility of leaving the placenta in the uterus during caesarean section with its ingrowth. It is difficult to answer the question of whether leaving the placenta in situ is a panacea, since we could only present data from two observations. But it is clear that: 1) in patients with IVP, an incision on the uterus (often in the bottom) during caesarean section should be made above the location of the placenta; 2) if the operating physician unexpectedly detects placenta ingrowth during cesarean section, no attempts should be made to remove it in order to avoid massive bleeding. 1. Ailamazyan E.K., Repina M.A., Kuzminykh T.U. Another look at the problem of obstetric bleeding // Zhurn. obstetrics and wives. Bol. - 2008. - No. 3. - C. 3–11.
houses in Moscow in TsPSiR with suspected ingrowth of placenta previa. No complaints were made on admission. From the anamnesis it is known that the pregnant woman received tocolytic therapy for 4 weeks with a positive effect on the threat of abortion. Despite the fact that the patient was registered for pregnancy from an early date and was repeatedly treated in a hospital, placenta previa was diagnosed only at 27 weeks. nine0003
nine0003 
 At 34–35 weeks, due to the release of 250 ml of blood from the genital tract, an emergency delivery was performed. The femoral arteries were catheterized on the operating table before the incision of the anterior abdominal wall, the conductors were installed in the uterine arteries. Under epidural anesthesia, a median laparotomy was performed, a longitudinal incision was made in the fundus of the uterus. A live premature girl weighing 2220 g, 46 cm long, with an Apgar score of 7/8 points, according to Silverman - 2/3 points, was retrieved. Uterine artery embolization was performed. The placenta was left in situ, 50 mg of methotrexate was injected into the umbilical cord vein. The cord residue is ligated, cut off. The incision on the uterus is sutured with a 3-row vicryl suture. Intraoperative blood loss is
At 34–35 weeks, due to the release of 250 ml of blood from the genital tract, an emergency delivery was performed. The femoral arteries were catheterized on the operating table before the incision of the anterior abdominal wall, the conductors were installed in the uterine arteries. Under epidural anesthesia, a median laparotomy was performed, a longitudinal incision was made in the fundus of the uterus. A live premature girl weighing 2220 g, 46 cm long, with an Apgar score of 7/8 points, according to Silverman - 2/3 points, was retrieved. Uterine artery embolization was performed. The placenta was left in situ, 50 mg of methotrexate was injected into the umbilical cord vein. The cord residue is ligated, cut off. The incision on the uterus is sutured with a 3-row vicryl suture. Intraoperative blood loss is
fork 400 ml, total - 650 ml. In the postoperative period, antibiotic therapy was performed, enzaprost was used as a uterotonic, and methotrexate 50 mg was administered intravenously on days 1, 8, and 15.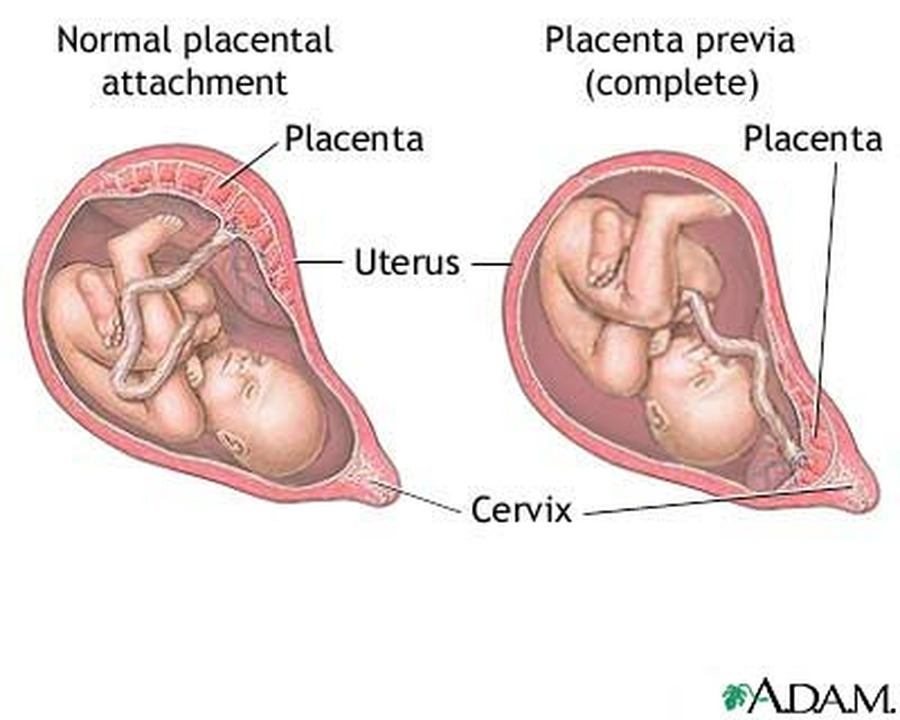
 2, see insert). nine0003
2, see insert). nine0003
curette after embolization of the uterine arteries. The blood loss was 1000 ml.
to 80×64×67 mm. Reliably placental tissue in the uterine cavity was not observed. Deformation of the myometrium was detected in the lower third of the anterior wall (thinning of the wall up to 8–9mm).
Patient M. , 32 years old, was transferred from the maternity hospital in Moscow to the Center for planned operative delivery, taking into account placenta previa and suspected true placenta ingrowth.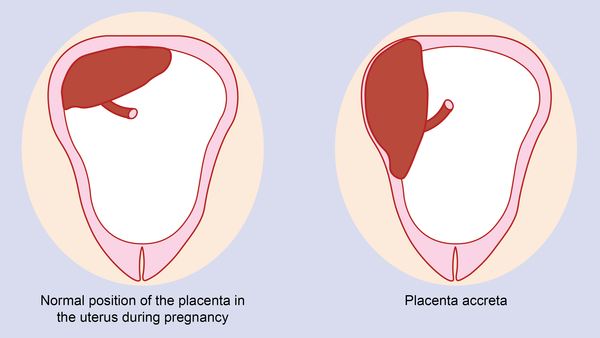 No complaints were made on admission. From the anamnesis it is known that placenta previa was first diagnosed at 17 weeks. Pregnancy was complicated by the threat of termination in the third trimester, for which tocolytic therapy was carried out in a hospital. nine0003
No complaints were made on admission. From the anamnesis it is known that placenta previa was first diagnosed at 17 weeks. Pregnancy was complicated by the threat of termination in the third trimester, for which tocolytic therapy was carried out in a hospital. nine0003
one pregnancy, third birth. The first birth ended with a caesarean section due to the weakness of labor, the second - operational, given the inconsistent scar on the uterus.  The placenta was located on the anterior wall, blocking the internal os. Attention was drawn to the absence of the myometrium of the anterior wall of the uterus in the region of the lower segment for 18–20 cm, as well as the pronounced vascularization of the placental tissue.
The placenta was located on the anterior wall, blocking the internal os. Attention was drawn to the absence of the myometrium of the anterior wall of the uterus in the region of the lower segment for 18–20 cm, as well as the pronounced vascularization of the placental tissue. 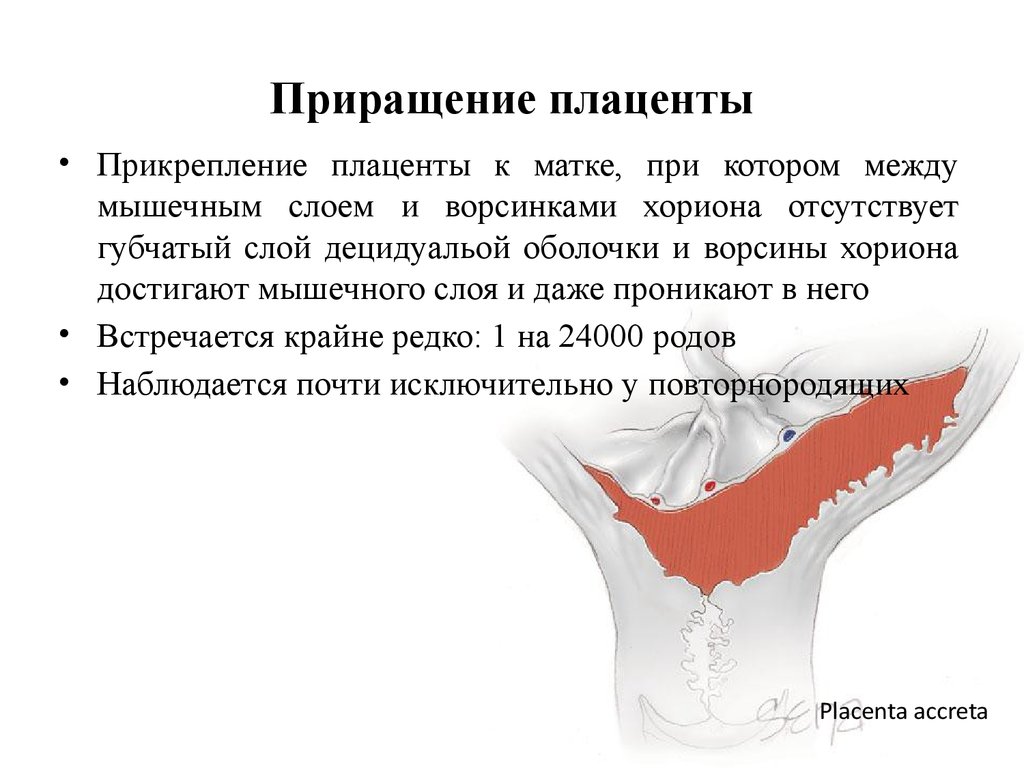 nine0003
nine0003
area could not be excluded.
 In the future, either a delayed hysterectomy is performed, or the dynamics of placental involution is monitored in a qualified institution. According to indications, the placenta can be removed later. nine0003
In the future, either a delayed hysterectomy is performed, or the dynamics of placental involution is monitored in a qualified institution. According to indications, the placenta can be removed later. nine0003
2. Angstmann T., Gard G., Harrington T. et al. Surgical management of placenta accreta: a cohort series and suggested approach // Am. J. Obstet. Gynecol. - 2010. - Vol. 202. – P. 38–39.
3. Arulkumaran S., Ng C.S., Ingemarsson I. et al. Medical treatment of placenta accreta with methotrexate // Acta Obstet. Gynecol Scand. - nineteen86.-Vol. 65, No. 3. – P. 285–286.
4. Chan B.C.P., Lam H. S.W., Yuen J.H.F. et al. Conservative management of placenta previa with accreta // Hong Kong Med. J. - 2008. - Vol. 14 - P. 479-484.
5. Clement D., Kayem G., Cabrol D. Conservative treatment of placenta percreta: a safe alternative // Eur.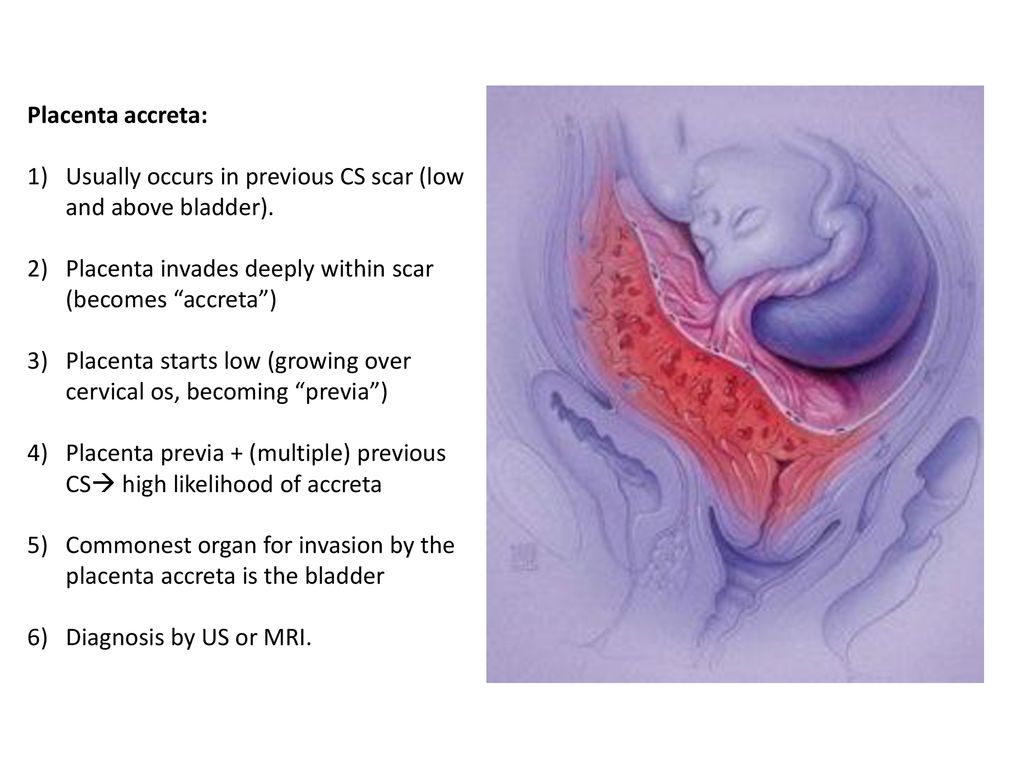 J. Obstet. Gynecol. reproduction. Biol. - 2004. - Vol. 114. – P. 108–109.
J. Obstet. Gynecol. reproduction. Biol. - 2004. - Vol. 114. – P. 108–109.
6. Flood K.M., Said S., Geary M. et al. Changing trends in peripartum hysterectomy over the last 4 decades // Am. J. Obstet. Gynecol. – 2009. – Vol. 200.-P. 632.el-632.e6.
7. Henrich W., Surbek D., Kainer F. et al. Diagnosis and treatment of peripartum bleeding // J. Perinat. Med. - 2008. - Vol. 36, No. 6. - P. 467-478.
8. Kayem G., Davy C., Goffinet F. et al. Conservative versus extirpative management in cases of placenta accreta // Obstet. and Gynecol. - 2004. - Vol. 104. – P. 531–536.
9. Kent A. Management of placenta accreta // Rev. obstet. Gynecol. - 2009. - Vol. 2, No. 2. – P. 127–128.
10. Kotsuji F., Nishijima K., Kurokawa T. et al. Usefulness of the transverse uterine fundal incision for placenta previa // Abstracts of the XXII European congress of perinatal medicine. - Granada, 2010. - P. 618.
11. Lam H., Pun T.C., Lam P.W. Successful conservative management of placenta previa accreta during caesarean section // Int.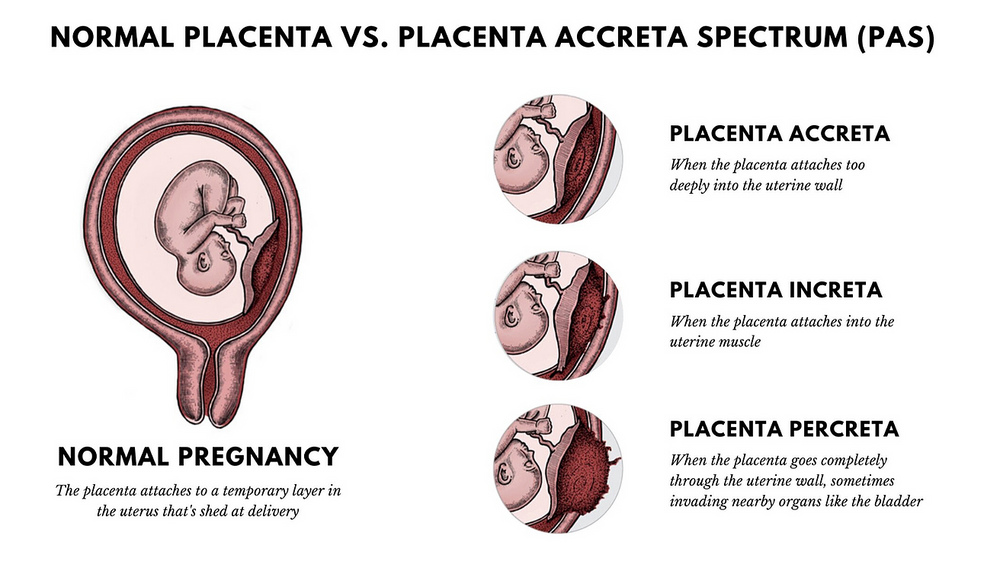 J. Gynecol. obstet. - 2004. - Vol. 86. – P. 31–32.
J. Gynecol. obstet. - 2004. - Vol. 86. – P. 31–32.
12. Mussalli G.M., Shah J., Berck D.J. et al. Placenta accreta and methotrexate therapy: three case reports // J. Perinatol. - 2000. - Vol. 20. – P. 331–334.
13. Ophir E., Singer-Jordan J., Odeh M. et al. Abnormal placental invasion – a novel approach to treatment case report and review // Obstet. Gynecol. Surv. – 2009. – Vol. 64, No. 12. - P. 811-822.
14. Palacios Jaraquemada J.M., Pesaresi M., Nassif J.C. et al. Anterior placenta percreta: surgical approach, hemostasis and uterine repair // Acta Obstet. Gynecol. Scand. - 2004. - Vol. 83. – P. 738–744.
15. Palacios Jaraquemada J.M., Bruno C.H. MRI in 300 cases of placenta accereta: surgical correlation of new findings // Acta Obstet. Gynecol. Scand. - 2005. - Vol. 84. – P. 719–727.
16. Son G., Kwon J., Cho H. et al. A case of placenta increta presenting as delayed postabortal intraperitoneal bleeding in the first trimester // J. Korean Med. sci. - 2007. - Vol. 22. – P. 932–935.
22. – P. 932–935.
17. Sumigama S., Itakura A., Ota T. et al. Placenta previa increta/percreta in Japan: a retrospective study of ultrasound findings, management and clinical course // J. Obstet. Gynecol. Res. - 2007. - Vol. 33, No. 5. - P. 606-611.
18. Thia E.W.H., Tan L.-K., Devendra K. et al. Lessons learned from two women with morbiditly adherent placentas and a review of literature // Ann. Acad. Med. Singapore. - 2007. - Vol. 36. – P. 298–303.
19. Timmermans S., van Hof A.C., Duvekot J.J. Conservative management of abnormally invasive placement // Obstet. Gynecol. Surv. - 2007. - Vol. 62, No. 8. - P. 529–539.
20. Tong S.Y.P., Tay K.H., Kwek Y.C.K. Conservative management of placenta accreta: review of three cases // Singapore Med. J. - 2008. - Vol. 49, No. 6. - P. e156-e159.
21. Vazquez J.A., Rivera G.V., Higareda S.H. et al. Obstetric hysterectomy. Incidence, indications and complications // Ginecol. obstet. Mex. - 2008. - Vol.76, No. 3. - P. 156–160.