Private scans in pregnancy
Ultrasound scans during pregnancy - benefits, about
Ultrasound scans during pregnancy - benefits, about | Pregnancy Birth and Baby beginning of content8-minute read
Listen
What is an ultrasound scan?
An ultrasound is a procedure that uses soundwaves to create images of your baby while it’s in the uterus (womb). During the scan, gel is placed on your abdomen (tummy) and a probe called a transducer is placed against your skin. Pulses of sound waves are then sent from the probe to your baby, creating echoes that are turned into images by computer. You can see these images on a monitor.
In some situations, your doctor might recommend a transvaginal ultrasound to get better pictures of your baby. This will only be done with your consent. In this case, you will be covered with a sheet while the probe is inserted into your vagina. The probe would be moved around in the vagina to take pictures of your baby. It may be a little uncomfortable, but it shouldn’t hurt
Why have an ultrasound scan?
Ultrasound offers a safe, accessible test that can provide you and your healthcare team with more information about your pregnancy and unborn baby to help inform and guide your ongoing care.
Depending on how many weeks pregnant you are and the type of ultrasound you are having, it can:
- confirm your pregnancy is viable (meaning everything appears to be progressing well and your baby's heart is beating)
- check for multiple pregnancies (for example, twins) or triplets)
- confirm your baby’s age and estimate your due date
- check your baby’s organs and other structures are developing normally
- confirm your baby’s position in your uterus
- check the length of your cervix
- check the location of your placenta
- check your baby's wellbeing
- check your baby's growth and size
Checkups, scans and tests
Find out what checkups, scans and tests you might have during your pregnancy.
What routine scans might be offered during pregnancy?
Several types of scan are routinely recommended and offered during pregnancy. Although, the option to go ahead and have an ultrasound is yours.
Dating scan
The dating scan is usually done in the first trimester, although can be done anytime between 6 and 14 weeks of pregnancy. This ultrasound can confirm your pregnancy is viable and estimate your baby’s due date. It can also confirm how many babies you are carrying and check that your baby is growing in your uterus, and is not ectopic (growing outside the uterus).
Nuchal translucency scan
The nuchal translucency scan (also called a ‘12 week scan’) is usually done at 12 weeks of pregnancy, although it can be done anytime between 11 weeks and 13 weeks, 6 days of pregnancy. The term ‘nuchal translucency’ is referring to one of the key measurements taken during this ultrasound. This measurement provides some information to assess your babies risk of being affected by a chromosomal abnormality. If you choose to have additional prenatal screening, results of this ultrasound may also be combined with a blood test to further calculate the risk that your baby may have a chromosomal abnormality, such as Down syndrome.
If you choose to have additional prenatal screening, results of this ultrasound may also be combined with a blood test to further calculate the risk that your baby may have a chromosomal abnormality, such as Down syndrome.
Similar to a dating ultrasound, this scan can also check your babies growth, estimate due date and check the physical and structural development of you baby.
Morphology scan
A morphology scan (also known as a ‘fetal anomaly scan’) is an ultrasound usually done between 18 and 22 weeks of pregnancy. It checks your baby’s body organs, specifically looking at their structure and growth, their gestational age and size will also be estimated based on these measurements. This scan also checks your baby’s heart rate and rhythm, and makes sure your placenta is not lying near or over the cervix and that the cervix is long and closed. Depending on your baby’s position, this scan may also reveal your baby’s sex, this detail will only be shared if requested.
Why else might I need an ultrasound during pregnancy?
In some cases, if you are experiencing pregnancy complications or are worried about your baby's movements, your doctor or midwife might recommend additional ultrasound assessments on top of those routinely offered, to ensure safe care of both you and your baby.
Can an ultrasound scan hurt my baby?
Ultrasound is a safe and pain-free test, and there is no increased risk of miscarriage or harm to your baby. The sound waves used are at very low frequency and so will not hurt you or your baby and your baby will not be able to hear them.
Do I need to have ultrasound scans?
Your doctor or midwife is likely to recommend you have one or more ultrasound scans during your pregnancy so they can check how your baby is developing, but you’re still free to choose whether or not you have the scan.
Talk to your doctor or midwife about tests and scans to understand why they might be offered to you.
Questions you might want to ask your doctor
Here are some questions you might want to ask your midwife or doctor:
- Why are you recommending this ultrasound?
- What are the benefits of having this ultrasound?
- Are there risks if I choose not to have the ultrasound?
- What does the ultrasound involve?
- When will I get the results?
More questions to ask your doctor about tests and scans.
Who performs an ultrasound scan?
Some medical specialists, such as obstetrician, have had specialised training and are certified to carry out ultrasound scans. In other cases, your doctor may refer you to an imaging clinic where a trained ultrasound operator known as a sonographer will check your baby. Some midwives are also trained to perform certain ultrasounds.
You might have your ultrasound in a community clinic, an imaging centre or in a hospital.
Ask your health team if you can have printed copies of your baby’s ultrasound images to take home.
How do I prepare for an ultrasound scan?
Your doctor, midwife or the ultrasound clinic you’ve been referred to, will tell you how to best prepare for your scan. In many cases you won’t need to do anything prior to or after having an ultrasound. But for certain ultrasounds sometimes having a full bladder may be helpful. Its always best to check with your healthcare team what they prefer when you book your appointment.
How much does an ultrasound cost?
Medicare will cover part of the cost of your ultrasound scans. Ask your doctor if you should expect any out-of-pocket costs for your specific situation.
When will I get the results of my ultrasound scan?
The results from the scan are generally available on the same day. A copy of the report will be sent to your referring doctor. If there are any abnormalities or reason for concern, a specialist doctor will contact you to discuss the findings, what this may mean and next steps.
More information
One of the aims of having ultrasound scans in pregnancy is to offer a safe, accessible test that can provide you with more information about your pregnancy and unborn baby.
While these scans can reassure you that your baby is developing normally, you may also learn that your baby has an abnormality. For this reason, before you have the test it’s a good idea to think about why you are choosing to do it, and how you will feel once you get the results. Consider also who you might want to discuss any important decisions with. Your partner, a friend or family member, or a health professional such as your GP or midwife are all good options.
Consider also who you might want to discuss any important decisions with. Your partner, a friend or family member, or a health professional such as your GP or midwife are all good options.
If the results of your ultrasound bring up any concerns about genetic conditions, you can talk to your doctor or midwife about other diagnostic tests, such as chorionic villus sampling or amniocentesis, for these conditions.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
RANZCOG (Antenatal care during pregnancy), Queensland Government (Consent information – patient copy, obstetric ultrasound), Mater Mother’s Hospital (Ultrasound scan – your 18-to-20-week scan), Mater Imaging (Obstetric Ultrasound), RANZCOG (Prenatal assessment of fetal structural conditions), NPS MedicineWise (Ultrasound during pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Checkups, scans and tests during pregnancy
- Antenatal care during your pregnancy
- Routine antenatal tests
- Questions to ask your doctor about tests and scans
Need more information?
Molar pregnancy - Better Health Channel
Most molar pregnancies are diagnosed when bleeding early in pregnancy prompts an ultrasound scan.
Read more on Better Health Channel website
Pregnancy: blood tests, ultrasound & more | Raising Children Network
In pregnancy, you’ll be offered blood tests, ultrasound scans, urine tests and the GBS test. Pregnancy tests identify health concerns for you and your baby.
Read more on raisingchildren.net.au website
Routine antenatal tests
During pregnancy, you'll be offered a range of tests, including blood tests and ultrasound scans. Each test can tell you something about you and your baby’s health.
Read more on Pregnancy, Birth & Baby website
Nuchal translucency scan
A nuchal translucency scan is an ultrasound scan that helps in estimating your risk of having a baby with chromosomal abnormality.
Read more on Pregnancy, Birth & Baby website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
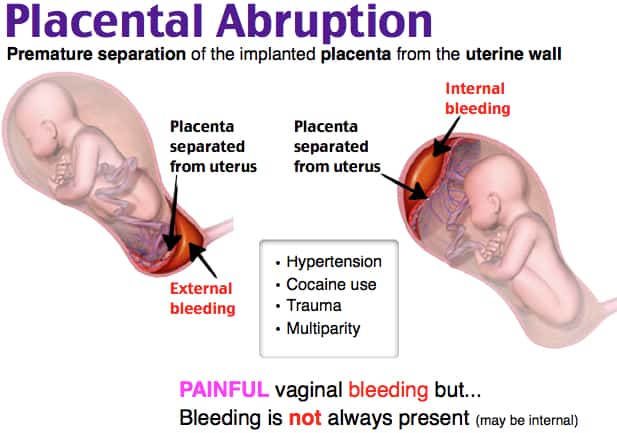
Bleeding during pregnancy
Bleeding during pregnancy is relatively common, however you should always contact your midwife or doctor immediately if it happens to you.
Read more on Pregnancy, Birth & Baby website
Beta HCG Test | HealthEngine Blog
A Beta HCG (BHCG or Blood Pregnancy Test) May Be Performed by Your Doctor If They Suspect That You May Be Pregnant, or if You Suspect Pregnancy Yourself!
Read more on HealthEngine website
Pregnant with twins? About twin pregnancy | Raising Children Network
Pregnant with twins? Twin pregnancy can have more complications, so you’ll need more check-ups. Here’s what to expect in your pregnancy and antenatal care.
Read more on raisingchildren.net.au website
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
Molar pregnancy
A molar pregnancy is a type of pregnancy where a baby does not develop. A molar pregnancy can be either complete or partial.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Ultrasound scans in pregnancy - NHS
Ultrasound scans use sound waves to build a picture of the baby in the womb. The scans are painless, have no known side effects on mothers or babies, and can be carried out at any stage of pregnancy. Talk to your midwife, GP or obstetrician about any concerns you have.
Having a scan in pregnancy is usually a happy event, but be aware that ultrasound scans may detect some serious health conditions, so try to be prepared for that information.
See What if a screening test finds something for more information on if a scan or other screening test suggests your baby may be more likely to have a condition.
What will happen at the scan?
Most scans are carried out by sonographers. The scan is carried out in a dimly lit room so the sonographer is able to get good images of your baby.
You'll be asked to lie on your back and reveal your tummy.
The sonographer will put ultrasound gel on your tummy, which makes sure there is good contact between the machine and your skin.
The sonographer passes a probe over your tummy and a picture of the baby will appear on the ultrasound screen.
During the exam, sonographers need to keep the screen in a position that gives them a good view of the baby.
The sonographer will carefully examine your baby's body. The sonographer may need to apply slight pressure on your tummy to get the best views of the baby.
How long will a scan take?
A scan usually takes around 20 to 30 minutes. However, the sonographer may not be able to get good views if your baby is lying in an awkward position or moving around a lot.
If it's difficult to get a good image, the scan may take longer or have to be repeated at another time.
Can an ultrasound scan harm me or my baby?
There are no known risks to the baby or the mother from having an ultrasound scan, but it's important that you consider carefully whether to have the scan or not.
This is because the scan can provide information that may mean you have to make further important decisions. For example, you may be offered further tests, such as amniocentesis, that have a risk of miscarriage.
When are scans offered?
Hospitals in England offer at least 2 ultrasound scans during pregnancy:
- at 10 to 14 weeks
- and between 18 and 21 weeks
The first scan is sometimes called the dating scan. The sonographer estimates when your baby is due (the estimated date of delivery, or EDD) based on the baby's measurements.
The dating scan can include a nuchal translucency (NT) scan, which is part of the combined screening test for Down's syndrome, if you choose to have this screening.
The second scan offered during pregnancy usually takes place between 18 and 21 weeks of pregnancy. It's sometimes called the mid-pregnancy scan. This scan checks for 11 physical conditions in your baby.
You may be offered more than 2 scans, depending on your health and the pregnancy. You can find out more about the 12-week dating scan and the 20-week or mid-pregnancy scan.
When will I get the results?
The sonographer will be able to tell you the results of the scan at the time.
Do I have to have ultrasound scans?
No, not if you do not want to. Some people want to find out if their baby is more likely to have a condition, while others do not. The 12-week dating scan and 20-week scan will be offered to you, but you do not have to have them.
Your choice will be respected if you decide not to have the scans, and your antenatal care will continue as normal. You'll be given the chance to discuss it with your maternity team before making your decision.
What can an ultrasound scan be used for?
An ultrasound scan can be used to:
- check your baby's size – at the 12-week dating scan, this gives a better idea of how many weeks pregnant you are; your due date, which is originally calculated from the first day of your last period, may be adjusted according to the ultrasound measurements
- check whether you're having more than 1 baby
- detect some physical conditions
- show the position of your baby and the placenta – for example, when the placenta is low down in late pregnancy, a caesarean section may be advised
- check that the baby is growing normally – this is particularly important if you're carrying twins, or you've had problems in this pregnancy or a previous pregnancy
Can I bring family or friends with me when I have the scan?
Yes. You may like someone to come with you to the scan appointment.
Most hospitals do not allow children to attend scans as childcare is not usually available. Please ask your hospital about this before your appointment.
Remember, an ultrasound scan is an important medical examination and it is treated in the same way as any other hospital investigation. Ultrasound scans can sometimes find problems with the baby.
If everything appears normal, what happens next?
Most scans show that the baby is developing normally and no problems are found. This is because most babies are healthy. You can continue with your routine antenatal care.
If the scan shows your baby is more likely to have a condition, what happens next?
If the scan shows your baby is more likely to have a condition, the sonographer may ask for a second opinion from another member of staff. You might be offered another test to find out for certain if your baby has the condition.
If you're offered further tests, you will be given more information about them so you can decide whether or not you want to have them. You'll be able to discuss this with your midwife or consultant.
If necessary, you will be referred to a specialist, possibly in another hospital.
Can I find out the sex of my baby?
Finding out the sex of your baby is not offered as part of the national screening programme.
If you want to find out the sex of your baby, you can usually do so during the 20-week mid-pregnancy scan but this depends on the policy of your hospital. Tell the sonographer at the start of the scan that you'd like to know your baby's sex.
Be aware, though, that it's not possible for the sonographer to be 100% certain about your baby's sex. For example, if your baby is lying in an awkward position, it may be difficult or impossible to tell.
Some hospitals have a policy of not telling patients the sex of their baby. Speak to your sonographer or midwife to find out more.
Can I have a picture of my baby?
You will need to check if your hospital provides this service. If they do, there may be a charge.
Video: What happens at a scan and what will they tell me?
In this video, a midwife explains what happens at your ultrasound scans during pregnancy.
Media last reviewed: 5 April 2020
Media review due: 5 April 2023
Prenatal screening of the 1st and 2nd trimesters of pregnancy ("double", "triple" and "quadruple" tests). First screening.
Prenatal screening are tests performed on pregnant women to identify risk groups for pregnancy complications.
The word screening means "sifting". In medicine, screening is understood as the conduct of simple and safe studies of large groups of the population in order to identify risk groups for the development of a particular pathology. nine0005
Prenatal screening are tests performed on pregnant women to identify risk groups for pregnancy complications. A special case of prenatal screening is a study to identify risk groups for the development of congenital malformations in the fetus. They are carried out at certain times of pregnancy.
Neither the first nor the second screening makes it possible to identify all women who may have this or that problem, but it makes it possible to identify a relatively small group of patients, within which most of the people with this type of pathology will be concentrated. Finding an increased risk of malformations in the fetus through screening methods is not a diagnosis. The diagnosis can be made or rejected with additional tests. nine0005
To calculate prenatal screening, patients are required to fill out a special questionnaire, which is necessary to take into account all factors (patient weight, singleton or multiple pregnancy, medication, IVF, etc.)
Prenatal screening at the CIR Laboratory
Combined screening is carried out in the CIR laboratory - a combination of biochemical and ultrasound screenings. To calculate the risks, special software is used, which is certified for use with the purpose of prenatal screening. For the calculation, patients are required to fill out a special questionnaire, which is necessary to take into account all factors (patient weight, singleton or multiple pregnancy, medication, IVF, etc.). nine0005
It is also possible to calculate risks taking into account external ultrasound data with the name of the institution and the name of the doctor who performed the procedure. However, if there is no ultrasound data, biochemical screening will be performed using software.
Complete combined screening of the 1st and 2nd trimesters of pregnancy:
Prenatal Screening Program
- First trimester ultrasound 11 weeks to 13 weeks 6 days
- Extended prenatal screening of the first trimester with calculation of the risk of preeclampsia (preeclampsia)
- Prenatal screening II trimester - quadruple test (16-18 weeks) (total hCG, AFP, free estriol, inhibin A)
Program "Prenatal screening by an ultrasound doctor, Ph.D. Te S.A."
- Expert ultrasound of the 1st trimester from 11 to 13 weeks 6 days (2D-3D-4D) by an ultrasound doctor, Ph.D. Cho S.A.
- Prenatal screening of the first trimester extended with the calculation of the risk of preeclampsia (preeclampsia)
- Prenatal screening II trimester - quadruple test (16-18 weeks) (total hCG, AFP, free estriol, inhibin A)
1st trimester screening options (at 11 weeks - 13 weeks 6 days):
Prenatal screening of the first trimester (free hCG, PAPP-A)
Prenatal screening of the first trimester extended with the calculation of the risk of preeclampsia
Second trimester screening options (14 weeks - 20 weeks 6 days, recommended 16-18 weeks):
Prenatal screening II trimester - triple test (hCG, AFP, free estriol)
Prenatal screening II trimester - quadruple test (hCG, AFP, St. estriol, inhibin A)
Prenatal screening II trimester - triple test with f.hCG (f.hCG, AFP, f.estriol)
Prenatal screening II trimester - double test (hCG, AFP)
AFP with calculation of MoM by gestational age
Prenatal screening II trimester - double test with f.hCG (f.hCG, AFP) nine0005
Calculation of prenatal screening with free hCG β-subunit in the second trimester
Test conditions
- We calculate the gestational age, it is better after consulting a doctor. Prenatal screenings are performed at certain stages of pregnancy.
- We do an ultrasound (it is recommended to have at least an ultrasound performed at a period of 11-13 weeks)
- Carry out blood sampling (not earlier than 3-4 hours after the last meal (do not eat fatty)). We fill out a special form. nine0039
Screening transcript. What is MoM?
The content of hormonal indicators in the blood can vary in different populations and ethnic groups of the population and depends on the method of determination. That is why individual levels of markers in pregnant women should be assessed using the indicator MoM (Multiple of Median) - a coefficient showing the degree of deviation of the indicator value from the average value for the gestational age (median). To calculate the MoM, the concentration of the hormonal indicator, ultrasound data, the patient's history, including height, weight, smoking, pregnancy as a result of IVF, etc. are taken into account. If the MoM value in the patient is close to one, then the value of the indicator is close to the average in the population; - above the average in the population, if below one - below the average in the population. nine0005
Neither the first nor the second screening makes it possible to identify all women who may have this or that problem, but it makes it possible to identify a relatively small group of patients, within which most of the people with this type of pathology will be concentrated. Finding an increased risk of malformations in the fetus through screening methods is not a diagnosis. The diagnosis can be made or rejected with additional tests.
See also:
Non-invasive prenatal aneuploidy test NIPT (from 10 weeks to completion of pregnancy)
Panorama non-invasive prenatal test + NIPT microdeletions (expanded panel)
Non-invasive prenatal test VERACITY (from 10 weeks)
Read the articles and answers from clinic specialists CIR:
- The riddle of the quadruple test
- Which is better - double, triple or quintuple?
- PAPP-A reduction in screening
- What is the difference between triple and quadruple?
- Ultrasound, screening, norms, MoM, triple and quadruple tests
- the need for biochemical screening II trimester
- ARI and first trimester screening (double test)
- high hCG in screening
-
ToRCH infections and pregnancy
What are ToRCH infections, what are the dangers of these infections during pregnancy, how and when is the examination performed, how to interpret the results.
Perinatal infections account for approximately 2-3% of all congenital fetal anomalies.
-
Pregnancy Tests in the CIR Laboratories
In our laboratory you can undergo a complete examination at the onset of pregnancy, take tests at any time, and in our clinics you can conclude an agreement on pregnancy management. nine0005
-
Pregnancy hCG calculator online
The hCG calculator is used to calculate the increase in hCG (the difference between two tests taken at different times).
The increase in hCG is important for assessing the development of pregnancy. Normally, in the early stages of pregnancy, hCG increases by about 2 times every two days. As the hormone levels increase, the rate of increase decreases.
-
False positive pregnancy test or why hCG is positive but not pregnant? nine0005
When can a pregnancy test be positive?
-
The norm of a complete blood count during pregnancy. Hemoglobin, platelets, hematocrit, erythrocytes and leukocytes during pregnancy.
Clinical blood test during pregnancy. Hematological changes during pregnancy.
A normal pregnancy is characterized by significant changes in almost all organs and systems to adapt to the requirements of the fetoplacental complex, including changes in blood tests during pregnancy. nine0005
-
The norm of hCG during pregnancy. Table of hCG values by week. Elevated HCG. Low HCG. HCG in ectopic pregnancy. hCG during IVF (hCG after replanting, hCG at 14 dpo).
hCG or beta-hCG or total hCG - human chorionic gonadotropin - a hormone produced during pregnancy. HCG is formed by the placenta, which nourishes the fetus after fertilization and implantation (attachment to the wall of the uterus).
-
Assessing the risk of pregnancy complications through prenatal screening
Prenatal screening data make it possible to assess not only the risks of congenital pathology, but also the risk of other pregnancy complications: intrauterine fetal death, late toxicosis, intrauterine hypoxia, etc.
-
Parvovirus B19 and parvovirus infection: what you need to know when planning and getting pregnant.
What is a parvovirus infection, how is the virus transmitted, who can get sick, what is the danger of the virus during pregnancy, what tests are taken for diagnosis. nine0007
-
Pregnancy planning
Obstetrics differs from other specialties in that during the physiological course of pregnancy and childbirth, in principle, it is not part of medicine (the science of treating diseases), but is part of hygiene (the science of maintaining health). Examination during pregnancy planning.
-
Testosterone during pregnancy. Androgens: their formation and metabolism during normal pregnancy. Hyperandrogenism during pregnancy. "Male" hormones during pregnancy. nine0005
Testosterone and other androgens levels change during pregnancy. The change in these levels depends, among other things, on the sex of the fetus.
All articles of the section
Site map
Site map When visiting the clinic, a mandatory thermometry is carried out.