Does throwing up hurt the baby second trimester
8 Thoughts Every Pregnant Woman Has When She's Puking Her Guts Out
Life
andriano_cz/Fotolia
by Kimmie Fink
Morning sickness is one of the most common ailments pregnant women endure in their first trimester. Many expectant mamas experience nausea by itself (which is awful, don't get me wrong), but those of us who have vomiting know how much worse it can get. It's different than throwing up from the flu or from a night of one-too-many martinis. It sucks in a singular way, and that's why every pregnant woman is thinking the same thing when she's puking her guts out.
According to the American Pregnancy Association (APA), 60-70 percent of pregnant women experience vomiting as a side effect of morning sickness. Count me among them. During my first pregnancy, it got so bad that it landed me in urgent care. I needed IV fluids to address my dehydration. It was definitely worse the first trimester, but I continued to throw up randomly throughout my pregnancy. It's not any better this time around, either. Just the other day, I found my 11 week pregnant self leaning out my car door, revisiting my breakfast in the parking lot of a dentist's office.
I can't think of an instance when throwing up feels good, but at least you usually get some relief. When you're pregnant, you just go back to feeling like hot garbage. If you're in the throes of tossing your pregnant cookies, I feel you, and I have a feeling I know what's going through your mind:
"This Can't Be Good For The Baby"
That all this vomiting will hurt the baby is a pretty common fear. I mean, how can they be getting any nutrients if you aren't? My midwife assured me, however, that baby will take what they need from mom, and she was right. According to BabyMed, vomiting normally does not harm the fetus, and in case this was on your list of worries, retching won't cause miscarriage.
However, if you get to the point where you can't keep anything (liquids or solids) down, or you're losing weight, you may have a condition called hyperemesis gravidarum. In that case, you do want to see a doctor because severe dehydration can hurt your baby.
"How Much Longer?"
I don't care which pregnancy you're on, if you have severe vomiting, you know exactly how many weeks you are. Like, I know I am 11 weeks and one day and I absolutely count that one day because it puts me that much closer to the magical 12 week mark where most women experience relief.
"Oh, God. Please Don't Let Me Pee."
Yep, so this is a thing. Not only can you leak a little when you sneeze or cough, the act of vomiting can also make you urinate. It's called stress-induced incontinence, friends, and let this voice of experience tell you that, without a single doubt, it's the goddamn worst. When I'm hunched over that porcelain bowl, I'm praying to all the gods that my pantyliner holds up.
"Did Everyone Hear That?"
It's one thing to throw up in the privacy of your own home, but public barfing is its own circle of hell. I don't know about you, but I am not a quiet puker. So when I open the bathroom door and do the Starbucks walk of shame, I just know that every patron has been listening (and judging) over their peppermint mochas.
"Gross. Splash Back."
When we were kids, my sister dared me to drink toilet water. She assured me it was sanitary because she'd just flushed and it was "fresh" water. I understand now how evil she was being. You guys, the toilet water is not clean, and this is never more evident than when you blow chunks into it only to have it splash back onto your forehead (although I won't judge you if you are momentarily refreshed).
"I Have Regrets"
Those barbecue-flavored Pringles don't look so good now, do they?
"F*ck You, Vitamin B6 & Ginger"
When you've taken preventive measures, vomiting can feel like a personal affront. I can personally take Zofran and puke 30 minutes later, so I know this to be true. There are any number of vomiting remedies you can try, so it feels extra bad when nothing works. (I'll tell you where you can stick your seasickness bands.)
I can personally take Zofran and puke 30 minutes later, so I know this to be true. There are any number of vomiting remedies you can try, so it feels extra bad when nothing works. (I'll tell you where you can stick your seasickness bands.)
"Never Again"
Holding my hair back as I lost my curry, my husband gently chided, "Just remember this next time you think you want another baby." Annoying, yes, but not wrong. We are actually capping our family at two kids because I'm not willing to do this again. I'll do it once more for this baby, but I can think of a million things I'd rather do than throw up for two straight months.
Check out Romper's new video series, Romper's Doula Diaries:
Watch full episodes of Romper's Doula Diaries on Facebook Watch.
Morning sickness | March of Dimes
Morning sickness is when you have nausea and vomiting during pregnancy. Even though it’s called morning sickness, it can happen any time of day.
Morning sickness usually starts at about 6 weeks of pregnancy and goes away in the second trimester.
Lots of pregnant women have morning sickness. It usually doesn’t cause harm to you or your baby.
Hyperemesis gravidarum is severe nausea and vomiting that needs treatment (sometimes in a hospital) to help you get better.
If your morning sickness is severe or if it goes into your fourth month of pregnancy, tell your health care provider right away.
What is morning sickness?
Morning sickness (also called nausea and vomiting of pregnancy) is nausea (feeling sick to your stomach) and vomiting that happens in the first few months of pregnancy. Even though it's called morning sickness, it can last all day and happen any time of day.
At least 7 in 10 pregnant women have morning sickness in the first trimester (first 3 months) of pregnancy. It usually starts at about 6 weeks of pregnancy and is at its worst at about 9 weeks. Most women feel better in their second trimester, but some have morning sickness throughout pregnancy. If you have morning sickness, tell your health care provider.
Most women feel better in their second trimester, but some have morning sickness throughout pregnancy. If you have morning sickness, tell your health care provider.
Mild morning sickness doesn’t harm you or your baby. But if nausea and vomiting becomes severe (called hyperemesis gravidarum), it can cause serious problems during pregnancy. You may need to stay in the hospital for treatment.
What is hyperemesis gravidarum?
About 3 in 100 women may have hyperemesis gravidarum. This is extreme, excessive nausea and vomiting during pregnancy. It can cause you to lose weight and become dehydrated (not have enough water in your body). It can start early in pregnancy and last the entire pregnancy. If you have hyperemesis gravidarum, you need treatment to help keep you and your baby safe.
You may be at risk for hyperemesis gravidarum if you:
- Are pregnant for the first time.
- Are pregnant with a girl.
- Are pregnant with multiples (twins, triplets or more).
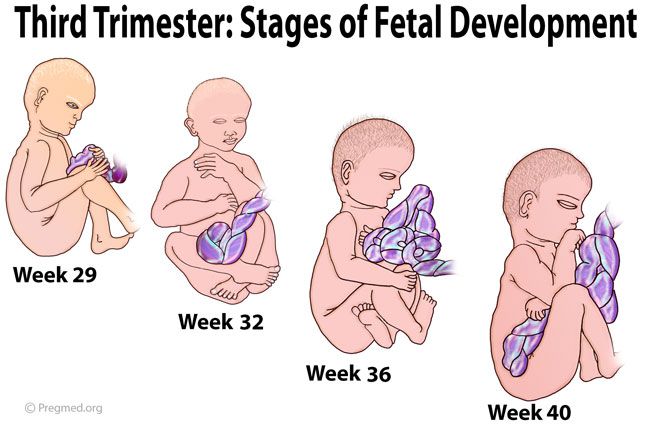
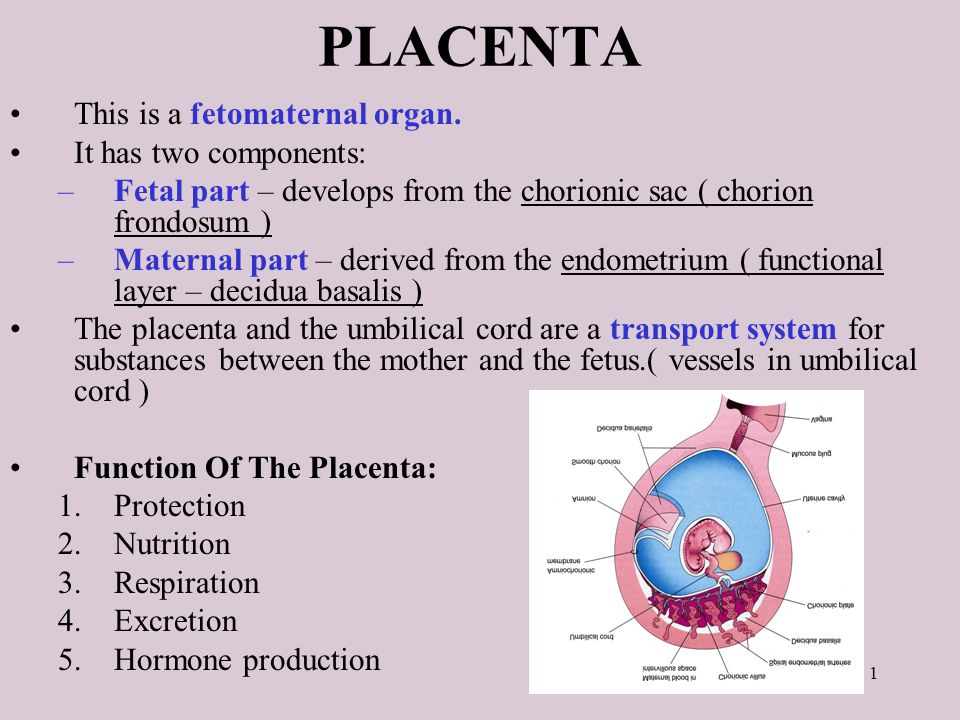
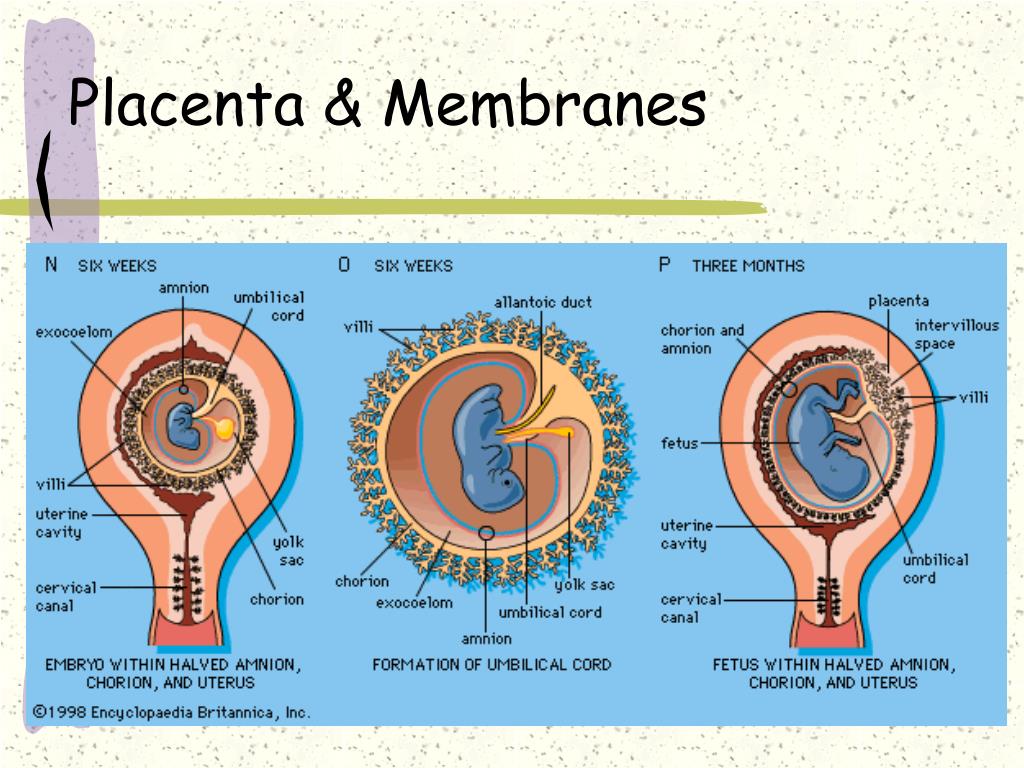
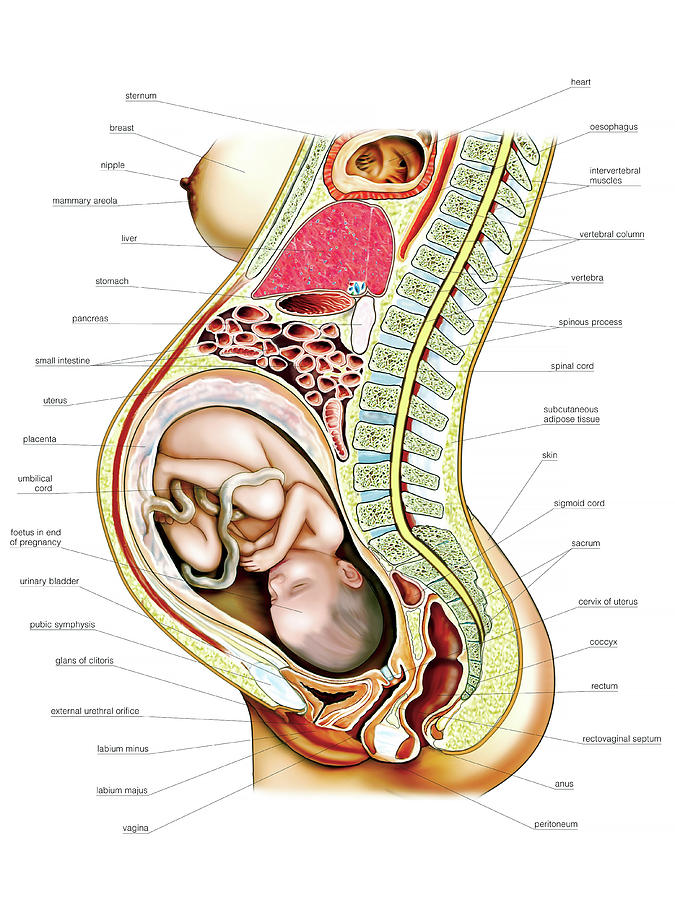
 Being pregnant with more than one baby may increase your risk for severe morning sickness because you may have a large placenta and increased pregnancy hormones. The placenta grows in your uterus (womb) and supplies your babies with food and oxygen through the umbilical cord.
Being pregnant with more than one baby may increase your risk for severe morning sickness because you may have a large placenta and increased pregnancy hormones. The placenta grows in your uterus (womb) and supplies your babies with food and oxygen through the umbilical cord. - Had mild or severe morning sickness in a previous pregnancy, or your mother or sister had severe morning sickness during pregnancy. Take your family health history to help you find out about health conditions that run in your family.
- Have motion sickness or migraines. A migraine is a severe headache that may make you sensitive to bright lights and sound.
- Are overweight.
- Have trophoblastic disease, a condition that leads to abnormal cell growth in the uterus (womb).
Signs and symptoms of hyperemesis gravidarum include:
- Vomiting more than 3 to 4 times a day
- Vomiting that makes you dizzy or lightheaded
- Vomiting that makes you dehydrated.
 Signs and symptoms of dehydration include feeling thirsty, dry mouth, a fast heart beat or making little to no urine.
Signs and symptoms of dehydration include feeling thirsty, dry mouth, a fast heart beat or making little to no urine. - Losing more than 10 pounds in pregnancy
If you have hyperemesis gravidarum, your provider may treat you with medicine to help relieve your nausea and vomiting. You may need treatment in a hospital with intravenous (also called IV) fluids. IV fluids go through a needle into your vein. They help you stay hydrated and can give you nutrients that you usually get from food. If you continue to lose weight, you may need a feeding tube to make sure you’re getting enough nutrients for you and your baby.
What causes morning sickness?
We don’t know for sure what causes morning sickness. It may be caused by low blood sugar or increased pregnancy hormones. Morning sickness may be worse if you’re stressed or overly tired, if you eat certain foods or if you’re traveling (if you often have motion sickness).
Can you prevent or relieve morning sickness?
Yes. Here’s what you can do to help you feel better and even prevent morning sickness:
Here’s what you can do to help you feel better and even prevent morning sickness:
- Take a prenatal vitamin before you get pregnant. Talk to your health care provider about which one to take. Sometimes vitamins can upset your stomach, so take it with a snack.
- Keep snacks by your bed. Eat a few crackers before you get up in the morning to help settle your stomach.
- Eat 5 or 6 small meals each day instead of 3 larger meals.
- Eat foods that are low in fat and easy to digest, like cereal, rice and bananas. Don’t eat spicy or fatty foods.
- Eat healthy snacks between meals. This can help keep your stomach from being empty and helps prevent nausea. Try snacks that are high in protein, like milk or yogurt.
- Drink plenty of fluids, especially water.
- Avoid smells that upset your stomach.
You may have heard about these ways to prevent or relieve morning sickness. Talk to your provider before trying any of these:
- Acupressure and acustimulation (also called electrical nerve stimulation) wristbands.
 These involve putting pressure on or stimulating certain points of the body (called pressure points) to help prevent nausea.
These involve putting pressure on or stimulating certain points of the body (called pressure points) to help prevent nausea. - Acupuncture. This is a kind of treatment in which thin needles are put into your skin. If you’re thinking about acupuncture to help with morning sickness, tell your provider and find an acupuncturist who is trained to work with pregnant women.
- Ginger. Ginger is an herb (plant) used in cooking and medicine. Ginger ale, tea or candies may help relieve morning sickness.
Even if it’s legal where you live for either personal or medical use, it’s not safe to use marijuana to treat morning sickness. No amount of marijuana has been proven safe to use during pregnancy. If you’re thinking of using marijuana to help with morning sickness, talk to your provider about other treatments that are safer for your baby.
Is there medical treatment for morning sickness?
Yes. If you can’t relieve morning sickness on your own or if you have severe nausea and vomiting of pregnancy, your provider may treat you with these medicines:
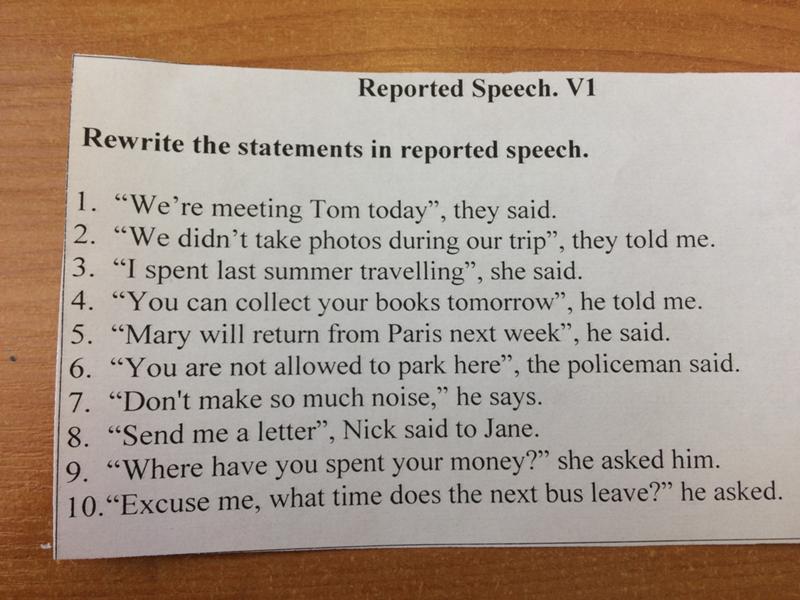
- Vitamin B6 and doxylamine.
 Your provider may treat you with these medicines separately or together. You can get vitamin B6 and doxylamine over-the-counter (OTC), which means you don’t need a prescription for them from your provider. Doxylamine is found in some OTC sleep aids (medicines that help you sleep). Or your provider may prescribe you a medicine that combines them.
Your provider may treat you with these medicines separately or together. You can get vitamin B6 and doxylamine over-the-counter (OTC), which means you don’t need a prescription for them from your provider. Doxylamine is found in some OTC sleep aids (medicines that help you sleep). Or your provider may prescribe you a medicine that combines them. - Antiemetic drugs. These are drugs that help prevent vomiting. If Vitamin B6 and doxylamine don’t work, your provider may prescribe an antiemetic drug for you. Not all are safe to use during pregnancy, so talk to your provider to make sure the medicine is a good choice for you.
Talk to your provider before you take any medicine during pregnancy, even medicine to help treat morning sickness.
When should you call your health care provider about morning sickness?
For most women, morning sickness is mild and goes away over time. But call your provider if:
- Your morning sickness continues into your 4th month of pregnancy.

- You lose more than 2 pounds.
- Your vomit is brown in color or has blood in it. If so, call your provider right away.
- You vomit more than 3 times a day and can’t keep food or fluids down.
- Your heart beats faster than usual.
- You’re tired or confused.
- You’re making much less urine than usual or no urine at all.
Last reviewed: September, 2020
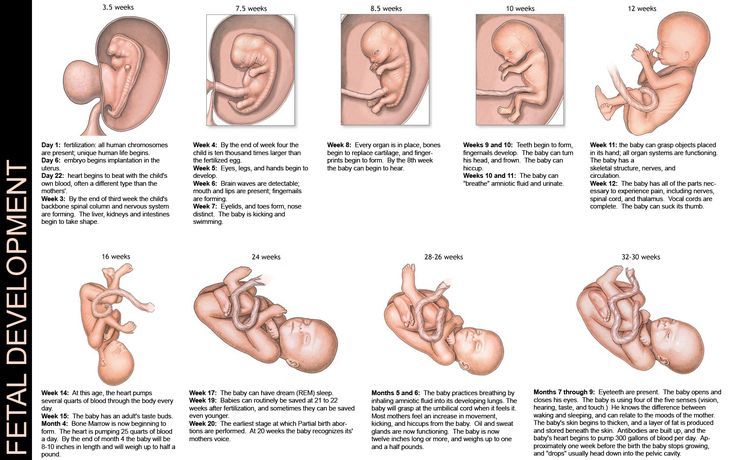
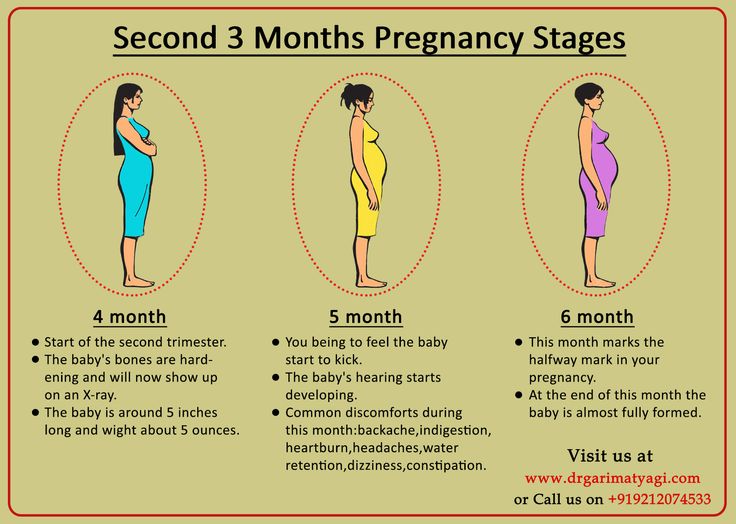
Second trimester of pregnancy (from 13 to 28 weeks)
The beginning of the second trimester is traditionally considered one of the calmest. Walk more. Walking is very helpful. Sit down to rest only when you are tired. Movement in the fresh air improves the supply of oxygen to the fetus, which is very necessary for its normal development.
Nausea disappears, appetite improves. Do not eat a lot of salty, refuse marinades, smoked meats, if you have not done this before. The increased need of the child's body for proteins and vitamins begins. The daily diet should include meat or fish (boiled or stewed), dairy products, especially cottage cheese, eggs. Do not forget about vegetables, fruits, greens. An excellent source of vitamin C is sauerkraut (rather than salted) cabbage. Salads from carrots, cabbage, beets, apples, green radish should be on your table every day. nine0003
Do not forget about vegetables, fruits, greens. An excellent source of vitamin C is sauerkraut (rather than salted) cabbage. Salads from carrots, cabbage, beets, apples, green radish should be on your table every day. nine0003
At 17-20 weeks you will feel your baby's first kicks. From them you can determine how comfortable the baby feels. Intense tremors are a signal of lack of oxygen. Maybe you haven’t walked for a long time or, on the contrary, you are engaged in hard physical labor. Get out into the fresh air or lie down to rest and you will immediately feel how the child has calmed down.
But the lack of movement is an alarm. See a doctor immediately!
The fetal need for calcium sharply increases - intensive growth of the skeleton has begun. If you don't have enough free calcium in your body right now, you could lose your teeth. To prevent this from happening, start taking calcium supplements in consultation with your doctor. nine0003
At this time, toxicosis of the second half of pregnancy may occur, the child suffers greatly from it.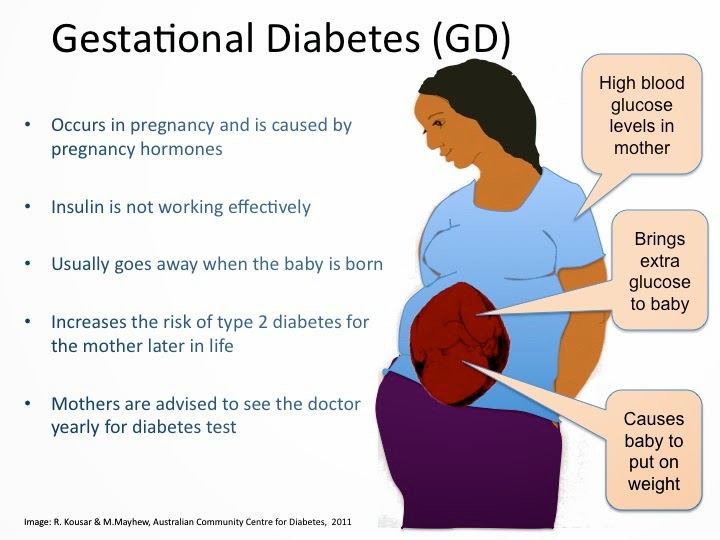 Therefore, if the doctor suggests hospitalization, do not refuse. Toxicosis can, if not be avoided, then at least reduce its manifestations. Be sure to follow your diet. Completely exclude salty, smoked, fried, spicy, canned food, chocolate. Do not eat a lot of grapes and drink fresh milk. Limit flour and rich products. As before, your diet should include boiled meat and fish, oatmeal and buckwheat porridge, vegetables and fruits
Therefore, if the doctor suggests hospitalization, do not refuse. Toxicosis can, if not be avoided, then at least reduce its manifestations. Be sure to follow your diet. Completely exclude salty, smoked, fried, spicy, canned food, chocolate. Do not eat a lot of grapes and drink fresh milk. Limit flour and rich products. As before, your diet should include boiled meat and fish, oatmeal and buckwheat porridge, vegetables and fruits
Periodically, once a week, check for fluid retention in the body. It is allowed to release liquid 200-300 ml less than what was drunk. If little urine is released, this is a signal of latent edema and the onset of toxicosis.
It is very good if you can measure your blood pressure at home. Show the results of measurements at the next visit to the doctor. Both high and too low pressure should alert. With low pressure, blood sluggishly crosses the placenta, and the baby does not receive enough nutrients. nine0003
Do not neglect blood tests - it is important not to miss the development of anemia. In this case, you will be prescribed iron supplements and multivitamins. The diet should include beef liver, tomato juice, buckwheat porridge, apples, preferably Antonovskie (they contain more iron than other varieties).
In this case, you will be prescribed iron supplements and multivitamins. The diet should include beef liver, tomato juice, buckwheat porridge, apples, preferably Antonovskie (they contain more iron than other varieties).
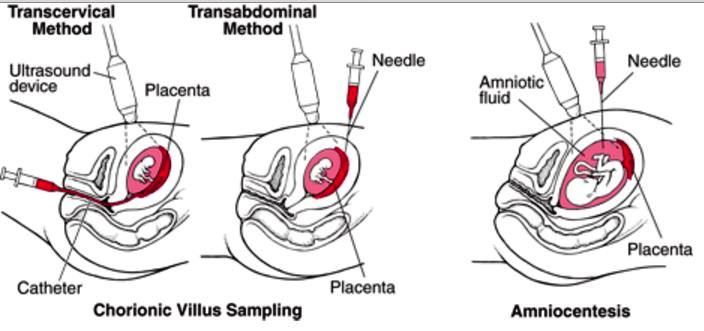
Women who are at risk of giving birth to a child with a genetic pathology (those who have severe hereditary ailments in their families), as well as women over 35 years old (they have an increased likelihood of having a child with Down syndrome) are referred for a consultation by a geneticist. nine0003
In case of a normal pregnancy at 20-22 weeks of pregnancy, a second scheduled ultrasound examination is prescribed.
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects the digestive tract, which trimesters are more likely to cause symptoms of indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn. nine0003
And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn. nine0003
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
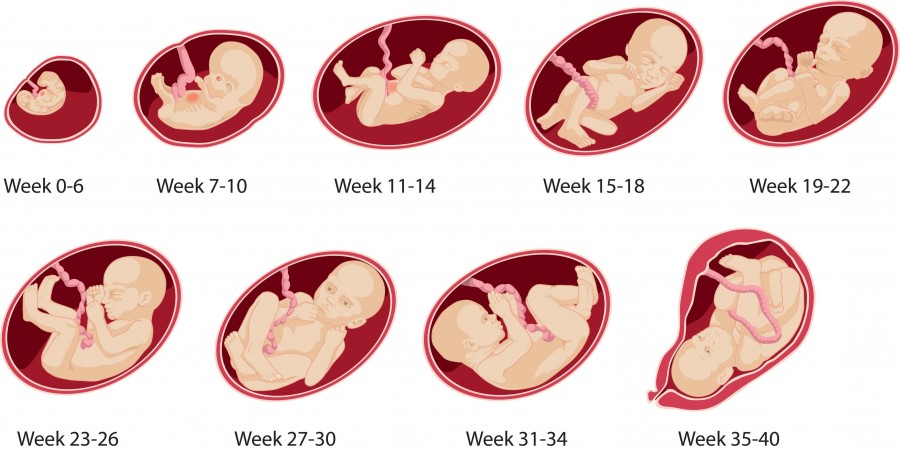
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child. nine0003
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid Reflux | Zapor Acid Office 9000 900 Flatulence Constipation Heartburn Violation of the outflow of bile Hemorrhoids |
The Atlas Genetic Test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet; nine0034
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
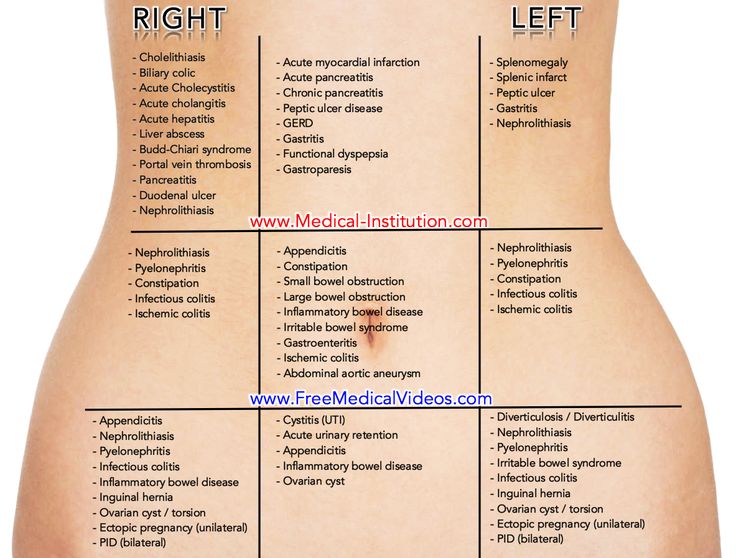
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time. nine0003
nine0003
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
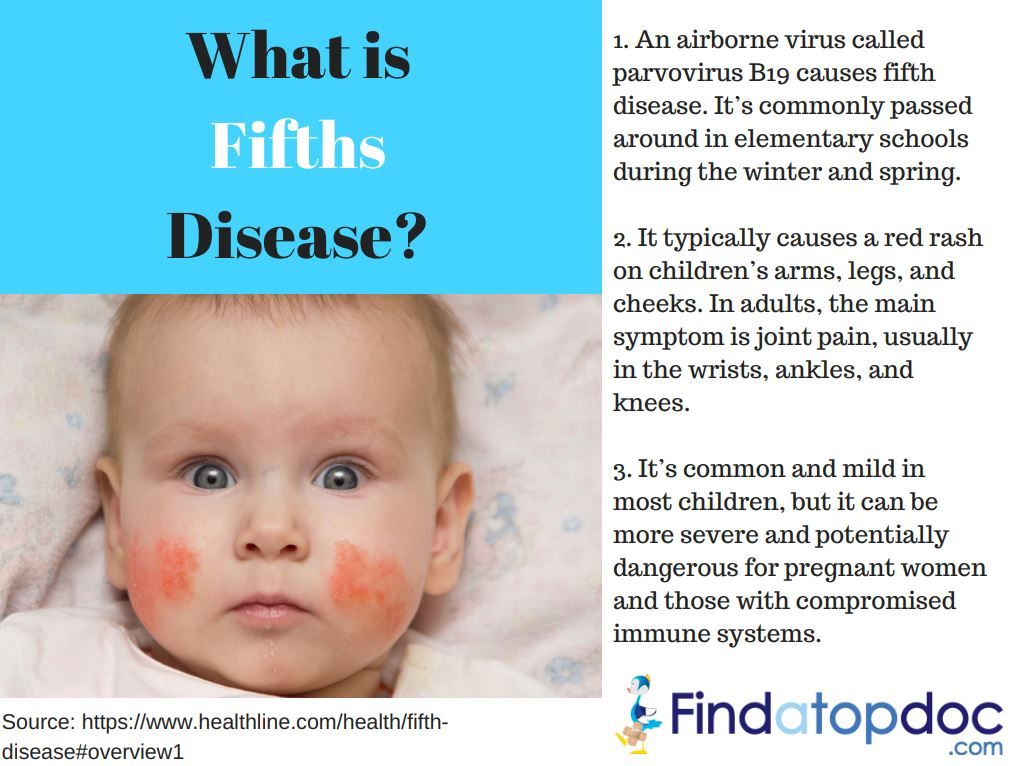
- Multiple pregnancy;
- Toxicosis during a previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy; nine0034
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person more:
- Get plenty of rest - fatigue increases toxicosis; nine0034
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water. nine0034
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include: dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a holiday in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible. nine0150
nine0150
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor. nine0003
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potatoes |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Use the Atlas Microbiota Test to find out your body's ability to break down lactose and gluten. nine0150
nine0150
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas. nine0003
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
Avoid cramps and heartburn during pregnancy is unlikely.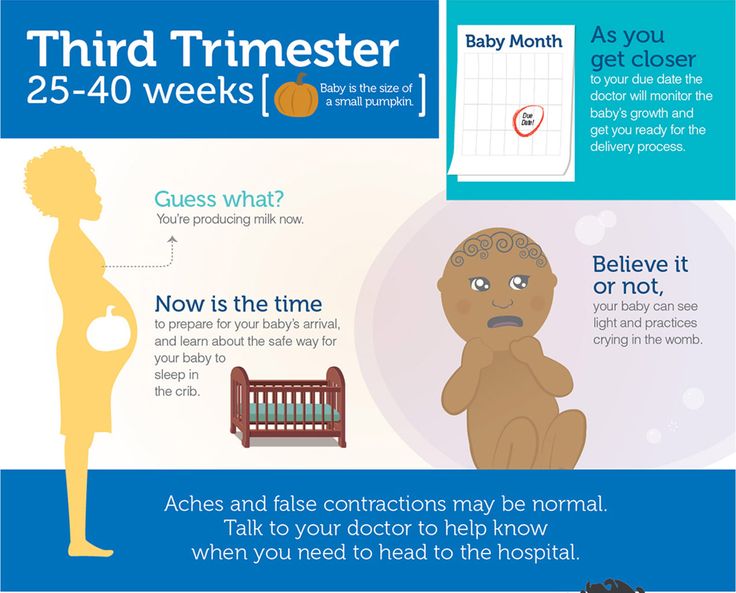 However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less. nine0003
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk. nine0003
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge/ spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone.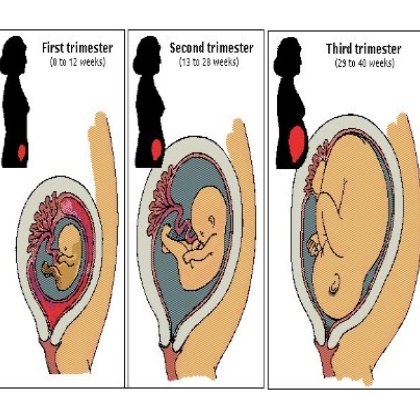 This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases. nine0003
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases. nine0003
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation is accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor. nine0003
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body. nine0003
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for a future pregnancy and reduce the risk of digestive problems. nine0150
nine0150
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities; nine0034
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems in the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012 nine0033 Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.