Statistics of pcos
Polycystic ovary syndrome | Office on Women's Health
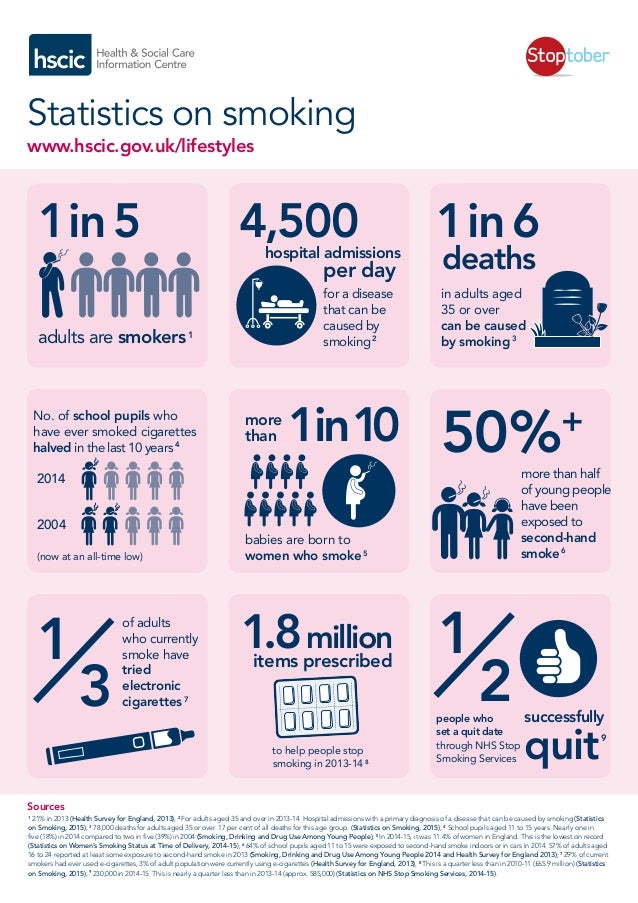
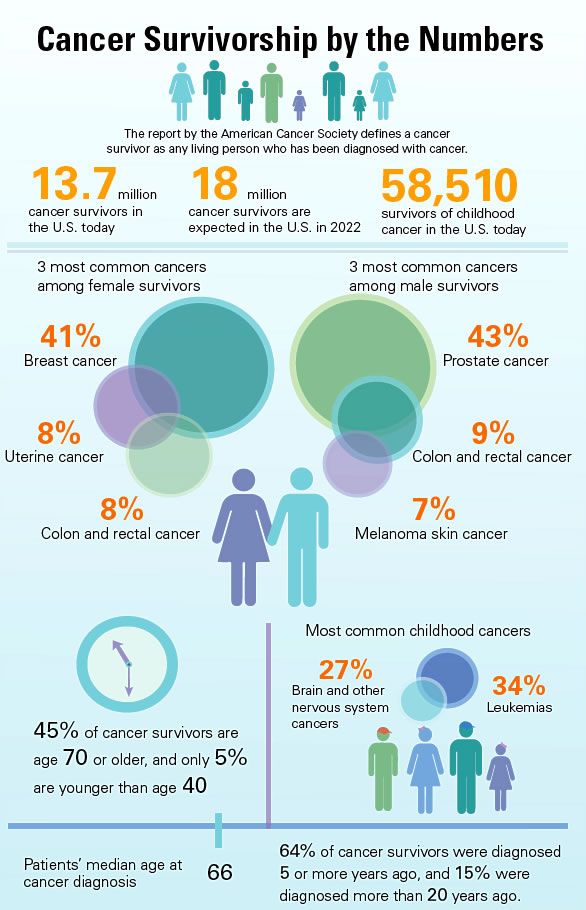
Polycystic ovary syndrome (PCOS) is a health problem that affects 1 in 10 women of childbearing age. Women with PCOS have a hormonal imbalance and metabolism problems that may affect their overall health and appearance. PCOS is also a common and treatable cause of infertility.
What is polycystic ovary syndrome (PCOS)?
Polycystic ovary syndrome (PCOS), also known as polycystic ovarian syndrome, is a common health problem caused by an imbalance of reproductive hormones. The hormonal imbalance creates problems in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be.
PCOS can cause missed or irregular menstrual periods. Irregular periods can lead to:
- Infertility (inability to get pregnant). In fact, PCOS is one of the most common causes of infertility in women.
- Development of cysts (small fluid-filled sacs) in the ovaries
Who gets PCOS?
Between 5% and 10% of women between 15 and 44, or during the years you can have children, have PCOS.1 Most women find out they have PCOS in their 20s and 30s, when they have problems getting pregnant and see their doctor. But PCOS can happen at any age after puberty.2
Women of all races and ethnicities are at risk of PCOS. Your risk of PCOS may be higher if you have obesity or if you have a mother, sister, or aunt with PCOS.
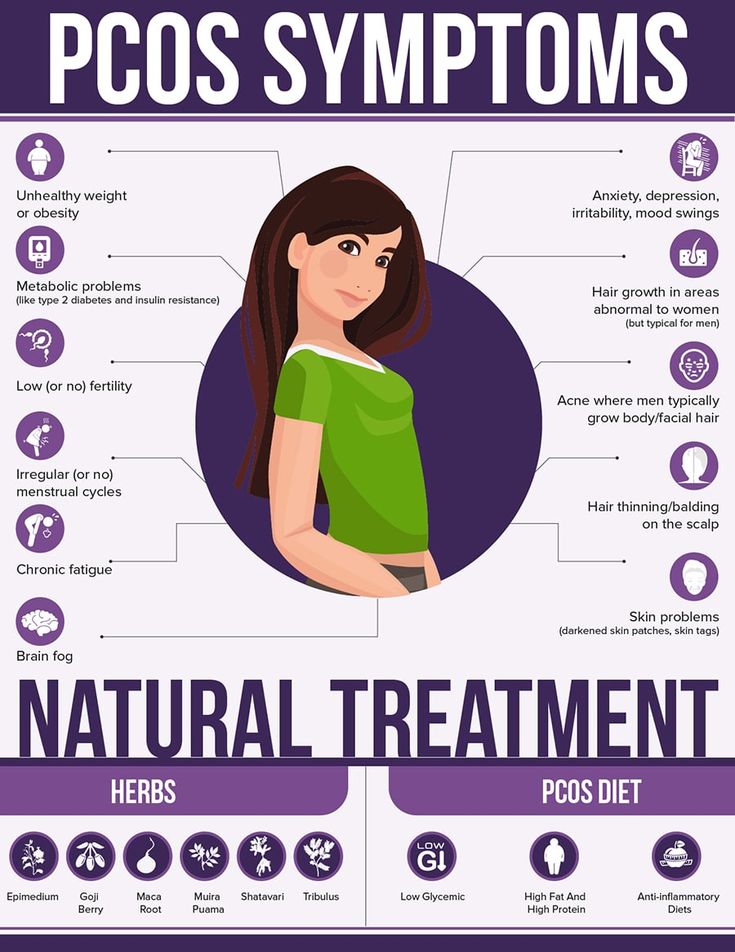
What are the symptoms of PCOS?
Some of the symptoms of PCOS include:
- Irregular menstrual cycle. Women with PCOS may miss periods or have fewer periods (fewer than eight in a year). Or, their periods may come every 21 days or more often. Some women with PCOS stop having menstrual periods.
- Too much hair on the face, chin, or parts of the body where men usually have hair.
 This is called "hirsutism." Hirsutism affects up to 70% of women with PCOS.3
This is called "hirsutism." Hirsutism affects up to 70% of women with PCOS.3 - Acne on the face, chest, and upper back
- Thinning hair or hair loss on the scalp; male-pattern baldness
- Weight gain or difficulty losing weight
- Darkening of skin, particularly along neck creases, in the groin, and underneath breasts
- Skin tags, which are small excess flaps of skin in the armpits or neck area
What causes PCOS?
The exact cause of PCOS is not known. Most experts think that several factors, including genetics, play a role:
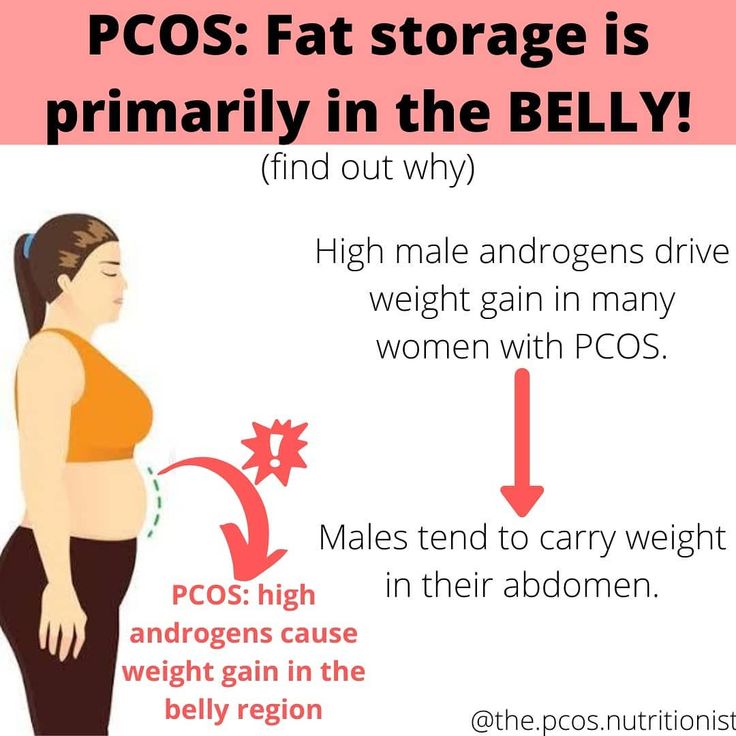
- High levels of androgens. Androgens are sometimes called "male hormones," although all women make small amounts of androgens. Androgens control the development of male traits, such as male-pattern baldness. Women with PCOS have more androgens than normal. Higher than normal androgen levels in women can prevent the ovaries from releasing an egg (ovulation) during each menstrual cycle, and can cause extra hair growth and acne, two signs of PCOS.
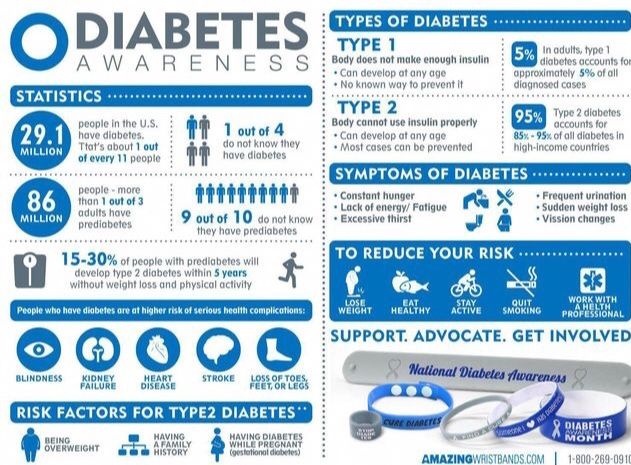
- High levels of insulin. Insulin is a hormone that controls how the food you eat is changed into energy. Insulin resistance is when the body's cells do not respond normally to insulin. As a result, your insulin blood levels become higher than normal. Many women with PCOS have insulin resistance, especially those who have overweight or obesity, have unhealthy eating habits, do not get enough physical activity, and have a family history of diabetes (usually type 2 diabetes). Over time, insulin resistance can lead to type 2 diabetes.
Can I still get pregnant if I have PCOS?
Yes. Having PCOS does not mean you can't get pregnant. PCOS is one of the most common, but treatable, causes of infertility in women. In women with PCOS, the hormonal imbalance interferes with the growth and release of eggs from the ovaries (ovulation). If you don't ovulate, you can't get pregnant.
Your doctor can talk with you about ways to help you ovulate and to raise your chance of getting pregnant. You can also use our Ovulation Calculator to see which days in your menstrual cycle you are most likely to be fertile.
You can also use our Ovulation Calculator to see which days in your menstrual cycle you are most likely to be fertile.
Is PCOS linked to other health problems?
Yes, studies have found links between PCOS and other health problems, including:
- Diabetes. More than half of women with PCOS will have diabetes or prediabetes (glucose intolerance) before the age of 40.4 Learn more about diabetes on our Diabetes page.
- High blood pressure. Women with PCOS are at greater risk of having high blood pressure compared with women of the same age without PCOS. High blood pressure is a leading cause of heart disease and stroke. Learn more about heart disease and stroke.
- Unhealthy cholesterol. Women with PCOS often have higher levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol. High cholesterol raises your risk of heart disease and stroke.
- Sleep apnea. This is when momentary and repeated stops in breathing interrupt sleep.
 Many women with PCOS have overweight or obesity, which can cause sleep apnea. Sleep apnea raises your risk of heart disease and diabetes.
Many women with PCOS have overweight or obesity, which can cause sleep apnea. Sleep apnea raises your risk of heart disease and diabetes. - Depression and anxiety. Depression and anxiety are common among women with PCOS.
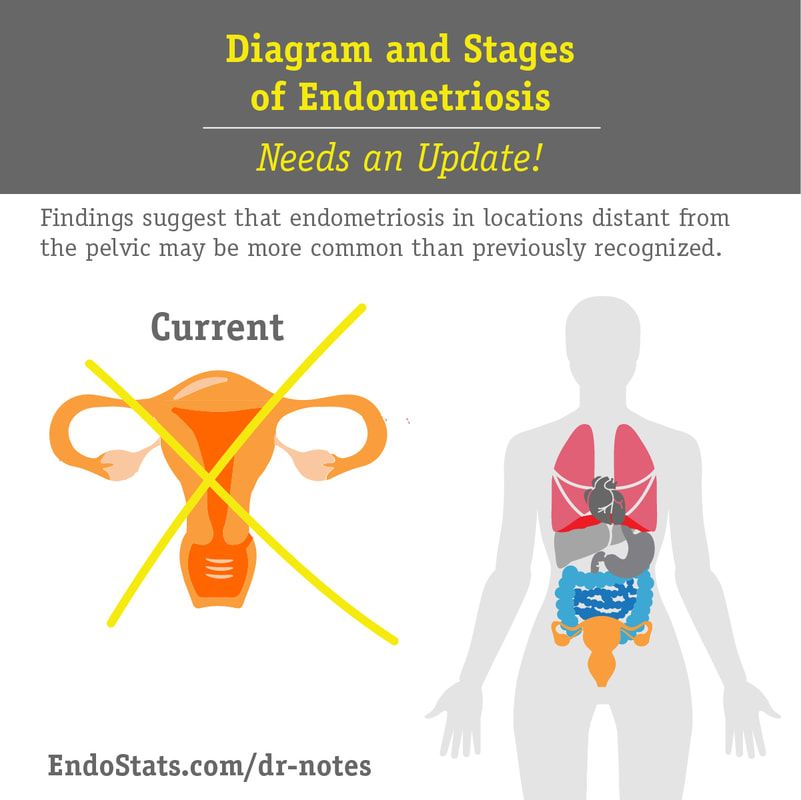
- Endometrial cancer. Problems with ovulation, obesity, insulin resistance, and diabetes (all common in women with PCOS) increase the risk of developing cancer of the endometrium (lining of the uterus or womb).
Researchers do not know if PCOS causes some of these problems, if these problems cause PCOS, or if there are other conditions that cause PCOS and other health problems.
Will my PCOS symptoms go away at menopause?
Yes and no. PCOS affects many systems in the body. Many women with PCOS find that their menstrual cycles become more regular as they get closer to menopause. However, their PCOS hormonal imbalance does not change with age, so they may continue to have symptoms of PCOS.
Also, the risks of PCOS-related health problems, such as diabetes, stroke, and heart attack, increase with age.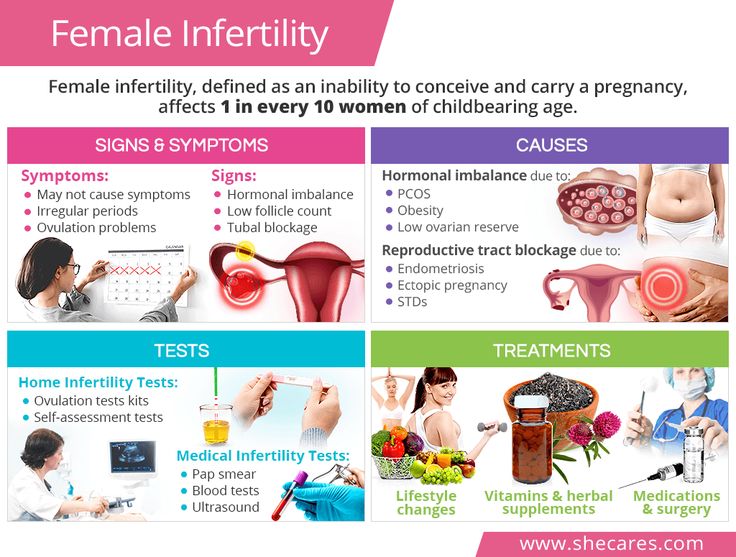 These risks may be higher in women with PCOS than those without.
These risks may be higher in women with PCOS than those without.
How is PCOS diagnosed?
There is no single test to diagnose PCOS. To help diagnose PCOS and rule out other causes of your symptoms, your doctor may talk to you about your medical history and do a physical exam and different tests:
- Physical exam. Your doctor will measure your blood pressure, body mass index (BMI), and waist size. They will also look at your skin for extra hair on your face, chest or back, acne, or skin discoloration. Your doctor may look for any hair loss or signs of other health conditions (such as an enlarged thyroid gland).
- Pelvic exam. Your doctor may do a pelvic exam for signs of extra male hormones (for example, an enlarged clitoris) and check to see if your ovaries are enlarged or swollen.
- Pelvic ultrasound (sonogram). This test uses sound waves to examine your ovaries for cysts and check the endometrium (lining of the uterus or womb).
- Blood tests. Blood tests check your androgen hormone levels, sometimes called "male hormones." Your doctor will also check for other hormones related to other common health problems that can be mistaken for PCOS, such as thyroid disease. Your doctor may also test your cholesterol levels and test you for diabetes.
Once other conditions are ruled out, you may be diagnosed with PCOS if you have at least two of the following symptoms:5
- Irregular periods, including periods that come too often, not often enough, or not at all
- Signs that you have high levels of androgens:
- Extra hair growth on your face, chin, and body (hirsutism)
- Acne
- Thinning of scalp hair
- Higher than normal blood levels of androgens
- Multiple cysts on one or both ovaries
How is PCOS treated?
There is no cure for PCOS, but you can manage the symptoms of PCOS. You and your doctor will work on a treatment plan based on your symptoms, your plans for having children, and your risk of long-term health problems such as diabetes and heart disease. Many women will need a combination of treatments, including:
Many women will need a combination of treatments, including:
- Steps you can take at home to help relieve your symptoms
- Medicines
What steps can I take at home to improve my PCOS symptoms?
You can take steps at home to help your PCOS symptoms, including:
- Losing weight. Healthy eating habits and regular physical activity can help relieve PCOS-related symptoms. Losing weight may help to lower your blood glucose levels, improve the way your body uses insulin, and help your hormones reach normal levels. Even a 10% loss in body weight (for example, a 150-pound woman losing 15 pounds) can help make your menstrual cycle more regular and improve your chances of getting pregnant.3 Learn more about healthy weight.
- Removing hair. You can try facial hair removal creams, laser hair removal, or electrolysis to remove excess hair. You can find hair removal creams and products at drugstores. Procedures like laser hair removal or electrolysis must be done by a doctor and may not be covered by health insurance.
- Slowing hair growth. A prescription skin treatment (eflornithine HCl cream) can help slow down the growth rate of new hair in unwanted places.
What types of medicines treat PCOS?
The types of medicines that treat PCOS and its symptoms include:
- Hormonal birth control, including the pill, patch, shot, vaginal ring, and hormone intrauterine device (IUD). For women who don't want to get pregnant, hormonal birth control can:
- Make your menstrual cycle more regular
- Lower your risk of endometrial cancer
- Help improve acne and reduce extra hair on the face and body (Ask your doctor about birth control with both estrogen and progesterone.)
- Anti-androgen medicines. These medicines block the effect of androgens and can help reduce scalp hair loss, facial and body hair growth, and acne. They are not approved by the Food and Drug Administration (FDA) to treat PCOS symptoms.
 These medicines can also cause problems during pregnancy.
These medicines can also cause problems during pregnancy. - Metformin. Metformin is often used to treat type 2 diabetes and may help some women with PCOS symptoms. It is not approved by the FDA to treat PCOS symptoms. Metformin improves insulin's ability to lower your blood sugar and can lower both insulin and androgen levels. After a few months of use, metformin may help restart ovulation, but it usually has little effect on acne and extra hair on the face or body. Recent research shows that metformin may have other positive effects, including lowering body mass and improving cholesterol levels.
What are my treatment options for PCOS if I want to get pregnant?
You have several options to help your chances of getting pregnant if you have PCOS:
- Losing weight. If you have overweight or obesity, losing weight through healthy eating and regular physical activity can help make your menstrual cycle more regular and improve your fertility.
 Find a personalized healthy eating plan using the MyPlate Plan tool.
Find a personalized healthy eating plan using the MyPlate Plan tool. - Medicine. After ruling out other causes of infertility in you and your partner, your doctor might prescribe medicine to help you ovulate, such as clomiphene (Clomid).
- In vitro fertilization (IVF). IVF may be an option if medicine does not work. In IVF, your egg is fertilized with your partner's sperm in a laboratory and then placed in your uterus to implant and develop. Compared to medicine alone, IVF has higher pregnancy rates and better control over your risk of having twins and triplets (by allowing your doctor to transfer a single fertilized egg into your uterus).
- Surgery. Surgery is also an option, usually only if the other options do not work. The outer shell (called the cortex) of ovaries is thickened in women with PCOS and thought to play a role in preventing spontaneous ovulation. Ovarian drilling is a surgery in which the doctor makes a few holes in the surface of your ovary using lasers or a fine needle heated with electricity.
 Surgery usually restores ovulation, but only for 6 to 8 months.
Surgery usually restores ovulation, but only for 6 to 8 months.
Read more about treating infertility in PCOS.
How does PCOS affect pregnancy?
PCOS can cause problems during pregnancy for you and for your baby. Women with PCOS have higher rates of:6
- Miscarriage
- Gestational diabetes
- Preeclampsia
- Cesarean section (C-section)
Your baby also has a higher risk of being heavy (macrosomia) and of spending more time in a neonatal intensive care unit (NICU).
How can I prevent problems from PCOS during pregnancy?
You can lower your risk of problems during pregnancy by:
- Reaching a healthy weight before you get pregnant. Use this interactive tool to see your healthy weight before pregnancy and what to gain during pregnancy.
- Reaching healthy blood sugar levels before you get pregnant. You can do this through a combination of healthy eating habits, regular physical activity, weight loss, and medicines such as metformin.
- Taking folic acid. Talk to your doctor about how much folic acid you need.
What is the latest research on PCOS?
Researchers continue to search for new ways to treat PCOS. Some current studies focus on:
- Genetics and PCOS
- Environmental exposure and PCOS risk
- Ethnic and racial differences in PCOS symptoms
- Medicines and supplements to restart ovulation
- Obesity and its link to PCOS
- Health risks for children of women with PCOS
To learn more about current PCOS treatment studies, visit ClinicalTrials.gov.
Did we answer your question about PCOS?
For more information on PCOS, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), NIH, HHS
Phone Number: 1-800-370-2943 - American Association of Clinical Endocrinologists
Phone Number: 904-353-7878 - American College of Obstetricians and Gynecologists
Phone Number: 1-800-673-8444 - American Society for Reproductive Medicine
Phone Number: 205-978-5000 - InterNational Council on Infertility Information Dissemination, Inc.
Phone Number: 703-379-9178 - PCOS Foundation
Phone Number: 713-487-7267 - PCOS Awareness Association
- PCOS Challenge
Sources
- Trivax, B., & Azziz, R. (2007). Diagnosis of polycystic ovary syndrome. Clinical Obstetrics and Gynecology, 50(1), 168–177.
- Bremer, A. A. (2010). Polycystic ovary syndrome in the pediatric population. Metabolic Syndrome and Related Disorders, 8(5), 375–394.
- American College of Obstetricians and Gynecologists. (2015). Polycystic ovary syndrome.
- Lorenz, L. B., & Wild, R. A. (2007). Polycystic ovarian syndrome: an evidence-based approach to evaluation and management of diabetes and cardiovascular risks for today's clinician. Clinical Obstetrics and Gynecology, 50, 226–243.
- Goodman, N. F., Cobin, R. H., Futterweit, W., Glueck, J. S., Legro, R. S., & Carmina, E. (2015). American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - part 1.
 Endocrine Practice, 11, 1291–300.
Endocrine Practice, 11, 1291–300. - Boomsma, C. M., Fauser, B. C., & Macklon, N.S. (2008). Pregnancy complications in women with polycystic ovary syndrome. Seminars in Reproductive Medicine, 26, 72–84.
The Office on Women's Health is grateful for the medical review by:
- Violanda Grigorescu, M.D., M.S.P.H., Chief, Partnerships and Evaluation Branch, Division of Health Informatics and Surveillance, Center for Surveillance, Epidemiology and Laboratory Services, Centers for Disease Control and Prevention
- Torie Comeaux Plowden, M.D., M.P.H., Fellow, Reproductive Endocrinology and Infertility, Eunice Kennedy Shriver National Institute of Child Health and Human Development
- Lubna Pal, M.B.B.S., M.R.C.O.G., M.S., F.A.C.O.G., Associate Professor, Director of the Polycystic Ovary Syndrome (PCOS) Program, Department of Obstetrics, Gynecology & Reproductive Sciences, Yale School of Medicine
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U. S. Department of Health and Human Services. Citation of the source is appreciated.
S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
PCOS (Polycystic Ovary Syndrome) and Diabetes
More than half of women with PCOS develop type 2 diabetes by age 40.
Ever heard of polycystic ovary syndrome (PCOS)? If you’re a woman who has had trouble getting pregnant, you might have. Just about everyone else? Probably not.
What is PCOS?
PCOS is one of the most common causes of female infertility, affecting 6% to 12% (as many as 5 million) of US women of reproductive age. But it’s a lot more than that. This lifelong health condition continues far beyond the child-bearing years.
Women with PCOS are often insulin resistant; their bodies can make insulin but can’t use it effectively, increasing their risk for type 2 diabetes. They also have higher levels of androgens (male hormones that females also have), which can stop eggs from being released (ovulation) and cause irregular periods, acne, thinning scalp hair, and excess hair growth on the face and body.
Women with PCOS can develop serious health problems, especially if they are overweight:
- Diabetes—more than half of women with PCOS develop type 2 diabetes by age 40
- Gestational diabetes (diabetes when pregnant)—which puts the pregnancy and baby at risk and can lead to type 2 diabetes later in life for both mother and child
- Heart disease—women with PCOS are at higher risk, and risk increases with age
- High blood pressure—which can damage the heart, brain, and kidneys
- High LDL (“bad”) cholesterol and low HDL (“good”) cholesterol—increasing the risk for heart disease
- Sleep apneaexternal icon—a disorder that causes breathing to stop during sleep and raises the risk for heart disease and type 2 diabetes
- Stroke—plaque (cholesterol and white blood cells) clogging blood vessels can lead to blood clots that in turn can cause a stroke
PCOS is also linked to depression and anxiety, though the connection is not fully understood.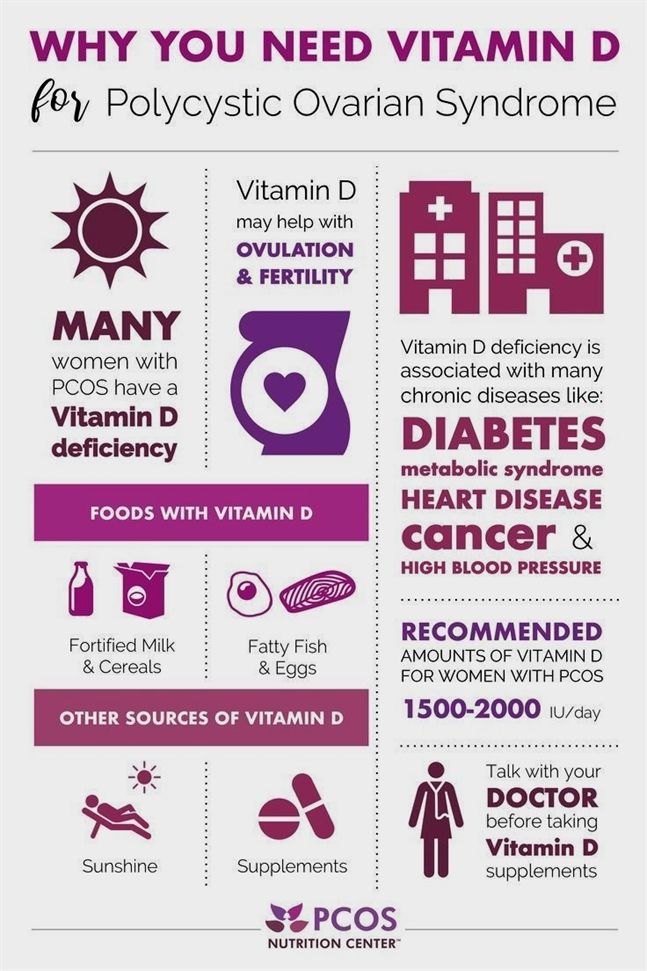
What Causes PCOS?
The exact causes aren’t known at this time, but androgen levels that are higher than normal play an important part. Excess weight and family history—which are in turn related to insulin resistance—can also contribute.
Weight…
Does being overweight cause PCOSexternal icon? Does PCOS make you overweight? The relationship is complicated and not well understood. Being overweight is associated with PCOS, but many women of normal weight have PCOS, and many overweight women don’t.
Family History…
Women whose mother or sister has PCOS or type 2 diabetes are more likely to develop PCOS.
…and Insulin Resistance
Lifestyle can have a big impact on insulin resistance, especially if a woman is overweight because of an unhealthy diet and lack of physical activity. Insulin resistance also runs in families. Losing weight will often help improve symptoms no matter what caused the insulin resistance.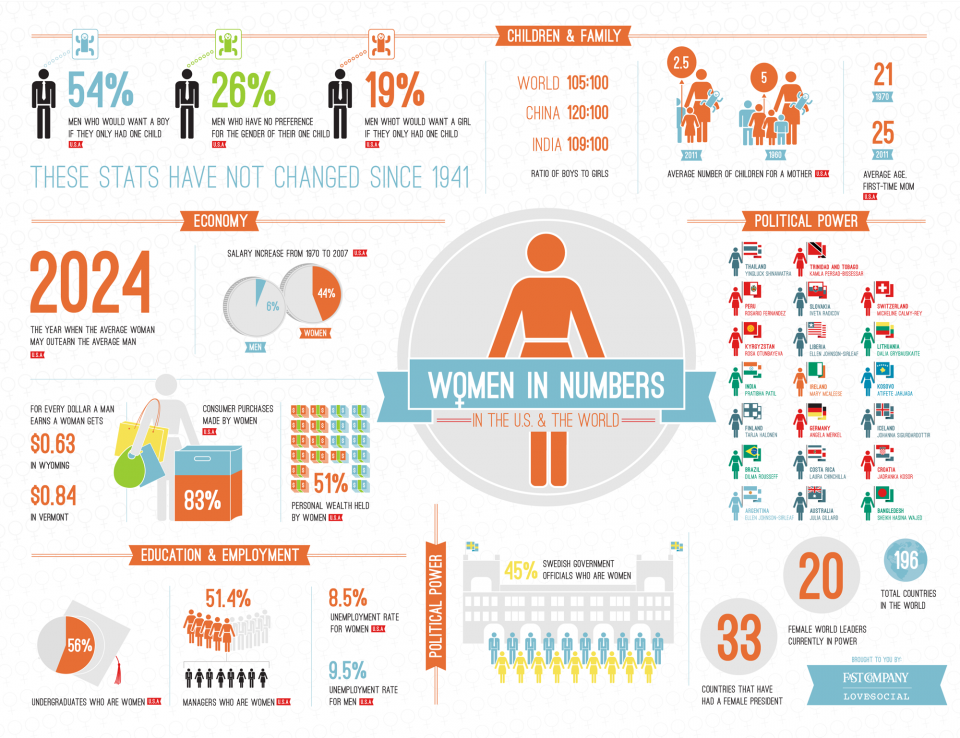
Do You Have PCOS?
Sometimes symptoms are clear, and sometimes they’re less obvious. You may visit a dermatologist (skin doctor) for acne, hair growth, or darkening of the skin in body creases and folds such as the back of the neck (acanthosis nigricans), a gynecologist (doctor who treats medical conditions that affect women and female reproductive organs) for irregular monthly periods, and your family doctor for weight gain, not realizing these symptoms are all part of PCOS. Some women will have just one symptom; others will have them all. Women of every race and ethnicity can have PCOS.
It’s common for women to find out they have PCOS when they have trouble getting pregnant, but it often begins soon after the first menstrual period, as young as age 11 or 12. It can also develop in the 20s or 30s.
To determine if you have PCOS, your doctor will check that you have at least 2 of these 3 symptoms:
- Irregular periods or no periods, caused from lack of ovulation
- Higher than normal levels of male hormones that may result in excess hair on the face and body, acne, or thinning scalp hair
- Multiple small cysts on the ovaries
Just having ovarian cysts isn’t enough for a diagnosis. Lots of women without PCOS have cysts on their ovaries and lots of women with PCOS don’t have cysts.
Lots of women without PCOS have cysts on their ovaries and lots of women with PCOS don’t have cysts.
Treatment
See your health care provider if you have irregular monthly periods, are having trouble getting pregnant, or have excess acne or hair growth. If you’re told you have PCOS, ask about getting tested for type 2 diabetes and how to manage the condition if you have it. Making healthy changes such as losing weight if you’re overweight and increasing physical activity can lower your risk for type 2 diabetes, help you better manage diabetes, and prevent or delay other health problems.
There are also medicines that can help you ovulate, as well as reduce acne and hair growth. Make sure to talk with your health care provider about all your treatment options.
European project launched to find a new treatment for polycystic ovary syndrome in young women
Latest news
The project will study the impact of a new treatment on improving the quality of life of adolescents and young girls suffering from polycystic ovary syndrome, which is diagnosed in 5-10% women in the world.
Lourdes Ibáñez, Endocrinologist at the Hospital Sant Joan de Deu in Barcelona and Head of the Metabolic Endocrinology Group at the Research Institute Sant Joan de Deu is coordinating the European project SPIOMET4HEALTH , a Phase II multicentre clinical trial to evaluate the efficacy of a new treatment for adolescents and young women with polycystic ovary syndrome (PCOS) .
SPIOMET4HEALTH is the first study to treat PCOS , a syndrome for which there is currently no approved treatment and which affects 5 to 10% of women worldwide.
Polycystic Ovary Syndrome (PCOS) has a profound effect on women's health and quality of life and can also affect their fertility. This pathology is the most common cause of anovulatory infertility and may also be associated with other types of diseases, such as type 2 diabetes , pre-menopausal cancer, anxiety or depression.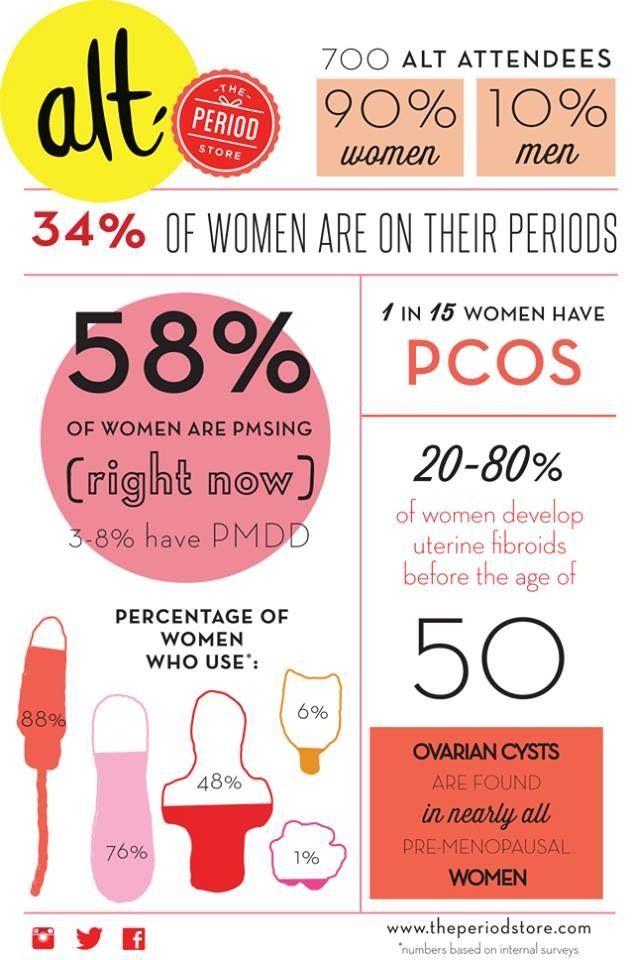
There is currently no approved treatment for PCOS in adolescents and young women , and in about 98% of cases they are prescribed oral contraceptives for other purposes.
Oral contraceptives relieve the underlying symptoms but do not change the underlying pathophysiology, and PCOS patients remain at risk for infertility after treatment. This project received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 899671.0007 Dr. Lourdes Ibáñez , head of the metabolic endocrinology group at the Research Institute Sant Joan de Deu and a pediatrician specializing in endocrinology at the Hospital Sant Joan de Deu , as well as some members of the consortium, have identified a new treatment for polycystic ovary syndrome, by combining three drugs: spironolactone, pioglitazone and metformin.
However, this is treatment for PCOS has some limitations: the drugs used in these studies are combinations of generic products that had to be administered separately, requiring three different tablets to be taken, leading to possible dose compliance issues.
In addition, these studies were conducted in small populations in limited ethnic groups and mainly in adolescents without overweight/obesity, which limits the relevance of the results in obese patients, which are approximately 50% of the population with PCOS.
“The SPIOMET4HEALTH project will overcome these limitations, as participants will only need to take one tablet per day, which will be a combination of three drugs, and their treatment will also be completed with measures to improve their lifestyle. Our goal is to achieve normalization of ovulation and endocrine-metabolic status by reducing excess hepato-visceral fat,” says Dr. Lourdes Ibáñez, study coordinator. nine0003
SPIOMET4Health may change the current paradigm for the treatment of polycystic ovary syndrome (PCOS) by offering a pathophysiological approach, as the new therapy will not only focus on the gonadotrophic axis, but also address the underlying causes of PCOS.
“We hope that through these projects, the number of adolescents and young women with PCOS will decrease, their quality of life will improve, and the economic burden on European health systems will decrease,” emphasizes the project coordinator. nine0003
Polycystic ovary syndrome (PCOS): description of the disease, causes, symptoms, cost of treatment in Moscow
Polycystic ovary syndrome (PCOS) is a pathological gynecological disease of the ovaries in a woman, in which cysts and benign tumors appear. It is caused by the growth of cystic growths inside and outside the ovaries. It appears as a result of a malfunction of the ovaries, pancreas or pituitary gland. The disease can be congenital, appear in adolescence even before the onset of the menstrual cycle. Appears as a result of inflammatory diseases and chronic pathologies. nine0003
Occurs when there is an excessive release of the male hormone. Therefore, it is often accompanied by obesity and an increase in hairline.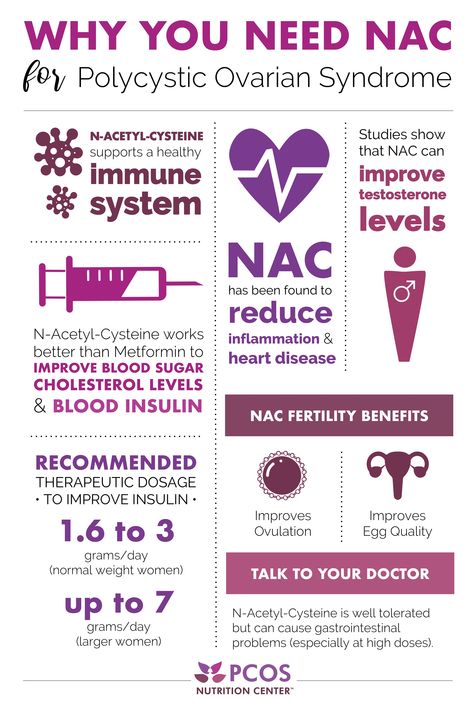 It most often occurs during puberty in girls, but women after menopause are also at risk. The development of cysts on the ovaries prevents the conception of a child or even leads to infertility. Women of mature age should not run chronic diseases, in order to avoid secondary PCOS.
It most often occurs during puberty in girls, but women after menopause are also at risk. The development of cysts on the ovaries prevents the conception of a child or even leads to infertility. Women of mature age should not run chronic diseases, in order to avoid secondary PCOS.
To determine this diagnosis, a number of studies will be required: examination by a gynecologist, various tests and masks, ultrasound. There is medical treatment, but the only way to get rid of the disease is surgery. nine0003
PCOS classification
The disease is divided into two types:
1. Primary (Stein-Leventhal syndrome) is due to congenital occurrence, and changes in the ovaries against the background of a hormonal disorder. This refers to the initial disruption of the female genital organs.
2. The secondary syndrome is characterized by abnormal functioning of the nervous and neuronal systems.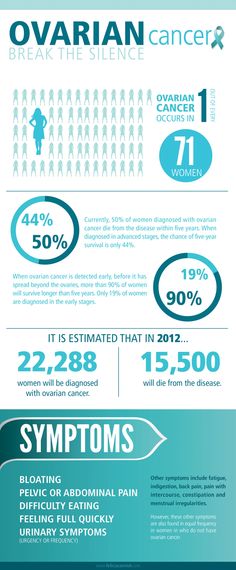 The causes are thyroid disease, diabetes mellitus. This includes obesity. nine0003
The causes are thyroid disease, diabetes mellitus. This includes obesity. nine0003
Causes
The first causes are violations of the functions of the endocrine system. The reason for this failure is the wrong interaction between the ovaries and the hypothalamus. Heredity also has its place in the causes of occurrence. Consider the following reasons:
-
Violation of the pituitary gland and hypothalamus. These organs are responsible for the functionality of the endocrine system, including the ovaries.
nine0101 -
Violation of the ovaries.
-
Incorrect work of the pancreas.
-
Insensitivity to insulin, excessive production of it in the body.
Adrenal failure. The level of male glands in the female body increases.
Experts cannot determine the exact reasons. There are many reasons why. Together they cause this syndrome. Increase the likelihood of confirming PCOS: nine0003
There are many reasons why. Together they cause this syndrome. Increase the likelihood of confirming PCOS: nine0003
-
obesity of varying degrees;
-
injuries in the groin area;
-
difficult births;
-
hypertension;
-
diabetes mellitus;
-
pathologies of the pituitary, thyroid or hypothalamus;
- nine0082 infections;
-
congenital pathologies of the female reproductive system;
-
termination of pregnancy;
-
hypothermia;
-
inflammatory processes;
-
overload;
-
change of climate zone; nine0003
-
mental disorders;
-
painful intercourse;
-
non-compliance with the rules of personal hygiene.
Violation of each factor leads to the immaturity of the follicle. The remaining underdeveloped parts form into brushes, which settle on the ovaries. They can be either single or multiple, reaching different sizes. They are a kind of bubbles with a liquid. This pathology occurs in 7% of patients. The growth of cysts leads to hyperplasia. It limits reproduction and leads to the absence of ovulation. Running ovarian syndrome, as a result, can lead to endometrial cancer. nine0191 How to recognize the disease
According to her feelings and symptoms, a woman will be able to recognize her diagnosis on her own. The sensations are quite specific, and if they are present, you should immediately seek medical help.
When the ovaries are damaged, their structure and function are disturbed. Starting its development, pathology from a young age of a girl can be painless and asymptomatic. Most often, the girl is not even aware of his presence. Manifestations can be very diverse: nine0003
Manifestations can be very diverse: nine0003
-
Failure of menstruation. There is not only a violation of the cycle, but also its complete absence. Sometimes the absence is accompanied by profuse bleeding.
-
Overweight. One of the symptoms, which is both the cause and the main violation of the hormonal background. In the presence of PCOS, a sharp weight gain is noticed.
-
Acne and pimples. All different forms of acne.
nine0104 -
Increased sweating. The appearance of greasiness, in particular on the hair of the head.
-
Increasing hairline on unintended areas of the female body. Black dense hairs appear. For example, on the chest, fingers, chin, in the perineum and above the lips of the mouth.
-
Drawing pain in lower abdomen. The pain is transient. It can give in different directions and be smooth or sharp.
 nine0003
nine0003 -
Inability to conceive. Long attempts to get pregnant do not work.
-
Change in appearance. The woman takes on a masculine face and body.
-
Alopecia. Hair loss occurs, as in men. Mainly on the crown and temporal sides of the head.
-
Dandruff in the hair. Unexpected appearance. If the water, hygiene products did not change, they did not wear other people's hats, etc. nine0003
-
The appearance of stretch marks. In the abdomen, thighs, chest. This is due to a sharp weight gain and an imbalance of hormones.
-
Acanthosis. The appearance of dark spots on the body. In particular, the axillary and papillary zone.
-
Increasing the level of insulin in the blood.
-
Hyperplasia. Excess and lack of hormones leads to the growth of uterine tissue.
 nine0003
nine0003 -
Increased blood pressure.
There are a number of other symptoms that are less common. Statistics show that 50% of women diagnosed with PCOS are obese. Also, the disease may be accompanied by:
Diagnosis and treatment of disease
Unfortunately, women seek medical help when the diagnosis of infertility can no longer be changed. Therefore, doctors insist on regular visits to the examination room. Confirmation of the diagnosis is carried out through various studies. nine0003
To begin with, the gynecologist examines the woman on the gynecological chair. He studies the medical history, listens to complaints and establishes the probable cause of PCOS. Visual examination of a woman - the condition of the skin, hair, physique. Measurement of body weight and calculation of the index and degree of obesity.
A biochemical blood test is prescribed to determine the level of hormones.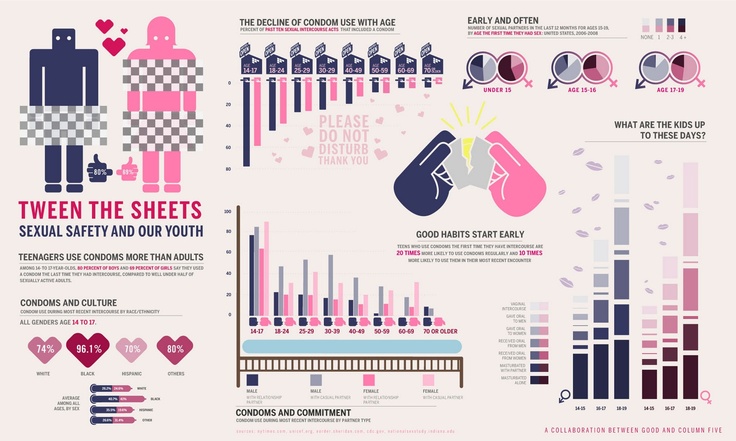 The presence of polycystic disease will be indicated by the level of FSH and LH. High blood levels of progesterone, androgen. Sugar can be elevated and cholesterol levels elevated. Perform ultrasound of the internal genital organs and abdominal cavity. Ultrasound shows the fouling of small cysts, an increase and thickening of the ovarian tissue. Carry out studies on the absence of the development of malignant tumors - CT and MRI. Scraping from the uterine mucosa will help establish the microflora and conduct a study for the presence of hyperplasia. As an additional therapy, an endocrinologist's consultation is prescribed. nine0003
The presence of polycystic disease will be indicated by the level of FSH and LH. High blood levels of progesterone, androgen. Sugar can be elevated and cholesterol levels elevated. Perform ultrasound of the internal genital organs and abdominal cavity. Ultrasound shows the fouling of small cysts, an increase and thickening of the ovarian tissue. Carry out studies on the absence of the development of malignant tumors - CT and MRI. Scraping from the uterine mucosa will help establish the microflora and conduct a study for the presence of hyperplasia. As an additional therapy, an endocrinologist's consultation is prescribed. nine0003
Treatment outcomes and goals:
1. Restoration of the menstrual cycle.
2. Stimulation of ovulation and conception of a child.
3. Correction of weight and improvement of well-being.
4. Elimination of visual problems and discomfort in a woman.
Reduce calorie intake (from 1200 to 1800 kcal per day). Limit the intake of animal fats. Add more vegetables and fruits, fiber, vitamins and nutritional supplements to the diet. Increase protein and carbohydrate levels. Exclude salty, fried, sweet and flour. Physical activity is also encouraged. Normalization of weight leads to the normalization of the menstrual cycle and leads to an improvement in the general condition of the patient. nine0003
Treatment of infertility in a woman consists of two stages: preparatory and the beginning of ovulation. Apply drugs depending on the form and syndrome of the disease. Start by lowering your insulin levels. Apply drugs that help reduce the sensitivity of the hypothalamus and pituitary gland. For example, Leuprorelin, Buserelin, Triptorelin.
In case of metabolic disorders, biguanides are prescribed. The dosage and course of treatment are selected individually. Antiestrogen is used to stimulate ovulation. The drug Clomiphene restores ovulation in 65% of women, and pregnancy occurs in every 3 patients. nine0003
The drug Clomiphene restores ovulation in 65% of women, and pregnancy occurs in every 3 patients. nine0003
At the second stage, stimulation of ovulation begins. According to the results of research and laboratory tests, a combination of drugs is prescribed to restore and resume the normal menstrual cycle in young women. With the effectiveness of the course of treatment, the childbearing function will be restored.
If a woman does not plan pregnancy, contraceptives are prescribed. Due to their properties, they restore the menstrual cycle. Treatment is carried out under the supervision of a specialist. The course of treatment lasts at least 6 months. nine0003
It is divided into 4 types:
1. Removal of a cyst with an electric current.
2. The epithelium of the ovaries changes with the help of electrical stimulation.
3. Burning of the follicular formation.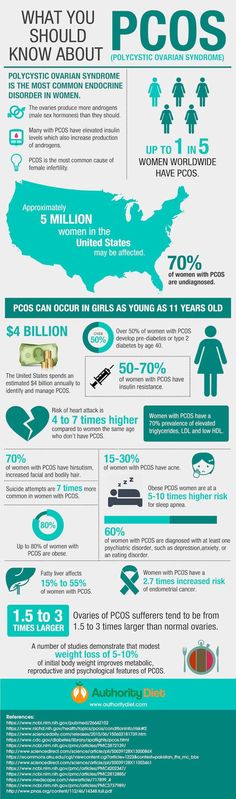
4. Removal of the pathological part of the ovaries.
Only the surgeon can choose the type of intervention. The least traumatic operations are performed. With PCOS, a wedge resection is also performed. It leads to the production of androgens and normalizes ovulation. More than 60% of women can get pregnant. Unfortunately, the effect lasts only 2-3 years, and then there is a relapse of polycystic disease. The most favorable is the first half of the year after the operation. A woman should undergo a course of treatment and be under constant supervision by a gynecologist in order to resolve the issue of conception as soon as possible. nine0003
Operation in progress
Resection is performed most often in gynecological operations. It is caused by the removal of a fragment of the ovary. The operation is not difficult. But it has complications, therefore it is performed only if this is the only and extreme measure for recovery.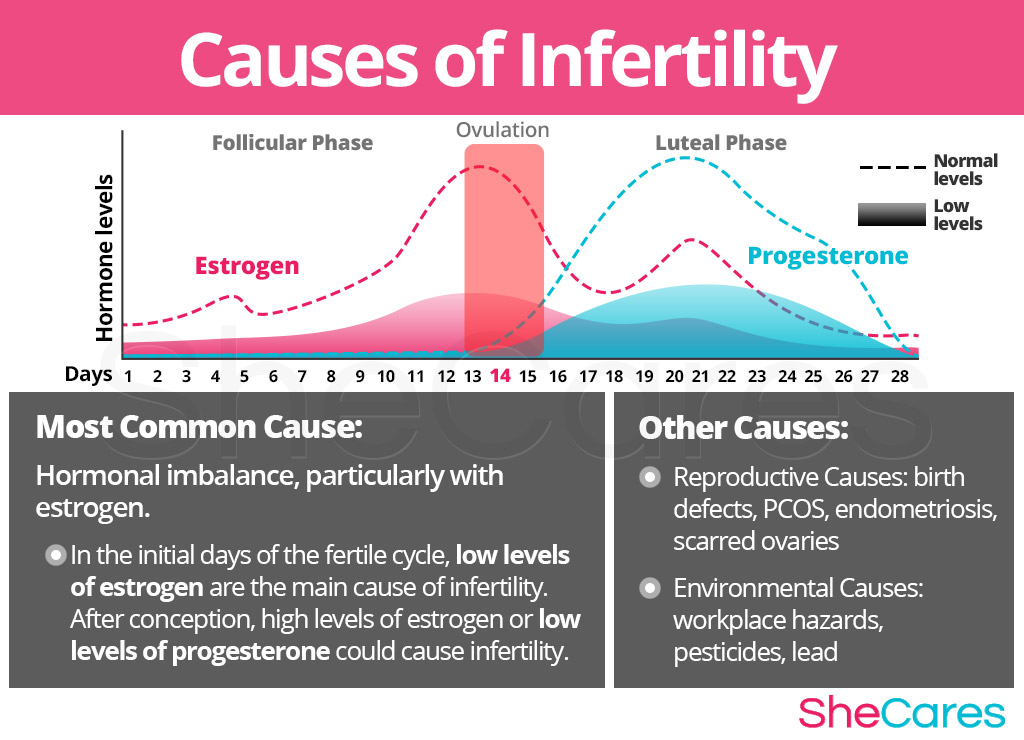 It is performed under general anesthesia. When the patient wants to improve reproductive function, save part of the ovary.
It is performed under general anesthesia. When the patient wants to improve reproductive function, save part of the ovary.
Indications:
1. Benign tumors of various origins. nine0003
2. Not the effectiveness of conservative treatment;
3. Polycystic and infertility.
4. Injuries.
5. A sharp deterioration in the condition, as a result of rupture of the cyst.
Contraindications:
1. Inflammatory process.
2. Infectious diseases (SARS, influenza, E. coli).
3. Malignant tumor, oncology. nine0003
4. Thrombophlebitis, poor blood clotting.
5. Pathologies of the cardiovascular or respiratory system.
6. Intolerance to anesthetics.
Before the start of the operation, the woman takes a standard set of tests.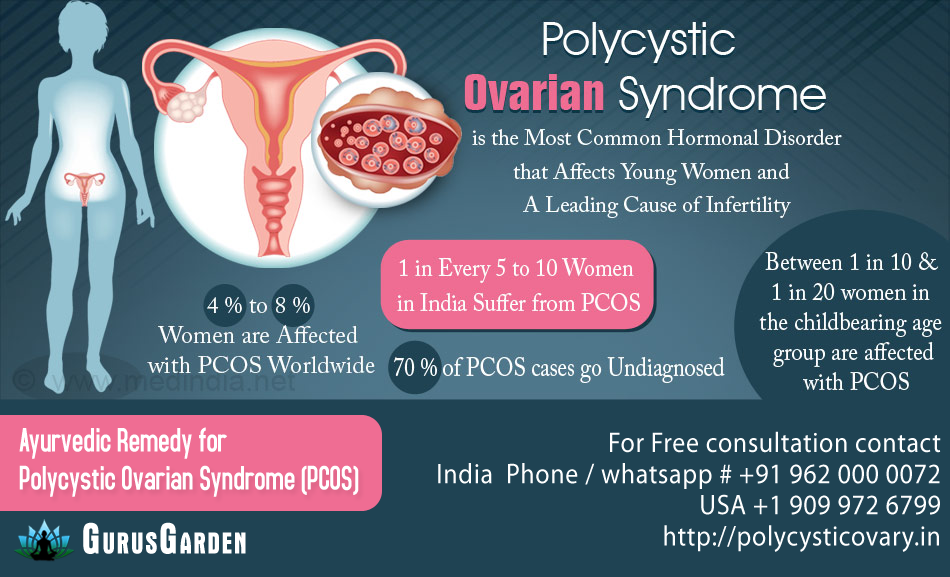 Urine and blood for biochemistry, coagulogram. A test is carried out for HIV infections, syphilis, AIDS, hepatitis, etc. Gynecological examination of the vagina. The results of ultrasound and x-rays of the pelvis. Fluorography and ECG. nine0003
Urine and blood for biochemistry, coagulogram. A test is carried out for HIV infections, syphilis, AIDS, hepatitis, etc. Gynecological examination of the vagina. The results of ultrasound and x-rays of the pelvis. Fluorography and ECG. nine0003
To avoid pneumonia after the surgical process, it is recommended not to eat 15 hours before the start. Perform bowel and stomach cleansing. To do this, use a laxative and cleansing enema.
During the operation, the surgeon performs several different incisions, introduces the necessary instruments to the affected area and performs the following actions:
-
Release of the ovary from cysts, organs and adhesions.
nine0101 -
Vessels are cauterized to stop bleeding.
-
The remaining gland is sutured with special threads.
-
All pelvic organs and the second ovary are examined.
-
Drain is installed.
nine0101
An incision is made in the ovary above the cystic tissue.
The instruments are removed and the incisions are sutured.
Rehabilitation
Pain begins a few hours after the operation. Painkillers are used. Over time, the pain will decrease as it heals. If the pain lasts longer than a week, complications may develop. The stitches are removed on the 7-10th day. Full recovery after surgery takes 4 to 8 weeks. Menstruation is restored within a couple of weeks. Ovulation sets in. nine0003
If the amount of tissue removed is of a normal size, then chances of getting pregnant are present. During the first weeks, sexual intercourse is excluded, and after the passage of pain and healing, you can begin to conceive. If pregnancy has not occurred within a year, you should again seek a gynecological consultation in order to exclude the diagnosis of complete infertility.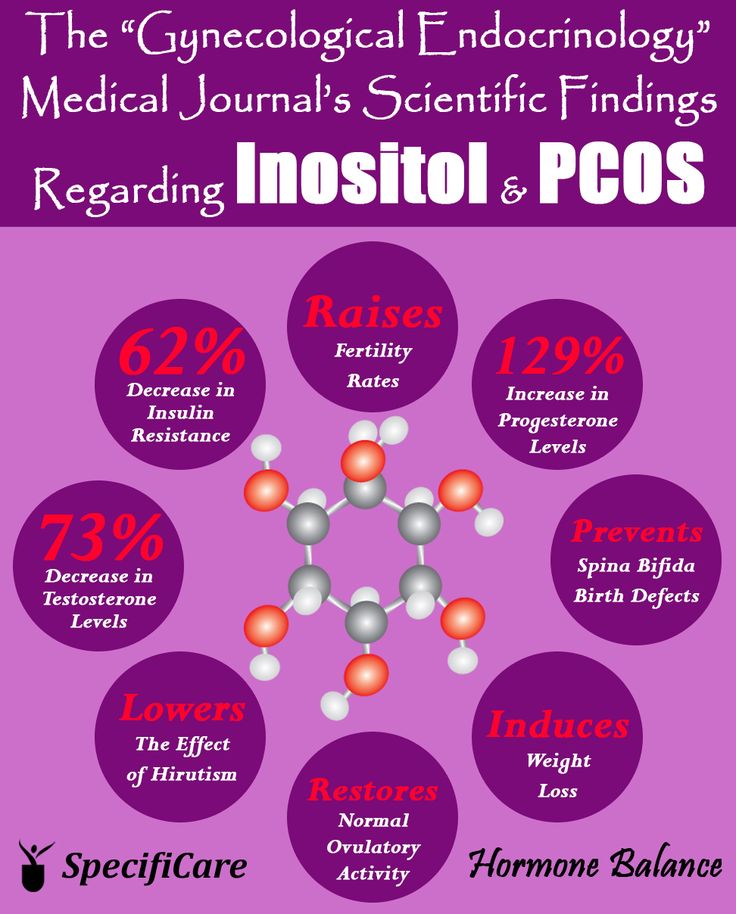
The consequence of the resection may be the rapid onset of menopause. The second type of complications are adhesions. These are adhesions between the intestines and the genitals, which do not allow pregnancy to occur. Infectious and inflammatory processes may develop, hematomas or hernias may appear, internal bleeding may open. nine0003
Infertility is the complete absence of ovulation. It may not occur at all or occur periodically up to 3 times a year. Lack of ovulation and hormonal imbalances lead to infertility. The running process of polycystic disease increases the risk of developing benign and malignant tumors, as well as cancer of the uterus and breast. The disease is accompanied by obesity, baldness and diabetes. Violations of the endocrine system lead to heart attack, stroke, kidney and liver diseases. Early detection and treatment of PCOS significantly reduces the risk of developing irreversible processes and increases the chance of returning to normal sexual and reproductive life.