Does bleeding always mean miscarriage
Bleeding in early pregnancy | The Royal Women's Hospital
If you bleed in early pregnancy it does not always mean that you are having a miscarriage; in fact it is quite common.
One in four women will bleed in early pregnancy, many of whom go on to have a healthy baby. However, if you have any bleeding at any time during your pregnancy, contact a health professional, so that appropriate investigation and treatment can be started.
Miscarriage and ectopic pregnancy (where the fetus is growing inside the fallopian tube) can both cause bleeding. It is also possible that you will have tests and investigations but the reason for your bleeding will not be found.
Investigating early bleeding
Your doctor is likely to begin with an internal examination to feel the size of your uterus and to look for any obvious visible sign of bleeding.
Ultrasound
After about six weeks of pregnancy the baby’s heart beat can usually be seen on ultrasound. If you have been bleeding, you will likely be offered a vaginal ultrasound because it offers the best possible view of your pregnancy. A vaginal ultrasound is a narrow probe, which is put inside the vagina; it feels much like an internal examination and is quite safe.
Before six weeks, the embryo is so small that it can be very difficult to see its heartbeat. An ultrasound this early is not likely to give any definite answers about the future of the pregnancy. The benefit of an early ultrasound is that it may locate a pregnancy that is growing in the fallopian tubes (an ectopic pregnancy). An ectopic pregnancy is very serious and if found you will be treated immediately.
If a heartbeat is found during an ultrasound it is likely that your pregnancy will continue with no further problems. Your chances of having a miscarriage in this scenario are less than one in twenty.
The ultrasound can also show if a pregnancy has stopped growing. Sometimes it is also possible to see that a miscarriage has begun and that some of the pregnancy tissue has been passed out of the uterus.
Blood tests
A blood test can measure the level of the pregnancy hormone hCG (human Chorionic Gonadotrophin), which changes depending on how pregnant you are.
- If the pregnancy hormone is lower than expected it might mean that you are not as pregnant as you thought or it could mean that the pregnancy is not growing normally. Usually a repeat blood test is needed after two days.
- If the pregnancy hormone is rising slower than is usual it might mean that you are miscarrying or the pregnancy is ectopic, sometimes though it is due to unusual hormonal patterns in an otherwise normal pregnancy.
- If the pregnancy hormone is falling this usually means that the pregnancy is ending and that you will miscarry.
Related Health Topics
-
- Pain and bleeding in early pregnancy
Bleeding in early pregnancy can be very distressing but it does not always mean that you are having a miscarriage.
 Bleeding is very common in early pregnancy, affecting about one in four women, many of whom will go on to have a healthy baby.
Bleeding is very common in early pregnancy, affecting about one in four women, many of whom will go on to have a healthy baby. -
- (English) PDF (166 KB)
- (Arabic) PDF (1 MB)
- (Chinese) (548 KB)
- (Somali) PDF (471 KB)
- (Turkish) PDF (351 KB)
- (Urdu) PDF (350 KB)
- (Vietnamese) PDF (323 KB)
- Pain and bleeding in early pregnancy
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy.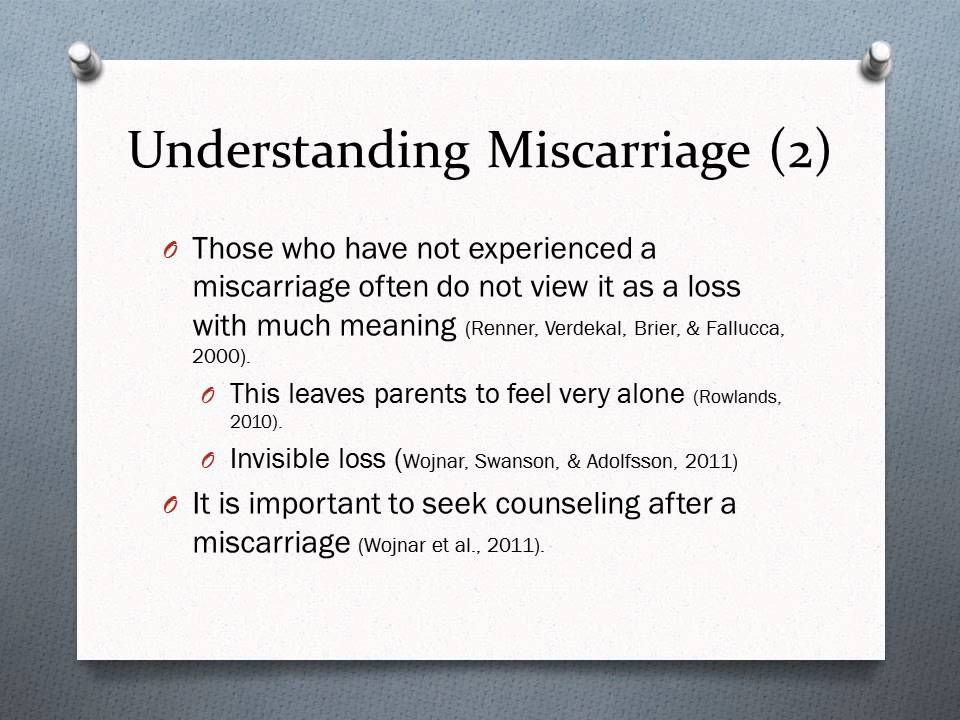 Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Vaginal Bleeding and Blood Clots During Pregnancy
Written by Stephanie Watson
In this Article
- Bleeding in the First Trimester
- Bleeding in the Second and Third Trimesters
- What to Do If You Have Abnormal Bleeding During Pregnancy
Bleeding during pregnancy is common, especially during the first trimester, and usually it's no cause for alarm. But because bleeding can sometimes be a sign of something serious, it's important to know the possible causes, and get checked out by your doctor to make sure you and your baby are healthy.
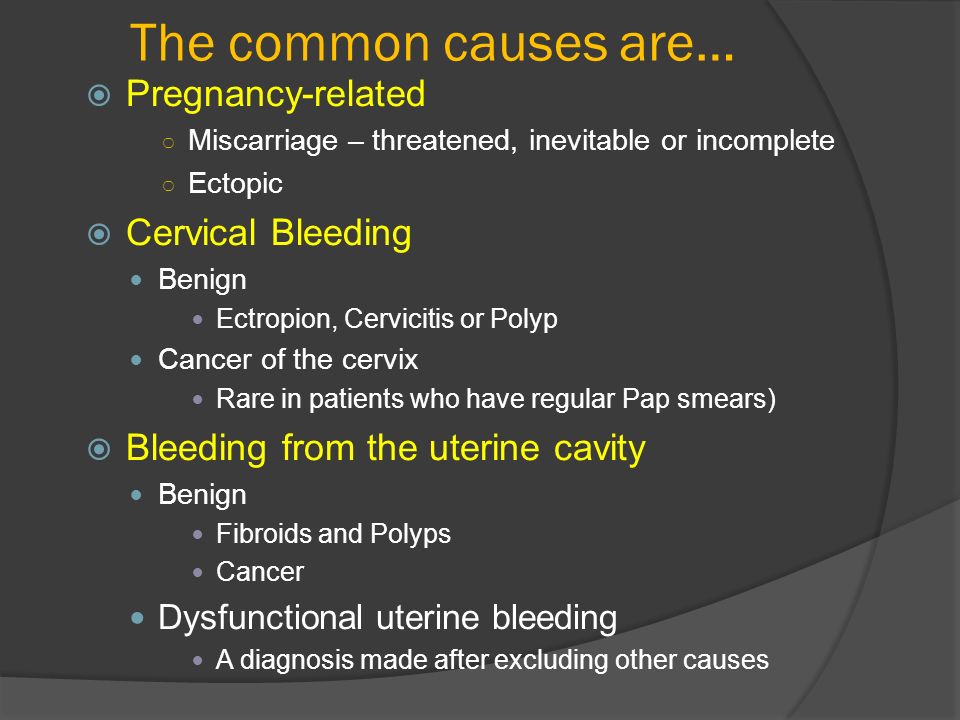
Bleeding in the First Trimester
About 20% of women have some bleeding during the first 12 weeks of pregnancy. Possible causes of first trimester bleeding include:
Possible causes of first trimester bleeding include:
Implantation bleeding. You may experience some normal spotting within the first six to 12 days after you conceive as the fertilized egg implants itself in the lining of the uterus. Some women don't realize they are pregnant because they mistake this bleeding for a light period. Usually the bleeding is very light and lasts from a few hours to a few days.
Miscarriage. Because miscarriage is most common during the first 12 weeks of pregnancy, it tends to be one of the biggest concerns with first trimester bleeding. However, first trimester bleeding does not necessarily mean that you’ve miscarried or will miscarry. In fact, if a heartbeat is seen on ultrasound, over 90% of women who experience first trimester vaginal bleeding will not miscarry.
Other symptoms of miscarriage are strong cramps in the lower abdomen and tissue passing through the vagina.
Ectopic pregnancy. In an ectopic pregnancy, the fertilized embryo implants outside of the uterus, usually in the fallopian tube. If the embryo keeps growing, it can cause the fallopian tube to burst, which can be life-threatening to the mother. Although ectopic pregnancy is potentially dangerous, it only occurs in about 2% of pregnancies.
If the embryo keeps growing, it can cause the fallopian tube to burst, which can be life-threatening to the mother. Although ectopic pregnancy is potentially dangerous, it only occurs in about 2% of pregnancies.
Other symptoms of ectopic pregnancy are strong cramps or pain in the lower abdomen, and lightheadedness.
Molar pregnancy (also called gestational trophoblastic disease). This is a very rare condition in which abnormal tissue grows inside the uterus instead of a baby. In rare cases, the tissue is cancerous and can spread to other parts of the body.
Other symptoms of molar pregnancy are severe nausea and vomiting, and rapid enlargement of the uterus.
Additional causes of bleeding in early pregnancy include:
- Cervical changes. During pregnancy, extra blood flows to the cervix. Intercourse or a Pap test, which cause contact with the cervix, can trigger bleeding. This type of bleeding isn't cause for concern.
- Infection. Any infection of the cervix, vagina, or a sexually transmitted infection (such as chlamydia, gonorrhea, or herpes) can cause bleeding in the first trimester.

Bleeding in the Second and Third Trimesters
Abnormal bleeding in late pregnancy may be more serious because it can signal a problem with the mother or baby. Call your doctor as soon as possible if you experience any bleeding in your second or third trimester.
Possible causes of bleeding in late pregnancy include:
Placenta previa. This condition occurs when the placenta sits low in the uterus and partially or completely covers the opening of the birth canal. Placenta previa is very rare in the late third trimester, occurring in only one in 200 pregnancies. A bleeding placenta previa, which can be painless, is an emergency requiring immediate medical attention.
Placental abruption. In about 1% of pregnancies, the placenta detaches from the wall of the uterus before or during labor and blood pools between the placenta and uterus. Placental abruption can be very dangerous to both the mother and baby.
Other signs and symptoms of placental abruption are abdominal pain, clots from the vagina, tender uterus, and back pain.
Uterine rupture. In rare cases, a scar from a previous C-section can tear open during pregnancy. Uterine rupture can be life-threatening, and requires an emergency C-section.
Other symptoms of uterine rupture are pain and tenderness in the abdomen.
Vasa previa. In this very rare condition, the developing baby's blood vessels in the umbilical cord or placenta cross the opening to the birth canal. Vasa previa can be very dangerous to the baby because the blood vessels can tear open, causing the baby to bleed severely and lose oxygen.
Other signs of vasa previa include abnormal fetal heart rate and excessive bleeding.
Premature labor. Vaginal bleeding late in pregnancy may just be a sign that your body is getting ready to deliver. A few days or weeks before labor begins, the mucus plug that covers the opening of the uterus will pass out of the vagina, and it will usually have small amounts of blood in it (this is known as "bloody show"). If bleeding and symptoms of labor begin before the 37th week of pregnancy, contact your doctor right away because you might be in preterm labor.
Other symptoms of preterm labor include contractions, vaginal discharge, abdominal pressure, and ache in the lower back.
Additional causes of bleeding in late pregnancy are:
- Injury to the cervix or vagina
- Polyps
- Cancer
What to Do If You Have Abnormal Bleeding During Pregnancy
Because vaginal bleeding in any trimester can be a sign of a problem, call your doctor. Wear a pad so that you can keep track of how much you're bleeding, and record the type of blood (for example, pink, brown, or red; smooth or full of clots). Bring any tissue that passes through the vagina to your doctor for testing. Don't use a tampon or have sex while you are still bleeding.
Your doctor might recommend that you rest as much as you can and avoid exercise and travel.
You should expect to receive an ultrasound to identify what the underlying cause of your bleeding may be. Vaginal and abdominal ultrasounds are often performed together as part of a full evaluation.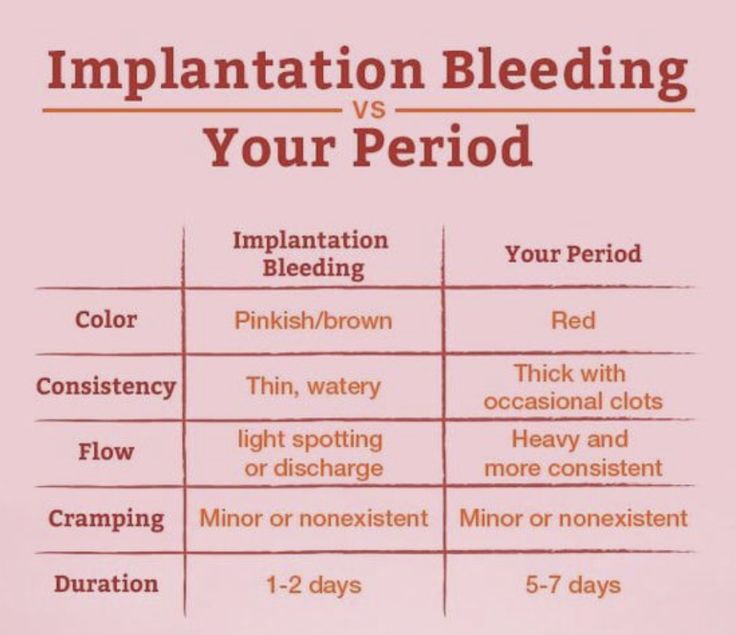
Go to the emergency room or call 911 right away if you have any of the following symptoms, which could be signs of a miscarriage or other serious problem:
- Severe pain or intense cramps low in the abdomen
- Severe bleeding, with or without pain
- Discharge from the vagina that contains tissue
- Dizziness or fainting
- A fever of more than 100.4 or more degrees Fahrenheit and/or chills
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
12 important things to know about miscarriage
Most miscarriages occur in the first trimester
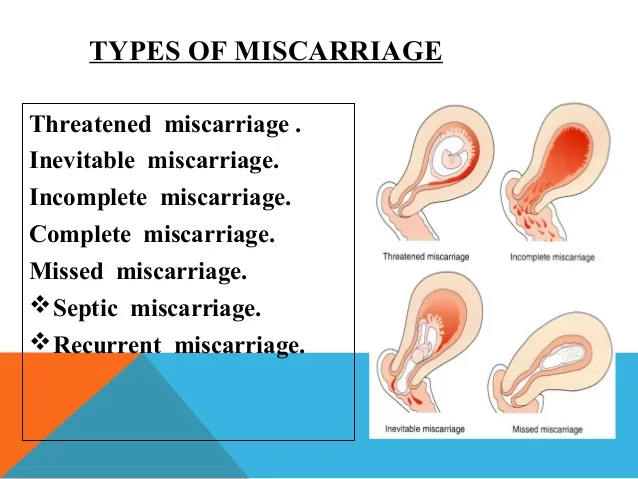
A miscarriage is considered a loss of pregnancy that occurs before the 20th week of pregnancy, after which it will be called intrauterine fetal death.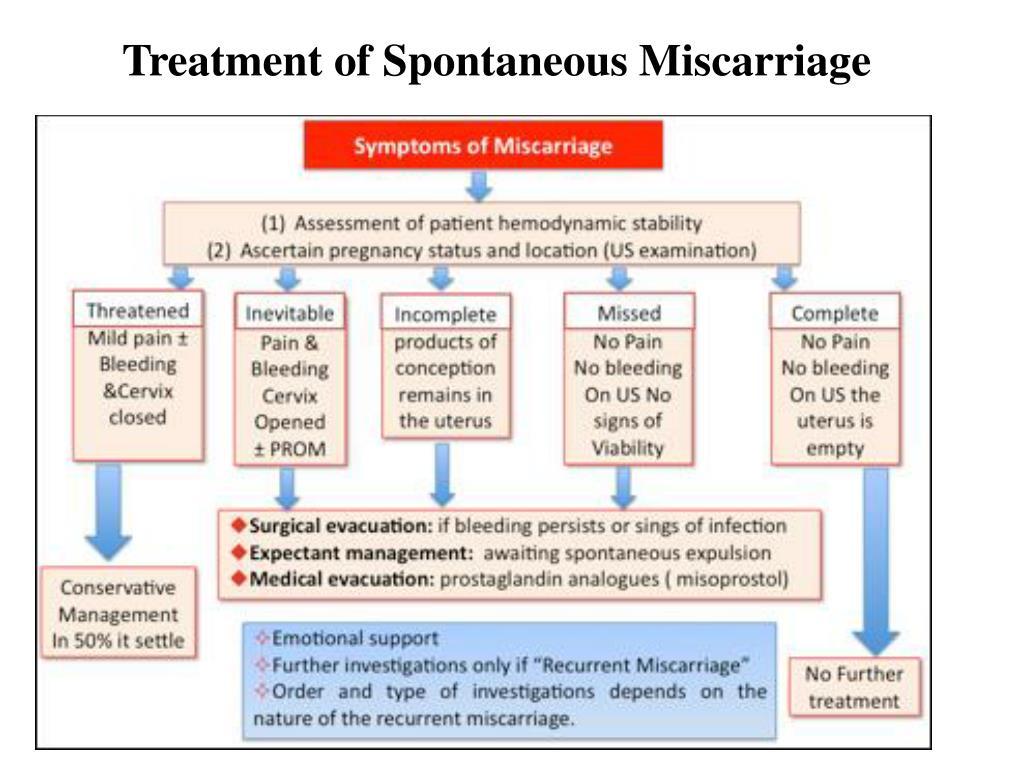 In most cases, miscarriages occur between the sixth and 12th weeks of pregnancy. One out of four clinically confirmed pregnancies ends in miscarriage. This is the most common "complication" of the first trimester.
In most cases, miscarriages occur between the sixth and 12th weeks of pregnancy. One out of four clinically confirmed pregnancies ends in miscarriage. This is the most common "complication" of the first trimester.
Bloody discharge is not always a sign of a miscarriage
Most miscarriages are accompanied by cramping and bleeding. However, the appearance of spotting is not always a sign that the pregnancy is lost. According to experts, spotting accompanies 15-25 percent of pregnancies.
It is quite common to have spotting after sex during pregnancy. They can last up to 72 hours after intercourse and do not cause any discomfort to the woman.
However, any reddish discharge (especially if it is profuse and bright) that makes a woman anxious should be discussed with a doctor as soon as possible.
If you have a miscarriage, this does not mean that a new attempt to get pregnant is doomed to failure. “Miscarriages happen quite often. Two inconsistent spontaneous abortions for one couple are considered normal. However, only about five percent of women experience two consecutive miscarriages, and only one percent three miscarriages in a row,” says OB/GYN, reproductive endocrinologist Sally Tazuki.
Two inconsistent spontaneous abortions for one couple are considered normal. However, only about five percent of women experience two consecutive miscarriages, and only one percent three miscarriages in a row,” says OB/GYN, reproductive endocrinologist Sally Tazuki.
If a woman has had two miscarriages in a row, there is a 23 percent chance that a third miscarriage will also result in a miscarriage. With three miscarriages in a row, the risk is 32 percent; with four, it goes up to 37 percent. And yet, if miscarriages do not occur due to diagnosed reproductive problems, their history does not affect reproductive potential in any way.
In most cases, miscarriage is an accidental situation
According to Tazuka, 75 percent of miscarriages are due to aneuploidy, a disorder in the number of chromosomes in the fetal genome. And again, there is usually no particular reason for this. Even in the 50-75 percent of women who have had multiple miscarriages (called recurrent miscarriages), it is often impossible to diagnose any one problem leading to miscarriage.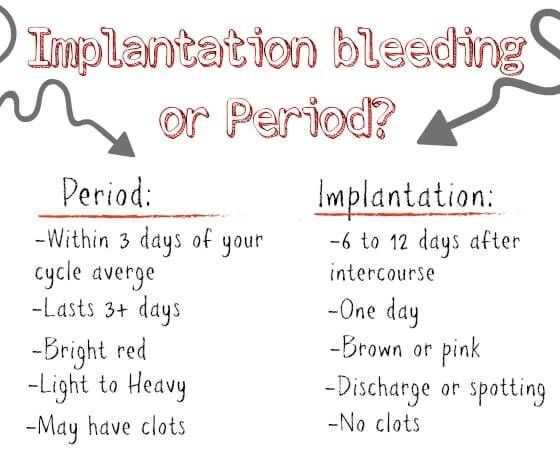
In addition to aneuploidy (or other chromosomal abnormalities), other common causes of pregnancy loss include anatomical abnormalities (such as uterine fibroids and uterine septum), hormonal disorders (such as thyroid dysfunction and diabetes), and an autoimmune disease known as antiphospholipid syndrome.
Youth helps prevent miscarriages
The younger the mother-to-be, the more likely she is to carry a pregnancy without losing it. If you are under 30 years old, the chance of spontaneous abortion is ten percent, and closer to 40 years, this risk is already 33 percent. Yes, miscarriage is an accident, but after the age of 30, these accidents happen more often. If you are in your 30s and have already had miscarriages, there is a good chance that you will have to go through IVF.
A man's age also affects the ability to carry a pregnancy
The age of a woman is only one side of the story. There are studies that show that the success of carrying a pregnancy also depends on the age of the future father.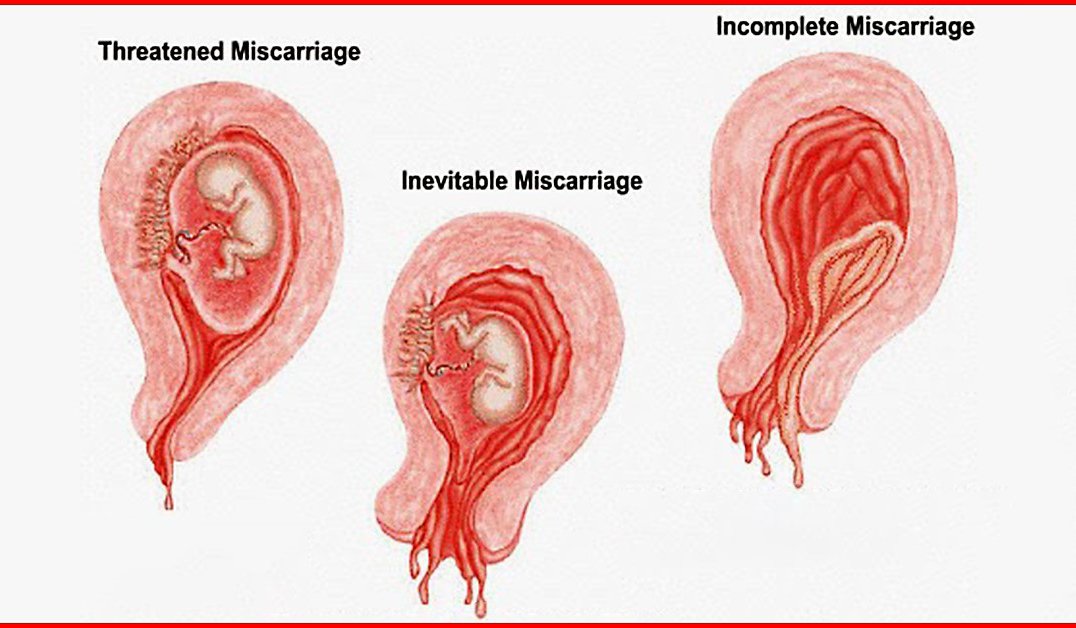 So, Mayo Clinic tells us that if a man is over 40 years old, the likelihood of spontaneous termination of pregnancy from him increases.
So, Mayo Clinic tells us that if a man is over 40 years old, the likelihood of spontaneous termination of pregnancy from him increases.
Health matters
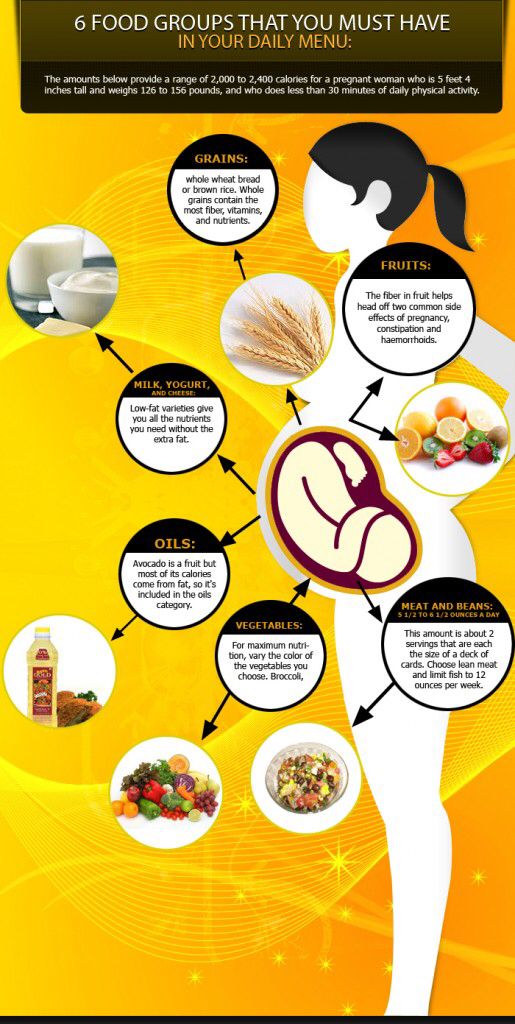
Women with chronic conditions such as diabetes, thyroid disorders and obesity are at risk. Sudden weight changes are also bad for the chances of carrying a pregnancy, although obesity is more dangerous, as it usually comes with associated problems, including diabetes.
Doctors also strongly recommend quitting smoking and drinking alcohol at the planning stage. While there is well-established evidence that nicotine and alcohol interfere with a woman's ability to sustain future pregnancies, the gynecological community believes that these substances should be avoided to reduce the risks.
Just in case, doctors advise avoiding coffee and caffeinated drinks. Current research suggests that 200 milligrams of caffeine per day (the equivalent of two servings of natural coffee) is a safe dose. You should also avoid unpasteurized milk cheeses and deli meats from the culinary department, as these products can contain listeria, bacteria that can cause intrauterine fetal death in the second and third trimester.
Toxins are dangerous for pregnancy
Toxins that a pregnant woman interacts with can also affect the course of gestation. For example, exposure to solvents, pesticides, lead, or BPA can lead to fetal abnormalities and possible miscarriage.
But there is some good news
Sex, sports and stress - the three C's - are not dangerous activities during pregnancy. Sex can be engaged in a mode that suits both parents-to-be both physically and emotionally. Yes, it is better to avoid stress, simply because without them, life, and even more so pregnancy, is generally easier. And you can continue the sport if you already have such a habit. But you should not start pulling barbells as soon as you find out about pregnancy. The load should remain the same.
Fertility treatment does not affect the risk of miscarriage
Women undergoing fertility treatment are at the same risk of miscarriage as those who conceive naturally.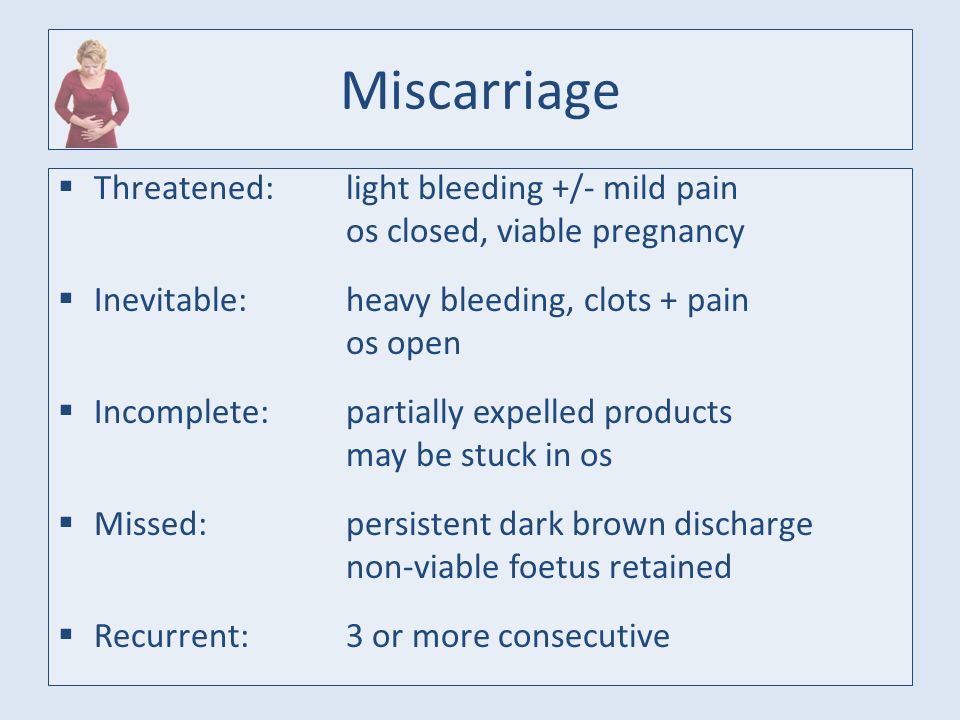 The fact that immediately after IVF some people cannot bear pregnancy is not explained by the procedure itself, but most often by the age of the patient.
The fact that immediately after IVF some people cannot bear pregnancy is not explained by the procedure itself, but most often by the age of the patient.
After a miscarriage, medical intervention is not always required.
According to Dr. Tazuka, there are three types of spontaneous abortion: complete, incomplete, and miscarriage. In the first case, during heavy bleeding, all the products of conception come out of the woman’s internal genital organs (this, one way or another, requires confirmation by ultrasound), in the second, some fetal tissues remain in the woman’s body, despite the fact that she survived bleeding and cramping. pain. In the third case, the pregnancy simply stops developing, and the frozen fetus remains in the womb. As a rule, the remaining products of conception are completely removed using scraping. The recovery period after the procedure is different for everyone, but if everything is okay and you feel normal, you can try again after the next period.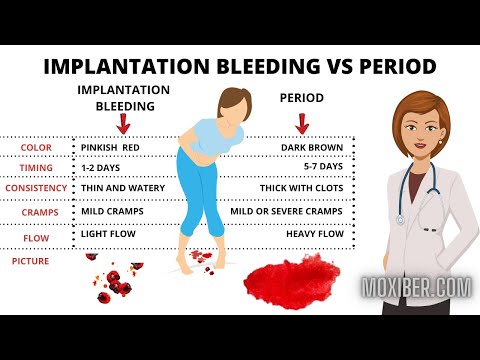 They usually start six weeks after the procedure.
They usually start six weeks after the procedure.
It is normal to worry about losing a pregnancy
Many people think that a miscarriage is nothing, a common thing, because there has never been a “real” child. You don't have to listen to those who hold this opinion. A lost pregnancy - at any time - is painful and scary. You can mourn the loss, experience and grieve. Do not keep feelings in yourself, talk with your partner and loved ones, do not be ashamed of your pain. Ask for support, especially since there is now a service on RuNet that helps couples cope with pregnancy loss.
90,000 miscarriage, symptoms - Health Clinic 365 G. YekaterinburgCauses of miscarriage
Questions to the doctor about miscarriages
Diagnostics of miscarriage
Treatment and prevention of miscarriage
Patterns - this is a spontaneous termination of pregnancy in a period of up to 20 weeks. According to statistics, 10 to 20% of all pregnancies end in miscarriage.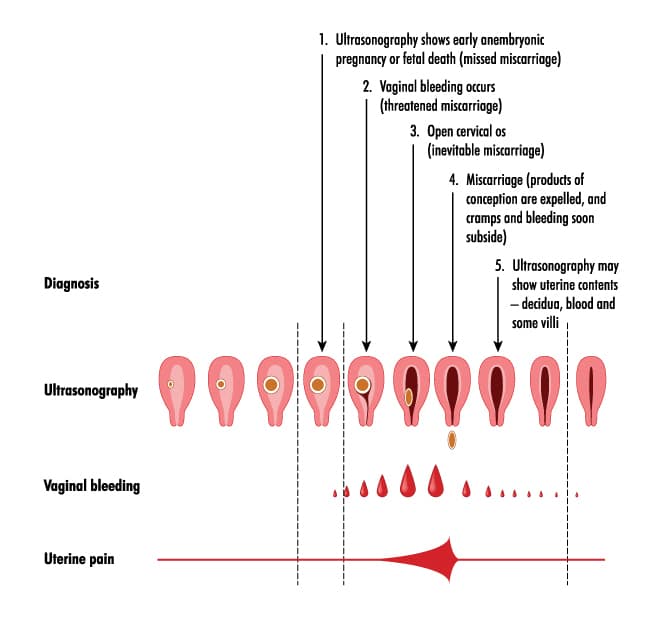 However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Symptoms of miscarriage .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common.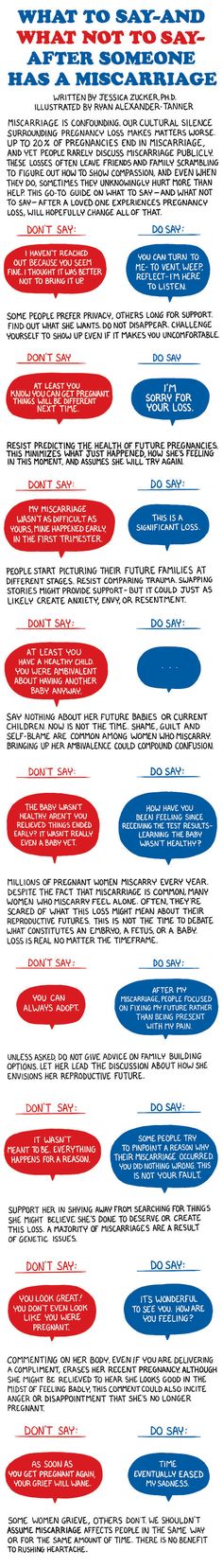 In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Call your doctor if:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.