Pregnancy skin irritation
6 skin problems that can develop during pregnancy | Your Pregnancy Matters
You’re well into pregnancy, so where’s that “pregnancy glow” you’ve heard about? Instead of bright, radiant-looking skin, you might look more like a pimple-faced teenager. Maybe dark splotches have popped up on your face. Or perhaps you’re itchy from a rash that has sprung up around the stretch marks on your belly.
Pregnancy can bring about many strange symptoms, and your skin is not immune to the hormone changes you’re experiencing. Fortunately, while annoying, most of these conditions are harmless and will subside after you give birth.
Let’s take a look as some of the most common skin problems that pop up during pregnancy and how to manage them. We’ll also discuss one serious condition of which to be aware.
‘Mask of pregnancy’ and linea nigra
Both of these benign conditions are the result of increased pigmentation caused by a surge of pregnancy hormones. Melasma, also known as the “mask of pregnancy,” causes dark splotches to appear on your face, often on the nose and cheeks. Linea nigra is a dark line that can form between your belly button and pubic area during pregnancy.
If you experience either of these, you’re not alone. Nearly 75 percent of pregnant women will have the mask of pregnancy, and 90 percent will notice linea nigra.
This increase in pigmentation can affect any area of your body that is more pigmented. Many women, for example, report much darker freckles or areolas than normal. And the darker your skin tone, the more you may notice these changes.
You can’t totally prevent these conditions, but using a good sunscreen, especially on your face, can help reduce the effects. Don’t worry – you won’t be stuck with these changes forever. Most should fade after you give birth. Melasma sometimes doesn’t go away, but a dermatologist can treat it with medication after pregnancy.
Stretch marks
Almost every pregnant woman will get stretch marks, which are reddish streaks that run down your breasts or belly. They’re more likely to appear if you gain weight rapidly, so follow your doctor’s recommendation regarding weight gain. However, getting stretch marks sometimes just comes down to genetics.
However, getting stretch marks sometimes just comes down to genetics.
After birth, your stretch marks should turn a less-obvious silver or white color. You can try to prevent stretch marks by keeping your skin moisturized with cocoa butter or lotion. If you’re tempted to try an herbal remedy, talk to your doctor first.
Acne
Many of my patients complain about this during pregnancy. All those hormones in your body can cause oil glands to secrete more oil, causing breakouts.
Try cleaning your face with an over-the-counter-face soap in the morning and evening. Most over-the-counter topical treatments are safe in pregnancy, but if you have any concerns about a certain product, you can ask your doctor. There are a few topical prescription medications we can try during pregnancy, but your acne should get better after your baby is born.
Skin tags
These small, loose, harmless growths of skin can appear anywhere on your body during pregnancy, but most commonly pop up under the arms and breasts. Unfortunately, there’s nothing you can do to prevent them, but they can easily be removed after pregnancy if you want.
Unfortunately, there’s nothing you can do to prevent them, but they can easily be removed after pregnancy if you want.
PUPPP
Itchy rashes are common during pregnancy. PUPPPs, pruritic urticarial papules and plaques of pregnancy, is the most common pregnancy rash. These itchy, red patches spring up around stretch marks – usually toward the end of pregnancy when your belly is stretched the most – and can spread to the arms, legs, and buttocks.
This condition is harmless, but I know from experience it can be annoying. PUPPPs will go away after you give birth, but don’t feel like you need to suffer through it until then. We can give you a steroid cream that will relieve the itching and prevent it from spreading. This cream is safe for you and your baby.
Cholestasis of pregnancy
There are times you shouldn’t ignore itchy skin. Cholestasis of pregnancy is a liver disease that results from high amounts of pregnancy hormones affecting the normal flow of bile in the gallbladder.
This condition occurs in the third trimester and can cause severe itching over the whole body. It’s often worse on the palms and soles of the feet and causes patients to feel miserable and be unable to sleep. Cholestasis of pregnancy also may be accompanied by jaundice (a yellow discoloration of the skin and eyes).
A simple blood test can verify if you have cholestasis of pregnancy, and oral medication may treat it. Delivery also cures it, so we may recommend inducing labor when you are closer to your due date.
Your body goes through immense changes during pregnancy. Most skin conditions are more annoying than anything. But tell your doctor about your symptoms to rule out anything serious – and to find potential relief!
Symptoms and what they look like
Some people develop skin rashes during pregnancy. The medical name for this is pregnancy dermatosis. Rashes can vary in severity and duration, depending on what causes them.
Hormone levels, stretching skin, genetics, and blood flow can all play a role.
This article discusses seven types of rash that can occur during pregnancy, including their symptoms and treatments. It also looks at how people can manage the symptoms at home.
Itchy skin is common during pregnancy, and some people also develop rashes. Some types of rash are specific to pregnancy, while others can occur at any time. However, some rashes may be more likely during pregnancy for some people due to the physical changes their body is going through.
In most cases, skin rashes are not serious and do not indicate a problem with the fetus. However, identifying the cause early on is important, as some rashes are a symptom of an underlying condition.
Some rashes that can occur during pregnancy include:
- heat rash
- hives
- atopic eruption of pregnancy
- pruritic urticarial papules and plaques of pregnancy (PUPPP) rash
- intrahepatic cholestasis of pregnancy (ICP)
- impetigo herpetiformis
- pemphigoid gestationis
Pregnancy can cause people to feel unusually warm because of increased blood supply to the skin. As a result, a person may find that they sweat more, which, in some cases, may lead to a heat rash.
As a result, a person may find that they sweat more, which, in some cases, may lead to a heat rash.
A heat rash, or prickly heat, causes an itchy patch of tiny blisters on the skin. Staying cool and dry can help heat rashes heal. If a person experiences heat rashes, they can try:
- wearing loose clothing made from natural fibers, such as cotton
- working and sleeping in cool, well-ventilated rooms
- changing out of wet clothing as soon as possible
- using cool water compresses on the rash
Hives look like raised bumps or welts on the skin. They itch and often occur due to an allergic reaction. However, there are other possible causes, including:
- heat
- scratching the skin
- stress
- pressure on the skin
Feeling hot and itchy is common during pregnancy and may lead to hives. In addition, the authors of a 2013 article suggest that hormonal changes may also induce hives.
A person can treat mild hives at home by cooling the skin. If the hives are severe or occur alongside swelling or difficulty breathing, a person should seek immediate medical help.
If the hives are severe or occur alongside swelling or difficulty breathing, a person should seek immediate medical help.
Atopic eruption of pregnancy is the most common pregnancy-specific skin disorder. The term groups several similar pregnancy rashes together. These include:
- atopic eczema
- prurigo of pregnancy
- pruritic folliculitis of pregnancy
Eczema is a very dry and itchy rash that appears red in lighter skin and gray or brown in darker skin. People who develop eczema during pregnancy may find that lesions flare up more than usual during the first and second trimesters.
Prurigo of pregnancy involves a rash that consists of papules, which are small bumps filled with fluid. Pruritic folliculitis causes papules that resemble pimples, or acne.
These conditions are uncomfortable but do not pose a risk to the pregnant person or the fetus. The rash will often disappear after delivery. Until then, a doctor may prescribe emollients, steroid creams, or antihistamines to reduce itching.
PUPPP rash affects about 1 in every 160 pregnancies. This condition is more common in people carrying multiple fetuses, as with twins or triplets.
A PUPPP rash develops when the skin stretches, damaging the layer of tissue underneath. This causes inflammation, which appears as a rash. A PUPPP rash sometimes begins in the second trimester but usually develops in the final 3 months of pregnancy. It goes away after giving birth.
A PUPPP rash is itchy and produces bumps on the skin, but it does not cause complications. A doctor may suggest using oral antihistamines, skin emollients, or steroid medication to treat it.
ICP, or obstetric cholestasis (OC), is a potentially serious liver condition that can occur during pregnancy. It causes severe itching that begins on the palms of the hands and the soles of the feet before spreading to other parts of the body. The itching may occur with or without a rash.
Sometimes, itching is the only symptom of ICP. Occasionally, a person may also develop jaundice, which causes the nails, skin, and eyes to become slightly yellow. ICP typically occurs in the third trimester.
ICP typically occurs in the third trimester.
The likelihood of developing ICP differs among ethnic groups. The condition affects 1% of females of Northern European ancestry. It is more common in people of Scandinavian or Araucanian Indian descent.
ICP can cause pregnancy complications, so early recognition, diagnosis, treatment, and close surveillance are very important. Severe itching in pregnancy is not normal, so a person should see a doctor immediately if this occurs.
Impetigo herpetiformis is a rare skin condition that appears during pregnancy, often in the last trimester. It is similar to pustular psoriasis, which causes severe skin inflammation.
This rash begins as lesions in the skin folds. These can then spread across the surface of the skin, covering large patches. The skin may crust or become infected. People can also experience:
- fever
- diarrhea
- dehydration
- rapid heartbeat
- seizures
Impetigo herpetiformis usually resolves after a person gives birth, but there is a risk of stillbirth. In rare cases, this condition is fatal. Doctors manage the condition and reduce these risks by prescribing systemic corticosteroids and antibiotics.
In rare cases, this condition is fatal. Doctors manage the condition and reduce these risks by prescribing systemic corticosteroids and antibiotics.
If a person experiences impetigo herpetiformis during one pregnancy, they may experience it again in future pregnancies.
Pemphigoid gestationis is a rare autoimmune disease that affects 1 in every 50,000 pregnancies. It causes an itchy, hive-like rash that begins around the navel and then spreads to other parts of the body. The rash may also include blisters.
This condition often begins in the second or third trimester. It can resolve during late pregnancy, but it often flares up before delivery. After pregnancy, the menstrual cycle or use of oral birth control pills may trigger the rash to return.
In 5–10% of pemphigoid gestationis cases, newborns are born with skin lesions. However, the exact risk that this condition poses to the fetus is unclear.
Mild rashes, such as hives, heat rash, or mild eczema, can improve with home management. A person can try the following methods to soothe irritated skin and ease itching:
A person can try the following methods to soothe irritated skin and ease itching:
- keeping the skin clean and dry using a gentle, unscented cleanser
- washing with cool or lukewarm water rather than hot or cold water
- moisturizing the skin using an unscented emollient, particularly after bathing, showering, or washing the hands
- avoiding products that may irritate the skin, such as harsh soaps or perfumes
- wearing loose, soft fabrics, such as cotton or linen
- using cool compresses, colloidal oatmeal baths, or calamine lotion to soothe itching
- avoiding scratching the skin, as this can make some skin conditions worse
Many forms of pregnancy rash are harmless, but it is always best to see a doctor so that they can identify the cause and confirm that a person does not need medical treatment. A doctor can also advise on the best way to care for skin conditions during pregnancy.
A person should seek immediate treatment if a rash:
- appears suddenly and spreads quickly
- causes severe itching or pain
- co-occurs with difficulty breathing and swelling
- is weeping pus or looks infected
A person should also see a doctor as soon as possible if they experience severe itchiness without a rash.
Rashes and itchy skin are common during pregnancy. Many rashes are harmless and may resolve after giving birth. However, in rare cases, rashes can be a sign of a more serious condition.
If a person does not know the cause of a pregnancy rash, they should see a doctor for a diagnosis.
Why does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Dermatoses of pregnancy
Cost: from 1500 rubles
Sign up
Pregnancy is a wonderful time for any woman, especially when it is a planned and desired event in the life of a couple. Unfortunately, due to various circumstances, pregnancy does not always occur naturally - in such cases, modern medicine offers various procedures for assisted reproductive technologies. This makes the woman's attitude to such a natural process even more reverent. And here, often, our skin can present surprises. A number of skin conditions can worsen during pregnancy. However, traditionally prescribed drugs have limitations for use in such a situation. And here it is important that the specialist has experience in treating such situations.
Our Clinic is unique in some way, since not only the chief physician, who has been a consultant at the D. O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
Now let's try to explain the causes and identify the most common skin diseases during pregnancy.
During pregnancy, the main cause of skin lesions is considered to be changes in the immune system of the pregnant woman. Pathological processes can be manifested by an exacerbation of chronic skin diseases or the appearance of specific pregnancy-associated dermatosis, the so-called "pregnancy dermatosis".
Changes on the skin are very diverse both in manifestations and in the mechanisms of development. Conventionally, they can be divided into 3 groups:
I. Pregnancy stigmas:
Chloasma is the most famous of them. As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Pregnancy melanosis - skin changes in the form of hyperpigmentation in the nipples, genitals, white line of the abdomen, also without subjective sensations or inflammation. After childbirth, these disorders disappear. Chloasma and melanosis usually do not require special treatment and spontaneously regress after delivery.
II. Skin diseases that are relatively often registered during pregnancy:
This group includes a variety of skin changes and diseases that often accompany pregnancy, as well as some common dermatoses, the course of which usually worsens during gestation. The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
This group includes: hyperhidrosis
- hypertrichosis
- palmoplantar telangiectasias
- erythema of the palms
- alopecia - hair loss
- onychodystrophy - changes in the nail plates
Most of these and other conditions, as a rule, disappear after childbirth. Their treatment, if necessary, is symptomatic.
The course and severity of symptoms of other skin diseases also change during pregnancy. These primarily include eczema, atopic dermatitis, psoriasis, lichen planus, acne, Dühring's herpetiformis. During pregnancy, they often worsen, and exacerbations are usually more pronounced, more severe than before gestation. Sometimes, on the contrary, during pregnancy, a remission occurs, which continues until childbirth, after which another exacerbation occurs. Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
Therefore, external symptomatic therapy becomes the leading method.
III. Actually dermatoses of pregnant women
The four skin diseases characteristic of pregnancy, gestational pemphigoid, polymorphic dermatosis of pregnancy, atopic dermatitis of pregnancy, and cholestasis of pregnancy can be distinguished by clinical presentation, histopathology, risk of fetal complications. Only gestational pemphigoid and intrahepatic cholestasis of pregnancy are associated with significant risk to the fetus. Because all of these dermatoses are characterized by pruritus, careful evaluation of any pruritic pregnancies is necessary.
Pregnancy pemphigoid , formerly known as herpes gestationis, is the rarest of the skin disorders of pregnancy and is an autoimmune disease. Clinically, it manifests itself in the form of papules and plaques, transforming into vesiculobullous elements, localized in the umbilical region with spread to the chest, back and limbs.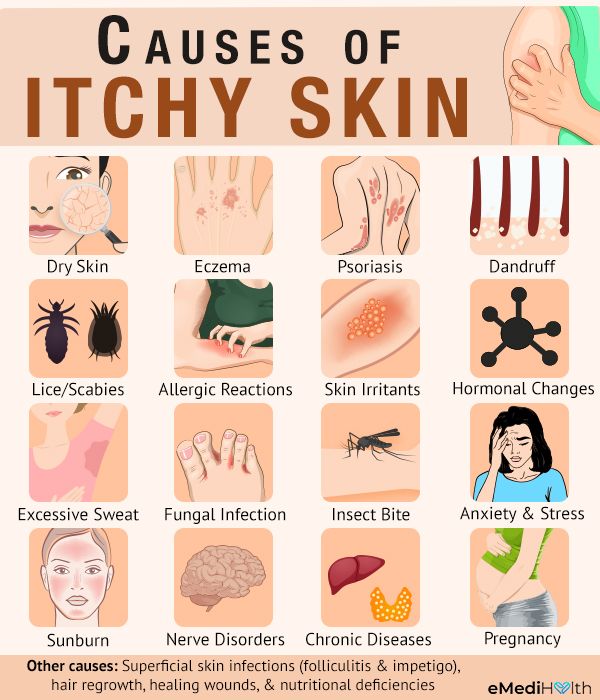 Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Polymorphic dermatosis of pregnancy (PEP) is a benign, pruritic inflammatory disease. It usually occurs at the end of the third trimester or immediately after delivery in the first pregnancy. Urticarial papules and plaques appear first on the abdomen and, unlike gestational pemphigoid, do not affect the umbilical region. The rash usually spreads to the thighs and buttocks, and can rarely be widespread. Eruptions with clear boundaries regress spontaneously within 4-6 weeks without treatment. Treatment for PEP is based on symptomatic relief with topical corticosteroids and antihistamines.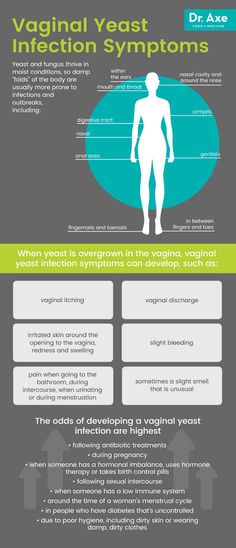 If the rash becomes generalized, a short course of systemic corticosteroids may be used.
If the rash becomes generalized, a short course of systemic corticosteroids may be used.
Atopic dermatitis of pregnancy (AEP) is the most common skin disorder in pregnancy. AEP is a benign disease characterized by an pruritic eczematous or papular rash. Two-thirds of AEP cases are characterized by eczematous skin changes localized to atopic areas of the body such as the neck and flexor surfaces of the extremities. The remaining cases are characterized by a papular rash in the abdomen and extremities. Lesions usually respond well to treatment and resolve spontaneously after delivery. However, AEP is more likely to recur in subsequent pregnancies. Dermatosis does not significantly affect the fetus, but there is an increased risk of developing atopic dermatitis in an infant.
Intrahepatic cholestasis of pregnancy (ICP) - characterized by itching with acute onset, which often begins on the palms and soles, and then generalizes. The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
Treatment is aimed at normalizing the level of bile acids in the blood serum in order to reduce the risk to the fetus and to control symptoms in the mother. Treatment with ursodeoxycholic acid (UDCA) is recommended. Other drugs that reduce itching may be used, such as antihistamines, dexamethasone. Treatment of pregnant women with dermatoses is very difficult, especially in the first trimester of pregnancy. If dermatosis is detected in a pregnant woman, it is necessary to jointly manage it by a dermatologist, an obstetrician-gynecologist. Treatment of dermatoses in pregnant women requires a differentiated approach to therapy, taking into account the duration of pregnancy, exacerbation of the disease and the prevalence of the process.