Complications in third trimester
The Third Trimester of Pregnancy: Complications
Overview
Weeks 28 through 40 bring the arrival of the third trimester. This exciting time is definitely the home stretch for expectant mothers, but it’s also a time when complications can occur. Just as the first two trimesters can bring their own challenges, so can the third.
Prenatal care is especially important in the third trimester because the types of complications that can arise at this time are more easily managed if detected early.
You’ll likely start visiting your obstetrician every other week from 28 to 36 weeks and then once per week until your little one arrives.
What is gestational diabetes?
As many as 9.2 percent of pregnant women in the United States have gestational diabetes.
Gestational diabetes occurs because the hormonal changes of pregnancy make it more difficult for your body to effectively use insulin. When insulin can’t do its job of lowering blood sugar to normal levels, the result is abnormally high glucose (blood sugar) levels.
Most women have no symptoms. While this condition isn’t usually dangerous for the mother, it poses several problems for the fetus. Specifically, macrosomia (excessive growth) of the fetus can increase the likelihood of cesarean delivery and the risk of birth injuries. When glucose levels are well-controlled, macrosomia is less likely.
At the beginning of the third trimester (between weeks 24 and 28), all women should get tested for gestational diabetes.
During the glucose tolerance test (also known as the screening glucose challenge test), you’ll consume a drink that contains a certain amount of glucose (sugar). At a specified time later, your doctor will test your blood sugar levels.
For the oral glucose tolerance test, you fast for at least eight hours and then have 100 milligrams of glucose, after which your blood sugar levels are checked. Those levels will be measured at one, two, and three hours after you drink the glucose.
The typical expected values are:
- after fasting, is lower than 95 milligrams per deciliter (mg/dL)
- after one hour, is lower than 180 mg/dL
- after two hours, is lower than 155 mg/dL
- after three hours, is lower than 140 mg/dL
If two of the three results are too high, a woman likely has gestational diabetes.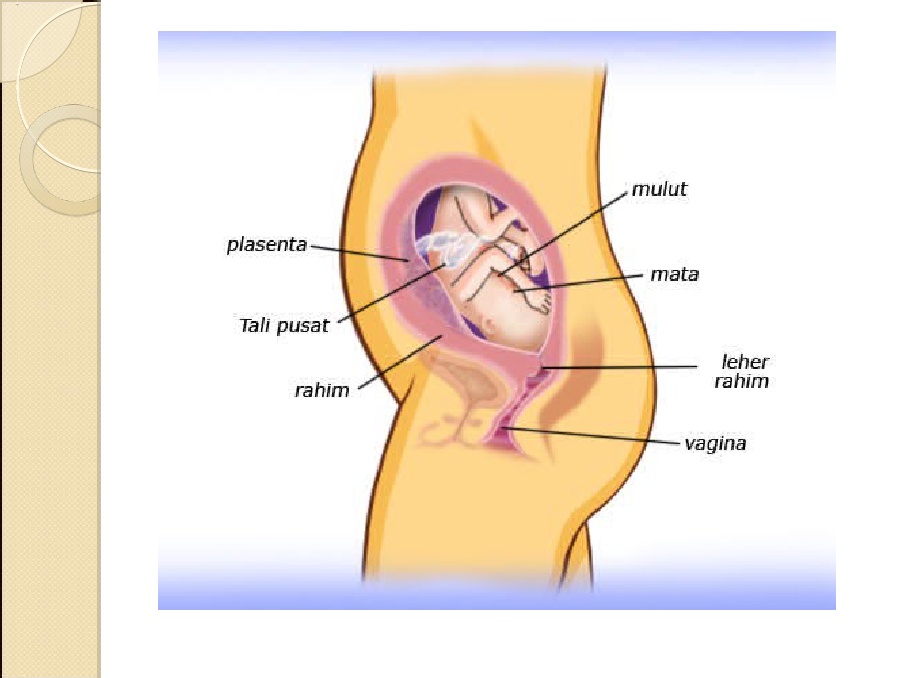
Treatment
Gestational diabetes can be treated with diet, lifestyle changes, and medicines, in some instances. Your doctor will recommend dietary changes, such as decreasing your carbohydrate intake and increasing fruits and veggies.
Adding low-impact exercise can also help. In some instances, your doctor may prescribe insulin.
The good news is that gestational diabetes usually goes away during the postpartum period. Blood sugars will be monitored after delivery to be sure.
However, a woman who has had gestational diabetes has a higher risk of having diabetes later in life than a woman who hasn’t had gestational diabetes.
The condition could also impact a woman’s chances of becoming pregnant again. A doctor will likely recommend checking a woman’s blood sugar levels to make sure they’re under control before she tries to have another baby.
What is preeclampsia?
Preeclampsia is a serious condition that makes regular prenatal visits even more important. The condition typically occurs after 20 weeks of pregnancy and can cause serious complications for mom and baby.
The condition typically occurs after 20 weeks of pregnancy and can cause serious complications for mom and baby.
Between 5 and 8 percent of women experience the condition. Teenagers, women 35 and older, and women pregnant with their first baby are at a higher risk. African American women are at higher risk.
Symptoms
Symptoms of the condition include high blood pressure, protein in the urine, sudden weight gain, and swelling of the hands and feet. Any of these symptoms warrant further assessment.
Prenatal visits are essential because screening done during these visits can detect symptoms like high blood pressure and increased protein in the urine. If left untreated, preeclampsia can lead to eclampsia (seizures), kidney failure, and, sometimes even death in the mother and fetus.
The first sign that your doctor usually sees is high blood pressure during a routine prenatal visit. Also, protein might be detected in your urine during a urinalysis. Some women may gain more weight than expected.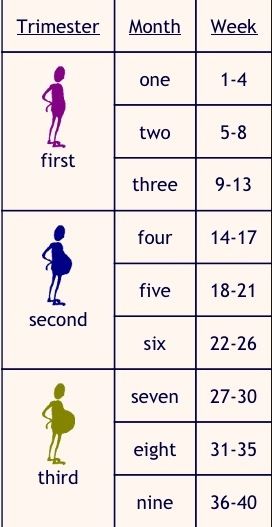 Others experience headaches, vision changes, and upper abdominal pain.
Others experience headaches, vision changes, and upper abdominal pain.
Women should never ignore symptoms of preeclampsia.
Seek emergency medical treatment if you have rapid swelling in the feet and legs, hands, or face. Other emergency symptoms include:
- headache that doesn’t go away with medication
- loss of vision
- “floaters” in your vision
- severe pain on your right side or in your stomach area
- easy bruising
- decreased amounts of urine
- shortness of breath
These signs may suggest severe preeclampsia.
Blood tests, such as liver and kidney function tests and blood-clotting tests, may confirm the diagnosis and can detect severe disease.
Treatment
How your doctor treats preeclampsia depends on its severity and how far along in the pregnancy you are. Delivering your baby may be necessary to protect you and your little one.
Your doctor will discuss several considerations with you depending on your weeks of gestation.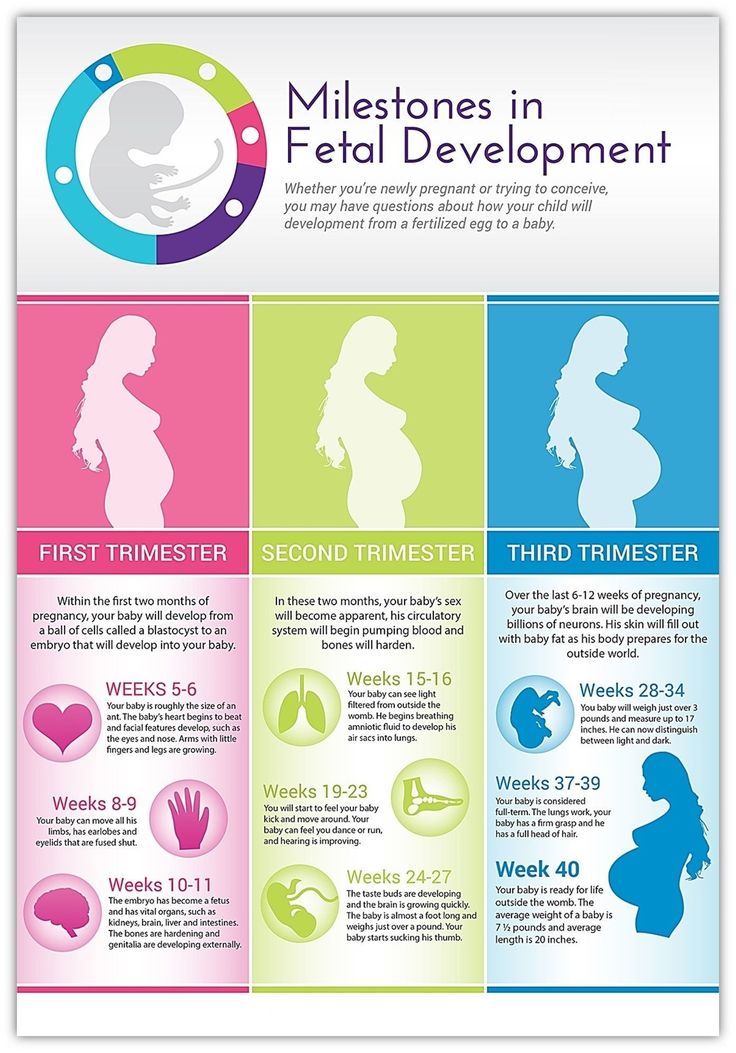 If you are close your due date it may be safest to deliver the baby.
If you are close your due date it may be safest to deliver the baby.
You may have to stay at the hospital for observation and to manage your blood pressure until the baby is old enough for delivery. If your baby is younger than 34 weeks, you will probably be given medication to speed up the baby’s lung development.
Preeclampsia can continue past delivery, though for most women symptoms start to diminish after giving birth. However, sometimes blood pressure medication is prescribed for a short time after delivery.
Diuretics may be prescribed to treat pulmonary edema (fluid in the lungs). Magnesium sulfate given before, during, and after the delivery can help to reduce seizure risks. A woman who has had preeclampsia symptoms before delivery will continue to be monitored after the baby is born.
If you’ve had preeclampsia, you’re at greater risk for having the condition with future pregnancies. Always talk with your doctor about how you can lower your risk.
Cause and prevention
Despite years of scientific study, the true cause of preeclampsia isn’t known, nor is there any effective prevention. The treatment, however, has been known for many decades and that is delivery of the baby.
The treatment, however, has been known for many decades and that is delivery of the baby.
The problems associated with preeclampsia can continue even after delivery, but this is unusual. Timely diagnosis and delivery is the best way to avoid serious problems for mother and baby.
What is preterm labor?
Preterm labor occurs when you start having contractions that cause cervical changes before you’re 37 weeks pregnant.
Some women are at greater risk for preterm labor, including those who:
- are pregnant with multiples (twins or more)
- have an infection of the amniotic sac (amnionitis)
- have excess amniotic fluid (polyhydramnios)
- have had a previous preterm birth
Symptoms
Signs and symptoms of preterm labor can be subtle. An expectant mom may pass them off as part of pregnancy. Symptoms include:
- diarrhea
- frequent urination
- lower back pain
- tightness in the lower abdomen
- vaginal discharge
- vaginal pressure
Of course, some women may experience more severe labor symptoms.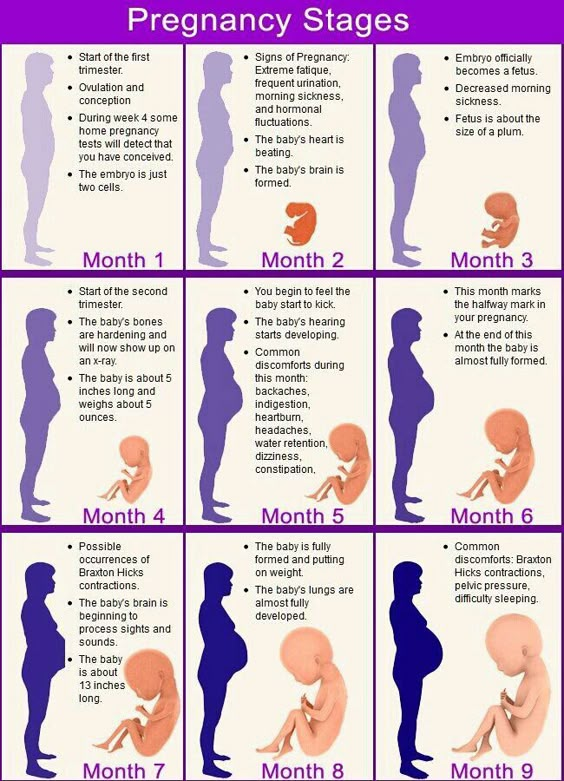 These include regular, painful contractions, leaking of fluid from the vagina, or vaginal bleeding.
These include regular, painful contractions, leaking of fluid from the vagina, or vaginal bleeding.
Treatment
Infants born prematurely are at risk for health problems because their bodies haven’t had time to fully develop. One of the greatest concerns is lung development because the lungs develop well into the third trimester. The younger a baby is when born, the greater the possible complications.
Doctors don’t know the exact cause of premature labor. However, it’s important for you to receive care as soon as possible. Sometimes medicines like magnesium sulfate can help stop preterm labor and delay delivery.
Each day your pregnancy is prolonged increases your chances for a healthy baby.
Doctors often give a steroid medication to moms whose preterm labor starts before 34 weeks. This helps your baby’s lungs mature and reduces the severity of lung disease if your labor can’t be stopped.
Steroid medication has its peak effect within two days, so it’s best to prevent delivery for at least two days, if possible.
All women with preterm labor who haven’t been tested for the presence of group B streptococcus should receive antibiotics (penicillin G, ampicillin, or an alternative for those who are allergic to penicillin) until delivery.
If preterm labor begins after 36 weeks, the baby is usually delivered since the risk of lung disease from prematurity is very low.
Premature rupture of membranes (PROM)
Rupture of membranes is a normal part of giving birth. It’s the medical term for saying your “water has broken.” It means that the amniotic sac that surrounds your baby has broken, allowing the amniotic fluid to flow out.
While it’s normal for the sac to break during labor, if it happens too early, it can cause serious complications. This is called preterm / premature rupture of membranes (PROM).
Although the cause of PROM isn’t always clear, sometimes an infection of the amniotic membranes is the cause and other factors, such as genetics, come into play.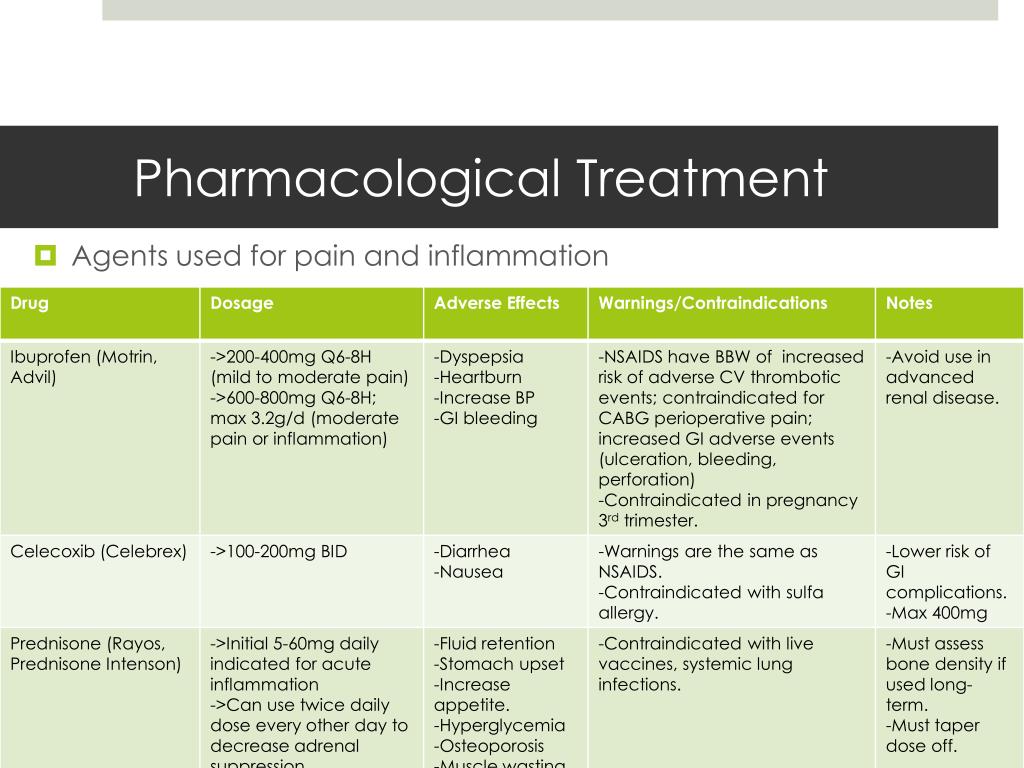
Treatment
Treatment for PROM varies. Women are often hospitalized and given antibiotics, steroids, and drugs to stop labor (tocolytics).
When PROM occurs at 34 weeks or more, some doctors might recommend delivering the baby. At that time, the risks of prematurity are less than the infection risks. If there are signs of infection, labor must be induced to avoid serious complications.
Occasionally, a woman with PROM experiences resealing of the membranes. In these rare cases, a woman can continue her pregnancy to near term, although still under close observation.
The risks associated with prematurity decrease significantly as the fetus nears term. If PROM occurs in the 32- to 34-week range and the remaining amniotic fluid shows that the fetus’ lungs have matured enough, the doctor may discuss delivering the baby in some cases.
With improved intensive care nursery services, many preterm infants born in the third trimester (after 28 weeks) do very well.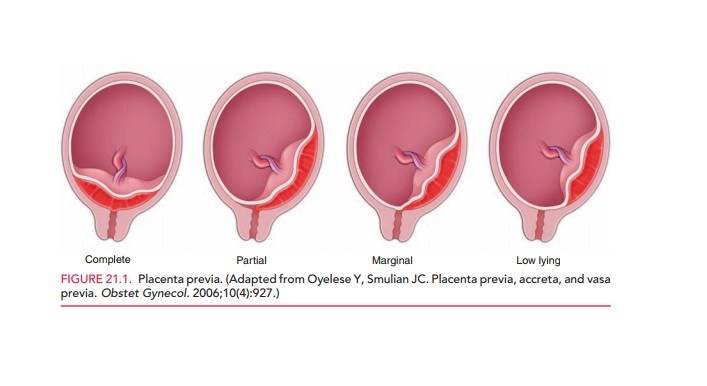
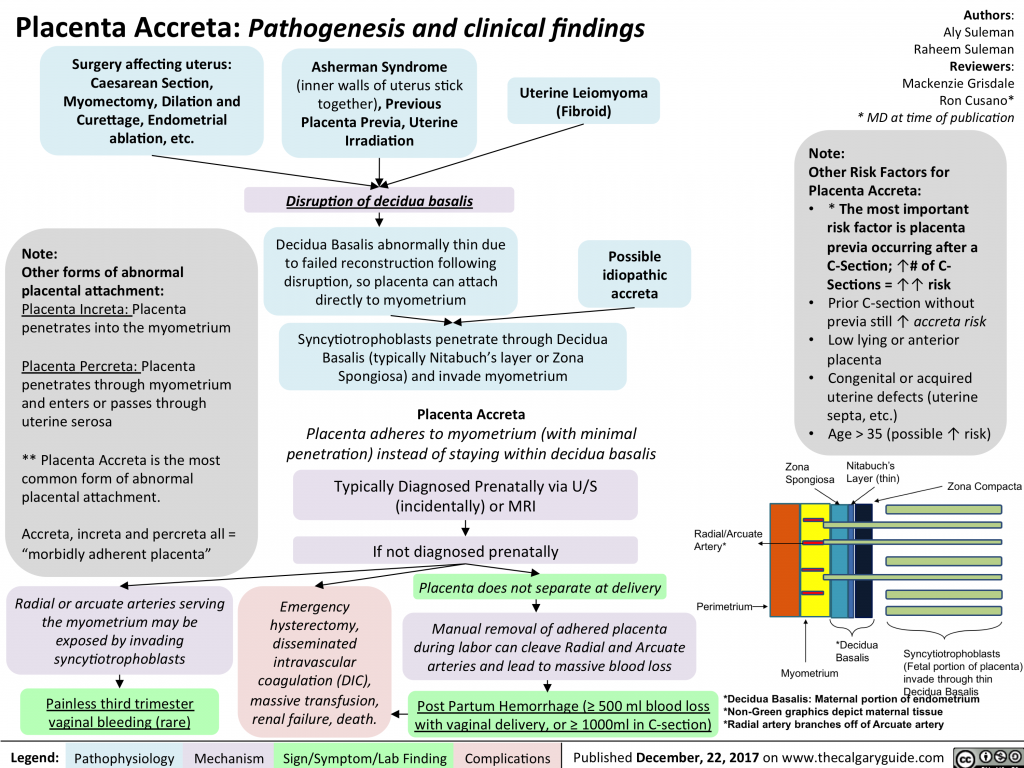
Problems with the placenta (previa and abruption)
Bleeding in the third trimester may have several causes. The more serious causes are placenta previa and placental abruption.
Placenta previa
The placenta is the organ that nourishes your baby while you’re pregnant. Usually, the placenta is delivered after your baby. However, women with placenta previa have a placenta that comes first and blocks the opening to the cervix.
Doctors don’t know the exact cause of this condition. Women who’ve had a previous cesarean delivery or uterine surgery are at greater risk. Women who smoke or have a larger-than-normal placenta are also at greater risk.
Placenta previa increases risk of bleeding before and during delivery. This can be life-threatening.
A common symptom of placenta previa is bright red, sudden, profuse, and painless vaginal bleeding, which usually occurs after the 28th week of pregnancy. Doctors usually use an ultrasound to identify placenta previa.
Treatment depends on whether the fetus is preterm and the amount of bleeding. If labor is unstoppable, the baby is in distress, or there is life-threatening hemorrhage, immediate cesarean delivery is indicated no matter the fetus’ age.
If the bleeding stops or isn’t too heavy, delivery can often be avoided. This allows more time for the fetus to grow if the fetus is near-term. A doctor usually recommends cesarean delivery.
Thanks to modern obstetric care, ultrasound diagnosis, and the availability of blood transfusion, if needed, women with placenta previa and their infants usually do well.
Placental abruption
Placental abruption is a rare condition in which the placenta separates from the uterus prior to labor. It occurs in up to 1 percent of pregnancies. Placental abruption can result in fetal death and can cause serious bleeding and shock in the mother.
Risk factors for placental abruption include:
- advanced maternal age
- cocaine use
- diabetes
- heavy alcohol use
- high blood pressure
- pregnancy with multiples
- preterm premature rupture of the membranes
- prior pregnancies
- short umbilical cord
- smoking
- trauma to the stomach
- uterine distention due to excess amniotic fluid
Placental abruption doesn’t always cause symptoms. But some women experience heavy vaginal bleeding, severe stomach pain, and strong contractions. Some women have no bleeding.
But some women experience heavy vaginal bleeding, severe stomach pain, and strong contractions. Some women have no bleeding.
A doctor can evaluate a woman’s symptoms and the baby’s heartbeat to identify potential fetal distress. In many instances, rapid cesarean delivery is necessary. If a woman loses excess blood, she may also need a blood transfusion.
Intrauterine growth restriction (IUGR)
Occasionally a baby won’t grow as much as they’re expected to at a certain stage in a woman’s pregnancy. This is known as intrauterine growth restriction (IUGR). Not all small babies have IUGR — sometimes their size can be attributed to the smaller size of their parents.
IUGR can result in symmetrical or asymmetrical growth. Babies with asymmetrical growth often have a normal-sized head with a smaller-sized body.
Maternal factors that can lead to IUGR include:
- anemia
- chronic renal disease
- placenta previa
- placental infarction
- severe diabetes
- severe malnutrition
Fetuses with IUGR may be less able to tolerate the stress of labor than infants of normal size. IUGR babies also tend to have less body fat and more trouble maintaining their body temperature and glucose levels (blood sugar) after birth.
IUGR babies also tend to have less body fat and more trouble maintaining their body temperature and glucose levels (blood sugar) after birth.
If growth problems are suspected, a doctor can use an ultrasound to measure the fetus and calculate an estimated fetal weight. The estimate can be compared with the range of normal weights for fetuses of similar age.
To determine whether the fetus is small for gestational age or growth restricted, a series of ultrasounds is done over to time to document weight gain or lack thereof.
A specialized ultrasound monitoring umbilical blood flow can also determine IUGR. Amniocentesis may be used to check for chromosomal problems or infection. Monitoring the fetal heart pattern and measurement of the amniotic fluid are common.
If a baby stops growing in the womb, a doctor may recommend induction or cesarean delivery. Luckily, most growth-restricted babies develop normally after birth. They tend to catch up in growth by two years old.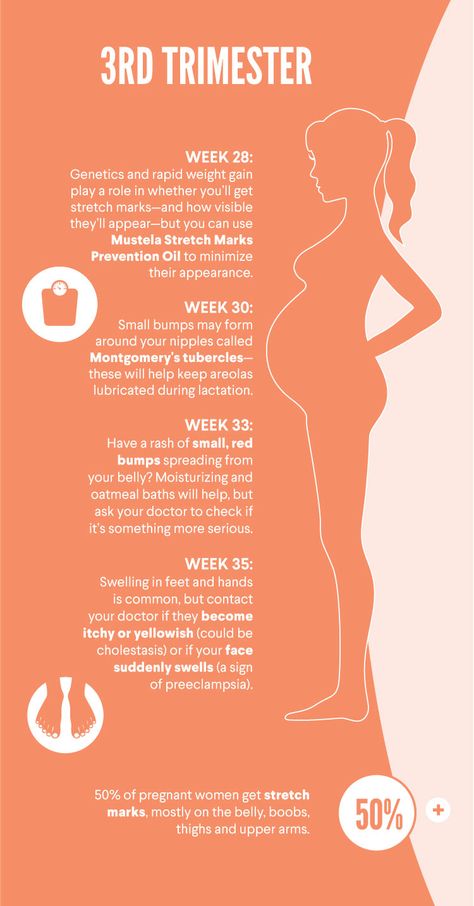
Post-term pregnancy
About 7 percent of women deliver at 42 weeks or later. Any pregnancy lasting longer than 42 weeks is considered post-term or post-dates. The cause of post-term pregnancy is unclear, although hormonal and hereditary factors are suspected.
Sometimes, a woman’s due date isn’t calculated correctly. Some women have irregular or long menstrual cycles that make ovulation harder to predict. Early in pregnancy, an ultrasound can help to confirm or adjust the due date.
Post-term pregnancy isn’t generally dangerous to the mother’s health. The concern is for the fetus. The placenta is an organ that is designed to work for about 40 weeks. It provides oxygen and nutrition for the growing fetus.
After 41 weeks of pregnancy, the placenta is less likely to work well, and this may result in decreased amniotic fluid around the fetus (oligohydramnios).
This condition can cause compression of the umbilical cord and decrease oxygen supply to the fetus. This may be reflected on the fetal heart monitor in a pattern called late decelerations. There is a risk of sudden fetal death when the pregnancy is post-term.
This may be reflected on the fetal heart monitor in a pattern called late decelerations. There is a risk of sudden fetal death when the pregnancy is post-term.
Once a woman reaches 41 weeks of pregnancy, she usually has fetal heart rate monitoring and a measurement of the amniotic fluid. If the testing shows low fluid levels or abnormal fetal heart rate patterns, labor is induced. Otherwise, spontaneous labor is awaited until no more than 42 to 43 weeks, after which it’s induced.
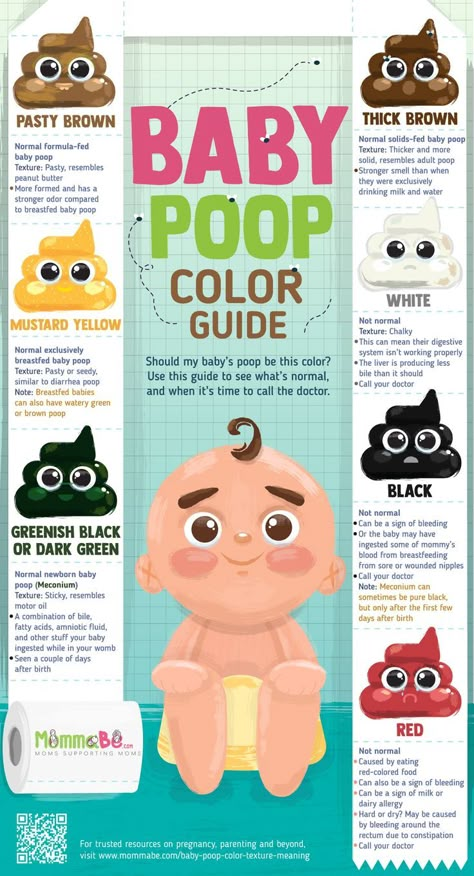
Meconium aspiration syndrome
The other risk is meconium. Meconium is a fetus’ bowel movement. It’s more common when the pregnancy is post-term. Most fetuses that have a bowel movement inside the uterus have no problems.
However, a stressed fetus can inhale the meconium, causing a very serious type of pneumonia and, rarely, death. For these reasons, doctors work to clear a baby’s airway as much as possible if a baby’s amniotic fluid is meconium-stained.
Malpresentation (breech, transverse lie)
As a woman approaches her ninth month of pregnancy, the fetus generally settles into a head-down position inside the uterus.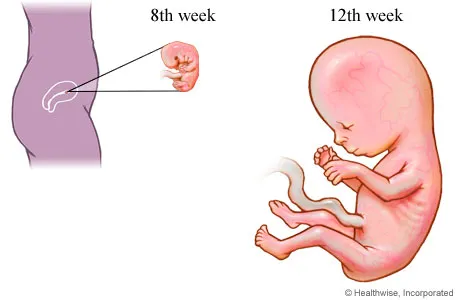 This is known as vertex or cephalic presentation.
This is known as vertex or cephalic presentation.
The fetus will be bottom or feet first (known as breech presentation) in about 3 to 4 percent of full-term pregnancies.
Occasionally, the fetus will be lying sideways (transverse presentation).
The safest way for a baby to be born is head first or in the vertex presentation. If the fetus is breech or transverse, the best way to avoid problems with delivery and prevent a cesarean is to try to turn (or vert) the fetus to vertex presentation (head down). This is known as external cephalic version. It’s usually attempted at 37 to 38 weeks, if the malpresentation is known.
External cephalic version is somewhat like a firm massage of the abdomen and can be uncomfortable. It’s usually a safe procedure, but some rare complications include placental abruption and fetal distress, necessitating emergency cesarean delivery.
If the fetus is successfully turned, spontaneous labor can be awaited or labor can be induced. If it’s unsuccessful, some doctors wait a week and try again.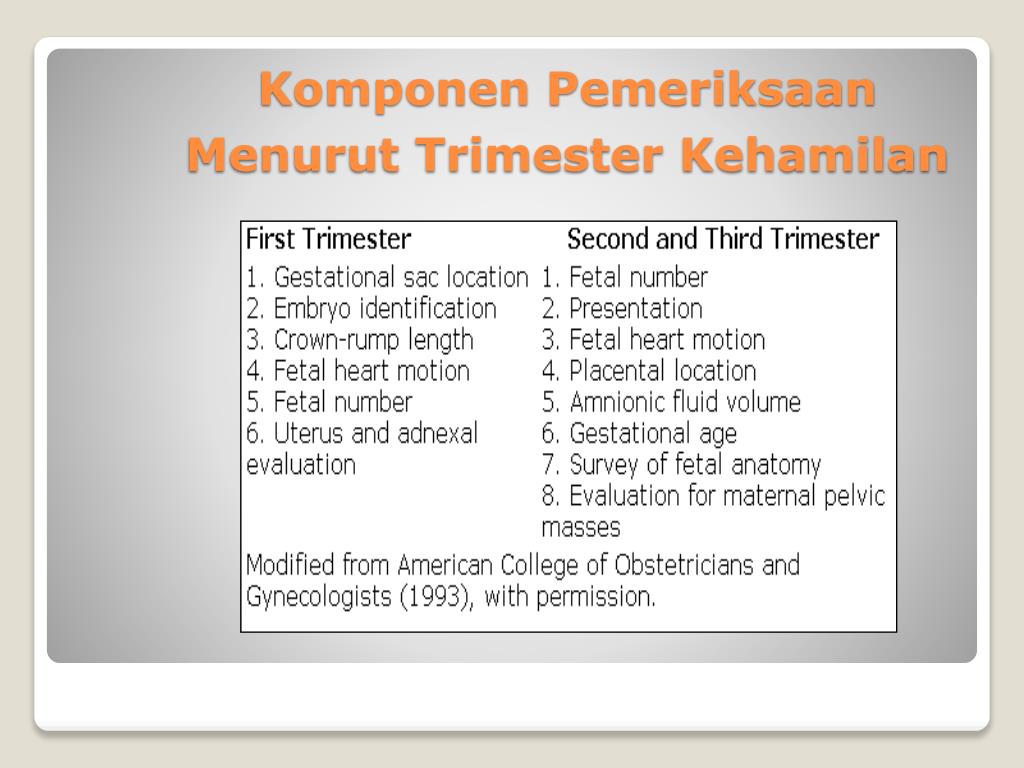 If unsuccessful after reattempts, you and your doctor will decide the best type of delivery, vaginal or cesarean.
If unsuccessful after reattempts, you and your doctor will decide the best type of delivery, vaginal or cesarean.
Measurement of the bones of the mother’s birth canal and ultrasound to estimate fetal weight are often obtained in preparation for breech vaginal deliveries. Transverse fetuses are delivered by cesarean.
The Third Trimester of Pregnancy: Complications
Overview
Weeks 28 through 40 bring the arrival of the third trimester. This exciting time is definitely the home stretch for expectant mothers, but it’s also a time when complications can occur. Just as the first two trimesters can bring their own challenges, so can the third.
Prenatal care is especially important in the third trimester because the types of complications that can arise at this time are more easily managed if detected early.
You’ll likely start visiting your obstetrician every other week from 28 to 36 weeks and then once per week until your little one arrives.
What is gestational diabetes?
As many as 9.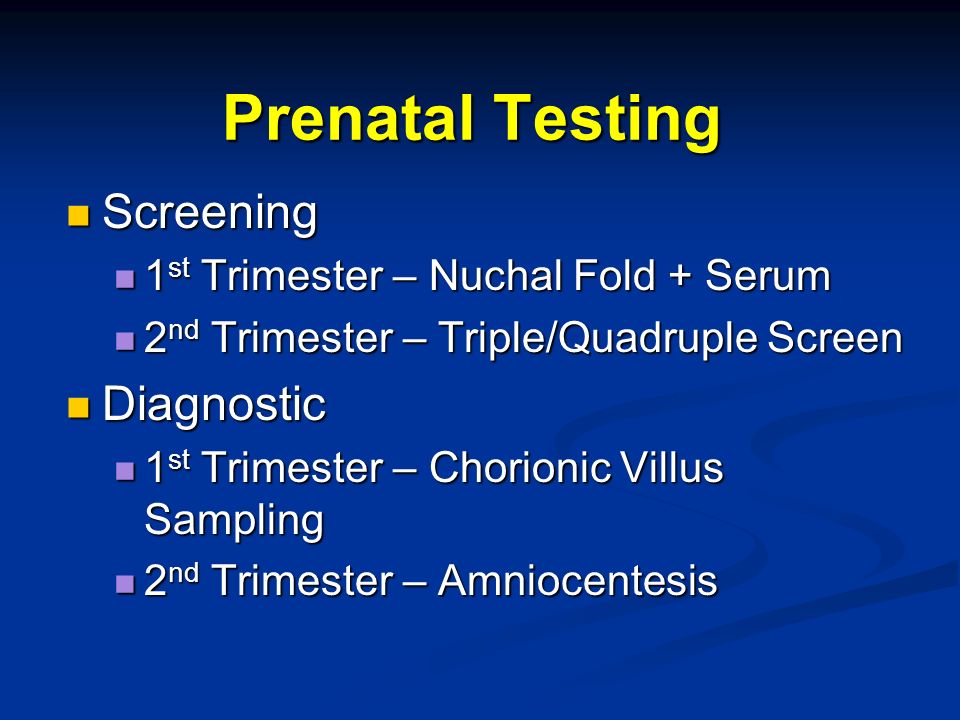 2 percent of pregnant women in the United States have gestational diabetes.
2 percent of pregnant women in the United States have gestational diabetes.
Gestational diabetes occurs because the hormonal changes of pregnancy make it more difficult for your body to effectively use insulin. When insulin can’t do its job of lowering blood sugar to normal levels, the result is abnormally high glucose (blood sugar) levels.
Most women have no symptoms. While this condition isn’t usually dangerous for the mother, it poses several problems for the fetus. Specifically, macrosomia (excessive growth) of the fetus can increase the likelihood of cesarean delivery and the risk of birth injuries. When glucose levels are well-controlled, macrosomia is less likely.
At the beginning of the third trimester (between weeks 24 and 28), all women should get tested for gestational diabetes.
During the glucose tolerance test (also known as the screening glucose challenge test), you’ll consume a drink that contains a certain amount of glucose (sugar). At a specified time later, your doctor will test your blood sugar levels.
For the oral glucose tolerance test, you fast for at least eight hours and then have 100 milligrams of glucose, after which your blood sugar levels are checked. Those levels will be measured at one, two, and three hours after you drink the glucose.
The typical expected values are:
- after fasting, is lower than 95 milligrams per deciliter (mg/dL)
- after one hour, is lower than 180 mg/dL
- after two hours, is lower than 155 mg/dL
- after three hours, is lower than 140 mg/dL
If two of the three results are too high, a woman likely has gestational diabetes.
Treatment
Gestational diabetes can be treated with diet, lifestyle changes, and medicines, in some instances. Your doctor will recommend dietary changes, such as decreasing your carbohydrate intake and increasing fruits and veggies.
Adding low-impact exercise can also help. In some instances, your doctor may prescribe insulin.
The good news is that gestational diabetes usually goes away during the postpartum period.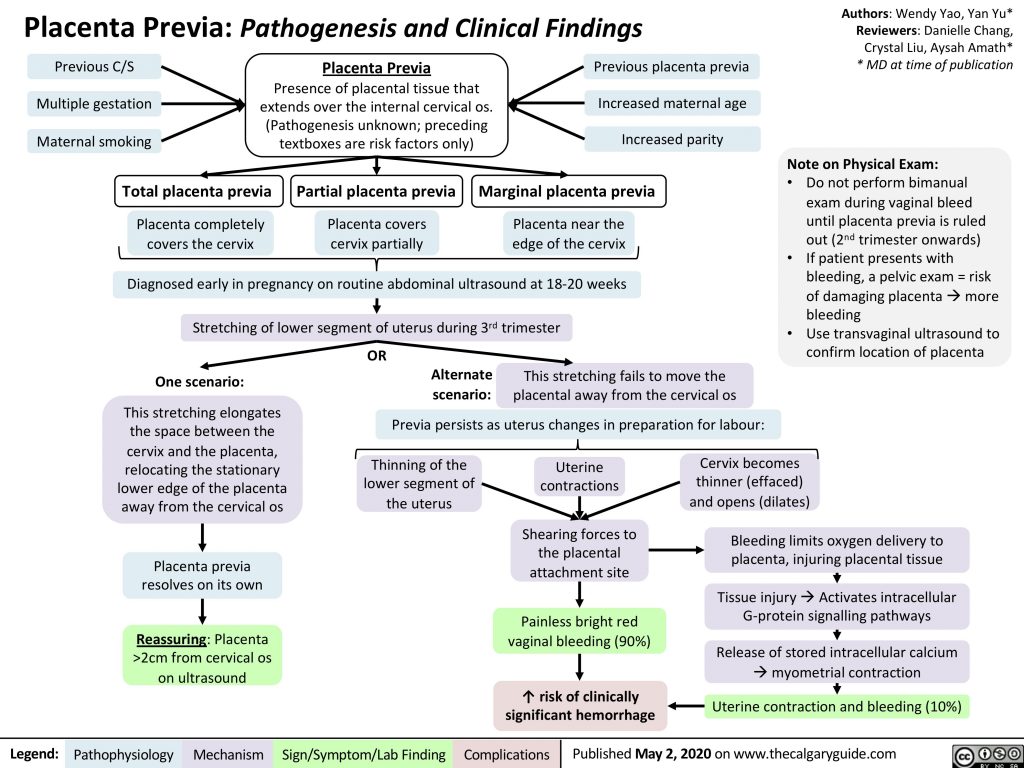 Blood sugars will be monitored after delivery to be sure.
Blood sugars will be monitored after delivery to be sure.
However, a woman who has had gestational diabetes has a higher risk of having diabetes later in life than a woman who hasn’t had gestational diabetes.
The condition could also impact a woman’s chances of becoming pregnant again. A doctor will likely recommend checking a woman’s blood sugar levels to make sure they’re under control before she tries to have another baby.
What is preeclampsia?
Preeclampsia is a serious condition that makes regular prenatal visits even more important. The condition typically occurs after 20 weeks of pregnancy and can cause serious complications for mom and baby.
Between 5 and 8 percent of women experience the condition. Teenagers, women 35 and older, and women pregnant with their first baby are at a higher risk. African American women are at higher risk.
Symptoms
Symptoms of the condition include high blood pressure, protein in the urine, sudden weight gain, and swelling of the hands and feet.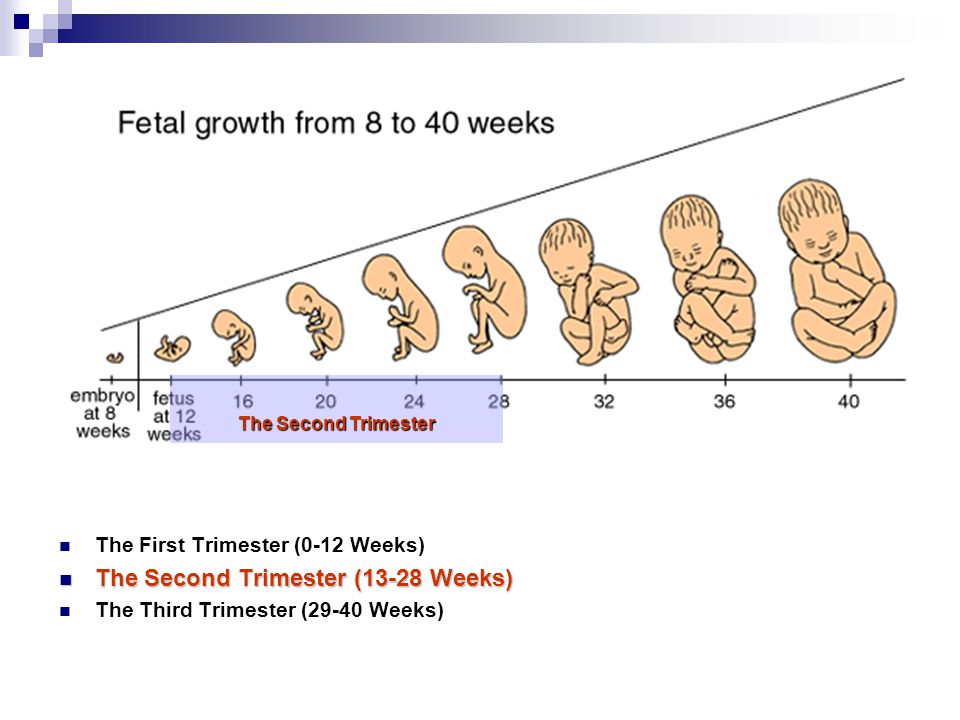 Any of these symptoms warrant further assessment.
Any of these symptoms warrant further assessment.
Prenatal visits are essential because screening done during these visits can detect symptoms like high blood pressure and increased protein in the urine. If left untreated, preeclampsia can lead to eclampsia (seizures), kidney failure, and, sometimes even death in the mother and fetus.
The first sign that your doctor usually sees is high blood pressure during a routine prenatal visit. Also, protein might be detected in your urine during a urinalysis. Some women may gain more weight than expected. Others experience headaches, vision changes, and upper abdominal pain.
Women should never ignore symptoms of preeclampsia.
Seek emergency medical treatment if you have rapid swelling in the feet and legs, hands, or face. Other emergency symptoms include:
- headache that doesn’t go away with medication
- loss of vision
- “floaters” in your vision
- severe pain on your right side or in your stomach area
- easy bruising
- decreased amounts of urine
- shortness of breath
These signs may suggest severe preeclampsia.
Blood tests, such as liver and kidney function tests and blood-clotting tests, may confirm the diagnosis and can detect severe disease.
Treatment
How your doctor treats preeclampsia depends on its severity and how far along in the pregnancy you are. Delivering your baby may be necessary to protect you and your little one.
Your doctor will discuss several considerations with you depending on your weeks of gestation. If you are close your due date it may be safest to deliver the baby.
You may have to stay at the hospital for observation and to manage your blood pressure until the baby is old enough for delivery. If your baby is younger than 34 weeks, you will probably be given medication to speed up the baby’s lung development.
Preeclampsia can continue past delivery, though for most women symptoms start to diminish after giving birth. However, sometimes blood pressure medication is prescribed for a short time after delivery.
Diuretics may be prescribed to treat pulmonary edema (fluid in the lungs). Magnesium sulfate given before, during, and after the delivery can help to reduce seizure risks. A woman who has had preeclampsia symptoms before delivery will continue to be monitored after the baby is born.
Magnesium sulfate given before, during, and after the delivery can help to reduce seizure risks. A woman who has had preeclampsia symptoms before delivery will continue to be monitored after the baby is born.
If you’ve had preeclampsia, you’re at greater risk for having the condition with future pregnancies. Always talk with your doctor about how you can lower your risk.
Cause and prevention
Despite years of scientific study, the true cause of preeclampsia isn’t known, nor is there any effective prevention. The treatment, however, has been known for many decades and that is delivery of the baby.
The problems associated with preeclampsia can continue even after delivery, but this is unusual. Timely diagnosis and delivery is the best way to avoid serious problems for mother and baby.
What is preterm labor?
Preterm labor occurs when you start having contractions that cause cervical changes before you’re 37 weeks pregnant.
Some women are at greater risk for preterm labor, including those who:
- are pregnant with multiples (twins or more)
- have an infection of the amniotic sac (amnionitis)
- have excess amniotic fluid (polyhydramnios)
- have had a previous preterm birth
Symptoms
Signs and symptoms of preterm labor can be subtle.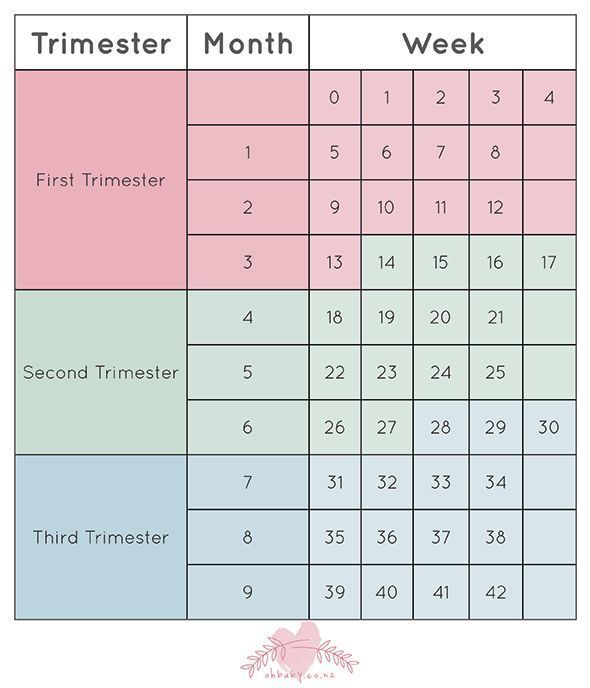 An expectant mom may pass them off as part of pregnancy. Symptoms include:
An expectant mom may pass them off as part of pregnancy. Symptoms include:
- diarrhea
- frequent urination
- lower back pain
- tightness in the lower abdomen
- vaginal discharge
- vaginal pressure
Of course, some women may experience more severe labor symptoms. These include regular, painful contractions, leaking of fluid from the vagina, or vaginal bleeding.
Treatment
Infants born prematurely are at risk for health problems because their bodies haven’t had time to fully develop. One of the greatest concerns is lung development because the lungs develop well into the third trimester. The younger a baby is when born, the greater the possible complications.
Doctors don’t know the exact cause of premature labor. However, it’s important for you to receive care as soon as possible. Sometimes medicines like magnesium sulfate can help stop preterm labor and delay delivery.
Each day your pregnancy is prolonged increases your chances for a healthy baby.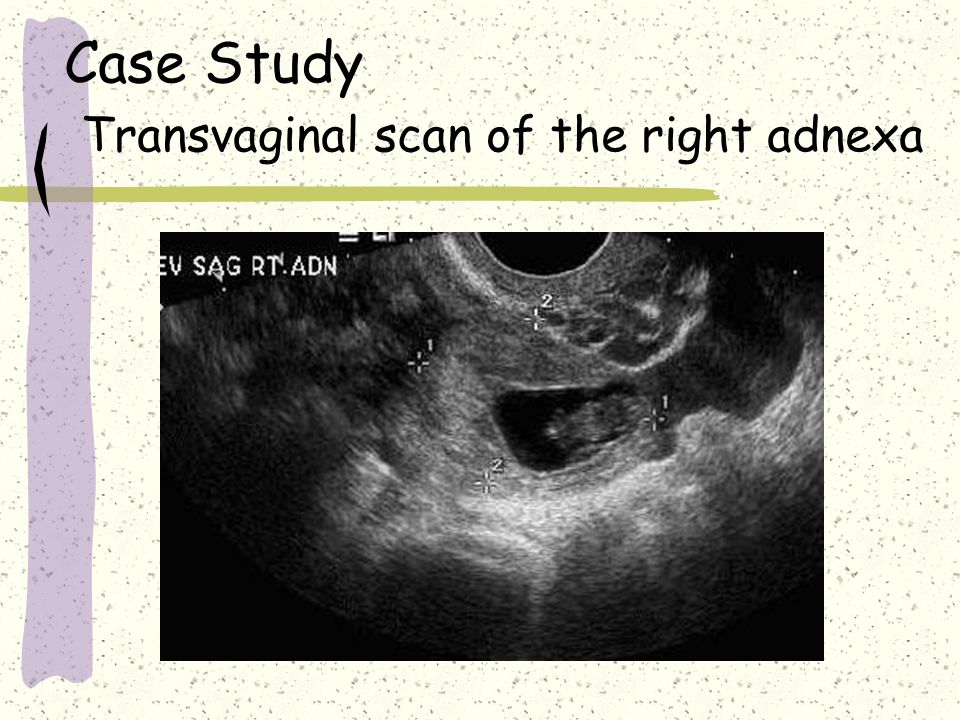
Doctors often give a steroid medication to moms whose preterm labor starts before 34 weeks. This helps your baby’s lungs mature and reduces the severity of lung disease if your labor can’t be stopped.
Steroid medication has its peak effect within two days, so it’s best to prevent delivery for at least two days, if possible.
All women with preterm labor who haven’t been tested for the presence of group B streptococcus should receive antibiotics (penicillin G, ampicillin, or an alternative for those who are allergic to penicillin) until delivery.
If preterm labor begins after 36 weeks, the baby is usually delivered since the risk of lung disease from prematurity is very low.
Premature rupture of membranes (PROM)
Rupture of membranes is a normal part of giving birth. It’s the medical term for saying your “water has broken.” It means that the amniotic sac that surrounds your baby has broken, allowing the amniotic fluid to flow out.
While it’s normal for the sac to break during labor, if it happens too early, it can cause serious complications.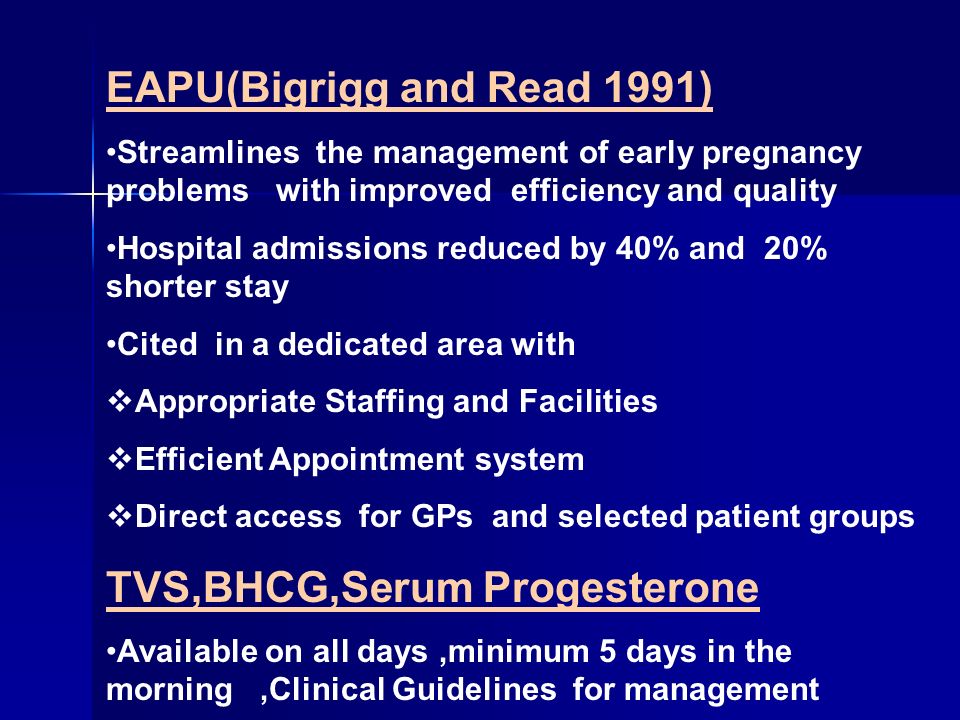 This is called preterm / premature rupture of membranes (PROM).
This is called preterm / premature rupture of membranes (PROM).
Although the cause of PROM isn’t always clear, sometimes an infection of the amniotic membranes is the cause and other factors, such as genetics, come into play.
Treatment
Treatment for PROM varies. Women are often hospitalized and given antibiotics, steroids, and drugs to stop labor (tocolytics).
When PROM occurs at 34 weeks or more, some doctors might recommend delivering the baby. At that time, the risks of prematurity are less than the infection risks. If there are signs of infection, labor must be induced to avoid serious complications.
Occasionally, a woman with PROM experiences resealing of the membranes. In these rare cases, a woman can continue her pregnancy to near term, although still under close observation.
The risks associated with prematurity decrease significantly as the fetus nears term. If PROM occurs in the 32- to 34-week range and the remaining amniotic fluid shows that the fetus’ lungs have matured enough, the doctor may discuss delivering the baby in some cases.
With improved intensive care nursery services, many preterm infants born in the third trimester (after 28 weeks) do very well.
Problems with the placenta (previa and abruption)
Bleeding in the third trimester may have several causes. The more serious causes are placenta previa and placental abruption.
Placenta previa
The placenta is the organ that nourishes your baby while you’re pregnant. Usually, the placenta is delivered after your baby. However, women with placenta previa have a placenta that comes first and blocks the opening to the cervix.
Doctors don’t know the exact cause of this condition. Women who’ve had a previous cesarean delivery or uterine surgery are at greater risk. Women who smoke or have a larger-than-normal placenta are also at greater risk.
Placenta previa increases risk of bleeding before and during delivery. This can be life-threatening.
A common symptom of placenta previa is bright red, sudden, profuse, and painless vaginal bleeding, which usually occurs after the 28th week of pregnancy. Doctors usually use an ultrasound to identify placenta previa.
Doctors usually use an ultrasound to identify placenta previa.
Treatment depends on whether the fetus is preterm and the amount of bleeding. If labor is unstoppable, the baby is in distress, or there is life-threatening hemorrhage, immediate cesarean delivery is indicated no matter the fetus’ age.
If the bleeding stops or isn’t too heavy, delivery can often be avoided. This allows more time for the fetus to grow if the fetus is near-term. A doctor usually recommends cesarean delivery.
Thanks to modern obstetric care, ultrasound diagnosis, and the availability of blood transfusion, if needed, women with placenta previa and their infants usually do well.
Placental abruption
Placental abruption is a rare condition in which the placenta separates from the uterus prior to labor. It occurs in up to 1 percent of pregnancies. Placental abruption can result in fetal death and can cause serious bleeding and shock in the mother.
Risk factors for placental abruption include:
- advanced maternal age
- cocaine use
- diabetes
- heavy alcohol use
- high blood pressure
- pregnancy with multiples
- preterm premature rupture of the membranes
- prior pregnancies
- short umbilical cord
- smoking
- trauma to the stomach
- uterine distention due to excess amniotic fluid
Placental abruption doesn’t always cause symptoms.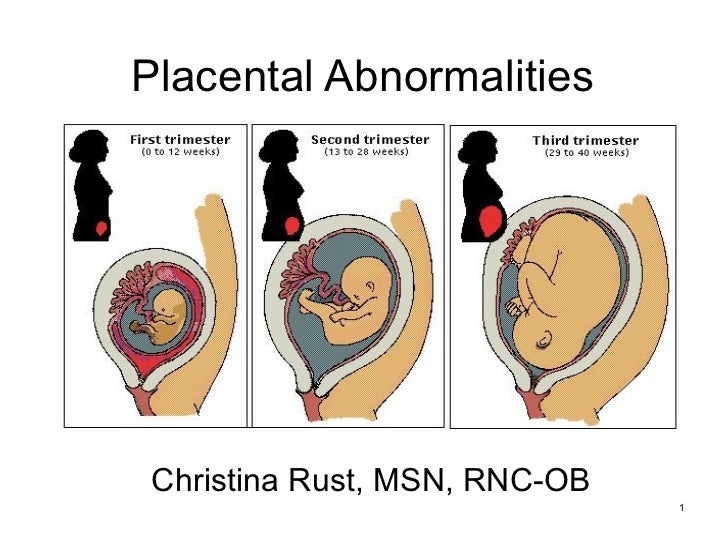 But some women experience heavy vaginal bleeding, severe stomach pain, and strong contractions. Some women have no bleeding.
But some women experience heavy vaginal bleeding, severe stomach pain, and strong contractions. Some women have no bleeding.
A doctor can evaluate a woman’s symptoms and the baby’s heartbeat to identify potential fetal distress. In many instances, rapid cesarean delivery is necessary. If a woman loses excess blood, she may also need a blood transfusion.
Intrauterine growth restriction (IUGR)
Occasionally a baby won’t grow as much as they’re expected to at a certain stage in a woman’s pregnancy. This is known as intrauterine growth restriction (IUGR). Not all small babies have IUGR — sometimes their size can be attributed to the smaller size of their parents.
IUGR can result in symmetrical or asymmetrical growth. Babies with asymmetrical growth often have a normal-sized head with a smaller-sized body.
Maternal factors that can lead to IUGR include:
- anemia
- chronic renal disease
- placenta previa
- placental infarction
- severe diabetes
- severe malnutrition
Fetuses with IUGR may be less able to tolerate the stress of labor than infants of normal size.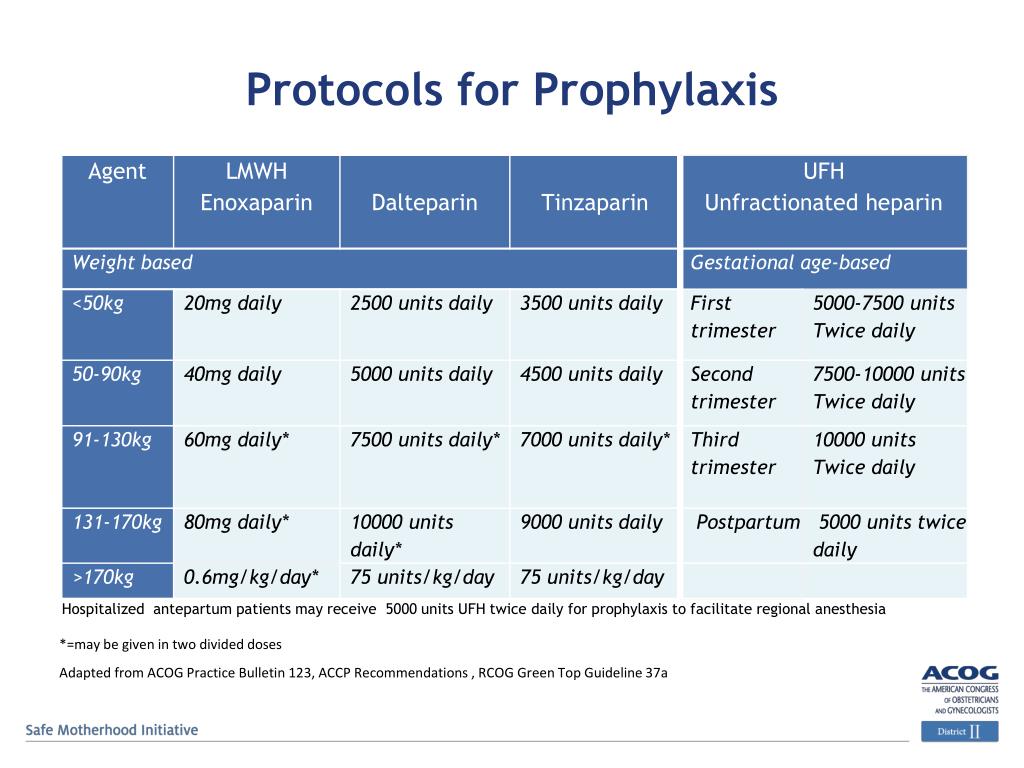 IUGR babies also tend to have less body fat and more trouble maintaining their body temperature and glucose levels (blood sugar) after birth.
IUGR babies also tend to have less body fat and more trouble maintaining their body temperature and glucose levels (blood sugar) after birth.
If growth problems are suspected, a doctor can use an ultrasound to measure the fetus and calculate an estimated fetal weight. The estimate can be compared with the range of normal weights for fetuses of similar age.
To determine whether the fetus is small for gestational age or growth restricted, a series of ultrasounds is done over to time to document weight gain or lack thereof.
A specialized ultrasound monitoring umbilical blood flow can also determine IUGR. Amniocentesis may be used to check for chromosomal problems or infection. Monitoring the fetal heart pattern and measurement of the amniotic fluid are common.
If a baby stops growing in the womb, a doctor may recommend induction or cesarean delivery. Luckily, most growth-restricted babies develop normally after birth. They tend to catch up in growth by two years old.
Post-term pregnancy
About 7 percent of women deliver at 42 weeks or later. Any pregnancy lasting longer than 42 weeks is considered post-term or post-dates. The cause of post-term pregnancy is unclear, although hormonal and hereditary factors are suspected.
Sometimes, a woman’s due date isn’t calculated correctly. Some women have irregular or long menstrual cycles that make ovulation harder to predict. Early in pregnancy, an ultrasound can help to confirm or adjust the due date.
Post-term pregnancy isn’t generally dangerous to the mother’s health. The concern is for the fetus. The placenta is an organ that is designed to work for about 40 weeks. It provides oxygen and nutrition for the growing fetus.
After 41 weeks of pregnancy, the placenta is less likely to work well, and this may result in decreased amniotic fluid around the fetus (oligohydramnios).
This condition can cause compression of the umbilical cord and decrease oxygen supply to the fetus. This may be reflected on the fetal heart monitor in a pattern called late decelerations. There is a risk of sudden fetal death when the pregnancy is post-term.
This may be reflected on the fetal heart monitor in a pattern called late decelerations. There is a risk of sudden fetal death when the pregnancy is post-term.
Once a woman reaches 41 weeks of pregnancy, she usually has fetal heart rate monitoring and a measurement of the amniotic fluid. If the testing shows low fluid levels or abnormal fetal heart rate patterns, labor is induced. Otherwise, spontaneous labor is awaited until no more than 42 to 43 weeks, after which it’s induced.
Meconium aspiration syndrome
The other risk is meconium. Meconium is a fetus’ bowel movement. It’s more common when the pregnancy is post-term. Most fetuses that have a bowel movement inside the uterus have no problems.
However, a stressed fetus can inhale the meconium, causing a very serious type of pneumonia and, rarely, death. For these reasons, doctors work to clear a baby’s airway as much as possible if a baby’s amniotic fluid is meconium-stained.
Malpresentation (breech, transverse lie)
As a woman approaches her ninth month of pregnancy, the fetus generally settles into a head-down position inside the uterus. This is known as vertex or cephalic presentation.
This is known as vertex or cephalic presentation.
The fetus will be bottom or feet first (known as breech presentation) in about 3 to 4 percent of full-term pregnancies.
Occasionally, the fetus will be lying sideways (transverse presentation).
The safest way for a baby to be born is head first or in the vertex presentation. If the fetus is breech or transverse, the best way to avoid problems with delivery and prevent a cesarean is to try to turn (or vert) the fetus to vertex presentation (head down). This is known as external cephalic version. It’s usually attempted at 37 to 38 weeks, if the malpresentation is known.
External cephalic version is somewhat like a firm massage of the abdomen and can be uncomfortable. It’s usually a safe procedure, but some rare complications include placental abruption and fetal distress, necessitating emergency cesarean delivery.
If the fetus is successfully turned, spontaneous labor can be awaited or labor can be induced. If it’s unsuccessful, some doctors wait a week and try again. If unsuccessful after reattempts, you and your doctor will decide the best type of delivery, vaginal or cesarean.
If unsuccessful after reattempts, you and your doctor will decide the best type of delivery, vaginal or cesarean.
Measurement of the bones of the mother’s birth canal and ultrasound to estimate fetal weight are often obtained in preparation for breech vaginal deliveries. Transverse fetuses are delivered by cesarean.
Pregnancy management: 3rd trimester
In the last stages, the expectant mother needs support and care more than ever, so pregnancy management in the 3rd trimester can be a great solution for the whole family! At the final stage of pregnancy, the baby is still growing, childbirth is approaching, and the woman's body is experiencing an increased load. In the 3rd trimester of pregnancy, the expectant mother should visit the obstetrician-gynecologist more often - 2-3 times a month. Analyzes, screenings, ultrasound diagnostics - it takes time and effort. Our clinic has all the conditions for convenient and comfortable pregnancy. We will conduct the necessary examinations ourselves and fill out the pregnant woman's exchange card. Attentive, sensitive and experienced obstetrician-gynecologists are always in touch with their patients and are ready not only to answer all questions, provide medical assistance, but even help make a decision in favor of a maternity hospital. In our clinic it is possible management of pregnancy after IVF (ART) . In a day hospital, complications can be corrected in a timely manner: toxicosis, the threat of miscarriage or early delivery.
Attentive, sensitive and experienced obstetrician-gynecologists are always in touch with their patients and are ready not only to answer all questions, provide medical assistance, but even help make a decision in favor of a maternity hospital. In our clinic it is possible management of pregnancy after IVF (ART) . In a day hospital, complications can be corrected in a timely manner: toxicosis, the threat of miscarriage or early delivery.
The doctors of the Department of Gynecology and Obstetrics of the Pirogov Clinic have been specializing in pregnancy management for many years, behind each doctor there are internships in medical institutions in Europe and St. Petersburg.
How does the fetus develop in the 3rd trimester of pregnancy?
The period from 29 to 40 weeks of pregnancy is the 3rd trimester.
By 29-30 weeks the weight of the fetus already exceeds 1 kg. The movements of the baby become less active due to the fact that it already occupies almost the entire uterine cavity. At this stage, women begin to worry about contractions. However, sometimes they are mistakenly confused with increased uterine tone, and this is no longer the norm. Therefore, severe pain in the lower abdomen and frequent contractions are a reason to contact an obstetrician-gynecologist.
At this stage, women begin to worry about contractions. However, sometimes they are mistakenly confused with increased uterine tone, and this is no longer the norm. Therefore, severe pain in the lower abdomen and frequent contractions are a reason to contact an obstetrician-gynecologist.
By the beginning of the 3rd trimester of pregnancy, the fetus has already formed vision and hearing, the formation of the brain and nervous system is completed - the baby becomes receptive to the outside world. His heartbeat can be heard with a stethoscope.
By 31-32 weeks of pregnancy, the fetus continues to actively develop the structures of the brain, liver and pancreas. The latter is responsible for the production of enzymes that break down proteins, fats and carbohydrates. In the womb, the baby takes its final prenatal position - head down. The volume of the fetal brain by this time is already approximately 75% of the brain of an adult. However, not all children by this time are in the correct position.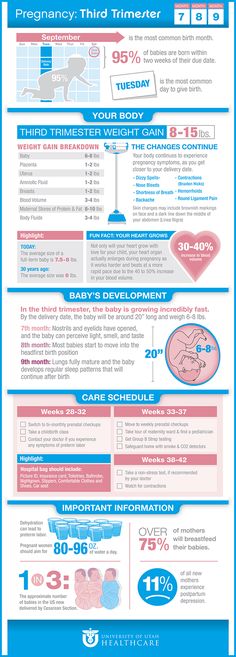 In this case, the obstetrician-gynecologist will certainly consult the mother and recommend a set of special exercises during pregnancy.
In this case, the obstetrician-gynecologist will certainly consult the mother and recommend a set of special exercises during pregnancy.
At the eighth month of pregnancy, the legs of the expectant mother and internal organs may experience increased physical activity. A woman may experience discomfort due to pain in the ligaments and joints, especially in the pelvic region. The endocrine glands of the expectant mother during pregnancy produce special hormones that increase the elasticity of tissues. You should not worry about these pains, but if they are too strong, you need to tell the doctor about it. Varicose veins during pregnancy most often manifest themselves in the 3rd trimester of pregnancy. Phlebologists also conduct appointments in our clinic. The doctor will help solve the problem - for example, he will select a suitable compression stocking that will prevent progressive varicose veins from deforming during pregnancy.
Another common problem that can occur due to high loads is hemorrhoids. During pregnancy, there are a number of restrictions on the treatment of diseases, but a proctologist can help in solving this problem.
During pregnancy, there are a number of restrictions on the treatment of diseases, but a proctologist can help in solving this problem.
The beginning of of the ninth month (36 weeks) is the time to decide on the choice of a maternity hospital and an obstetrician. Also, depending on the data of ultrasound diagnostics and the individual characteristics of the development of pregnancy, the obstetrician-gynecologist decides whether there is a need for a caesarean section.
Starting from 38 weeks , the fetus is already considered full-term. Mom should rest more and prepare for the joyful event of the birth of a child. If the pregnancy is multiple, childbirth may occur before the term 40 weeks - this is normal. The obstetrician-gynecologist who oversees the management of pregnancy in the 3rd trimester is always in touch, and you can contact him with any question.
3rd trimester pregnancy management program
The pregnancy management program in our clinic (St.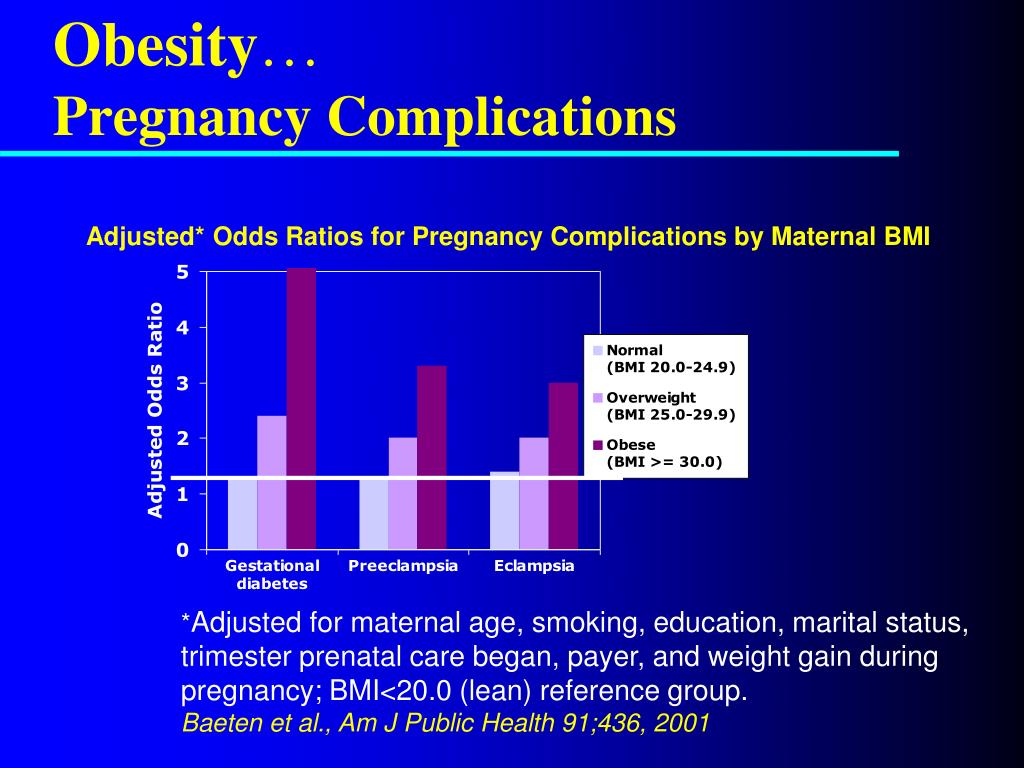 Petersburg) was developed in accordance with the order of the Ministry of Health of the Russian Federation, current clinical guidelines and does not include unnecessary examinations.
Petersburg) was developed in accordance with the order of the Ministry of Health of the Russian Federation, current clinical guidelines and does not include unnecessary examinations.
End-of-term pregnancy management program includes:
- Obstetrician-gynecologist appointments at 30, 32, 34, 36 and 38 weeks of pregnancy.
- Ultrasound during pregnancy - carried out by a doctor of prenatal diagnostics at 32-34 weeks; a very important examination, which allows timely detection of late congenital malformations of the fetus in order to correct them.
- Physician's appointment with electrocardiography (ECG) - available at any time.
- Dopplerography of uteroplacental blood flow — carried out at term pregnancy 36-38 weeks.
- CTG during pregnancy (cardiotocography) - performed at week 36, allows you to identify hypoxic changes (oxygen starvation) that can harm the health of the baby.
- Laboratory tests (blood biochemistry, urine culture, coagulogram, etc.) - can be taken at any convenient time for a period of 34-36 weeks
Find out more about the pregnancy management program in the 3rd trimester and the price (at the Pirogov Clinic, St. Petersburg)
Complications of pregnancy in the 3rd trimester
The most significant risks and complications that may occur at this stage are: threatened preterm delivery and intrauterine growth retardation syndrome . The first complication of pregnancy is caused by increased uterine tone. It manifests itself in bouts of pain in the lower abdomen, which are easy to confuse with training fights. Lack of amniotic fluid (oligohydramnios) can also lead to premature birth, impaired development and growth of the fetus. Screening diagnostics and observation by an obstetrician-gynecologist make it possible to identify this disorder and correct it.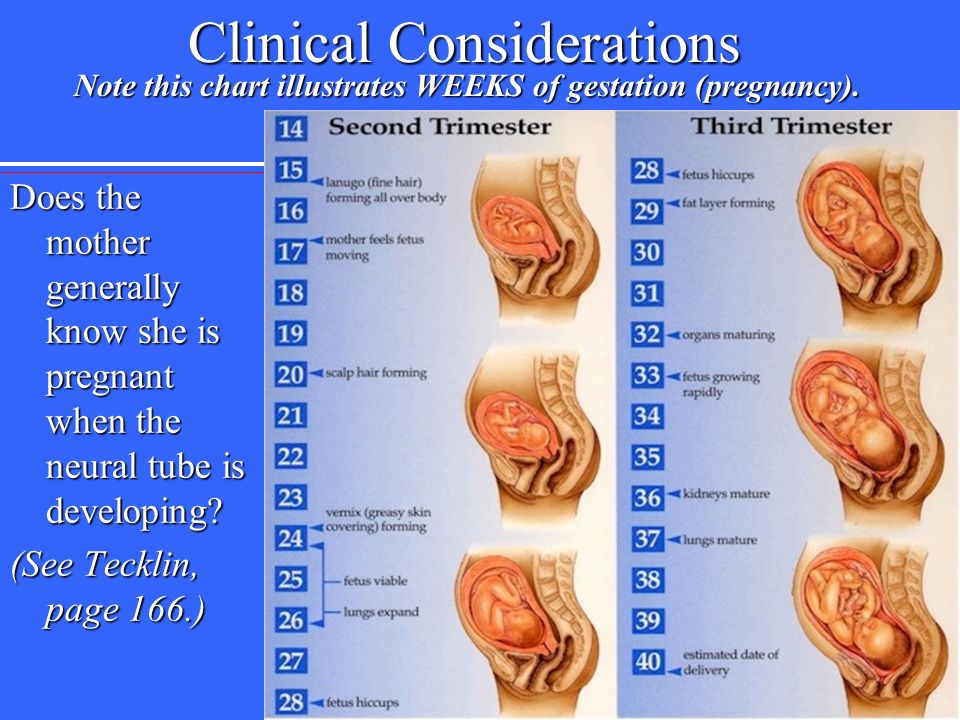
Intrauterine developmental delays are detected during the 1st, 2nd or 3rd ultrasound diagnosis of the fetus. It is important that the baby receives enough nutrients and oxygen from the mother, and that the placenta, internal organs and vital signs (blood pressure, weight, hemoglobin) are not disturbed during pregnancy.
ADVANTAGES OF PREGNANCY MANAGEMENT IN THE PIROGOV CLINIC (St. Petersburg)
- A team of experienced, professional and attentive obstetrician-gynecologists - our doctors have experience in clinics in Europe and the USA, as well as in various medical institutions and maternity hospitals in St. Petersburg.
- Availability of all the necessary narrow-profile doctors of various specializations and our own laboratory in one place - the results of the analyzes are fast and with a guarantee of reliability.
- Exceptionally positive feedback on the management of pregnancy in our clinic at independent sites.
- Diagnostics using new generation equipment.
- Online consultations of obstetrician-gynecologists
- The clinic is located in a picturesque part of the city on Bolshoy Prospekt of Vasilyevsky Island (free parking, walking distance from the Vasileostrovskaya metro station)
- Service under VHI policies.
Sign up for a consultation with an obstetrician-gynecologist: 320-70-00 - we are always happy to answer your questions!
Pregnancy - III trimester
A comprehensive test that includes a group of laboratory tests to determine the general health, functioning of the main systems and organs of a pregnant woman in the third trimester of pregnancy.
Synonyms Russian
Pregnancy, III trimester.
Synonyms English
Pregnancy third (III) trimester.
What biomaterial can be used for research?
Venous blood, mid morning urine.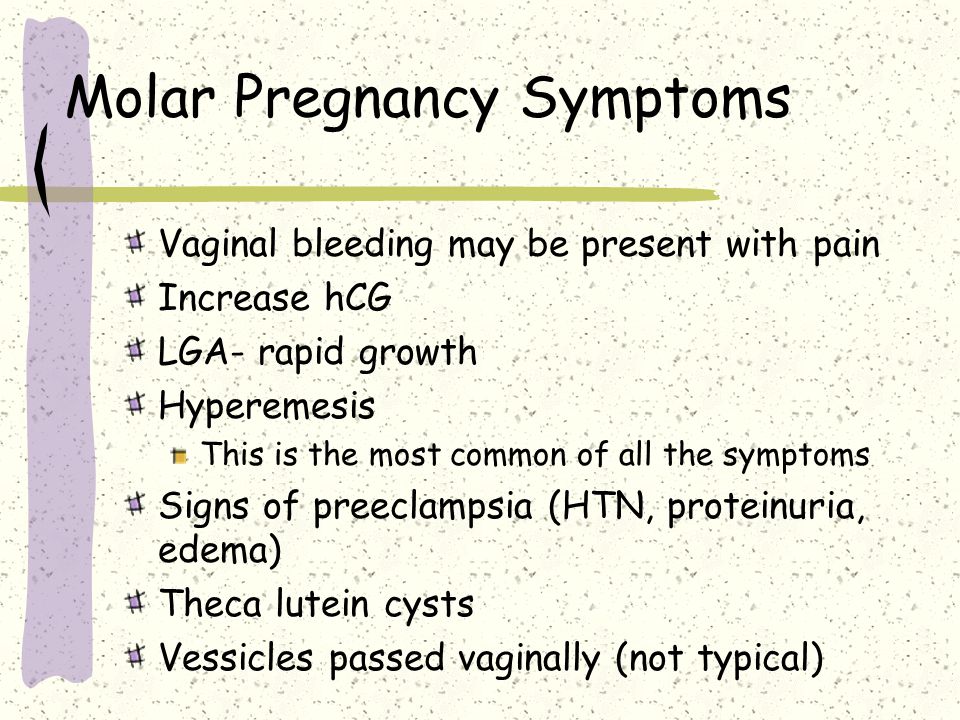
How to properly prepare for an examination?
- Eliminate alcohol from the diet for 24 hours prior to the study.
- Eliminate fatty foods for 24 hours prior to the study.
- Do not eat for 12 hours before the study, you can drink clean still water.
- Exclude (in agreement with the doctor) the use of diuretics within 48 hours before urine collection.
- Completely exclude (in agreement with the doctor) the use of drugs within 24 hours before the study.
- It is recommended to collect urine before menstruation or 2-3 days after it ends.
- Avoid physical and emotional stress for 30 minutes prior to examination.
- HIV testing can be conducted anonymously and confidentially. For a confidential examination, it is mandatory to present a passport.
- Do not smoke for 30 minutes before the test.
General information about the study
The third (III) trimester of pregnancy includes the period between 27 (28) and 38 (40) weeks of pregnancy. During this period, there is an active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, the maturation of the nervous system. Clinical laboratory diagnostics is aimed at assessing the functioning of the main organs and systems, in particular the kidneys, liver, blood coagulation system, the endocrine system of a pregnant woman, as well as the control of infection during pregnancy.
During this period, there is an active growth of the fetus, the improvement of organ systems, in particular the respiratory system, the development of the sense organs, the maturation of the nervous system. Clinical laboratory diagnostics is aimed at assessing the functioning of the main organs and systems, in particular the kidneys, liver, blood coagulation system, the endocrine system of a pregnant woman, as well as the control of infection during pregnancy.
A clinical blood test allows you to evaluate the qualitative and quantitative composition of blood according to the main indicators: erythrocytes, leukocytes and their varieties in absolute and percentage terms, platelets. Identification of deviations in these indicators may indicate the presence of pathological processes and diseases in a pregnant woman. A reduced number of erythrocytes, hemoglobin content in erythrocytes may indicate the presence of anemia in pregnant women. This condition can lead to placental insufficiency - the main cause of miscarriage, the birth of small children and fetal death. Changes in the leukocyte formula may indicate a wide range of changes in the body of a pregnant woman. These may be laboratory signs of inflammatory and infectious diseases, pathologies that a woman has, but not previously diagnosed. The number of platelets during pregnancy may be below normal, which must be taken into account. Significant changes in these indicators, developing thrombocytopenia require special monitoring, as they can be indirect signs of pathologies of the blood coagulation system, as well as such a severe pregnancy complication as DIC (disseminated intravascular coagulation syndrome). A change in ESR can be observed in the presence of acute and chronic inflammatory diseases, in infectious processes. A slight increase in ESR can be observed during pregnancy. This test has high sensitivity, but low specificity and is prescribed in combination with other indicators.
Changes in the leukocyte formula may indicate a wide range of changes in the body of a pregnant woman. These may be laboratory signs of inflammatory and infectious diseases, pathologies that a woman has, but not previously diagnosed. The number of platelets during pregnancy may be below normal, which must be taken into account. Significant changes in these indicators, developing thrombocytopenia require special monitoring, as they can be indirect signs of pathologies of the blood coagulation system, as well as such a severe pregnancy complication as DIC (disseminated intravascular coagulation syndrome). A change in ESR can be observed in the presence of acute and chronic inflammatory diseases, in infectious processes. A slight increase in ESR can be observed during pregnancy. This test has high sensitivity, but low specificity and is prescribed in combination with other indicators.
Urinalysis with microscopy of the urinary sediment is a set of diagnostic tests that allow assessing the general properties of urine, its physico-chemical properties, the content of metabolic products, and identifying the qualitative and quantitative content of a number of organic compounds.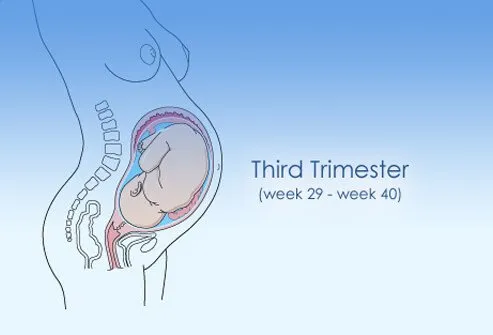 These tests reflect the functional state of the kidneys, urinary tract, allow us to judge the general metabolic processes, suggest the presence of possible disorders, infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, diabetes in pregnant women. The detection of protein in the urine may be a sign of developing nephropathy in pregnant women, proteinuria of more than 0.3 g in daily urine may indicate the development of a severe pregnancy complication - preeclampsia. The severity of this condition varies greatly. So, with the development of mild preeclampsia after 36 weeks, the prognosis is usually favorable. On the contrary, the threat to the health of the mother or fetus is seriously increased if preeclampsia develops early (before 33 weeks) and is aggravated by the presence of concomitant diseases.
These tests reflect the functional state of the kidneys, urinary tract, allow us to judge the general metabolic processes, suggest the presence of possible disorders, infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, diabetes in pregnant women. The detection of protein in the urine may be a sign of developing nephropathy in pregnant women, proteinuria of more than 0.3 g in daily urine may indicate the development of a severe pregnancy complication - preeclampsia. The severity of this condition varies greatly. So, with the development of mild preeclampsia after 36 weeks, the prognosis is usually favorable. On the contrary, the threat to the health of the mother or fetus is seriously increased if preeclampsia develops early (before 33 weeks) and is aggravated by the presence of concomitant diseases.
In the third trimester of pregnancy, it is also necessary to monitor the functional state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to assess the extrinsic pathway of blood clotting. The following indicators are obtained as results: prothrombin time according to Quick and international normalized ratio. Activated partial thromboplastin time (APTT) characterizes the intrinsic pathway of blood coagulation. Fibrinogen is the factor I (first) factor of the blood plasma coagulation system. These indicators make it possible to assess the functional state of the liver, the main pathways of the blood coagulation system, and to assess the functional state of its components. Their determination is important for predicting thrombosis during pregnancy, diagnosing such a complication as DIC, the planned appointment of the necessary therapy during childbirth - a process accompanied by massive blood loss. It should be noted that there is a physiological increase in the levels of prothrombin and fibrinogen in the third trimester of pregnancy. But a sharp increase in these indicators requires special monitoring and the appointment of the necessary therapy.
The prothrombin time test is used to assess the extrinsic pathway of blood clotting. The following indicators are obtained as results: prothrombin time according to Quick and international normalized ratio. Activated partial thromboplastin time (APTT) characterizes the intrinsic pathway of blood coagulation. Fibrinogen is the factor I (first) factor of the blood plasma coagulation system. These indicators make it possible to assess the functional state of the liver, the main pathways of the blood coagulation system, and to assess the functional state of its components. Their determination is important for predicting thrombosis during pregnancy, diagnosing such a complication as DIC, the planned appointment of the necessary therapy during childbirth - a process accompanied by massive blood loss. It should be noted that there is a physiological increase in the levels of prothrombin and fibrinogen in the third trimester of pregnancy. But a sharp increase in these indicators requires special monitoring and the appointment of the necessary therapy. The level of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, but a sharp increase in the concentration of D-dimer may indicate a large number of blood clots, which is most often caused by venous thromboembolism or DIC.
The level of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, but a sharp increase in the concentration of D-dimer may indicate a large number of blood clots, which is most often caused by venous thromboembolism or DIC.
Determination of such biochemical indicators as alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin and direct bilirubin fraction, total protein in serum allows assessing the functional state of the liver. ALT levels may be slightly elevated while AST levels are lowered. A significant increase in the concentration of transaminases may indicate the presence of liver damage, hepatitis, and the development of preeclampsia. A decrease in the level of total protein in the blood serum along with the loss of protein in the urine and with an increase in blood pressure over 140/90 mmHg Art. is also a sign of developing preeclampsia.
To exclude the development of diabetes in pregnancy (gestational diabetes), the development of complications, in particular diabetic nephropathy, it is necessary to determine the level of glucose in the blood plasma.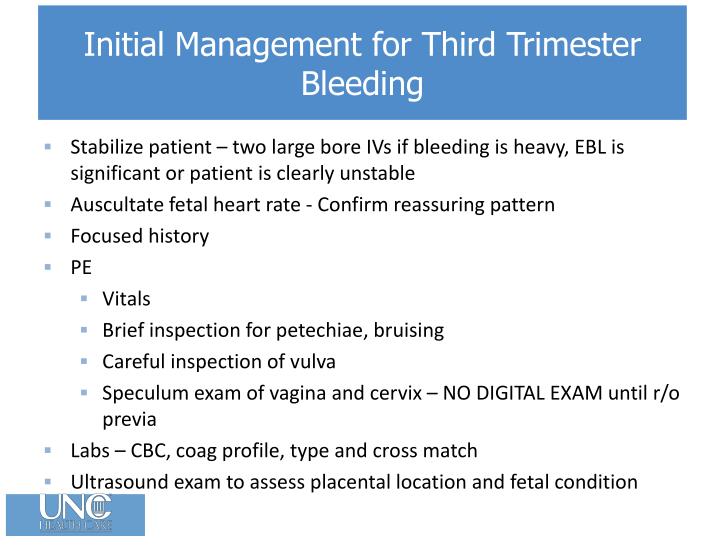
To assess the functional state of the kidneys, in particular the preservation of glomerular filtration processes, several diagnostic parameters are used. The most important and characteristic is the determination of the levels of urea and creatinine in the blood serum, as well as the assessment of the glomerular filtration rate. Importantly, creatinine levels are reduced by almost half in pregnant women due to increased blood volume, increased blood flow to the kidneys and, consequently, an increasing degree of filtration. Also, an increase in renal filtration causes a decrease in the amount of urea in pregnant women.
Generally, pregnancy occurs with normal levels of thyroid-stimulating hormone (TSH) in the blood. This euthyroid state is maintained by all components of the thyroid system and placental hormones, in particular human chorionic gonadotropin and chorionic thyrotropin. The maternal and fetal thyroid hormone systems are independent of each other and poorly penetrate the mature placenta. The level of TSH in the blood of pregnant women may increase with the development of preeclampsia.
The level of TSH in the blood of pregnant women may increase with the development of preeclampsia.
In the third trimester of pregnancy, it is also recommended to re-test for hepatitis B - HBsAg, hepatitis C - anti-HCV, antibodies, HIV infection - HIV 1.2 Ag/AbCombo (determination of antibodies to HIV types 1 and 2 and p24 antigen) , syphilis - antibodies to Treponema pallidum. The incubation period of some infections varies greatly and a negative test result at the beginning of pregnancy may change in the last weeks of pregnancy or remain negative as well. This is necessary to prevent infection of the fetus during childbirth, the appointment of the necessary treatment or a planned caesarean section.
What is research used for?
- For preventive examination of pregnant women in the third trimester of pregnancy.
- If there is a suspicion of deviations in the normal functioning of the systems and organs of pregnant women.
- For diagnosing complications of the third trimester of pregnancy.

When is the test scheduled?
- Pregnant women in the third trimester at 27-38 (40) weeks of pregnancy.
What do the results mean?
Reference values
For each indicator included in the complex:
- [02-005] Clinical blood test (with leukocyte formula)
- [02-006] Urinalysis with microscopy
- [02-007] Erythrocyte sedimentation rate (ESR)
- [03-001] D-dimer
- [03-003] Activated partial thromboplastin time (APTT)
- [03-007] Coagulogram No. 1 (prothrombin (according to Quick), INR)
- [03-011] Fibrinogen
- [06-003] Alanine aminotransferase (ALT)
- [06-010] Aspartate aminotransferase (AST)
- [06-015] Plasma glucose
- [06-021] Serum creatinine (with GFR determination)
- [06-034] Serum urea
- [06-035] Total serum protein
- [06-036] Bilirubin total
- [06-037] Bilirubin direct
- [07-009] anti-HCV, antibodies
- [07-025] HBsAg
- [07-032] HIV 1.
 2 Ag/Ab Combo (detection of antibodies to HIV types 1 and 2 and p24 antigen)
2 Ag/Ab Combo (detection of antibodies to HIV types 1 and 2 and p24 antigen) - [07-049] Treponema pallidum, antibodies
- [08-118] Thyroid stimulating hormone (TSH)
What can influence the result?
- The use of drugs, in particular hormonal drugs.
Who orders the examination?
Obstetrician-gynecologist, general practitioner, endocrinologist, internist, infectious disease specialist.
Literature
- Dolgov V.V., Menshikov V.V. Clinical laboratory diagnostics: national guidelines. - T. I. - M. : GEOTAR-Media, 2012. - 928 p.
- Moon HW, Chung HJ, Park CM, Hur M, Yun YM1. Establishment of trimester-specific reference intervals for thyroid hormones in Korean pregnant women / Ann Lab Med. 2015 Mar;35(2):198-204.
- Angueira AR, Ludvik AE, Reddy TE, Wicksteed B, Lowe WL Jr, Layden BT. New insights into gestational glucose metabolism: lessons learned from 21st century approaches.