Birthmarks on babies heads
Infantile Hemangiomas: About Strawberry Baby Birthmarks
Hemangiomas are clusters of extra blood vessels on a baby's skin. They may be there when a baby is born, or form within a few weeks or months of birth. Some may look like rubbery, bumpy red "strawberry" patches while others resemble deep bruises. Seeing a hemangioma develop can be worrisome for new parents.
The American Academy of Pediatrics (AAP) guidelines say it's important to identify and begin monitoring infantile hemangiomas right after they appear―when they tend to change most quickly.
While hemangiomas can vary a lot in size, appearance, and placement, they are universally benign (non-cancerous). Most will go away on their own without causing any problems. Some hemangiomas―particularly those on the face or those that are very large―need treatment early to prevent them from interfering with body functions or causing permanent scars. Thankfully, there are excellent treatments available today to can prevent these problems if treated early on.
About Infantile Hemangiomas:
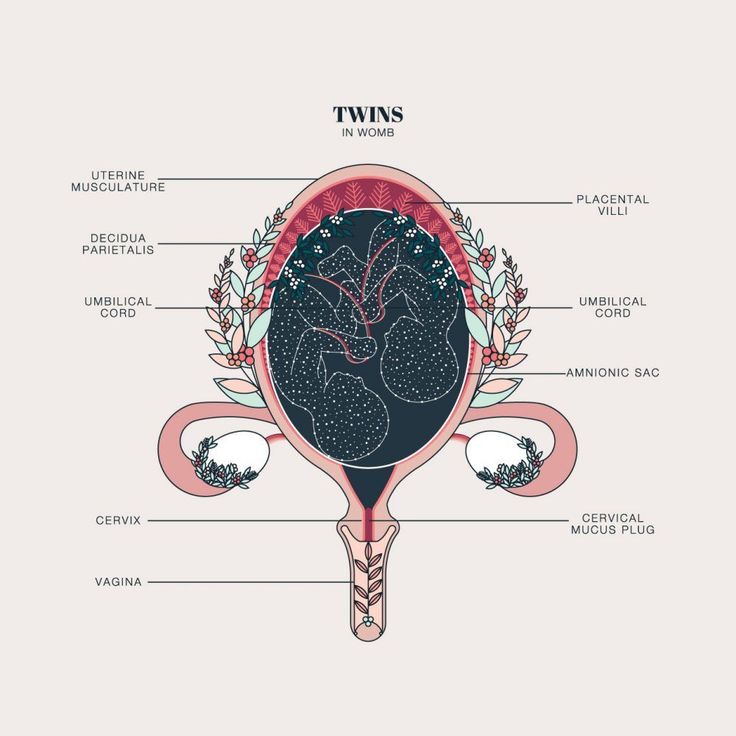
Infantile hemangiomas appear after a baby is born, typically within a month. Roughly 4% to 5% of all infants get them, although they are more common in Caucasians, girls, twins, and preterm or low-birth-weight babies. Infantile hemangiomas typically go through a period of rapid growth, followed by more gradual fading and flattening.
There are different types of infantile hemangiomas:
Superficial hemangiomas have been called "strawberry marks," because they can resemble the surface of berries. They may begin as small white, pink, or red areas on the skin that quickly change into brighter red, raised lesions. Superficial hemangiomas may be focused in one spot or spread out over a larger area.
Deep hemangiomas have a smooth surface and form under the skin. They may have a bluish tint and resemble bruises. Some cause the skin to look swollen.
Mixed hemangiomas are a combination of superficial and deep growths.
Are there other birthmarks like it?
Some of the other marks that can show up on a baby's skin include port wine stains and "stork bites." These also are caused when more blood than usual floods the capillaries under the skin. Port wine stains turn a reddish-purple and are often permanent; like hemangiomas, stork bites usually disappear, but can remain if they're on the back of the neck.
What to do if you think your baby has an infantile hemangioma:
Infantile hemangiomas usually become noticeable by 4 weeks of age. They may start out looking like a tiny bump or scratch. But many then grow especially fast between 5 and 7 weeks old. If you think your baby might have a hemangioma, it's best to contact your baby's pediatrician right away. He or she probably will want to see your baby within a short timeframe. According to the AAP, the best "window of opportunity" to be evaluated and start treatment if needed is about 1 month of age.
Your pediatrician will want to know:
Size: Is the hemangioma small (3/4" or less across) or larger?
Location: Is it located on the face or in the diaper area, or in a different area?
Number: Is there one or more than one? If more than one, how many?
If your doctor can't see you in the office right away, they may ask you to send photos or recommend a telemedicine visit to have a look without delay.
What to expect next:
It's important to continue monitoring the hemangioma until it stops growing.
Superficial hemangiomas typically reach their full size by 5 months of age, although
deep hemangiomas sometimes keep growing a while longer. In some cases, your pediatrician may give a referral to an infantile hemangioma specialist with expertise in
pediatric dermatology, hematology-oncology, otolaryngology, or
plastic surgery.
By the time a baby is 6-18 months old, most hemangiomas begin to slowly improve. In a process called "involution," the hemangioma will become less red and more grey or whitish and gradually flatten and shrink from the center outward.
Each case is different. Most hemangiomas have finished or almost finished flattening and shrinking by 4 to 5 years of age. |
When does a hemangioma need to be treated?
Whether a hemangioma needs treatment depends on the age of the baby, where the hemangioma is located and how fast it is growing, whether it becomes sore or scabby, and the risk of it causing medical complications with a child's health and well-being.
There are 3 main reasons for treatment:
Medical problems. In rare cases and depending where they are located and how fast they are growing, hemangioma may begin to interfere with vital functions.
 Hemangiomas near the child's eyes, nose or mouth, for example, can affect the child's ability to see, eat, breath or hear well. In rare cases, hemangiomas grow inside the body, which may need to be monitored with imaging tests.
Hemangiomas near the child's eyes, nose or mouth, for example, can affect the child's ability to see, eat, breath or hear well. In rare cases, hemangiomas grow inside the body, which may need to be monitored with imaging tests.Skin breakdown. Sometimes, skin on the hemangioma's surface breaks down and becomes an open sore (called an ulcer) that could lead to bleeding, infection, or scarring.
Permanent skin changes. Changes in the skin's texture or color can remain even after the hemangioma has gone away. This can be a concern, especially for hemangiomas on the child's face. Large hemangiomas on facial features such as the nose or lip can also distort growth.
What kinds of treatments are available for hemangiomas?
If a baby's hemangioma risks causing problems, medications can be applied directly to the skin or taken by mouth. The goal is to keep them from getting any bigger during their period of rapid growth, or to make them shrink more quickly.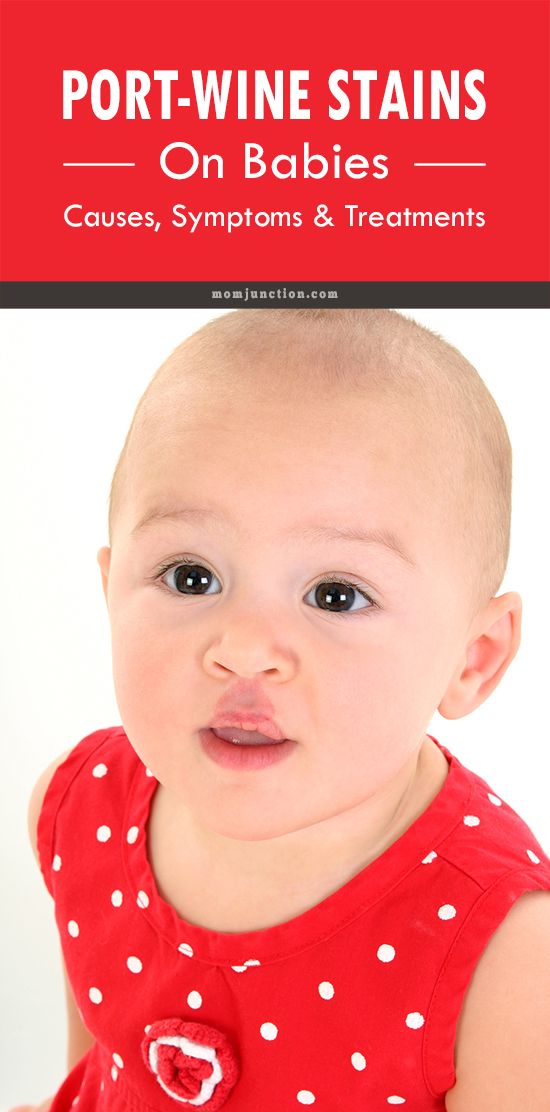 Laser procedures or surgery may be an option in some cases, although it generally is avoided during early infancy to avoid increased anesthesia risks.
Laser procedures or surgery may be an option in some cases, although it generally is avoided during early infancy to avoid increased anesthesia risks.
Systemic treatments
Propranolol, a beta blocker medication used for many years to treat high blood pressure, is now commonly given by mouth as an effective treatment for problem hemangiomas. To avoid a growth rebound, the pediatrician may recommend therapy continue until your child's first birthday. The drug must be used with close observation by your healthcare provider to watch for possible side effects and complications.
Oral steroids have been largely replaced by safer and more effective options, but are still used in select cases, determined by the healthcare provider.
Localized treatments
Topical medications applied directly on the skin may be used for small, superficial hemangiomas. Prescription creams or ointments containing beta-blockers are the most effective topical treatment option to help stop growth and sometimes shrink and fade hemangiomas.
 In some cases, steroid creams may be prescribed for smaller, thinner hemangiomas.
In some cases, steroid creams may be prescribed for smaller, thinner hemangiomas.Steroid injections can be given directly into the hemangioma to help slow its growth. This works best for smaller, localized hemangiomas.
Other treatments
Surgery is usually only considered for smaller hemangiomas in areas where they may cause problems, or for small hemangiomas with broken skin. Because surgery will always leave a scar itself--and because most hemangiomas get better with time--early surgery is only recommended for a small minority of cases. Surgery can also repair extra skin or scars left by a hemangioma, but usually is delayed until a child is between 3 and 5 years old.
Laser treatment may be helpful in some cases to stop bleeding or to help heal hemangiomas with open sores (ulcers). They can also help to remove some of the redness or texture changes that may be left behind after the hemangioma improves.

Remember:
Contact your pediatrician if you notice anything developing on your baby's skin. Your baby's first few well-child visits are also a great time to bring it up. Few hemangiomas cause any trouble, and most go away on their own. But prompt evaluation, monitoring and treatment, when needed, can help ensure problem hemangiomas have as little impact as possible on your child.
Additional Information:
Baby Birthmarks & Rashes
Management of Infantile Hemangiomas (AAP Clinical Practice Guideline)
HemangiomaEducation.org
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Birthmarks in Infants | Johns Hopkins Medicine
A baby's skin coloring can vary greatly, depending on the baby's age, race or ethnic group, temperature, and whether or not the baby is crying. Skin color in babies often changes with both the environment and health. Some of these differences are just temporary. Others, such as certain birthmarks, may be permanent.
Skin color in babies often changes with both the environment and health. Some of these differences are just temporary. Others, such as certain birthmarks, may be permanent.
Birthmarks are areas of discolored and/or raised skin that are present at birth or within a few weeks of birth. Birthmarks are made up of abnormal pigment cells or blood vessels.
Although the cause of birthmarks is not known, most of them are harmless and do not require treatment. Babies with birthmarks should be examined by your child's health care provider, especially if they are:
-
Located in the middle of the back, along the spine (may be related to spinal cord problems)
-
Large birthmarks on the face, head or neck
-
Interfering with movement of activity, for example a birthmark on the eyelid that may interfere with vision
Some common birthmarks include:
| Birthmark | What it looks like |
|---|---|
| Stork bites, angel kisses, or salmon patches | These are small pink or red patches often found on a baby's eyelids, between the eyes, upper lip, and back of the neck. The "stork bite" name comes from the marks on the back of the neck where, as the myth goes, a stork may have picked up the baby. They are caused by a concentration of immature blood vessels and may be the most visible when the baby is crying. Most of these fade and disappear completely. The "stork bite" name comes from the marks on the back of the neck where, as the myth goes, a stork may have picked up the baby. They are caused by a concentration of immature blood vessels and may be the most visible when the baby is crying. Most of these fade and disappear completely. |
| Congenital dermal melanocytosis (also known as Mongolian spots) | Congenital dermal melanocytosis refers to areas of blue or purple-colored, typically on the baby's lower back and buttocks. These can occur in darker-skinned babies of all races. The spots are caused by a concentration of pigmented cells. They usually disappear in the first 4 years of life. |
| Strawberry hemangioma | This is a bright or dark red, raised or swollen, bumpy area that looks like a strawberry. Hemangiomas are formed by a concentration of tiny, immature blood vessels. Most of these occur on the head. They may not appear at birth, but often develop in the first 2 months. Strawberry hemangiomas are more common in premature babies and in girls. These birthmarks often grow in size for several months, and then gradually begin to fade. They may bleed or get infected in rare cases. Nearly all strawberry hemangiomas completely disappear by 9 years of age. Most of these occur on the head. They may not appear at birth, but often develop in the first 2 months. Strawberry hemangiomas are more common in premature babies and in girls. These birthmarks often grow in size for several months, and then gradually begin to fade. They may bleed or get infected in rare cases. Nearly all strawberry hemangiomas completely disappear by 9 years of age. |
| Port-wine stain | A port-wine stain is a flat, pink, red, or purple colored birthmark. These are caused by a concentration of dilated tiny blood vessels called capillaries. They usually occur on the head or neck. They may be small, or they may cover large areas of the body. Port-wine stains do not change color when gently pressed and do not disappear over time. They may become darker and thicker when the child is older or as an adult. Port-wine stains on the face may be associated with more serious problems. Skin-colored cosmetics may be used to cover small port-wine stains. The most effective way of treating port-wine stains is with a special type of laser. This is done when the baby is older by a plastic surgery specialist. The most effective way of treating port-wine stains is with a special type of laser. This is done when the baby is older by a plastic surgery specialist. |
| Congenital moles | These common moles (less than 3 inches in diameter) occur in about 1 out of every 100 newborns. They increase in size as the child grows, but usually don't cause any problems. Your child's health care provider will watch them closely as rarely they can develop into a cancerous mole. |
Baby birthmarks, recommended medical supervision. Lakhta Junior in St. Petersburg
Let's talk about children's birthmarks, their possible and most common options.
“Like a baby,” we envy about the most healthy, satiny, velvety, uniform skin. But the idea that any spot on the skin of a baby is obviously a pathology is nothing more than a myth.
Birthmarks are called so because they are often visible already in the newborn, although sometimes they appear at later stages of development. The color, size, shape of a birthmark can be very different. Some of these marks disappear over time, others become brighter and/or remain permanently.
The color, size, shape of a birthmark can be very different. Some of these marks disappear over time, others become brighter and/or remain permanently.
Much and completely justified attention is paid today to the dangers that moles carry in themselves in adulthood and old age. On the contrary, most children's moles do not pose any danger.
Vascular ("stork's mark", "angel's kiss", hemangiomas, venous malformations, etc.). The cause of such spots are problems with small blood vessels, usually transient. Vascular spots are distinguished by a red-violet color in one shade or another; may rise slightly above the surface of the skin or be flat.
Age spots (“café au lait”, melanocystosis, Mongolian spots, etc.). Formed by various skin cells; look, as a rule, brown-gray, usually do not rise above the skin.
Again, in most cases, both main varieties of birthmarks are quite safe and harmless. And yet, only a doctor can judge whether it is possible to confine oneself to observation or whether the stain is to be removed for medical reasons. This type of consultation is strictly required.
This type of consultation is strictly required.
Let's take a closer look at common types of birthmarks.
Stork Mark (stork peck, stork mark, etc.).
This is the name in many countries for reddish-pink spots that a newborn may have on the back of the head or back of the neck. As a rule, such spots do not rise above the surface and have an uneven shape. Most often, the stork mark occurs in children with fair skin.
The explanation that this is a trace of the "transportation" of the baby by the stork, older brothers and sisters, as a rule, is accepted unconditionally, and even with delight. "Stork peck" usually disappears without a trace by 18 months of age. Otherwise, especially if the stain causes noticeable discomfort, it is removed (for example, using minimally invasive laser technology).
Port-wine stain
Port-wine stain or, in medical terminology, flaming nevus - flat capillary moles, outwardly and really resembling a puddle of spilled purple-red wine. They occur with a frequency of 3-5 cases per 1000 newborns. With age, they can increase and acquire a darker shade.
They occur with a frequency of 3-5 cases per 1000 newborns. With age, they can increase and acquire a darker shade.
Treatment is not usually required, but the skin in this area tends to become dry and irritated. Sometimes they resort to the method of laser removal, which, however, does not always completely eliminate the cosmetic defect.
"Strawberry hemangioma"
Obsolete name for infantile hemangioma, a bright red congenital benign vascular tumor that rises above the surface of the skin and has a characteristic surface texture. It occurs in about 5% of newborns, more often in girls, twins and premature babies.
Usually localized on the face, head or chest; as a rule, decreases with age and finally disappears in the preschool period. It is possible to remove a hemangioma, especially if it is large and / or located near the eyes, nose, mouth. Both minimally invasive surgical and conservative methods of removal are practiced.
Venous malformations
These are blue-violet spots that can sometimes appear on the skin, especially during moments of intense crying. Venous malformations (lit. "malformations") are always congenital in nature, but sometimes remain almost invisible until adolescence. They can be located on any part of the body. Compared to other types of birthmarks, they are rare - in one case in about five thousand.
Venous malformations (lit. "malformations") are always congenital in nature, but sometimes remain almost invisible until adolescence. They can be located on any part of the body. Compared to other types of birthmarks, they are rare - in one case in about five thousand.
Coffee with milk
Localized abnormal pigmentation that occurs in 30% of people. The color of such a spot is usually light brown or beige, which is reflected in the name. The edges are usually even, the perimeter is sometimes darker than the inner area. In most cases, a café au lait pigment spot is quite harmless, but it can enlarge and/or darken with age. Such spots are subject to observation in dynamics, in some cases they can be removed.
Moles proper
Well-known round or oval freckle-like formations. The color varies from light brown or pink-red to almost black. Sizes in individual cases also vary widely. They can be both flat and protruding above the surface.
Moles should be inspected regularly to prevent any damage (mechanical, chemical, etc.). If a mole begins to bleed, change color, shape, appearance and any other characteristics, you should see a specialist as soon as possible - a dermatologist or oncologist at the Lakhta Junior Children's Clinic in St. Petersburg.
What are the types of infantile (infantile) hemangiomas?
Erstellt am 2017/10/19, last modified: 2017/10/19 https://kinderkrebsinfo.de/doi/e195094
Contents
- Local infantile hemangiomas
- Segmental infantile hemangiomas
- Special forms
Typically, infantile hemangiomas (that is, hemangiomas in newborns and infants, and many doctors use the term infantile hemangiomas) appear in the first days or weeks after the birth of a child. First, the first symptoms appear (specialists talk about the precursor forms of hemangiomas) - dilated subcutaneous vessels in a limited area of \u200b\u200bthe skin (telangiectasia in the language of specialists), or, for example, very pale spots, or spots of bright red or cyanotic color, or changes in the skin, similar to red birthmarks (doctors talk about vascular nevus). The classic infantile hemangioma at the birth of a child does not yet look like a tumor, it becomes one after some time.
The classic infantile hemangioma at the birth of a child does not yet look like a tumor, it becomes one after some time.
Good to know: infantile hemangioma goes through three stages:
- Active growth phase: the first stage lasts from 6 to 9 months
- Growth arrest phase: tumor size no longer changes
- Regression phase (gradual reverse development of hemangioma, that is, the tumor begins to “resolve”, the recovery process is underway): as a rule, recovery ends by the 9th year of the child's life.
Local infantile hemangiomas
90% of all infantile hemangiomas are local. This means that they have clear boundaries and grow from one central point.
Local infantile hemangiomas are divided into:
- superficial skin infantile hemangiomas. They grow on the surface of the skin (flat) or may protrude above the skin (convex, i.e. do not grow deep)
- deep subcutaneous hemangiomas.
 They grow deep under the skin
They grow deep under the skin - combined hemangiomas. That is, a mixed type, when an infantile hemangioma simultaneously grows as a superficial skin and deep subcutaneous
Usually, at birth, an infantile hemangioma is not yet visible in a child. But then, during repeated examinations in the first weeks after birth, a small spot of red color becomes noticeable. Some infantile hemangiomas do not change for weeks or months. Others begin to grow rapidly and grow to enormous size. Most infantile hemangiomas (60%) appear in the head and neck.
Segmental infantile hemangiomas
Segmental infantile hemangiomas (that is, a large hemangioma will grow in a certain area of the body) are less common than local ones. They can appear both in the head and neck, and in the region of the lumbar spine and in the coccyx. Usually the size of segmental infantile hemangiomas is larger than that of local forms. In addition, they often appear when abnormal development of blood vessels or internal organs begins in the body (in this case, doctors talk about malformations or developmental anomalies). Characteristic of segmental hemangiomas is that they are very large and cover a certain department (segment) of the body. They are almost invisible at birth. But they can grow very quickly and then the baby often has various health problems.
Characteristic of segmental hemangiomas is that they are very large and cover a certain department (segment) of the body. They are almost invisible at birth. But they can grow very quickly and then the baby often has various health problems.
For example, segmental infantile hemangiomas in the face or shoulder region are associated with the so-called PHACES syndrome (P.H.A.C.E.S. syndrome is a set of several congenital malformations, each letter of the abbreviation denotes a specific malformation). First, anomalies in the development of the chest, aorta, as well as heart defects and cysts in the brain (in the language of specialists, the so-called Dandy-Walker variant) are found in the baby, and then a segmental hemangioma appears. Another complication is a tendency to form ulcers and a tendency to frequent infections.
Hemangiomas that grow in the perineum are part of the PELVIS (in the pelvis) and SAKRAL (in the sacrum) syndromes. They are accompanied by skin growths, as well as anomalies in the development of the bladder, spinal cord and spinal cord membranes, and abnormal development of the anus.
In rare cases, infantile hemangiomas can also grow in the area of internal organs, such as the liver or kidneys.
Special shapes
"Rapid Involuting Congenital Hemangioma / abbreviated as RICH":
These forms may also be referred to as congenital rapidly regressing hemangiomas. Already at the birth of a child, they are fully developed (doctors say "fully formed") and quickly (in English " rapid " ) completely disappear, usually by the third year of a baby's life (doctors often use the term "involution “ , from the English term "involuting" , which means reverse development of ).
"Congenital non-involuting hemangioma (Non involuting congenital hemangioma / abbreviated NICH)"
These infantile hemangiomas may also be referred to as congenital nonregressive hemangiomas. They don't disappear on their own, but they don't grow either.
Benign neonatal hemangiomatosis
A child has many small hemangiomas on the skin that look like small millet.