Radiation in pregnancy
Radiation and Pregnancy: Information for Clinicians
This overview provides physicians with information about prenatal radiation exposure as an aid in counseling pregnant women.
How to use this document
This information is for clinicians. If you are a patient, we strongly advise that you consult with your physician to interpret the information provided, as it may not apply to you. Information on radiation exposure during pregnancy for members of the public can be found on the Health Information for Specific Groups webpage.
CDC recognizes that providing information and advice about radiation to expectant mothers falls into the broader context of preventive healthcare counseling during prenatal care. In this setting, the purpose of the communication is always to promote health and long-term quality of life for the mother and child.
This page is also available as a PDF pdf icon[365 KB]
Radiation exposure to a fetus
Most of the ways a pregnant woman may be exposed to radiation, such as from a diagnostic medical exam or an occupational exposure within regulatory limits, are not likely to cause health effects for a fetus. However, accidental or intentional exposure above regulatory limits may be cause for concern.
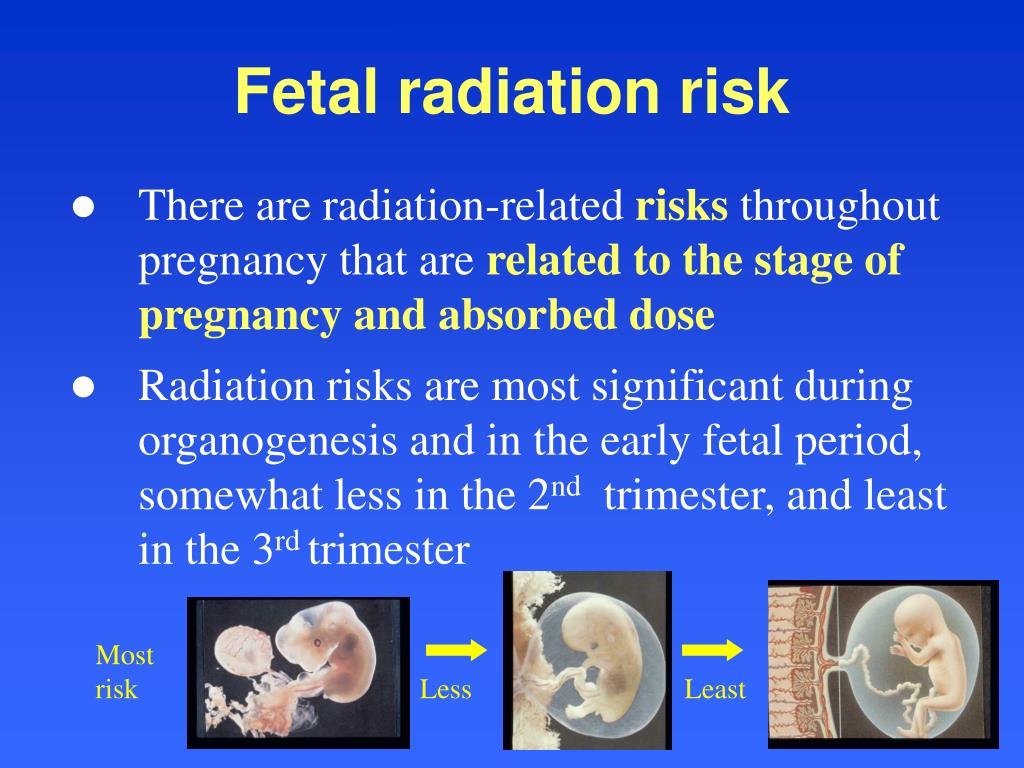
Although radiation doses to a fetus tend to be lower than the dose to the mother, due to protection from the uterus and surrounding tissues, the human embryo and fetus are sensitive to ionizing radiation at doses greater than 0.1 gray (Gy). Depending on the stage of fetal development, the health consequences of exposure at doses greater than 0.5 Gy can be severe, even if such a dose is too low to cause an immediate effect for the mother. The health consequences can include growth restriction, malformations, impaired brain function, and cancer.
Estimating the Radiation Dose to the Embryo or Fetus
Health effects to a fetus from radiation exposure depend largely on the radiation dose. Estimating the radiation dose to the fetus requires consideration of all sources external and internal to the mother’s body, including the following:
- Dose from an external source of radiation to the mother’s abdomen.

- Dose from inhaling or ingesting a radioactive substance that enters the bloodstream and that may through the placenta.
- Dose from radioactive substances that may concentrate in maternal tissues surrounding the uterus, such as the bladder, and that could irradiate the fetus.
Most radioactive substances that reach the mother’s blood can be detected in the fetus’ blood. The concentration of the substance depends on its specific properties and the stage of fetal development. A few substances needed for fetal growth and development (such as iodine) can concentrate more in the fetus than in corresponding maternal tissue.
Consideration of the dose to specific fetal organs is important for substances that can localize in specific organs and tissues in the fetus, such as iodine-131 or iodine-123 in the thyroid, iron-59 in the liver, gallium-67 in the spleen, and strontium-90 and yttrium-90 in the skeleton.
Radiation experts can assist in estimating the radiation dose to the embryo or fetus
Hospital medical physicists and health physicists are good resources for expertise in estimating the radiation dose to the fetus.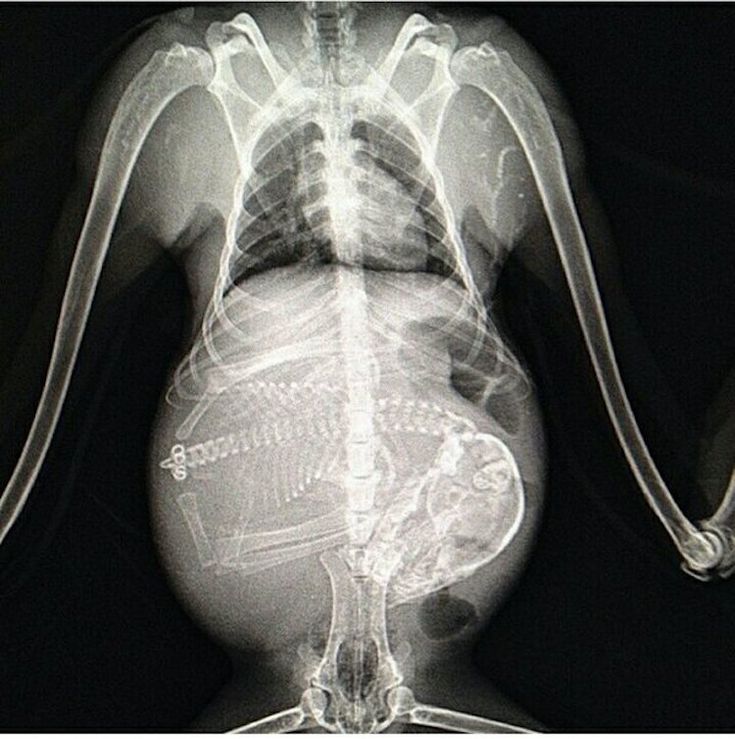 In addition to the hospital or clinic’s specialized staff, physicians may access resources from or contact the following organizations for assistance in estimating fetal radiation dose.
In addition to the hospital or clinic’s specialized staff, physicians may access resources from or contact the following organizations for assistance in estimating fetal radiation dose.
- The National Council on Radiation Protection and Measurementsexternal icon’ Report No. 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013] provides detailed information for assessing fetal doses from internal uptakes.
- The International Commission on Radiological Protection’s “Publication 84: Pregnancy and Medical Radiation”external icon [ICRP2000] provides fetal dose estimations from medical exposures to pregnant women.
- The Conference of Radiation Control Program Directorsexternal icon maintains a list of state Radiation Control/Radiation Protection program contact information.
- The Health Physics Societyexternal icon maintains a list of active certified Health Physicists.
- The American Association of Physicists in Medicineexternal icon provides information resources.
Once the fetal radiation dose is estimated, potential health effects can be assessed.
Potential Health Effects of Prenatal Radiation Exposure (Other Than Cancer)
Table 1 summarizes the potential non-cancer health risks of concern. This table is intended to help physicians advise pregnant women who may have been exposed to radiation, not as a definitive recommendation. The indicated doses and times post-conception are approximations.
| Acute Radiation Dose* to the Embryo/Fetus | Time Post Conception (up to 2 weeks) | Time Post Conception (3rd to 5th weeks) | Time Post Conception (6th to 13th weeks) | Time Post Conception (14th to 23rd weeks) | Time Post Conception (24th week to term) |
|---|---|---|---|---|---|
<0. 10 Gy 10 Gy (10 rads) | Noncancer health effects NOT detectable | ||||
| 0.10–0.50 Gy (10–50 rads) | Failure to implant may increase slightly, but surviving embryos will probably have no significant (non-cancer) health effects. | Growth restriction possible | Growth restriction possible | Noncancer health effects unlikely | |
| > 0.50 Gy (50 rads) The expectant mother may be experiencing acute radiation syndrome in this range, depending on her whole-body dose. | Failure to implant will likely be high, depending on dose, but surviving embryos will probably have no significant (non- cancer) health effects. | Probability of miscarriage may increase, depending on dose. Probability of major malformations, such as neurological and motor deficiencies, increases. Growth restriction is likely | Probability of miscarriage may increase, depending on dose. Growth restriction is likely. | Probability of miscarriage may increase, depending on dose. Growth restriction is possible, depending on dose. (Less likely than during the 6th to 13th weeks post conception) Probability of major malformations may increase | Miscarriage and neonatal death may occur, depending on dose. § |
| 8th to 25th Weeks Post Conception: The most vulnerable period for intellectual disability is 8th to 15th weeks post conception Severe intellectual disability is possible during this period at doses > 0.5 Gy Prevalence of intellectual disability (IQ<70) is 40% after an exposure of 1 Gy from 8th to 15th week Prevalence of intellectual disability (IQ<70) is 15% after an exposure of 1 Gy from 16th to 25th week Table adapted from Table 1.1. of the National Council on Radiation Protection and Measurements’ Report No. | |||||
Gestational age and radiation dose are important determinants of potential non-cancer health effects. The following points are of particular note.
- During the first 2 weeks post-conception, the health effect of concern from an exposure of ≥ 0.1 Gy is the possibility of death of the embryo. Because the embryo is made up of only a few cells, damage to one cell, the progenitor of many other cells, may cause the death of the embryo, and the blastocyst may fail to implant in the uterus. Embryos that survive, however, are unlikely to exhibit congenital abnormalities or other non-cancer health effects, no matter what dose of radiation they received.
- In all stages post-conception, radiation-induced non-cancer health effects are not detectable for fetal doses below about 0.10 Gy.
Carcinogenic Effects of Prenatal Radiation Exposure
Radiation exposure to an embryo/fetus may increase the risk of cancer in the offspring, especially at radiation doses > 0. 1 Gy, which are well above typical doses received in diagnostic radiology. However, attempting to quantify cancer risks from prenatal radiation exposure presents many challenges. These challenges include the following:
1 Gy, which are well above typical doses received in diagnostic radiology. However, attempting to quantify cancer risks from prenatal radiation exposure presents many challenges. These challenges include the following:
- The primary data for the risk of developing cancer from prenatal exposure to radiation come from the lifespan study of the Japanese atomic bomb (A-bomb) survivors. [Preston et al. 2008]. The analysis of that cohort includes cancer incidence data only up to the age of 50 years. This precludes making lifespan risk estimates as a result of prenatal radiation exposure.
- From the Japanese lifespan study [Preston et al. 2008], it can be concluded that for those exposed
in early childhood (birth to age 5 years), the theoretical risk of an adult-onset cancer by age 50 is approximately ten-fold greater than the risk for those who received prenatal exposure. Therefore, the risk following prenatal exposure may be considerably lower than for radiation exposure in early childhood
[NCRP2013].
- No reliable epidemiological data are available from studies to determine which stage of pregnancy is the most sensitive for radiation-induced cancer in the offspring [NCRP2013].
The lifespan study of the Japanese A-bomb survivors is continuing as the cohort ages. Future analyses of the accumulating data should provide a better understanding of the lifetime risk of cancer from prenatal and early childhood radiation exposure.
References
ICRP2000] International Commission on Radiological Protection. 2000. Valentin, J. (2000). Pregnancy and medical radiation. Oxford: Published for the International Commission on Radiological Protection.
[NCRP2013] National Council on Radiation Protection and Measurements. 2013. Preconception and Prenatal Radiation Exposure Health Effects and Protective Guidance. (2013). Bethesda: National Council on Radiation Protection & Measurements.
Preston DL, Cullings H, Suyama A, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K, Kasagi F, Shore RE. 2008. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428-436.
2008. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428-436.
[UNSCEAR2013] United Nations Scientific Committee on the Effects of Atomic Radiation. 2013. Sources, effects and risks of ionizing radiation. Vol. II, Scientific Annex B: Effects of radiation exposure of children.
For more information on medical management and other topics on radiation emergencies:
Radiation Emergency Assistance Center/Training Siteexternal icon (REAC/TS) is a program uniquely qualified to teach medical personnel, health physicists, first responders and occupational health professionals about radiation emergency medical response.
Radiation Emergency Medical Management (REMM)external icon provides guidance to health care providers (primarily physicians) about clinical diagnosis and treatment of radiation injury during radiological and nuclear emergencies.
Conference of Radiation Control Program Directorsexternal icon
Health Physics Societyexternal icon
International Commission on Radiological Protectionexternal icon
National Council on Radiation Protection and Measurementsexternal icon
American Association of Physicists in Medicineexternal icon
Radiation and pregnancy
Topics
In This Topic
Radiation is a kind of energy. It travels as rays or particles in the air. Radiation can attach itself to materials like dust, powder or liquid. These materials can become radioactive, which means that they give off radiation.
You are exposed to (come in contact with) small amounts of radiation nearly every day. This radiation comes from natural sources (like sun rays) and man-made sources (like microwave ovens and medical X-rays). These kinds of radiation don’t cause serious harm. However, radiation emergencies, like a nuclear power plant accident, may expose you to larger, more dangerous amounts of radiation. This may cause harm to you and your baby.
If you think you've been exposed to large amounts of radiation, tell your health care provider immediately.
How can you protect yourself and your baby from radiation during pregnancy?
Tell any health care provider you see, including your dentist, that you’re pregnant before you get an X-ray or other tests that use radiation, like computed tomography (also called CT or CAT scan). CT scans use special X-ray equipment and powerful computers to make pictures of the inside of your body. Most X-rays are safe to get during pregnancy. But if you’re pregnant and need an X-ray or a CT scan of your belly, your provider may want to wait until your baby’s born, modify the test to reduce the amount of radiation or use another test that doesn't use radiation, like ultrasound. You and your provider can decide what treatment is best for you.
If you work with radiation at your job, talk to your boss. Tell him that you’re pregnant. You may be able to change job responsibilities to help keep you and your baby safe during pregnancy.
If you've been in a radiation emergency with possible exposure to large amounts of radiation, follow these guidelines from the Centers for Disease Control and Prevention (also called CDC):
- Get inside.
 Get to the middle of a building or a basement, away from doors and windows. Bring pets inside.
Get to the middle of a building or a basement, away from doors and windows. Bring pets inside. - Stay inside. Close and lock windows and doors. Take a shower or wipe any exposed parts of your body with a damp cloth. Drink bottled water and eat food in sealed containers.
- Stay tuned. Use radios, TVs, computers and mobile devices to get current information from officials in your area.
If you think you’ve been exposed to large amounts of radiation, tell your health care provider immediately.
How does radiation affect you and your baby during pregnancy?
During pregnancy, your body protects your baby from most radiation that you’re exposed to every day. Most babies born to moms who come in contact with low amounts of radiation during pregnancy aren’t at increased risk for birth defects. A birth defect is a health condition that a baby has at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, in how the body develops, or in how the body works.
If you swallow or breathe in radioactive material during pregnancy, it can get into your bloodstream and pass through the umbilical cord to your baby. It also can build up in areas of your body that are close to your uterus (womb), such as your bladder. The effect on your baby depends on the amount of radiation your body takes in, the kind of radiation it is, and the length of time you’re in contact with it. Your baby is most sensitive to radiation between 2 and 18 weeks of pregnancy. Exposure to radiation during pregnancy can:
- Slow your baby’s growth
- Cause birth defects
- Affect your baby’s brain development
- Cause cancer in your baby
- Cause miscarriage. This is the death of a baby in the womb before 20 weeks of pregnancy.
Exposure to large amounts of radiation, equal to having more than 500 chest X-rays at one time, is not common. It did happen to women in Japan after the atomic bombs dropped on Hiroshima and Nagasaki in 1945.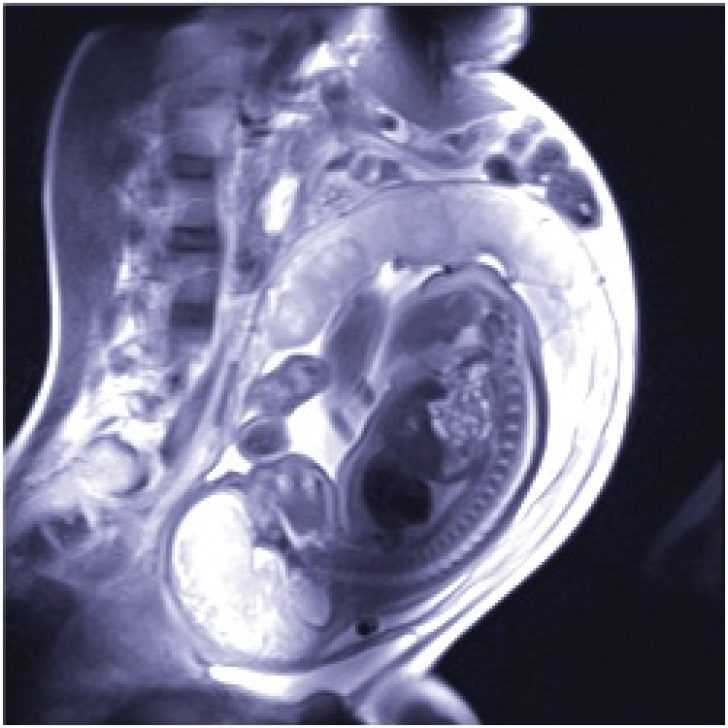 If you do come in contact with large amounts of radiation, you may not feel sick, but the radiation may cause serious problems in your baby
If you do come in contact with large amounts of radiation, you may not feel sick, but the radiation may cause serious problems in your baby
Exposure to extremely large amounts of radiation, equal to having more than 5,000 chest X-rays at one time, also is not common. It did happen to women in the Chernobyl nuclear power plant accident in the Ukraine in 1986. If you do come in contact with extremely large amounts of radiation, you may show signs of radiation sickness, including:
- Vomiting, diarrhea, bloody stools
- Fever
- Fatigue (being really tired)
- Hair loss
Contact your health care provider immediately if you think you’ve been exposed to large amounts of radiation.
Last reviewed: December, 2014
') document.write('
Nutrition, weight & fitness
') document.write('') }
') document. write('') }
write('') }
Is X-ray examination dangerous during pregnancy - MEDSI
01/15/2018
Is X-ray examination dangerous during pregnancy
X-ray examinations are carried out to determine the presence of any pathologies, neoplasms or diseases. For this, a directed beam of electromagnetic waves of a given length and frequency is used. It passes through human organs, the tissues of which reflect and absorb it in different ways.
Due to this difference, various anomalies can be seen. The result is sent to the screen or recorded on a special film.
During a preventive examination, this examination is carried out in a special room. In case of injury to the patient, it can be used immediately in the emergency department, operating room or intensive care unit.
Influence of irradiation on the fetus
X-rays in general are not always beneficial for the body, as it destroys those of its cells that are in a state of constant division.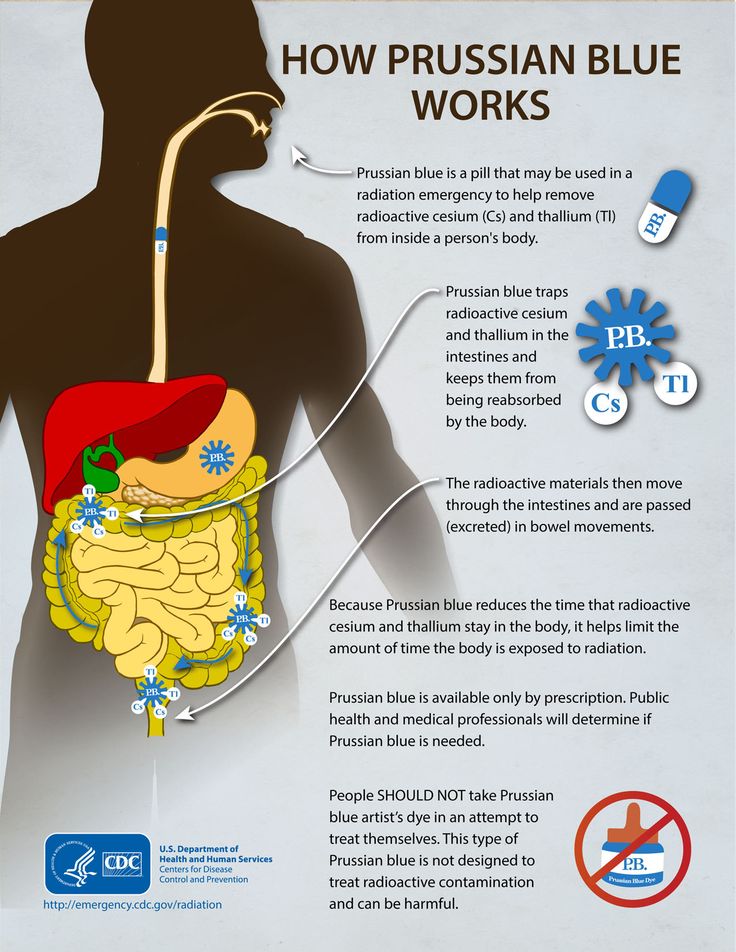 This leads to the destruction or mutation of DNA chains.
This leads to the destruction or mutation of DNA chains.
There are not many such newly formed cells in the body of an adult. But in the fetus in the early stages of development, they are the basis. Therefore, such an examination is quite dangerous for him. The most likely occurrence of complications when using x-rays during pregnancy in its first trimester (initial 12 weeks).
What problems can X-rays cause in early pregnancy?
Due to the gradual development of the fetus, in each week of its existence, the formation of future systems of the child's body takes place. Therefore, the mother's body receiving a large amount of X-rays at these stages can have various serious consequences:
- The first two weeks. Possible death of the embryo, miscarriage, ectopic pregnancy.
- Weeks three and four. Pathologies at an early stage of fetal development, miscarriage.
- Fifth-sixth weeks. Disturbances in the development of a number of organs and systems: thyroid, thymus and gonads; immune, nervous, circulatory, endocrine systems.

- Seventh week. Damage to the liver, intestines. Metabolic disease.
- Eighth. Pathologies of the development of joints and limbs, the oral cavity.
- Ninth week. Damage to the respiratory and reproductive systems.
- Tenth and eleventh weeks. Problems associated with the development of teeth. Heart disease.
- Twelfth week. Pathology of the thyroid gland, disorders of the immune system.
After this period, the effect of radiation on the fetus decreases, but it is still not recommended to do such a study until the end of pregnancy, except in cases of emergency.
X-rays in early pregnancy
Doctors try not to prescribe X-rays to pregnant women, because even a minimal risk of harm from radiation always remains. It is especially great in the first twelve weeks.
The most dangerous tests for the fetus are:
- Abdominal X-ray
- X-ray of the pelvis and spine
- Mammography
- Fluorography
- Computed tomography
- Isotope scanning
Less dangerous X-rays are:
- Chest (lungs, heart)
- Brain
- Limbs
Are there any non-hazardous examinations?
The safest types of X-ray examination are:
- X-ray of teeth
- X-ray of the nose
In these cases, the exposure occurs locally, so the radiation dose is minimal.
The amount of radiation that a fetus can receive in two months is regulated by the Sanitary Rules and Regulations and should not exceed 1 millisievert (mSv).
There are other types of examinations that can be used instead of X-ray during pregnancy:
- MRI
- Visiography
- Ultrasound
Nevertheless, doctors try not to prescribe MRI in the first trimester of pregnancy, since statistical studies are not enough to clarify its safety during this period.
What if X-rays are indispensable?
X-rays for pregnant women may be necessary in a situation where the disease or injury threatens the life and health of the mother and child, and it is impossible to use other diagnostic methods. And the harm from not using x-rays outweighs the potential harm from its use.
- If it is necessary to examine an area that does not touch the pelvis, abdomen or spine, they must be shielded with lead aprons and pads.
- If an X-ray is to be taken directly through the fetus in early pregnancy, the doctor may suggest that it be interrupted to avoid mutations and miscarriage.

- A woman may refuse to have an abortion, but in this case she must understand the risks she is taking and the pathologies that may appear in the fetus.
In all these cases, after passing the examination, it is recommended to go for an ultrasound scan to monitor the condition of the fetus and the appearance of certain pathologies.
If it is possible to postpone the use of x-rays until the last trimester or postpartum, then this should be done.
At the earliest possible time, a woman may not be aware of the pregnancy. Therefore, before x-rays, it is recommended to undergo an additional examination.
Benefits of X-ray analysis at MEDSI:
- 30 x-ray examinations
- The latest equipment with the ability to control the intensity of radiation
- Urgent examination in case of injury or other medical indications
- Technologies suitable for both adults and children
- Radiologists of high qualification categories, candidates of medical sciences
- Appointment for research and consultation by phone 8 (495) 7-800-500
- More than 20 diagnostic centers
Do not delay treatment, see a doctor right now:
- Pregnancy tests
- Planning and management of pregnancy
- Obstetrician-gynecologist appointment
Can X-rays be taken during early and late pregnancy? July 8th, 2016, 08:01 am
Is it possible to do x-rays during early and late pregnancy?
I am often asked the question: is it possible to have X-rays for pregnant women. What are the indications and contraindications for x-rays and what can replace the examination.
What are the indications and contraindications for x-rays and what can replace the examination.
An x-ray may be required if pneumonia or tuberculosis is suspected, when visiting a dental clinic, in case of a broken bone.
X-ray examination is a special method of examination using X-rays to examine a patient for the diagnosis or prevention of diseases, consisting of one or more X-ray procedures.
Irradiation of a pregnant woman has a detrimental effect on actively developing fetal cells and can lead to hydrocephalus (hydrocephalus), microphthalmia (reduction of all sizes of the eyeball), general developmental delay, up to mental retardation in a child. Therefore, preventive X-ray examinations are not allowed for pregnant women.
Due to the potential risk of radiation exposure to the embryo or fetus, which has a particularly high radiosensitivity, radiographic studies during pregnancy should be performed only for very narrow clinical indications with the participation of the attending physician. ("Protection of the population in the appointment and conduct of X-ray diagnostic studies. Guidelines", approved by the Ministry of Health of the Russian Federation on February 6, 2004 N 11-2 / 4-09) . Such indications may be suspicion of acute pneumonia or tuberculosis, complicating pregnancy. In this case, X-ray of the lungs is done after 1st trimester of pregnancy.
("Protection of the population in the appointment and conduct of X-ray diagnostic studies. Guidelines", approved by the Ministry of Health of the Russian Federation on February 6, 2004 N 11-2 / 4-09) . Such indications may be suspicion of acute pneumonia or tuberculosis, complicating pregnancy. In this case, X-ray of the lungs is done after 1st trimester of pregnancy.
- The most dangerous is the irradiation of the fetus in the early stages of its development. Therefore, studies should be conducted during the second half of pregnancy , limited to the third trimester of pregnancy, when there is less chance of negative x-ray exposure to the fetus. An exception is the need to provide emergency or emergency medical care.
- When radiography of areas of the body remote from the fetus (chest, skull or upper limbs), it can be performed at any stage of pregnancy according to clinical indications subject to safety measures (diaphragm and shielding) Guidelines, approved.
 Ministry of Health of the Russian Federation 06.02.2004 N 11-2 / 4-09.
Ministry of Health of the Russian Federation 06.02.2004 N 11-2 / 4-09. - Examination of the pelvic area in pregnant women is carried out only for health reasons.
- X-ray examinations of pregnant women should be carried out using all possible means of protection and methods of dose reduction so that the dose received by the fetus, did not exceed 1.0 mSv in any two months.
- If the fetus receives a dose of exceeding 100 mSv or 0.1 Sv , the doctor must warn the patient about the possible negative consequences of exposure to and recommend termination of pregnancy. Such cases may occur when it is necessary to repeat X-ray examinations (most often fluoroscopy) of the digestive system, urinary tract, pelvic area in severe diseases, when the correct diagnosis and control of treatment are impossible without X-ray examinations.
- If a woman of childbearing age is referred for an x-ray, the referring doctor must specify the time of the last menstrual period.
 X-ray examinations related to radiation exposure to the gonads (examinations of the pelvis, gastrointestinal tract, urinary system) are best done in the first 10 days of the menstrual cycle (unless the examination cannot be postponed for clinical reasons). It is during this period that the probability of pregnancy is the lowest. If pregnancy is suspected, the issue of the admissibility of an X-ray examination is decided on the assumption that there is a pregnancy.
X-ray examinations related to radiation exposure to the gonads (examinations of the pelvis, gastrointestinal tract, urinary system) are best done in the first 10 days of the menstrual cycle (unless the examination cannot be postponed for clinical reasons). It is during this period that the probability of pregnancy is the lowest. If pregnancy is suspected, the issue of the admissibility of an X-ray examination is decided on the assumption that there is a pregnancy.
X-ray of a tooth during pregnancy
It is advisable to treat your teeth at the planning stage of pregnancy, but if you are pregnant and you have certain dental problems that require an X-ray of the tooth, then it is best to choose the second trimester of pregnancy. In this case, the radiation dose from an x-ray at a dentist - equal to 0.15-0.35 mSv (on average 0.2 mSv) does not exceed the permissible dose, while the focus of inflammation in the oral cavity can threaten the development of infection and adversely affect the development of the fetus .

 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013].
174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013].