Cervical infections during pregnancy
Bacterial vaginosis and pregnancy
Donate
Contact
Events
DONATE
- Home >
- Complications & Loss >
- Pregnancy complications > Bacterial vaginosis and pregnancy
Topics
In This Topic
KEY POINTS
Bacterial vaginosis (BV) is a common infection that’s easily treated, but it can cause problems for your baby during pregnancy.
Having BV during pregnancy can increase your baby’s risk for premature birth and low birthweight.
BV can increase your risk for pelvic inflammatory disease, which can cause problems if you’re trying to get pregnant.
BV isn’t a sexually transmitted infection, but it is common in sexually active women.
Getting treated for BV during pregnancy can help protect your baby.
What is bacterial vaginosis?
Bacterial vaginosis (also called BV or vaginitis) is an infection caused when there’s too much of certain bacteria in the vagina. It’s the most common vaginal infection in women ages 15 to 44.
BV is not a sexually transmitted infection (also called STI, sexually transmitted disease or STD), but it is common in sexually active women and it rarely happens to women who haven’t had sex. An STI is an infection you can get from having unprotected sex or intimate physical contact with someone who is infected. If you have BV that’s not treated, it can increase your risk of getting an STI. It’s important to have any infection treated during pregnancy to help protect you and your baby.
What causes BV?
We don’t know for sure what causes BV. Any woman can get it, but you’re at increased risk for BV if you:
- Have new sex partners
- Have more than one sex partner
- Douche (use water or other liquid to clean inside the vagina)
- Are pregnant
- Are African-American. BV is twice as common in African-American women than in white women.
- Have an intrauterine device (also called IUD), especially if you have irregular bleeding. An IUD is a kind of birth control. It's a t-shaped piece of plastic that's placed in your uterus that helps prevents prevent pregnancy.
How can BV affect pregnancy?
The Centers for Disease Control and Prevention (also called CDC) estimates that 1 million pregnant women get BV each year. Pregnant women are at increased risk for BV because of hormone changes that happen during pregnancy. Hormones are chemicals made by the body.
If you have BV during pregnancy, your baby is at increased risk for premature birth and low birthweight. Premature birth is birth before 37 weeks of pregnancy. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces. Being born too early or too small can cause health problems for your baby.
Premature birth is birth before 37 weeks of pregnancy. Low birthweight is when your baby is born weighing less than 5 pounds, 8 ounces. Being born too early or too small can cause health problems for your baby.
BV also can cause pelvic inflammatory diseases (also called PID). PID is an infection in the uterus that can increase your risk for infertility (not being able to get pregnant).
How can you reduce your risk for BV?
Here are some things you can do to help protect yourself from BV:
- Don’t have sex. BV isn’t an STI, but you’re more likely to get it if you have sex than if you don’t.
- Limit the number of sex partners you have. Have sex with only one person who doesn’t have other sex partners.
- Use a condom every time you have sex. Condoms are barrier methods of birth control. Barrier methods help prevent pregnancy (and STIs) by blocking or killing your partner’s sperm. Other kinds of birth control, like the pill and implants, don’t protect you from STIs.

- Don’t douche. Douching can remove normal bacteria in your vagina that can help protect you from infection.
- Use warm water only and no soap to clean the outside of your vagina. Always wipe front to back.
What are the signs and symptoms of BV?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Many women with BV have no signs or symptoms, but you may have:
- Thin white or grey vaginal discharge
- Strong, fishy odor, especially after having sex
- Pain, itching or burning in the vagina
- Itching around the outside of the vagina
- Burning feeling when you urinate
If you think you may have BV, tell your health care provider right away. Your provider can check your vagina for signs of vaginal discharge and test a sample of vaginal fluid for bacteria associated with BV.
BV is treated with antibiotics. Antibiotics are medicines that kill infections caused by bacteria. The antibiotic may be oral (taken by mouth) or a cream or gel that you put into your vagina. Treatment with antibiotics for BV is safe for your baby during pregnancy, and it may help reduce your risk for STIs.
If you have BV:
- Take all your medicine exactly as your provider tells you to. Take all of it even if you have no signs or symptoms.
- If you have female sex partners, tell them you have BV so they can get tested and treated.
- Don’t have sex until you finish your treatment.
- Tell your provider if you have signs or symptoms after you finish your treatment.
More information
- Bacterial vaginosis—CDC fact sheet
- Bacterial vaginosis fact sheet from womenshealth.gov
- Vaginitis FAQ from the American College of Obstetricians and Gynecologists
Last reviewed: January, 2018
') document. write('
write('
Preterm labor & premature birth
') document.write('') }
') document.write('
The newborn intensive care unit (NICU)
') document.write('') }
Infections in pregnancy and how they affect the baby
During pregnancy, people may worry more about contracting infections and how they might affect the developing baby.
Vaginal infections, including yeast infections, are common during pregnancy and are usually not a cause for concern. Uterine infections may produce more complications, however.
This article looks at common infections during pregnancy, how they might affect the baby, and how to prevent them from developing.
Someone who is pregnant might be more vulnerable to certain infections and may develop more severe complications if the infections are left untreated. Anyone who has even a minor infection during pregnancy should talk to a doctor or midwife.
Anyone who has even a minor infection during pregnancy should talk to a doctor or midwife.
Typical vaginal infections during pregnancy include:
Vaginal yeast infections
Vaginal yeast infections are caused by a fungus called Candida. These infections tend to occur during pregnancy because of changes in the immune system, increased production of glycogen, and higher estrogen levels.
According to a 2015 report, about 20 percent of all women have Candida, which rises to 30 percent during pregnancy. It appears to be more common during the second and third trimesters.
The most common symptoms of a vaginal yeast infection include:
- itchiness around the vagina or vulva
- a thick, white, cottage cheese-like vaginal discharge
- an odor of bread or beer coming from the vagina
- pain or burning in or around the vagina
- pain or burning during sexual intercourse
People can use prescription or over-the-counter medications to treat a vaginal yeast infection. However, anyone who is pregnant should not use these drugs without first talking to a doctor or midwife.
However, anyone who is pregnant should not use these drugs without first talking to a doctor or midwife.
It is essential to get a diagnosis before beginning treatment as other infections, such as bacterial vaginosis and chlamydia, can be confused with yeast infections.
Bacterial vaginosis
Bacterial vaginosis (BV) is an easily treated bacterial infection in the vagina. Symptoms include:
- itching, burning, or pain in the vagina or vulva
- a fishy odor coming from the vagina
- a bad smell that gets worse after sexual intercourse
- a large amount of thin, grey colored discharge
If BV is left untreated during pregnancy, it might cause preterm labor, premature birth, and lower birth weight babies.
Group B Streptococcus (GBS)
Group B streptococcus (GBS) is a group of bacteria that come and go in the body but often frequent the vagina and rectum. They do not typically cause symptoms or even an infection. However, women who have GBS in their bodies when they give birth may pass it to their babies.
Mothers who have GBS will pass it on to their babies in 1 to 2 percent of cases. Although uncommon, GBS in a newborn can be fatal.
Testing between the beginning of week 36 and the end of week 37 of pregnancy can detect GBS and is a standard part of most prenatal care.
Treatment with antibiotics through a needle in a vein (IV antibiotics) can significantly reduce the risk of a GBS infection passing to the baby.
An infection in the uterus can be dangerous for a variety of reasons. The infection may affect the placenta, harm the developing baby, cause premature labor, or lead to birth abnormalities.
Uterine infections can also make labor more dangerous and difficult. Some individuals experience organ failure and other life-threatening complications.
Uterine infections often develop when bacteria from the vagina travels to the uterus, so an untreated vaginal infection is a risk factor for uterine infections. A person is more susceptible to uterine infections if their membranes rupture during an extended labor.
Treatment includes antibiotics and may require hospitalization. If a fever develops during labor, a doctor or midwife will monitor the fetus. If the symptoms are severe, the doctor may recommend a cesarean delivery.
Pregnancy causes many changes in the body, making people more susceptible to complications from many infections.
For example, hormone-related skin changes during pregnancy can cause conditions such as eczema or severely dry skin. If the skin cracks open and bleeds, a serious skin infection, such as cellulitis, can develop. A rare skin disorder called Sweet’s syndrome is also more common during pregnancy than at other times.
Some other infections that may be more serious during pregnancy include:
- the flu
- hepatitis E, which is a typically mild viral form of hepatitis
- herpes, including herpes simplex virus (HSV) and varicella zoster virus (VZV)
- Listeria, which can cause food poisoning
- measles
- HIV
The increased risk of these infections during pregnancy is not well understood but may be due to hormone and other changes that alter the number of blood cells in the body. For example, late in pregnancy, T cells that help fight infection decrease in number.
For example, late in pregnancy, T cells that help fight infection decrease in number.
Pregnancy also causes increased blood circulation and demands on the heart. These demands can also worsen complications. For example, if a pregnant person develops pneumonia from the flu, they may have more difficulty breathing because of the increased demands the fetus places on the heart and lungs.
Some medications that can effectively treat common infections may be less safe during pregnancy. So it is essential that pregnant people who have an infection talk to their doctor or midwife to weigh up the benefits and risks of various treatment options.
Numerous infections can affect the developing baby. However, it is difficult for doctors to tell whether and to what extent a fetus will be affected.
Infections can affect a developing baby in one of three ways:
- They may harm the mother, making her body less able to nurture the baby or requiring the use of drugs that may harm a fetus.

- They can directly harm the baby by causing changes that lead to birth abnormalities.
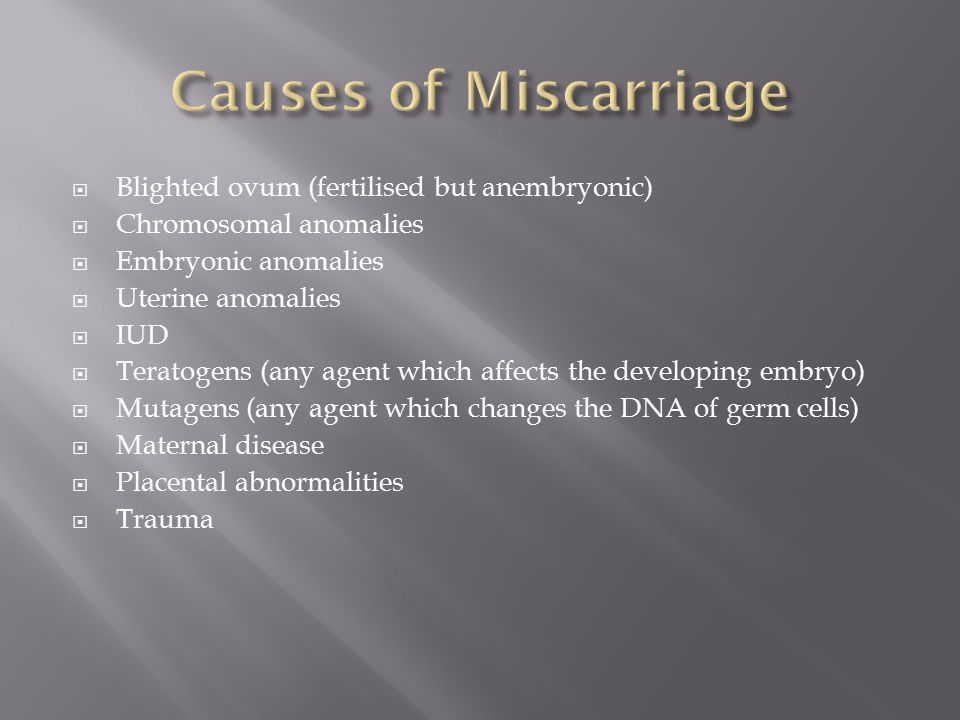
- They can trigger premature labor or a miscarriage.
According to the National Institutes of Health (NIH), infections that are known to harm the developing baby include, but are not exclusive to:
- bacterial vaginosis, which might cause preterm labor
- contagious diseases, such as hepatitis, syphilis, herpes, and HIV, which can infect the fetus
- chlamydia, which can cause eye infections and pneumonia
- gonorrhea, which can contaminate the amniotic fluid, cause preterm labor, and lead to eye infections and possible blindness
- fifth disease, which can trigger a miscarriage or cause fetal anemia
- group B streptococcus, which can cause severe complications in newborns, and in rare cases can be fatal
- toxoplasmosis, which can cause birth abnormalities and intellectual disabilities
- Listeria, which can cause miscarriage, stillbirth, and birth abnormalities
- cytomegalovirus, which is often harmless but can also cause birth abnormalities and intellectual disabilities
- Zika, which is usually mild, can cause pregnancy loss or birth abnormalities in an infant
Zika infection, which is a disease carried by mosquitoes, may cause birth abnormalities and increase the risk for stillbirths and miscarriages in those who have the virus.![]() However, it is unclear why some fetuses are affected, and others are not.
However, it is unclear why some fetuses are affected, and others are not.
Other infections may also harm a developing baby, depending on the overall health of the pregnant person, when the infection developed, and whether the person has received treatment.
The Centers for Disease Control and Prevention (CDC) provide some strategies to reduce the risk of developing an infection during pregnancy, including:
- avoiding travel to areas where Zika is prevalent, and using bug spray to prevent mosquito bites
- using a condom and asking a partner to be tested for sexually transmitted infections (STIs)
- washing hands carefully and diligently
- avoiding people who have contagious infections
- getting a flu shot
- avoiding unpasteurized foods
- asking someone else to change the cat litter
- testing for STDs and group B strep
Most people who experience an infection during pregnancy will not experience complications. Prompt treatment increases the likelihood of a healthy birth.
Anyone who experiences any unusual symptoms during their pregnancy should talk to their doctor or midwife. Prenatal care is also crucial since it can detect certain infections even before they cause symptoms.
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
other gynecological operations
07.
Telemedicine for adults
08. examinations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Treatment of inflammation of the cervix (cervicitis) at any stage in the Primorsky district of St. Petersburg
- Symptoms of disease
- Disease diagnosis
- Treatment of disease
Inflammation of the cervix (cervicitis) is an inflammation of the tissue of the inner wall of the uterus (endometrium). As a rule, it is accompanied by infections that are sexually transmitted, for example, chlamydia, trichomoniasis, genital herpes, gonorrhea.
As a rule, it is accompanied by infections that are sexually transmitted, for example, chlamydia, trichomoniasis, genital herpes, gonorrhea.
TREATMENT OF CERVICAL INFLAMMATION AVAILABLE IN BRANCHES:
Treatment of cervical inflammation in Primorsky district
Address: St. Petersburg , Primorsky district, Repishcheva, 13
Treatment of inflammation of the cervix in the Petrogradsky district
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
Treatment of inflammation of the cervix in Vsevolozhsk
Address: Vsevolozhsk , Oktyabrsky Ave, 96
Symptoms of inflammation of the cervix
Symptoms of inflammation of the cervix, caused, for example, by chlamydia pathogens, are:
- clear or yellowish vaginal discharge;
- itching;
- redness;
- may experience pain during urination.
In addition to genital infections, inflammation can be caused by various pathogens, such as E. coli, streptococci, staphylococci, gonococci.
coli, streptococci, staphylococci, gonococci.
Symptoms of the disease are often blurred and because of this, a woman may not see the problem for a long time and not go to the doctor.
In some cases, inflammation of the cervix can be caused by various injuries, including prolapse of the vagina, rupture of the cervix during childbirth. Inflammation can occur due to infections that have penetrated as a result of abortions and diagnostic curettage. It is also believed that inflammatory processes in the cervix can occur due to allergies to intimate hygiene products, latex condoms.
The weakening of the immune system can also be the cause of inflammatory processes.
Diagnosis of inflammation of the cervix
Inflammation of the vaginal part of the cervix, the exocervix, is called exocervicitis, and on examination is detected as redness of the mucous membrane that covers this part of the cervix. Inflammation of the cervical canal is called endocervicitis.
Diagnosis of inflammation of the cervix, usually accompanied by a determination of the degree of complexity of the disease:
- Acute inflammation of the cervix is a fresh and actively developing infection in the body.
- Chronic inflammation of the cervix - occurs if the infection that caused the inflammation of the cervix is not cured and destroys tissues for a long time.
- Purulent inflammation of the cervix - means that inflammation is accompanied by suppuration in the cervical canal, the presence of purulent cervicitis among expectant mothers increases the risk of disruption of the normal course of the entire pregnancy and subsequent childbirth.
- Viral inflammation of the cervix - the cause of inflammation is a sexually transmitted virus.
- Bacterial inflammation of the cervix - the cause of inflammation is a bacterial infection (gonorrhea, bacterial vaginosis).
- Candidal inflammation of the cervix - the cause of inflammation is a fungal infection.

- Non-specific inflammation of the cervix - inflammation of the cervix arose as a result of a change in the microflora.
- Cystic inflammation of the cervix - the cause of the disease is a combination of viral and bacterial lesions, which leads to the growth of columnar epithelium (cylindrical cells that make up the mucous membrane) along the surface of the uterus, which leads to the formation of cysts.
- Atrophic inflammation of the cervix - inflammation is accompanied by thinning of the tissues of the cervix (with chronic cervicitis, cervical erosion, cystitis, inflammation of the appendages).
- Focal inflammation of the cervix - inflammation manifests itself in certain areas of the mucous membrane of the cervix.
Inflammation of the cervix during pregnancy
The presence of inflammation of the cervix during pregnancy increases the risk of complications during childbirth. The inflammation itself, as well as the disease that caused it, can cause premature birth, infection of the fetus and the development of various forms of diseases in it.
In early pregnancy, inflammation can lead to fetal failure and miscarriage. In the later stages - to intrauterine growth retardation and infection of the child.
The possibility of getting pregnant in the presence of inflammation of the cervix is also low, since the disease is complex and affects the entire reproductive system of a woman.
Treatment of inflammation of the cervix
Particular attention should be paid to the fact that the absence of treatment of inflammation of the cervix can lead to the appearance of erosions and spread of infection to the upper genital organs.
When choosing a treatment for inflammation of the uterus, the stage of inflammation, set during the examination by a doctor, is taken into account.
For the treatment of inflammatory processes, antiviral, antibacterial and other agents are used, taking into account the causes of the disease, the nature of the pathogen and its sensitivity to the selected drug. It is also possible to use local preparations: creams and suppositories.
It is also possible to use local preparations: creams and suppositories.
In chronic stages of the disease, surgical interventions (such as laser therapy, cryotherapy, diathermocoagulation) may be required.
It is very important to note that along with the treatment of inflammation of the cervix, comorbidities must also be treated. And for the effectiveness of treatment, it is necessary to simultaneously examine and treat the sexual partner.
If there is a suspicion of inflammatory processes in the cervix, as well as in the presence of characteristic symptoms (very painful PMS), you should consult a gynecologist. In addition, you may need to consult a urologist.
Do not wait for the disease to go away by itself! Do not self-medicate.
In our clinic you can undergo a complete examination and the necessary course of treatment at the modern level, get recommendations and advice from highly qualified specialists.
Reception is conducted by doctors:
Choose the Dynasty branch on Novocherkassky avenue, Krasnogvardeisky district Dynasty on Lenina street, Petrogradsky district Dynasty on Repishcheva street, Primorsky district Dynasty in Vsevolozhsk Field service
Children’s specialists
Consults online
Abazyan Lilit Gagikovna
Obstetrician-gynecologist, gynecologist-endocrinologist, first category
Atajanyan Anna Sarikovna
Obstetrician-gynecologist, gynecologist-endocrinologist, ultrasound specialist
Ivanova Ekaterina Alekseevna
Obstetrician-gynecologist
Krisanenko Julia Georgievna
Obstetrician-gynecologist
Najaryan Marine Tigranovna
Obstetrician-gynecologist
Sadovaya Natalya Dmitrievna
Obstetrician-gynecologist
Samarina Olga Vladimirovna
Obstetrician-gynecologist, gynecologist-endocrinologist
Foos Oksana Vyacheslavovna
Obstetrician-gynecologist, gynecologist-endocrinologist








/cdn.vox-cdn.com/uploads/chorus_asset/file/9892303/tpc5.png)


