Burping a lot pregnant
7 Safe Home Remedies for Gas During Pregnancy
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Got gas while pregnant? You’re not alone. Gas is a common (and potentially embarrassing) symptom of pregnancy.
You’re likely paying special attention to what you eat and the medications you ingest right now, which often means that typical gas remedies should be shelved for the time being.
Fortunately, there are several home remedies that can help ease any gas troubles you’re having, and some are as easy as reaching for a tall glass of water.
Your body goes through many changes during pregnancy, and unfortunately gas is an uncomfortable result of some very normal body processes, says Sheryl Ross, MD, an OB/GYN and women’s health expert at Providence Saint John’s Health Center in Santa Monica, California.
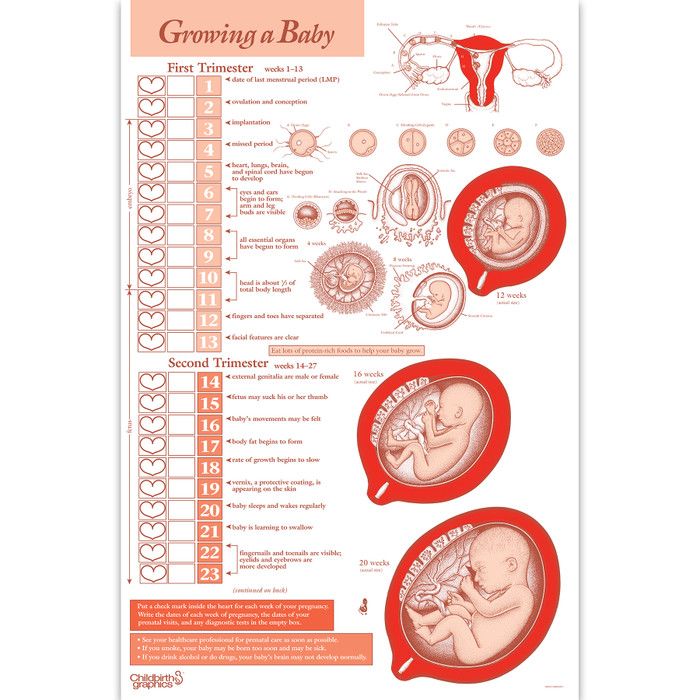
The hormone progesterone is one of the main causes of excess gas during pregnancy. As your body produces more progesterone to support your pregnancy, progesterone relaxes muscles in your body.
This includes the muscles of your intestine. Slower moving intestine muscles mean that your digestion slows down. This allows gas to build up, which in turn leads to bloating, burping, and flatulence.
This allows gas to build up, which in turn leads to bloating, burping, and flatulence.
Learn more about how your body changes during pregnancy.
Once you get further along in your pregnancy, the increased pressure from your growing uterus on your abdominal cavity can slow down digestion, leading to more gas.
Some foods can also contribute to gas, and your prenatal vitamins (especially the iron component) can cause constipation, leading, you guessed it, to even more gas.
This uncomfortable, and sometimes painful, gas is generally due to constipation, and it can get worse as your pregnancy progresses.
Thankfully, there are various things you can do to combat the gas. The more consistent you are with these lifestyle changes, the better results you’re likely to see.
1. Drink plenty of fluids
Water is your best bet. Aim for eight to 10 (8-ounce) glasses every day, but other fluids count too.
If your gas is causing pain or extreme bloating, you may have irritable bowel syndrome (IBS), in which case make sure any juice you drink is low in certain types of gas and bloating-promoting sugars called FODMAPs.
Cranberry, grape, pineapple, and orange juice are all considered low-FODMAP juices.
Be sure to monitor sugar intake when drinking juices and sodas, especially if you’re at an increased risk for developing gestational diabetes.
Also, many varieties of carbonated drinks can lead to more gas.
2. Get moving
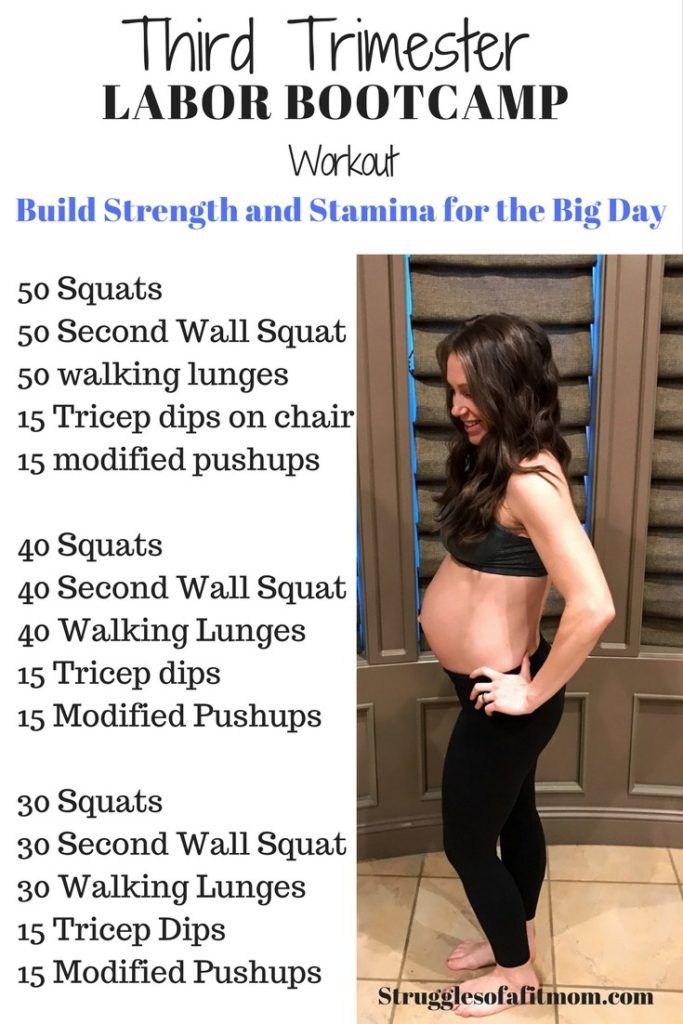
Physical activity and exercise should be a part of your daily routine. If you can’t make it to a gym, add a daily walk to your routine. Aim to walk or exercise for at least 30 minutes.
Not only can exercise help keep you physically and emotionally fit, but it can also help prevent constipation and speed up digestion.
Be sure to consult your obstetrician first before starting any exercise regimen during pregnancy.
Learn more about how to safely exercise in the third trimester of pregnancy.
3. Test out your diet
Try removing potential food triggers from your diet one at a time, until your gas symptoms improve, recommends Brett Worly, MD, an assistant professor in the OB/GYN department at the Ohio State University Wexner Medical Center.
It’s recommended that you continue to eat a balanced diet while doing any form of elimination diet.
Weight gain is necessary for most pregnancies, so it’s important to avoid restrictive diets.
That way, you’re only eliminating foods that are contributing to the problem. Brussels sprouts, cabbage, broccoli, wheat, and potatoes are common gas culprits, says Worly.
Some women experience IBS during pregnancy, but talk with your doctor and dietitian before starting a low-FODMAP diet.
This diet can be very restrictive and put you and your baby at risk for not getting adequate nutrition.
4. Fill up on fiber
Many foods that make gas worse in the short term can actually help manage constipation.
Why? “Fiber brings water into the intestines, softening the stool and allowing it [to pass more easily],” explains Ross.
Try including 25 to 30 grams of high fiber foods into your diet to help ease gas concerns.
Many fruits, such as prunes, figs, and bananas, and vegetables as well as whole grains like oats and flax meal are all good fiber boosters to consider.
5. Ask about fiber supplements
If you’re not a fan of high fiber foods, or you’re looking for a quick and easy alternative, ask your doctor about whether a fiber supplement, such as psyllium (Metamucil), methylcellulose (Citrucel), or polyethylene glycol 3350 (MiraLAX), might benefit you.
You can buy Metamucil, Citrucel, or MiraLAX online.
6. … And stool softeners
Docusate (Colace), a gentle stool softener, moistens the stool, allowing easier and regular passage. Only take docusate if you’re experiencing constipation or having too much gas.
Ross encourages women to take 50 to 100 mg of docusate two times a day throughout the duration of their pregnancy.
It’s important to avoid any stimulant laxatives, such as sennosides (Ex-Lax, Senokot), as these can cause complications during pregnancy.
7. When in doubt, just breathe
Anxiety and stress can increase the amount of air you swallow, which may increase upper abdominal gas, bloating, and belching, says Michael R. Berman, MD, medical director of labor and delivery at Mount Sinai Beth Israel Medical Center.
Berman, MD, medical director of labor and delivery at Mount Sinai Beth Israel Medical Center.
Try to eliminate as much stress from your life as possible. Here are several recommendations:
- Assign chores to someone else, or allow yourself to accept that they may not get done at a specific time — or at all — and that’s OK.
- Find some quiet time during the day to take some deep breaths and relax, or look into a prenatal spa day.
- Do whatever you need to do to stay calm.
Gas isn’t always a laughing matter.
To ensure something more serious isn’t going on, seek immediate medical attention if you have severe pain without improvement for more than 30 minutes or constipation for more than 1 week.
Otherwise, choose the remedies that work best for your lifestyle. Then stick with them because consistency is key.
“Pregnancy is not a sprint; it’s a marathon,” says Ross. “So pace yourself and keep a healthy and positive attitude as it relates to your diet and exercise. ”
”
Causes & Overcoming Excessive Burping In Pregnancy
- Home
- Pregnancy
- Nutrition
- How to ease excessive burping during pregnancy & what are the causes?
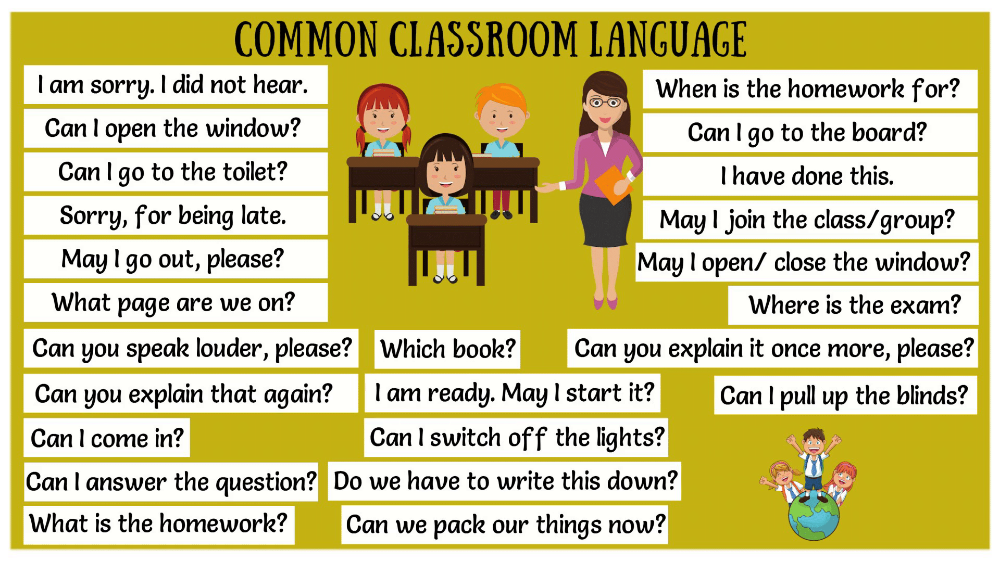
During pregnancy, overeating or eating too fast, eating certain foods and drinks or anxiety and depression can lead to heartburn and bloating, leading to burps. It actually can be minimized with simple lifestyle changes- 1-Wear loose, comfortable clothing, nothing tight around your waist or stomach. 2-Instead of eating three big meals, have several small meals throughout the day. Take your time eating, and chew thoroughly. Wait at least an hour after meals before lying down. 3-Avoid foods that cause gastrointestinal distress like sugary, fizzy drinks (like coke), carbonated water, caffeinated beverages, alcohol, processed meats, or foods that are spicy, highly-seasoned, fried, or fatty.
4-Eat a serving of plain yogurt a day, preferably with live cultures. 5-Avoid gassy foods such as cabbage, beans, fried foods and onions that affects your digestive tract. 6-Try to relax. Stress and anxiety may cause you to swallow air, both during meals and throughout the day. 7-Use pillows to elevate your head when you sleep to prevent stomach acid from rising. If these changes do not ease symptoms, over-the-counter medicines such as antacids may be safe to take. Always consult your doctor before taking any type of medication while you are pregnant.
I am also constantly burping. 100 plus work for me. You can try.
I had the same problem too when I was expecting, especially during the 3rd trimester. Consulted my dr and she told me cos the uterus is pressing against our diaphragm as the baby grows, so she suggested that we sit on a flat surface and get hubby to hold our armpits and help us stretch upwards gently (i.
e. like someone trying to pull u to stand up). This is to create some space and will help us breathe better and less heartburn. It works for me, especially after a heavy meal. Give it a try to see if it works :)
I also had the same issue when I was expecting my second child. You may want to avoid food that is gassy, like cabbage.May try some warm ginger water.For me it gets better after my 2nd trimester. Just to encourage you, to hang in will get better. All the best to you!
Read More
Preventive measures against regurgitation in children
08.03.2017
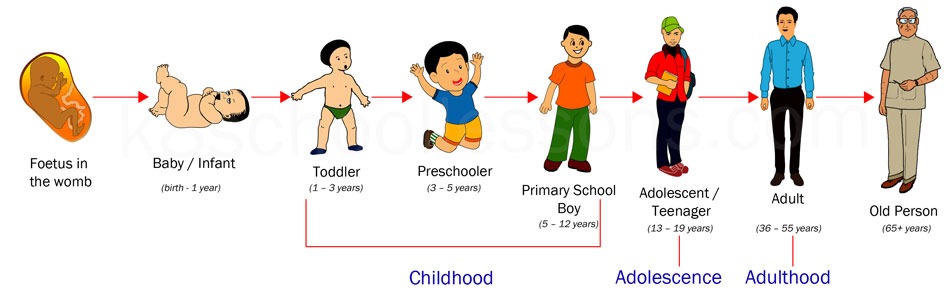
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes: nine0003
The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes: nine0003
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body. nine0003
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile. nine0003
In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile. nine0003
What explains physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation. nine0003
These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation. nine0003
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled. nine0003
-
Swallowing air during feeding (aerophagia). A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk.
 Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. nine0003
Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. nine0003 -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up. nine0003
Pathological regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
nine0010 -
increased intracranial pressure.

Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year. nine0003
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
nine0010
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air.
 Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again. nine0003
Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again. nine0003 -
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency. nine0003
-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.

-
The surface in the bed on which the baby lies should rise 10 cm at the head. nine0003
-
In addition, it is possible to use special "thickeners" of milk or anti-reflux mixtures, which the doctor will help you choose.
In the event that regurgitation begins to become more frequent or becomes abundant, or first began after six months of the baby's life, or does not subside by one and a half to two years of life, the child should be consulted by a pediatrician. With a high probability, additional help from a gastroenterologist will be needed. nine0003
In our Family Medical Center you can always find highly professional help.
← Back to the list of articles
Regurgitation and vomiting in children
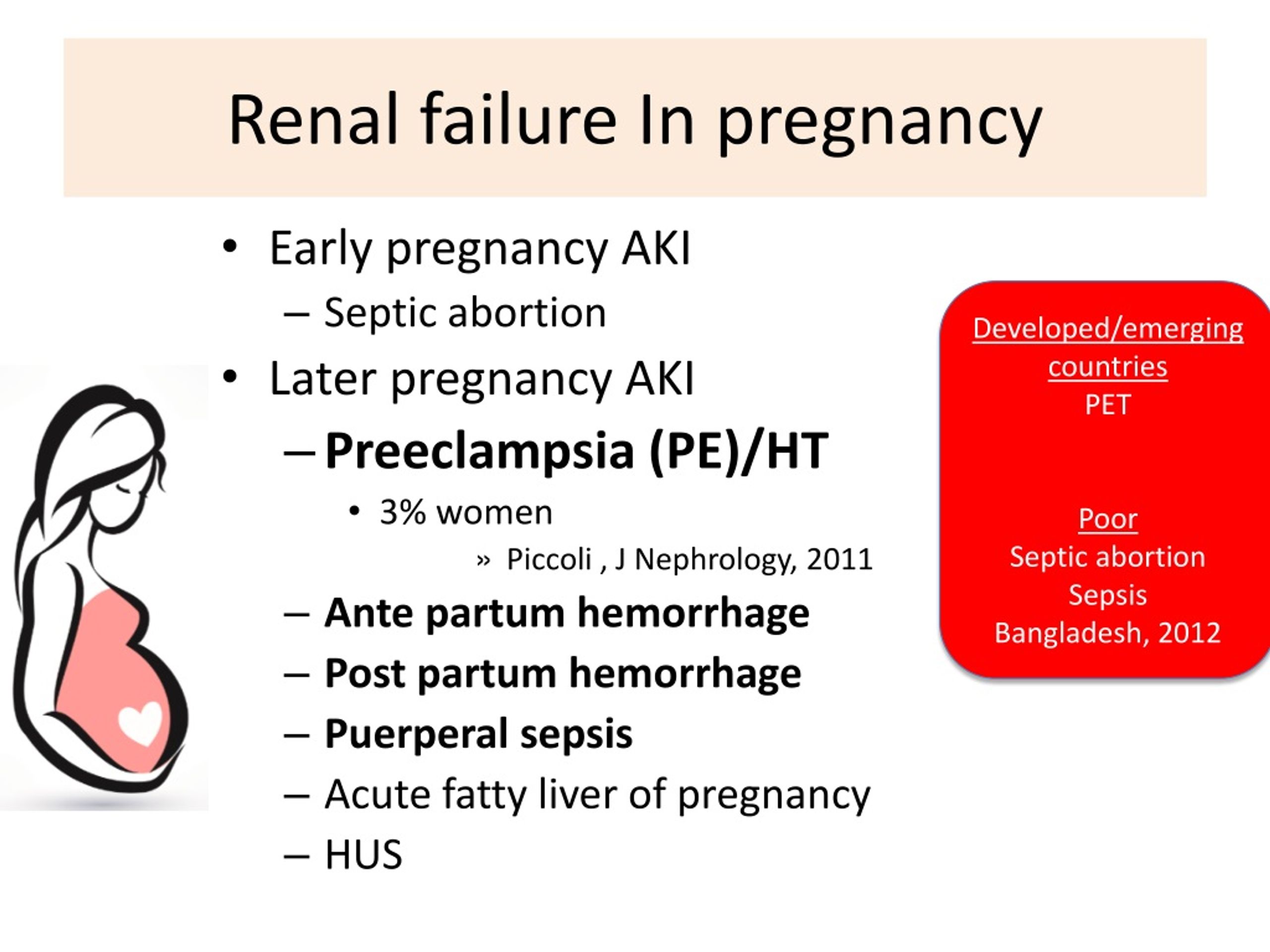
Regurgitation syndrome is one of the most common reasons for parents of young children to visit a pediatrician and a surgeon. The causes of regurgitation in children under 1 year old are different: anatomical and functional features, neurological disorders, infectious processes, malformations or other problems. The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
The mechanism that prevents regurgitation and vomiting in children is very complex and depends on the anatomical structure and physiological processes of the child. The formation of this mechanism occurs in the last trimester of pregnancy and continues in the first months of a child's life. Although regurgitation and vomiting can be a symptom of various diseases, in themselves these processes are physiological, i.e. normal. The pathological reflux of stomach contents into the esophagus is called gastroesophageal reflux, and the mechanism that prevents vomiting is called the antireflux mechanism. nine0003
Anti-reflux mechanism in children
In children, the nervous regulation of the antireflux mechanism is very complex and easily disturbed under the influence of external and internal factors. Regurgitation and vomiting easily occur in children with an immature antireflux mechanism, if the mode or volume of feeding is incorrectly selected, as a reaction to artificial mixtures, at the slightest sign of infectious processes. This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc. nine0003
This is especially often observed in children with intrauterine growth retardation and premature babies, as well as in severe pregnancy and toxicosis, caesarean section, complicated childbirth, etc. nine0003
When to see a doctor
Despite the fact that moderate spitting up in a child under 6 months is considered a variant of the norm, parents should definitely tell the pediatrician about this during a routine examination. The reason for serious concern and immediate examination of the child is an increase in the frequency or increase in the volume of regurgitation, the appearance of streaks of blood or bile impurities, a lag in recruitment or weight loss, and high temperature. In this case, it is urgent to consult a surgeon to rule out surgical causes. nine0003
Diagnostics
In most cases, an ultrasound examination (ultrasound) is necessary to establish an accurate diagnosis and select the correct treatment. An experienced doctor of ultrasound diagnostics helps to establish the correct diagnosis in more than half of the cases. Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
Sometimes, for a more accurate diagnosis, a flexible gastroscopy, X-ray examination, or computed tomography of the abdominal organs is performed.
When surgery is required
Pyloric stenosis, or impaired patency of the gastric outlet, is the cause of the most severe regurgitation syndrome (vomiting "fountain") in children under 2 months, accompanied by severe weight loss and progressive deterioration of the child's condition. This disease requires urgent surgical care. In leading clinics, such operations are performed using a minimally invasive laparoscopic method. The current level of development of surgery and pediatric anesthesiology allows the use of endoscopic surgery techniques even in children in the first weeks of life. nine0003
There are also other causes of regurgitation that require surgical intervention, such as hiatal hernia, chalazia (gaping) of the esophagus, and others. These malformations are characterized by a violation of the formation of the antireflux mechanism and lead to constant regurgitation in a child, impaired weight gain, decreased appetite, chronic cough, bronchial asthma, and anemia. If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
If drug therapy is ineffective, then a gastrofundoplication operation is indicated, in which an artificial antireflux valve is surgically formed. Like many other interventions, in modern children's clinics this operation is performed laparoscopically - with less trauma, minimal blood loss, minimal cosmetic defect and a quick recovery of the child after the operation. nine0003
Of course, vomiting and regurgitation can be symptoms of many other diseases and occur at any age in a child. Thus, vomiting is often observed in acute appendicitis and intestinal obstruction, it can be a symptom of an intestinal infection, intoxication, etc. In addition to the disease itself, vomiting and profuse regurgitation are dangerous because the child loses a large amount of water and salts necessary for life, which can lead to dehydration - exsicosis. The younger the child, the faster the disruption of compensatory mechanisms and the worsening of his condition. Therefore, the appearance in a child of symptoms of vomiting or severe regurgitation in young children requires immediate medical attention to identify the causes, establish the correct diagnosis and select the optimal treatment, and, if necessary, surgical.