How to help child cough up phlegm
Cystic Fibrosis: Helping Your Child Cough Up Mucus
Introduction
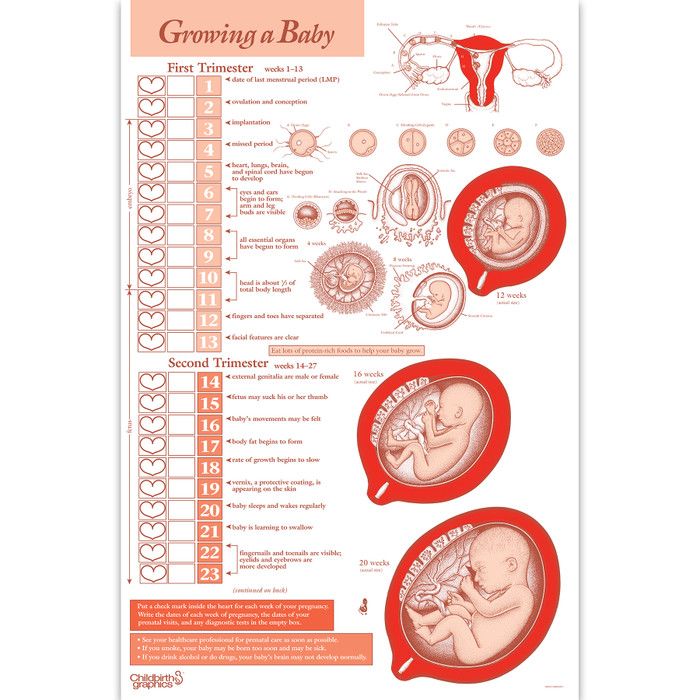
Cystic fibrosis causes mucus to become thick and sticky, which can clog the lungs and cause serious problems. You can help your child maintain lung function and avoid complications from mucus buildup and blockage by performing an airway clearance technique (ACT). Postural drainage and chest percussion (PD & P) is one of several airway clearance techniques that help clear mucus from your child's lungs.
- To help keep the lungs clear, it is important to do an airway clearance technique (such as postural drainage and chest percussion) every day. PD & P works well when used regularly.
- These techniques are one part of a larger treatment plan for cystic fibrosis.
- You may not notice an improvement in your child's lung function right away. But stopping these treatments will cause decreased lung function after about 3 weeks in children who have mild to moderate lung problems.footnote 1
It is important for your child to visit his or her doctor regularly and make any needed changes in treatment.
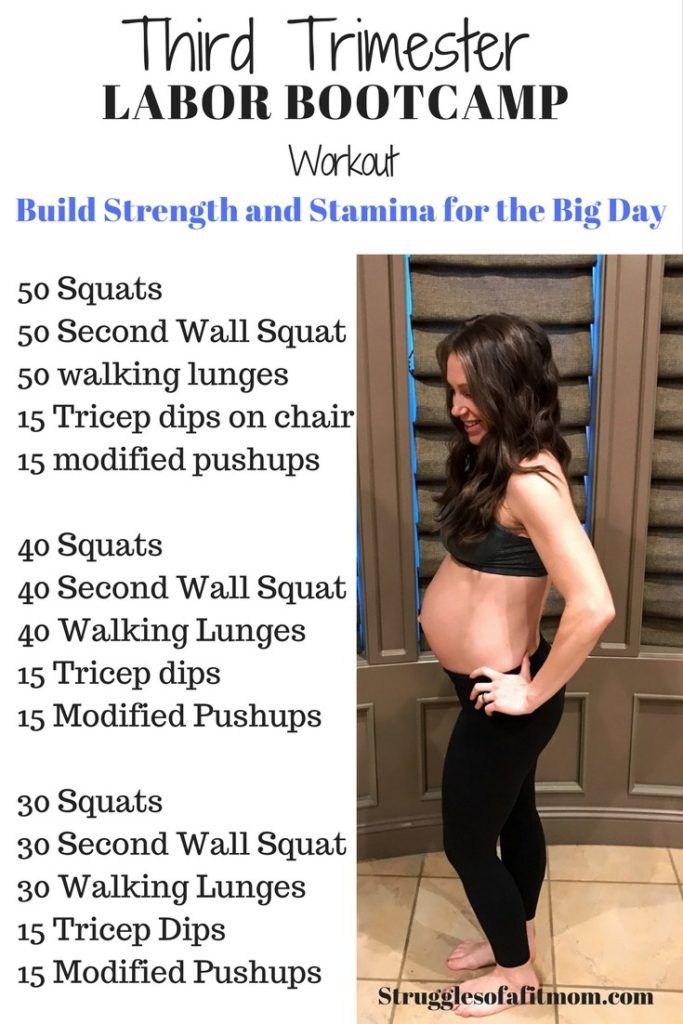
How do I do postural drainage?
There are several postural drainage positions. The different positions help drain mucus from different sections of the lungs. All people who have cystic fibrosis should do all the positions except babies, who should not be placed in the head-down position ("tipping"). Tipping a baby can cause reflux, which is when the contents of the stomach enter the esophagus.
Talk to your doctor or your respiratory therapist before starting PD & P. He or she can show you how the treatment is done and tell you how often and how long the treatment should be. Most doctors recommend that PD & P be done at least once a day.
PD & P is a time-consuming process. It usually takes 20 to 30 minutes. In general, a baby or small child who has no symptoms of congestion may require less treatment time than an older child who sounds congested and is coughing a lot.
At first, PD & P can seem complicated. But with help and practice, the treatment becomes easier, especially when you notice the benefits to your child.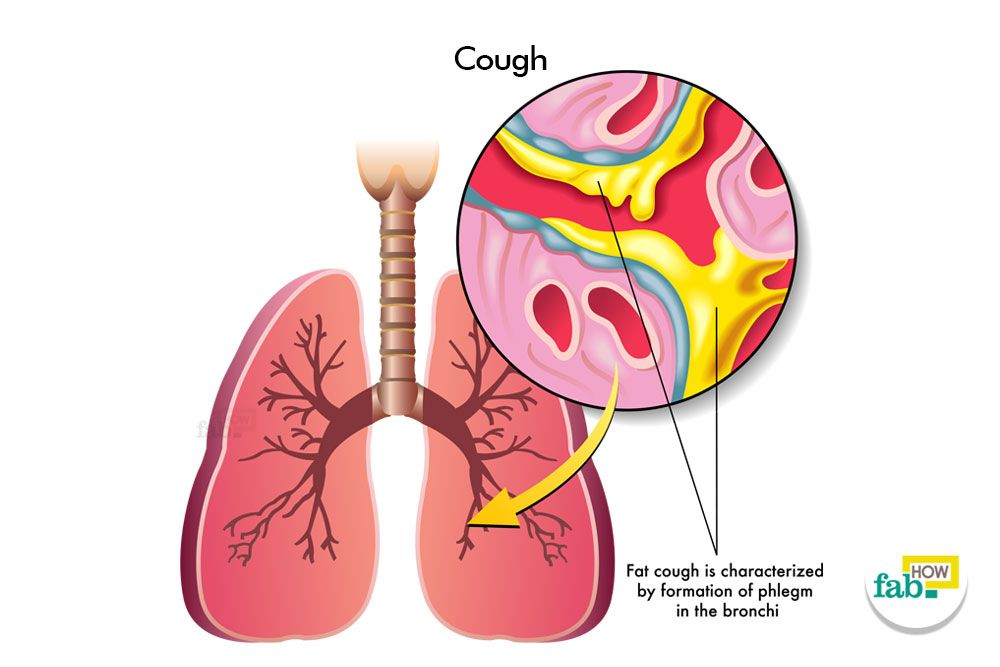 It is important to do these exercises exactly as instructed.
It is important to do these exercises exactly as instructed.
- Before you start, gather the materials you need, such as tissues, pillows, a thin cloth, or towels. If you have a baby or small child, you may sit in a chair with the child in your lap. If your child is older, he or she may be in bed using pillows for the different positions. You may need to experiment to find the best place to do the treatment so that both you and your child are comfortable.
- Position your child. Your doctor or therapist will recommend certain positions to use.
- Upper lobes (back)
- Upper lobes (front)
- Lower lobes (side)
- Lower lobes (back)
- Lower lobes (front)
- Clap your child's back or chest with your cupped hand quickly and rhythmically. This loosens the mucus, allowing it to drain. Do not clap directly on the skin—cover the area with thin clothing or a cloth. Bend your hand at the wrist and form a cup.
 When you clap, you should hear a hollow "popping" sound. If you hear a slapping sound, your hand is not cupped enough. You may safely clap over the ribs, but do not clap below the lower ribs or over the spine or female breasts. Follow this procedure for each position.
When you clap, you should hear a hollow "popping" sound. If you hear a slapping sound, your hand is not cupped enough. You may safely clap over the ribs, but do not clap below the lower ribs or over the spine or female breasts. Follow this procedure for each position. - How much force to use while clapping, and how long you clap, depends on the child. Consider the following:
- Younger and smaller children require less force and time than older and larger children or teens.
- Watch the child for signs of pain and discomfort. If you notice this, you may be using too much force.
- Is your child congested but mucus isn't coming up? If so, you may need to use more force.
- After clapping, apply vibrations. At the end of each position, you can vibrate the chest area to help loosen and move mucus. Have your child take a big breath and blow it out forcefully. As the child is blowing out, place your hand over the chest area and apply a little bit of pressure.
 Then quickly contract and relax your arm and shoulder muscles to produce vibrations throughout the chest area. To get the most out of this technique, ask your doctor or respiratory therapist to teach you how to do it properly. When your child is old enough, having his or her co-operation will make it easier to do this technique.
Then quickly contract and relax your arm and shoulder muscles to produce vibrations throughout the chest area. To get the most out of this technique, ask your doctor or respiratory therapist to teach you how to do it properly. When your child is old enough, having his or her co-operation will make it easier to do this technique. - After vibrations, have your child huff and cough. A huff is a forced exhalation that moves mucus higher and makes it possible to cough up more mucus. Huffing is best learned through demonstration, so ask your doctor or respiratory therapist to show you and your child how to do it. Huffing involves taking a deep breath and then breathing out forcefully, saying "huff." Your child will do this 2 or 3 times before he or she coughs. If huffing is done well, you can actually hear the mucus moving upwards. Your child will spit out the mucus that comes up.
References
Citations
- Egan M (2011).
Cystic fibrosis. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1481–1497. Philadelphia: Saunders.
Credits
- Postural drainage for children: Upper lobes (back)
- Postural drainage for children: Upper lobes (front)
- Postural drainage for children: Lower lobes (sides)
- Postural drainage for children: Lower lobes (back)
- Postural drainage for children: Lower lobes (front)
- Hand position for postural drainage
- About This Page
- General Feedback
- Email Link
- Physical Activity Services
We appreciate your feedback. Comments submitted through the form below can help us fix errors in page content, get rid of interface bugs, and update the HealthLinkBC website to better suit the needs of the people who use it.
Comments submitted through the form below can help us fix errors in page content, get rid of interface bugs, and update the HealthLinkBC website to better suit the needs of the people who use it.
To submit feedback about this web page, please enter your comments, suggestions, compliments or questions in the form below. To submit general feedback about the HealthLink BC website, please click on the General Feedback tab.
Page
Content
Functionality
Message:
Your name:
Your email:
To submit general feedback about the HealthLink BC website, please enter your comments, suggestions, compliments or questions in the form below. To submit feedback about a specific web page, please click on the About This Page tab.
Please note that we are unable to provide general health information or advice about symptoms by email. For general health information or symptom advice, please call us at 8-1-1 any time of the day or night.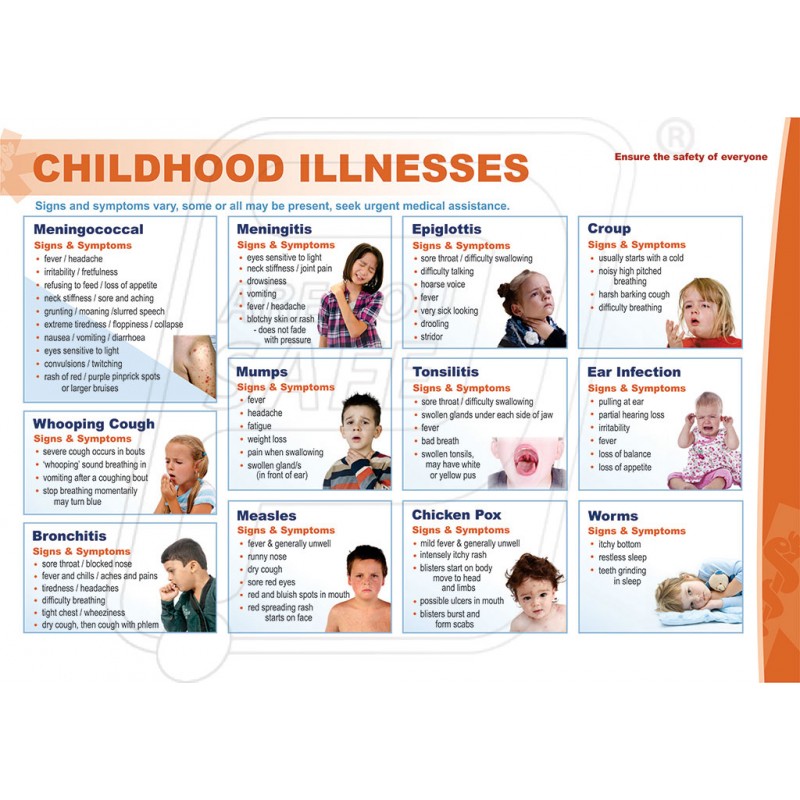
For questions about food and nutrition, please click on Email a HealthLinkBC Dietitian.
What is your message about? -- Select --8-1-1 Telephone ServicesBC Health Service Locater AppBrand Name Food List (BNFL)Website ContentTechnical ProblemsPrint media requirements / Web buttonsOther
Message:
Your name:
Your email:
Cough
Is this your child's symptom?
- The sound made when the cough reflex clears the airway of irritants
- Most coughs are part of a cold
- A coughing fit or spell is over 5 minutes of nonstop coughing
- Coughs can be dry (no mucus) or wet (with white, yellow or green mucus)
Causes of Cough
- Common Cold. Most coughs are part of a cold that includes the lower airway. The medical name is viral bronchitis. The bronchi are the lower part of the airway that go to the lungs. Bronchitis in children is always caused by a virus.
 This includes cold viruses, influenza and croup. Bacteria do not cause bronchitis in healthy children.
This includes cold viruses, influenza and croup. Bacteria do not cause bronchitis in healthy children. - Sinus Infection. The exact mechanism of the cough is unknown. It may be that post-nasal drip irritates the lower throat. Or pressure within the sinus may trigger the cough reflex.
- Allergic Cough. Some children get a cough from breathing in an allergic substance. Examples are pollens or cats. Allergic coughs can be controlled with allergy medicines, such as Benadryl.
- Asthma. Asthma with wheezing is the most common cause of chronic coughs in children. In adults, it's smoking.
- Cough Variant Asthma. 25% of children with asthma only cough and never wheeze. The coughing spells have the same triggers as asthma attacks.
- Air Pollution Cough. Fumes of any kind can irritate the airway and cause a cough. Tobacco smoke is the most common example. Others are auto exhaust, smog and paint fumes.
- Exercise Induced Cough. Running will make most coughs worse. If the air is cold or polluted, coughing is even more likely.
- Serious Causes. Pneumonia, bronchiolitis, whooping cough and airway foreign object
Trouble Breathing: How to Tell
Trouble breathing is a reason to see a doctor right away. Respiratory distress is the medical name for trouble breathing. Here are symptoms to worry about:
- Struggling for each breath or shortness of breath
- Tight breathing so that your child can barely speak or cry
- Ribs are pulling in with each breath (called retractions)
- Breathing has become noisy (such as wheezes)
- Breathing is much faster than normal
- Lips or face turn a blue color
Phlegm or Sputum: What's Normal?
- Yellow or green phlegm is a normal part of the healing of viral bronchitis.
- This means the lining of the trachea (windpipe) was damaged by the virus.
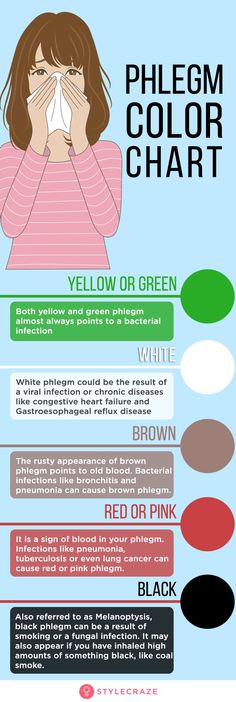 It's part of the phlegm your child coughs up.
It's part of the phlegm your child coughs up. - Bacteria do not cause bronchitis in healthy children. Antibiotics are not helpful for the yellow or green phlegm seen with colds.
- The main treatment of a cough with phlegm is to drink lots of fluids. Also, if the air is dry, using a humidifier will help. Sipping warm clear fluids will also help coughing fits.
Vaping Risks
- Talk with your child about the dangers of vaping.
- Vaping can cause severe lung injury. The lung damage can be permanent.
- Vaping can even cause death.
- Vaping tobacco also causes nicotine addiction.
- The legal age to purchase vaping products is 21 in the US.
- Encourage your teen to avoid vaping. If they have started, urge them to quit.
- Warning: never use home-made or street-purchased vaping solutions. Reason: they have caused most lung damage.
When to Call for Cough
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Passed out or stopped breathing
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe.
- Lips or face have turned bluish during coughing
- Harsh sound with breathing in (called stridor)
- Wheezing (high-pitched purring or whistling sound when breathing out)
- Breathing is much faster than normal
- Can't take a deep breath because of chest pain
- Severe chest pain
- Coughed up blood
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- High-risk child (such as cystic fibrosis or other chronic lung disease)
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Nonstop coughing spells
- Age less than 6 months old
- Earache or ear drainage
- Sinus pain (not just congestion) around cheekbone or eyes
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Chest pain even when not coughing
- Concerns about vaping
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Coughing causes vomiting 3 or more times
- Coughing has kept home from school for 3 or more days
- Allergy symptoms (such as runny nose and itchy eyes) also present
- Runny nose lasts more than 14 days
- Cough lasts more than 3 weeks
- You have other questions or concerns
Self Care at Home
- Cough with no other problems
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Cough
- What You Should Know About Coughs:
- Most coughs are a normal part of a cold.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- A cough can be a good thing. We don't want to fully turn off your child's ability to cough.
- Here is some care advice that should help.
- Homemade Cough Medicine:
- Goal: decrease the irritation or tickle in the throat that causes a dry cough.

- Age 6 months to 1 year: give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: use a dose of 1-2 teaspoons (5-10 mL). Give 4 times per day when coughing. Caution: do not use honey until 1 year old.
- Age 1 year and older: use honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup. You can also buy cough products that have honey in them at drug stores. They do not work better than plain honey and cost much more.
- Age 6 years and older: use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
- Goal: decrease the irritation or tickle in the throat that causes a dry cough.
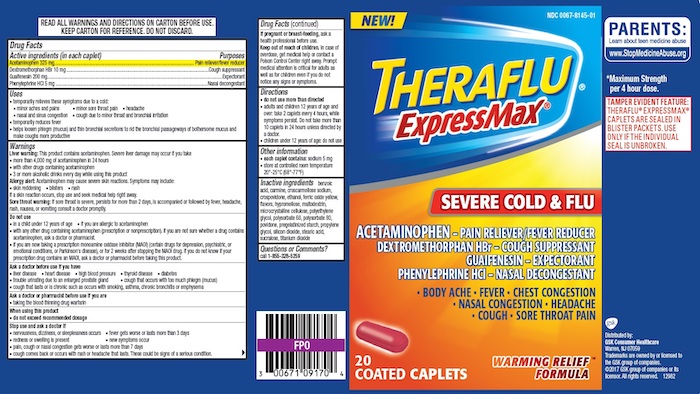
- Non-Prescription Cough Medicine (DM):
- Non-prescription cough medicines are not advised. Reason: no proven benefit for children and not approved under 6 years old (FDA).
- Honey has been shown to work better for coughs.
 Caution: do not use honey until 1 year old.
Caution: do not use honey until 1 year old. - If age 6 years or older, you might decide to use a cough medicine. Choose one with dextromethorphan (DM), such as Robitussin Cough syrup. DM is present in most non-prescription cough syrups. Follow the instructions on the package.
- When to Use: give only for severe coughs that interfere with sleep or school.
- DM Dose: give every 6 to 8 hours as needed.
- Coughing Fits or Spells - Warm Mist and Fluids:
- Breathe warm mist, such as with shower running in a closed bathroom.
- Give warm clear fluids to drink. Examples are apple juice and lemonade.
- Age less than 6 months, only give breast milk or formula.
- Age 6 - 12 months. Give 1-2 teaspoons (5-10 mL) each time. Limit to 4 times per day.
- Age older than 1 year. Can also offer warm lemonade or herbal teas. Amount: a few ounces (30 mL) each time.
- Reason: both relax the airway and loosen up any phlegm.
- Vomiting from Hard Coughing:
- For vomiting that occurs with hard coughing, give smaller amounts per feeding.
- Also, feed more often.
- Reason: vomiting from coughing is more common with a full stomach.
- For vomiting that occurs with hard coughing, give smaller amounts per feeding.
- Encourage Fluids:
- Try to get your child to drink lots of fluids.
- Goal: keep your child well hydrated.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
- It also will thin out the mucus discharge from the nose.
- Humidifier:
- If the air in your home is dry, use a humidifier. Reason: dry air makes coughs worse.
- Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: keep your child well hydrated. Give lots of cold fluids.
- Avoid Tobacco Smoke:
- Tobacco smoke makes coughs much worse.
- Tobacco smoke makes coughs much worse.
- Return to School:
- Your child can go back to school after the fever is gone.
- Your child should also feel well enough to join in normal activities.
- For practical purposes, the spread of coughs and colds cannot be prevented.
- Extra Advice- Allergy Medicine for Allergic Cough:
- Allergy medicine can bring an allergic cough under control within 1 hour. The same is true for nasal allergy symptoms.
- A short-acting allergy medicine (such as Benadryl) is helpful. No prescription is needed. Age limit: 1 and older.
- Do not use Benadryl longer than a few days.
- Switch to a long-acting antihistamine, such as Zyrtec. Age limit: 2 and older.
- What to Expect:
- Viral coughs most often last for 2 to 3 weeks.
- Sometimes, your child will cough up lots of phlegm (mucus). The mucus can normally be gray, yellow or green.
- Antibiotics are not helpful.

- Call Your Doctor If:
- Trouble breathing occurs
- Wheezing occurs
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/16/2022
Last Revised: 09/23/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Teaching a child to cough correctly | Med center b-healthy clinic Kharkiv
It is quite difficult to make a baby cough up sputum, and for young parents it seems impossible at all. However, they should help the child and teach him to cough, as this is a normal reaction of the body to irritation of the upper or lower respiratory tract. From the point of view of human physiology, there is nothing in the process of coughing that could cause unrest. On the contrary, its presence helps sputum to come out of the baby's lungs or bronchi. nine0004
On the contrary, its presence helps sputum to come out of the baby's lungs or bronchi. nine0004
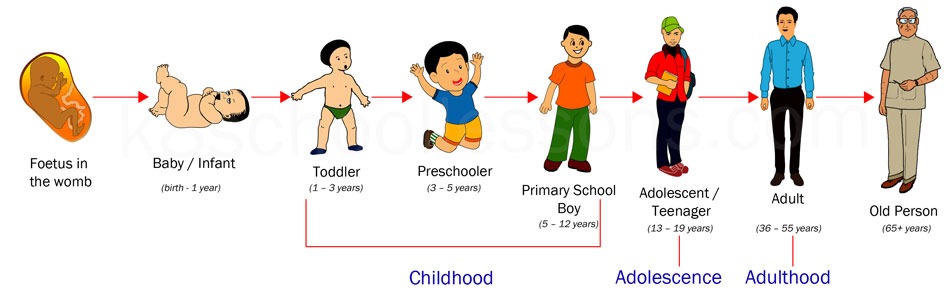
In children who have not yet reached the age of two, the mechanism of coughing is not sufficiently developed. Of course, even newborns can cough, but the effectiveness of such a cough is very small due to a weak cough shock. What to do if the baby is ill and has to cough up the accumulated mucus, but has not yet learned how to do it?
How to make a baby cough
While an adult child can simply be asked to cough, things are a little more complicated with an infant. Since the baby is almost constantly in a horizontal position, mucus accumulates in the airways with a vengeance. There are several effective measures that help the child cough. nine0005
- Active games.
Babies love spending time with their parents, especially playing. This is a great opportunity to teach your child to cough while playing. The kid will quickly remember the skill and will not be capricious.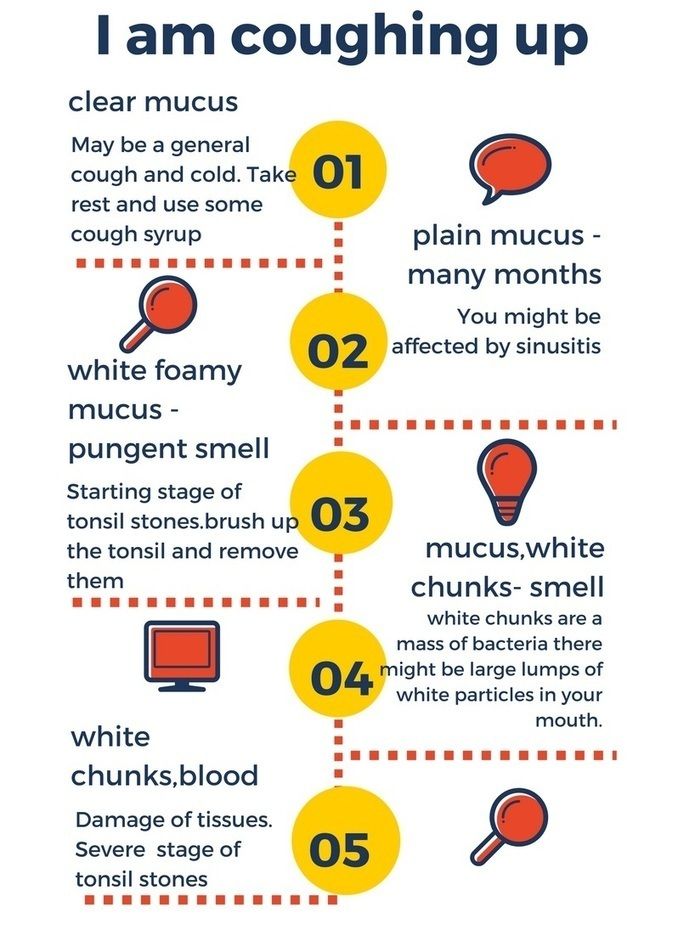 To do this, lift the baby as high as possible and tilt the head down a little. Simulating flight will help the baby cough.
To do this, lift the baby as high as possible and tilt the head down a little. Simulating flight will help the baby cough.
- Correct air readings.
The child will breathe easier if the air in the room is cool. The ideal parameters are a temperature of 18 degrees and a relative humidity of 50-60%. Open the window even in winter, and do not forget about regular wet cleaning and air humidification. nine0005
- Drainage massage.
The procedure must be carried out exclusively by a specialist who has a medical background.
Only some simple exercises can be done at home so as not to accidentally harm the baby. Warm up the back with massage movements, and then lightly tap with your fingers at the shoulder blades. The baby should be placed on your lap so that the head is slightly lower than the body. This will help the baby to cough effectively and recover faster. nine0005
- Staying upright.
Even for a very young child who has recently turned 2 months old, it is good to spend time in an upright position.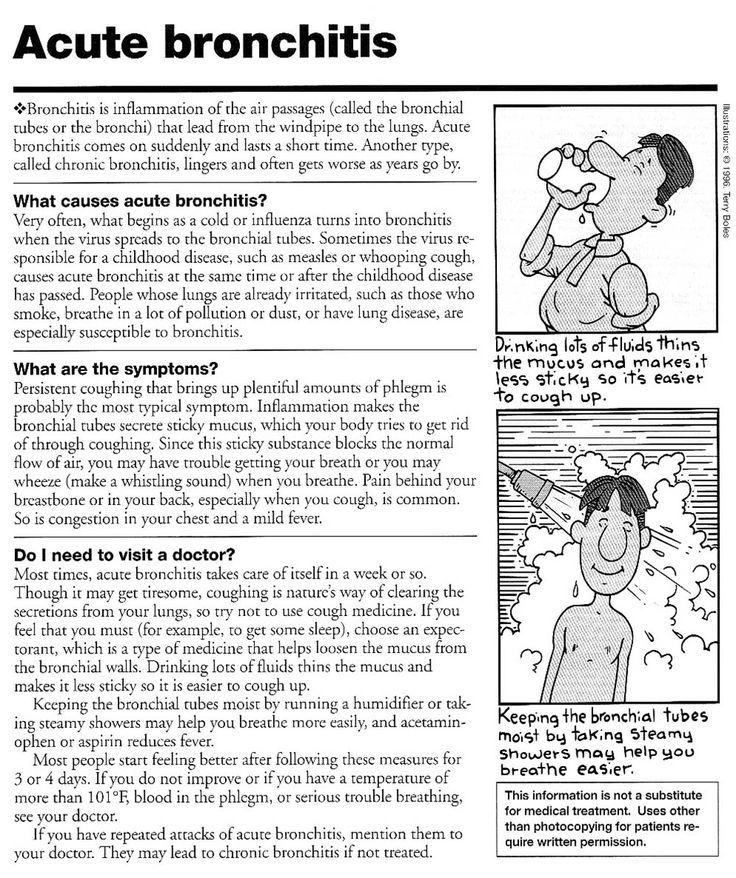 For daytime sleep, the crumbs can be arranged in a car seat. Such an exercise will reduce the amount of sputum formation and improve the well-being of the baby.
For daytime sleep, the crumbs can be arranged in a car seat. Such an exercise will reduce the amount of sputum formation and improve the well-being of the baby.
- Gentle pressure on the root of the tongue.
If you notice that sputum has collected in the child's trachea or throat, try gently pressing the spoon against the root of the tongue. Do as the doctor does when examining the throat. Several of these procedures will help the child cough well, but do not make too much effort, otherwise vomiting may occur. So that the baby is not afraid, distract him with an interesting game, activity. Turn on your favorite cartoon or put together puzzles. nine0005
These tips will help your child to cough correctly, as well as remember the mechanism of coughing. And you can also make an appointment with our pediatrician or call a pediatrician at home who will teach the child to cough properly.
SERVICES
- Make an appointment with a pediatrician
- Calling a pediatrician at home
Cough in children - Alexandrovskaya Family Clinic
Cough in children! Recommendations .
..
Another cough... How often one hears such a complaint from the parents of their little patients to a pediatrician. At the same time, it is the frequency of occurrence of this symptom, and the variety of medicines in pharmacies aimed at ridding the baby of a painful cough, that leads many adults to believe that they can quite cope on their own, acting as the attending physician of their child. And the abundance of advertising and the sale of these drugs without prescription only exacerbates the situation. nine0005
So, what is a cough? What diseases of the child can he testify to? And why is it impossible to resort to self-treatment, motivating your choice of a drug with the fact that “they prescribed it for us last time and it helped”?
Cough - a sharp exhalation of air, reflexively relieving the mucous membrane of the respiratory tract from viscous sputum or foreign substances. The most common symptom in various infections, up to 9They occupy 0% of the causes of coughing.
So, coughing can occur when:
nine0002 What other diseases can be accompanied by a cough?
- respiratory tract infections (rhinitis, pharyngitis, tonsillitis, bronchitis, pneumonia…)
- and also, in diseases of the ENT organs (with otitis media, reflex cough often develops, adenoiditis - inflammation of the nasopharyngeal tonsil)
- whooping cough would be very specific
- the leading place among them is occupied by bronchial asthma
- occurs in some helminthic infestations, such as ascariasis
- Cough can be a sign of diseases not related to the bronchopulmonary system, so it can be a leading sign of gastroesophageal reflux disease, or heart defects that occur with signs of heart failure
- cough is a formidable symptom if a foreign body enters the respiratory tract
You can list the diseases indefinitely, it is important to understand that its treatment will also depend on determining the cause of the cough.
Almost each of the listed diseases has its own calling card in the form of a kind of cough, given the characteristics of which it is possible to establish the cause of its occurrence. nine0003 For example, at:
- various acute infections of the upper respiratory tract - cough is frequent, superficial, accompanied by a rise in body temperature, profuse mucous discharge from the nose, sore throat.
- with obstructive bronchitis, as well as bronchial asthma - paroxysmal cough, accompanied by wheezing, shortness of breath and wheezing, which can be heard at a distance
- with stenosing laryngotracheitis - breathing is difficult, the cough becomes "barking", rough, the voice is hoarse, it may disappear completely
- with a foreign body in the respiratory tract - against the background of complete well-being, a paroxysmal cough suddenly appears, with a low sound at the beginning and a whistling high sound at the end. An indication that before the onset of such a cough the child played with small objects can help in the diagnosis.

- The hallmark of such an infectious disease as whooping cough is a paroxysmal cough, the tremors of which follow one after another, at the end of the attack there is a loud noisy breath. The face turns purple, may be accompanied by vomiting. nine0018
- with adenoiditis - cough, mostly in the morning or after sleep, against the background of significantly difficult nasal breathing, with profuse, mucopurulent discharge. The child breathes with an open mouth, in a dream - snores.
- cough in gastroesophageal reflux disease is associated with frequent regurgitation in the first year of life, later with frequent vomiting, belching and abdominal pain.
So, the characteristics of a cough can tell a lot about the cause of its occurrence, but only a pediatrician can correctly assess the child's condition and determine the disease that led to the appearance of a cough. nine0003 In what cases is a doctor's call obligatory and urgent?
- for cough accompanied by shortness of breath (rapid breathing, retraction of intercostal spaces)
- when combined with cough and fever in a child
- when a baby coughs in the first year of life
- if sputum is green or bloody
- for prolonged cough, lasting more than 10-14 days
- if the cough appeared suddenly, against the background of complete well-being (especially if the child played with small toys or ate shortly before it appeared)
It should be borne in mind that after examining the child and talking with the parents, the pediatrician may need additional research methods, starting with laboratory: a general blood test and tests to determine antibodies to a particular pathogen, swabs from the nose and throat for flora, sputum culture on the flora (to determine the exact diagnosis of respiratory infections).

In addition, it may be necessary to conduct a number of instrumental examination methods: spirography with the determination of the function of external respiration (to exclude bronchial asthma), ECG and ultrasound of the heart (to exclude heart defects), chest x-ray (to exclude pneumonia). nine0005
But now, the diagnosis is established, and the doctor prescribes treatment. Let's talk about the most prescribed groups of drugs, but let's start, as always, with regime moments.
- The regimen should be at home, but it is not necessary to limit the child in his physical activity, since movements stimulate sputum discharge and reduce the time of illness.
- Be sure to drink, increasing the amount of water the child usually drinks by 30% - 50%. nine0018
- Humidification is also a must! Achieved with the help of humidifiers. If you don’t have such a “miracle machine”, don’t worry, you can achieve the same effect with wet laundry (hang wet bedding on batteries).

- Postural drainage is recommended to facilitate expectoration of sputum. After inhalation, the child lies on his stomach, his head and chest are tilted slightly lower, an adult taps on the back of the child with his fingers (in children of the first year of life) or with the edge of his palm (in older children). nine0018
- And remember! After the child recovers from bronchitis or pneumonia, a course of chest massage is required.
Drug treatment of cough is prescribed only if the cough significantly disturbs the child's condition and in any case begins with the elimination of the cause that caused it. Medicines can be prescribed for dry, paroxysmal, unproductive cough, which significantly changes the child's well-being for the worse. Most often, such a cough is caused by the presence of thick, viscous sputum and a violation of its removal from the bronchial mucosa. Therefore, the purpose of prescribing drugs in this case is to thin the sputum and facilitate its excretion.
That is, the efforts of the pediatrician will be aimed at transferring a dry cough into a productive (wet). Treatment of wet cough most often does not require the use of drug therapy. Exceptions are cases of intense wet cough, exhausting the child, accompanied by vomiting, sleep disturbance, or when there is a threat of aspiration. nine0005
By clicking on the button you can make an appointment with a specialist!
Now let's move on to the main medicines that can be prescribed by a pediatrician for diseases accompanied by a cough in a child:
- Perhaps one of the most effective cough suppressants is moisturizing the mucous membranes. It is achieved by inhalation with saline or in combination with another drug (as prescribed by a doctor). Moisturizing the mucosa leads to a decrease in its irritation, liquefaction of sputum and facilitates its removal. Inhalations can be carried out using various types of inhalers.
Remember that inhalations using boiling water in children are not allowed! Currently, nebulizers are becoming increasingly popular, they are easy to use, are used in children from the first year of life, with their help, the medicinal substance in the form of an aerosol of small particles reaches the most distant parts of the bronchi. nine0018
- For coughs associated with respiratory infections of the upper respiratory tract, so-called enveloping agents have proven themselves well. These are various means for resorption in the oral cavity, teas, syrups, their use is aimed at the appearance of a protective layer of the drug components on the oral mucosa, as a result of which its irritation is reduced.
- Antitussives (tusuprex, libexin, synecode) are designed to suppress the cough center in the central nervous system. In children, their scope is very limited, mainly in cases of whooping cough, especially in children of the first years of life. nine0018
- Mucolytics (ACC, ambrohexal, carbocysteine) are designed to thin the sputum, practically without affecting its volume.
nine0015 Expectorants act by reducing the viscosity of sputum while increasing its volume. These mainly include preparations based on medicinal herbs (marshmallow, elecampane, coltsfoot, wild rosemary, oregano, licorice). Remember that the natural composition of such products does not indicate their complete safety, and in children, especially in the first years of life, there is a high risk of developing allergic reactions. And the thermopsis herb enhances the gag and cough reflexes, which, combined with increased sputum volume, can lead to aspiration in young children. nine0018They are used for dry, unproductive cough to convert it into a productive one, and to facilitate sputum discharge. They can be used not only as drugs used by mouth, but also for inhalation. It is important to remember that a drug such as ACC can increase bronchospasm, so it should not be used for obstructive bronchitis.
- Bronchodilators (berodual, salbutamol) are used to reduce the effects of bronchospasm, with obstructive bronchitis or bronchial asthma, inhaled or through a nebulizer
- Anti-inflammatory drugs - used to reduce inflammation of the respiratory mucosa.