Bumps rash on face child
What are those bumps on my child's skin?
Diseases & conditions
- Coronavirus Resource Center
- Acne
- Eczema
- Hair loss
- Psoriasis
- Rosacea
- Skin cancer
- A to Z diseases
- A to Z videos
- DIY acne treatment
- How dermatologists treat
- Skin care: Acne-prone skin
- Causes
- Is it really acne?
- Types & treatments
- Childhood eczema
- Adult eczema
- Insider secrets
- Types of hair loss
- Treatment for hair loss
- Causes of hair loss
- Hair care matters
- Insider secrets
- What is psoriasis
- Diagnosis & treatment
- Skin, hair & nail care
- Triggers
- Insider secrets
- What is rosacea
- Treatment
- Skin care & triggers
- Insider secrets
- Types and treatment
- Find skin cancer
- Prevent skin cancer
- Raise awareness
- Español
Featured
How Natalie cleared her adult acneNatalie tried many acne products without success. Find out how a board-certified dermatologist helped Natalie see clear skin before her wedding.
JAK inhibitors are helping patients with alopecia areata, eczema/atopic dermatitis, psoriasis, and vitiligo. Here’s what you need to know.
Everyday care
- Skin care basics
- Skin care secrets
- Injured skin
- Itchy skin
- Sun protection
- Hair & scalp care
- Nail care secrets
- Basic skin care
- Dry, oily skin
- Hair removal
- Tattoos and piercings
- Anti-aging skin care
- For your face
- For your skin routine
- Preventing skin problems
- Bites & stings
- Burns, cuts, & other wounds
- Itch relief
- Poison ivy, oak & sumac
- Rashes
- Shade, clothing, and sunscreen
- Sun damage and your skin
- Aprenda a proteger su piel del sol
- Your hair
- Your scalp
- Nail care basics
- Manicures & pedicures
Featured
Practice Safe SunEveryone's at risk for skin cancer. These dermatologists' tips tell you how to protect your skin.
These dermatologists' tips tell you how to protect your skin.
Find out what may be causing the itch and what can bring relief.
Darker Skin Tones
- Skin care secrets
- Hair care
- Hair loss
- Diseases & Conditions
- Acne
- Dark spots
- Dry skin
- Light spots
- Razor bumps
- Caring for Black hair
- Scalp psoriasis
- Weaves & extensions
- Central centrifugal cicatricial alopecia
- Frontal fibrosing alopecia
- Hairstyles that pull can cause hair loss
- Acanthosis nigricans
- Acne keloidalis nuchae
- Hidradenitis suppurativa
- Keloid scars
- Lupus and your skin
- Sarcoidosis and your skin
- Skin cancer
- Vitiligo
- More diseases & conditions
Featured
Fade dark spotsFind out why dark spots appear and what can fade them.
If you have what feels like razor bumps or acne on the back of your neck or scalp, you may have acne keloidalis nuchae. Find out what can help.
Cosmetic treatments
- Your safety
- Age spots & dark marks
- Cellulite & fat removal
- Hair removal
- Scars & stretch marks
- Wrinkles
- Younger-looking skin
Featured
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
Do you know which one?
If you want to diminish a noticeable scar, know these 10 things before having laser treatment.
BotoxIt can smooth out deep wrinkles and lines, but the results aren’t permanent. Here’s how long botox tends to last.
Public health programs
- Skin cancer awareness
- Free skin cancer screenings
- Kids' camp
- Good Skin Knowledge
- Shade Structure grants
- Skin Cancer, Take a Hike!™
- Awareness campaigns
- Flyers & posters
- Get involved
- Lesson plans and activities
- Community grants
Featured
Free materials to help raise skin cancer awarenessUse these professionally produced online infographics, posters, and videos to help others find and prevent skin cancer.
Free to everyone, these materials teach young people about common skin conditions, which can prevent misunderstanding and bullying.
Find a dermatologist
- Find a dermatologist
- What is a dermatologist?
- FAAD: What it means
- How to select a dermatologist
- Telemedicine appointments
- Prior authorization
- Dermatologists team up to improve patient care
Featured
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist that’s right for you.
A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
12 Common Summertime Skin Rashes in Children
Sunny days and starlit evenings spent playing, splashing, and exploring can leave kids with more than warm summertime memories. Balmy weather also can lead to itchy, irritated skin.
Check out the list from the American Academy of Pediatrics (AAP) to see how you can help prevent, identify, and soothe these common summertime skin rashes.
1. Heat Rash
Heat rash (also known as prickly heat or miliaria) is seen most often in babies and young children when sweat gland pores become blocked and perspiration can't escape. The rash looks like patches of small pink or red bumps or blisters under clothing or spots where skin tends to fold—on the neck, elbows, armpits, or thighs—although heat rash can occur on other covered areas.
What parents can do:
Keep kids cool. Dress your child in clothing that keeps the skin cool and dry. If possible, use fans and air conditioning to avoid overheating.
Pay attention to hot spots. Wash areas of the skin that stay wet with sweat, urine, or drool with cool water. Pat them dry.
Keep skin bare. Leave areas open to air without clothing. Do not apply skin ointments.
2. Poison Ivy & Other Plant Rashes
Many children get a burning, intensely itchy rash where their skin touches plants—such as poison ivy, poison oak, sumac—containing a sticky oil called urushiol. An allergic skin reaction causes redness, swelling and blisters. Other plants—such as wild parsnip, giant hogweed, and citrus—contain chemicals that make skin hypersensitive to sunlight and cause a phytophotodermatitis rash.
What parents can do:
Prevent exposure.
 Teach your child what these plants look like and how to avoid them. Both poison ivy and poison oak have shiny green leaves that grow three to a stem, so you might share the rhyme: "Leaves of three, let them be." The sumac shrub has stems that contain 7-13 leaves arranged in pairs, while wild parsnip and giant hogweed have clusters of small, flat-topped yellow and white flowers. If you have younger children, inspect the parks they play in and have rash-causing plants removed.
Teach your child what these plants look like and how to avoid them. Both poison ivy and poison oak have shiny green leaves that grow three to a stem, so you might share the rhyme: "Leaves of three, let them be." The sumac shrub has stems that contain 7-13 leaves arranged in pairs, while wild parsnip and giant hogweed have clusters of small, flat-topped yellow and white flowers. If you have younger children, inspect the parks they play in and have rash-causing plants removed.Wash and trim. If your child comes into contact with these plants, wash all of his or her clothes and shoes in soap and water. Also, wash the area of the skin that was exposed with soap and water for at least 10 minutes after the plant or the oil is touched. To discourage scratching and further damage to the skin, keep your child's fingernails trimmed. This will also prevent the rash from spreading if there is still a small amount of oil under the fingernails.
Soothing salves.
 If the rash is mild, apply calamine lotion to cut down on the itching. Avoid ointments containing anesthetics or antihistamines—they can cause allergic reactions themselves. Another good option to reduce skin inflammation is 1% hydrocortisone cream.
If the rash is mild, apply calamine lotion to cut down on the itching. Avoid ointments containing anesthetics or antihistamines—they can cause allergic reactions themselves. Another good option to reduce skin inflammation is 1% hydrocortisone cream.Talk with your pediatrician. While mild cases can be treated at home, talk with your pediatrician if your child is especially uncomfortable, the rash is severe and/or isn't going away, if the rash is on your child's face or groin area, or if you notice signs of infection (i.e., fever, redness, swelling beyond the poison ivy or oak lesions).
3. Eczema
Eczema (also called atopic dermatitis or AD) is a chronic condition common in children that causes patches of dry, scaly red skin and tends to flare up during colder months when there's less moisture in the air. But dryness caused by air conditioning and pressurized planes during summer travel can cause problems, too. Overheating, sweating and chlorine in swimming pools also can trigger eczema.
Overheating, sweating and chlorine in swimming pools also can trigger eczema.
What parents can do:
Moisturize. Apply fragrance-free creams or ointments at least once a day or more often if needed. After a bath or swimming, gently pat your child's skin with a towel and then apply moisturizer to his or her damp skin.
Dress wisely. Choose clothing made of soft, breathable fabrics like cotton when possible. Wash clothes in a detergent free of irritants such as perfumes and dyes.
Don't scratch. Keep your child's fingernails short and smooth, and remind him or her not to scratch. Scratching can make the rash worse and lead to infection.
Talk with your pediatrician. Ask your child's pediatrician if allergies, sometimes triggered by trees and plants that bloom during summer, could be a cause of the eczema. Your child's pediatrician may recommend medicines to help your child feel better and to keep the symptoms of eczema under control.
4. Insect Bites & Stings
Insects such as bees, wasps, mosquitos, fire ants, and ticks can cause itching and minor discomfort where they prick the skin. For some children, insect bites and stings can cause a severe allergic reaction called anaphylaxis—which includes a rash or hives and life-threatening symptoms such as airway swelling. (For children with a known allergy to insect bites and stings, it is important to have anaphylaxis emergency care plan in place). Other times, diseases spread by insects such as Lyme Disease, Rocky Mountain Spotted Fever, and Zika Virus can cause rashes and other health problems.
What parents can do:
Avoidance. When spending time outdoors, avoid scented soaps and shampoos and brightly colored clothing—they can attract insects. If possible, steer clear of areas where insects nest and gather (i.e., stagnant pools of water, uncovered food, and blooming flowers).

Use insect repellent. Products with DEET can be used on the skin, but look for family-friendly products that contain concentrations of no more than 30% DEET. Wash the insect repellent off with soap and water when your child returns indoors.
Cover up. When in wooded areas or in or near tall grass, stay on cleared trails as much as possible. Have your child wear a long-sleeved shirt, pants, and hat. Avoid wearing sandals in an area where ticks may live.
Look closely. Wear light-colored clothing to make it easier to spot ticks. After coming indoors, check for ticks on your child's skin—they often hide behind the ears or along the hairline.
Remove stingers and ticks. To remove a visible stinger from skin, gently scrape it off horizontally with a credit card or your fingernail. If you find a tick, gently grasp it with fine-tipped tweezers as close to the skin as possible.
 Without squeezing the tick's body, slowly pull it away from the skin. See How To Remove A Tick for more information.
Without squeezing the tick's body, slowly pull it away from the skin. See How To Remove A Tick for more information. Clean the skin. After the stinger or tick is out, clean the bitten area with rubbing alcohol or other first aid ointment.
Treat swelling. Apply a cold compress or an ice pack to any swelling for at least 10 minutes.
Help relieve the itch. Applying ice, along with calamine lotion or 1% hydrocortisone cream, can also help relieve itching.
5. Impetigo
Impetigo is a bacterial skin infection that's more common during hot, humid weather. It causes a rash that may have fluid-filled blisters or an oozing rash covered by crusted yellow scabs. Impetigo is more likely to develop where there is a break in the skin, like around insect bites.
What parents can do:
Clean and cover. Clean the infected area with soap and water.
Cover the infected area loosely to help prevent contact that would spread the infection to others or to other parts of the body. Wash your own hands well after treating your child's sores.
Avoid scratching. Trim your child's fingernails and discourage scratching. A child can spread the infection to other parts of his or her body by scratching. You can cover the rash loosely with a bandage to discourage your child from touching the rash, but make sure air can flow through so the skin can heal.
Talk with your pediatrician. While mild cases may respond to over-the-counter antibiotics such as bacitracin or bacitracin-polymyxin, impetigo is usually treated with prescription antibiotics—either a skin cream or oral medication. Your pediatrician may order a skin culture (test of your child's skin) to determine which bacteria are causing the rash.
6. Swimmer's Itch
Swimmer's itch (also called clam digger's itch or cercarial dermatitis) may appear after playing in lakes, oceans, and other bodies of water. The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
What parents can do:
Be aware. Don't swim near or wade in marshy areas where snails are commonly found. Try not to attract birds (by feeding them, for example) where your family swims. Birds may eat the snails and spread the parasites in the water.
Shower or towel dry. Shower or briskly rub the skin with a towel immediately after getting out of the water. The parasites start to burrow when the water on skin begins evaporating. If your skin child's skin stings with rubbing—and the rash appears under the swimsuit—he or she may instead have Seabather's Eruption from stinging larvae of sea critters such as jellyfish or sea anemone. Stop rubbing and shower instead.

Don't scratch. Trim your child's fingernails and discourage scratching. Home treatments such cool compresses on the affected areas, Epsom salt or oatmeal baths, or baking soda paste may help to relieve the discomfort. If itching is severe, talk with your child's pediatrician. He or she may suggest prescription-strength lotions or creams to reduce your child's symptoms.
7. Cutaneous Larva Migrans (Sandworms)
Sandworms may be present in sand contaminated with feces from pets or stray animals. When a child stands or sits in contaminated sand on a beach or in a sandbox, the worms may burrow under the skin, usually around the feet or buttocks. Lines of itchy, reddish rash known as a creeping eruption appear as the worms move under the skin, up to a few centimeters a day. The condition is more common subtropical and tropical areas such as the Caribbean, as well as parts of the southwestern United States.
What parents can do:
Keep shoes on.
 Don't let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn't sit in the sand without a blanket or towel.
Don't let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn't sit in the sand without a blanket or towel.Talk with your pediatrician. Your pediatrician can prescribe anti-parasitic medications such as albendazole or ivermectin to treat the rash. Without treatment, the larvae usually will die off in 5 to 6 weeks. Your pediatrician may suggest a cream to help relieve itching.
8. Folliculitis (Hot Tub Rash)
Folliculitis (hot tub rash) is an itchy, pimply rash that occurs when bacteria in unclean pools and hot tubs gets into hair follicles on the skin. The area where hairs grow from the skin becomes infected and inflamed, sometimes forming small, pus-filled blisters. A similar rash may come from wearing a damp swimsuit that wasn't washed and dried well after previous use. Hot rub rash typically starts 12-48 hours after being in a hot tub.
What parents can do:
Avoid dirty pools. If you're unsure whether the acid and chlorine levels are properly controlled in a heated pool, don't allow your child to go in.
Don't allow young children in spas or hot tubs. In addition to the risk for drowning and overheating, young children are also at higher risk of bacterial skin infection because they tend to spend more time in the water than teens or adults.
Talk with your pediatrician. Hot tub rash usually clears up without medical treatment. In the meantime, warm compresses and an over-the-counter anti-itch cream recommended by your pediatrician can help your child be more comfortable. If your child's rash lasts more than a few days, talk with your pediatrician.
9. Molluscum Virus
Molluscum contagiosum is a viral infection that causes pearly bumps on the skin on a child's chest, back, arms or legs. The dome-shaped bumps, also known as "water warts," may have a dimple in the center. The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
What parents can do:
Wait it out. In most cases, molluscum contagiosum does not need treatment. The bumps usually will go away in 6 to 12 months.
Stop the spread. A child with molluscum contagiosum should not share towels, bedding, or clothing with others to avoid spreading the virus. The bumps are contagious as long as they are present.
Avoid scratching. Scratching the bumps can spread the virus and cause a second, bacterial infection where the skin is open.
10. Juvenile Plantar Dermatosis (Sweaty Sock Syndrome)
A smooth, reddened rash on your child's feet, sometimes with peeling, cracking skin or scaly skin, could be from a condition called Juvenile Plantar Dermatosis (Sweaty Sock Syndrome). It happens when feet get wet and then dry quickly, again and again—like when shoes are taken on and off coming in and out of the house during summer.
What parents can do:
Breathable footwear. Reduce how often the feet go from wet to dry quickly by having your child wear open or more breathable footwear made of materials like mesh or cotton (i.e., water shoes) and/or thicker more absorbent socks.
Apply ointment. Applying moisturizing ointment or an over-the-counter steroid cream to the affected areas of your child's foot immediately after taking shoes off or getting out of water can help. If the condition does not improve, or if you notice any sign of infection where your child's skin is cracking, talk to your pediatrician.
11. Tinea (Ringworm)
Despite having "worm" in its misleading name, tinea (ringworm) is an infection caused by a fungus that thrives in warm, damp conditions. It is similar to athlete's foot and jock itch and can appear on a child's scalp or other parts of the body. It's called ringworm because the rash from the infection tends to form round or oval spots that become smooth in the center as they grow while the border remains red and scaly. The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
What parents can do:
Stop the spread. Check and treat any pets that may have the fungus—look for scaling, itchy, hairless areas on their fur. Family members, playmates, or schoolmates who show symptoms also should be treated. Do not allow your child to share combs, brushes, hair clips, barrettes, or hats. Make sure mats used in sports like wrestling and gymnastics are properly disinfected after use.
Talk with your pediatrician. A single ringworm patch on the body can be treated with an over-the-counter cream recommended by your pediatrician. If there are any patches on the scalp or more than one on the body, or if the rash is getting worse while being treated, your pediatrician may prescribe a stronger medication and special shampoo.
12.
 Hand, Foot & Mouth Disease
Hand, Foot & Mouth DiseaseMany parents assume virus season winds down after winter. But some viral illnesses, such as hand, foot, and mouth disease, are more common during summer and early fall. Outbreaks are most common in younger children and can spread in child care centers, preschools, and summer camps. Caused by Enterovirus coxsackie, the illness starts with a fever, sore throat, and runny nose—much like the common cold—but then a rash with tiny blisters may appear on any or all the following places on the body:
In the mouth (inner cheeks, gums, sides of the tongue or back of the mouth)
Fingers or palms of hands
Soles of feet
Buttocks
Symptoms are the worst in the first few days, but they are usually gone within a week. Peeling skin on the fingers, toes, and nails may begin after a week or two, but it is harmless. Parents of children with a history of atopic dermatitis or eczema should be aware that their children may be prone to a more severe outbreak.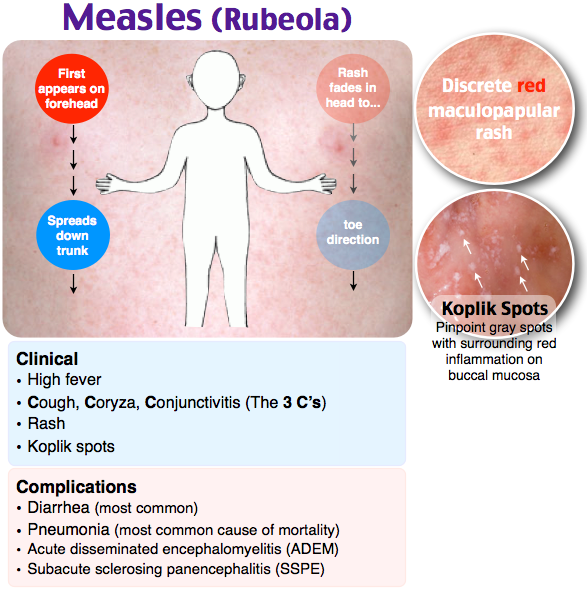
What parents can do:
Monitor symptoms. Be sure to call your pediatrician if your child's fever lasts more than 3 days or if he or she is not drinking fluids. If symptoms are severe, your pediatrician may collect samples from your child's throat for lab testing.
Ease the pain. For fever and pain, the pediatrician may also recommend acetaminophen or ibuprofen. Liquid mouth-soothing remedies may be useful to alleviate mouth ulcer pain. Do not use regular mouthwashes, because they sting.
Avoid dehydration: Children with hand, foot, and mouth disease need to drink plenty of fluids. Call your pediatrician or go to the ER if you suspect your child is dehydrated. See Signs of Dehydration in Infants & Children for more information.
Inform others. Tell child care providers and playmates' parents to watch for symptoms of the illness.
 Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child's fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child's fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Remember…
Protecting your child's skin is a year-round concern, but it's especially important in the summer months when so much skin is exposed and vulnerable. Fortunately, many summertime rashes clear up quickly on their own. Be sure to talk with your pediatrician about any rash that you're unsure about—especially if you don't know what caused it, if it is making your child feel miserable or doesn't clear up quickly, or if it shows signs of infection or is accompanied by any shortness of breath.
Additional Information:
- Summer Safety Tips: Staying Safe Outdoors
- Antibiotic Prescriptions for Children: 10 Common Questions Answered
- American Academy of Dermatology
- American College of Allergy, Asthma & Immunology
- Society for Pediatric Dermatology
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Red pimples on the face of a newborn: symptoms, causes and treatment
A rash on the face of a newborn is a common occurrence, which is considered a sign of the baby's adaptation to the environment. In most cases, rashes go away on their own and require only competent care without the use of drugs. How to distinguish harmless red pimples from dermatological diseases and allergies? How to understand that the rash will pass by itself, and what signs are a reason to see a doctor?
Allergic rash in a newborn
An allergy in an infant is an unfavorable immune response of a child's body to a potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberries;
- nuts.

The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.
Neonatal acne
Neonatal acne may appear in the first weeks of a child's life on the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the reason for the appearance of acne is increased production of sebum, which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system. The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Sweating
Sweating is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small vesicles with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Prickly heat in itself is not dangerous for the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection. In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn. These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
In fact, the disease is caused by a high content of maternal hormones in the blood or a change in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only to take care of proper care , but diligently removing the crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns. He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Milk crust cream which helps to completely remove milk crusts in an average of 7 days [5. 3].
3].
Atopic dermatitis
Atopic dermatitis is an allergic disease accompanied by chronic skin inflammation . The causes of uncontrolled allergic reactions in infants are:
- food allergens - animal protein, soy products, some types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.
Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.1]
- Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper area zone in infants. The rash appears as a result of prolonged contact of the body with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious). The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
For non-drug treatment of pathology, air baths [7], bathing in a decoction of string and celandine [8], and thorough hygiene procedures are indicated. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, repairs and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
____________________________________________________________________________________________
Literature:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Herani M.I., Ando I. Acne in infancy and acne genetics // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3. Zanko NI Efficiency of new technologies for skin care in young children: Abstract of the thesis. dis. ... cand. honey. Sciences, M., 2000
4. Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis.
N Engle Gee Med. 360(4):387-96 (2009 January).
5. Results of the study 1035 F4.
5.1 Study results 1016F10.01.02
5.2 Study results 1008F4.01.16
5.3 Study results 1042F3.01.24
Dermatol. 2005; 53: S214-S219.
7. Galliamova Yu.A. Diaper dermatitis and skin trauma in children. Attending doctor. – 2013; 9: 42-6.
– 2013; 9: 42-6.
8. Zverkova F.A. Skin diseases in young children. SPb.: Sotis, 1994.
9. Tamrazova OB, Zaslavsky DV Diseases of the sebaceous glands in infants. Medical advice. 2019; 2:152-160.
10. Atopic-prone skin: latest discoveries (Laboratoire Expansion Center for Development and Research)
11. Inhibits the synthesis of inflammatory mediators. “A study of the activity of sunflower oil distillate on inflammatory mediators. June 2010»
Skin rashes in babies - contraindications to vaccination
Dear Parents! Your baby needs to see a pediatrician on the day of vaccination . Of course, the child must be healthy , he needs to measure his body temperature the night before and in the morning before leaving the house and examine the skin. In the presence of skin rashes, vaccination is most often delayed, as this is a contraindication for most vaccines. Therefore, we recommend that parents be careful about skin rashes in their baby and always discuss the cause of their appearance with health workers.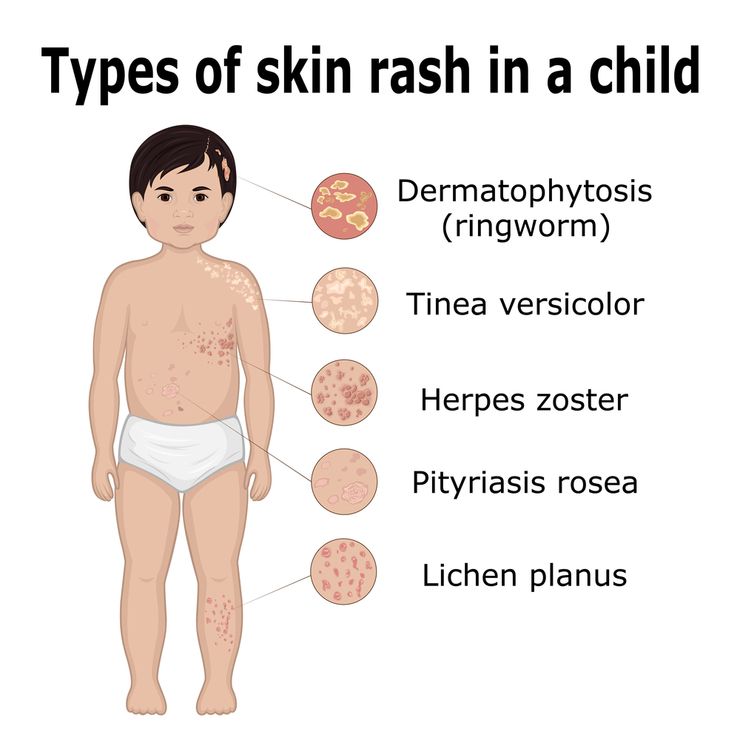
Due to the frequent occurrence at appointments before vaccination of situations when parents of babies do not pay attention to skin manifestations in a child and come to an appointment on the day of vaccination, we suggest that you familiarize yourself with the causes of skin rashes in children.
Since the most intensive vaccination schedule is available for children in the first year of life, we will consider the causes of rash in young children (up to 3 years). But even at an older age, parents should not neglect the rule - we vaccinate children against the background of complete health, the absence of acute manifestations of the disease, if there are indications - against the background of the necessary medical preparation, in most cases - against the background of following a hypoallergenic diet.
So, the causes of skin rashes in young children:
- Allergic rash
- Intertrigo (diaper rash)
- Prickly heat
- Eruptions on the skin due to parasitic infestations
- Rash in infectious diseases
- Hemorrhagic eruptions in diseases of the blood and vessels
- Insect bites
Allergic rash
The most common cause of rashes in children of the first year of life is food allergy, the manifestations of which are diverse:
- rash of different shape and brightness on the body, more often on the cheeks,
- redness, peeling of the skin, accompanied by itching,
- persistent diaper rash,
- gneiss on the scalp and eyebrows, persisting after the 3-4th month of a baby's life,
- copious prickly heat with slight overheating,
- appearance on the skin of blisters similar to nettle burn (urticaria),
- the appearance of swelling of the skin, subcutaneous fat and mucous membranes (angioedema).

In recent years, the number of children with skin manifestations of allergies has been growing. An increased risk of food allergies exists in children in whose families cases of allergies have already been recorded. In the presence of allergic diseases on the part of both parents, the risk of allergies in a child is approximately 70-80%, in the presence of an allergic pathology on the mother's side - 60%, on the father's side - 30%, in the absence of allergic problems on the part of the parents - from 10 to 18 %. In addition to hereditary factors, allergic reactions in an infant can be caused by fetal hypoxia (oxygen deficiency) during pregnancy and childbirth, a quick transition to artificial feeding, acute respiratory viral and intestinal infections suffered by the baby, followed by a violation of the composition of the intestinal microflora.
The occurrence of food allergies in children of the first year of life is associated with the functional features of their digestive tract: low enzyme activity, low production of IgA - protective antibodies located on the surface of the mucous membranes of the gastrointestinal tract. They provide local protection of the intestinal mucosa from foreign agents. With the introduction of complementary foods (individually for each child - from 4-6 months of life), further maturation of enzyme systems occurs. In case of violation of the terms and rules for the introduction of complementary foods, fermentopathy, imbalance of the microflora in the intestine, the appearance of rashes on the skin associated with an inflammatory reaction in the intestinal wall, requiring correction and treatment, may occur.
They provide local protection of the intestinal mucosa from foreign agents. With the introduction of complementary foods (individually for each child - from 4-6 months of life), further maturation of enzyme systems occurs. In case of violation of the terms and rules for the introduction of complementary foods, fermentopathy, imbalance of the microflora in the intestine, the appearance of rashes on the skin associated with an inflammatory reaction in the intestinal wall, requiring correction and treatment, may occur.
And of course, allergic reactions in breastfed children are associated with eating disorders of the nursing mother, with her excessive consumption of highly allergenic foods.
The so-called food diary helps to identify the causative allergen, in which the mother regularly (at least 14 days) notes all types of food and drink received by her or the baby during the day, indicates the composition of the dishes, the features of their culinary processing, feeding time and the appearance of unwanted reactions ( loose stools, regurgitation, skin rashes, etc. ). In children after a year, rashes are noted on the introduction of foods such as sweets, chocolate, cakes, muffins and other industrial culinary products containing a large amount of dyes and preservatives, which often cause allergic manifestations on the skin, even in adults. Given the immaturity of the enzymatic systems of the digestive tract in young children, the immaturity of the immune system, these products are not recommended to be introduced into the diet of children under 3 years of age.
). In children after a year, rashes are noted on the introduction of foods such as sweets, chocolate, cakes, muffins and other industrial culinary products containing a large amount of dyes and preservatives, which often cause allergic manifestations on the skin, even in adults. Given the immaturity of the enzymatic systems of the digestive tract in young children, the immaturity of the immune system, these products are not recommended to be introduced into the diet of children under 3 years of age.
If your baby periodically has manifestations of food allergies on the skin, vaccination is postponed until the rash fades and is carried out against the background of taking antihistamines prescribed by a pediatrician or an allergist-immunologist a few days before and after vaccination. It is necessary to follow a hypoallergenic diet for a nursing mother and child at least 7-10 days before and after the proposed vaccination. According to the doctor's prescription, probably, to stabilize the skin process, it will be necessary to use external agents to treat the skin so that vaccination does not serve as a factor that provoked an exacerbation.
Intertrigo (diaper rash)
Diaper rash usually appears in large folds of skin, especially where a child's skin comes into contact with urine, feces, and diapers. Most often, diaper rash appears on the buttocks, in the inguinal-femoral folds, but sometimes the skin can turn red in a similar way in the axillary and cervical folds and even behind the ears. In advanced cases, cracks, erosions and sores may appear on the surface.
Prevention of diaper rash is the timely change of diapers and diapers, air baths. In case of diaper rash, the pediatrician, in accordance with the type of skin, will prescribe baths with decoctions of certain herbs, as well as a remedy for application after bathing in skin folds.
Prickly heat
Prickly heat is associated with the peculiarities of the structure and functioning of the sweat glands. Usually occurs in hot weather, when the child overheats due to fever, high air temperature or excessive wrapping.
Prickly heat appears on the skin with multiple small (1–2 mm) bright red spots. Rashes in babies often appear on the neck, chest and abdomen. The prickly heat of the baby practically does not bother, and if the rules of skin care are followed, it quickly disappears. Small manifestations of miliaria are not a reason for a medical withdrawal from vaccination if there are no infected elements.
Rashes in babies often appear on the neck, chest and abdomen. The prickly heat of the baby practically does not bother, and if the rules of skin care are followed, it quickly disappears. Small manifestations of miliaria are not a reason for a medical withdrawal from vaccination if there are no infected elements.
Rashes on the skin due to parasitic infestations
In infants, more often from the age of 6 months, infection with various parasites is very likely - pinworms, giardia, roundworms. Toxins, waste products of parasites, helminths are absorbed into the blood and are an allergenic factor, in most cases they can cause rashes on the skin of a child.
Only a pediatrician can identify this type of rash after an examination and necessary examinations, after which treatment is prescribed individually.
Rashes in infectious diseases
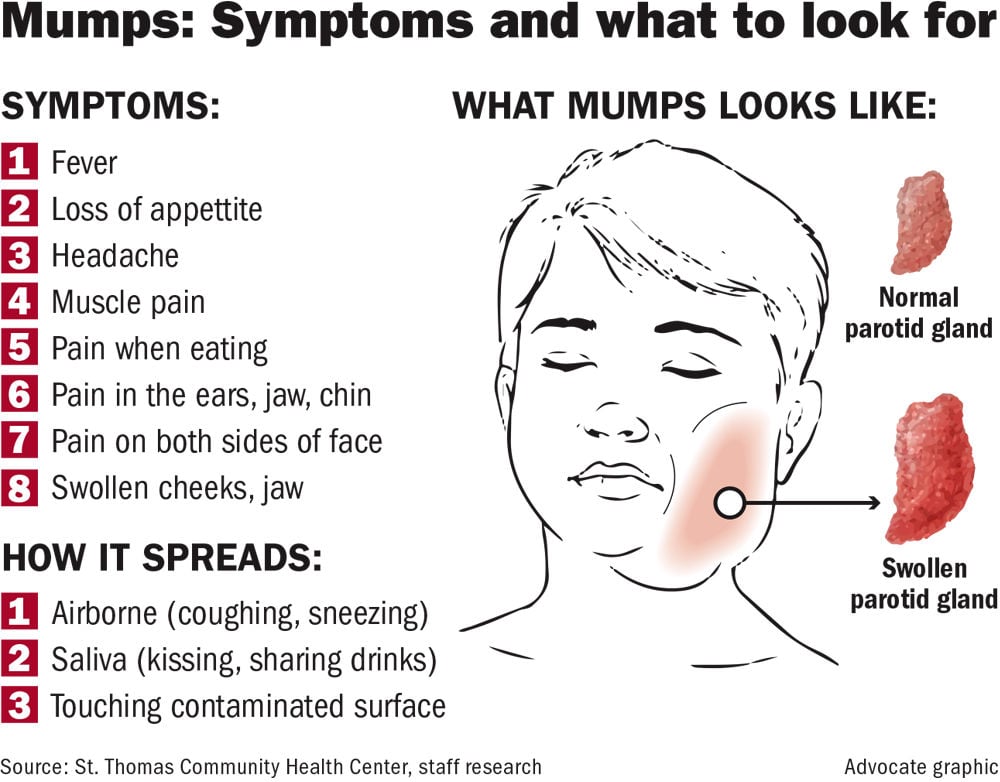
If the rash on the skin is accompanied by fever, chills, runny nose, general malaise, loss of appetite, if there has been contact with patients in the family or in a public place for 7–14 days, the child is likely to have manifestations of infection.
Rashes occur with such infectious diseases as: chicken pox, measles, rubella, scarlet fever, infectious mononucleosis, meningococcal infection, enterovirus infection and other viral diseases. To make a diagnosis, an examination of a child by a pediatrician must be carried out at home or in a special box in a children's clinic.
Hemorrhagic eruptions in diseases of the blood and vessels
In addition to infections, a rash occurs in diseases of the blood and blood vessels. Hemorrhagic rashes look like red or dark spots (bruises) that do not disappear when pressed. In the presence of a hemorrhagic rash, it is necessary to consult a pediatrician, a hematologist and conduct additional research methods.
Insect bites
Young children often suffer from mosquito and midge bites. Parents notice skin rashes in the morning, after the child wakes up or after walking in the forest park area. The appearance of pink or reddish spots is characteristic, mainly on open areas of the body, and the presence of elements on the face or on one half of it is obligatory (in the event that the child slept on his side).