What is a neonatal death
Neonatal death | March of Dimes
The most common causes of neonatal death are premature birth, low birthweight and birth defects.
An autopsy may help you find out why your baby died. You can choose whether or not you want to have an autopsy on your baby.
Your health care provider or a genetic counselor may help you learn why your baby died and if you may have the same problems in another pregnancy.
Getting counseling and support can help you cope with your baby’s death.
What is neonatal death?
Neonatal death is when a baby dies in the first 28 days of life. If your baby dies this soon after birth, you may have many questions about how and why it happened. Your baby’s health care provider can help you learn as much as possible about your baby’s death.
Neonatal death happens in about 4 in 1,000 babies (less than 1 percent) each year in the United States. Non-Hispanic black women are more likely to have a baby die than women of other races or ethnicities.
What are common causes of neonatal death?
The most common causes of neonatal death are:
- Premature birth. This is when a baby is born too early, before 37 weeks of pregnancy. Babies born too early may have more health problems than babies born on time.
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces. Babies born too small may have more health problems than babies born at a healthy weight.
- Birth defects. Birth defects are health conditions that are present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, how the body develops or in how the body works.
Premature birth and low birthweight cause about 1 in 4 neonatal deaths (25 percent). Birth defects cause about 1 in 5 neonatal deaths (20 percent).
Other causes of neonatal death include:
- Problems in pregnancy, like preeclampsia.
 This is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Signs and symptoms of preeclampsia include having protein in the urine, changes in vision and severe headaches.
This is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Signs and symptoms of preeclampsia include having protein in the urine, changes in vision and severe headaches. - Problems with the placenta, umbilical cord and amniotic sac (bag of waters). The placenta grows in your uterus (womb) and supplies the baby with food and oxygen through the umbilical cord. The amniotic sac contains the fluid that surrounds the baby in the womb.
- Infections, like sepsis. Sepsis is a serious blood infection.
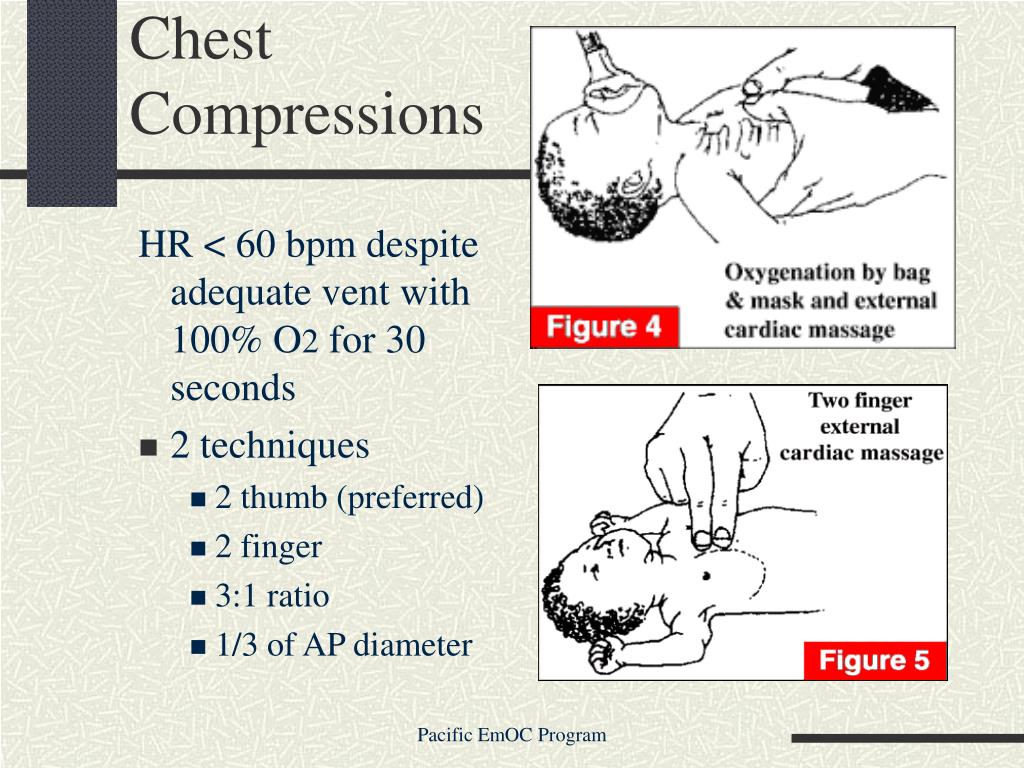
- Asphyxia. This is when a baby doesn’t get enough oxygen before or during birth.
Why are premature babies more likely to die shortly after birth than babies born on time?
Some premature babies may develop serious complications that can sometimes cause death.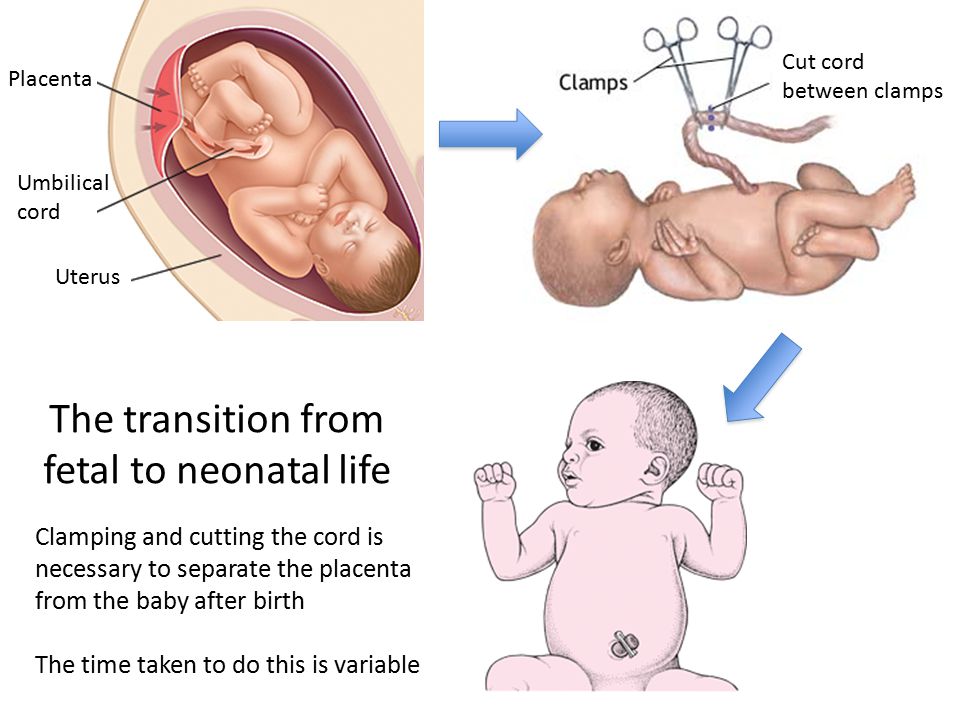 These complications include:
These complications include:
- Respiratory distress syndrome (also called RDS). This is a breathing problem most common in babies born before 34 weeks of pregnancy. Babies with RDS don’t have a protein called surfactant that keeps small air sacs in the lungs from collapsing. RDS causes about 825 neonatal deaths each year.
- Intraventricular hemorrhage (also called IVH). This is bleeding in the brain. Most brain bleeds are mild and resolve themselves with no or few lasting problems. More severe bleeds can cause serious problems for a baby.
- Necrotizing enterocolitis (also called NEC). This is a problem with a baby’s intestines. It can cause feeding problems, a swollen belly and diarrhea. It sometimes happens 2 to 3 weeks after a premature birth. It can be treated with medicine and sometimes surgery. But in serious cases, it can cause death.
- Infections. Premature babies often have trouble fighting off germs because their immune systems aren’t fully formed.
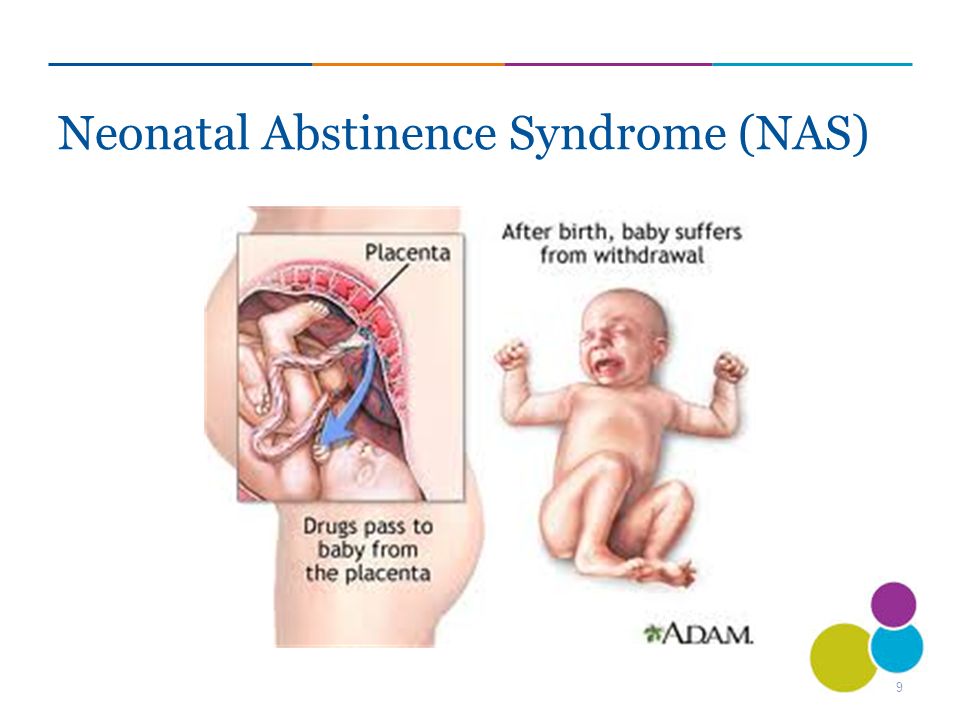 Infections that may cause death in a premature baby include pneumonia (a lung infection), sepsis and meningitis (an infection in the fluid around the brain and spinal cord).
Infections that may cause death in a premature baby include pneumonia (a lung infection), sepsis and meningitis (an infection in the fluid around the brain and spinal cord).
What birth defects most often cause neonatal death?
The most common birth defects that cause neonatal death include:
- Heart defects. Most babies with heart defects survive and do well because of medical treatments and surgery. But babies with serious heart defects may not survive long enough to have treatment, or they may not survive after treatment.
- Lung defects. A baby may be born with problems in one or both lungs or with lungs that aren’t fully developed. Lung defects can happen when the lungs don’t develop correctly due to other birth defects or pregnancy problems (such as not enough amniotic fluid). Premature babies can have lung problems that cause neonatal death.
- Genetic conditions. Genes are part of the cells in your body.
 They store instructions for the way your body grows, looks and works. Genetic conditions are caused by a gene that’s changed from its regular form. A gene can change on its own, or the changed gene can be passed from parents to children.
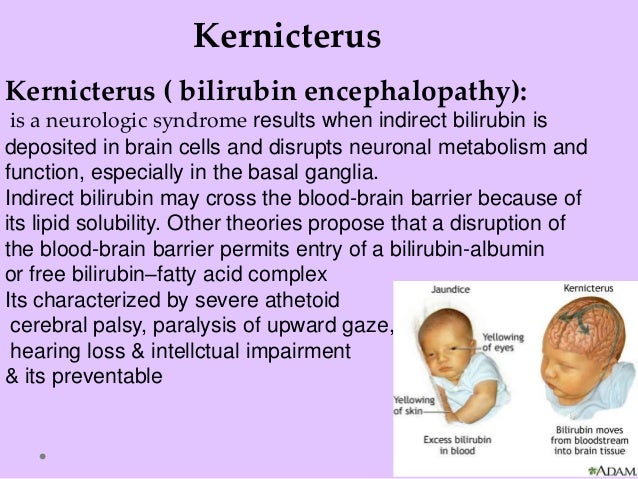
They store instructions for the way your body grows, looks and works. Genetic conditions are caused by a gene that’s changed from its regular form. A gene can change on its own, or the changed gene can be passed from parents to children. - Brain conditions. Neonatal death can be caused by problems in the brain, like anencephaly. This is a condition called a neural tube defect (also called NTD) in which most of a baby’s brain and skull are missing. Babies with anencephaly may be stillborn (when a baby dies in the womb after 20 weeks of pregnancy) or die in the first days of life. If you’ve had a baby with anencephaly, talk to your health care provider about taking folic acid to help prevent NTDs in your next pregnancy.
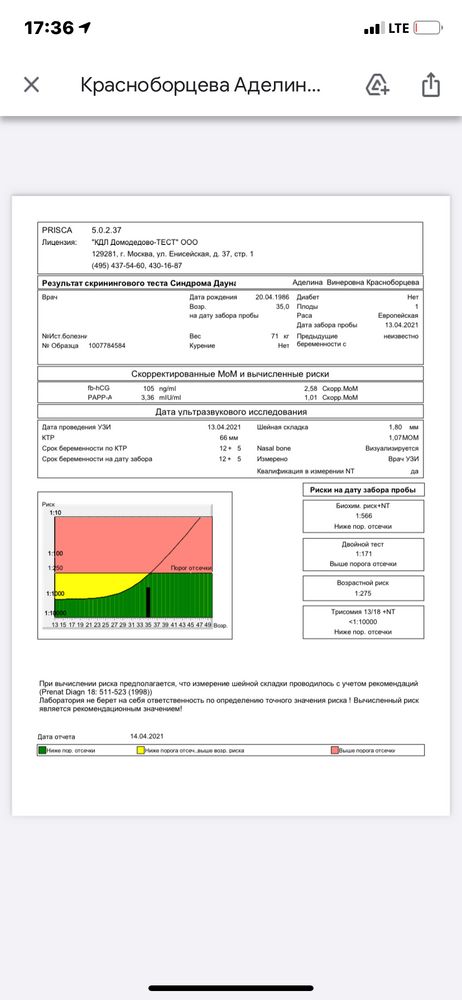
Your health care provider can use prenatal tests (medical tests you get during pregnancy) to check your baby for birth defects before birth. These tests include:
- Amniocentesis (also called amnio). In this test, your provider takes some amniotic fluid from around your baby in the uterus.
 The test checks for birth defects and genetic conditions in your baby. You can get this test at 15 to 20 weeks of pregnancy.
The test checks for birth defects and genetic conditions in your baby. You can get this test at 15 to 20 weeks of pregnancy. - Chorionic villus sampling (also called CVS). This test checks tissue from the placenta to see if your baby has a genetic condition, like Down syndrome. You can get CVS at 10 to 12 weeks of pregnancy.
- Ultrasound. This test uses sound waves and a computer screen to show a picture of a baby in the womb. It can help find birth defects like spina bifida, anencephaly and heart defects.
Do you need to have an autopsy on your baby?
Your baby’s health care providers can tell you what they know about what caused your baby to die. If you want more information, you may want to have an autopsy on your baby. An autopsy is a surgical exam of your baby’s body after death to help find the cause of death and any diseases or injuries. An autopsy gives information about why a baby dies in more than 1 in 3 cases.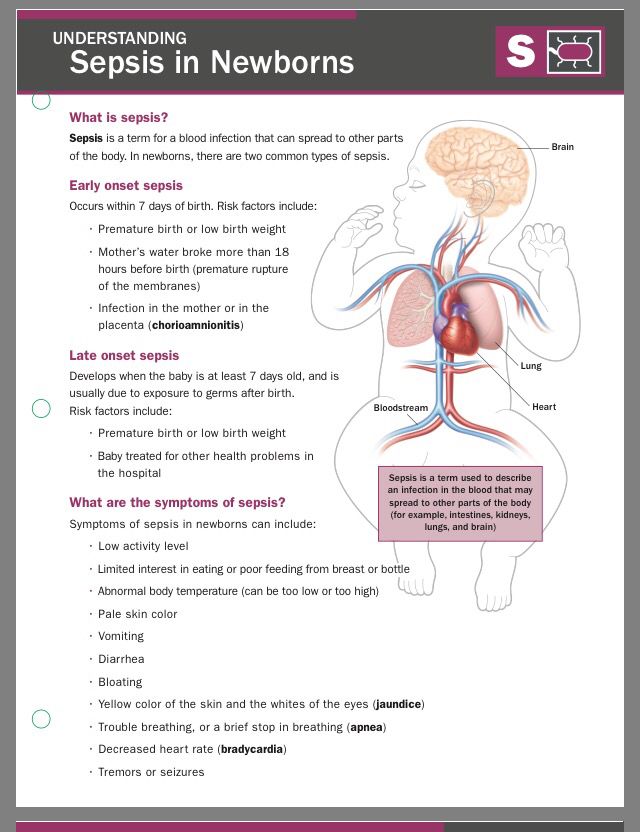 This information can be helpful to you if you think you may want to have another baby in the future. It’s your choice whether or not to have an autopsy on your baby. Families often have to pay for an autopsy, so ask your baby’s health care provider about payment. Some hospitals or states may pay for a baby’s autopsy; most health insurance companies don’t pay for one.
This information can be helpful to you if you think you may want to have another baby in the future. It’s your choice whether or not to have an autopsy on your baby. Families often have to pay for an autopsy, so ask your baby’s health care provider about payment. Some hospitals or states may pay for a baby’s autopsy; most health insurance companies don’t pay for one.
If you don’t want to have an autopsy, your baby’s health care provider may be able to use other tests to find more information about why your baby died. These tests include genetic tests, X-rays and tests on the placenta and umbilical cord.
If the cause of your baby’s death was a birth defect, you can meet with a genetic counselor to learn more about it. You also can learn about the chances of having another baby with the same birth defect. A genetic counselor is a person who is trained to help you understand about how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby’s health.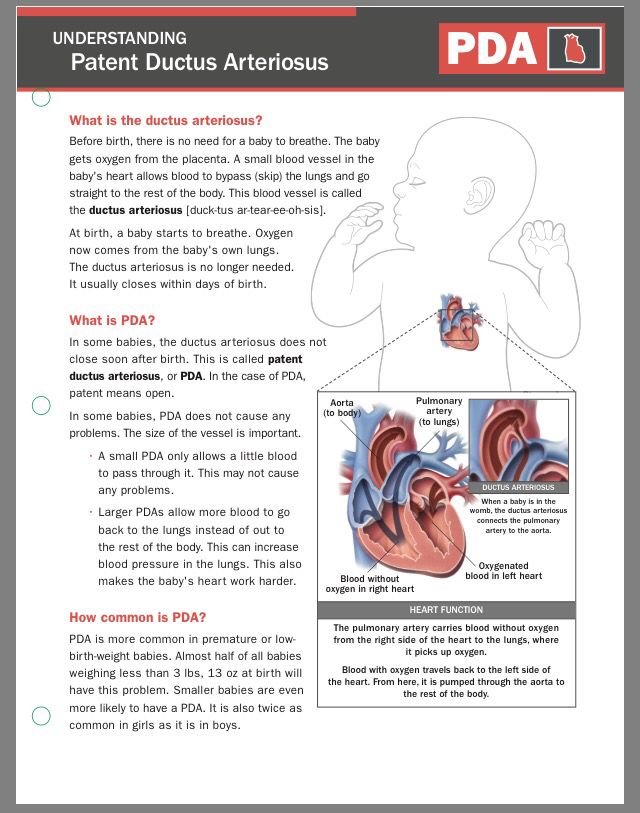
How can you deal with your grief?
Talking about your feelings may help you deal with the grief you feel about your baby’s death. Grief is all the feelings you have when a loved one dies. Visit shareyourstory.org, our online community where families who have lost a baby can talk to and comfort each other. Sharing your baby’s story may ease your pain and help you heal.
More information
- From hurt to healing (free booklet from the March of Dimes for grieving parents)
- Share Your Story (March of Dimes online community for families to share experiences with prematurity, birth defects and loss)
- Centering Corporation (general grief information and resources)
- Compassionate Friends (resources for families after the death of a child)
- First Candle (resources for families after the death of a child)
- Journey Program of Seattle Children’s Hospital (resources for families after the death of a child)
- Now I Lay Me Down to Sleep (remembrance photography)
- Perinatal Hospice & Palliative Care (resources for parents who find out during pregnancy that their baby has a life-limiting condition
- Share Pregnancy & Infant Loss Support (resources for families with pregnancy or infant loss)
- Star Legacy Foundation (resources for families who have had a stillbirth)
Last reviewed: October, 2017
What is a neonatal death?
What is a neonatal death? | Pregnancy Birth and Baby beginning of content5-minute read
Listen
A neonatal death is when a baby dies within the first 4 weeks after they are born.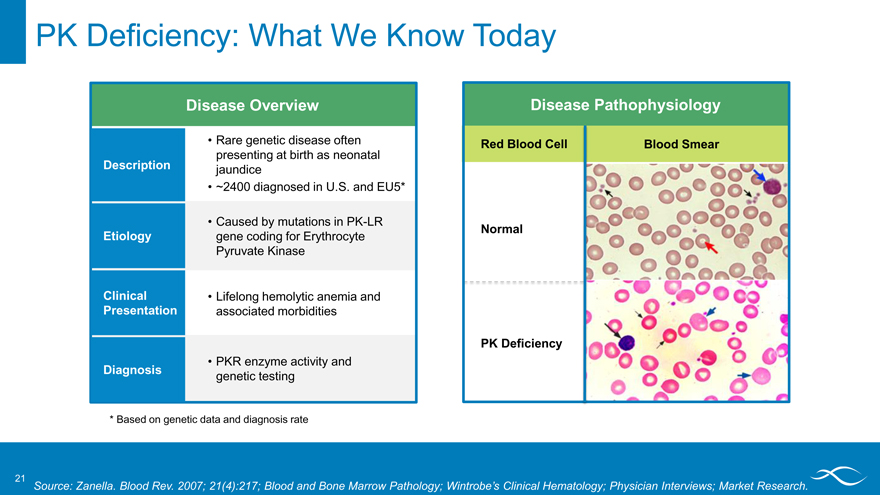 Dealing with a neonatal death can be very difficult for the whole family, but there is help and support available.
Dealing with a neonatal death can be very difficult for the whole family, but there is help and support available.
What is a neonatal death?
A neonatal death (also called a newborn death) is when a baby dies during the first 28 days of life. Most neonatal deaths happen in the first week after birth.
Neonatal death is different from stillbirth. A stillbirth is when the baby dies at any time between 20 weeks of pregnancy and the due date of birth.
Globally around 2.4 million children die in the first 28 days after birth. This is around half of all child deaths under the age of 5.
Neonatal death is rare in Australia, and rates are falling — there are about 700 neonatal deaths a year in Australia.
What are the causes of a neonatal death?
It’s not always known why a baby dies. However, the risk of neonatal death may be greater if a baby is born prematurely, is low birthweight, or has birth defects.
Prematurity and low birthweight cause about 1 in 4 neonatal deaths.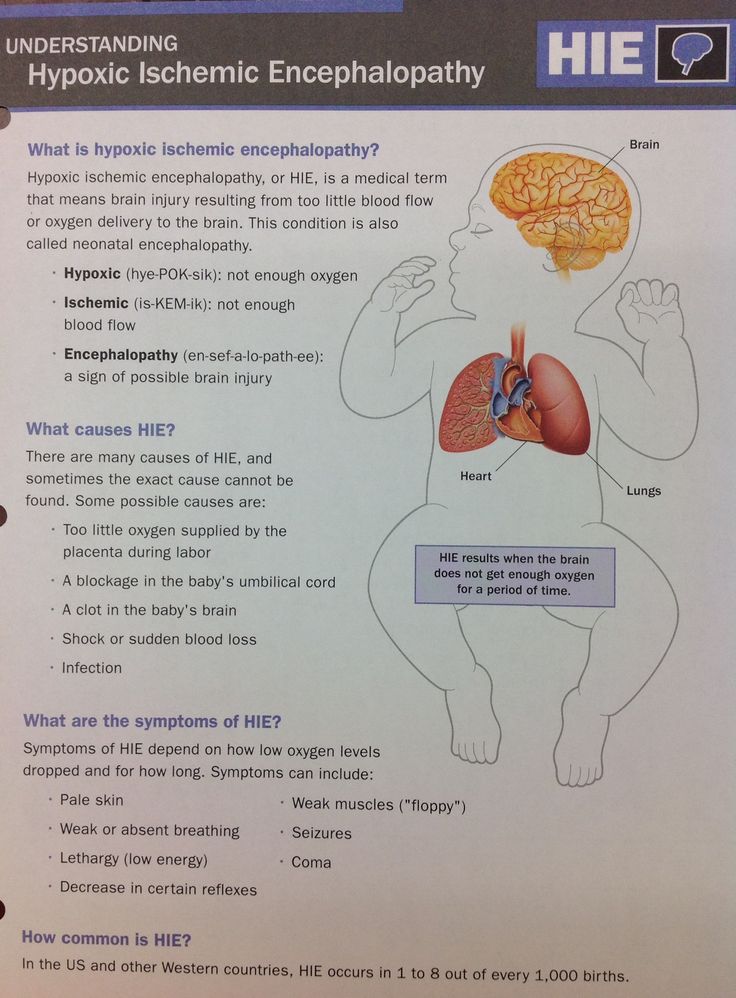 Premature babies can develop life-threatening complications such as breathing problems, bleeding on the brain, infections and problems in their intestines (necrotising enterocolitis).
Premature babies can develop life-threatening complications such as breathing problems, bleeding on the brain, infections and problems in their intestines (necrotising enterocolitis).
Low birthweight — if the baby weighs less than 2.5kg at birth — can also cause serious health problems such as difficulty breathing and feeding.
The most common birth defects that cause neonatal death include heart defects, lung defects, genetic conditions and brain conditions such as neural tube defect or anencephaly.
Sometimes a neonatal death may be caused by problems during the pregnancy, such as pre-eclampsia, problems with the placenta, or infections. It can also be caused by complications during the labour — for example, if the baby didn’t get enough oxygen.
What happens after a neonatal death?
If your baby dies, you might want to spend some time with them. You should take as long as you like. Some parents create memories of the baby by taking photos, handprints and footprints.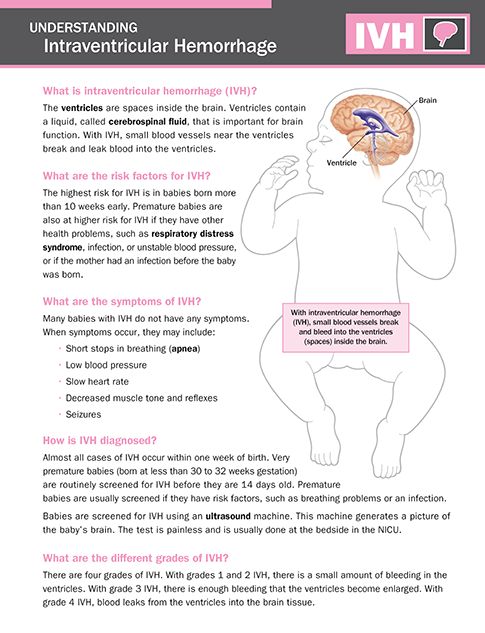
When you are ready to say goodbye, the hospital or a funeral director will take your baby to a funeral home. There will then be a burial or cremation.
By law, you must register both the birth and the death with Births, Deaths and Marriages in your state or territory.
In Australia, not all neonatal deaths are investigated by conducting an autopsy, also known as a post mortem examination. An autopsy is an examination to try to work out why the baby has died.
An autopsy cannot be done without the parents’ consent and it is up to you whether to agree to an autopsy after a neonatal death. The only time when an autopsy may be carried out without consent is if the case is referred to a coroner. This might happen if the death occurred in suspicious circumstances or if it was something to do with the health care the baby received.
An autopsy is done by a trained pathologist. If you agree to an autopsy, you can decide how detailed you would like it to be — whether it involves just examining the baby or removing organs to test why the death has happened.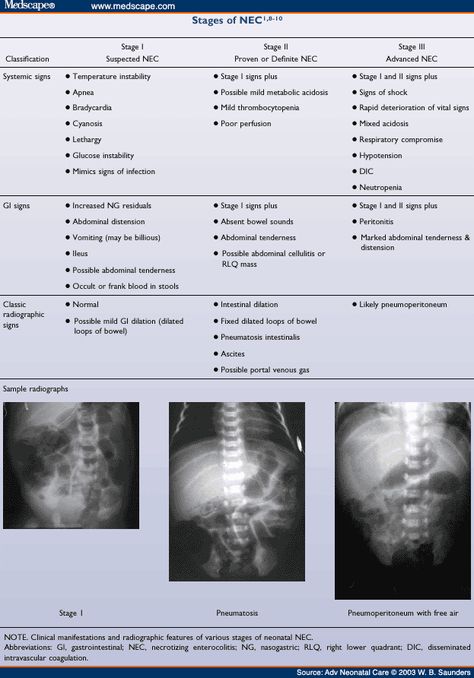
Sometimes no cause of death can be found, even after an autopsy. It’s a good idea to discuss the benefits and downsides of an autopsy with a doctor, midwife or social worker. They will guide you through what needs to be done and will answer any questions you might have.
Learn more here about what happens after a neonatal death and what changes might occur to your body.
Where to find help
The death of a newborn baby can be devastating, both for the parents and for the whole family. So it’s important to get as much support as possible to help you through this difficult time.
Your doctor, midwife, maternal child health nurse or social worker will be able to guide you through what happens after the baby has died.
Sands Australia provides information and support for anyone who has experienced stillbirth or newborn death. You can speak to someone 24 hours a day on their helpline, 1300 072 637.
Red Nose Grief and Loss has information and resources. You can call their helpline 24 hours a day on 1300 308 307.
Lifeline supports anyone having a personal crisis — call 13 11 14 or chat online.
Griefline provides telephone support — call 1300 845 745, Mon to Fri, 8am to 8pm (AEST).
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
World Health Organization (Newborn deaths and illnesses), Raising Children Network (Neonatal death - a guide), March of Dimes (Neonatal death), The Royal Women’s Hospital Melbourne (Learning why a baby has died), Queensland Courts (Reportable deaths), Australian Institute of Health and Welfare (Stillbirth and neonatal deaths in Australia), Sands (Stillborn and newborn death), myDr (Low-birth-weight babies)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Dealing with a neonatal death
- Birth trauma (emotional)
- Your body after stillbirth or neonatal death
Need more information?
Baby and Infant Death
Baby and Infant Death A neonatal death is when a baby is born alive but dies within the first 28 days of life
Read more on Gidget Foundation Australia website
Death of a baby - Better Health Channel
Miscarriage, stillbirth or neonatal death is a shattering event for those expecting a baby, and for their families. Grief, relationship stresses and anxiety about subsequent pregnancies are common in these circumstances.
Read more on Better Health Channel website
When Your Baby is Stillborn or Dies Soon After Birth | Guiding Light - Red Nose Grief and Loss
Read more on Red Nose website
Breast care for breastfeeding mothers after the death of a child | Sydney Children's Hospitals Network
Time after the death of your infant can be physically and emotionally exhausting
Read more on Sydney Children's Hospitals Network website
Smoking | Red Nose Australia
Read more on Red Nose website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.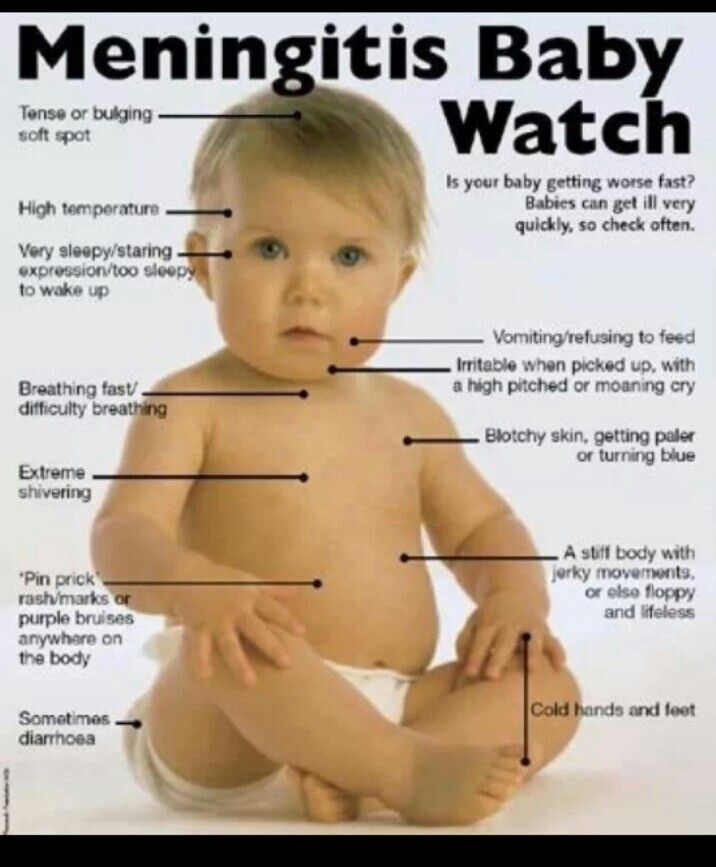
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Early neonatal mortality in the Russian Federation in 2010
The key to the success of perinatal care is objective knowledge about the number and causes of perinatal losses, the level and structure of which require systematic analysis, as they reflect the quality of obstetric and neonatal care. In addition, they are considered as an integral indicator of the level of socio-economic development of the country, the quality of life, the availability and quality of medical care, the effectiveness of the activities of health authorities and institutions.
The report is devoted to the analysis of early neonatal mortality, which was interpreted as the death of a child born at a gestational age of 28 weeks or more with a body weight of 1000 g or more and who died in the first 168 hours of life, and is based on an analysis of Rosstat data for 2000–2010. According to the WHO definition (ICD-10), the perinatal period begins at the 22nd completed week of pregnancy (154 days of fetal life, when the body weight normally reaches 500 g) and ends after 6 completed days (168 hours after birth). Consequently, newborns weighing less than 1000 g and who died during the 1st week of life were not registered in the state statistics bodies either as born children or as dead.
Analyzing the dynamics of perinatal mortality in the Russian Federation according to data for 2000-2010. (Table 1), , annual fluctuations in the absolute number of deaths in the perinatal period and stillbirths should be noted, with a constant decrease in the number of deaths in the early neonatal period. Indeed, the absolute number of newborn deaths and the average values of the early neonatal mortality rate in the Russian Federation tend to steadily decrease.
Indeed, the absolute number of newborn deaths and the average values of the early neonatal mortality rate in the Russian Federation tend to steadily decrease.
In 2000-2010 the rate of early neonatal mortality (calculated as the number of children who died in the first 6 days after birth, per 1000 live births) decreased by 57.8%. For comparison, we indicate the following data: the perinatal mortality rate during this time decreased by 44.1%, and the stillbirth rate - by 32.1%. The most pronounced rates of reduction in early neonatal mortality are observed in 2007 and 2008.
At the same time, there is also an annual decrease in the proportion of early neonatal deaths among all cases of perinatal death (see Table 1) . If in 2000 it was 49.5%, in 2010 it was almost 1 / 3 (37.3%). Such facts of a progressive decline in early neonatal death objectively reflect medical advances, both in obstetrics and neonatology.
When characterizing the indicators of early neonatal mortality, one more pattern should be emphasized - a progressive decrease in the number of dead newborns with an increase in life expectancy. Thus, the largest number of dead newborns in the early neonatal period is observed on the first day: in 2010 in the Russian Federation it amounted to 29.9% of the total number of early neonatal deaths (Fig. 1). Figure 1. The indicator of early neonatal mortality in the Russian Federation in 2010 depending on the age of the deceased. The abscissa shows age (days); the ordinate shows the proportion of total early neonatal mortality. The smallest number of dead newborns was noted at the age of 6 days (5.0%). Such changes, apparently, are due to an increase in the level of the child's viability as the child's body grows and matures, and at the same time, in our opinion, indicate the urgent need for organizing a resuscitation service for newborns in an obstetric hospital.
Thus, the largest number of dead newborns in the early neonatal period is observed on the first day: in 2010 in the Russian Federation it amounted to 29.9% of the total number of early neonatal deaths (Fig. 1). Figure 1. The indicator of early neonatal mortality in the Russian Federation in 2010 depending on the age of the deceased. The abscissa shows age (days); the ordinate shows the proportion of total early neonatal mortality. The smallest number of dead newborns was noted at the age of 6 days (5.0%). Such changes, apparently, are due to an increase in the level of the child's viability as the child's body grows and matures, and at the same time, in our opinion, indicate the urgent need for organizing a resuscitation service for newborns in an obstetric hospital.
The greatest number of reproductive losses is recorded in the earliest periods of gestation, and with increasing age of the fetus, the level of losses decreases.
In 2010, the number of deaths before 12 weeks of pregnancy was 72. 5%, at the period of 12-21 and 22-27 weeks 13.5 and 7.8%, respectively, the number of deaths in the early neonatal period was 2.3% of the total the number of prenatal (up to 28 weeks) and perinatal losses [1].
5%, at the period of 12-21 and 22-27 weeks 13.5 and 7.8%, respectively, the number of deaths in the early neonatal period was 2.3% of the total the number of prenatal (up to 28 weeks) and perinatal losses [1].
All over the Russian Federation in 2010 were born alive 1,788 948 children, 4948 children died in the first 168 hours. In accordance with this, the average value of the indicator of early neonatal mortality in the Russian Federation in 2010 was 2.75‰. At the same time, there are significant differences in its level in federal districts (Fig. 2). Figure 2. Indicators of early neonatal mortality in the federal districts of the Russian Federation in 2010 Far Eastern District. The lowest mortality rate (1.57‰) was registered in the Northwestern Federal District, the highest (6.32‰), which is 2.3 times higher than the national average, is observed in the North Caucasian Federal District.
For comparison, we point out that the highest rates of early neonatal mortality in 2000 were noted in Mauritania (52‰) and Liberia (48‰), while the lowest rates were in Austria, Germany, and Finland (2 per 1,000 live births) [2].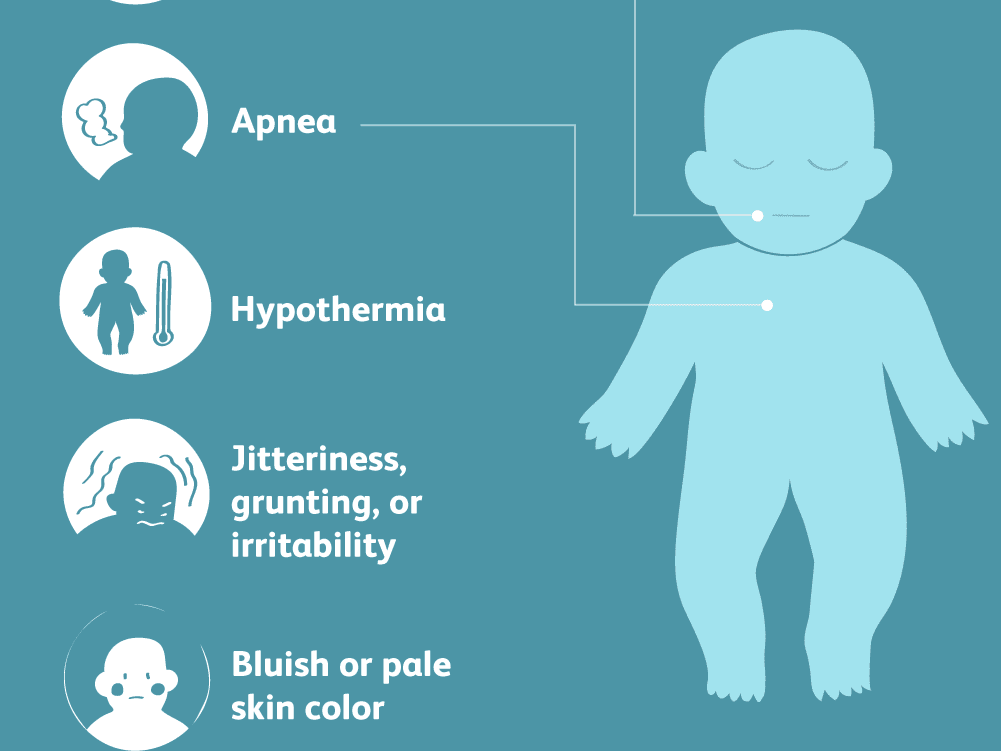 The average value of the early neonatal mortality rate, calculated by WHO on the basis of data for 192 countries of the world, in 2000 was 23‰.
The average value of the early neonatal mortality rate, calculated by WHO on the basis of data for 192 countries of the world, in 2000 was 23‰.
Even more significant differences in indicators of early neonatal mortality are determined in individual subjects of the Russian Federation. The minimum level of early neonatal mortality, or rather the absence of deaths in newborns in the first 6 days of life (0‰), was noted in the Nenets Autonomous Okrug, and the maximum (9.70‰) - in the Chechen Republic. In this regard, in order to analyze the regional characteristics of the mortality rate, the available range (0–9.7) of its values was divided by us into 3 parts, including 33% of the range of differences [3] and characterizing low (less than 3.23‰), medium (3 .23–6.46‰) or high (more than 6.46‰) mortality rate.
The distribution of subjects according to the level of early neonatal mortality is presented in tab. 2.
All federal districts, except for the North Caucasus and Far East, are characterized by the predominance of subjects with a low level of early neonatal mortality.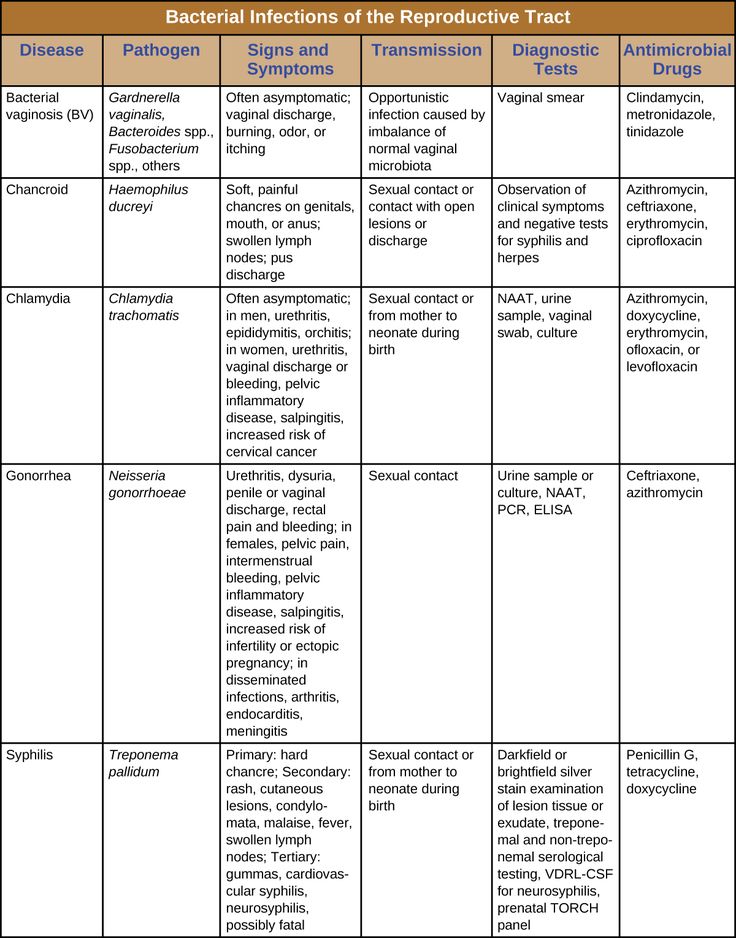 In the Central Federal District, there are 15 subjects (out of 18) with a low level and 3 (Bryansk, Lipetsk and Ryazan regions) with an average level. All 11 subjects of the Northwestern and 6 subjects of the Ural Federal District are characterized by a low level of early neonatal mortality. In the Southern District (6 subjects), one part of the regions has a low level, the other has an average level. Far Eastern District (9subjects) has 1 region with a high (Chukotka Autonomous Okrug - 8.01‰) and 5 with an average rate of early neonatal mortality. The most difficult situation is observed in the North Caucasian District, where in 3 regions (the Republic of Dagestan - 7.45‰, the Republic of Ingushetia - 6.4‰, the Chechen Republic - 9.7‰) high mortality rates were registered, in 3 - medium and in one - low (Kabardino-Balkarian Republic - 2.14‰).
In the Central Federal District, there are 15 subjects (out of 18) with a low level and 3 (Bryansk, Lipetsk and Ryazan regions) with an average level. All 11 subjects of the Northwestern and 6 subjects of the Ural Federal District are characterized by a low level of early neonatal mortality. In the Southern District (6 subjects), one part of the regions has a low level, the other has an average level. Far Eastern District (9subjects) has 1 region with a high (Chukotka Autonomous Okrug - 8.01‰) and 5 with an average rate of early neonatal mortality. The most difficult situation is observed in the North Caucasian District, where in 3 regions (the Republic of Dagestan - 7.45‰, the Republic of Ingushetia - 6.4‰, the Chechen Republic - 9.7‰) high mortality rates were registered, in 3 - medium and in one - low (Kabardino-Balkarian Republic - 2.14‰).
In general, in the Russian Federation, 59 (71.1%) subjects with low, 20 (24.1%) - with medium and 4 (4.8%) - with high levels of early neonatal mortality were noted.
An objective indicator of the assessment of the activities of health authorities and institutions is the characteristics of the causes of death. According to the regulations in force in 2010, in all cases of death of newborns born at a gestational age of at least 28 weeks and weighing at least 1000 g, medical certificates of perinatal death were drawn up (form No. 106-2 / y-98), on the basis of which the statistical form A-05 of Rosstat was formed. This form consists of cross tables, in which the main diseases and conditions of the child that caused death in the perinatal period are presented horizontally, and the diseases or conditions of the mother, complications from the placenta, umbilical cord and membranes, pathology of pregnancy and childbirth, which caused ( contributed to) the onset of death of the newborn (Table 3).
According to Rosstat, the most common cause of early neonatal death in 2010 is respiratory disorders (P22-P28 ICD-10) - 103.2 per 100,000 live births, which is 37.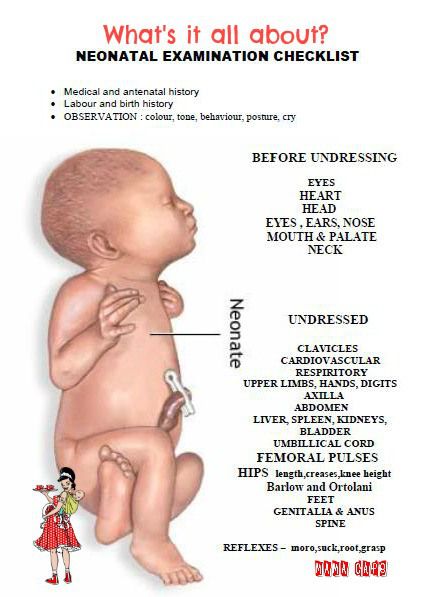 3%. More than half (57.0%) of observations in this group are related to hyaline membrane disease. Moreover, hyaline membrane disease (respiratory distress syndrome), according to Rosstat, was the most common cause of early neonatal death in Russia in 2010 and accounted for 21.3%. The group of respiratory disorders also includes congenital pneumonia, which ranks second (8.8%) among all causes of death.
3%. More than half (57.0%) of observations in this group are related to hyaline membrane disease. Moreover, hyaline membrane disease (respiratory distress syndrome), according to Rosstat, was the most common cause of early neonatal death in Russia in 2010 and accounted for 21.3%. The group of respiratory disorders also includes congenital pneumonia, which ranks second (8.8%) among all causes of death.
For the group "Congenital anomalies (malformations), deformities and chromosomal disorders" (Q00-Q99 ICD-10), the early neonatal mortality rate is 50.1 per 100,000 live births - 18.1% of all causes of death. In this regard, apparently, it is necessary to more carefully examine pregnant women and, during the perinatal consultation, evaluate the prognosis of the life of the newborn, in particular, with anencephaly, which accounts for 0.06% of all causes of death. The most common cause of death in newborns was heart disease: 35.9% of all developmental anomalies and 6.5% in the overall structure of causes of death.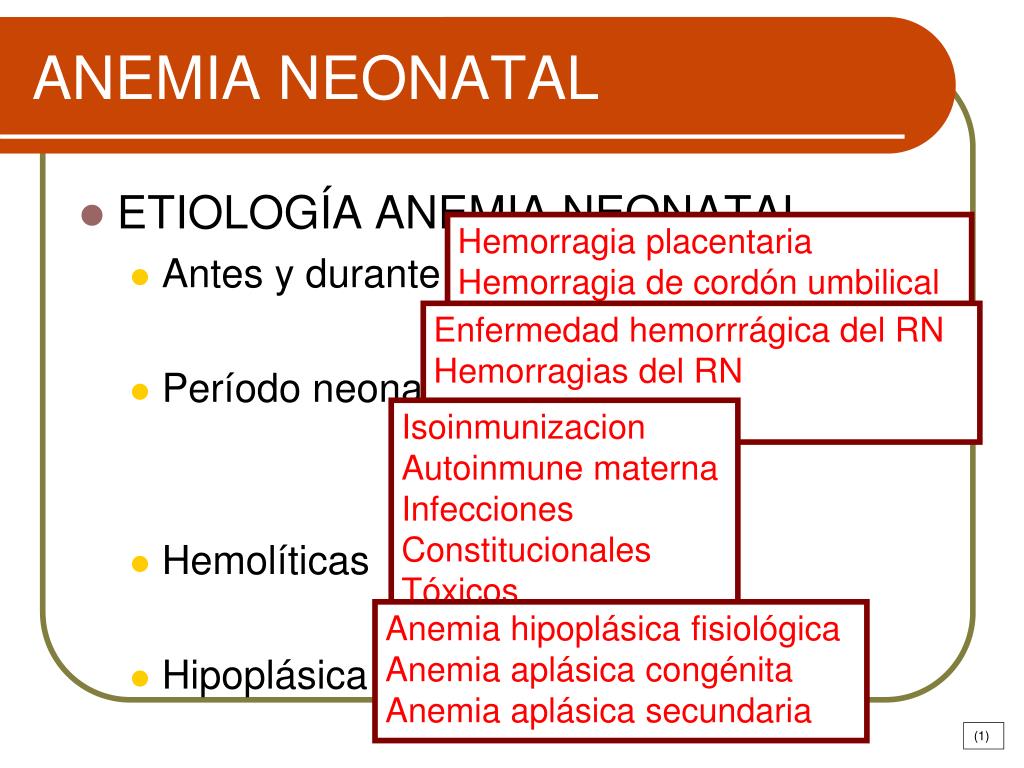 Congenital anomalies of the circulatory system and digestive organs as the initial cause of death account for 8.9 and 5.0% of all malformations, respectively. However, according to the literature [4], with timely diagnosis and surgical correction of congenital defects in the first hours and days of life, in 90% of cases, the life and health of the child can be saved.
Congenital anomalies of the circulatory system and digestive organs as the initial cause of death account for 8.9 and 5.0% of all malformations, respectively. However, according to the literature [4], with timely diagnosis and surgical correction of congenital defects in the first hours and days of life, in 90% of cases, the life and health of the child can be saved.
The third place among the causes of death is occupied by the group “Endocrine, metabolic and other disorders specific to the perinatal period”: the mortality rate is 36.3 per 100,000 live births, which is 13.1% among the causes of death. Such a significant number of deaths in this group, in our opinion, is due to the large number of various nosologies included in it, in particular, the observations "Extreme immaturity of the fetus" and "Other disorders associated with pregnancy and fetal growth." In our opinion, in order to obtain reasonable conclusions, the group “Endocrine, metabolic and other disorders specific to the perinatal period”, allocated in the statistical form A-05 of Rosstat, should be divided into independent groups.
In this regard, it should be noted that the problem of perinatal mortality in general and early neonatal mortality in particular is largely a problem of miscarriage, the main cause of which is extragenital pathology of pregnant women [5]. According to the literature [6], the survival rate among live births at 22–27 weeks does not exceed 12%.
At the same time, in the Russian Federation there is a paradoxical dynamics of perinatal and early neonatal mortality: the mortality rate of full-term newborns at the 1st week of life decreases to a lesser extent than that of preterm infants. According to L.P. Sukhanova [7], this situation indicates, first of all, the insufficient organization of perinatal care in case of timely delivery. Delivery of women with premature pregnancy is more often carried out in medical institutions that have the appropriate specialists and modern treatment and diagnostic technologies, while the vast majority of full-term fetuses and children are born in hospitals of the first and second levels, in some cases without the necessary resources to prevent and elimination of complications developing in childbirth.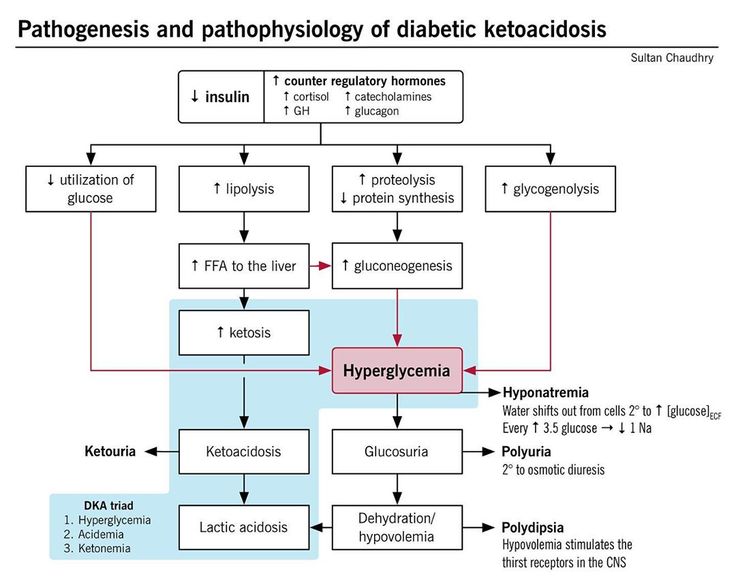
"Infectious diseases" (R35-R39 ICD-10) account for 9.9% of the causes of early death of newborns.
These include congenital sepsis (21.2%). Among all causes of death, congenital sepsis is 2.1%.
Among the causes that contributed to the death of a newborn, in 22.7% of cases, maternal diseases not related to pregnancy were indicated. Of these, 24.7% are infectious and parasitic diseases, 8.6% are diseases of the kidneys and urinary tract. At the same time, toxicosis of the second half of pregnancy was registered in 12.5% of cases (34.5 per 100,000 live births). However, they are noted in 39.6% of deaths from hyaline membrane disease.
Placenta pathology is indicated in 17.2% of cases. Most often it was about lesions of the placenta. At the same time, chorioamnionitis was detected only in 6.9 and 14.4% of deaths from congenital pneumonia and congenital sepsis, respectively.
According to Rosstat, in almost 1 / 3 cases of early neonatal death “the cause of the mother’s side has not been established”.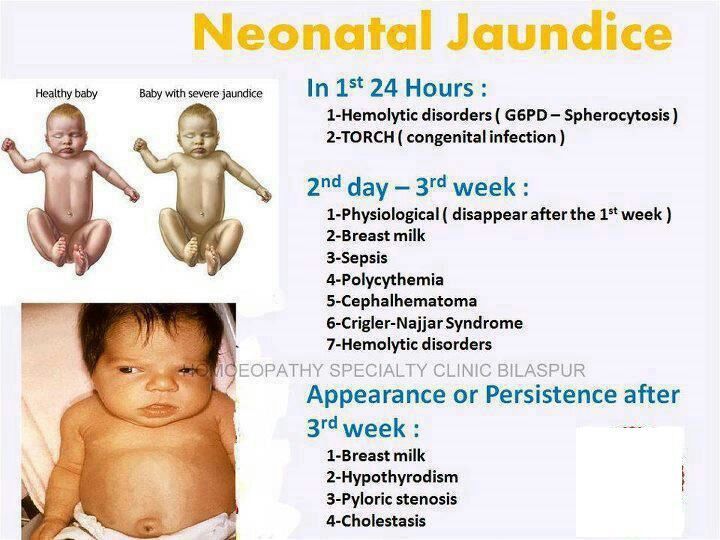 In this case, apparently, it is about the absence of an entry in paragraph 23 of the Medical Certificate of perinatal death. It should also be noted that in 0.7% of cases, caesarean section was indicated as the condition that caused the death of the child. In our opinion, most likely we are not talking about iatrogenic, but only about ascertaining the fact of the operation in the Medical certificate of perinatal death. However, in any case, such observations must be subjected to a thorough clinical and anatomical analysis.
In this case, apparently, it is about the absence of an entry in paragraph 23 of the Medical Certificate of perinatal death. It should also be noted that in 0.7% of cases, caesarean section was indicated as the condition that caused the death of the child. In our opinion, most likely we are not talking about iatrogenic, but only about ascertaining the fact of the operation in the Medical certificate of perinatal death. However, in any case, such observations must be subjected to a thorough clinical and anatomical analysis.
Thus, the analysis of the regional characteristics of early neonatal mortality indicates that in most subjects of the Russian Federation there is a positive trend in a significant decrease in its indicators. At the same time, the organization of perinatal care in Russia cannot be unified for all regions, since the high scatter of early neonatal mortality rates and the peculiarities of the structure of causes of death in the regions dictate the need for a differentiated approach to optimizing the maternal and child health service.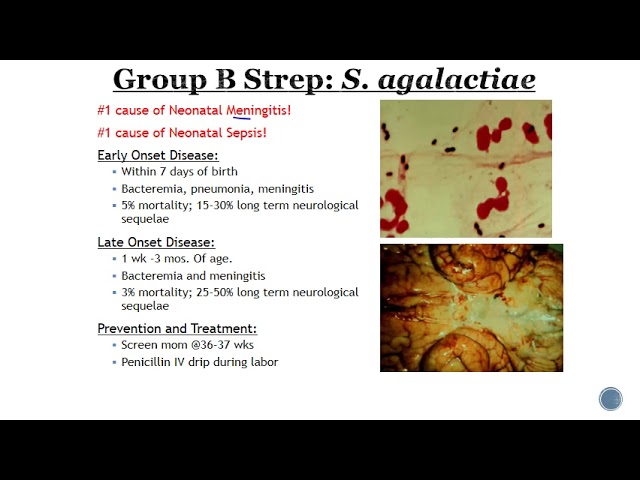 The main task in improving the health of the next generation should be to improve basic care for every woman and every newborn child. Along with this, it is necessary to constantly analyze the causes of early neonatal death through clinical and pathological comparisons.
The main task in improving the health of the next generation should be to improve basic care for every woman and every newborn child. Along with this, it is necessary to constantly analyze the causes of early neonatal death through clinical and pathological comparisons.
Infant mortality in the Russian Federation: statistics, causes, dynamics
In the last issue of Urology Digest N3-2016, we considered the issue of maternal mortality. Infant mortality has always been considered a “sensitive barometer” of the social well-being of society, according to which, as well as life expectancy, the general state of health and quality of life of the population and the level of socio-economic development and well-being of society as a whole are assessed. Together with the level of maternal mortality, it indicates the state of the reproductive health of the population, as well as the state of obstetric services and pediatrics.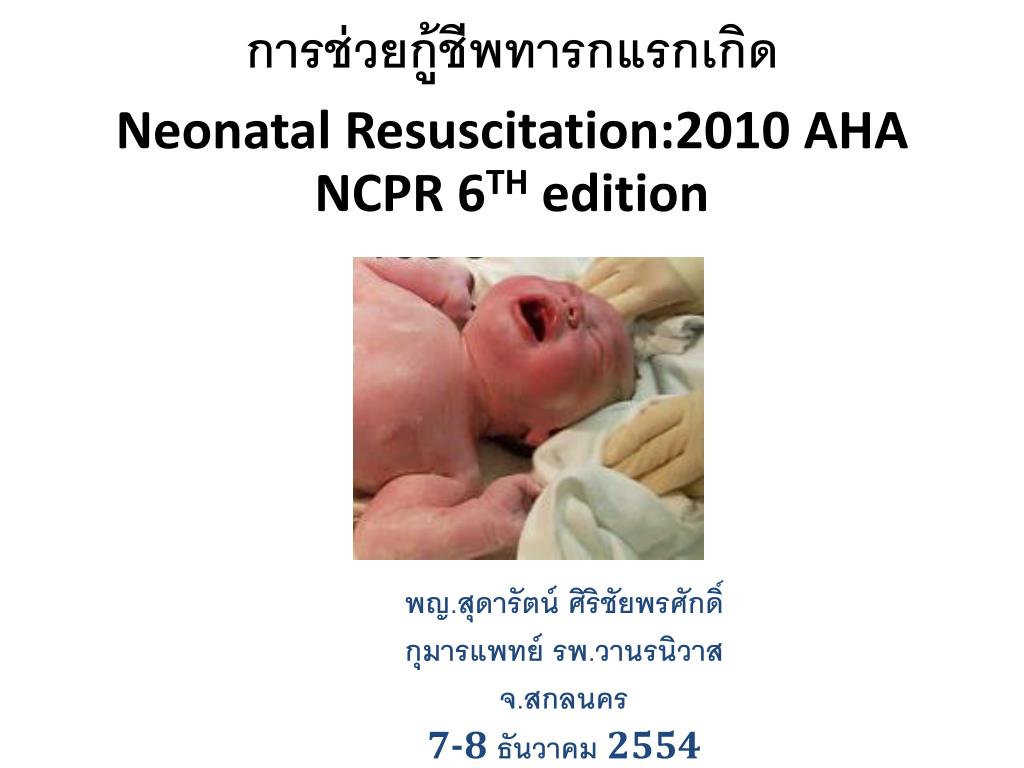
Statistics
Infant mortality characterizes the mortality of children in the first year of life. Mortality under the age of 1 year is much higher than the mortality rate at most ages: its probability in this period of time is comparable to the probability of death of people who have reached 55 years of age. At the same time, according to WHO, newborns account for 40% of all deaths of children under the age of five years. The majority of all deaths in the neonatal period (75%) occur in the first week of life, and 25-45% of them occur within the first 24 hours.
According to the WHO classification, there is the following distribution of periods of infant mortality (Fig. 1):
Infant mortality characterizes the mortality of children in the first year of life. Mortality under the age of 1 year is much higher than the mortality rate at most ages: its probability in this period of time is comparable to the probability of death of people who have reached 55 years of age.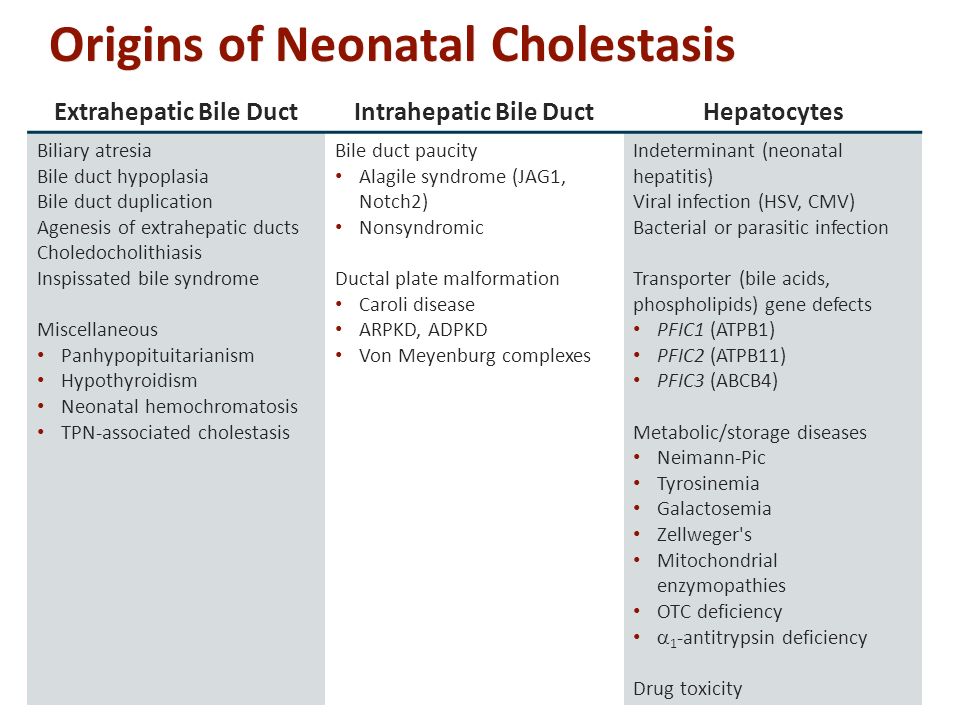 At the same time, according to WHO, newborns account for 40% of all deaths of children under the age of five years. The majority of all deaths in the neonatal period (75%) occur in the first week of life, and 25-45% of them occur within the first 24 hours. According to the WHO classification, there is the following distribution of periods of infant mortality (Fig. 1): perinatal period (from 22 weeks of pregnancy to 7 days of life (including early neonatal - from the moment of live birth to 7 days - given that when calculating neonatal mortality directly, the denominator contains only born alive, and perinatal - all born, including stillborns) late neonatal period (from 8 to 28 days of life) post-neonatal period (until the end of 1 year of life)
At the same time, according to WHO, newborns account for 40% of all deaths of children under the age of five years. The majority of all deaths in the neonatal period (75%) occur in the first week of life, and 25-45% of them occur within the first 24 hours. According to the WHO classification, there is the following distribution of periods of infant mortality (Fig. 1): perinatal period (from 22 weeks of pregnancy to 7 days of life (including early neonatal - from the moment of live birth to 7 days - given that when calculating neonatal mortality directly, the denominator contains only born alive, and perinatal - all born, including stillborns) late neonatal period (from 8 to 28 days of life) post-neonatal period (until the end of 1 year of life)
In addition, there is a separate period from age 1 to age 5, when death is classified as “child mortality”.
Fig. 1. Terminology for classifying deaths during pregnancy and early childhood
Calculation of indicators
Algorithms for calculating the infant mortality rate:
The formula adopted by the state statistics bodies in the Russian Federation (Fig.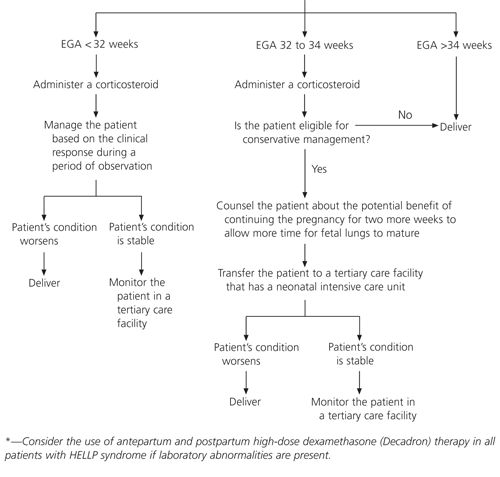 2):
2):
However, due to the fact that a child can be born in one calendar year (for example, in December 2015) and die in another calendar year (for example, in January 2016), the following calculation method is also used to determine the indicator: .3): By order of the Ministry of Health and Social Development of the Russian Federation of December 26, 2008 N 782n "On the approval and procedure for maintaining medical records certifying cases of birth and death", documents for registering infant mortality were approved by the "Medical death certificate" (f. 106 /u-08) and "Medical certificate of perinatal death" (f. 106-2/u-08).
Fig. 2. Algorithm for calculating the infant mortality rate adopted by the state statistics authorities of the Russian Federation
Fig. 3. WHO algorithm for calculating the infant mortality rate using the Rats formula
Dynamics in Russia
According to the latest data, in the first half of 2015 the infant mortality rate in Russia reached 6.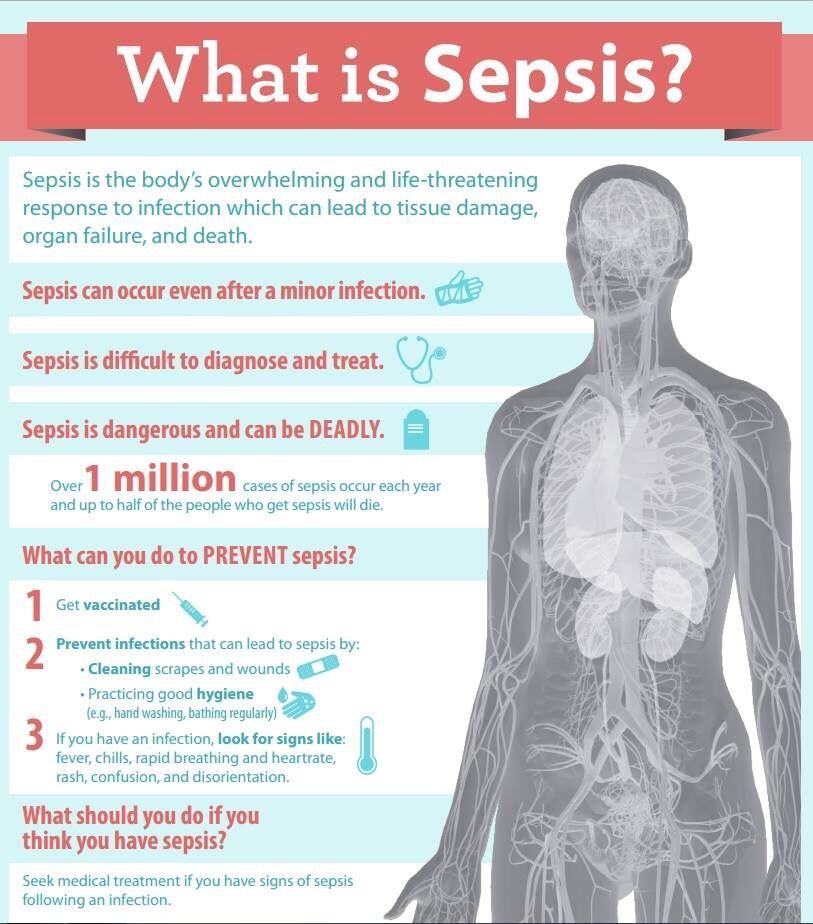 6 per 1,000 live births. Considering that this indicator is only semi-annual, the coefficient is really high. As Eduard Gavrilov, head of the Health Foundation, notes, “... such an increase in infant mortality was not even during the economic crisis of 2008 and in subsequent years.”
6 per 1,000 live births. Considering that this indicator is only semi-annual, the coefficient is really high. As Eduard Gavrilov, head of the Health Foundation, notes, “... such an increase in infant mortality was not even during the economic crisis of 2008 and in subsequent years.”
It should be noted that the dynamics of changes in the infant mortality rate in the Russian Federation is still not stable. In various periods of time, the Federal State Statistics Service of the Russian Federation notes both its decrease and increase (Fig. 4).
Fig. 4. Dynamics of changes in the infant mortality rate in the Russian Federation in the period 2008-2014
For example, in 2014 the infant mortality rate was 7.4 per 1000, which is lower than in 2013 – 8.2 per 1000 live births. At the same time, as the Deputy Director for Research of the Federal State Budgetary Institution Scientific Center for Obstetrics, Gynecology and Perinatology named after V.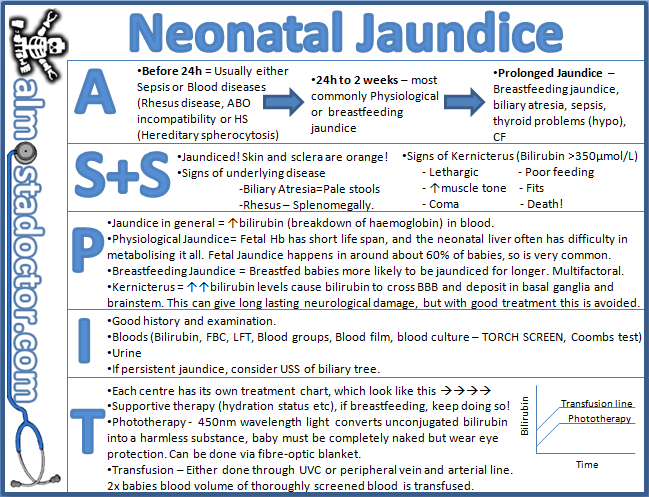 I. IN AND. Kulakova Dmitry Degtyarev, the decline in infant mortality is never synchronous in all regions. Thus, in the first half of 2013, infant mortality rates above the national average were observed in 25 regions (30.11%), in the first half of 2014 - in 16 (18.8%), and in the first half of 2015 an increase in infant mortality mortality rates were higher than the national average in 20 out of 85 regions, amounting to 23.5%.
I. IN AND. Kulakova Dmitry Degtyarev, the decline in infant mortality is never synchronous in all regions. Thus, in the first half of 2013, infant mortality rates above the national average were observed in 25 regions (30.11%), in the first half of 2014 - in 16 (18.8%), and in the first half of 2015 an increase in infant mortality mortality rates were higher than the national average in 20 out of 85 regions, amounting to 23.5%.
Fig. 5. Distribution by indicators of infant mortality in the Russian Federation depending on the place of residence
The infant mortality rate also differs depending on whether the woman in labor lives in the city or in the countryside (Fig. 5). As in the case of the statistics of the Federal State Statistics Service of the Russian Federation on maternal mortality, mortality rates among the rural population exceed those among the urban population.
Infant mortality by regions of the Russian Federation
As noted above, infant mortality rates vary by region as well. According to the Federal State Statistics Service of the Russian Federation on infant mortality in the constituent entities of the Russian Federation for the period January-December 2015, the districts with the highest infant mortality rate are the North Caucasian Federal (11.9‰ in 2014 and 10.3‰ in 2015) and Far Eastern Federal (9.1‰ in 2014 and 7.6‰ in 2015). Districts by the lowest indicator are Privolzhsky Federal (7.2‰ in 2014 and 6.1‰ in 2015) and Northwestern Federal - (5.8‰ in 2014 and 5.3‰ in 2015) ( Fig. 6)
According to the Federal State Statistics Service of the Russian Federation on infant mortality in the constituent entities of the Russian Federation for the period January-December 2015, the districts with the highest infant mortality rate are the North Caucasian Federal (11.9‰ in 2014 and 10.3‰ in 2015) and Far Eastern Federal (9.1‰ in 2014 and 7.6‰ in 2015). Districts by the lowest indicator are Privolzhsky Federal (7.2‰ in 2014 and 6.1‰ in 2015) and Northwestern Federal - (5.8‰ in 2014 and 5.3‰ in 2015) ( Fig. 6)
Fig. 6. Infant mortality by constituent entities of the Russian Federation in 2014 and 2015
Periods of infant mortality
Within the framework of the first year of human life, which considers the infant mortality rate, three periods are distinguished, differing both in the probability of death and in the structure of the dominant pathology.
The perinatal period is the period from the 22nd week of pregnancy to the end of the 7th day of extrauterine life.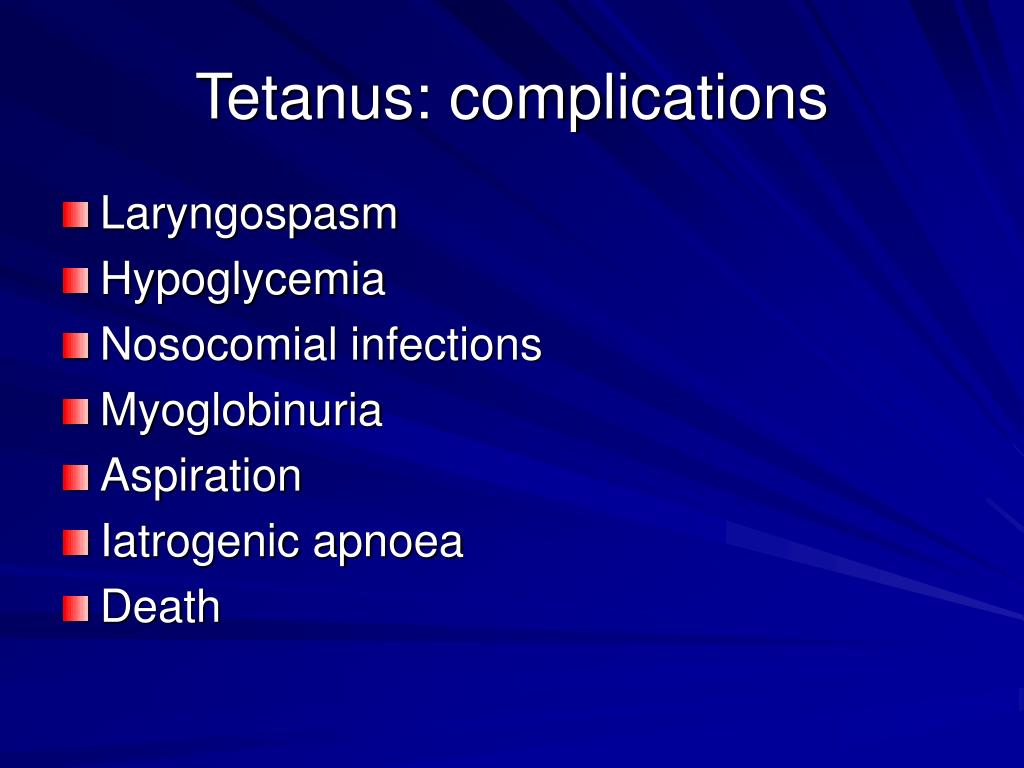 Separately, intranatal (from the time of the appearance of regular labor pains to the moment of ligation of the umbilical cord - 6-8 hours) and early neonatal periods (from the moment of live birth to 7 days of life) are distinguished in it. Difference: when calculating neonatal mortality, the denominator is only those born alive, when calculating perinatal - including stillborns. This period is the most important time in the life of the fetus and newborn, characterized by the highest risk of death (taking into account the fact that it includes children born prematurely). It accounts for up to 75% of deaths in the first year of life and up to 40% of all infant deaths under 5 years of age. The value of this indicator, especially in interregional and interstate comparisons, characterizes the level of a mother's reproductive health, her quality of life, the state of obstetric care, and many other aspects of medical and social development. It is also believed that with sharp fluctuations in the indicator, the dynamics of perinatal mortality indicates distortions in the statistics of infant mortality, since the number of deaths during this period correlates with the total number of births, both alive and dead.
Separately, intranatal (from the time of the appearance of regular labor pains to the moment of ligation of the umbilical cord - 6-8 hours) and early neonatal periods (from the moment of live birth to 7 days of life) are distinguished in it. Difference: when calculating neonatal mortality, the denominator is only those born alive, when calculating perinatal - including stillborns. This period is the most important time in the life of the fetus and newborn, characterized by the highest risk of death (taking into account the fact that it includes children born prematurely). It accounts for up to 75% of deaths in the first year of life and up to 40% of all infant deaths under 5 years of age. The value of this indicator, especially in interregional and interstate comparisons, characterizes the level of a mother's reproductive health, her quality of life, the state of obstetric care, and many other aspects of medical and social development. It is also believed that with sharp fluctuations in the indicator, the dynamics of perinatal mortality indicates distortions in the statistics of infant mortality, since the number of deaths during this period correlates with the total number of births, both alive and dead.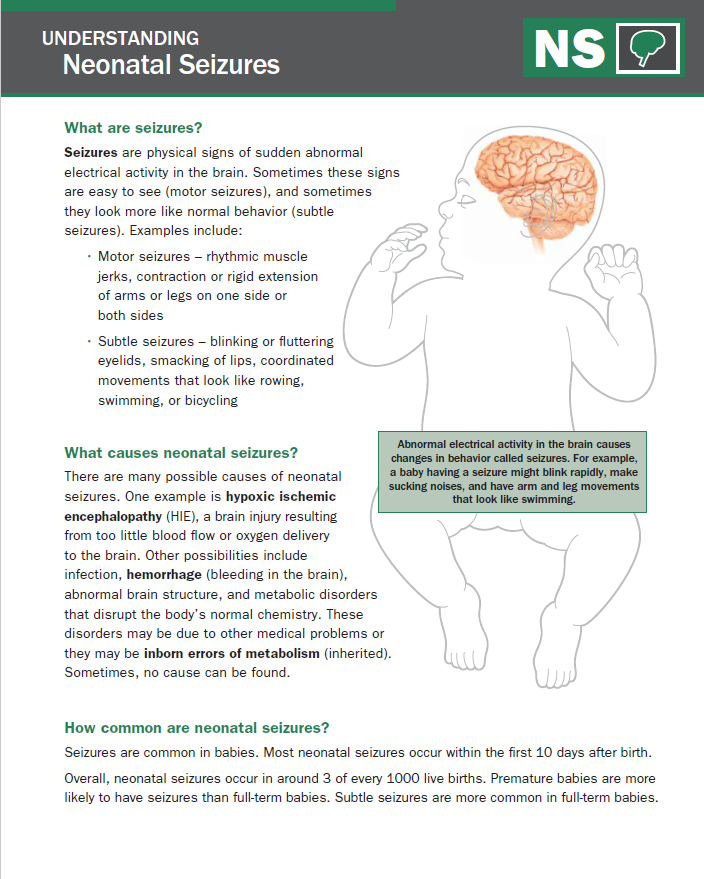
Since 2012, the Russian Federation switched to birth registration according to the WHO criteria (gestation period of 22 weeks or more, body weight at birth of a child of 500 g or more or less than 500 g in case of multiple births; body length of a child at birth of 25 cm or more - in if the birth weight of the child is unknown). Caring for these children represents a challenge of a new level of complexity and guides the search for solutions to reduce fetal loss, neonatal disability and infant mortality.
Causes of infant mortality in the perinatal period are usually divided into two groups:
- diseases or conditions of the mother or placenta, pathology of pregnancy and childbirth;
- diseases and condition of the fetus
The first group of causes includes complications from the placenta, umbilical cord and membranes - premature detachment of the placenta, pathology of the umbilical cord, etc.; such complications of pregnancy as toxicosis of the second half of pregnancy, premature rupture of amniotic fluid; directly complications of childbirth and delivery.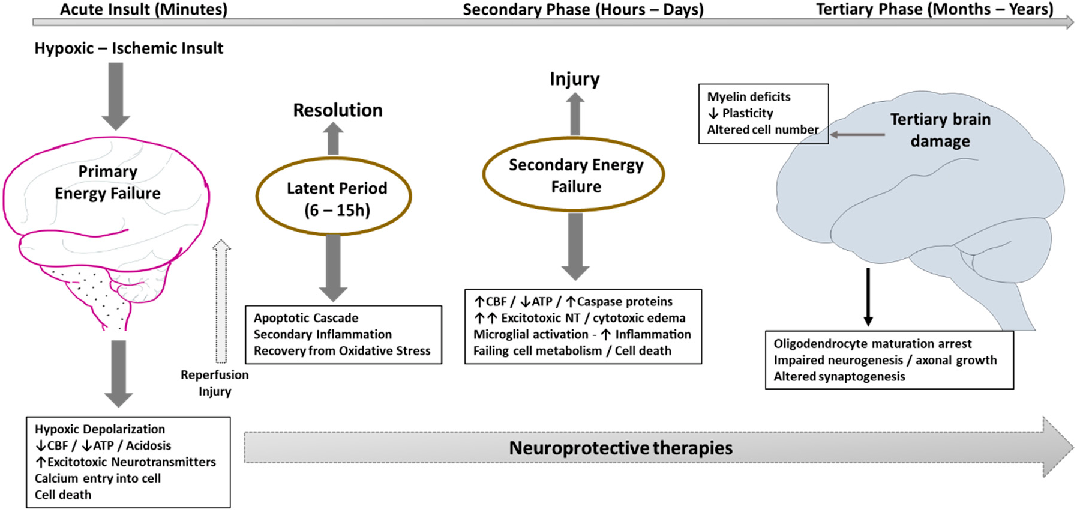
Causes of perinatal death by a child in developing countries are: 22.5% each - asphyxia and birth trauma, 12.7% - congenital malformations, 1.4% - infections. Developed countries have a higher proportion of congenital anomalies and a lower proportion of intrapartum causes and infections.
The neonatal period is the period of a child's life from the moment of birth to the age of 28 days. Within the framework of the neonatal period, two are distinguished: early (1st week of life) and late (2nd - 4th weeks), which correspond to the concepts and indicators of early and late neonatal mortality.
The main causes of neonatal mortality are: congenital malformations, birth trauma, neonatal pneumonia (excluding congenital). The ratio of these causes varies depending on the standard of living and the state of healthcare in terms of obstetric care. The fundamental feature of infant mortality in Russia, which qualitatively distinguishes it from the EU indicators, is a steady trend towards a decrease in the share of neonatal mortality in favor of an increase in postneonatal mortality.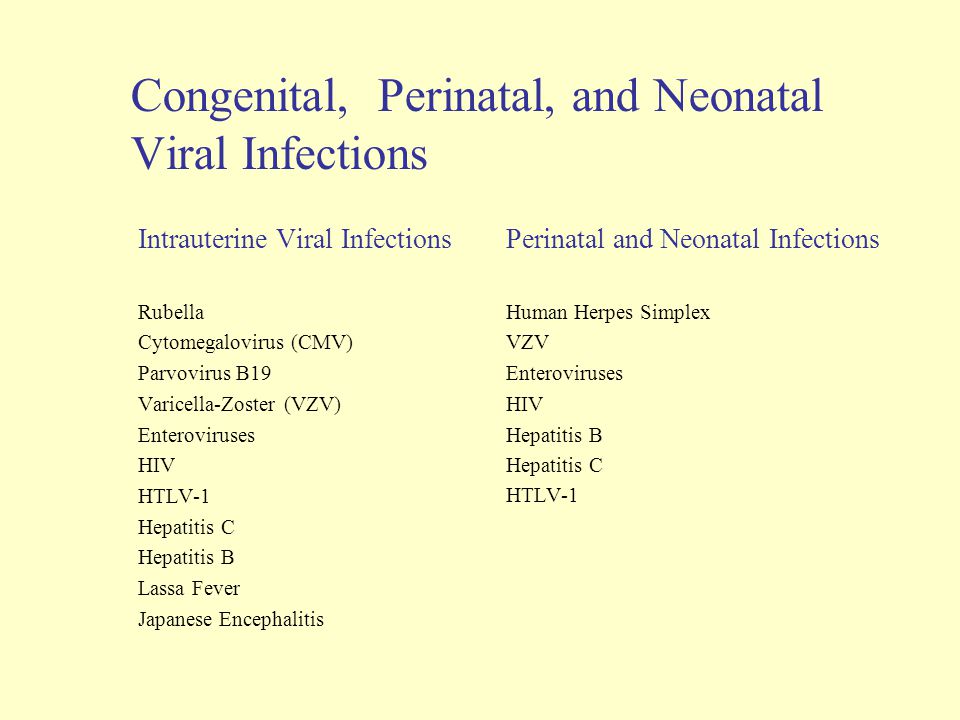 This feature of the dynamics of the indicator is due to the so-called. "underregistration" of dead newborns. The main ways to underestimate the infant mortality rate are the “transfer” of dead children to stillbirths that are not taken into account in state statistics, or the assignment of a deceased child to “fetuses” unregistered in the registry office (“miscarriages”, which in domestic medicine - up to 2011 inclusive - included termination of pregnancy up to 27 completed weeks). In practice, these two "mechanisms" are identified on the basis of obvious structural disproportions in the number of live and stillborns, as well as on the dissociation of the weight structure of the dead - the disappearance of children of borderline body weight (1000-1499d), "thrown" into unregistered "fruits".
This feature of the dynamics of the indicator is due to the so-called. "underregistration" of dead newborns. The main ways to underestimate the infant mortality rate are the “transfer” of dead children to stillbirths that are not taken into account in state statistics, or the assignment of a deceased child to “fetuses” unregistered in the registry office (“miscarriages”, which in domestic medicine - up to 2011 inclusive - included termination of pregnancy up to 27 completed weeks). In practice, these two "mechanisms" are identified on the basis of obvious structural disproportions in the number of live and stillborns, as well as on the dissociation of the weight structure of the dead - the disappearance of children of borderline body weight (1000-1499d), "thrown" into unregistered "fruits".
The third period, which is allocated within the framework of the first year of life, is postneonatal - starting from the 29th day of life and until reaching 1 year, for which the corresponding indicator of postneonatal mortality is calculated.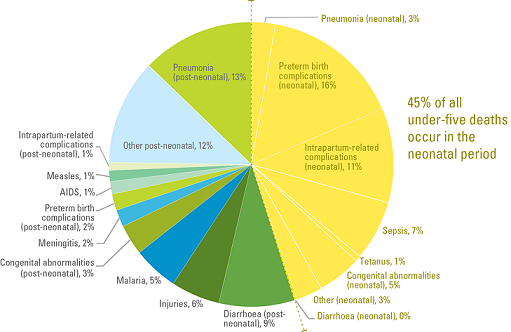 Among the main causes of postneonatal mortality are congenital anomalies, respiratory diseases, and external causes. The latter include the quality of care and nutrition, the timeliness of pediatric care, and injuries.
Among the main causes of postneonatal mortality are congenital anomalies, respiratory diseases, and external causes. The latter include the quality of care and nutrition, the timeliness of pediatric care, and injuries.
Dynamics - historical facts
The past century has been marked by a significant decline in infant mortality throughout the world. If at the beginning of the twentieth century in Norway, every twelfth-thirteenth newborn died before reaching the age of one, in France - every seventh, in Germany - every fifth, in Russia - every fourth, then in the period from the middle to the end of the twentieth century. the infant mortality rate has fallen unprecedentedly.
However, changes have taken place with varying degrees of success. At the beginning of the XX century. infant mortality rates in Russia were extremely high: at 19In 01, the proportion of deaths at this age was 40.5%, gradually decreasing to 38% in 1910. During this period, Russian indicators exceeded the corresponding data in developed countries by 1.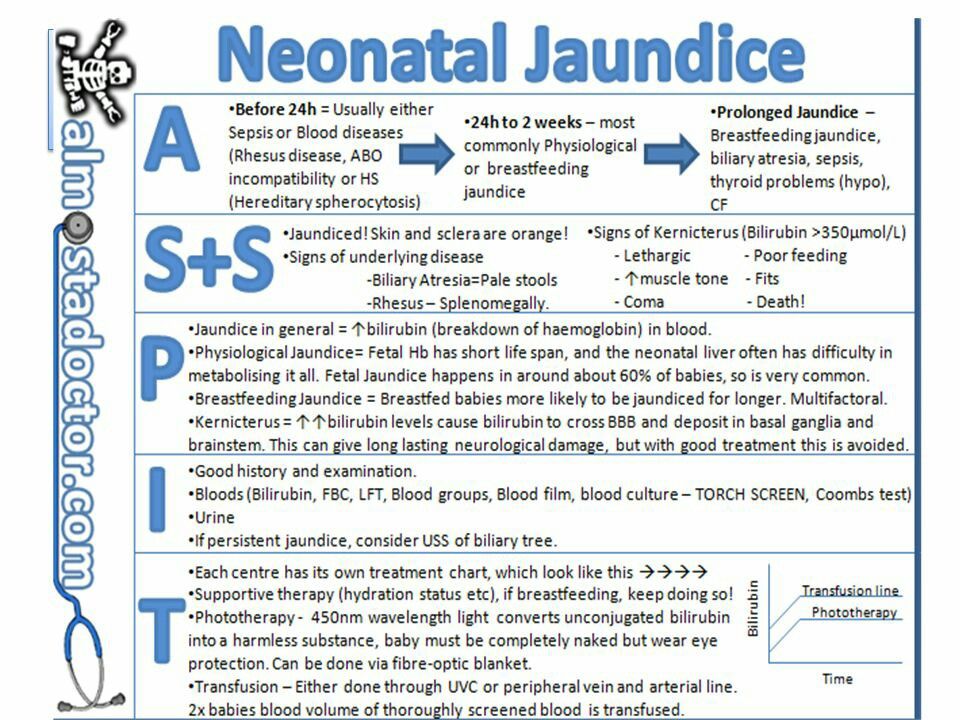 5-3 times. The main causes of infant mortality in the early XX century. were gastrointestinal and infectious diseases, respiratory diseases. In many ways, such a high level was associated with the peculiarities of feeding infants in Russian families, where it was traditionally accepted almost from the first days of life to give a child complementary foods or completely deprive him of breast milk, leave him without a mother in the care of adolescent children or the elderly. .
5-3 times. The main causes of infant mortality in the early XX century. were gastrointestinal and infectious diseases, respiratory diseases. In many ways, such a high level was associated with the peculiarities of feeding infants in Russian families, where it was traditionally accepted almost from the first days of life to give a child complementary foods or completely deprive him of breast milk, leave him without a mother in the care of adolescent children or the elderly. .
Also, the causes of high mortality were the underdevelopment of the system of medical care and obstetrics, the difficult sanitary conditions of work, life and living conditions, lack of knowledge of hygiene, low literacy of the population. In Russia, there was no legislation on the protection of motherhood and childhood, which has existed in many European countries for a long time. In the 1920s as a result of health care reforms on the adoption and implementation of legislative acts and decrees on the protection of motherhood and childhood, on the development of the system of obstetrics and medical care for mother and child, on the creation of infrastructure for caring for children (dairy kitchens, nurseries, patronage system, shelters for infants) , to carry out health education as an integral part of the cultural revolution, a reduction in infant and maternal mortality was achieved. At 1926, the Russian mortality rate for children under 1 year old was 188 per 1,000 births, i.e., for the first quarter of the 20th century, having decreased by almost a third.
At 1926, the Russian mortality rate for children under 1 year old was 188 per 1,000 births, i.e., for the first quarter of the 20th century, having decreased by almost a third.
1930s characterized again by fluctuations in the level of infant mortality due to influencing economic and social causes. There was a curtailment of the NEP, the process of industrialization and collectivization of agriculture began, which contributed to the growth of indicators to the level of the first decade of the 20th century. In 1933, the highest level of infant mortality was reached - 295.1‰ - largely due to the mass starvation of the population, and only by the end of the 1930s. began to decline again. The main reason for this was the implementation of measures to protect motherhood and childhood, the growth of sanitary literacy of the population, and the improvement in the quality of medical care.
After the Great Patriotic War, there were again improvements in performance. First of all, this is due to the appearance and use of antibiotics and sulfanilamide drugs in the treatment of gastrointestinal infections and pneumonia, which led to a significant reduction in the mortality of children under 1 year of age from respiratory diseases and infectious diseases. As a result, at 1946, the infant mortality rate in Russia was 124.0‰ compared to 205.2‰ in 1940. And by the mid-1960s. mortality in the first year of life decreased in the country by another 5 times: to 26.6‰ in 1965
As a result, at 1946, the infant mortality rate in Russia was 124.0‰ compared to 205.2‰ in 1940. And by the mid-1960s. mortality in the first year of life decreased in the country by another 5 times: to 26.6‰ in 1965
The reduction in infant mortality continued in the future. From the 1960s to the end of the twentieth century. its level decreased by 2.5 times. However, this decline was repeatedly interrupted by periods of increase: in 1971-1976, 1984, 1987, 1990-1993 and 1999. Significant was the growth of the indicator in 1990−1993 from 17.4 to 19.9‰, which is associated with the transition from January 1, 1993 to the definitions of live birth recommended by WHO.
At the World Summit for Children, held in 1990, the first agreed goal was to substantially reduce infant and under-5 mortality. Subsequently, significant emphasis was placed on this in the commitments made in the outcome document "A world fit for children" during the special session of the UN General Assembly on children in 2002. In addition, since 2000, reducing child mortality by 2/3 by 2015 was included in the list of the UN Millennium Development Goals. And, according to the 2015 MDG report, the under-five mortality rate worldwide has more than halved, falling from 90 to 43 deaths per 1,000 live births over the period 1990–2015
In addition, since 2000, reducing child mortality by 2/3 by 2015 was included in the list of the UN Millennium Development Goals. And, according to the 2015 MDG report, the under-five mortality rate worldwide has more than halved, falling from 90 to 43 deaths per 1,000 live births over the period 1990–2015
Currently, as mentioned at the beginning of this work, infant mortality rates are not stable, but compared to the 20th century. the dynamics are definitely positive. According to the Federal State Statistics Service of the Russian Federation in 2014, the infant mortality rate will be 7.4, although the figures for 2015, judging by the data for the first half of the year, are likely to be higher. In accordance with the analysis of existing problems to reduce infant mortality, which is one of the goals of the "Strategy for the development of healthcare in the Russian Federation until 2020", the following provisions can be put forward:
- ensuring equal access to highly qualified specialized care regardless of residence in urban or rural areas through the regionalization of care;
- tiered perinatal care system
- expanding the network of perinatal centers with the ability to provide optimal care for seriously ill and extremely immature premature babies
- providing equitable high-tech care for pregnant women and high-risk women in childbirth;
- ensuring a full examination of potential parents for congenital diseases and possible pathologies of the unborn fetus;
- improving the quality and regularity of observation of pregnant women for timely referral to institutions of the required functional level, corresponding to the state of health of the woman, the condition of the fetus, the nature of the course of pregnancy and the expected timing of delivery;
- monitoring the effectiveness and timeliness of hospitalization in compliance with the principles of regionalization; development of an emergency transport service for pregnant women, women in labor and newborns;
- providing conditions for continuous medical education and advanced training of personnel;
- a comprehensive analysis of the causes of perinatal mortality (including stillbirths) separately for full-term and preterm infants in order to identify existing reserves to reduce perinatal losses;
- improving the reproductive education of Russian youth and the development of the appropriate mentality of future parents, based on a responsible attitude to their own health.