Discoloration during pregnancy
Changes to your skin during pregnancy
beginning of content3-minute read
Listen
As your pregnancy develops, you may find that you experience changes to your skin and hair. Some women can develop dark patches on their face and hormonal changes can make your skin a little darker.
You may also develop stretch marks on your body, particularly around your stomach where your skin is stretching to accommodate your growing baby.
Chloasma - dark patches on the face
Some pregnant women develop dark irregular patches on their face most commonly on the upper cheek, nose, lips, and forehead. This is called 'chloasma'. It is also sometimes known as 'melasma' or the 'mask of pregnancy'.
Chloasma is thought to be due to stimulation of pigment-producing cells by female sex hormones so that they produce more melanin pigments (dark coloured pigments) when the skin is exposed to sun. Some women develop these patches when they take oral contraceptives (the pill).
Women with a light brown skin type who are living in regions with intense sun exposure are more likely to develop these patches. The patches usually fade over a period of several months after giving birth, though they may last for several years for some women.
Careful protection of the skin using broad spectrum sunscreens every day during pregnancy and while taking the pill may make it less likely that chloasma will develop. It is necessary to continue to use sunscreen after pregnancy as sun exposure may cause the patches to reappear. Some creams that need to be prescribed by doctors may help to fade the patches.
Skin and hair changes
Hormonal changes taking place in pregnancy will make your nipples and the area around them go darker. Your skin colour may also darken a little, either in patches or all over. Birthmarks, moles and freckles may also darken. Some women develop a dark line down the middle of their stomach, called 'linea nigra'. These changes will gradually fade after the baby is born, although your nipples may remain a little darker.
These changes will gradually fade after the baby is born, although your nipples may remain a little darker.
If you sunbathe while you are pregnant, you may burn more easily. Protect your skin with a good high-factor sunscreen and don't stay in the sun for a long time.
Hair growth can also increase in pregnancy, and your hair may be greasier. After the baby is born, it may seem as if you are losing a lot of hair but you are simply losing the extra hair.
Stretch marks
Many women develop stretch marks during their pregnancy, usually in the last 3 months.
They usually appear on your stomach or sometimes on your upper thighs or breasts. Stretch marks are not harmful and over time, your skin will shrink and the stretch marks will fade into white-coloured scars.
Find out more on stretch marks.
Sources:
Royal Women's Hospital Victoria (Common concerns in early pregnancy - itching and skin), The Australasian College of Dermatologists (Striae), The Australasian College of Dermatologists (Melasma)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2020
Back To Top
Related pages
- Common discomforts during pregnancy
- Stretch marks
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Skin darkening during pregnancy (melasma or chloasma)
It's common to develop blotchy spots of darker skin when you're pregnant, a condition called melasma or chloasma. Women with darker complexions are more likely to have melasma than women with lighter skin. Changes in skin pigmentation due to melasma usually disappear on their own after delivery.
Women with darker complexions are more likely to have melasma than women with lighter skin. Changes in skin pigmentation due to melasma usually disappear on their own after delivery.
Is it normal to have melasma during pregnancy?
Yes, it's common to develop blotchy spots of darker skin when you're pregnant, a condition called melasma or chloasma. Melasma is also sometimes referred to as the mask of pregnancy because the splotches typically show up around your upper lip, nose, cheekbones, and forehead in the shape of a mask.
You may also develop dark patches on your cheeks, along your jawline, or on your forearms and other parts of your body that are exposed to the sun. What's more, skin that's already more pigmented – such as your nipples, freckles, scars, and the skin of your genitals – may become even darker during pregnancy. This also tends to happen in areas where friction is common, such as your underarms and inner thighs.
What causes melasma?
Melasma may be triggered by hormonal changes during pregnancy, which stimulate a temporary increase in the amount of melanin your body produces.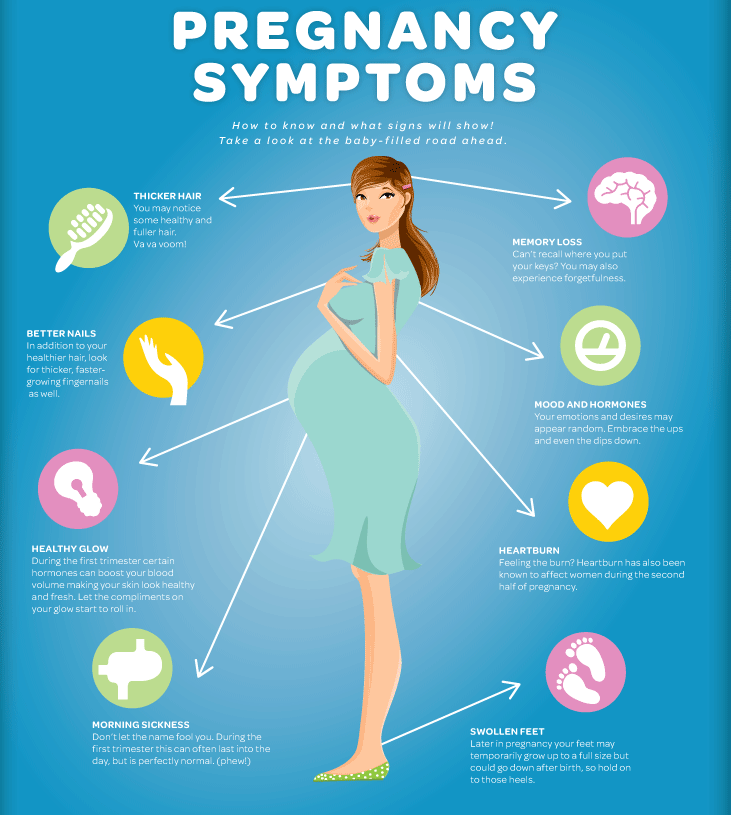 Melanin is the natural substance that gives color to hair, skin, and eyes.
Melanin is the natural substance that gives color to hair, skin, and eyes.
Sun exposure plays a role too. Women with darker complexions are more likely to have melasma than women with lighter skin.
You're also more likely to develop melasma if it runs in your family.
The same increased production of melanin that causes the facial splotches of melasma also causes the linea nigra, or dark line that you may notice running down your belly.
The linea nigra will probably fade back to its pre-pregnancy color several months after you deliver your baby, but may not completely disappear.
How can I prevent melasma from getting worse during pregnancy?
All changes in skin pigmentation due to melasma usually disappear on their own after delivery, but you can do a few things to safely minimize darkened spots on your skin during pregnancy:
- Use sun protection. This is crucial because exposure to the sun's ultraviolet (UV) rays triggers melasma and intensifies pigment changes.
 Use a broad-spectrum sunblock (a formula that protects against both UVA and UVB rays) with SPF 30 or higher every day, even when it's not sunny, and reapply often during the day if you're outside. This is true even if you have dark skin. Although dark skin has more melanin (pigment) than lighter skin and doesn't sunburn as quickly, it's not enough to protect you from harmful UV radiation.
Use a broad-spectrum sunblock (a formula that protects against both UVA and UVB rays) with SPF 30 or higher every day, even when it's not sunny, and reapply often during the day if you're outside. This is true even if you have dark skin. Although dark skin has more melanin (pigment) than lighter skin and doesn't sunburn as quickly, it's not enough to protect you from harmful UV radiation.Even if you don't plan to leave the house or spend much time outside, it's a good idea to apply sun protection as part of your morning routine. The American Academy of Dermatology cautions that your skin is exposed to a significant amount of UV light whenever you walk down the street, ride in a car, or even sit inside near a window.
When you're outside, wear a wide-brimmed hat as well as a long-sleeved shirt if you have pigmentation changes on your arms. Limit the time you spend in the sun, especially between 10 a.m. and 2 p.m. And definitely avoid tanning salons.
- Don't wax.
 Using wax to remove hair can cause skin inflammation that worsens melasma, especially in areas of your body that are affected by pigmentation changes.
Using wax to remove hair can cause skin inflammation that worsens melasma, especially in areas of your body that are affected by pigmentation changes. - Use hypoallergenic skin care products. Cleansers and face creams that irritate your skin may make melasma worse.
- Apply concealer. If the darkened spots bother you, cover them up by using makeup for now. Concealer with white and yellow undertones often helps, but consult the makeup salespeople at your local store to find the right product for your skin type. You can also seek the advice of a board-certified dermatologist. Don't use skin-bleaching products while you're pregnant, and talk to your doctor before starting them if you are breastfeeding.
Advertisement | page continues below
Will I still have melasma after my pregnancy?
Melasma usually fades without treatment after you have your baby. The darkened spots probably will fade within a year after delivery, and your skin should return to its normal shade, although sometimes the changes never completely disappear.
For some women, contraceptives containing estrogen (such as the Pill, the patch, and the vaginal ring) can also contribute to melasma. If the skin changes are bothersome, consider another birth control option.
If your skin is still blotchy a few months after giving birth and it's bothering you, talk to your healthcare provider or a dermatologist about treatment options for melasma. She may suggest using a bleaching cream that contains hydroquinone (and possibly sunscreen), a topical medication that contains tretinoin (Retin-A), or a chemical peel such as azelaic acid.
If you're breastfeeding or plan to get pregnant again soon, let your provider know and check with her before using any over-the-counter treatments.
Don't expect instant results – it may take many months to see improvement. If other treatments haven't helped, a dermatologist can lighten dark spots with laser treatments, but that's not the first option.
In any case, continue to protect your skin from the sun by using sunscreen every day, wearing protective clothing, and staying out of the sun during peak hours.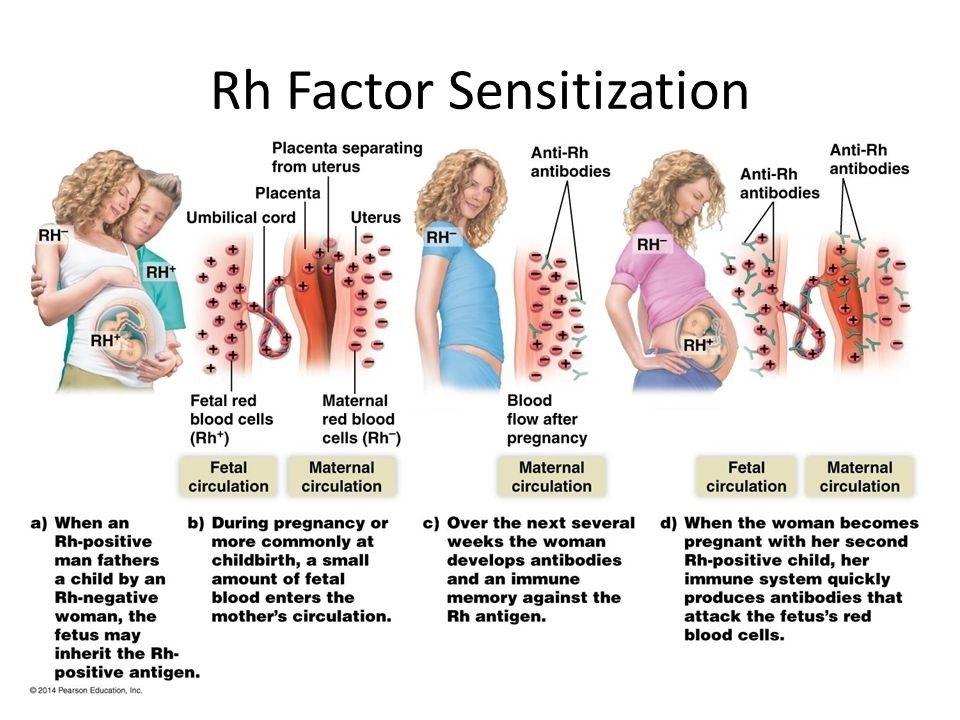
Certain types of skin discoloration can be a symptom of skin cancer or other medical problems.
Call your provider if you have changes in skin pigmentation as well as pain, tenderness, redness, or bleeding, or if you notice any changes in the color, shape, or size of a mole.
You may be referred to a dermatologist for a diagnosis and appropriate treatment.
Wondering what skin care products are safe and which to avoid while pregnant? Check out our article on safe skin care during pregnancy.
Learn more:
- Acne during pregnancy
- Hair and nail changes during pregnancy
- Varicose veins during pregnancy
Was this article helpful?
Yes
No
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.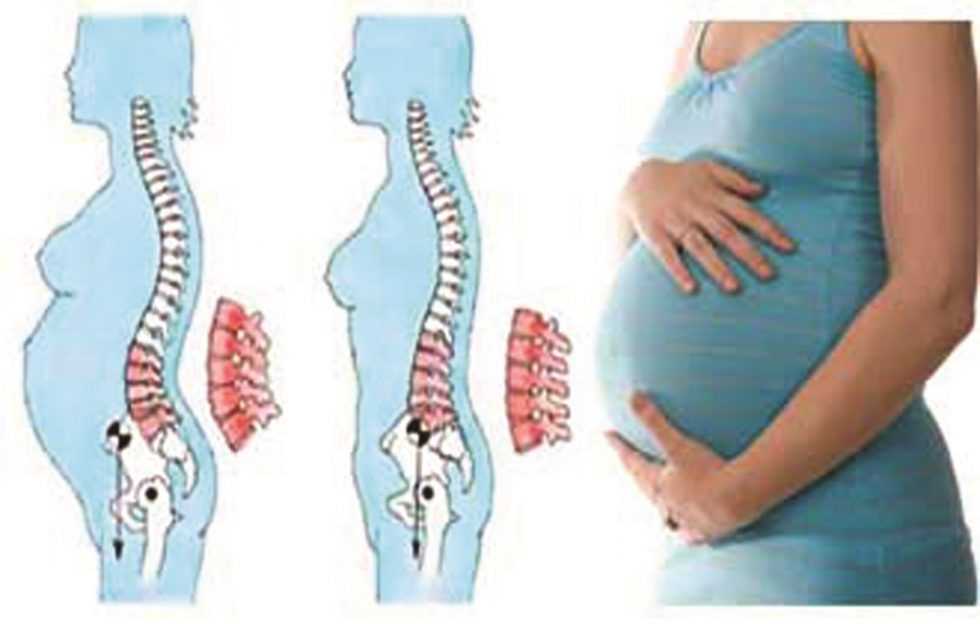
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows.
The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners.
 The mucous membrane of the female genital organs finally matures by the age of 20–23. If an infection interferes with this delicate process, erosion is practically unavoidable;
The mucous membrane of the female genital organs finally matures by the age of 20–23. If an infection interferes with this delicate process, erosion is practically unavoidable; - is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital IDKMother and Child Clinic Enthusiastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children)Molecular genetics laboratoryGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsAdult ultrasound examinations
01.
Specialist consultations (adults)
02.
Consultations of specialists (children's)
03.
Laboratory of molecular genetics
04.
Adult Telemedicine
08.
Therapeutic Research
09.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to update the price list posted on the website in a timely manner, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of tests by calling
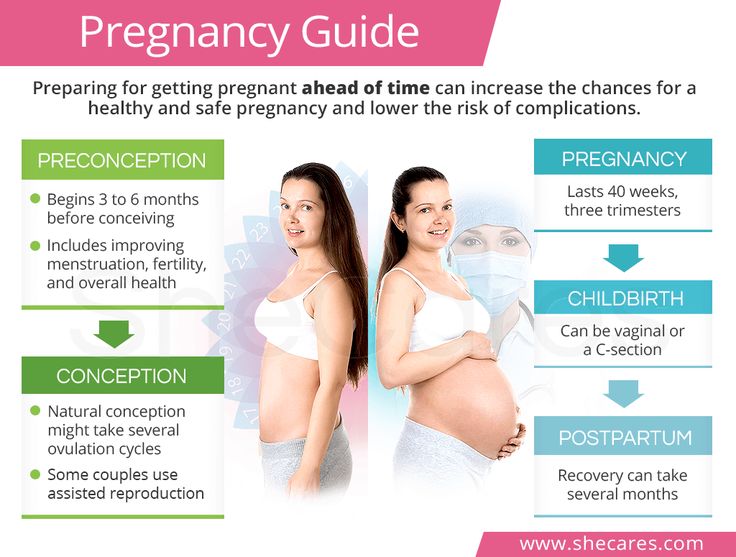
Physiological changes in the body during pregnancy
transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body. During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth. Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
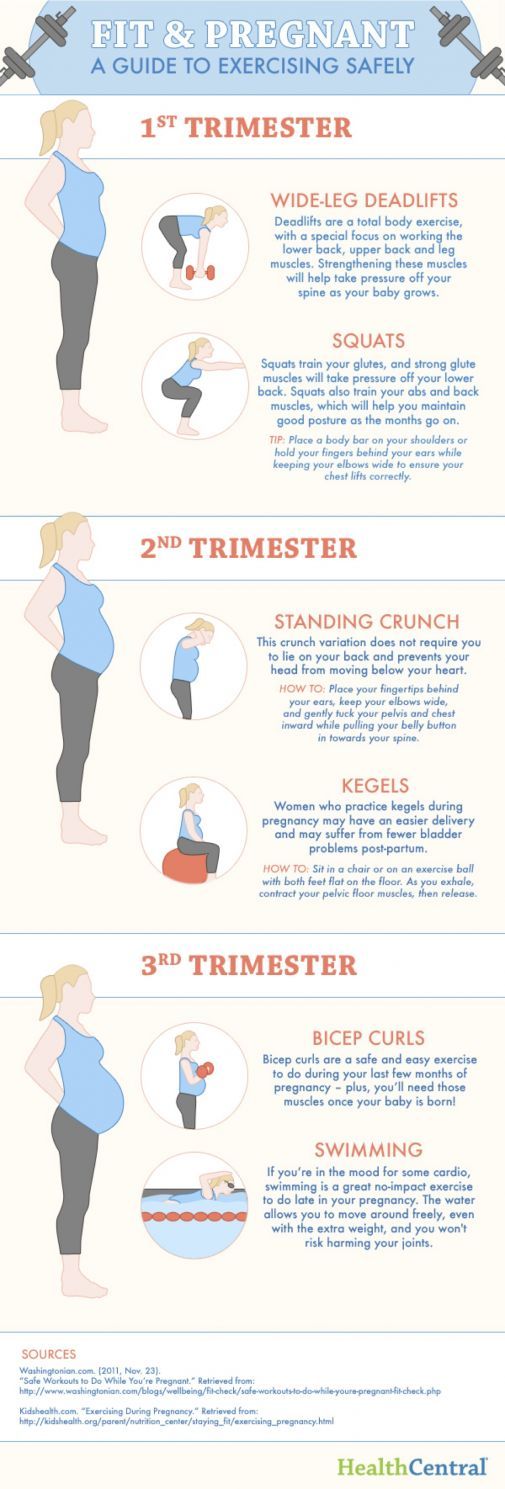
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
The mother's circulatory system during pregnancy is forced to pump more blood to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of blood vessels during pregnancy decreases, which creates favorable conditions for increased supply of tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure.
And changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), cravings for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
The most significant changes, however, occur in genitals of pregnant women. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
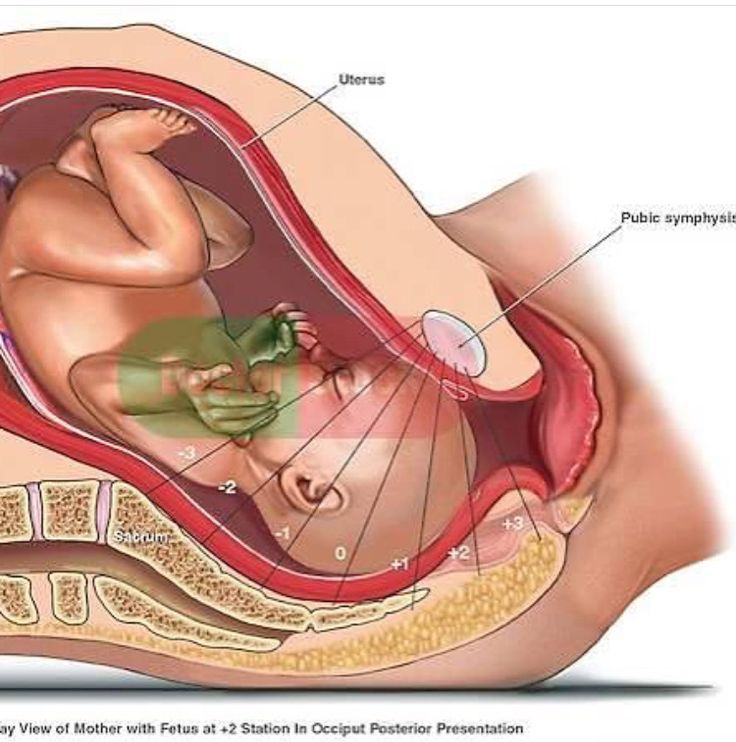
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy. Walls vaginas will loosen and become more elastic. External genitalia (labia minor and major), also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
Skin in the genital area and in the midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released.
Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This helps to reduce the rigidity of the joints between the bones of the pelvis and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Also, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
Changes in the nervous system .