How much bleeding is ok in early pregnancy
How Much Bleeding Is Normal In Early Pregnancy?
Light amounts of vaginal bleeding early in your pregnancy can occur. In most cases, it’s not serious. It can happen in the first 20 weeks for different reasons. It can be the result of something serious or non-serious. Continued bleeding throughout the pregnancy is not common. Call your doctor immediately if you are bleeding heavily. Go to the emergency room if you have severe pain.
Path to improved health
Vaginal bleeding can happen from conception to delivery. Spotting is a type of light bleeding. You may see just a few drops of blood in your underwear. Heavy bleeding is more noticeable. It will require a sanitary pad to protect your clothing.
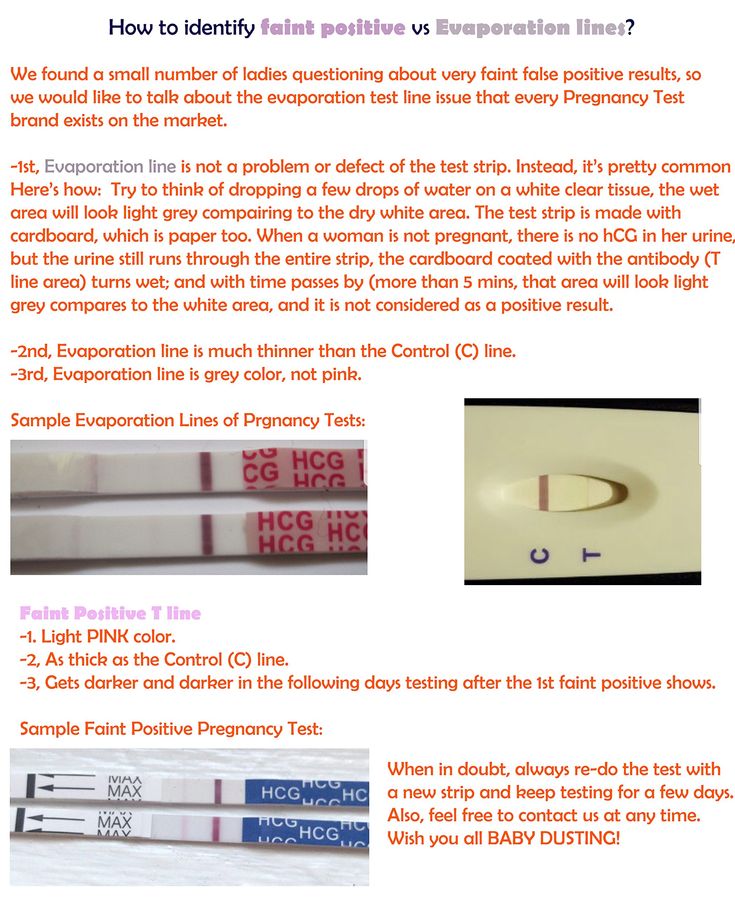
Call your doctor whenever you experience bleeding of any kind. Call your doctor if you have vaginal bleeding or spotting. This is important even if an ultrasound test confirms your pregnancy is normal. An ultrasound is where a technician moves a wand around your stomach to see an image of the baby.
Non-serious reasons for bleeding early in your pregnancy can include:
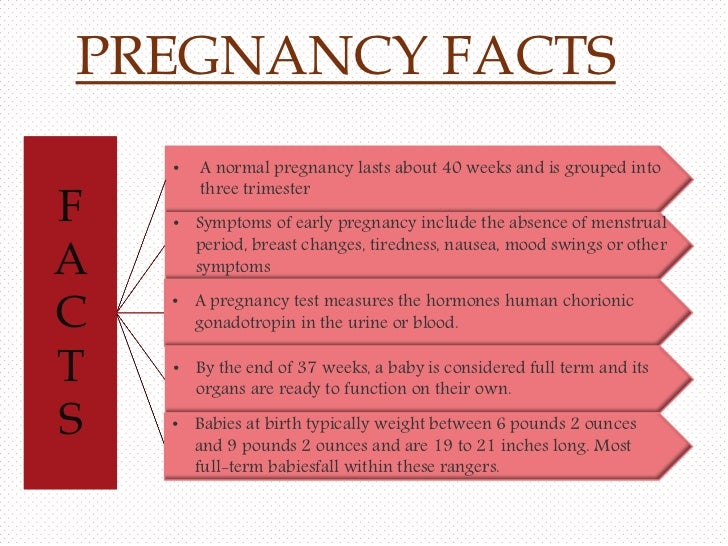
- Implantation (as the egg settles into your uterus the first 6-12 days)
- Sex
- Infection
- Hormones.
More serious causes of vaginal bleeding during the early part of pregnancy can include:
- An ectopic pregnancy (a pregnancy that starts outside the uterus and will not survive but can be life threatening).
- A miscarriage (losing the baby early in a pregnancy).
- A molar pregnancy (a fertilized egg that implants in the uterus that does not live).
In later pregnancy, the following serious medical conditions can cause vaginal bleeding:
- Placental abruption (the placenta detaches from the wall of the uterus before birth).
- Placenta previa (the placenta is lying too low in the uterus and nearly covers the cervix).
- Placenta accreta (when the placenta invades the uterus and doesn’t separate from the uterine wall).
- Preterm labor (labor that starts before completing 37 of 40 weeks of pregnancy).
Bleeding may be just one sign of preterm labor. Preterm labor also can include vaginal discharge, pressure in your pelvis or abdomen (lower stomach), a dull backache, cramps, contractions, and your water breaking.
If you are bleeding early in your pregnancy, your doctor will want to know how long and how much. If you have cramps and pain early in the pregnancy, he or she will order tests. This may include an ultrasound, blood, and urine tests.
If continued bleeding is not serious, your doctor may treat it by recommending that you rest, relax, stay off your feet, and not have sex. Keep your body healthy. Take a prenatal vitamin with folic acid daily while pregnant. Take it earlier if you plan to get pregnant. Avoid smoking, drinking alcohol, and taking illegal drugs. Talk to your doctor before taking prescription medicine. When you are pregnant, you should never douche (use vaginal cleansing products) or use tampons.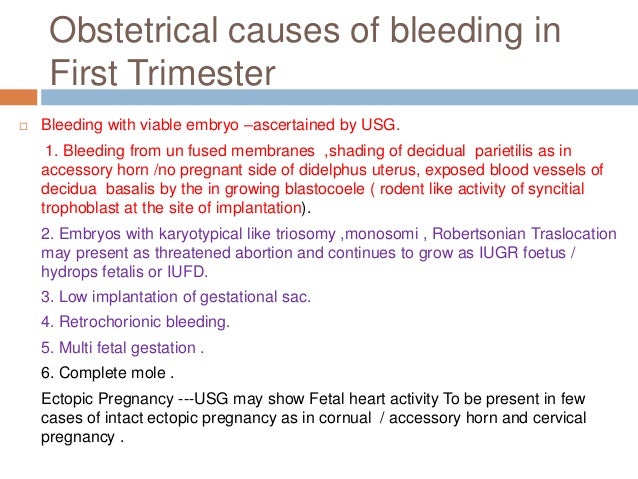 Serious bleeding may need to be treated with a long-term bed rest, hospitalization, or surgery.
Serious bleeding may need to be treated with a long-term bed rest, hospitalization, or surgery.
You cannot prevent a miscarriage after it has started. The exact cause is usually unknown. It’s rarely something the mother did wrong. Most women can have healthy pregnancies in the future. If you have lost more than 3 pregnancies, talk to your doctor.
Things to consider
If you experience bleeding or spotting at any time during your pregnancy, your doctor will want to collect as much information as possible. That will include:
- How far along is your pregnancy?
- Have you had bleeding at any other time during your pregnancy?
- When did the bleeding start?
- Is the bleeding heavy or spotting?
- Does it start and stop?
- How much blood is there?
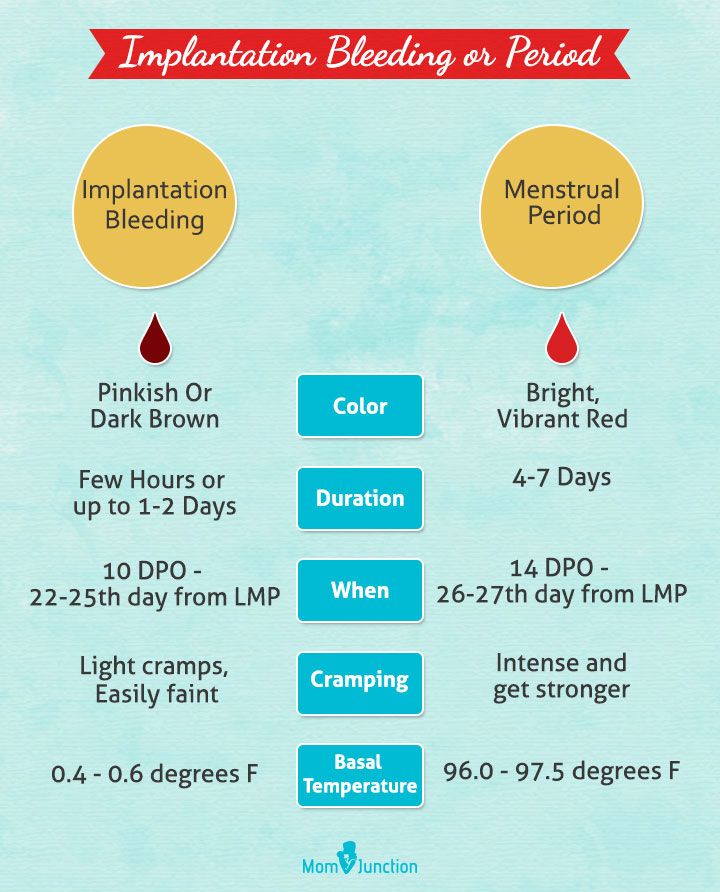
- What color is the blood (bright red or dark brown)?
- Does the blood have an odor?
- Do you have cramps or pain?
- Do you feel weak, tired, faint, or dizzy?
- Have you experienced vomiting, nausea, or diarrhea?
- Do you have a fever?
- Were you recently injured (such as a fall or car accident)?
- Have you engaged in any physical activity?
- Are you under extra stress?
- When did you last have sex? Did you bleed afterward?
- Do you have a bleeding disorder? Women with bleeding disorders are at risk of complications during and after pregnancy.
 This includes iron-deficiency anemia, bleeding during pregnancy, and serious bleeding after delivery (postpartum hemorrhage). Talk to your doctor before getting pregnant if you have a bleeding disorder. Also, bleeding disorders are genetic.
This includes iron-deficiency anemia, bleeding during pregnancy, and serious bleeding after delivery (postpartum hemorrhage). Talk to your doctor before getting pregnant if you have a bleeding disorder. Also, bleeding disorders are genetic. - What is your blood type? If your blood type is Rh negative, you will need treatment with a medicine called Rho(D) immune globulin. This prevents complications with future pregnancies.
Vaginal bleeding is usually blood without clots or tissue. If you see something other than blood, call your doctor immediately. Try to collect the discharge in a container and bring it with you when you see your doctor. It may mean you have miscarried. If that is the case, your doctor will provide additional care. If not all the tissue from the miscarriage has passed, your doctor may need to perform a procedure. This procedure is called a dilation and curettage (D and C). It involves opening (dilating) the cervix. Your doctor will gently suction out the remaining tissue from the miscarriage.
Questions to ask your doctor
- Can certain foods (such as spicy foods) cause bleeding?
- Is it best to avoid having sex throughout your entire pregnancy?
- Is spotting during later pregnancy normal?
- Is my life at risk?
- I feel sad. Is there someone I could talk to about my feelings? Is there a support group?
Resources
U.S. National Library of Medicine, Vaginal bleeding in early pregnancy
March of Dimes, Bleeding and Spotting From the Vagina During Pregnancy
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Bleeding and spotting from the vagina during pregnancy
Bleeding and spotting from the vagina during pregnancy are common
If you bleed or spot during pregnancy, it doesn’t always mean there’s a problem but in some cases they may be signs of a problem for you or your baby’s health
If you have heavy bleeding, call your health care provider right away
Tell your provider about any bleeding or spotting you have during pregnancy
Bleeding and spotting from the vagina during pregnancy are common. Up to 1 out of 4 (up to 25%) of all pregnant women have some bleeding or spotting during their pregnancy.
Up to 1 out of 4 (up to 25%) of all pregnant women have some bleeding or spotting during their pregnancy.
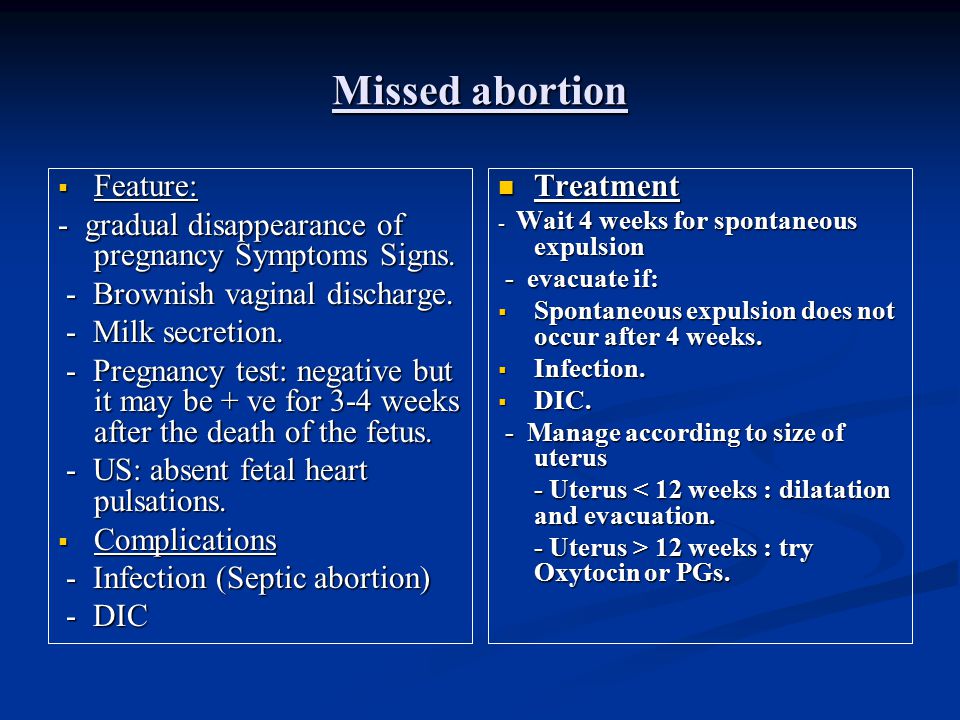
Bleeding and spotting in pregnancy don’t always mean there’s a problem, but they can be a sign of miscarriage or other serious complications. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Call your health care provider if you have any bleeding or spotting, even if it stops. It may not be caused by anything serious, but your provider needs to find out what’s causing it.
What’s the difference between bleeding and spotting?
Bleeding or spotting can happen anytime, from the time you get pregnant to right before you give birth. Spotting is light bleeding. It happens when you have a few drops of blood on your underwear. Spotting is so light that the blood wouldn’t cover a panty liner. Bleeding is when the blood flow is heavier, enough that you need a panty liner or pad to keep the blood from soaking your underwear and clothes.
What should you do if you have bleeding or spotting during pregnancy?
Call your health care provider if you have any kind of bleeding during pregnancy and do these things:
- Keep track of how heavy your bleeding is, if it gets heavier or lighter, and how many pads you are using.
- Check the color of the blood. Your provider may want to know. It can be different colors, like brown, dark or bright red.
- Don’t use a tampon, douche or have sex when you’re bleeding.
Call your health care provider right away at any time during pregnancy or go to the emergency room if you have:
- Heavy bleeding
- Bleeding with pain or cramping
- Dizziness and bleeding
- Pain in your belly or pelvis
What causes bleeding or spotting early in pregnancy?
It’s normal to have some spotting or bleeding early in pregnancy. Bleeding or spotting in the first trimester may not be a problem..jpg) It can be caused by:
It can be caused by:
- Having sex
- An infection
- Implantation. When a fertilized egg (embryo) attaches to the lining of the uterus (womb) and begins to grow.
- Hormone changes. Hormones are chemicals made by the body.
- Changes in your cervix. The cervix is opening to the uterus that sits at the top of the vagina.
- Certain types of testing during pregnancy like an amniocentesis or Chorionic villus sampling (CVS). These are tests that are done to check for genetic abnormalities in your baby. Genetic abnormalities are changes in the genes that are passed down to a baby from mom or dad. These genetic changes can cause health problems for a baby.
- Problems related to smoking. If you smoke, it’s best to stop before pregnancy or as soon as you know you’re pregnant.
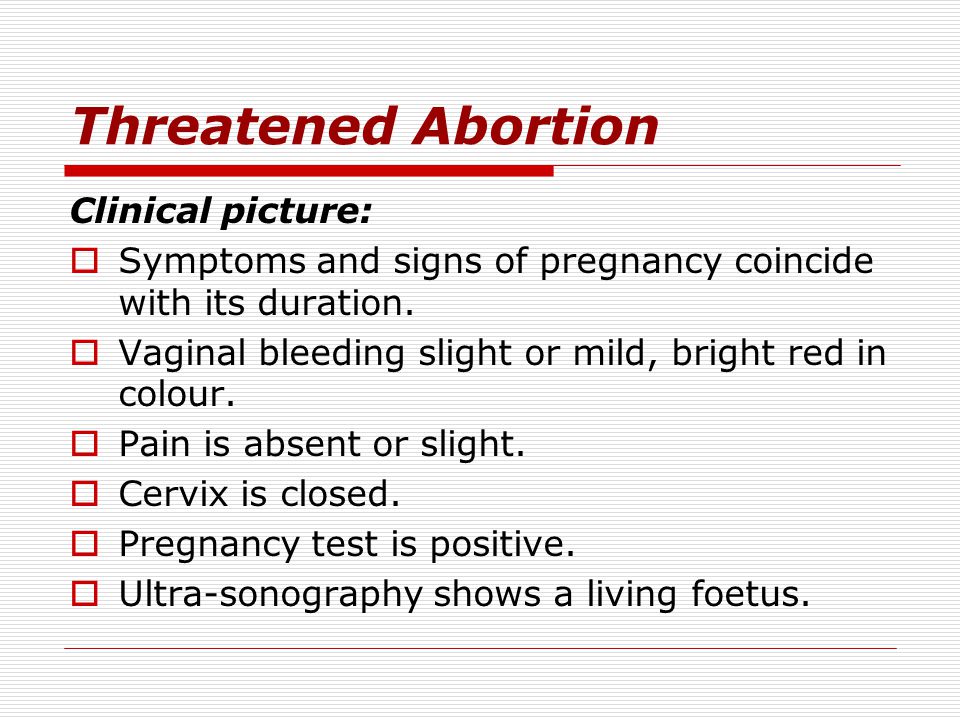
Sometimes bleeding or spotting in the first trimester is a sign of a serious problem, like:
- Miscarriage. Almost all women who miscarry have bleeding or spotting before the miscarriage.
- Ectopic pregnancy. This is when a fertilized egg implants itself outside of the uterus and begins to grow. An ectopic pregnancy cannot result in the birth of a baby. It can cause serious, dangerous problems for the pregnant woman.
- Molar pregnancy. This is when a mass of tissue forms inside the womb, instead of a baby. Molar pregnancy is rare.
What causes bleeding or spotting later in pregnancy?
Bleeding or spotting later in pregnancy may be caused by:
- Labor
- Having sex
- An internal exam by your health care provider
- Problems with the cervix, like an infection, growths, inflammation or cervical insufficiency. This is when a woman’s cervix opens too early. Inflammation of the cervix is when it may be painful, swollen, red or irritated.
Bleeding or spotting later in pregnancy may be a sign of a serious problem, like:
- Preterm labor.
 This is labor that happens too early, before 37 weeks of pregnancy.
This is labor that happens too early, before 37 weeks of pregnancy. - Placenta previa. This is when the placenta lies very low in the uterus and covers all or part of the cervix.
- Placenta accreta. This is when the placenta grows into the wall of the uterus too deeply.
- Placental abruption. This is when the placenta separates from the wall of the uterus before birth.
- Uterine rupture. This is when the uterus tears during labor. This happens very rarely. It can happen if you have a scar in the uterus from a prior cesarean birth (also called c-section) or another kind of surgery on the uterus. A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
How are bleeding and spotting treated?
Your treatment depends on what caused your bleeding. You may need a medical exam and tests.
You may need a medical exam and tests.
Most of the time, treatment for bleeding or spotting is rest. Your provider may also suggest treatments like:
- Take time off from work and stay off your feet for a little while
- You may need medicine to help protect your baby from Rh disease. Rh disease is when your blood and baby’s blood are incompatible (can’t be together). This disease can cause serious problems — even death — for your baby.
- Don’t have sex, douche or use tampons
- If you have heavy bleeding, you may need a hospital stay or surgery
Last reviewed April 2020
Bleeding during pregnancy. What is Bleeding During Pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.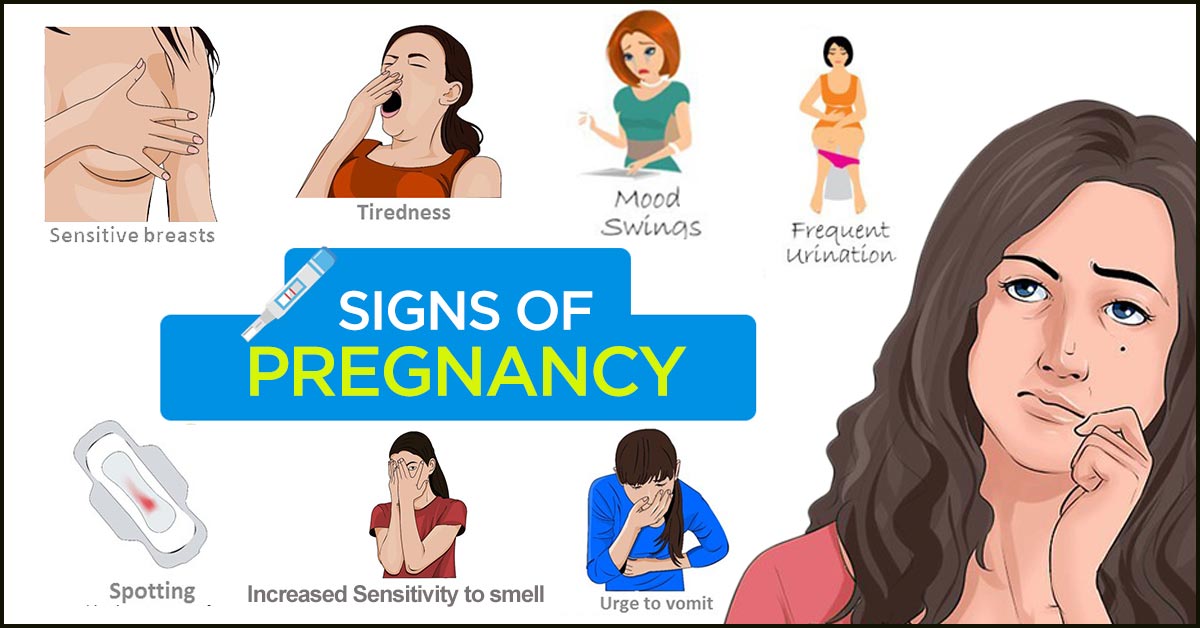
Bleeding during pregnancy is a sign that can occur regardless of the period of embryogenesis and indicates ongoing changes in the woman's body. It can be observed with spontaneous miscarriage, ectopic pregnancy, Rh conflict, placenta previa and other conditions. This manifestation can develop against the background of general well-being or be accompanied by painful sensations in the lower abdomen, lower back, and sacrum. Diagnosis of bleeding during pregnancy is carried out on the basis of data from a gynecological examination, an ultrasound assessment of the condition of the patient and the fetus. The treatment of this pathological symptom is determined by its cause and is prescribed exclusively by a specialist.
- Causes of bleeding during pregnancy
- Classification and symptoms of bleeding during pregnancy
- Diagnosis and treatment of bleeding during pregnancy
- Prognosis and prevention of bleeding during pregnancy
- Prices for treatment
General
Bleeding during pregnancy is an obstetric symptom, indicating the possible development of a number of disorders, the cause of which can be both physiological changes in the body of a woman after conception, and pathological conditions. Only an obstetrician-gynecologist can finally find out the etiology of such a manifestation after a complete examination. Bleeding during pregnancy occurs in about one in five patients. In 50%, they indicate pathological changes and end in spontaneous miscarriage. In half of the patients, the symptom is physiological in nature. Bleeding occurs more often in the first and third trimester of embryogenesis.
Only an obstetrician-gynecologist can finally find out the etiology of such a manifestation after a complete examination. Bleeding during pregnancy occurs in about one in five patients. In 50%, they indicate pathological changes and end in spontaneous miscarriage. In half of the patients, the symptom is physiological in nature. Bleeding occurs more often in the first and third trimester of embryogenesis.
The danger of bleeding during pregnancy lies in the fact that a variety of factors can provoke them, including those that pose a threat to the mother and fetus. In some situations, there are no other pathological signs. Any bleeding during pregnancy should be a reason for immediate medical attention. Only a specialist is able to assess the danger to the health of a woman and the fetus, as well as decide on further tactics. Timely assistance provided even with an abnormal course of pregnancy allows you to continue its management and save the life of the child.
Bleeding during pregnancy
Causes of bleeding during pregnancy
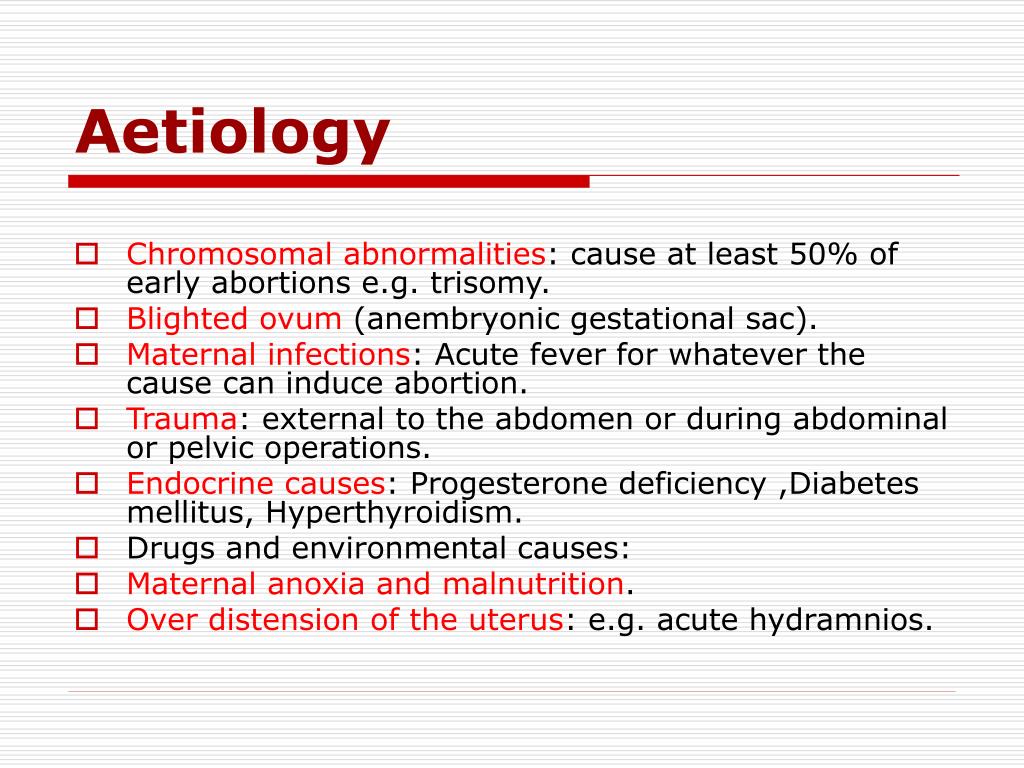
Bleeding during pregnancy can occur at any time of embryogenesis, develops both against the background of physiological changes in the woman's body, and as a result of the formation of a certain obstetric pathology. In the early stages, half of the women have a slight separation of blood due to the implantation of the fetal egg in the uterine cavity. Such bleeding during pregnancy is often regarded by the patient as menstrual, so she does not seek medical help, which in the future may make it difficult to determine the timing of embryogenesis. A similar symptom is possible with insufficient production of progesterone in the early stages of gestation.
In the early stages, half of the women have a slight separation of blood due to the implantation of the fetal egg in the uterine cavity. Such bleeding during pregnancy is often regarded by the patient as menstrual, so she does not seek medical help, which in the future may make it difficult to determine the timing of embryogenesis. A similar symptom is possible with insufficient production of progesterone in the early stages of gestation.
The most common cause of abnormal bleeding during pregnancy in the first trimester is spontaneous miscarriage. This symptom appears both with a just-started and with a complete abortion. Approximately 6 weeks after conception, the symptom occurs with an ectopic attachment of the fetal egg. Also, bleeding during pregnancy at this time may indicate an Rhesus conflict, fetal fading. Similar manifestations are characteristic of women suffering from varicose veins that feed the uterus. In this case, bleeding during pregnancy is due to increased blood supply to the tissues.
Bleeding during pregnancy in the second trimester is diagnosed much less frequently, in about 5-10% of all cases of gestation. As a rule, the symptom is caused by pathological changes and in most cases indicates spontaneous late abortion or isthmic-cervical insufficiency. Sometimes the separation of blood from the genital tract is observed during intrauterine death of the fetus. Bleeding during pregnancy in the third trimester also always speaks of the development of gestation pathology. The most common cause is placenta previa. In this case, the embryonic organ completely or partially covers the uterine os, while due to the high load on the lower segment, placental micro-ruptures occur, which causes a similar symptom.
Less commonly, bleeding during pregnancy in the third trimester is due to premature detachment of a normally located placenta. In this situation, there is a high threat to the life of the fetus. The danger also lies in the fact that initially internal bleeding develops during pregnancy or the formation of a hematoma, and only then the blood flows out. The rarest, but most dangerous for the life of the mother and child, the cause of the development of this symptom is uterine rupture. Such a complication is diagnosed in the presence of a scar on the myometrium and tissue overstretching, provoked by polyhydramnios, large fetuses or multiple pregnancies. It is extremely rare that bleeding during pregnancy occurs due to a violation of the integrity of the membranes or umbilical cord vessels.
The rarest, but most dangerous for the life of the mother and child, the cause of the development of this symptom is uterine rupture. Such a complication is diagnosed in the presence of a scar on the myometrium and tissue overstretching, provoked by polyhydramnios, large fetuses or multiple pregnancies. It is extremely rare that bleeding during pregnancy occurs due to a violation of the integrity of the membranes or umbilical cord vessels.
Also, bleeding during pregnancy can be triggered by causes that appear at any stage of embryogenesis. Such reasons include benign neoplasms - fibroids, polyposis growths in the cervical canal and uterine cavity. Often bleeding during pregnancy occurs in women with cervical erosion. Sometimes a sign occurs due to increased blood circulation in the pelvic organs. The risk of developing a symptom is also present with violent sexual intercourse, significant physical exertion, concomitant cardiovascular diseases associated with a weakening of the endothelium.
Classification and symptoms of bleeding during pregnancy
Depending on the origin of bleeding, two groups can be distinguished:
- Physiological bleeding during pregnancy - occurs due to the restructuring of the body, does not pose a threat to the health and life of the fetus or mother.
- Pathological bleeding during pregnancy - indicate its abnormal course, may be accompanied by a risk to the life and health of the woman and baby, require immediate medical attention.
The clinic of bleeding during pregnancy directly depends on the cause of this symptom. Isolation of blood from the genital tract in the early stages of embryogenesis, provoked by physiological changes, proceeds against the background of general well-being. Bleeding during pregnancy, which has developed due to the presence of polyps, erosion, fibroids in most cases also does not cause disturbances in well-being. In this case, there is a slight release of biological fluid - just a few drops, the symptom is of a short-term nature. More abundant, similar to menstrual, will be bleeding during pregnancy associated with a deficiency of progesterone.
More abundant, similar to menstrual, will be bleeding during pregnancy associated with a deficiency of progesterone.
In the case of bleeding during pregnancy associated with its spontaneous interruption, the patient is worried about constant or cramping pain in the lumbosacral region, abdomen. Additionally, nausea, dizziness, malaise, and a slight increase in body temperature may occur. Bleeding during pregnancy in this case can be of varying intensity, often in the discharge there are pieces of tissue. With an ectopic attachment of the fetal egg, as well as with a rupture of the uterus, a serious threat to the life of a woman arises. In such a situation, internal bleeding initially develops during pregnancy, and only then do pathological discharges from the external genital tract appear. There is acute pain in the abdomen with irradiation to the anal region, the lateral parts of the body. With significant blood loss, a state of shock occurs with a threat of death.
Bleeding during pregnancy in the later stages is also not always accompanied by a detailed clinical picture. In the case of placenta previa, this is the only symptom that should cause alertness in a woman and become a reason for contacting an obstetrician-gynecologist. As for the premature detachment of a correctly attached placenta, in this case, bleeding during pregnancy develops against the background of uterine hypertonicity, there is pain in the abdomen, deterioration in general well-being. During cardiac monitoring of the fetus, there is a violation of the heart rate, motor activity.
Diagnosis and treatment of bleeding during pregnancy
To identify the cause of bleeding during pregnancy, a gynecological examination of a woman is performed. With changes in physiological origin, no deviations from the norm can be detected. With pathological bleeding during pregnancy against the background of spontaneous abortion, an opening of the cervix is observed.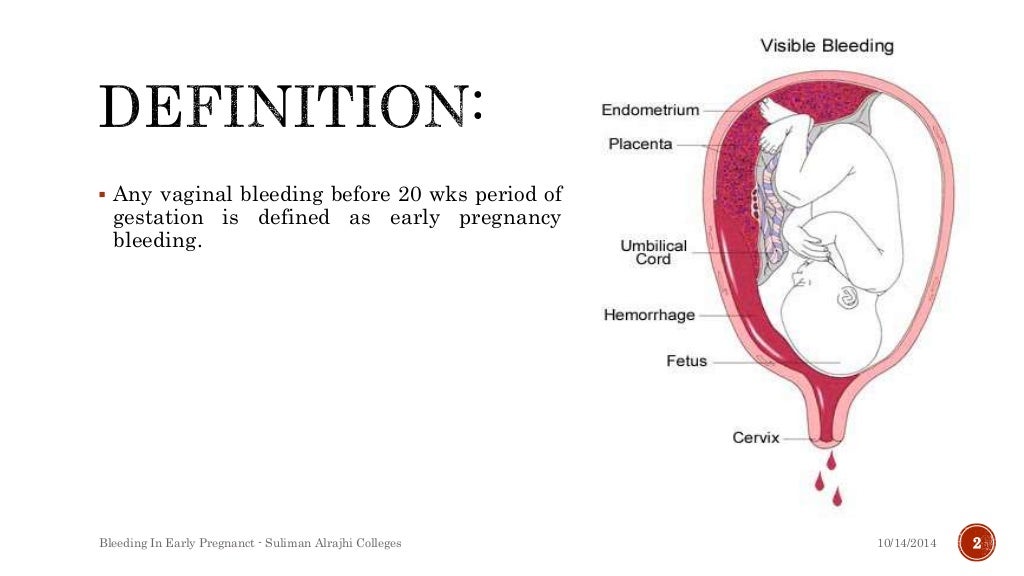 An increase in the tone of the myometrium may indicate the onset of placental abruption. Of the laboratory diagnostic methods, an analysis is used to determine the concentration of hCG (human chorionic gonadotropin). With ectopic pregnancy and bleeding, this figure will be reduced. Instrumental diagnosis of bleeding during pregnancy is to conduct an ultrasound scan. Using this method, it is possible to assess the state of the myometrium and the embryo, the level of blood flow in the vessels, the exact localization of the placenta and (possibly) its incipient detachment. Using CTG, the diagnostician can make a conclusion about the vital activity of the fetus.
An increase in the tone of the myometrium may indicate the onset of placental abruption. Of the laboratory diagnostic methods, an analysis is used to determine the concentration of hCG (human chorionic gonadotropin). With ectopic pregnancy and bleeding, this figure will be reduced. Instrumental diagnosis of bleeding during pregnancy is to conduct an ultrasound scan. Using this method, it is possible to assess the state of the myometrium and the embryo, the level of blood flow in the vessels, the exact localization of the placenta and (possibly) its incipient detachment. Using CTG, the diagnostician can make a conclusion about the vital activity of the fetus.
Treatment of bleeding during pregnancy also depends on the cause of the symptom. If there are no pathological changes or the manifestation is provoked by damage to the polyp, medical attention is not required. In rare cases, the doctor recommends its removal. Expectant tactics are also used in case of cervical erosion. Her cauterization is carried out after childbirth. Bleeding during pregnancy against the background of the threat of miscarriage and placenta previa requires immediate hospitalization in an obstetric hospital, followed by the appointment of drug treatment. To reduce uterine tone, sedatives, tocolytics are used. Pregnancy management in this case requires careful monitoring by a specialist.
Her cauterization is carried out after childbirth. Bleeding during pregnancy against the background of the threat of miscarriage and placenta previa requires immediate hospitalization in an obstetric hospital, followed by the appointment of drug treatment. To reduce uterine tone, sedatives, tocolytics are used. Pregnancy management in this case requires careful monitoring by a specialist.
Bleeding during pregnancy caused by ectopic attachment of the ovum, scar rupture, or completed spontaneous abortion requires hospitalization and surgical treatment. After removal of the remnants of fetal tissues or emergency delivery, antibiotic therapy is prescribed. In this case, stopping bleeding during pregnancy is carried out in different ways, depending on its intensity, often ligation of the uterine arteries is performed. With premature detachment of the placenta, an emergency caesarean section is indicated.
Prognosis and prevention of bleeding during pregnancy
Bleeding during pregnancy is usually accompanied by a favorable prognosis.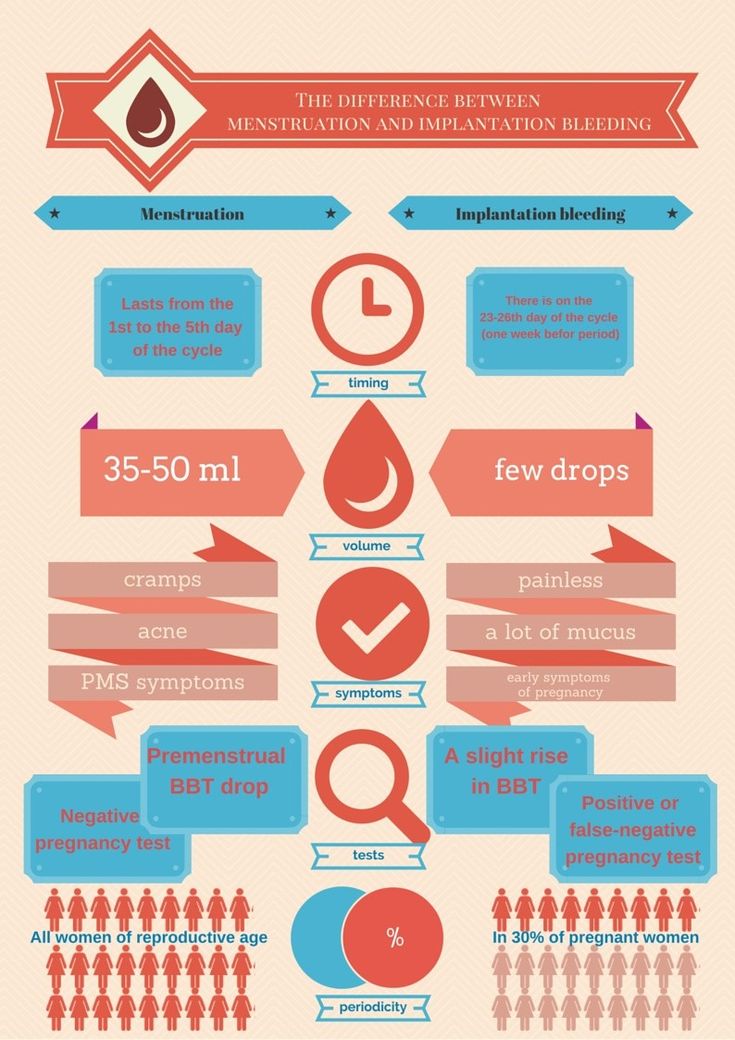 Timely medical care can save the life of the fetus and the woman. Lethal outcome is extremely rare. Prevention of bleeding during pregnancy consists in the early detection of benign neoplasms and their treatment even before conception. To prevent the development of a pathological symptom, you should register as soon as possible, take all the necessary tests, and if any violations occur, immediately seek advice from an obstetrician-gynecologist. Prevention of bleeding during pregnancy also consists in avoiding stress, physical exertion, violent sexual contacts.
Timely medical care can save the life of the fetus and the woman. Lethal outcome is extremely rare. Prevention of bleeding during pregnancy consists in the early detection of benign neoplasms and their treatment even before conception. To prevent the development of a pathological symptom, you should register as soon as possible, take all the necessary tests, and if any violations occur, immediately seek advice from an obstetrician-gynecologist. Prevention of bleeding during pregnancy also consists in avoiding stress, physical exertion, violent sexual contacts.
You can share your medical history, what helped you in the treatment of bleeding during pregnancy.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you.
 The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
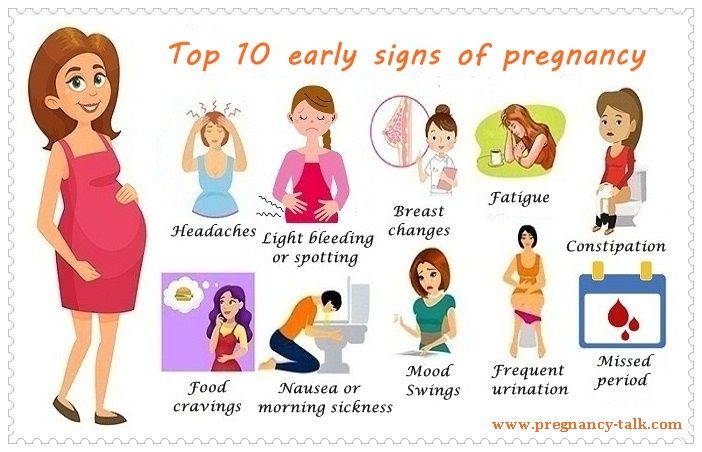
The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction. 1. Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder.
You should definitely see a doctor if:
- urination is painful (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! Under no circumstances should fluid intake be restricted! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods.
 It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen. 2. Nausea, vomiting, heartburn, increased susceptibility to smells.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To normalize bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions.
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day).
 You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day. You should definitely see a doctor if:
- the pain is severe
- mammary glands are very dense with redness and body temperature is increased
- discharge from the nipples appears (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own.
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, difficulty breathing, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries.
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
You should definitely see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7.
 Blood pressure fluctuations.
Blood pressure fluctuations. An ideal option for the course of any pregnancy is the stability of the blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130–139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits.
 Of the completely exotic for our days, but no less significant - the prevention of stress.
Of the completely exotic for our days, but no less significant - the prevention of stress. Life hack! If you first discovered that you have high normal pressure, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if:
- pressure increased by more than 10 mm Hg. relative to your usual
- an increase in the pressure index is accompanied by edema, the appearance of "flies" before the eyes
- one or both legs are severely swollen or discolored
- previously diagnosed varicose veins, family history of thrombosis
- along with itching there are areas of redness, spots, peeling
- itching increases
- you have loose teeth, sore gums, bad breath
- bleeding in the gum area increases
NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor.
Life hack! Keep a blood pressure diary, especially if you are prone to hypertension. Show your diary to your doctor at every appointment.
8. Heaviness and pain in the legs.
Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help.
You should always see a doctor if:
9. Skin changes.
During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs.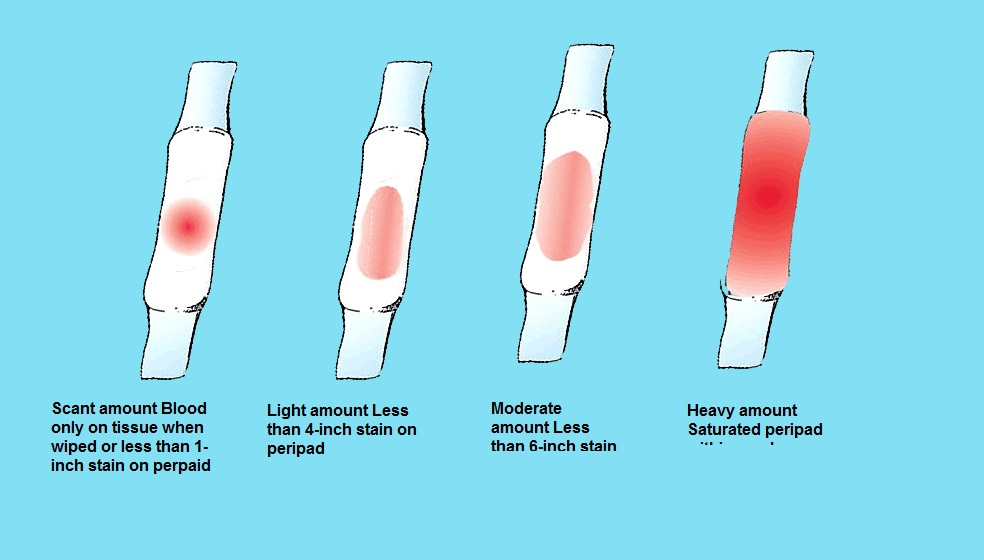 These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes.
You should definitely consult a doctor if:
10. Bleeding gums.
Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
You should definitely consult a doctor if:
11. Fatigue, mood instability.
Tearfulness, lack of strength, forgetfulness, distraction, the whole palette of feelings "here and now"... The list can be continued, and there is only one explanation for this - pregnancy. The most common early symptom is severe fatigue. There is no universal recipe, just as there is no single picture of these states. The main recommendation for all pregnant women is to rest often, relax and even sleep during the day. Most importantly, you need to remember: pregnancy is not a disease, but a great time to prepare for motherhood.