How to concive a child
Conceiving a baby - Better Health Channel
Most women under the age of 40 years who want to become pregnant (conceive) will achieve this within 12 months of starting to try. Here we explain how you can improve your chances of getting pregnant and having a healthy baby.
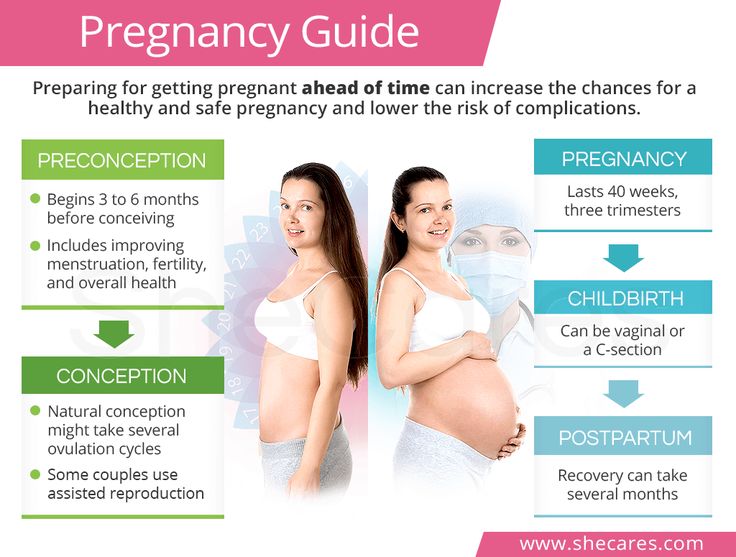
Planning for a baby
If you are planning to become pregnant, it’s important that you and your partner (if you have one) are as healthy as possible before you start trying. Your GP can help with a pre-conception health check.
A pre-conception health check usually includes:
- a medical history and a general examination
- blood tests to check your haemoglobin level, blood group, immunity for German measles (rubella) and chickenpox (varicella), hepatitis B and human immunodeficiency virus (HIV)
- tests for any sexually transmissible infection (STI)
- advice about lifestyle changes that will improve the chance of pregnancy and the health of the baby (lifestyle factors you may need to change include your weight, physical activity, alcohol consumption, recreational drug use, and whether you smoke)
- advising about folate and iodine supplements before conception and during pregnancy for the health of your baby
- referral to a specialist if either partner has a pre-existing medical condition that might affect the chances of pregnancy, or pregnancy health
- a review of any prescription medicines either partner may be taking
- referral for genetic counselling if needed
- information about health services and choices of pregnancy care.
Your FertilityExternal Link has some useful fact sheets about how to best prepare for pregnancy. On the Your Fertility website you can complete the Healthy Conception ToolExternal Link for personalised information about what you can do to improve your pre-conception health.
Timing and conception
To conceive, you need to have sex in the 5 days before you ovulate, or on the day you ovulate. This is called the ‘fertile window’. When the fertile window occurs depends on the length of your menstrual cycle.
Most women know when ovulation is approaching because they notice changes in their normal vaginal discharge, which becomes clear and slippery. Learn more about the fertile windowExternal Link and work out when yours occurs.
Age, fertility and conception
The most important factor for the chance of getting pregnant and having a healthy baby is the woman’s age. Fertility starts to slowly decline around age 32. By age 35, the fertility decline speeds up and by age 40, fertility has fallen by half.
The effect of men’s age on fertility is less dramatic but is an important factor too. Men aged 45 and older are less fertile, and some health conditions are more common in children with older fathers.
Find out more about the effects of age on fertility and pregnancy health.External Link
Weight, fertility and conception
Being overweight or underweight can cause hormonal changes that interfere with ovulation and reduce fertility. On average, women who are obese take longer to conceive than women in the healthy weight range and are more likely to experience infertility.
In men, obesity can lower fertility. This is likely due to a combination of factors including hormone problems, problems with erection or other health conditions linked to obesity.
Find out more about the effect of weight on fertility and pregnancy healthExternal Link.
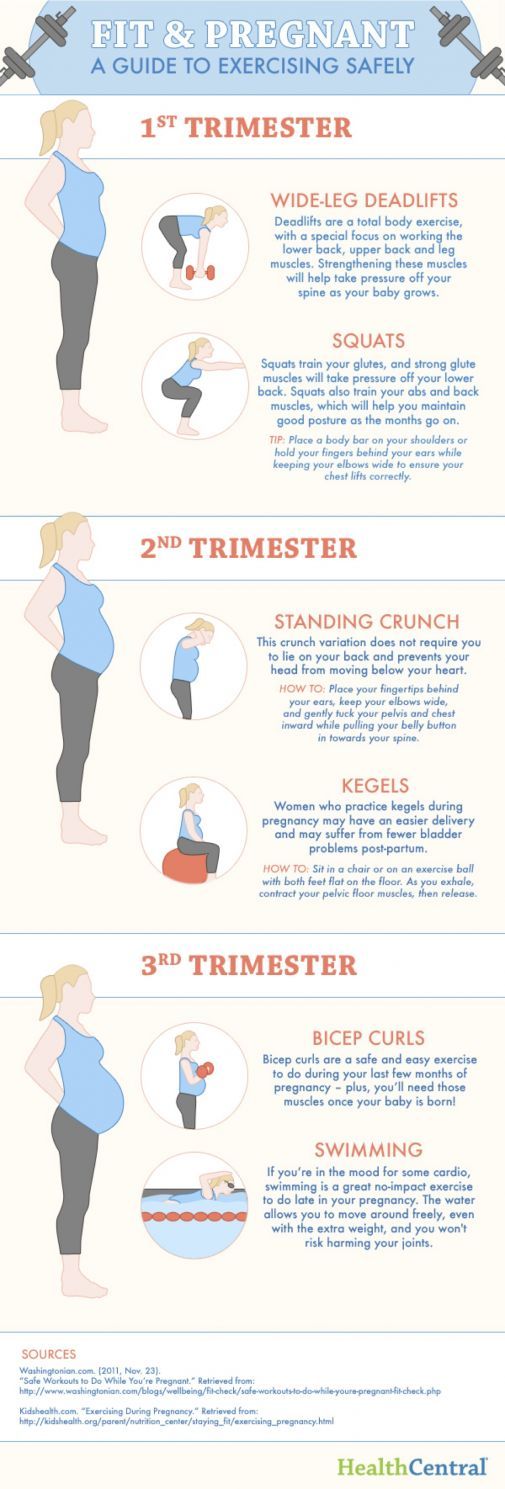
Diet, exercise and conception
There is no special diet that improves the odds of conception, but a healthy range of foods that includes lots of fresh fruits, vegetables and lean meats is recommended.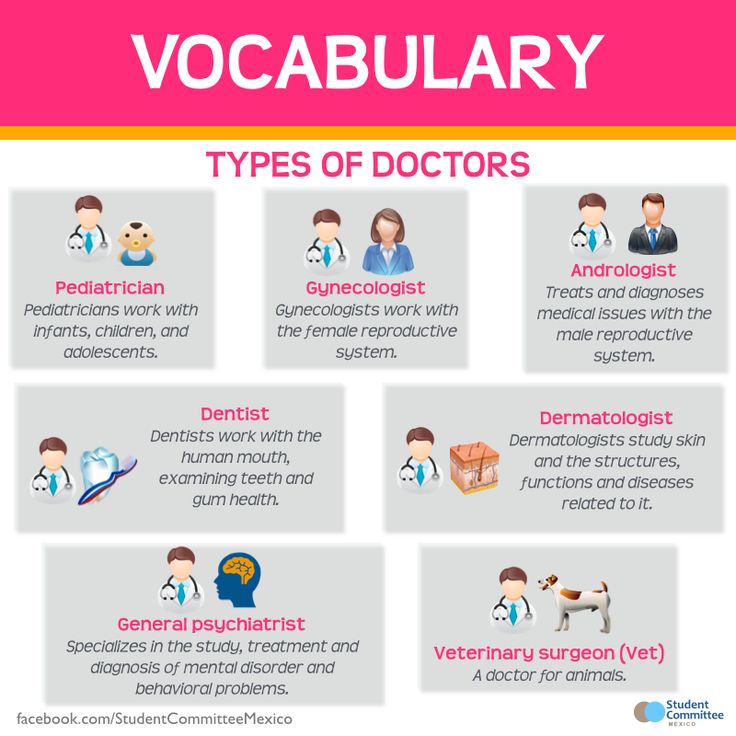
Vitamins and minerals (micronutrients) are essential for the body to function. Read more about the benefits of vitamins and minerals for fertility and pregnancy health, including folate, iodine, vitamin D, zinc and selenium supplements.
Regular exercise also improves fertility. Australian and international guidelines recommend you do at least 30 minutes of moderate-intensity physical activity – such as brisk walking, gardening or dancing – on most but preferably all days of the week. If possible, do some vigorous activity – such as running, fast cycling or fast swimming – every week as well.
For men and women who are overweight or obese, exercise can help to prevent further weight gain or achieve a modest weight loss that improves general health and fertility.
As part of weight management, international guidelines recommend that overweight or obese adults do 225-300 minutes of moderate-intensity exercise every week (this works out to about 35-45 minutes per day).
Tobacco, alcohol and drug use and conception
Tobacco, alcohol or recreational drug use reduces the chance of becoming pregnant. If you become pregnant and continue to smoke, drink alcohol or use recreational drugs, it can affect the health of your baby at birth and into adulthood.
Smoking and pregnancy
Smoking in pregnancy or exposure to second-hand smoke reduces fertility and increases the risk of pregnancy complications. To improve your own health and give your baby the best start in life, quit smoking before you try for a baby, and encourage your partner to do the same.
Quitting smoking can be very difficult, but there is help available. Read about the benefits of quittingExternal Link and visit QuitExternal Link for advice about how to kick the habit.
Alcohol and pregnancy
Alcohol can reduce both male and female fertility; even drinking lightly can reduce the likelihood of conception. In men, alcohol can impair fertility because it can cause impotence, reduce libido and affect sperm quality.
It is not clear what effect drinking small amounts of alcohol can have on unborn babies, but it is well known that high alcohol consumption can be harmful. The more alcohol consumed, the higher the risk to the unborn baby.
Binge drinking (more than six standard drinks on one occasion) can cause miscarriage, stillbirth, premature birth, small birth weight, and foetal alcohol spectrum disorder ( FASDExternal Link).
If you are pregnant or planning a pregnancy, not drinking alcohol is the safest option.
Drug use and pregnancy
Prescription medication and recreational drug use can potentially affect the health of the unborn baby. If you take prescription medication, speak to your pharmacist or doctor before trying for a baby.
Having trouble conceiving?
If you haven’t conceived within 12 months, there may be a fertility problem. About one in seven couples in Australia experiences infertility.
Fertility difficulties can be due to:
- female fertility problems (about 40 per cent)
- male fertility problems (about 40 per cent)
- both male and female fertility problems (about 10 per cent)
- unknown cause (about 10 per cent).
Female fertility problems include:
- problems with ovulation, including polycystic ovary syndrome (PCOS)
- blocked fallopian tubes
- endometriosis.
Male fertility problems include:
- poor sperm quality
- blockage of the spermatic cord, which is the tube that transports the sperm from the testis to the penis
- ejaculation disorders.
If you have trouble getting pregnant, talk with your GP who can refer you for tests to find out the cause of your problem. Find more information about causes of infertility and treatment options from the Victorian Assisted Reproductive Treatment AuthorityExternal Link.
Where to get help
- Your GP (doctor)
- Jean Hailes for Women’s HealthExternal Link
- Fertility Society of Australia and New ZealandExternal Link
- Healthy MaleExternal Link
- Your FertilityExternal Link
- Victorian Assisted Reproductive Treatment AuthorityExternal Link Tel.
 (03) 8601 5250
(03) 8601 5250 - Direct LineExternal Link – drug and alcohol counselling, information and referral service Tel. 1800 888 236
- Alcohol and Drug FoundationExternal LinkTel: 1300 85 85 84
- Women’s Alcohol and Drug ServiceExternal Link, the Royal Women’s Hospital Tel. (03) 8345 3931
- QuitlineExternal Link Tel. 13 78 48
- Billings LIFEExternal Link Tel. 1800 335 860
Conceiving a baby - Better Health Channel
Most women under the age of 40 years who want to become pregnant (conceive) will achieve this within 12 months of starting to try. Here we explain how you can improve your chances of getting pregnant and having a healthy baby.
Planning for a baby
If you are planning to become pregnant, it’s important that you and your partner (if you have one) are as healthy as possible before you start trying. Your GP can help with a pre-conception health check.
A pre-conception health check usually includes:
- a medical history and a general examination
- blood tests to check your haemoglobin level, blood group, immunity for German measles (rubella) and chickenpox (varicella), hepatitis B and human immunodeficiency virus (HIV)
- tests for any sexually transmissible infection (STI)
- advice about lifestyle changes that will improve the chance of pregnancy and the health of the baby (lifestyle factors you may need to change include your weight, physical activity, alcohol consumption, recreational drug use, and whether you smoke)
- advising about folate and iodine supplements before conception and during pregnancy for the health of your baby
- referral to a specialist if either partner has a pre-existing medical condition that might affect the chances of pregnancy, or pregnancy health
- a review of any prescription medicines either partner may be taking
- referral for genetic counselling if needed
- information about health services and choices of pregnancy care.
Your FertilityExternal Link has some useful fact sheets about how to best prepare for pregnancy. On the Your Fertility website you can complete the Healthy Conception ToolExternal Link for personalised information about what you can do to improve your pre-conception health.
Timing and conception
To conceive, you need to have sex in the 5 days before you ovulate, or on the day you ovulate. This is called the ‘fertile window’. When the fertile window occurs depends on the length of your menstrual cycle.
Most women know when ovulation is approaching because they notice changes in their normal vaginal discharge, which becomes clear and slippery. Learn more about the fertile windowExternal Link and work out when yours occurs.
Age, fertility and conception
The most important factor for the chance of getting pregnant and having a healthy baby is the woman’s age. Fertility starts to slowly decline around age 32. By age 35, the fertility decline speeds up and by age 40, fertility has fallen by half.
The effect of men’s age on fertility is less dramatic but is an important factor too. Men aged 45 and older are less fertile, and some health conditions are more common in children with older fathers.
Find out more about the effects of age on fertility and pregnancy health.External Link
Weight, fertility and conception
Being overweight or underweight can cause hormonal changes that interfere with ovulation and reduce fertility. On average, women who are obese take longer to conceive than women in the healthy weight range and are more likely to experience infertility.
In men, obesity can lower fertility. This is likely due to a combination of factors including hormone problems, problems with erection or other health conditions linked to obesity.
Find out more about the effect of weight on fertility and pregnancy healthExternal Link.
Diet, exercise and conception
There is no special diet that improves the odds of conception, but a healthy range of foods that includes lots of fresh fruits, vegetables and lean meats is recommended.
Vitamins and minerals (micronutrients) are essential for the body to function. Read more about the benefits of vitamins and minerals for fertility and pregnancy health, including folate, iodine, vitamin D, zinc and selenium supplements.
Regular exercise also improves fertility. Australian and international guidelines recommend you do at least 30 minutes of moderate-intensity physical activity – such as brisk walking, gardening or dancing – on most but preferably all days of the week. If possible, do some vigorous activity – such as running, fast cycling or fast swimming – every week as well.
For men and women who are overweight or obese, exercise can help to prevent further weight gain or achieve a modest weight loss that improves general health and fertility.
As part of weight management, international guidelines recommend that overweight or obese adults do 225-300 minutes of moderate-intensity exercise every week (this works out to about 35-45 minutes per day).
Tobacco, alcohol and drug use and conception
Tobacco, alcohol or recreational drug use reduces the chance of becoming pregnant. If you become pregnant and continue to smoke, drink alcohol or use recreational drugs, it can affect the health of your baby at birth and into adulthood.
Smoking and pregnancy
Smoking in pregnancy or exposure to second-hand smoke reduces fertility and increases the risk of pregnancy complications. To improve your own health and give your baby the best start in life, quit smoking before you try for a baby, and encourage your partner to do the same.
Quitting smoking can be very difficult, but there is help available. Read about the benefits of quittingExternal Link and visit QuitExternal Link for advice about how to kick the habit.
Alcohol and pregnancy
Alcohol can reduce both male and female fertility; even drinking lightly can reduce the likelihood of conception. In men, alcohol can impair fertility because it can cause impotence, reduce libido and affect sperm quality.
It is not clear what effect drinking small amounts of alcohol can have on unborn babies, but it is well known that high alcohol consumption can be harmful. The more alcohol consumed, the higher the risk to the unborn baby.
Binge drinking (more than six standard drinks on one occasion) can cause miscarriage, stillbirth, premature birth, small birth weight, and foetal alcohol spectrum disorder ( FASDExternal Link).
If you are pregnant or planning a pregnancy, not drinking alcohol is the safest option.
Drug use and pregnancy
Prescription medication and recreational drug use can potentially affect the health of the unborn baby. If you take prescription medication, speak to your pharmacist or doctor before trying for a baby.
Having trouble conceiving?
If you haven’t conceived within 12 months, there may be a fertility problem. About one in seven couples in Australia experiences infertility.
Fertility difficulties can be due to:
- female fertility problems (about 40 per cent)
- male fertility problems (about 40 per cent)
- both male and female fertility problems (about 10 per cent)
- unknown cause (about 10 per cent).
Female fertility problems include:
- problems with ovulation, including polycystic ovary syndrome (PCOS)
- blocked fallopian tubes
- endometriosis.
Male fertility problems include:
- poor sperm quality
- blockage of the spermatic cord, which is the tube that transports the sperm from the testis to the penis
- ejaculation disorders.
If you have trouble getting pregnant, talk with your GP who can refer you for tests to find out the cause of your problem. Find more information about causes of infertility and treatment options from the Victorian Assisted Reproductive Treatment AuthorityExternal Link.
Where to get help
- Your GP (doctor)
- Jean Hailes for Women’s HealthExternal Link
- Fertility Society of Australia and New ZealandExternal Link
- Healthy MaleExternal Link
- Your FertilityExternal Link
- Victorian Assisted Reproductive Treatment AuthorityExternal Link Tel.
 (03) 8601 5250
(03) 8601 5250 - Direct LineExternal Link – drug and alcohol counselling, information and referral service Tel. 1800 888 236
- Alcohol and Drug FoundationExternal LinkTel: 1300 85 85 84
- Women’s Alcohol and Drug ServiceExternal Link, the Royal Women’s Hospital Tel. (03) 8345 3931
- QuitlineExternal Link Tel. 13 78 48
- Billings LIFEExternal Link Tel. 1800 335 860
9 rules of conception - what to do to increase the chances of conceiving a child
Sometimes it happens that it is not possible to conceive a child immediately, but after several unsuccessful sexual intercourses, you should not sound the alarm and diagnose yourself with infertility. Perhaps your “stork”, who will bring you a baby, just needs to actively help.
Rule 1
Everyone knows that the male reproductive cell is the basis of conception, therefore, a certain energy is required from the spermatozoon to ensure its mobility, because an energetic spermatozoon is able to go further, and one should not expect conception from a weak one. And if pregnancy occurs, then there is a high risk of DNA breakdowns, which lead to a missed pregnancy or spontaneous abortion. That is why, two weeks before the decisive sexual intercourse, you need to start preparing a man. To do this, you need to start feeding him properly: include more meat, nuts, vitamin E in the diet. Such nutrition will help increase sperm motility.
And if pregnancy occurs, then there is a high risk of DNA breakdowns, which lead to a missed pregnancy or spontaneous abortion. That is why, two weeks before the decisive sexual intercourse, you need to start preparing a man. To do this, you need to start feeding him properly: include more meat, nuts, vitamin E in the diet. Such nutrition will help increase sperm motility.
It is worth noting that the excessive activity of partners for conception is not only useless, but also harmful. Therefore, before the decisive sexual intercourse, a man should abstain for 2-3 days in order to accumulate energy. One couple went to the doctor because they could not conceive a child. During the conversation, it turned out that the couple wants a child so much that they have sex 2-3 times a day. After that, the doctor advised to abstain from sex for several days. Following the recommendation of the doctor, the couple managed to conceive a child.
Rule 2
The first intercourse is decisive for conception. All further acts in the evening or night are just for fun. The fact is that after the first sexual intercourse, the concentration of spermatozoa decreases by almost half, so subsequent ejaculations, as experts joke, are one water.
All further acts in the evening or night are just for fun. The fact is that after the first sexual intercourse, the concentration of spermatozoa decreases by almost half, so subsequent ejaculations, as experts joke, are one water.
Rule 3
Immediately after ejaculation, a man should remove the penis from the vagina to help the sperm to penetrate further, which greatly increases the likelihood of conception.
Rule 4
The female orgasm can prevent conception. This happens because during orgasm, the cervix rises a little, so the spermatozoa have to climb this peak, which significantly reduces the chance of one of them reaching the egg.
Rule 5
Proper timing of conception plays a significant role in conception. A woman is more fertile in the middle of the cycle, when the egg matures (ovulation period). 5-6 days before ovulation are also considered favorable: this is how long a sperm cell can live, waiting for an egg and remaining capable. The period within 6 days after ovulation is also considered favorable, since the female egg remains viable during this period of time.
The period within 6 days after ovulation is also considered favorable, since the female egg remains viable during this period of time.
Rule 6
Douching with baking soda before intercourse can significantly increase your chances of getting pregnant. It is known that a woman may have hidden inflammation, which she does not even know about. As a result of inflammation, an acidic environment arises, which is extremely harmful to spermatozoa and can not only significantly reduce their activity, but even completely destroy them. If there is no inflammation, then douching still does not hurt.
7 rule
The actions of a woman after intercourse are of great importance. Little depends on the man and he can safely go to the shower, but the woman should lie down for a while. With the normal position of the uterus and cervix, it is best to lie on your back, while pressing your knees to your chest. If a woman has a bend of the uterus, it is better to lie on her stomach. These positions allow the cervix to sink freely into the semen pool, which increases the chance of sperm penetration. There are also specific cases, for example, when there is inflammation of the appendages. In this situation, the uterus can turn to the side, but in which one - this can only be determined by a gynecologist at a consultation. Then the doctor can tell you exactly which side is better to lie on.
These positions allow the cervix to sink freely into the semen pool, which increases the chance of sperm penetration. There are also specific cases, for example, when there is inflammation of the appendages. In this situation, the uterus can turn to the side, but in which one - this can only be determined by a gynecologist at a consultation. Then the doctor can tell you exactly which side is better to lie on.
8 rule
Choosing the right position can greatly increase your chances of conceiving a child. Unfortunately, the choice of correct poses is not great - this is the classic missionary pose. But if you try to get pregnant, for example, while standing, then the liquid will simply pour out. There is indeed an exception. If a woman has a uterine bend, then the back position is suitable.
Rule 9
After sexual intercourse, it is imperative to relax and preferably be in an excellent state of mind for the next few days. Meditation, nature walks, outdoor activities, etc. can help with this. Waiting and worrying is not the best condition for this period. In a state of stress, the contractile activity of the fallopian tubes, which promote spermatozoa to the egg, is disrupted. Listen to the recommendations of gynecologists and you will succeed.
can help with this. Waiting and worrying is not the best condition for this period. In a state of stress, the contractile activity of the fallopian tubes, which promote spermatozoa to the egg, is disrupted. Listen to the recommendations of gynecologists and you will succeed.
How to prepare for conception?
Pregnancy planning is really necessary, especially in our time, when a healthy woman is the exception rather than the rule. Not to mention the fact that pregnancy is a serious test for the body of even a perfectly healthy woman.
It can be said that entering into pregnancy without preliminary preparation for it is the same as flying on an airplane that has not been checked in advance: maybe it will cost, or maybe not. Of course, aircraft are tested before each flight. So why does a woman, ready to give birth to a new human being, not always conduct a similar check of her body? After all, the price of her neglect of herself and her health can be the life of the unborn child.
The process of preparing for pregnancy is quite complex and includes several stages. It is worth starting planning a few months (at least three) before the time when the couple intends to conceive a baby.
And at the stage of pregnancy planning , it is necessary to understand that the bearing and birth of a baby is not a woman's business, but a married couple's. Therefore, the active participation of the father in planning pregnancy is extremely necessary and important for himself, and for his wife, and for the unborn baby.
Without the help of doctors, it will not be possible to manage even at this stage. A visit to the gynecologist will allow you to identify possible diseases and treat them in a timely manner. After the first appeal, future parents undergo several examinations and pass certain tests in order to find out how ready their bodies are for conceiving a baby, as well as to prevent possible problems when carrying a child. The gynecologist will tell you what to do if, before planning a pregnancy, a woman was protected with hormonal contraceptives. It is necessary to stop taking hormonal contraceptives 3 months before the planned pregnancy.
It is necessary to stop taking hormonal contraceptives 3 months before the planned pregnancy.
It is important for a future mother to understand that only a healthy woman can bear and give birth to a healthy baby. In this regard, you need to start taking care of your own health long before conception. Good physical shape, the absence of diseases, proper nutrition and the rejection of bad habits, hygiene and a measured lifestyle - all this has a beneficial effect on the female body and subsequently makes it easier to endure pregnancy. However, not all vitamins can be obtained from food. For example, the body can only obtain folic acid in an artificial form, since its counterpart (folate), found in green vegetables, beans, asparagus, and citrus fruits, is much less absorbed. Folic acid is very important for the development of the baby to take place correctly, and the need for its intake exists throughout pregnancy. If the mother's body during the bearing of the child receives a sufficient amount of this substance, then the risk of pathology from the nervous system is minimized.
What tests should a married couple undergo
before planning a pregnancy?
- Gynecological examination, colposcopy for women.
- Blood type, Rh factor for both spouses. If a woman has a positive Rh factor, there is no problem. If a woman has a negative Rh factor - antibodies to the Rh factor (even if a man is also negative). If they are positive, pregnancy is not currently possible and needs to be corrected. If negative - repeat this analysis once a month, starting from 8 weeks of pregnancy. If a woman has 1 group, and a man has any other group, incompatibility by blood types is possible. An analysis for group antibodies, as well as an analysis for antibodies to the Rh factor, is carried out once a month, starting from 8 weeks of pregnancy.
- Tests for infections: routine smear, PCR for latent infections - both spouses.
- Blood test for TORCH-complex. Antibodies to rubella, toxoplasma, herpes, CMV, chlamydia - quantitative analysis (with titer).
 The presence of IgG antibodies means immunity to these infections, and is not an obstacle to pregnancy. The presence of IgM means an acute stage, planning in this case must be postponed until recovery. If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it.
The presence of IgG antibodies means immunity to these infections, and is not an obstacle to pregnancy. The presence of IgM means an acute stage, planning in this case must be postponed until recovery. If there are no IgG antibodies to rubella, it is necessary to be vaccinated and protected for another 3 months after it. - A trip to the dentist, a therapist, chest x-ray is a must for both spouses. By appointment of the therapist - consultation of narrow specialists (ENT doctor, urologist, endocrinologist, cardiologist, gastroenterologist).
- Spermogram. Desirable, but not required. It is done to determine the quality of spermatozoa and identify a hidden inflammatory process (a much more informative analysis than any smears and PCR).
- Ultrasound of the pelvic organs - at least 2 times per cycle: after menstruation and before menstruation. For the first time, the general condition of the pelvic organs is assessed, in the second, the presence of a corpus luteum and endometrial transformation, indicating that ovulation has occurred.