Breast feeding to boy
Frequently Asked Questions (FAQs) | Breastfeeding
What are the benefits of breastfeeding?
Breastfeeding is good for both infants and mothers. Breast milk is the best source of nutrition for most infants. As an infant grows, breast milk changes to meet the infant’s nutritional needs. Breastfeeding can also help protect the infant and mother against certain illnesses and diseases:
Benefits to Infants
Infants who are breastfed have a lower risk of:
- Asthma.
- Obesity.
- Type 1 diabetes.
- Severe lower respiratory disease.
- Acute otitis media (ear infections).
- Sudden infant death syndrome (SIDS).
- Gastrointestinal infections (diarrhea/vomiting).
- Necrotizing enterocolitis (NEC) for preterm infants.
Benefit to Mothers
Mothers who breastfeed their infants have a lower risk of:
- Breast cancer.
- Ovarian cancer.
- Type 2 diabetes.
- High blood pressure.
Families can visit CDC’s Infant and Toddler Nutrition website to learn more about what to expect while breastfeeding.
When should a mother avoid breastfeeding (contraindications)?
Breast milk provides the best nutrition for most infants, including premature and sick newborns. However, there are rare exceptions when breast milk or breastfeeding is not recommended. Learn more about contraindications to breastfeeding.
Only a few medications are contraindicated (not recommended) while breastfeeding. Although many medications do pass into breast milk, most have little or no effect on milk supply or on an infant’s well-being. However, health care providers should always weigh the risks and benefits when prescribing medications to breastfeeding mothers.
Learn more about safe prescription medication use while breastfeeding.
Top of Page
How is growth assessed for breastfed infants?
In the United States, the World Health Organization (WHO) Growth Standard Charts are recommended for use with both breastfed and formula-fed infants and children, from birth to 2 years of age, to monitor growth. The WHO growth charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
The WHO growth charts reflect growth patterns among children who were predominantly breastfed for at least 4 months and were still breastfeeding at 12 months. The WHO growth charts establish the growth of the breastfed infant as the norm for growth and are the standards for how children should grow when provided optimal conditions. Clinicians should be aware that healthy breastfed infants typically gain weight faster than formula-fed infants in the first few months of life but then gain weight more slowly for the remainder of infancy, even after complementary foods are introduced.
For children older than 2 years (2 to 19 years of age) CDC and the American Academy of Pediatrics recommend that health care providers use the CDC Growth Reference Charts.
Visit the Growth Chart Training website for a set of self-directed, interactive training courses.
Source: Grummer-Strawn LM, Reinold C, Krebs NF. Use of the World Health Organization and CDC growth charts for children aged 0 to 59 months in the United States. MMWR Recomm Rep. 2010;59(RR-9):1–15.
MMWR Recomm Rep. 2010;59(RR-9):1–15.
Top of Page
How long should a mother breastfeed?
The U.S. Dietary Guidelines for Americans [PDF-30.6MB] recommend that infants be exclusively breastfed for about the first 6 months, and then continuing breastfeeding while introducing appropriate complementary foods until your child is 12 months old or older. The American Academy of Pediatrics and the World Health Organization also recommend exclusive breastfeeding for about the first 6 months, with continued breastfeeding along with introducing appropriate complementary foods for up to 2 years of age or longer.
Mothers should be encouraged to breastfeed their children for at least 1 year. The longer an infant is breastfed, the greater the protection from certain illnesses and long-term diseases. The more months or years a woman breastfeeds (combined breastfeeding of all her children), the greater the benefits to her health as well.
The American Academy of Pediatrics recommends that children be introduced to foods other than breast milk or infant formula when they are about 6 months old. To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
To learn more about infant and toddler feeding, visit CDC’s Infant and Toddler Nutrition website.
Top of Page
What can happen if someone else’s breast milk is given to another child?
Very few illnesses are transmitted via breast milk. Learn more about what to do if an infant or child is mistakenly fed another woman’s expressed breast milk.
Top of Page
Are special precautions needed for handling breast milk?
CDC does not list human breast milk as a body fluid to which universal precautions apply. Occupational exposure to human breast milk has not been shown to lead to transmission of HIV or Hepatitis B infection. However, because human breast milk has been implicated in transmitting HIV from mother to infant, gloves may be worn as a precaution by health care workers who are frequently exposed to breast milk (e.g., people working in human milk banks (defined below). For additional information regarding universal precautions as they apply to breast milk in the transmission of HIV and Hepatitis B infections, visit the following resources:
Centers for Disease Control and Prevention. Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Perspectives in disease prevention and health promotion update: universal precautions for prevention of transmission of human immunodeficiency virus, Hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988;37(24):377–388.
Top of Page
Where can mothers find more information about preparation and storage of breast milk?
CDC has guidelines for proper storage and preparation of breast milk to maintain the safety and quality of expressed breast milk for the health of the baby.
For more information about specific storage and preparation of breast milk questions, such as where to store breast milk at work, and what to do when the power goes out, visit CDC’s Storage and Preparation of Breast Milk Frequently Asked Questions.
Top of Page
What are human milk banks?
Human milk banks are a service established for the purpose of collecting milk from donors and processing, screening, storing, and distributing donated milk to meet the specific needs of individuals for whom human milk is prescribed by licensed health care providers. When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
When possible, human milk banks also serve healthy infants who have been adopted or are not able to get their own mother’s milk.
Milk banks accept donations directly at their deposit sites or they can arrange for safe, overnight transportation of human milk at no cost to the donor. Learn more about donating to a milk bank by visiting the Human Milk Banking Association of North America (HMBANA).
Top of Page
Is it safe for families to buy breast milk on the internet?
The American Academy of Pediatrics and the Food and Drug Administration recommend avoiding Internet-based milk sharing sites and instead recommend contacting milk banks. Research has demonstrated that some milk samples sold online have been contaminated with a range of bacteria.1
Nonprofit donor human milk banks, where processed human milk comes from screened donors, have a long safety record in North America. All member banks of the Human Milk Banking Association of North America (HMBANA) must operate under specific evidence-based guidelines that require extensive testing and processing procedures as well as self-reported health information and a health statement from both the donor’s health care provider and the infant’s health care provider. Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
Because most of the milk from milk banks is given to hospitalized and fragile infants, milk banks may not have enough to serve healthy infants at all times. To find a human milk bank, contact HMBANA.
1Keim, SA, Hogan, JS, McNamara, KA, et al. Microbial contamination of human milk purchased via the internet. Pediatrics. 2013;132(5).
Top of Page
What legal rights do breastfeeding mothers have?
Breastfeeding Laws
- All 50 states, the District of Columbia, Puerto Rico and the Virgin Islands have laws that specifically allow women to breastfeed in any public or private location. Visit the National Conference of State Legislatures to learn more about federal and state laws that protect and support breastfeeding.
Workplace Laws
- The “Break Time for Nursing Mothers Provision” of the Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk.
 Visit the United States Department of Labor to learn more.
Visit the United States Department of Labor to learn more.
Travel Laws
- Air travelers are permitted by the Transportation Security Administration (TSA) to bring breast milk, formula, and juice in excess of 3.4 ounces in their carry-on baggage and it does not need to fit within a quart size bag. Ice packs, freezer packs, and other accessories needed to keep the liquid cool are also allowed in carry-on bags. All liquids and partially frozen accessories are subject to being screened by X-ray. TSA is required by the Bottles and Breastfeeding Equipment Screening Act (BABES act) to provide ongoing training to ensure TSA staff receive consistent training related to traveling with breast milk, formula, and infant feeding equipment. Visit the TSA to learn more about traveling with breast milk, formula, and juice. For tips on travel and breastfeeding, visit Travel Recommendations for the Nursing Mother.
Visit the Federal Policies, Programs, & Initiatives website to learn more about laws related to breastfeeding protections.
Top of Page
How can a mother continue to provide breast milk to her infant after returning to work or school?
Being prepared for returning to work or school can help a mother ease the transition and continue to breastfeed after her maternity leave is over. The Office on Women’s Health has information for making this transition easier.
When a mother is away from her infant, she can pump or hand express her breast milk so that her infant can drink breast milk from a bottle. Mothers can visit CDC’s Infant and Toddler Nutrition website to learn more about pumping breast milk.
Mothers who are expressing their breast milk should visit the CDC’s Proper Storage and Preparation of Breast Milk website to learn how to prepare and store breast milk safely for her infant.
The Patient Protection and Affordable Care Act (ACA) requires employers to support breastfeeding mothers to express breast milk for 1 year after each child’s birth by providing mothers with reasonable break time and a private, non-bathroom space to express their breast milk. For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
For more information about the types of employees and employers to which the requirements apply, refer to the United States Department of Labor’s Frequently Asked Questions.
Top of Page
Where can mothers find breastfeeding support and additional Information about breastfeeding?
Help mothers find lactation support through the following resources:
- International Lactation Consultant Association (IBCLCs)
- United States Lactation Consultant Association (IBCLCs)
- Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics
- La Leche League
Help mothers find resources about breastfeeding by directing them to the following websites:
- CDC— Infant and Toddler Nutrition
- Office on Women’s Health—Breastfeeding
- American Academy of Pediatrics—Healthy Children
- United States Breastfeeding Committee—State Coalitions Directory
- US Department of Agriculture—WIC Breastfeeding Support
Top of Page
Does breastfeeding during a child’s vaccine injections help with pain management?
Parents who are breastfeeding should be encouraged to breastfeed children age 2 years or younger before, during, and after their child’s vaccination. Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Several aspects of breastfeeding are thought to decrease pain by multiple mechanisms: being held by the parent, feeling skin-to-skin contact, suckling, being distracted, and ingesting breast milk. Potential adverse events such as gagging or spitting up have not been reported. Alternatives to breastfeeding include bottle-feeding with expressed breast milk or formula throughout the child’s procedure, which simulates aspects of breastfeeding.
Top of Page
Does breastfeeding after a child’s rotavirus vaccine impact the vaccine’s efficacy?
There is not sufficient evidence to suggest that breastfeeding can have a negative effect on rotavirus vaccine efficacy. A previous study found that human milk from women who live in areas with endemic rotavirus contains antibodies that can neutralize live rotavirus vaccine virus. However, in licensing trials, the effectiveness of rotavirus vaccine in breastfed infants was comparable to that in non-breastfed infants.
CDC does not recommend restricting or discontinuing breastfeeding before or after a child receives the rotavirus vaccine. Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Breastfed infants should be vaccinated according to the same schedule as non-breastfed infants.
Learn More about prevention of Rotavirus Gastroenteritis among infants and children.
Top of Page
Breast feeding and timing of puberty in boys and girls: A nationwide cohort study
. 2021 Sep;35(5):578-589.
doi: 10.1111/ppe.12767. Epub 2021 May 26.
Julie J Hvidt 1 , Nis Brix 1 2 , Andreas Ernst 1 3 , Lea L H Lunddorf 1 , Cecilia H Ramlau-Hansen 1
Affiliations
Affiliations
- 1 Department of Public Health, Research Unit for Epidemiology, Aarhus University, Aarhus, Denmark.

- 2 Department of Clinical Genetics, Aarhus University Hospital, Aarhus, Denmark.
- 3 Department of Urology, Aarhus University Hospital, Aarhus, Denmark.
- PMID: 34080724
- DOI: 10.1111/ppe.12767
Julie J Hvidt et al. Paediatr Perinat Epidemiol. 2021 Sep.
. 2021 Sep;35(5):578-589.
doi: 10.1111/ppe.12767. Epub 2021 May 26.
Authors
Julie J Hvidt 1 , Nis Brix 1 2 , Andreas Ernst 1 3 , Lea L H Lunddorf 1 , Cecilia H Ramlau-Hansen 1
Affiliations
- 1 Department of Public Health, Research Unit for Epidemiology, Aarhus University, Aarhus, Denmark.

- 2 Department of Clinical Genetics, Aarhus University Hospital, Aarhus, Denmark.
- 3 Department of Urology, Aarhus University Hospital, Aarhus, Denmark.
- PMID: 34080724
- DOI: 10.1111/ppe.12767
Abstract
Background: Breast feeding has been associated with improved infant health, but its impact on pubertal timing remains uncertain, particularly in boys.
Objective: The objective of this study was to investigate the association between duration of breast feeding and pubertal timing in boys and girls.
Methods: This population-based cohort study included 13 511 boys and girls from the Puberty Cohort nested within the Danish National Birth Cohort. The children gave half-yearly, self-reported information on pubertal development through questionnaires (Tanner stages, age at menarche, first ejaculation, voice break, axillary hair growth, and acne). Information on breast feeding was provided by the mothers when the children were 6 months of age. We estimated mean differences (in months) in age at attaining each pubertal marker and for overall timing of puberty (combined estimate) for every additional month of exclusive breast feeding. Furthermore, we estimated differences in pubertal age when comparing children never exclusively breastfed and exclusively breastfed <4 months using children exclusively breastfed ≥4 months as reference. In sub-analyses, we further adjusted for infant weight gain and childhood BMI at 7 years to investigate whether these variables mediated the association.
Results: Boys tended to reach pubertal markers later for every additional month of exclusive breast feeding (combined estimate: 0.2 (95% confidence interval [CI] 0.0, 0.4 months). Never exclusively breastfed boys reached pubertal markers earlier than the boys exclusively breastfed ≥4 months (combined estimate: -4.1 (95% CI -6.7, -1.6) months). Boys exclusively breastfed <4 months also reached pubertal markers earlier than those never exclusively breastfed but with smaller differences. In girls, duration of breast feeding was not associated with pubertal development. When including infant weight gain or childhood BMI, the results remained essentially unchanged.
Conclusions: Shorter duration of exclusive breast feeding was associated with earlier pubertal development in boys but not in girls.
Keywords: breast feeding; pubertal timing; puberty; tanner stages.
© 2021 John Wiley & Sons Ltd.
Similar articles
-
Parental time to pregnancy, medically assisted reproduction and pubertal development in boys and girls.
Ernst A, Lauridsen LLB, Brix N, Arah OA, Olsen J, Olsen LH, Ramlau-Hansen CH. Ernst A, et al. Hum Reprod. 2019 Apr 1;34(4):724-732. doi: 10.1093/humrep/dez008. Hum Reprod. 2019. PMID: 30753468 Free PMC article.
-
Timing of puberty in boys and girls: A population-based study.
Brix N, Ernst A, Lauridsen LLB, Parner E, Støvring H, Olsen J, Henriksen TB, Ramlau-Hansen CH. Brix N, et al. Paediatr Perinat Epidemiol. 2019 Jan;33(1):70-78. doi: 10.1111/ppe.12507. Epub 2018 Oct 11. Paediatr Perinat Epidemiol. 2019. PMID: 30307620 Free PMC article.

-
Childhood overweight and obesity and timing of puberty in boys and girls: cohort and sibling-matched analyses.
Brix N, Ernst A, Lauridsen LLB, Parner ET, Arah OA, Olsen J, Henriksen TB, Ramlau-Hansena CH. Brix N, et al. Int J Epidemiol. 2020 Jun 1;49(3):834-844. doi: 10.1093/ije/dyaa056. Int J Epidemiol. 2020. PMID: 32372073 Free PMC article.
-
Size at birth, infant growth, and age at pubertal development in boys and girls.
Hvidt JJ, Brix N, Ernst A, Lauridsen LLB, Ramlau-Hansen CH. Hvidt JJ, et al. Clin Epidemiol. 2019 Sep 19;11:873-883. doi: 10.2147/CLEP.S217388. eCollection 2019. Clin Epidemiol. 2019. PMID: 31572017 Free PMC article.
-
Early additional food and fluids for healthy breastfed full-term infants.

Becker GE, Remmington T. Becker GE, et al. Cochrane Database Syst Rev. 2014 Nov 25;(11):CD006462. doi: 10.1002/14651858.CD006462.pub3. Cochrane Database Syst Rev. 2014. PMID: 25420475 Updated. Review.
See all similar articles
Cited by
-
The Role of Pediatric Nutrition as a Modifiable Risk Factor for Precocious Puberty.
Calcaterra V, Verduci E, Magenes VC, Pascuzzi MC, Rossi V, Sangiorgio A, Bosetti A, Zuccotti G, Mameli C. Calcaterra V, et al. Life (Basel). 2021 Dec 7;11(12):1353. doi: 10.3390/life11121353. Life (Basel). 2021. PMID: 34947884 Free PMC article. Review.
References
REFERENCES
-
- UNICEF WHO. Global strategy for infant and young child feeding.
 2003.
2003.
- UNICEF WHO. Global strategy for infant and young child feeding.
-
- Victora CG, Bahl R, Barros AJD, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490.
-
- Ong KKL, Preece MA, Emmett PM, Ahmed ML, Dunger DB. Size at birth and early childhood growth in relation to maternal smoking, parity and infant breast-feeding: longitudinal birth cohort study and analysis. Pediatr Res. 2002;52(6):863-867.
-
- Azad MB, Vehling L, Chan D, et al. Infant feeding and weight gain: separating breast milk from breastfeeding and formula from food. Pediatrics. 2018;142(4).
-
- Wagner IV, Sabin MA, Pfäffle RW, et al.
 Effects of obesity on human sexual development. Nat Rev Endocrinol. 2012;8(4):246-254.
Effects of obesity on human sexual development. Nat Rev Endocrinol. 2012;8(4):246-254.
- Wagner IV, Sabin MA, Pfäffle RW, et al.
Publication types
MeSH terms
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger. Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
What is a "milk flush"?
At the beginning of each feed, a hungry baby actively sucks on the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin is distributed throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has had enough, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more.”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks to breastfeed very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, just when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own, and adult help is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“Nobody told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved and the body will be able to produce milk more efficiently so inflammation and leakage of milk will begin to subside.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11–13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” says Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding Beyond the First Month: What to Expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al. , Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
, Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation .Am J Clinl Nutr . 1988;48(6):1375-1386. at the beginning and at the peak of lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
- Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; Dec 2017 [ cited 2018 Feb ] - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas J Cancer Prev. 2014;15(12):4829-4837.
2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas J Cancer Prev. 2014;15(12):4829-4837.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch on to the nipple, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the love hormone, in you and your baby, and oxytocin plays a key role in the delivery of breast milk, colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this promotes the natural release of the placenta and reduces blood loss. 4
In the first hours after childbirth, this promotes the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a caesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding. ”
”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may take 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
7 Feeding may take 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- toss and turn in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so if in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the early days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does a newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.

- Colour: greenish black.
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. A doctor should also be consulted if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the feces, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, then he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
- Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its impact on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc. 2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology.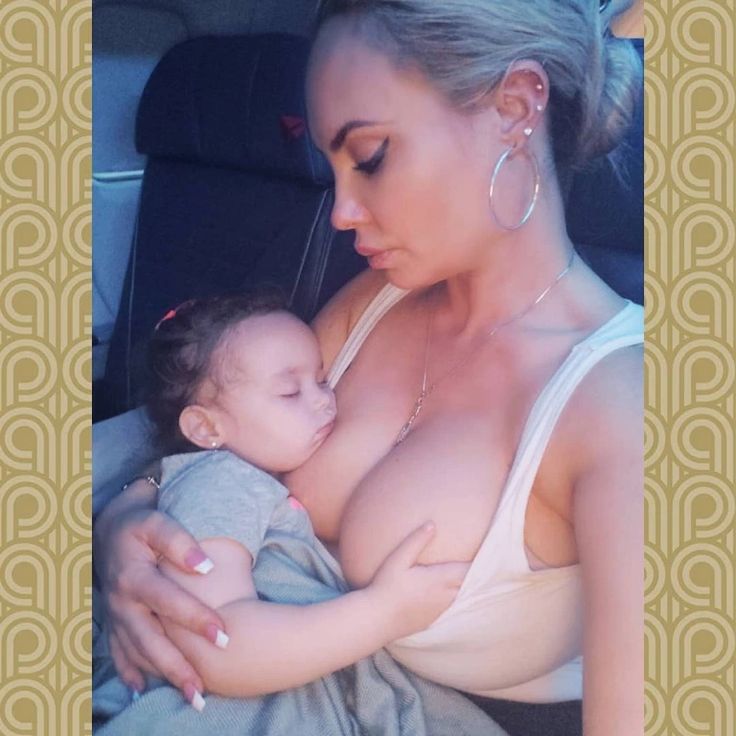 J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women s Health . 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production".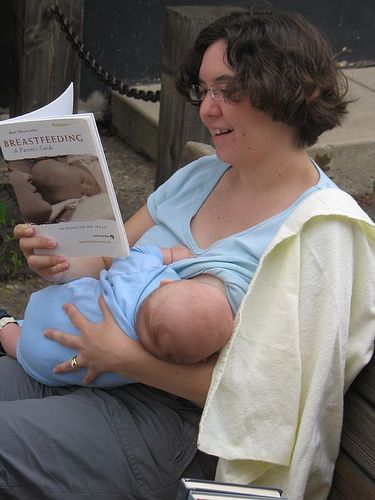 J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., Guidelines S -3 for the management of inflammatory breast disease during breastfeeding. Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession.![]()











