Breaking waters to induce labor
Inducing Labor (for Parents) - Nemours KidsHealth
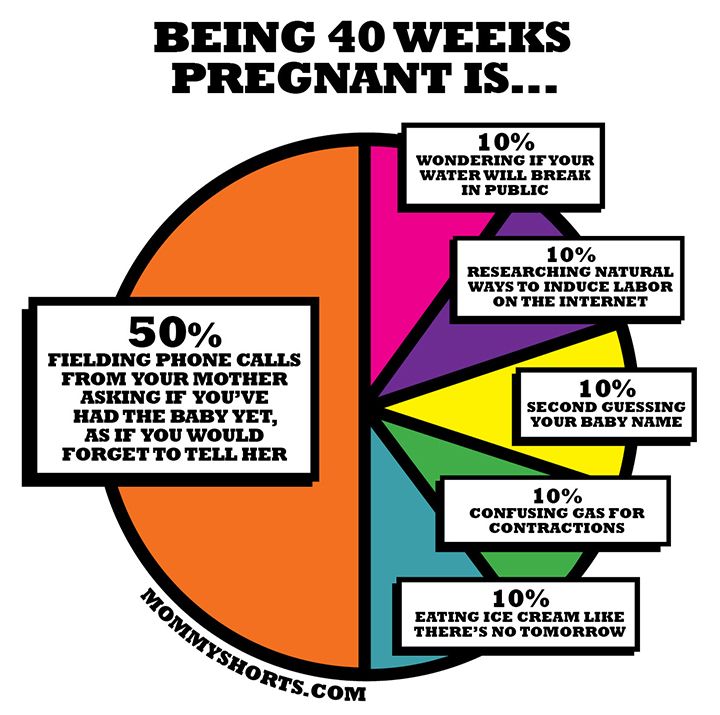
It's common for many pregnant women, especially first-time mothers, to watch their baby's due date come and go without so much as a contraction. The farther away from the expected delivery date (called the EDD) you get, the more anxious you might become. You may start to wonder — is this baby ever going to come?
Late pregnancy can be challenging — you may feel large all over, your feet and back might hurt, you might not have the energy to do much of anything, and you're beyond ready to meet the little one you've nurtured all this time. Which is why waiting a little longer than you'd expected can be particularly hard.
Still, being past your due date doesn't guarantee that your doctor (or other health care provider) will do anything to induce (or artificially start) labor — at least not right away.
What Is It?
Labor induction is what doctors use to try to help labor along using medications or other medical techniques. Years ago, some doctors routinely induced labor. But now it's not usually done unless there's a true medical need for it. Labor is usually allowed to take its natural course. However, in some situations, a health care provider may recommend induction.
Why It's Done
Your doctor might suggest an induction if:
- your water broke but you are not having contractions
- your baby still hasn't arrived by 2 weeks after the due date (when you're considered post-term — more than 42 weeks into your pregnancy)
- you have an infection in the uterus (called chorioamnionitis)
- you have certain risk factors (e.g., gestational diabetes or high blood pressure)
- there is not enough amniotic fluid
- there is a problem with the placenta
- the baby is not growing appropriately
Induction also can be appropriate under certain circumstances, as with a mother who is full term and has a history of rapid deliveries or lives far from a hospital.
Some mothers request elective inductions for convenience, but these do come with risks. Doctors try to avoid inducing labor early because the due date may be wrong and/or the woman's cervix might not be ready yet.
Page 2
How It's Done
Some methods of induction are less invasive and carry fewer risks than others. Ways that doctors may try to induce labor by getting contractions started include:
- Stripping the membranes. The doctor puts on a glove and inserts a finger into the vagina and through the cervix (the opening that connects the vagina to the uterus). He or she moves the finger back and forth to separate the thin membrane connecting the amniotic sac (which houses the baby and amniotic fluid) to the wall of the uterus. When the membranes are stripped, the body releases hormones called prostaglandins, which help prepare the cervix for delivery and may bring on contractions. This method works for some women, but not all.
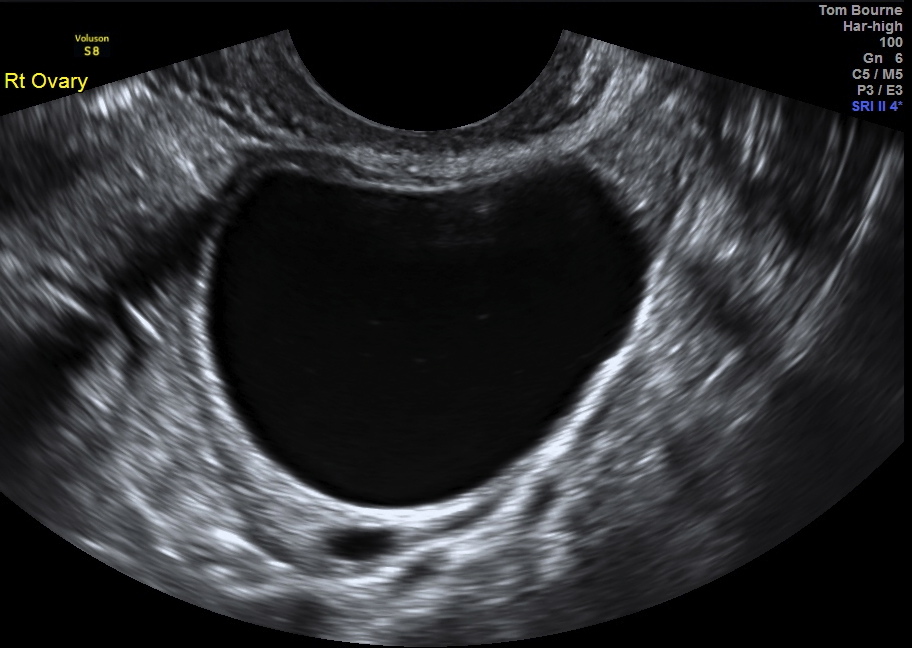
- Breaking your water (also called an amniotomy).
 The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours.
The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours. - Giving the hormone prostaglandin to help ripen the cervix. A gel or vaginal insert of prostaglandin is inserted into the vagina or a tablet is given by mouth. This is typically done overnight in the hospital to make the cervix "ripe" (soft, thinned out) for delivery. Administered alone, prostaglandin may induce labor or may be used before giving oxytocin.
- Giving the hormone oxytocin to stimulate contractions. Given continuously through an IV, the drug (Pitocin) is started in a small dose and then increased until labor is progressing well. After it's administered, the fetus and uterus need to be closely monitored. Oxytocin is also frequently used to spur labor that's going slowly or has stalled.
What Will It Feel Like?
Stripping the membranes can be a little painful or uncomfortable, although it usually only takes a minute or so.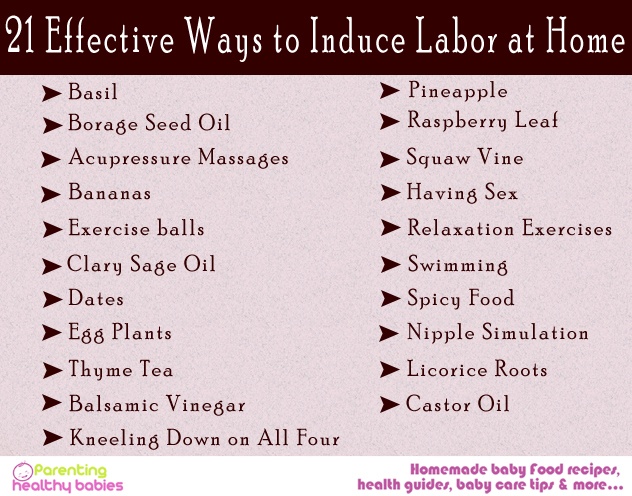 You may also have some intense cramps and spotting for the next day or two.
You may also have some intense cramps and spotting for the next day or two.
It can also be a little uncomfortable to have your water broken. You may feel a tug followed by a warm trickle or gush of fluid.
With prostaglandin, you might have some strong cramping as well. With oxytocin, contractions are usually more frequent and regular than in a labor that starts naturally.
Page 3
Risks and Precautions
Inducing labor is not like turning on a faucet. If the body isn't ready, an induction might fail and, after hours or days of trying, a woman may end up having a cesarean delivery (C-section). This appears to be more likely if the cervix is not yet ripe.
If the doctor ruptures the amniotic sac and labor doesn't begin, another method of inducing labor also might be necessary because there's a risk of infection to both mother and baby if the membranes are ruptured for a long time before the baby is born.
When prostaglandin or oxytocin is used, there is a risk of abnormal contractions developing. In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
Another potential risk of inducing labor is giving birth to a late pre-term baby (born after 34 and before 37 weeks). Why? Because the due date (EDD) may be wrong. Your due date is 40 weeks from the first day of your last menstrual period (LMP).
Babies born late pre-term are generally healthy but may have temporary problems such as jaundice, trouble feeding, problems with breathing, or difficulty maintaining body temperature. They may also be more likely than full term babies to have developmental or school problems later on.
Even though inductions do come with risks, going beyond 42 weeks of pregnancy can be risky, too. Many babies are born "post-term" without any complications, but concerns include:
Many babies are born "post-term" without any complications, but concerns include:
- A vaginal delivery may become harder as the baby gets bigger. As babies get bigger, the chance of an injury during delivery, such as a broken bone, increases.
- The placenta that helps to provide the baby with nourishment is deteriorating.
- The amniotic fluid can become low or contain meconium — the baby's first feces. If the baby breathes in meconium, it can cause breathing problems.
Old wives' tales abound about ways to induce labor, such as the use of castor oil. It is not safe to try to artificially start labor yourself by taking castor oil, which can lead to nausea, diarrhea, and dehydration. And herbs and herbal supplements meant to induce labor can be harmful. Breast stimulation can cause uterine contractions by causing the release of oxytocin. However, some studies have suggested that the baby might have abnormal heartbeats after breast stimulation. Some women feel that having sex in late pregnancy can induce labor, but there is no conclusion on this yet.
Talk to your doctor before doing anything to try to encourage your little one's arrival. Inducing labor is best left to medical professionals — you may cause more harm than good.
As frustrating as it can be waiting for your baby to finally decide to arrive, letting nature take its course is often best, unless your doctor tells you otherwise. Before you know it, you'll be too busy to remember your baby was ever late at all!
Stripping Membranes and Breaking Water for Labor Induction, Augmentation
Written by WebMD Editorial Contributors
In this Article
- What Is Labor Induction?
- Why Is Labor Induced?
- Reasons Not to Induce
- How Is Labor Induced?
- What Are the Risks of Inducing Labor?
- Can I Induce Labor Myself?
What Is Labor Induction?
If your doctor or midwife has concerns about your health or your baby's health toward the end of your pregnancy, they might suggest speeding up the process. This is called inducing labor, or induction. Instead of waiting for labor to start naturally, your doctor or midwife will use drugs or a procedure to start it sooner.
This is called inducing labor, or induction. Instead of waiting for labor to start naturally, your doctor or midwife will use drugs or a procedure to start it sooner.
Induction can be the right choice for some women, but it has risks. And it doesn’t always work. If it doesn’t, you may need another induction or a c-section. Most experts say it's best to let labor begin on its own and progress naturally unless there's a clear medical reason.
Why Is Labor Induced?
Induction is very common -- 1 out of 4 women in the U.S. starts labor with induction. Many times it's done for medical reasons, but it can be elective.
Why do some women need to have labor induced?
You’re 1-2 weeks past your due date. Studies show that inducing labor at 39 weeks doesn’t raise the risk for having a C-section or birth complications for the baby. After 41 weeks, you and your baby are at greater risk for complications.
 Being a little "late" isn’t a reason to induce. You also don’t want to be induced too early. Babies born before 39 weeks are more likely to have health problems, longer hospital stays, and time in neonatal intensive care.
Being a little "late" isn’t a reason to induce. You also don’t want to be induced too early. Babies born before 39 weeks are more likely to have health problems, longer hospital stays, and time in neonatal intensive care.Your water breaks but labor doesn’t start. Once your water breaks, you and your baby have a higher risk of infection. You might not need induction right away, though. Check with your doctor or midwife. Sometimes it's still safe to let labor begin on its own. After your water breaks, your doctor will limit the number of vaginal exams performed because of the potential for infection.
A problem puts you or your baby’s health at risk. Examples are infection (chorioamnionitis), too little amniotic fluid (oligohydramnios), and placental abruption. If you have conditions like diabetes, high blood pressure, preeclampsia, or eclampsia, your doctor or midwife might want to induce labor.

If your baby isn’t growing as it should be, or has an abnormal heart rate, your doctor or midwife might want to induce labor.
Some doctors recommend "elective" inductions for non-medical reasons. Maybe you live far from the hospital and your doctor worries that you won't get there in time. Or maybe your doctor asks you to accommodate their schedule. Experts say you should reconsider, though. Because induction poses some risks, experts say that women shouldn't be induced unless it's medically necessary.
Reasons Not to Induce
You doctor shouldn’t induce if:
You had C-section before that involved a classical incision or major surgery
The placenta is covering the cervix (placenta previa)
Your baby is in the wrong position (sideways or feet-first)
How Is Labor Induced?
There are a few ways a doctor or midwife can induce your labor, including:
Stripping the membranes.
 In this procedure, your doctor or midwife will use a gloved finger to gently separate the amniotic sac from the wall of the uterus at the cervix. This releases hormones that can trigger contractions. You can get it done in your doctor's or midwife's office. It can be uncomfortable. Afterward, you’ll probably go home to wait for contractions. You might have cramping and spotting.Studies disagree about how well membrane stripping works. Considering that and the discomfort it causes, talk over the pros and cons with your doctor or midwife beforehand.
In this procedure, your doctor or midwife will use a gloved finger to gently separate the amniotic sac from the wall of the uterus at the cervix. This releases hormones that can trigger contractions. You can get it done in your doctor's or midwife's office. It can be uncomfortable. Afterward, you’ll probably go home to wait for contractions. You might have cramping and spotting.Studies disagree about how well membrane stripping works. Considering that and the discomfort it causes, talk over the pros and cons with your doctor or midwife beforehand.Hormones. At the hospital, your doctor will give you hormones called prostaglandins to open the cervix and trigger contractions. If you’ve had a C-section in the past, your doctor won’t use this treatment, because it raises the risk of uterine rupture.
Mechanical dilation. Another way your doctor or midwife triggers labor is with a balloon catheter.
 At the hospital, your doctor inserts a thin tube through your vagina into your cervical opening. Then the doctor uses water to inflate the balloon at the end of the tube, causing your cervix to expand.
At the hospital, your doctor inserts a thin tube through your vagina into your cervical opening. Then the doctor uses water to inflate the balloon at the end of the tube, causing your cervix to expand.Medications. The medicine Pitocin (oxytocin) can start contractions. You get this at the hospital through an IV tube in your arm. Your doctor or midwife starts with a small dose and gradually increases it until your contractions are strong and frequent enough for your baby to be born.
Some women go into labor and deliver within a few hours after induction. Others take 1 or 2 days to start labor. If none of these methods starts your labor, and staying the course isn’t a good option, you'll most likely need a C-section, especially if your water has broken.
What Are the Risks of Inducing Labor?
Induction doesn’t work for everyone, and every pregnant mom’s body reacts differently to induction technique. Generally, inducing labor is safe, but there are risks:
Generally, inducing labor is safe, but there are risks:
Longer hospital stay. If you're induced, you may be in the hospital longer during labor and delivery. If you wind up needing a C-section after induction, your time in the hospital will be even longer.
Increased need for pain medicine. Inducing labor might cause contractions to come on stronger and more often than they would naturally. You're more likely to need an epidural or another medicine to manage the pain.
Increased risk of infection. Breaking the amniotic sac can lead to infection if you don't deliver within a day or two after induction.
Health problems for your baby. Women who are induced before the 39th week for medical reasons may deliver a baby who has problems with breathing.
 These babies have a higher risk of long-term developmental problems.
These babies have a higher risk of long-term developmental problems.Complications during delivery. Induction, especially with medications, might not be safe for women who’ve had a previous C-section or other surgery to the uterus. They have a higher risk of uterine rupture. Intense contractions also cause the placenta to detach from the wall of the uterus, called placental abruption. Both of these conditions are serious but rare, even with induction.
If your doctor or midwife recommends induction, ask questions. You want to be absolutely sure that it's the best decision for your health and your baby's health.
Can I Induce Labor Myself?
Tales abound of home remedies that supposedly bring on labor, but there is no scientific evidence to back them up. These methods include:
Having sex
Gently stimulating your nipples
Herbal remedies including blue or black cohosh (some herbs can be dangerous if you don’t use them properly)
Drinking small amounts of castor oil (Recent, well-controlled studies say it’s safe during late pregnancy but castor oil can have unpleasant side effects, like diarrhea.
 )
)Walking
Don’t try any of these methods without first talking to your doctor or midwife. Some can cause side effects or pose risks.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.

- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
What will help in childbirth - articles from the specialists of the clinic "Mother and Child"
Vovk Lyudmila Anatolyevna
Reproductologist, Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
We walk and dance
If earlier in the maternity hospital, with the onset of labor, a woman was put to bed, now obstetricians, on the contrary, recommend that the expectant mother move . For example, you can just walk: the rhythm of steps soothes, and gravity helps the neck to open faster. You need to walk as fast as it is convenient, without sprinting up the stairs, it’s better to just “cut circles” along the corridor or ward, from time to time (during the aggravation of the fight) resting on something. The gait does not matter - you can roll over like a duck, rotate your hips, walk with your legs wide apart. It is worth trying and dancing, even if you think that you do not know how. For example, you can swing your hips back and forth, describe circles and figure eights with your fifth point, sway in a knee-elbow position. The main thing is to move smoothly and slowly, without sudden movements.
The main thing is to move smoothly and slowly, without sudden movements.
Showering and bathing
For many people, water is a great way to relieve fatigue and tension, and it also helps with painful contractions. You can just stand in the shower, or you can lie down in the bath. Warm water will warm the muscles of the back and abdomen, they will relax, and the birth canal will relax - as a result, the pain may decrease. Well, if it does not decrease, then in any case, the water will relieve stress and at least for a while distract from the pain. So if there is a shower or jacuzzi bath in the delivery room, do not be shy and try this method of pain relief for contractions. The only thing is that the water should not be too hot, even if it seems that heat helps to better endure contractions.
Swinging on the ball
Until recently, fitball (rubber inflatable ball) in the rodblock was something outlandish, and today is found in many maternity hospitals. And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
And if you find a fitball in your rodblock, be sure to use it. You can sit on the ball astride and swing, rotate the pelvis, spring, roll from side to side. You can also kneel down, lean on the ball with your hands and chest and sway back and forth. All these movements on the ball will relax the muscles, increase the mobility of the pelvic bones, improve the opening of the neck, and reduce the pain of contractions. And while the woman is sitting on the ball, her partner (usually her husband) can massage her neck area for additional relaxation.
To be more comfortable, the ball should be soft, slightly deflated, and large, with a diameter of at least 75 cm.
We hang on a rope or wall bar
When the contractions become very strong and painful, you can take poses in which the stomach is in a “suspended” state. Some advanced maternity hospitals have wall bars and ropes attached to the ceiling for this. During contraction, you can hang on them, as a result, the weight of the uterus will put less pressure on large blood vessels, and this will improve uteroplacental blood flow. In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain.
In addition, in the “suspended” position, the load from the spine will be removed, which will also reduce pain.
Do not hang on a rope or a wall only if there is a desire to push, and the cervix has not yet opened and the efforts must be restrained.
Lying comfortably
If a woman in childbirth wants not to move, but, on the contrary, to lie down, then, of course, she can lie down. In modern maternity hospitals, instead of traditional ones, there are transforming beds: you can change their height, lower or raise the headboard or foot end, adjust the tilt level, push or push some part of the bed. There are also handrails in transforming beds (to use them to rest or even hang on them), and leg supports, and retractable pillows, and special backs - in general, everything in order to fit the bed under you and take it with it comfortable position. Moreover, this can be done without any physical effort - using the remote control.
We use everything we have
In any road block, even if it is minimally equipped, you can still find something useful. For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
For example, if during a fight you want to take a position with a support, you can lean forward and rest against something that turns up under your arm - a table, a headboard, a window sill. The main thing is that the support must be very stable. You can also get on all fours in the “cat pose” and focus on your hands, and to make it more convenient, put a pillow and a folded blanket under your chest. If you want to hang on something (and there is no rope or wall) and your husband will be nearby, you can use postures that allow you to transfer body weight to him: for example, hang on your husband’s neck. In general, it is worth showing imagination and adapting any item in the rodblock to your needs.
And don't be afraid to look stupid during childbirth. No one in the delivery room cares about how you move or lie down as long as it helps you get through your contractions, so calmly find your comfortable position.
Giving birth in an uncomfortable position is both difficult and inefficient.