Bleeding in 3rd trimester of pregnancy
Vaginal bleeding in late pregnancy: MedlinePlus Medical Encyclopedia
One out of 10 women will have vaginal bleeding during their 3rd trimester. At times, it may be a sign of a more serious problem. In the last few months of pregnancy, you should always report bleeding to your health care provider right away.
You should understand the difference between spotting and bleeding:
- Spotting is when you notice a few drops of blood every now and then on your underwear. It is not enough to cover a panty liner.
- Bleeding is a heavier flow of blood. With bleeding, you will need a liner or pad to keep the blood from soaking your clothes.
When labor begins, the cervix starts to open up more, or dilate. You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
Mid- or late-term bleeding may also be caused by:
- Having sex (most often just spotting)
- An internal exam by your provider (most often just spotting)
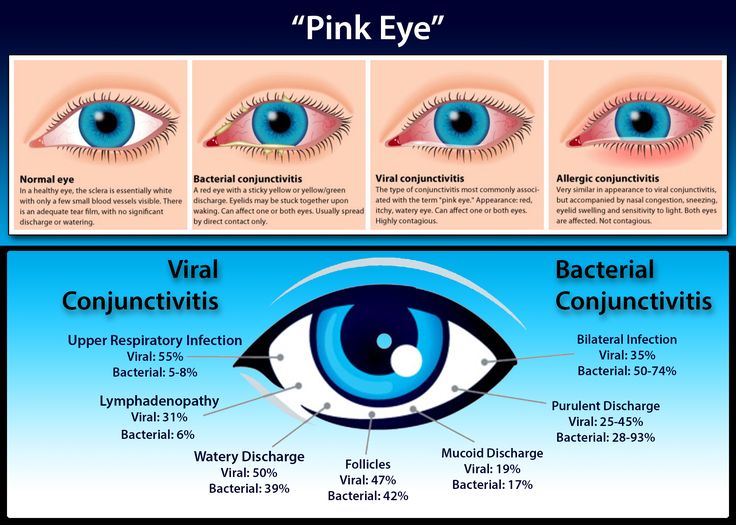
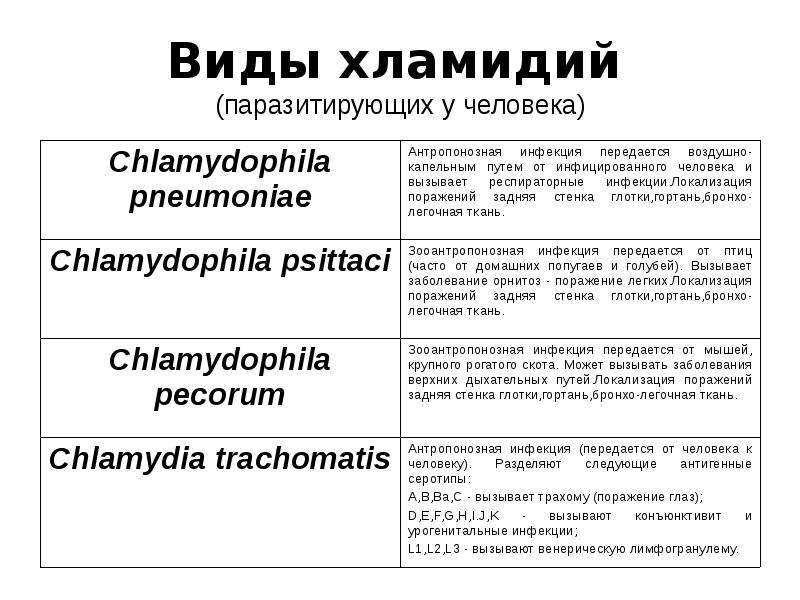
- Diseases or infections of the vagina or cervix
- Uterine fibroids or cervical growths or polyps
More serious causes of late-term bleeding may include:
- Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
- Placenta abruptio (abruption) occurs when the placenta separates from the inner wall of the uterus before the baby is born.
To find the cause of your vaginal bleeding, your provider may need to know:
- If you have cramping, pain, or contractions
- If you have had any other bleeding during this pregnancy
- When the bleeding began and whether it comes and goes or is constant
- How much bleeding is present, and whether it is spotting or a heavier flow
- The color of the blood (dark or bright red)
- If there is an odor to the blood
- If you have fainted, felt dizzy or nauseated, vomited, or had diarrhea or a fever
- If you have had recent injuries or falls
- When you last had sex and if you bled afterward
A small amount of spotting without any other symptoms that occurs after having sex or an exam by your provider can be watched at home. To do this:
- Put on a clean pad and recheck it every 30 to 60 minutes for a few hours.

- If spotting or bleeding continues, call your provider.
- If the bleeding is heavy, your belly feels stiff and painful, or you are having strong and frequent contractions, you may need to call 911 or your local emergency number.
For any other bleeding, call your provider right away.
- You will be told whether to go to the emergency room or to the labor and delivery area in your hospital.
- Your provider will also tell you whether you can drive yourself or you should call an ambulance.
Baeseman ZJ. Vaginal bleeding in pregnancy. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier 2021:1227-1229.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae.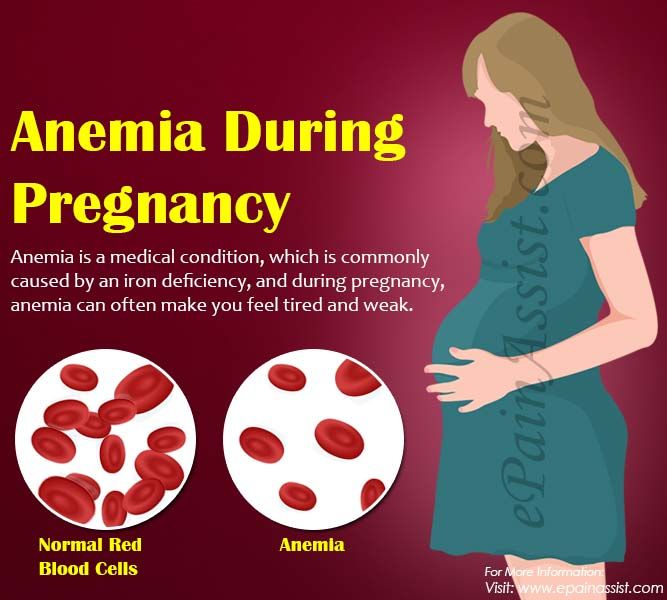 In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
Vaginal bleeding in late pregnancy Information | Mount Sinai
What Causes Bleeding Later in Pregnancy?
When labor begins, the cervix starts to open up more, or dilate.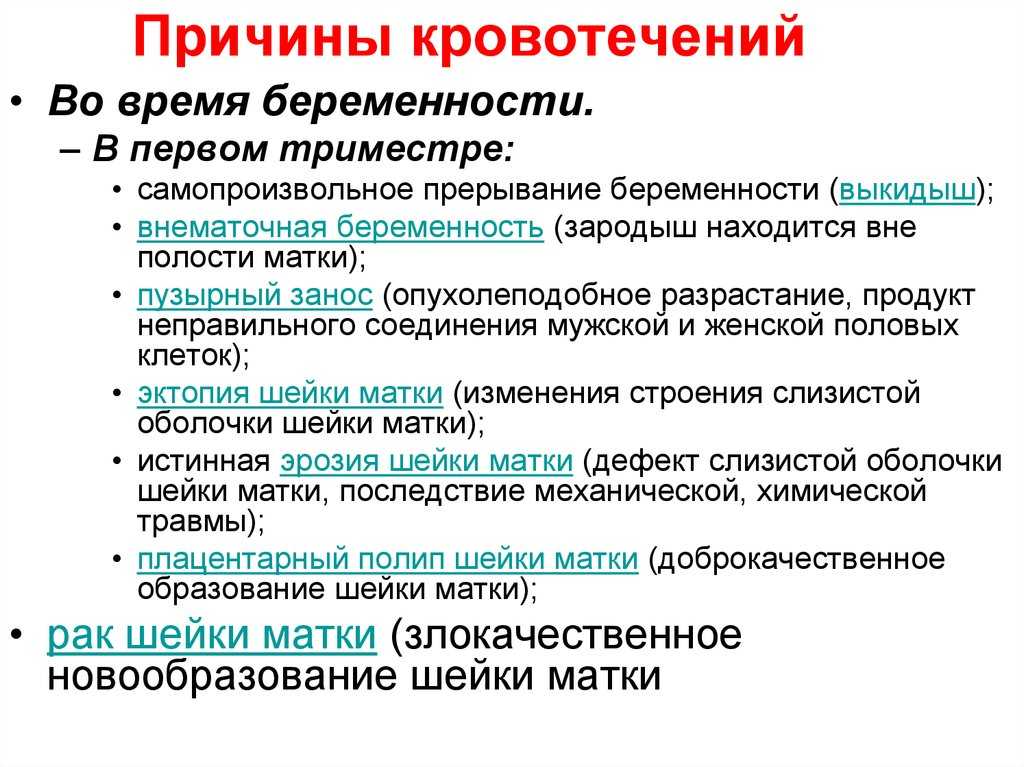 You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
Mid- or late-term bleeding may also be caused by:
- Having sex (most often just spotting)
- An internal exam by your provider (most often just spotting)
- Diseases or infections of the vagina or cervix
- Uterine fibroids or cervical growths or polyps
More serious causes of late-term bleeding may include:
- Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
- Placenta abruptio (abruption) occurs when the placenta separates from the inner wall of the uterus before the baby is born.
What to Tell Your Health Care Provider
To find the cause of your vaginal bleeding, your provider may need to know:
- If you have cramping, pain, or contractions
- If you have had any other bleeding during this pregnancy
- When the bleeding began and whether it comes and goes or is constant
- How much bleeding is present, and whether it is spotting or a heavier flow
- The color of the blood (dark or bright red)
- If there is an odor to the blood
- If you have fainted, felt dizzy or nauseated, vomited, or had diarrhea or a fever
- If you have had recent injuries or falls
- When you last had sex and if you bled afterward
What Should Happen Next?
A small amount of spotting without any other symptoms that occurs after having sex or an exam by your provider can be watched at home. To do this:
To do this:
- Put on a clean pad and recheck it every 30 to 60 minutes for a few hours.
- If spotting or bleeding continues, call your provider.
- If the bleeding is heavy, your belly feels stiff and painful, or you are having strong and frequent contractions, you may need to call 911 or your local emergency number.
For any other bleeding, call your provider right away.
- You will be told whether to go to the emergency room or to the labor and delivery area in your hospital.
- Your provider will also tell you whether you can drive yourself or you should call an ambulance.
Baeseman ZJ. Vaginal bleeding in pregnancy. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier 2021:1227-1229.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage.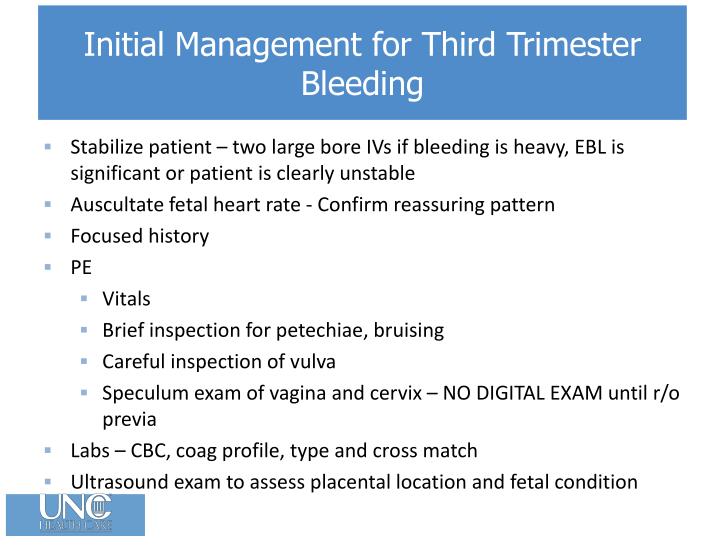 In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Last reviewed on: 10/5/2020
Reviewed by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A. D.A.M. Editorial team.
D.A.M. Editorial team.
Bleeding during pregnancy. What is Bleeding During Pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Bleeding during pregnancy is a sign that can occur regardless of the period of embryogenesis and indicates ongoing changes in the woman's body. It can be observed with spontaneous miscarriage, ectopic pregnancy, Rh conflict, placenta previa and other conditions. This manifestation can develop against the background of general well-being or be accompanied by painful sensations in the lower abdomen, lower back, and sacrum. Diagnosis of bleeding during pregnancy is carried out on the basis of data from a gynecological examination, an ultrasound assessment of the condition of the patient and the fetus. The treatment of this pathological symptom is determined by its cause and is prescribed exclusively by a specialist.
The treatment of this pathological symptom is determined by its cause and is prescribed exclusively by a specialist.
- Causes of bleeding during pregnancy
- Classification and symptoms of bleeding during pregnancy
- Diagnosis and treatment of bleeding during pregnancy
- Prognosis and prevention of bleeding during pregnancy
- Prices for treatment
General
Bleeding during pregnancy is an obstetric symptom, indicating the possible development of a number of disorders, the cause of which can be both physiological changes in the body of a woman after conception, and pathological conditions. Only an obstetrician-gynecologist can finally find out the etiology of such a manifestation after a complete examination. Bleeding during pregnancy occurs in about one in five patients. In 50%, they indicate pathological changes and end in spontaneous miscarriage. In half of the patients, the symptom is physiological in nature. Bleeding occurs more often in the first and third trimester of embryogenesis.
Bleeding occurs more often in the first and third trimester of embryogenesis.
The danger of bleeding during pregnancy lies in the fact that a variety of factors can provoke them, including those that pose a threat to the mother and fetus. In some situations, there are no other pathological signs. Any bleeding during pregnancy should be a reason for immediate medical attention. Only a specialist is able to assess the danger to the health of a woman and the fetus, as well as decide on further tactics. Timely assistance provided even with an abnormal course of pregnancy allows you to continue its management and save the life of the child.
Bleeding during pregnancy
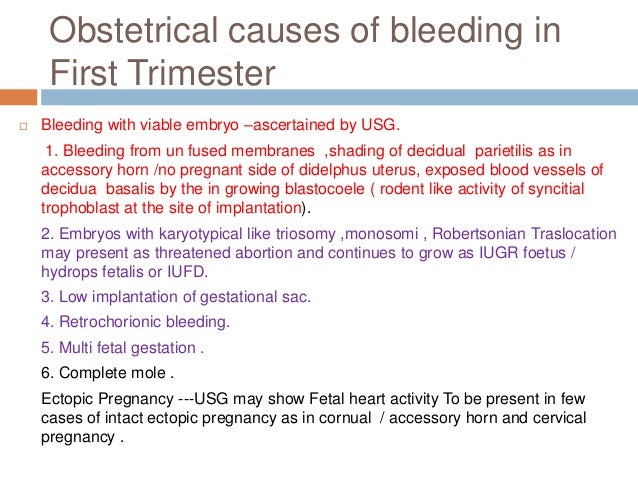
Causes of bleeding during pregnancy
Bleeding during pregnancy can occur at any time of embryogenesis, develops both against the background of physiological changes in the woman's body, and as a result of the formation of a certain obstetric pathology.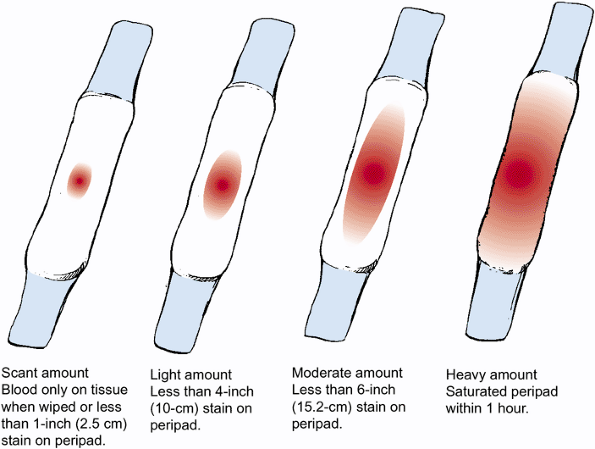 In the early stages, half of the women have a slight separation of blood due to the implantation of the fetal egg in the uterine cavity. Such bleeding during pregnancy is often regarded by the patient as menstrual, so she does not seek medical help, which in the future may make it difficult to determine the timing of embryogenesis. A similar symptom is possible with insufficient production of progesterone in the early stages of gestation.
In the early stages, half of the women have a slight separation of blood due to the implantation of the fetal egg in the uterine cavity. Such bleeding during pregnancy is often regarded by the patient as menstrual, so she does not seek medical help, which in the future may make it difficult to determine the timing of embryogenesis. A similar symptom is possible with insufficient production of progesterone in the early stages of gestation.
The most common cause of abnormal bleeding during pregnancy in the first trimester is spontaneous miscarriage. This symptom appears both with a just-started and with a complete abortion. Approximately 6 weeks after conception, the symptom occurs with an ectopic attachment of the fetal egg. Also, bleeding during pregnancy at this time may indicate an Rhesus conflict, fetal fading. Similar manifestations are characteristic of women suffering from varicose veins that feed the uterus. In this case, bleeding during pregnancy is due to increased blood supply to the tissues.
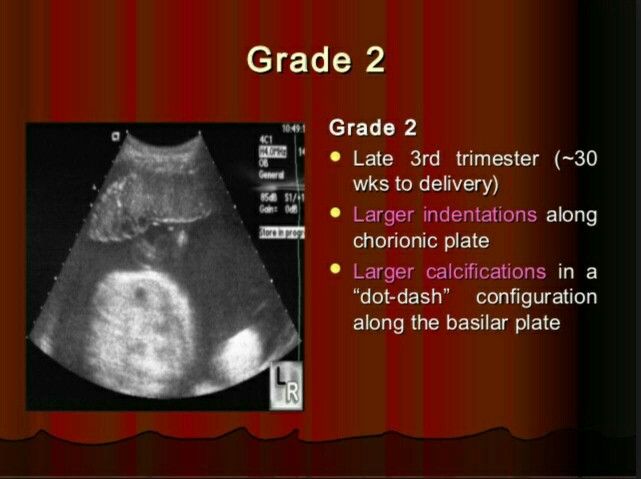
Bleeding during pregnancy in the second trimester is diagnosed much less frequently, in about 5-10% of all cases of gestation. As a rule, the symptom is caused by pathological changes and in most cases indicates spontaneous late abortion or isthmic-cervical insufficiency. Sometimes the separation of blood from the genital tract is observed during intrauterine death of the fetus. Bleeding during pregnancy in the third trimester also always speaks of the development of gestation pathology. The most common cause is placenta previa. In this case, the embryonic organ completely or partially covers the uterine os, while due to the high load on the lower segment, placental micro-ruptures occur, which causes a similar sign.
Less commonly, bleeding during pregnancy in the third trimester is due to premature detachment of a normally located placenta. In this situation, there is a high threat to the life of the fetus. The danger also lies in the fact that initially internal bleeding develops during pregnancy or the formation of a hematoma, and only then the blood flows out. The rarest, but most dangerous for the life of the mother and child, the cause of the development of this symptom is uterine rupture. Such a complication is diagnosed in the presence of a scar on the myometrium and tissue overstretching, provoked by polyhydramnios, large fetuses or multiple pregnancies. It is extremely rare that bleeding during pregnancy occurs due to a violation of the integrity of the membranes or umbilical cord vessels.
The rarest, but most dangerous for the life of the mother and child, the cause of the development of this symptom is uterine rupture. Such a complication is diagnosed in the presence of a scar on the myometrium and tissue overstretching, provoked by polyhydramnios, large fetuses or multiple pregnancies. It is extremely rare that bleeding during pregnancy occurs due to a violation of the integrity of the membranes or umbilical cord vessels.
Also, bleeding during pregnancy can be triggered by causes that appear at any stage of embryogenesis. Such reasons include benign neoplasms - fibroids, polyposis growths in the cervical canal and uterine cavity. Often bleeding during pregnancy occurs in women with cervical erosion. Sometimes a sign occurs due to increased blood circulation in the pelvic organs. The risk of developing a symptom is also present with violent sexual intercourse, significant physical exertion, concomitant cardiovascular diseases associated with a weakening of the endothelium.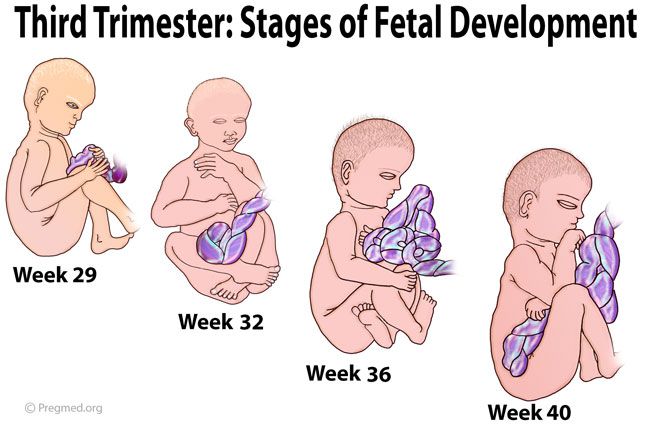
Classification and symptoms of bleeding during pregnancy
Depending on the origin of bleeding, two groups can be distinguished:
- Physiological bleeding during pregnancy - occurs due to the restructuring of the body, does not pose a threat to the health and life of the fetus or mother.
- Pathological bleeding during pregnancy - indicate its abnormal course, may be accompanied by a risk to the life and health of the woman and baby, require immediate medical attention.
The clinic of bleeding during pregnancy directly depends on the cause of this symptom. Isolation of blood from the genital tract in the early stages of embryogenesis, provoked by physiological changes, proceeds against the background of general well-being. Bleeding during pregnancy, which has developed due to the presence of polyps, erosion, fibroids in most cases also does not cause disturbances in well-being. In this case, there is a slight release of biological fluid - just a few drops, the symptom is of a short-term nature. More abundant, similar to menstrual, will be bleeding during pregnancy associated with a deficiency of progesterone.
More abundant, similar to menstrual, will be bleeding during pregnancy associated with a deficiency of progesterone.
In the case of bleeding during pregnancy associated with its spontaneous interruption, the patient is worried about constant or cramping pain in the lumbosacral region, abdomen. Additionally, nausea, dizziness, malaise, and a slight increase in body temperature may occur. Bleeding during pregnancy in this case can be of varying intensity, often in the discharge there are pieces of tissue. With an ectopic attachment of the fetal egg, as well as with a rupture of the uterus, a serious threat to the life of a woman arises. In such a situation, internal bleeding initially develops during pregnancy, and only then do pathological discharges from the external genital tract appear. There is acute pain in the abdomen with irradiation to the anal region, the lateral parts of the body. With significant blood loss, a state of shock occurs with a threat of death.
Bleeding during pregnancy in the later stages is also not always accompanied by a detailed clinical picture. In the case of placenta previa, this is the only symptom that should cause alertness in a woman and become a reason for contacting an obstetrician-gynecologist. As for the premature detachment of a correctly attached placenta, in this case, bleeding during pregnancy develops against the background of uterine hypertonicity, there is pain in the abdomen, deterioration in general well-being. During cardiac monitoring of the fetus, there is a violation of the heart rate, motor activity.
Diagnosis and treatment of bleeding during pregnancy
To identify the cause of bleeding during pregnancy, a gynecological examination of a woman is performed. With changes in physiological origin, no deviations from the norm can be detected. With pathological bleeding during pregnancy against the background of spontaneous abortion, an opening of the cervix is observed.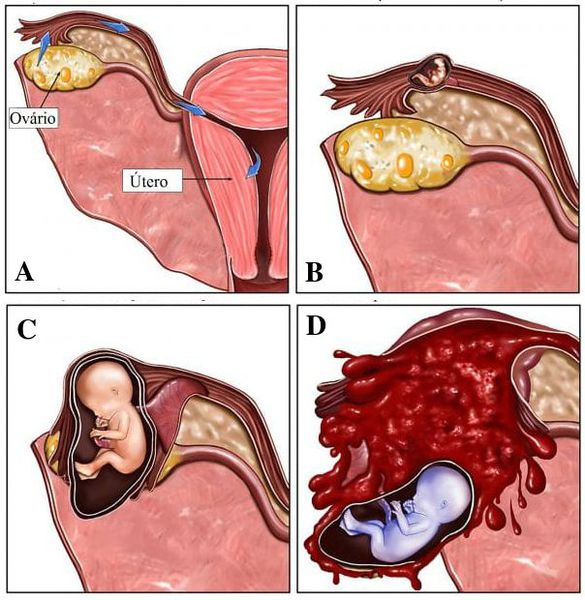 An increase in the tone of the myometrium may indicate the onset of placental abruption. Of the laboratory diagnostic methods, an analysis is used to determine the concentration of hCG (human chorionic gonadotropin). With ectopic pregnancy and bleeding, this figure will be reduced. Instrumental diagnosis of bleeding during pregnancy is to conduct an ultrasound scan. Using this method, it is possible to assess the state of the myometrium and the embryo, the level of blood flow in the vessels, the exact localization of the placenta and (possibly) its incipient detachment. Using CTG, the diagnostician can make a conclusion about the vital activity of the fetus.
An increase in the tone of the myometrium may indicate the onset of placental abruption. Of the laboratory diagnostic methods, an analysis is used to determine the concentration of hCG (human chorionic gonadotropin). With ectopic pregnancy and bleeding, this figure will be reduced. Instrumental diagnosis of bleeding during pregnancy is to conduct an ultrasound scan. Using this method, it is possible to assess the state of the myometrium and the embryo, the level of blood flow in the vessels, the exact localization of the placenta and (possibly) its incipient detachment. Using CTG, the diagnostician can make a conclusion about the vital activity of the fetus.
Treatment of bleeding during pregnancy also depends on the cause of the symptom. If there are no pathological changes or the manifestation is provoked by damage to the polyp, medical attention is not required. In rare cases, the doctor recommends its removal. Expectant tactics are also used in case of cervical erosion. Her cauterization is carried out after childbirth. Bleeding during pregnancy against the background of the threat of miscarriage and placenta previa requires immediate hospitalization in an obstetric hospital, followed by the appointment of drug treatment. To reduce uterine tone, sedatives, tocolytics are used. Pregnancy management in this case requires careful monitoring by a specialist.
Her cauterization is carried out after childbirth. Bleeding during pregnancy against the background of the threat of miscarriage and placenta previa requires immediate hospitalization in an obstetric hospital, followed by the appointment of drug treatment. To reduce uterine tone, sedatives, tocolytics are used. Pregnancy management in this case requires careful monitoring by a specialist.
Bleeding during pregnancy caused by ectopic attachment of the ovum, scar rupture, or completed spontaneous abortion requires hospitalization and surgical treatment. After removal of the remnants of fetal tissues or emergency delivery, antibiotic therapy is prescribed. In this case, stopping bleeding during pregnancy is carried out in different ways, depending on its intensity, often ligation of the uterine arteries is performed. With premature detachment of the placenta, an emergency caesarean section is indicated.
Prognosis and prevention of bleeding during pregnancy
Bleeding during pregnancy is usually accompanied by a favorable prognosis.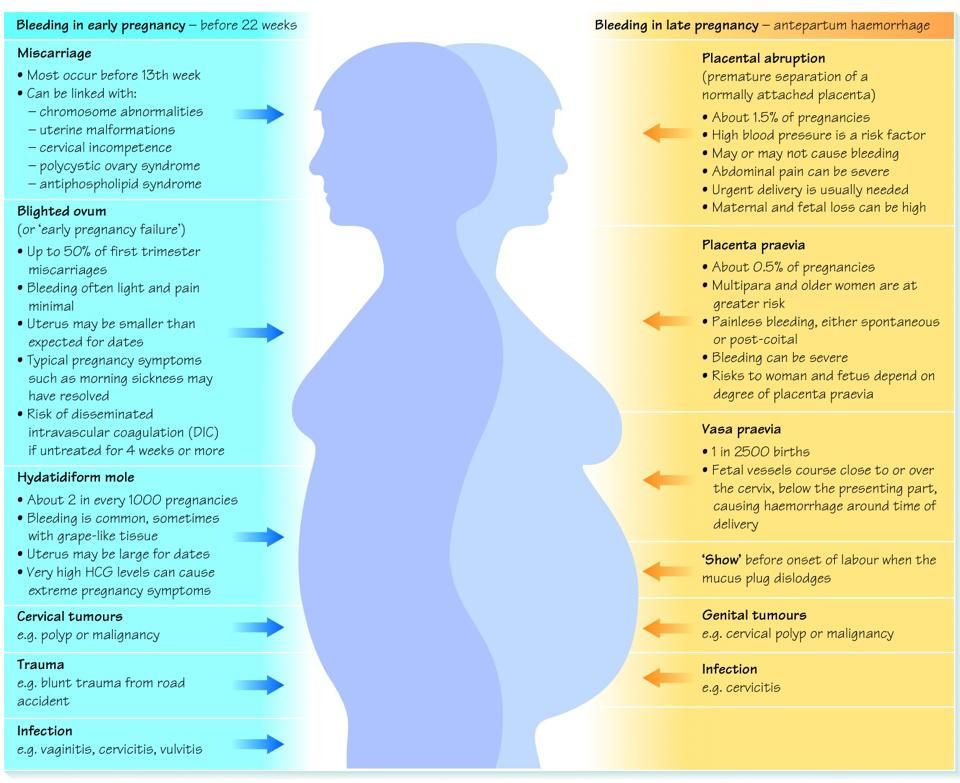 Timely medical care can save the life of the fetus and the woman. Lethal outcome is extremely rare. Prevention of bleeding during pregnancy consists in the early detection of benign neoplasms and their treatment even before conception. To prevent the development of a pathological symptom, you should register as soon as possible, take all the necessary tests, and if any violations occur, immediately seek advice from an obstetrician-gynecologist. Prevention of bleeding during pregnancy also consists in avoiding stress, physical exertion, violent sexual contacts.
Timely medical care can save the life of the fetus and the woman. Lethal outcome is extremely rare. Prevention of bleeding during pregnancy consists in the early detection of benign neoplasms and their treatment even before conception. To prevent the development of a pathological symptom, you should register as soon as possible, take all the necessary tests, and if any violations occur, immediately seek advice from an obstetrician-gynecologist. Prevention of bleeding during pregnancy also consists in avoiding stress, physical exertion, violent sexual contacts.
You can share your medical history, what helped you in the treatment of bleeding during pregnancy.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Medical advice for doctors | Remedium.ru
02/03/2023
How to avoid cracked teeth?
Permanent teeth are given to a person once and for life, however, the load on them can be excessive, which sometimes entails a wide variety of negative consequences.
 Tooth enamel is the hardest material in the body, when it is destroyed, the tooth most likely cannot be restored. Therefore...
Tooth enamel is the hardest material in the body, when it is destroyed, the tooth most likely cannot be restored. Therefore... More
02/03/2023
Results of correction of venous outflow disorders in patients with varicose veins and concomitant gonarthrosis
E.A. Shcheglov 1.2 , N.N. Alontseva 2 ; 1 PetrGU, 2 BSMP (Petrozavodsk)
Introduction. Chronic vein diseases in general and varicose veins in particular are a serious medical and social problem.
Purpose - to study the effect of treatment of venous outflow disorders on the results of treatment...
More
02/01/2023
Cognitive disorders in patients with cerebrovascular diseases in therapeutic practice: diagnostic and management algorithms
V.
 N. Shishkova ; National Medical Research Center for Internal Medicine and Preventive Medicine
N. Shishkova ; National Medical Research Center for Internal Medicine and Preventive Medicine
This review summarizes the main current data on the pathogenesis of cognitive impairment in patients with cardiovascular disease ...
More
01/30/2023
Second line drug therapy for biliary cancer
I.V. Savchenko 1.2 * , V.V. Breder 1 , I.S. Stilidi 1.2 , K.K. Laktionov 1.2 , N.E. Kudashkin 1.2 , A.V. Egorova 2 , S.V. Chulkova 1.2 ; 1 N.N. Blokhin, 2 Russian National Research Medical University named after ...
More
01/27/2023
Sinus lift in dentistry and its importance in dental implantation
The incompleteness of the dentition is not only an aesthetic problem, but also quite a medical one, entailing a rather large number of consequences.
 To make up for losses, modern dentistry has a huge arsenal of a wide variety of tools. However, the same dental implants must be placed...
To make up for losses, modern dentistry has a huge arsenal of a wide variety of tools. However, the same dental implants must be placed... More
01/26/2023
COVID-19-associated phlebopathy as an actual problem of modern phlebology
V.Yu. Bogachev 1.2 , B.V. Boldin 1 , P.Yu. Turkin 1.2 , O.V. Jenina 2 ; 1 Russian National Research Medical University named after N.I. Pirogova, 2 First phlebological center
Introduction . SARS-CoV-2 is accompanied by the development of dysfunction of the venous endothelium,...
More
01/24/2023
Treatment of metastatic bladder cancer: historical and modern aspects
A.
 A. Rumyantsev; National Medical Research Center of Oncology. N.N. Blokhin
A. Rumyantsev; National Medical Research Center of Oncology. N.N. Blokhin The standard of modern therapy for metastatic urothelial cancer (cancer of the bladder or other parts of the urinary tract) is systemic platinum-containing chemotherapy, however, despite the high immediate effectiveness of therapy (up to ...
More
01/20/2023
Atypical depression: frequency of occurrence of symptoms
P.V. Nikolaeva 1 , Yu.S. Fofanova 2 , I.A. Nikiforov 2 , P.V. Aronov 2 , G.N. Belskaya 3 ; 1 MGMSU im. A.I. Evdokimova, 2 Academy of Postgraduate Education FGBU FSCC FMBA of Russia, 3 NTsN
Introduction. Currently, there is a tendency towards an increase in the incidence of atypical forms of depression, which is especially .
 ..
.. More
01/18/2023
Therapy for BRCA-associated metastatic breast cancer. Efficacy and safety of talazoparib in real clinical practice
E.V. Lubennikova 1 *, A.L. Kornietskaya 2 , N.S. Dorofeeva 3 , E.I. Rossokha 4 , E.V. Markarova 5 , I.V. Yudina 6 , I.Ya. Bazaeva 1 , L.V. Bolotina 2 , T.I. Deshkina 2 , Ya.A. Zhulikov 1 , E.V. Stasenko 6 , T.V. Ustinova 2 , A.S. Tsareva 1 , E.V. Artamonova 1.5.7 ; ...
More
01/16/2023
Successful pregnancy with primary infertility as a result of simultaneous bariatric intervention and laparoscopic oophorectomy in a woman with large cystic ovarian teratoma and morbid obesity
V.