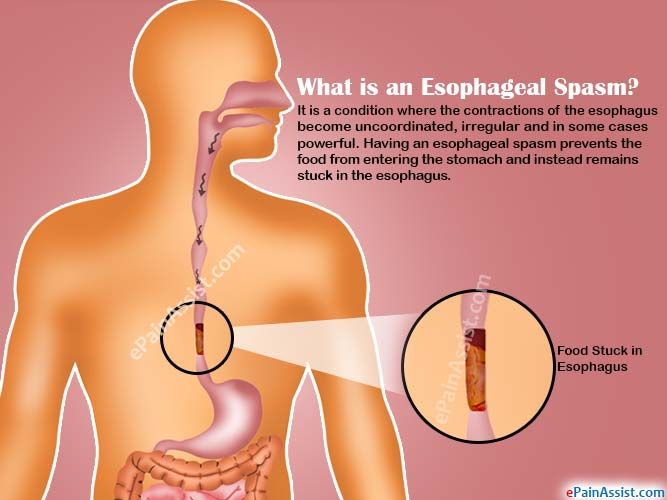
Can i use allergy eye drops while pregnant
What’s safe—and not so safe—to use in your pregnant patients
Cover Feature: Allergy
March 2007
by Vanessa Caceres
EyeWorld Contributing Editor
Ophthalmologists must navigate through uncharted areas when they treat their pregnant patients.
Soft contact lens-related corneal infiltrate in a 38-year-old woman. Infiltrates such as this one may require extra care in a pregnant patient.Source: Christopher J. Rapuano, M.D.
“My general rule of thumb in patients who are pregnant is to use the least amount of medication possible, even if I think the medications are safe,” said Christopher J. Rapuano, M.D., professor of ophthalmology, Jefferson Medical College of Thomas Jefferson University, and co-director, Cornea Service, Wills Eye Institute, Philadelphia.
“My second rule of thumb is to call the obstetrician and check with him on medications I think the patient needs to be on,” Dr. Rapuano said.
Practitioners said they would prefer to avoid the medicolegal risks that would accompany a child born with defects or other problems, which might cause a patient to wonder if the ophthalmic medication she used during pregnancy led to the child’s problem.
Practitioners generally follow the same guidelines while the patient is nursing, although they said they do not need to adhere as strictly to them. Although there is a dearth of research on the effects of ophthalmic medications during pregnancy, physicians take a cautious approach instead of waiting for such studies to be done.
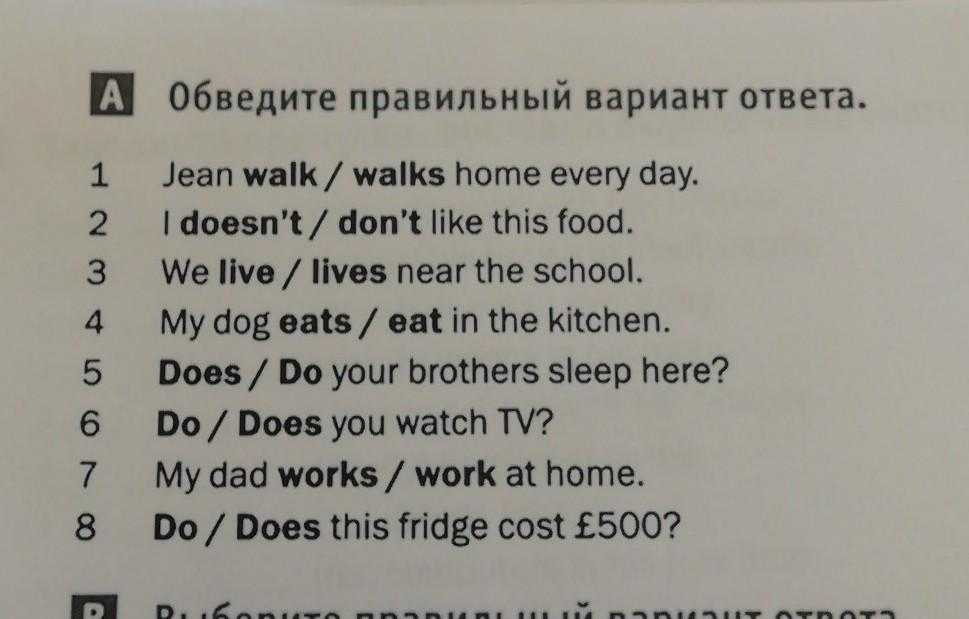
Food and Drug Administration medication safety categories
A. Safety established using human studies
B. Presumed safety based on animal studies
C. Uncertain safety; no human studies; animal studies show adverse effect
D. Unsafe; evidence of risk that in certain clinical circumstances may be justifiable
X. Highly unsafe
Source: Douglas J. Rhee, MD; Food and Drug Administration
“These studies are hard to do, and they’re risky,” Dr. Rapuano said. “An animal study may or may not translate perfectly to humans. And these studies are not cost effective” because pregnant patients make up such a small portion of the population.
Below are some treatment approaches that ophthalmologists use with their pregnant patients who wear contacts or have dry eye, allergies, glaucoma, corneal infections, and other conditions.
Contacts and refractive surgery
Corneal thickness, curvature, and sensitivity as well as tear composition can all change during pregnancy, said Elizabeth A. Davis, M.D., Bloomington, Minn., who co-authored a chapter on pregnancy and the eye for the book Principles and Practices of Ophthalmology. For this reason, pregnant patients who wear contact lenses may find their contacts do not always fit properly, she said, or their contacts may feel greasier because of an increased level of lysozyme in the tear film, she said.
If these patients want to opt for refractive surgery because their contacts are uncomfortable, they have to think again, Dr. Davis said.
“We don’t do refractive surgery in pregnant women,” she said. “We recommend patients wait three months after giving birth and/or breastfeeding because of all sorts of hormonal changes that can change the refractive error. ” Between the changes in refractive error that pregnancy can cause—which could lead surgeons to treat an inaccurate refractive error—and the unknown risks of any medications patients may take in conjunction with refractive surgery, waiting is a safer option, Dr. Davis said.
” Between the changes in refractive error that pregnancy can cause—which could lead surgeons to treat an inaccurate refractive error—and the unknown risks of any medications patients may take in conjunction with refractive surgery, waiting is a safer option, Dr. Davis said.
Dry eye and allergies
Dry eye can be an issue in pregnant patients who wear contact lenses and in those who experience nausea and vomiting, said John D. Sheppard, M.D., professor of ophthalmology, microbiology, and immunology, Eastern Virginia Medical School, Norfolk. The nausea and vomiting lead to dehydration, which can lead to drier eyes, he said. Certain medications that patients may take to inhibit nausea can also contribute to dry eye, he said. Practitioners seem to agree that artificial tear drops are a safe treatment option to lubricate the eyes. Another easy solution is asking patients to reduce contact lens wear or not wear them at all.
Beyond those easier steps, everyone has different ideas.
Dr. Sheppard said he “leans more toward the natural route” to treat pregnant dry-eye patients. This includes supplements such as fish oil, flaxseed oil, and black currant seed oil. Preliminary research and anecdotal evidence shows that omega-3 acids found in these supplements can help the ocular surface.
He uses silicone or plastic punctal plugs as well, an option that Dr. Davis also thinks is reasonable. “Punctal plugs and lubricant drops would be the mainstay of my treatment,” she said.
Restasis (cyclosporine ophthalmic emulsion 0.05%, Allergan, Irvine, Calif.), which is frequently used now to treat dry eye, may or may not be a good option for pregnant patients, physicians said.
“The use of Restasis is not contraindicated,” Dr. Sheppard said. “I have no problems treating pregnant patients with Restasis.” He said Restasis has an added benefit: helping to control ocular allergies.
However, “I’d take the patient off the Restasis, not because I think it’s unsafe but because it is cyclosporine and as far as I know, it’s not been tested [with pregnant women],” Dr. Rapuano said.
Rapuano said.
If the patient has severe dry eye, Dr. Sheppard is also comfortable using Lotemax (loteprednol etabonate ophthalmic suspension 0.5%, Bausch & Lomb, Rochester, N.Y.).
With seasonal allergies, Dr. Sheppard will use Restasis and drops such as Elestat (epinastine hydrocholoride 0.05%, Inspire Pharmaceuticals, Durham, N.C.) and Patanol (olopatadine hydrocholoride 0.1%, Alcon, Fort Worth, Texas). Still, he avoids oral antihistamines or antihistamines with a decongestant component. “With the systemic effects, we’re not 100 percent sure they’re safe for the fetus,” he said.
Patients who wear contact lenses and have seasonal allergies may find their symptoms more manageable if they avoid their contacts for awhile, Dr. Sheppard said.
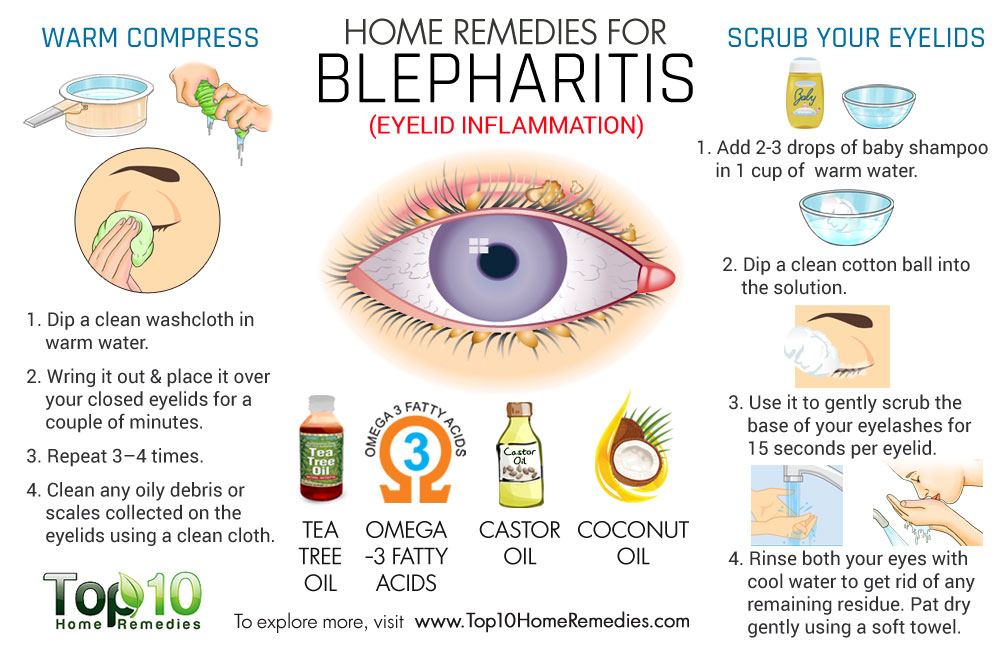
Using the lowest amount of drops necessary and encouraging patients with allergies to use cool compresses are other possible approaches, Dr. Davis said. “If they’re miserable, I say it’s OK” to use drops for ocular allergies, Dr. Rapuano said. Still, he tries to keep their use to a minimum during pregnancy.
Rapuano said. Still, he tries to keep their use to a minimum during pregnancy.
Dr. Rapuano also teaches his patients to perform digital punctal occlusion before they administer a drop and at least 60 seconds after they put a drop in.
“This significantly decreases the amount of the drop that gets into the nose and the bloodstream,” he said. “It keeps the medication more localized.”
Unusual situations
Dr. Rapuano said dilating drops are safe to occasionally use if it’s an urgent situation—a patient experiencing flashers and floaters, for example. If it is a routine examination, he advises the patient to wait until she has had the baby.
Even though practitioners generally prefer to avoid medications for pregnant patients, a corneal infection requires treatment, Dr. Davis said.
There are certain drops that are safer,” she said. “Erythromycin and polymixin B appear to be the safest antibiotics,” she said. “They’re not as broad spectrum as the fourth-generation fluoroquinolones, but I’d start with those and see if they’ll treat the problem. ”
”
A corneal infection is another good situation in which to consult the obstetrician about the treatment plan, Dr. Sheppard said.
Low-dose steroid drops are usually safe during pregnancy in patients such as those who’ve had a corneal transplant and are on anti-rejection steroids, Dr. Rapuano said. However, he said he generally stops the use of antiviral medications such as Valtrex (valacylovir, GlaxoSmithKline, United Kingdom) in patients with herpes.
EyeWorld factoid:
Allergies have a genetic component. If only one parent has allergies of any type, changes are 1 in 3 that each child will have an allergy. If both parents have allergies, it is much more likely (7 in 10) that their children will have allergies.
Source: Asthma and Allergy Foundation of America
Glaucoma medication risks
For glaucoma patients, one positive aspect is that IOP tends to decrease naturally during pregnancy, said Douglas J. Rhee, M.D., assistant professor of ophthalmology, Department of Ophthalmology, Glaucoma Section, Massachusetts Eye & Ear Infirmary, Boston.
Rhee, M.D., assistant professor of ophthalmology, Department of Ophthalmology, Glaucoma Section, Massachusetts Eye & Ear Infirmary, Boston.
He cites previous studies that have been done in this area. He also did some research regarding pregnancy and the eye for the Ophthalmic Drug Guide, a book he co-authored that was published this year. Beyond the IOP advantage, he said that glaucoma specialists are especially cautious in their treatment of pregnant patients because of the unknown effects of glaucoma medications.
“All glaucoma medications have the potential to cause fetal and embryonic harm,” he said. “It’s not a well-studied area.” In fact, most glaucoma medications are classified in category C of the Food and Drug Administration’s safety categories; this means the drugs have an uncertain safety profile, there have been no human studies, and animal studies may show an adverse effect.
Two exceptions to the risks from glaucoma medications: brimonidine is category B and reasonable to offer up to one month before delivery and oral acetazolaminde was reported safe in a case series for the treatment of intracranial hypertension, published in 2005 in the American Journal of Ophthalmology. Still, the series only involved 100 patients, Dr. Rhee said. Plus, “acetazolamide during late pregnancy has been associated with renal tubular acidosis in the newborn and may have potential teratogenic effects if administered during the first 12 weeks of fetal development,” Dr. Rhee said, citing a 2001 study from Survey of Ophthalmology.
Still, the series only involved 100 patients, Dr. Rhee said. Plus, “acetazolamide during late pregnancy has been associated with renal tubular acidosis in the newborn and may have potential teratogenic effects if administered during the first 12 weeks of fetal development,” Dr. Rhee said, citing a 2001 study from Survey of Ophthalmology.
Amtimetabolites such as 5-fluorouracil (5-FU) and mitomycin C and prostaglandin analogues are medications to definitely avoid during pregnancy, he said.
The best approach is avoidance of glaucoma medications during this period, he said.
“You see what happens to pressure when you take them off the medications, monitor the pressure, and see if the optic nerve can tolerate it,” Dr. Rhee said.
Selective or argon laser trabeculoplasty are potential surgical solutions for pregnant patients, he said. If those are not successful, some investigators have suggested cylcophotocoagulation as a good option, Dr. Rhee said. Trabeculectomy without anti-metabolites or post-op anti-inflammatory medication is another procedure to try. Still, the surgical methods have a lower success rate because of the young age of the patients.
Still, the surgical methods have a lower success rate because of the young age of the patients.
“It’s a notoriously difficult area,” he said. By the time the patient has delivered the baby and is nursing, glaucoma practitioners can once again consider how much the patient needs her medications. A switch to bottle feeding for the newborn may be the best option so the patient can resume their medicine, Dr. Rhee said.
Editors’ note
Dr. Rapuano lectures for Alcon (Fort Worth, Texas) and Allergan (Irvine, Calif.). Drs. Davis and Rhee have no financial interests related to their comments. Dr. Sheppard is a consultant for Alcon, Allergan, Bausch & Lomb (Rochester, N.Y.), and various other companies.
Contact Information
Davis: 952-888-5800, [email protected]
Rapuano: 215-928-3180, [email protected]
Rhee: 617-573-3670, [email protected]
Sheppard: 757-622-2220, docshep@hotmail. com
com
What Eye Drops Are Safe to Use During Pregnancy?
When you’re pregnant, you need to check that any type of medication you use is safe for both you and your unborn baby – including topical medication, such as eye drops.
Now you might not necessarily think of eye drops as being medication. Lots of people who wear contact lenses get dry eyes and use eye drops to relieve irritation. Or you might use eye drops to alleviate the symptoms of allergies, tired eyes or even the effects of other medications that you’re taking.
But the fact of the matter is that eye drops, or artificial tears as they are sometimes known, do count as a form of topical treatment. You should always take medical advice before starting any kind of medication, but this is especially true if you’re pregnant or breastfeeding.
This is because the medication that you take can pass to your baby via your bloodstream or milk, even those that are topical. Not all types of medication are unsafe, but some will be harmful to your baby. This is particularly true during the first trimester of pregnancy when an unborn baby is in the early stages of development.
This is particularly true during the first trimester of pregnancy when an unborn baby is in the early stages of development.
So how about those eye drops in your medicine cabinet. Are they OK to use? And if not, what eye drops are safe during pregnancy?
It’s difficult to provide a comprehensive list of the eye drops that are safe to use during pregnancy. Not many scientific studies have been carried out on humans due to the risks involved. Studies have been carried out on animals, but the results may not necessarily apply to human beings.
It is known that certain eye drops are not advised. This includes glaucoma eye drops such as Brinzolamide, Xalatan, Xalacom, Lumigan and Travatan. But others, like Miotics, haven’t been shown to have any adverse effects when taken during pregnancy.
Therefore because of the uncertainty involved, the best advice is not to use any eye drops until you’ve consulted a medical practitioner, such as an eye doctor, family doctor or pharmacist.
You’ll be advised of any risks involved, and whether these risks outweigh the benefits. If the eye drops are confirmed as being safe, you can rest assured that it’s OK to use them.
If you need to change the type of eye drops that you’re taking, you’ll need to consult with a medical practitioner once again. Different eye drops have different chemical make-ups. This means that some may contain ingredients that have potentially damaging effects, while others will be perfectly safe.
Relieving uncomfortable eyes during pregnancyNow if you’re suffering from excruciatingly itchy eyes and you’re pregnant, this might not be the answer you want to hear. Understandably you’ll just want something that makes that itch stop, and fast!
Itchy eyes are common amongst pregnant women and are caused by the fluctuation in hormone levels. This particular problem is caused by a decrease in the hormone that lubricates the eyes and produces tears.
Pregnancy can also exacerbate any allergies that you have. So if you usually have mild hay fever, the symptoms may get a whole lot worse while you’re pregnant.
So if you usually have mild hay fever, the symptoms may get a whole lot worse while you’re pregnant.
But as anyone who’s had dry and itchy eyes will know, it can be infuriating. It can impact on your ability to sleep and also increases the risk of eye infection.
So what can you do until you get some eye drops from your optometrist or family doctor? Well, there are some home remedies you can try first. These include:
- Applying warm or cold compresses to your eyes
- Increasing the air moisture in your home with a humidifier
- Keep your eyes clean and free of discharge by washing them with water
- Applying cucumber slices to your eyes
If these suggestions don’t provide any relief, or you’re worried that you might have an infection, be sure to visit an eye doctor straight away and ask about pregnancy eye drops.
How we can helpAt Image Optometry, we specialize in eye health. We can advise what eye drops are safe during pregnancy.
Maybe you’ve been using eye drops alongside your contact lenses prior to your pregnancy? Perhaps even for years now? Then we can say whether or not you should continue to use them, or whether an alternative product would be more suitable.
Or maybe you’ve developed dry and itchy eyes as a result of your pregnancy? If so we can explore the different treatments available, recommending the best option for you and your unborn baby.
To find out more, book an appointment with one of our optometrists.
what you can for the nose and eyes
Allergy drops for pregnant women are topical drugs that are allowed for women during the period of bearing a baby. What remedy to choose to relieve unpleasant symptoms and not harm the unborn baby?
Allergy: causes and symptoms
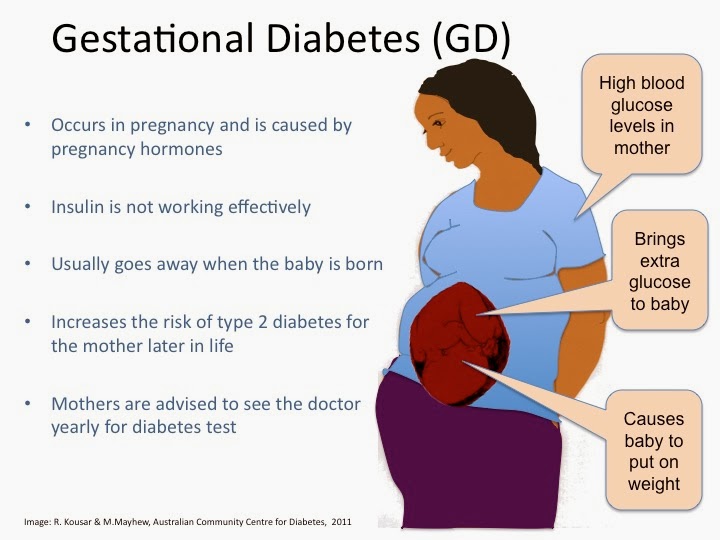
During pregnancy, allergies are possible even in women who have not experienced it before. Immunity works differently, all the forces of the mother's body are thrown to protect the fetus, plus hormonal changes; the result is an overreaction to stimuli.
There are countless allergens around us.
Most often, a strong reaction is caused by:
- hay fever (plant pollen) - watery and swollen eyes, a runny nose, itching and swelling in the nose, sneezing attacks, sore throat, less often - rashes on the skin, etc.;
- food (exotic fruits, nuts, sweets, seafood, etc.) - skin rashes, rhinitis, conjunctivitis, sore throat, gastrointestinal upset, etc.;
- insect bites - swelling, itching, runny nose, sore throat;
- pet hair - watery eyes, runny nose, itching and swelling in the nose, throat, urticaria, etc.;
- household chemicals and cosmetics - redness and itching of the skin, runny nose, swelling of the nose, eyes, throat.
During pregnancy, even a harmless allergic rhinitis or cough is serious.
Allergy affects the fetus not directly (allergens do not penetrate the placenta), but indirectly: a woman becomes restless and irritable, sleeps poorly, constant nasal congestion or swelling of the throat leads to oxygen deficiency.
Severe manifestations of allergies - Quincke's edema, anaphylactic shock are deadly for both mother and unborn baby.
Types of allergy drops
When you are pregnant, you need to be careful with medicines and do not use them without a doctor's prescription.
Many antihistamine pills and injections during gestation are prohibited or allowed in the most extreme cases.
Of the topical preparations that can be used in case of allergies to pregnant women in the nose, drops and sprays are the safest.
Homeopathic drops
The most popular are:
- Euphorbium Composite;
- Delufen;
- Edas-131.
Homeopathic preparations are allowed to be prescribed to pregnant and lactating mothers. They relieve swelling and moisturize the mucous membranes with rhinitis of various origins, act gently and effectively.
Sea salt preparations
Most popular:
- Aquamaris;
- Aqualor;
- Marimer;
- Salin (isotonic sodium chloride solution).
Salt has the ability to absorb liquid, so even ordinary salt water relieves swelling of the mucosa. Sea water is doubly effective: in addition to salts, it contains iodine, cleans the nasal cavity well, and soothes the mucous membranes.
Sea water products are the safest, non-addictive and approved for long-term use.
Hormonal preparations
Most popular:
- Aldecin;
- Nasobek;
- Nazarel;
- Flixonase;
- Nasonex;
- Avamix and others
Hormone-containing preparations act quickly and effectively, but they cannot be used without a doctor's prescription and supervision. During pregnancy and breastfeeding, they are contraindicated or used in isolated cases.
Antihistamines
In the list of permitted - sprays and nose drops for allergies during pregnancy:
- Zyrtec;
- Cromhexal;
- Levocabastin;
- Fenistil.

They are relatively safe, reduce mucus secretion, relieve itching, protect mucous membranes. But they must be used under the supervision of a doctor, strictly observing the dosage and duration of the course of treatment.
Allergy eye drops
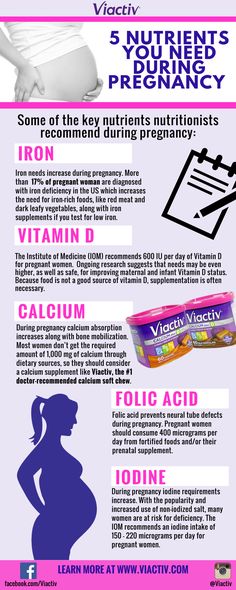
If your eyes are red and watery due to an allergy, drops will help. Safe eye drops for allergies for pregnant women, prescribed by doctors:
- Systein-ultra;
- Acyupar;
- Oftolik;
- Vizin;
- Hilozar;
- Vidisik;
- Okomistin.
Like nasal preparations, they should not be used without a doctor's prescription.
Do's and Don'ts
Drops and sprays are topical products, and the danger from them to the expectant mother and fetus is less than from tablets. But they also need to be treated with caution.
| Allowed during pregnancy | • homeopathic remedies: Euphorbium Composite, Delufen, Edas-131; • preparations based on sea water: Aquamaris, Aqualor, Merimer, Salin.  |
| Allowed in extreme cases under medical supervision | • some antihistamines: Zyrtec, Kromheksal, Levocabastine, Fenistil. |
| Prohibited during pregnancy | • hormonal agents: Aldecin, Nasobek, Nazarel, Flixonase, Nasonex, Avamix; • antihistamines: Xylometazoline, Reaktin, Allergodil, Histimet; • complex agents: Vibrocil; Tizin; Allergy. |
It is important to remember that antihistamines, including nasal sprays and eye drops for allergies, should not be used by pregnant women in the first trimester and late pregnancy, before childbirth: they can depress the baby's nervous system.
Summing up
We remind you that even relatively safe drugs should not be used during pregnancy without consulting a doctor.
Allergies sometimes come on suddenly and help is needed urgently. If it's flowering season, or if you have cats/dogs at home, or just in case, talk to your doctor ahead of time.
If you are not an experienced allergy sufferer, and your nose is stuffy from pollen or oranges for the first time, use an agent for washing that will definitely not harm - saline or salt water.
Be healthy!
| Share Contents:
General recommendations Today, even bronchial asthma is not considered a contraindication for pregnancy. If a woman has a predisposition to allergies, three types of influence of pregnancy on allergies can be distinguished:
In the first case, allergy symptoms are not aggravated by pregnancy, but arise, just as in normal times, from contact with allergens. If you know what you are allergic to, be very careful and attentive and avoid contact with allergens. If you don't know what you're allergic to and you're planning a pregnancy, see an allergist. The second variant of pregnancy is also quite common. Scientists have proven that during pregnancy, a woman increases the production of the hormone cortisol, which has anti-allergic effects. Therefore, in pregnant women, allergies can occur in a milder form, and even the manifestations of bronchial asthma and hay fever can become much weaker. After childbirth, the level of cortisol in the blood gradually returns to normal, and the manifestations of allergies resume. During the last 4 weeks before delivery, in almost all women, the course of any allergic diseases improves significantly. A more severe variant is also possible, when pregnancy negatively affects allergies. According to statistics, the most common allergic symptoms are runny nose and congestion, which usually occur from the 12th week of pregnancy. Another allergic disease - bronchial asthma - occurs in 2% of pregnant women. If a woman has never suffered from asthma, the likelihood that it will suddenly appear during pregnancy is very small. If there is bronchial asthma, then its exacerbation should be expected from the 24th to the 36th week of pregnancy. Of course, if you have bronchial asthma, you need regular consultations with an allergist when planning and during pregnancy. During the last 4 weeks before delivery, asthma almost always improves. There are a number of allergic skin manifestations (eg urticaria) that often occur during the first pregnancy. Do not panic: if the manifestations of hives are minor, they are likely to pass on their own. If the allergy bothers you, do not take any measures on your own and consult an allergist. If the allergen cannot be identified, doctors sometimes talk about an allergy to the pregnancy itself. There is an assumption (albeit controversial) that the hormonal surge that accompanies pregnancy may be the cause of the exacerbation of allergic reactions. According to statistics, pregnancy allergies are more likely to occur in women who are expecting the birth of their sons. In this case, it remains only to wait until the hormonal background returns to normal, the body gets used to the new situation and the manifestations of allergies, as well as toxicosis, subside and disappear. As a rule, relief occurs at 12-14 weeks, when the placenta is formed. Prevention One of the main ways to prevent allergies in mothers and unborn children is a hypoallergenic diet. All pregnant women are advised to observe it, starting from the seventh month. If the expectant mother suffers from allergies, then she needs to adhere to such a diet from the first days of pregnancy. The main principle of this diet is the elimination of allergenic foods from the diet. These include: milk, eggs, nuts, honey, seafood (crabs, shrimp, crayfish, oysters), fish, red and black caviar, soybeans, raspberries, strawberries, tomatoes, chocolate, cheese, citrus fruits, canned foods, everything spicy, salted, smoked and pickled, as well as ready-made juices. Allowed: cereals, cereals, lean meat and boiled poultry (veal, turkey, chicken), fresh and cooked vegetables and fruits of a soft color (potatoes, cabbage, cucumbers, zucchini, green and yellow apples, pears, etc. .). It is absolutely unacceptable to smoke (both active and passive) a pregnant and lactating woman. Ventilate the room more often, do wet cleaning daily, vacuum carpets and upholstered furniture at least once a week, knock out and dry pillows. Try to limit contact with cats and dogs during pregnancy, as well as remove cockroaches and ants. What can you do? An allergist should be consulted even before pregnancy. To get rid of an allergy, you must first identify the allergen and eliminate or minimize contact with it. Try taking vitamins that can relieve allergy symptoms (see article). Follow the recommendations of an allergist, do not self-medicate, lead a healthy lifestyle - and the pregnancy will go well. TreatmentWhat can a doctor do?An allergist can use special tests to find out what the expectant mother is allergic to and thus prevent exacerbations. To identify the allergen, an allergist conducts special examinations: skin scarification tests and, if necessary, determines the blood levels of IgE antibodies specific to certain allergens. Although it is impossible to get rid of the predisposition to allergic diseases, it is quite possible to alleviate the symptoms of allergies. Allergy medications during pregnancyPregnant women should be very careful when taking medications, including anti-allergy medications. It is necessary to constantly consult with an allergist and take medication only if the possible risk of affecting the fetus does not exceed the benefit received. All drugs are strictly not recommended to be taken in the first trimester of pregnancy; in the second and third trimesters, the restrictions are less severe. None of the antiallergic drugs guarantees complete safety for the unborn child. Take any drug only on the advice and under the supervision of a doctor. The antihistamine drug tavegil, when tested on pregnant rats, caused heart defects and paw defects in pups. The use of antihistamines during pregnancy: SUPRASTIN - The use of the drug is possible if the potential benefit to the mother outweighs the possible risk to the fetus, that is, in the case when the mother's allergic condition threatens the fetus more than taking the drug. PIPOLFEN - Not recommended during pregnancy and lactation. ALLERTEK - The use of the drug is possible if the potential benefit to the mother outweighs the possible risk to the fetus. TAVEGIL - During pregnancy, it is possible to use it only for health reasons, since a negative effect of this drug on the fetus has been revealed. Tavegil should be used only when an allergic reaction threatens the patient's life, and there is no possibility to use another drug for one reason or another. CLARITIN - There is no absolute contraindication to the use of Claritin during pregnancy. The use of the drug is possible if the intended benefit to the mother outweighs the potential risk to the fetus. FEXADIN - In pregnancy, the use is possible only if the effect of therapy outweighs the potential risk to the fetus. |
 The most important thing is the constant monitoring of the attending physician and compliance with all his recommendations, as well as reasonable prevention before pregnancy and during 9months of waiting for a baby. In addition, there are a number of drugs that, if necessary, are used in the second and third trimesters during pregnancy.
The most important thing is the constant monitoring of the attending physician and compliance with all his recommendations, as well as reasonable prevention before pregnancy and during 9months of waiting for a baby. In addition, there are a number of drugs that, if necessary, are used in the second and third trimesters during pregnancy.