Yeast infection baby symptoms
Thrush in newborns Information | Mount Sinai
Candidiasis - oral - newborn; Oral thrush - newborn; Fungal infection - mouth - newborn; Candida - oral - newborn
Thrush is a yeast infection of the tongue and mouth. This common infection can be passed between a mother and baby during breastfeeding.
Causes
Certain germs normally live in our bodies. While most germs are harmless, some can cause infection.
Thrush occurs when too much of a yeast called Candida albicans grows in a baby's mouth. Germs called bacteria and fungi naturally grow in our bodies. Our immune system helps keep these germs in check. But babies do not have fully-formed immune systems. That makes it easier for too much yeast (a type of fungus) to grow.
Thrush often occurs when mother or baby has taken antibiotics. Antibiotics treat infections from bacteria. They can also kill "good" bacteria, and this allows yeast to grow.
The yeast thrives in warm, moist areas. The baby's mouth and the mother's nipples are perfect places for a yeast infection.
Babies can also get a yeast infection on the diaper area at the same time. The yeast gets in the baby's stool and can cause a diaper rash.
Symptoms
Symptoms of thrush in the baby include:
- White, velvety sores in the mouth and on the tongue
- Wiping the sores may cause bleeding
- Redness in the mouth
- Diaper rash
- Mood changes, such as being very fussy
- Refusing to nurse because of soreness
Some babies may not feel anything at all.
Symptoms of thrush in the mother include:
- Deep-pink, cracked, and sore nipples
- Tenderness and pain during and after nursing
Exams and Tests
Your health care provider can often diagnose thrush by looking at your baby's mouth and tongue. The sores are easy to recognize.
Treatment
Your baby might not need any treatment. Thrush often goes away on its own in a few days.
Thrush often goes away on its own in a few days.
Your provider may prescribe antifungal medicine to treat thrush. You paint this medicine on your baby's mouth and tongue.
If you have a yeast infection on your nipples, your provider may recommend an over-the-counter or prescription antifungal cream. You put this on your nipples to treat the infection.
If both you and your baby have the infection, you both need to be treated at the same time. Otherwise, you can pass the infection back and forth.
Outlook (Prognosis)
Thrush in babies is very common and can easily be treated. Let your provider know if thrush keeps coming back. It may be a sign of another health issue.
When to Contact a Medical Professional
Contact your provider if:
- Your baby has symptoms of thrush
- Your baby refuses to eat
- You have symptoms of a yeast infection on your nipples
Prevention
You may not be able to prevent thrush, but these steps may help:
- If you bottle feed your baby, clean and sterilize all equipment, including nipples.

- Clean and sterilize pacifiers and other toys that go in baby's mouth.
- Change diapers often to help prevent yeast from causing diaper rash.
- Be sure to treat your nipples if you have a yeast infection.
Balest AL, Riley MM, O'Donnell B, Zarit JS. Neonatology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 2.
Harrison GJ. Approach to infections in the fetus and newborn. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, eds. Feigin and Cherry's Textbook of Pediatric Infectious Diseases. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 66.
Last reviewed on: 12/12/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA.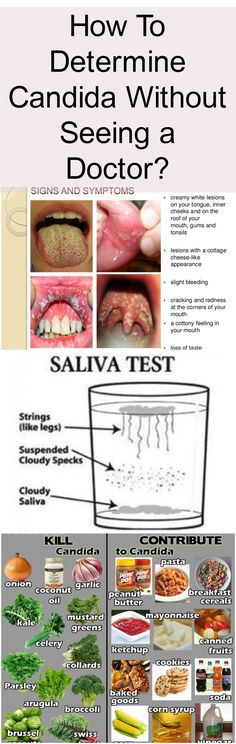 Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Yeast Diaper Rash (Candida Diaper Dermatitis): Symptoms, Causes, Treatments
Overview
The application of antifungal medication to a yeast diaper rash.What is a yeast diaper rash?
A diaper rash is a common condition that creates red and purple swollen, sore patches of skin near your baby’s diaper region.
Yeast is a type of fungus that naturally lives on your body in small amounts, often found in your mouth, skin and in your intestines. Your body also hosts healthy bacteria, which control the balance of yeast (microbiome) to prevent infection. If the balance of yeast and bacteria is off, yeast will overgrow, which will cause a rash.
Most common in diaper-wearing children, yeast, specifically Candida albicans yeast, could cause a diaper rash on infants if the balance of yeast and healthy bacteria is off balance. Infected feces are the main source for a Candida diaper rash.
Infected feces are the main source for a Candida diaper rash.
Diaper rashes are the result of irritation from their diaper causing friction against their skin, an infection or an allergic reaction. A combination of irritation and infection from Candida overgrowth is a yeast diaper rash, also known as Candida diaper dermatitis.
What is the difference between a diaper rash and a yeast infection?
A yeast infection could be the cause of a diaper rash, but there are differences between the two diagnoses.
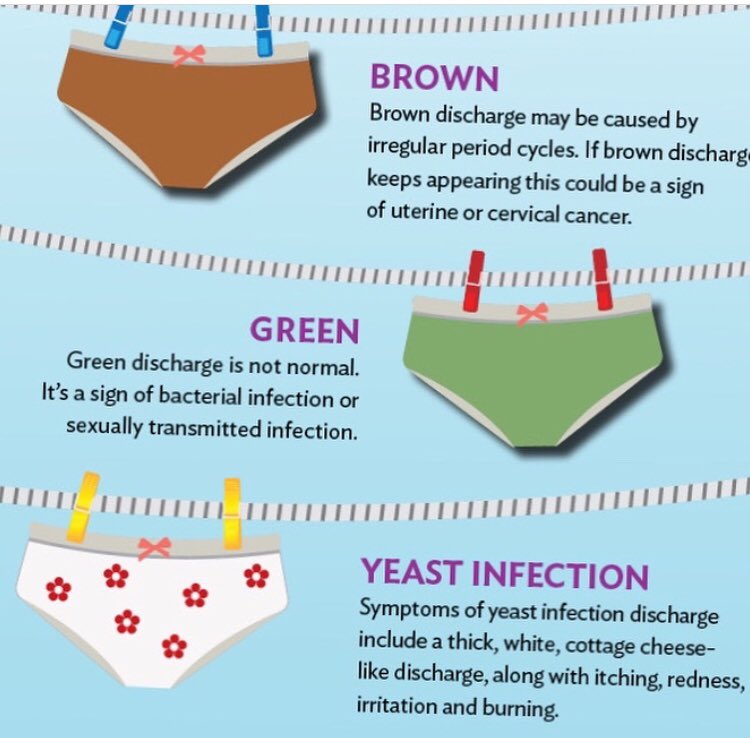
| Yeast Infection | Diaper Rash |
|---|---|
| Skin that is bumpy (pimples), shiny, cracked or oozy with a deep red or purple tone. | Skin that is dry, scaly or smooth with a light pink to purple tone. |
| Appears on skin folds near the groin, legs and genitals. | Appears on larger surfaces like the buttocks. |
Rash could be in several, smaller spots along the diaper region. | Rash is in one spot along the diaper region. |
| Treat with antifungal medication, which could take a few weeks to clear. | Treat with diaper creams that clear in a couple days. |
Who does a yeast diaper rash affect?
A yeast diaper rash affects anyone who wears a diaper, but it's most common in babies and infants. Rashes most often affect babies between nine months and one year.
How common are yeast diaper rashes?
Skin problems are common in infants and children. Most babies develop a form of diaper rash during the time that they wear a diaper. Studies show that nearly one out of every three infants could have a diaper rash at any point in time and more than half of children between four months and 15 months have a diaper rash at least once in a two-month period. A diaper rash is very common after taking systemic antibiotics.
How does a yeast diaper rash affect my baby’s body?
A diaper rash causes skin irritation and your baby will show signs of discomfort, like crying, trying to itch the area or they will become fussy, which might be difficult to ease. To lessen your baby’s reaction to the symptoms of the rash, visit or call your baby’s healthcare provider at the first sign to treat the condition.
To lessen your baby’s reaction to the symptoms of the rash, visit or call your baby’s healthcare provider at the first sign to treat the condition.
Symptoms and Causes
What does a yeast diaper rash look like?
Symptoms of a yeast diaper rash will appear in the diaper area in the folds of your baby’s skin, which includes the groin area, genitals, buttocks and upper thigh. Symptoms of a yeast diaper rash include:
- Deep red or purple raised patch of skin.
- Bumps or tiny fluid-filled pimples.
- Rash that appears shiny.
- Cracked or very dry skin.
- Itchiness, mild pain and discomfort.
Severe cases of a yeast diaper rash create painful open sores on your baby’s skin that may ooze clear fluid or bleed when the skin breaks due to friction from your baby’s diaper.
What causes a yeast diaper rash?
A type of yeast that lives on our bodies in small amounts is Candida albicans. Sometimes outside factors disrupt the balance of Candida and healthy bacteria (microbiome), causing a rash to form in the diaper area of our baby’s skin. Yeast is a type of fungus that thrives is warm and moist environments, making the diaper region the perfect place for yeast to grow.
Yeast is a type of fungus that thrives is warm and moist environments, making the diaper region the perfect place for yeast to grow.
Contributing factors to the development of yeast diaper rashes include:
- Little to no air circulation on the skin.
- Urine or stool touching skin for long periods of time (overnight).
- Diaper material rubbing on skin repeatedly.
- Side effect of taking antibiotics or receiving them from a chestfeeding (breastfeeding) parent.
Is a yeast diaper rash contagious?
Yeast diaper rashes are not contagious like a cold or virus. Yeast infections are the result of an overgrowth of yeast due to an imbalance of healthy bacteria in your baby’s body. It is important to wash your hands thoroughly after diaper changes to keep your body’s yeast and healthy bacteria balanced.
Diagnosis and Tests
How is a yeast diaper rash diagnosed?
Your baby’s healthcare provider will visually examine the affected area to begin the diagnosis. They will ask questions about your baby’s symptoms, including duration and severity, along with questions about any medications that you or your baby might be taking that could disrupt the balance of yeast in your baby’s body. Occasionally they will swab the rash with sterile cotton to examine the type of yeast under a microscope.
They will ask questions about your baby’s symptoms, including duration and severity, along with questions about any medications that you or your baby might be taking that could disrupt the balance of yeast in your baby’s body. Occasionally they will swab the rash with sterile cotton to examine the type of yeast under a microscope.
Management and Treatment
How do I treat a yeast diaper rash?
Since yeast is a fungus, your healthcare provider will recommend an antifungal medication (cream, ointment or pill) to stop the yeast overgrowth and treat the rash. For severe yeast diaper rash, your healthcare provider might recommend a steroid ointment (hydrocortisone) to combat the issue.
Your healthcare provider will give you instructions on how to apply the antifungal cream and how long you should be using it to make sure the infection clears up completely to reduce the likelihood of it returning.
Can I treat a yeast diaper rash with over-the-counter medicine?
Yes, you can use over-the-counter antifungal creams such as clotrimazole to treat a yeast diaper rash. This treatment option may be effective but it is not certain that it will clear the rash or treat the overgrowth of yeast completely without a diagnosis from your healthcare provider to target the specific type of yeast that caused the rash.
This treatment option may be effective but it is not certain that it will clear the rash or treat the overgrowth of yeast completely without a diagnosis from your healthcare provider to target the specific type of yeast that caused the rash.
How do I manage symptoms of a yeast diaper rash?
There are several ways that you can manage yeast diaper rash symptoms on your baby. Treatment options include:
- Cleaning the rash often: Since the rash causes discomfort, gently clean the diaper area with water and a soft washcloth. Disposable diaper wipes are helpful, but avoid wipes that contain alcohol and fragrances. Delicately pat the diaper area dry rather than rubbing or allowing the area to air dry.
- Applying an ointment or cream on the rash: After treating the rash with an antifungal medication, apply a thick layer of protective ointment or cream, like one that contains zinc oxide or petroleum jelly to create a barrier between the diaper and the skin.
 Ointments are usually thick and don't have to be completely removed at the next diaper change.
Ointments are usually thick and don't have to be completely removed at the next diaper change. - Frequently changing your baby’s diaper: Yeast thrives in warm and damp environments, so it is best to keep the diaper area as clean and dry as possible. Changing diapers often makes sure that there is less moisture on your baby’s skin. Change your baby’s diaper at least once during the night and, if possible, leave your baby’s diaper off for a short amount of time to increase airflow between diaper changes or during nap time. Keep the diaper loose so that the soiled area doesn’t rub against their skin as much.
How long does it take for a yeast diaper rash to go away?
After treating the yeast diaper rash with antifungal medication, symptoms will start to fade and may disappear after three days. The overgrowth of yeast may still be present after symptoms go away, so it is important to follow treatment guidelines from your healthcare provider from start to finish to make sure the rash does not return. It may take between two to three weeks for a yeast diaper rash to completely clear up.
It may take between two to three weeks for a yeast diaper rash to completely clear up.
Prevention
How can I prevent a yeast diaper rash?
You can prevent a yeast diaper rash by:
- Avoid using baby wipes with fragrances or alcohol.
- Changing diapers frequently.
- Cleaning skin between diaper changes.
- Not securing diapers too tightly to allow airflow or leaving diapers off for short periods of time.
- Using highly absorbent diapers.
- Using ointment or cream to create a barrier between skin and diaper.
- Discussing side effects of medications (antibiotics) you or your baby take with your healthcare provider.
Outlook / Prognosis
What can I expect if my baby has a yeast diaper rash?
If your baby has a yeast diaper rash, they will show signs of irritation and discomfort through crying or being fussy, especially during diaper changes. As their caretaker, you will notice a rash forming on or near their diaper area, noting color changes of their skin, elevated skin and small pimples forming in the folds of their skin. Treatment will clear the symptoms that are irritating your baby within the first couple of days, but it will take a couple of weeks for the rash to go away completely. Make sure you finish treatment as advised by your baby’s healthcare provider so the rash doesn’t return.
Treatment will clear the symptoms that are irritating your baby within the first couple of days, but it will take a couple of weeks for the rash to go away completely. Make sure you finish treatment as advised by your baby’s healthcare provider so the rash doesn’t return.
Living With
When should I see my healthcare provider?
If you notice signs of a diaper rash and traditional diaper creams or ointments don’t clear the rash, it increases in size and causes extreme discomfort for your baby, you should visit your healthcare provider. If your baby’s rash turns into an open sore, bleeds frequently or starts to ooze yellow or clear fluid, those are symptoms of an infection and you should visit your healthcare provider immediately.
What questions should I ask my doctor?
- How long should I use an antifungal cream on my baby’s skin?
- If I am chestfeeding (breastfeeding) and on antibiotics, how will that affect my baby?
- What can I do to make sure a yeast diaper rash does not come back after I finish treatment?
A note from Cleveland Clinic
Diaper rashes are very common among diaper-wearing children. It is easy to disrupt the balance of yeast on your baby’s growing body, making yeast diaper rashes a temporary discomfort, treatable with an antifungal medication. Talk with your baby’s healthcare provider to choose the right treatment option that best suits your baby’s needs and follow instructions on the antifungal medication to make sure the rash doesn’t return.
It is easy to disrupt the balance of yeast on your baby’s growing body, making yeast diaper rashes a temporary discomfort, treatable with an antifungal medication. Talk with your baby’s healthcare provider to choose the right treatment option that best suits your baby’s needs and follow instructions on the antifungal medication to make sure the rash doesn’t return.
Thrush in infants. What is Thrush in Infants?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Thrush is one of the clinical variations of fungal diseases caused by yeast-like fungi from the genus Candida. In infants, the most common oral form is candidal stomatitis. Clinical manifestations include a white cheesy coating on the mucous membranes of the cheeks, tongue and palate. In severe cases, the entire oral cavity is affected, the general condition of the child is disturbed. Diagnosis involves the identification of specific symptoms during examination, confirmation of the diagnosis by microscopic, bacteriological and cultural methods. Treatment is carried out with the help of local and systemic application of antimycotic drugs.
In severe cases, the entire oral cavity is affected, the general condition of the child is disturbed. Diagnosis involves the identification of specific symptoms during examination, confirmation of the diagnosis by microscopic, bacteriological and cultural methods. Treatment is carried out with the help of local and systemic application of antimycotic drugs.
- Causes of thrush in infants
- Symptoms of thrush in infants
- Complications of thrush in infants
- Diagnosis of thrush in infants
- Treatment of thrush in infants
- Prognosis and prevention of thrush in infants
- Prices for treatment
General
Candidiasis or thrush in infants is a fungal pathology that is caused by opportunistic or pathogenic strains of fungi of the genus Candida. At 80-90% of her cases are caused by C. albicans. For newborns and infants, oral candidiasis is most common. Candidiasis stomatitis was first described by Hippocrates around 400 BC. The pathology got the name "thrush" because of the white plaque on the mucous membranes, which looks like curdled milk, and also because of the curdled discharge. The incidence depends on a decrease in immunity against the background of underlying pathologies or external circumstances: candidiasis develops in 20-25% of children with type I diabetes, in 25-30% of oncological patients and in 70-90% of babies with AIDS.
The pathology got the name "thrush" because of the white plaque on the mucous membranes, which looks like curdled milk, and also because of the curdled discharge. The incidence depends on a decrease in immunity against the background of underlying pathologies or external circumstances: candidiasis develops in 20-25% of children with type I diabetes, in 25-30% of oncological patients and in 70-90% of babies with AIDS.
Thrush in infants
Causes of thrush in infants
The cause of thrush in infants, as in adults, are fungi from the genus Candida. Most often, C. albicans acts as the causative agent, less often - C. tropicalis, C. parapsilosis, C. glabrata, C. krusei. These yeast-like fungi are included in the list of opportunistic agents, since they are contained in the normal microflora of the oral cavity and small intestine. With the full functioning of the immune system, they do not have a negative effect. Against the background of a decrease in the body's resistance, fungi begin to grow and multiply rapidly, damaging the mucous membrane and underlying tissues.
Many exogenous and endogenous factors can contribute to the development of thrush in infants. Internal factors include prematurity, formula feeding, surgeries, hypo- and beriberi, alimentary dystrophy, anemia, rickets, disruption of normal intestinal microflora, SARS, chronic viral diseases (including HIV), metabolic disorders of proteins, fats and carbohydrates , endocrine pathologies (including diabetes mellitus), malignant neoplasms, frequent regurgitation and vomiting. External factors provoking the development of candidiasis are chemical or physical damage to the mucous membrane, prolonged antibiotic therapy, taking immunosuppressive drugs, hormonal drugs and cytostatics, vulvovaginal candidiasis during pregnancy and / or childbirth in the mother, contact with patients with candidiasis or carriers of pathogenic strains, IVL and being in the conditions of the RIT department.
Symptoms of thrush in infants
The incubation period for thrush in infants ranges from 2 days to 2 months, with an average of 3-6 days. The clinical picture depends on the severity of the lesion. There are mild, moderate and severe forms of candidal stomatitis. The mild form is the most common. It is characterized by damage to the oral cavity in the form of foci of curdled plaque. The most common localization is the inner surface of the cheeks, the upper part of the tongue, less often the hard and soft palate. Formations are effortlessly separated by scraping. The general condition of the child is not disturbed, there is no discomfort, no specific smell is observed.
The clinical picture depends on the severity of the lesion. There are mild, moderate and severe forms of candidal stomatitis. The mild form is the most common. It is characterized by damage to the oral cavity in the form of foci of curdled plaque. The most common localization is the inner surface of the cheeks, the upper part of the tongue, less often the hard and soft palate. Formations are effortlessly separated by scraping. The general condition of the child is not disturbed, there is no discomfort, no specific smell is observed.
Moderate and severe forms of thrush in infants are less common, since they develop only in the absence of regular preventive examinations by a pediatrician or a conscious refusal of parents to treat. Candidiasis stomatitis of moderate severity is manifested by a cheesy or film-like plaque, diffusely spreading over all typical lesions. Adjacent tissues are sharply hyperemic. When trying to separate plaque from the mucous membrane, only some of its parts are removed, in place of which drops of blood remain.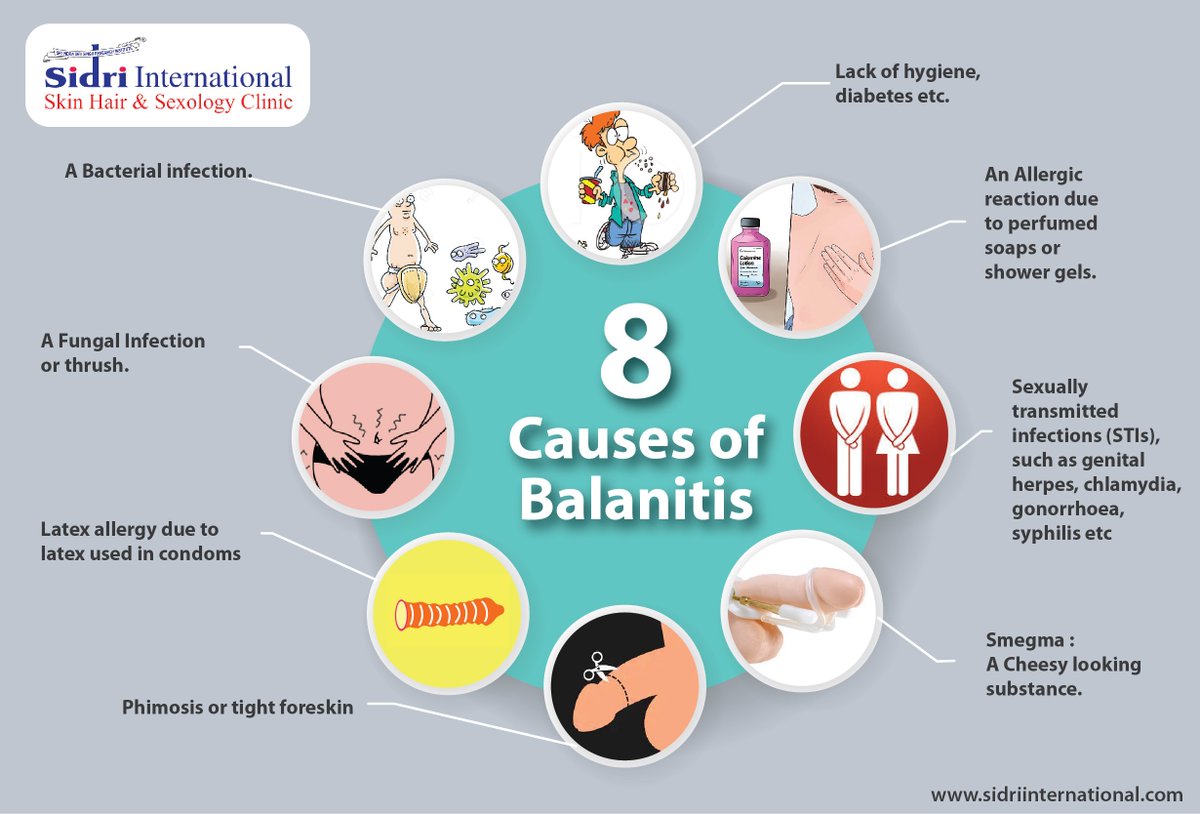 The general condition is somewhat disturbed: restless sleep, the child is naughty.
The general condition is somewhat disturbed: restless sleep, the child is naughty.
In a severe form of thrush in infants, a total lesion of all mucous membranes of the oral cavity, including the posterior pharyngeal wall, gums, and lips, is revealed. The plaque is tightly soldered to the underlying tissues, therefore, when scraping, it is possible to separate only small areas, under which a whitish film remains. On examination, a strong unpleasant odor is detected from the mouth. The general condition of the child is sharply disturbed: he is restless, sleeps badly, often cries, refuses his mother's breast.
Complications of thrush in infants
In children, unlike adults, there is a tendency to the rapid development and spread of pathological processes. Because of this, candidal stomatitis is often accompanied by damage to other parts of the body - candidiasis of the perineum, intestines, intergluteal and inguinal-femoral folds, candidal vulvovaginitis occur. In severe forms of thrush in infants, hematogenous and lymphogenous dissemination of fungi often occurs - sepsis develops. Ineffective treatment of acute candidiasis can lead to its transition to a chronic form. In addition to constant exacerbations and violations of the general condition of the child, this condition causes a further decrease in immunity, a tendency to allergic reactions and atopic diseases, such as bronchial asthma.
In severe forms of thrush in infants, hematogenous and lymphogenous dissemination of fungi often occurs - sepsis develops. Ineffective treatment of acute candidiasis can lead to its transition to a chronic form. In addition to constant exacerbations and violations of the general condition of the child, this condition causes a further decrease in immunity, a tendency to allergic reactions and atopic diseases, such as bronchial asthma.
In girls, against the background of oral thrush, vulvovaginal candidiasis very often develops. Clinically, it is manifested by hyperemia, swelling and dryness of the external genital organs with erosions of the mucous membranes. In pediatrics and neonatology, this pathology is of great danger, since in infancy, due to the special tenderness of tissues, there is a high risk of fusion of the labia and vaginal walls with each other. Such a complication, in addition to massive pharmacotherapy, requires surgical intervention.
Diagnosis of thrush in infants
Diagnosis of thrush in infants is based on a full collection of anamnestic data, an objective and laboratory examination of the child. Instrumental studies are usually not required. When collecting an anamnesis, the pediatrician establishes the etiological and contributing factors, determines the time of the onset of the disease, and evaluates the characteristics of the child's condition. The specialist must pay attention to the fungal pathologies of the mother during pregnancy and childbirth. The physical examination includes a thorough examination of the oral cavity, identifying characteristic deposits, determining the severity of the process, and examining other parts of the body that can potentially develop candidiasis. The leading role is played by laboratory diagnostics, which consists in microscopy, bacteriological and serological examination.
Instrumental studies are usually not required. When collecting an anamnesis, the pediatrician establishes the etiological and contributing factors, determines the time of the onset of the disease, and evaluates the characteristics of the child's condition. The specialist must pay attention to the fungal pathologies of the mother during pregnancy and childbirth. The physical examination includes a thorough examination of the oral cavity, identifying characteristic deposits, determining the severity of the process, and examining other parts of the body that can potentially develop candidiasis. The leading role is played by laboratory diagnostics, which consists in microscopy, bacteriological and serological examination.
Microscopic diagnosis is the first stage at which the material obtained during scraping is examined under a light or electron microscope. It makes it possible to identify the characteristic filaments of mycelium and yeast-like cells. The cultural method allows you to determine the type of fungus and its sensitivity to specific antimycotic drugs. This method is also used when initial empiric treatment with common agents has failed. Serological reactions (most often RSK) are indicated in the absence of a clear clinical picture and low informativeness of other studies. Based on the above studies, differential diagnosis of candidal stomatitis with acute tonsillitis, diphtheria and acute herpetic stomatitis in children is carried out.
This method is also used when initial empiric treatment with common agents has failed. Serological reactions (most often RSK) are indicated in the absence of a clear clinical picture and low informativeness of other studies. Based on the above studies, differential diagnosis of candidal stomatitis with acute tonsillitis, diphtheria and acute herpetic stomatitis in children is carried out.
Treatment of thrush in infants
Treatment of thrush in infants depends on the prevalence of the pathological process. In the early stages, with a local lesion, local therapy is indicated - the oral cavity is irrigated with anti-candidiasis (clotrimazole, nystatin) alkalizing (2% baking soda solution, 0.25% boron solution) and disinfectant (aniline dyes - Lugol's solution, methylene blue) means. When breastfeeding, the mother's breast is treated with a 2% soda solution and herbal infusions (oak, calendula, and others). Such treatment is carried out until the complete recovery of the child, but for a period of at least 14 days.
In moderate and severe forms, systemic therapy is recommended by oral or parenteral administration of antimycotic drugs. When using anti-candidiasis drugs through the mouth, preference is given to powders for injection (fluconazole), since the prepared solution has not only a general, but also a local effect on the mucous membranes of the oral cavity. In parallel, the treatment of concomitant diseases and symptomatic therapy according to indications is carried out in full. According to current recommendations, this approach should also be used for mild forms, since it allows to reduce the treatment time to 3-6 days.
Prognosis and prevention of thrush in infants
The prognosis for thrush in infants is favorable. With timely rational therapy, complete recovery occurs within 7-10 days. Severe forms and the development of complications are observed only against the background of the complete absence of antifungal treatment. Nonspecific prevention of candidal stomatitis consists in the full care of the skin and mucous membranes of the child, especially against the background of severe pathologies that reduce immunity. An important role is given to the rational use of antibacterial agents and the treatment of fungal diseases in the mother during the period of bearing a child.
An important role is given to the rational use of antibacterial agents and the treatment of fungal diseases in the mother during the period of bearing a child.
Specific prevention of thrush in infants is necessary if there are indications that include a burdened obstetric and gynecological history of the mother, prematurity and intrauterine malformations of the child, respiratory disorders, birth injuries of newborns, CNS pathologies. Newborns included in this group, the first 7 days of life, microscopy and bacteriology of samples of mucous membranes and feces are performed. For infants on antibiotic therapy, a prophylactic course of an antifungal drug, usually fluconazole, is given.
You can share your medical history, what helped you in the treatment of thrush in infants.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Candidiasis in the mouth of a child
Contents
What kind of disease is candidiasisSymptomsCausesTreatmentMethods of therapyPreventive measures
Many parents are aware of such a common problem in children as thrush, which is characterized by the appearance of white plaque on the tissues of the oral cavity. In medicine, this pathological condition has the term "candidiasis" and refers to fungal diseases.
Most often, candidiasis develops in the mouth of a child in the first year of life. Symptoms of thrush greatly disturb the baby, but timely treatment allows you to quickly and without consequences get rid of the fungus.
What kind of disease is candidiasis
According to statistics, about 30% of infants are faced with candidiasis. The causative agent of the disease is the Candida fungus. These specific microorganisms are normally present in the body of every person, even in the absence of health problems, but only in small quantities.

Oral candidiasis in children is much more common, since the immune system of babies is not yet formed and is not able to withstand pathogenic microorganisms and the effects of negative external factors.
With a weakened immune system and the concomitant effect of provoking factors, the fungus begins to actively multiply, affecting the mucous membranes. Without therapeutic treatment, candidiasis is eliminated in exceptional cases. If thrush is not treated, complications arise, and the infection itself spreads throughout the body.
Symptoms
Oral candidiasis in children can have a different form of manifestation and severity of symptoms: mild, moderate and severe. As a rule, each form corresponds to the stage of development of the disease. If therapy is not carried out in a timely manner, then the signs of a fungal infection become more intense and the number of symptoms increases.
With a mild form of the disease, a red rash appears on the oral mucosa, which is covered with a white coating on top.
 At the next stage, the child has swelling of the tissues and the formation of localized white spots with a touch of curd consistency. Gradually, these spots merge into a large affected area. When plaque is removed, bleeding sores open. If the thrush starts, then the fungus already spreads to the entire oral cavity, including the lips, tongue and throat. All fabrics are completely covered with cheesy bloom.
At the next stage, the child has swelling of the tissues and the formation of localized white spots with a touch of curd consistency. Gradually, these spots merge into a large affected area. When plaque is removed, bleeding sores open. If the thrush starts, then the fungus already spreads to the entire oral cavity, including the lips, tongue and throat. All fabrics are completely covered with cheesy bloom. Common symptoms of candidiasis in children include:
-
burning sensation and itching in the mouth;
-
discomfort and pain when eating;
-
frequent spitting up in babies;
-
the formation of cracks in the corners of the lips;
-
temperature increase.
Children of the first two years of life report their condition with refusal to eat, constant whims and causeless crying. It is not difficult to see signs of candidiasis, so if a child has a sharp rise in temperature or refuses to eat, pediatricians and dentists recommend checking the oral cavity for white plaque.
 If you suspect thrush, it is undesirable to delay a visit to a specialist, since the fungal infection progresses rapidly.
If you suspect thrush, it is undesirable to delay a visit to a specialist, since the fungal infection progresses rapidly. Reasons
The main reason for the development of candidiasis of the oral mucosa in children is a weakened immune system. If a child is born prematurely, then the likelihood of having thrush is very high. Children who are breastfed or have congenital pathologies are also often exposed to fungal infection.
Provoking factors include:
-
the presence of vaginal candidiasis in the mother during pregnancy - the child can become infected when passing through the birth canal;
-
insufficient hygiene of the female breast during breastfeeding - the fungus is often localized precisely on the nipples because of the favorable environment for it;
-
poor processing of the child's initial things - bottles, nipples, and so on;
-
the habit of parents to lick the nipples - even if the adult does not have signs of thrush, a fungus may be present in the mouth, which will be transmitted to the child;
-
long-term use of drugs of the "antibiotics" group - drugs help to reduce one's own immunity;
-
frequent regurgitation in infants - after regurgitation, an increased acidic environment, favorable for the fungus, remains inside the oral cavity;
-
excessive and frequent dry mouth - the absence of saliva, as a protective agent against the activity of pathological microorganisms.
Infection with Candida fungus in children older than 2 years can occur as a result of unwashed foods, raw milk or running water. If a child over 3 years of age has suddenly developed signs of thrush, one should be examined not only for a fungal infection, but also for other possible diseases that may be accompanied by a “fading” of the immune system.
Treatment
Children's fungal diseases can be dealt with by a pediatrician, infectious disease specialist or dermatologist. If we are talking about the treatment of thrush of the oral cavity, then the dentist can also carry out therapy.
The diagnosis of "candidiasis" is determined in most cases on the basis of a specialist examination of the oral cavity. If there is any doubt, the doctor directs the patient for additional examinations. To confirm the disease, a laboratory method is used to study a smear taken from the mouth for the presence of a fungus.
Treatment of thrush in children involves an integrated approach.
 If the disease is not advanced, then local therapy is carried out in combination with the adoption of measures to strengthen the immune system. In severe form, oral candidiasis in children is treated with systemic drugs, local remedies and compliance with preventive recommendations.
If the disease is not advanced, then local therapy is carried out in combination with the adoption of measures to strengthen the immune system. In severe form, oral candidiasis in children is treated with systemic drugs, local remedies and compliance with preventive recommendations. Methods of therapy
Treatment of candidiasis begins with the treatment of the oral cavity. The first procedure is already performed at the reception. Antiseptic agents are used to remove plaque. The doctor may then apply an antifungal agent.
The parent should carefully monitor the actions of the dentist, as in the future they will have to independently process the oral cavity at home. The necessary drugs will be prescribed by a specialist. Local antifungal agents are dangerous in case of overdose, especially for the child's body, so you must strictly follow the doctor's recommendations.
In advanced cases, medications are prescribed in the form of solutions, drops or tablets.
-