Pain medication labor
Intravenous/Intramuscular Labor Pain Relief - Brigham and Women's Hospital
Pain-relieving medications injected into the bloodstream may alleviate, but not eliminate, pain during labor.
These are medications that are given either intravenously (through an IV) or intramuscularly (with an injection) to decrease labor pain and are usually ordered by the obstetrician or midwife and administered by the nurse.
Opioids for Pain Relief
Opioids have a long history of use in obstetrics for the relief of labor and delivery pain. Although there are a great number of narcotics available today, only a few are commonly used for childbirth. They include meperidine (Demerol®), morphine, fentanyl, butorphanol (Stadol®) and nalbuphine (Nubain®).
These medications enter the bloodstream and allow you to better tolerate the pain of labor and delivery, although they do not normally provide complete pain relief. The amount of relief from these medications does vary, but they can take the "edge" off the pain and make your labor more tolerable
The vast majority of women who do not have a regional anesthetic for labor will opt for one of these medications, which can be taken prior to receiving an epidural or spinal anesthetic.
Patient-Controlled Analgesia
If the medications ordered by the obstetrician are not enough to provide satisfactory pain relief, the anesthesiologist can arrange for these medications administered via an intravenous infusion pump that you control. This method of administration pain relief is called patient-controlled analgesia, or PCA.
With this option, you are provided with a button that can be activated whenever you desire pain relief. The pump is programmed to push a certain (set) amount of medication into your system. You have control over how much medication you need depending on how much discomfort you are experiencing from your contractions.
The anesthesiologist and your nurse will monitor the intravenous medications that you are administering. The PCA pumps are programmed so that you cannot take too much of the medication.
Side Effects
A major disadvantage of IV medications is that they can make you drowsy and sleepy. In addition, there may be other side effects that include nausea, vomiting, decreased respirations, itching, constipation and urinary retention.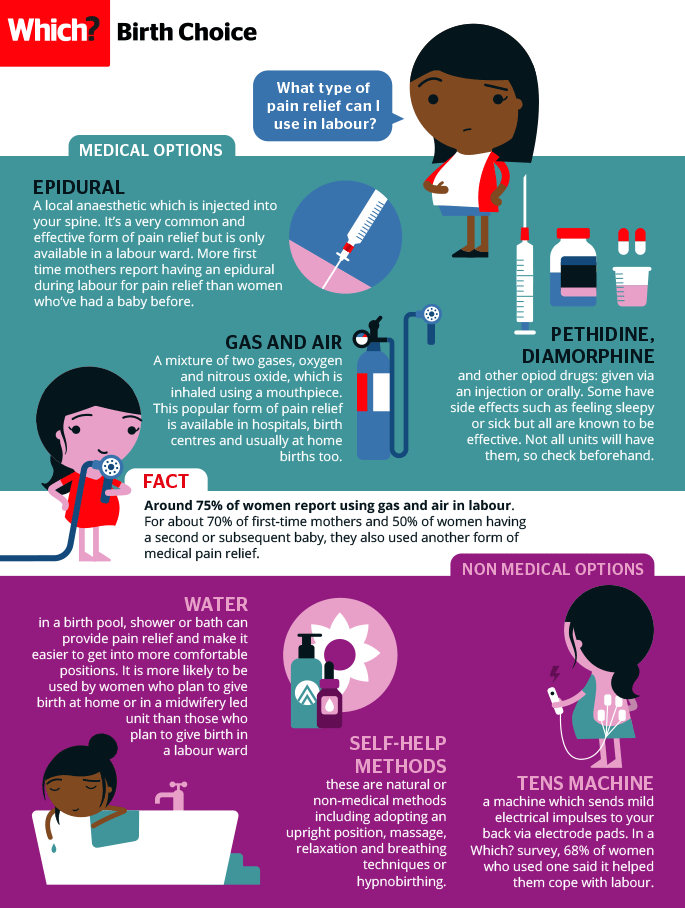
Effect on the Baby
Narcotics will cross the placenta and enter the baby's circulation. As a result, the baby may show some side effects. In utero, the baby's heart rate may change slightly in pattern. But there is no known long-term effect due to this change in heart rate pattern.
The baby has the ability to metabolize the medications, but it does so more slowly than the mother. After the baby is born, the baby may be slightly sleepy. Again, it is unlikely that the baby will be affected adversely as a result of small amount of mother's medication, but it is important to realize that the medication does impact the baby.
Seeing an effect of the mother's medication in the baby may be dependent on the dosing of medication in relation to the time of birth. If the baby has adequate time to break down the medication, only a minimal effect may be seen.
Childbirth - pain relief options
Actions for this page
Summary
Read the full fact sheet- Childbirth is usually a painful experience.

- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
Labour and childbirth is usually a painful experience and women vary in their response to it. Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options. For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
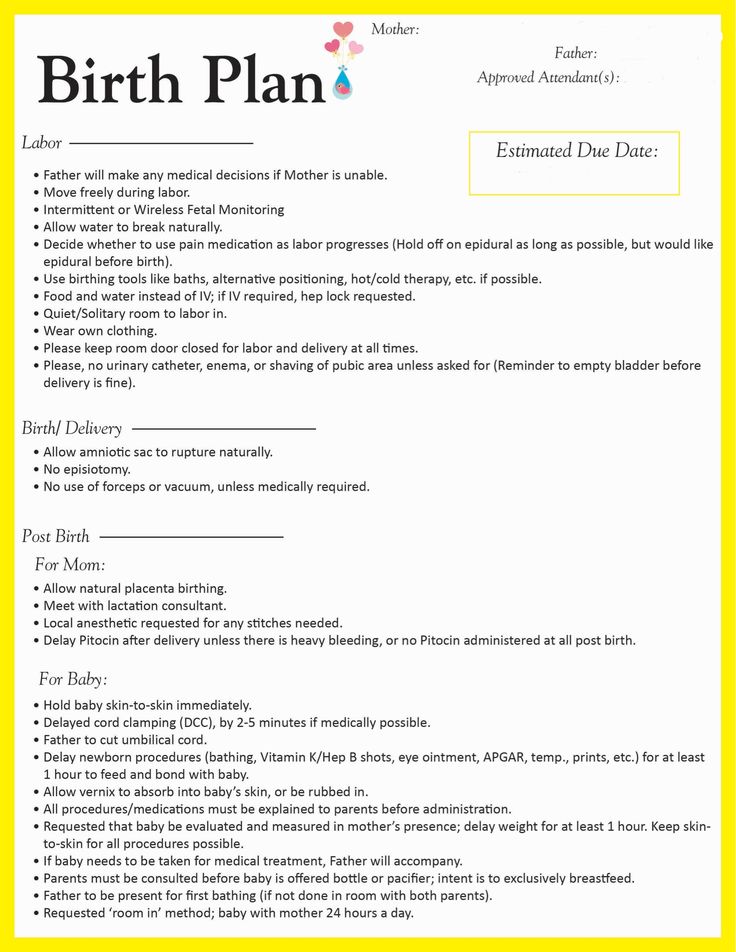
For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods. You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
Non-medical pain relief options for childbirth
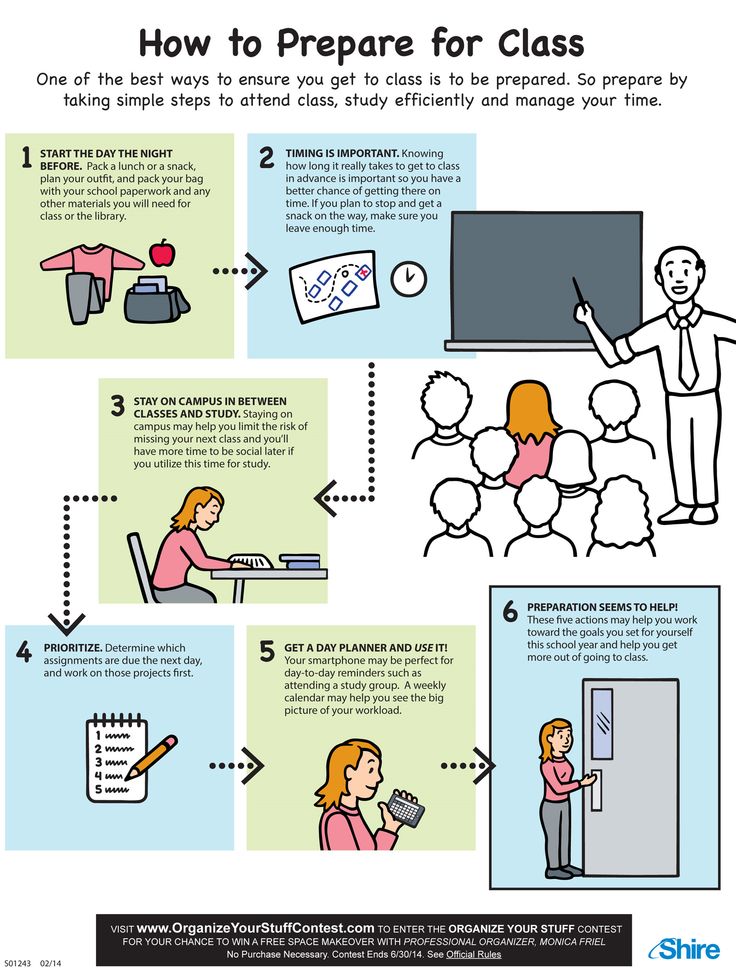
Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
- Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
- Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
- Breathing techniques may help you to ‘ride the waves’ of each contraction.
- Constant, close support from your partner (or a trusted friend or loved one) for the duration of labour can reduce anxiety.
- Using distractions like music can help to take your mind off the pain.
- Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
- Hypnosis, acupuncture and acupressure are areas in which there has been little research but these may be considered also.
Transcutaneous electrical nerve stimulation (TENS)
TENS is a technique in which nerves in the lower back are stimulated using a small hand-held device controlled by the woman. It has no known side effects for mother or baby and many women find it helpful either alone or in combination with other methods of pain relief.
Medical pain relief options for childbirth
The three main medical pain-relieving options for labour include:
- nitrous oxide
- pethidine
- epidural anaesthesia.
Nitrous oxide
Nitrous oxide, known as ‘laughing gas’, is mixed with oxygen and administered to the mother through a face mask or a tube held in the mouth. The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.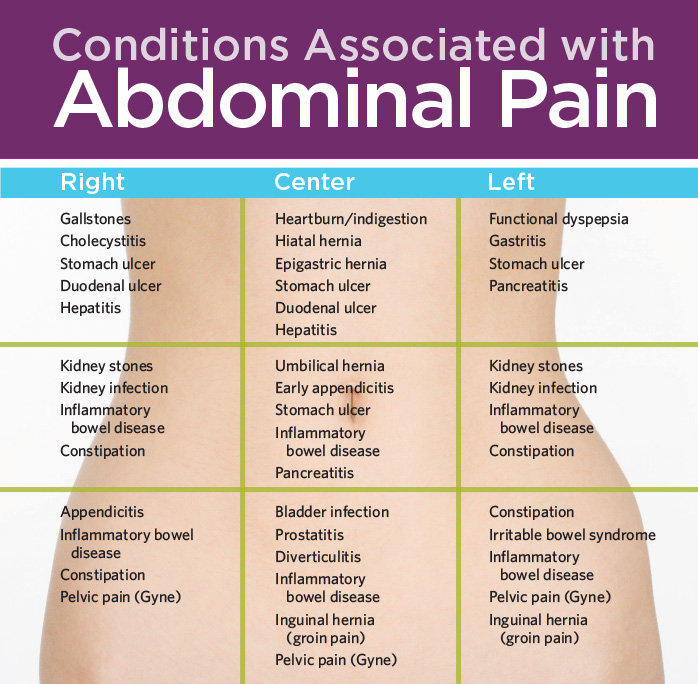
Nitrous oxide doesn’t stop the pain entirely, but takes the ‘edge’ off the intensity of each contraction. Many women prefer nitrous oxide because it allows them direct control – you can hold the mask yourself and take deep breaths whenever you feel the need.
Nitrous oxide doesn’t interfere with contractions and it doesn’t linger in either the woman’s or the baby’s body.
Possible problems with using nitrous oxide include:
- nausea and vomiting
- confusion and disorientation
- claustrophobic sensations from the face mask
- lack of pain relief – in some cases, nitrous oxide doesn’t offer any pain relief at all (this applies to around one-third of women).
Pethidine
Pethidine is a strong pain reliever (related to morphine and heroin), usually injected directly into a muscle in the buttock. It may also be administered intravenously (directly into a vein). Depending on various factors, the effect of pethidine can last anywhere from 2 to 4 hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Possible problems with pethidine for the mother include:
- giddiness and nausea
- disorientation and altered perception
- respiratory depression (reduced breathing)
- lack of pain relief, in some cases.
Possible problems with pethidine for the baby include:
- The unborn baby is exposed to the drug via the umbilical cord and may experience respiratory depression at birth, particularly if several doses are given or the baby delivers soon after a pethidine injection. This effect can be reversed by an injection given to the baby.
- The baby’s sucking reflex may also be depressed, as well as other normal reflexes. Debate persists over the effects of pethidine on newborns.
Epidural anaesthesia
Epidural injections are the most effective pain relief available. They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth.
Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Possible side effects and complications of epidural anaesthesia include:
- The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
- After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
- An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
- The lack of sensation in the lower body means that you will not be able to tell when you need to urinate. A urinary catheter will be inserted in most cases.
- Epidurals can lengthen the second stage of labour.
- The likelihood of having a normal vaginal delivery is reduced.
- If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
- Around one per cent of women experience headache immediately following the procedure.
- Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
- Some women experience pain or tenderness where the epidural was injected.
- Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
- Very rare complications include infection, blood clots and difficulty breathing.
An epidural does not:
- increase the length of the first stage of labour
- increase the likelihood of a caesarean section
- cause long-term backache.
Where to get help
- Your GP (doctor)
- Obstetrician
- Midwife
- Your local maternal and child health service
- Continuous support for women during childbirth, 2007, Cochrane Database of Systematic Reviews, Issue 2.
- Using water for pain relief during labour, 2007, The Royal Women’s Hospital, Melbourne.
- Epidural information, 2013, The Royal Women’s Hospital, Melbourne.
- Pain relief during labour and birth, Women’s and Children’s Health Network, Department of Health, South Australian Government.
- Epidural anaesthesia – side effects, NHS Choices, UK.
- Epidural anaesthesia, NHS, UK.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.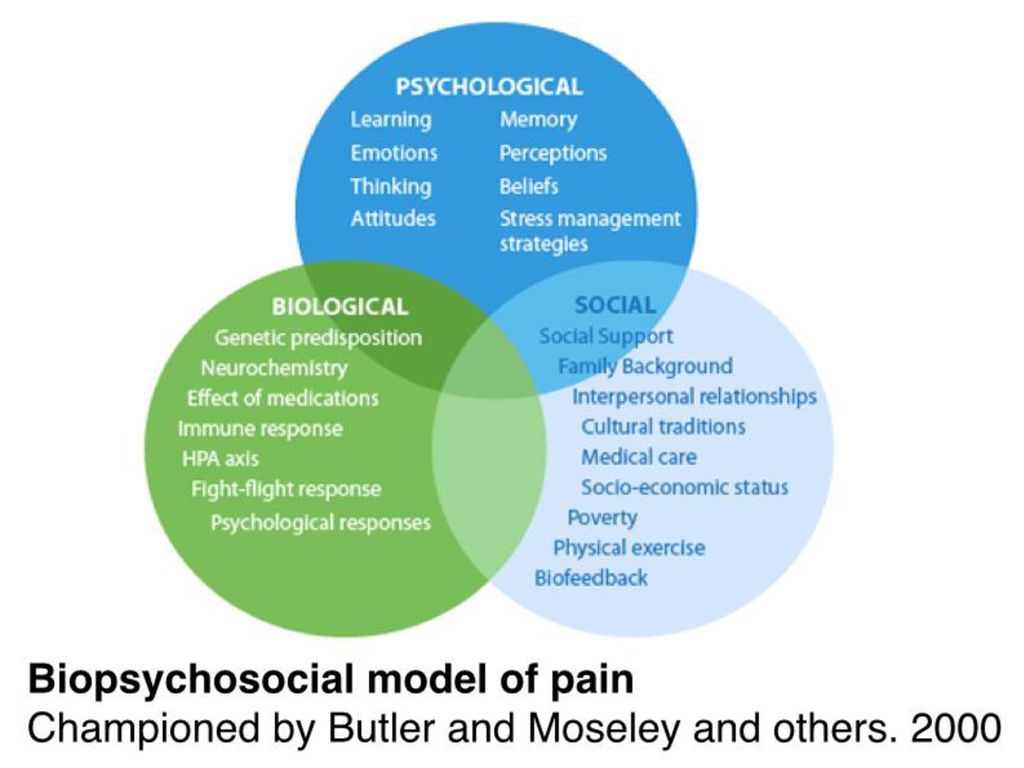 The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 31-08-2014
what are the dangers of painkillers and how to take them correctly?
Acute, aching, chronic and even phantom pain - pain can be so different, but in all cases it gives us a number of inconveniences. However, this is not the symptom with which we rush to the doctor: even if the pain is very severe, most people choose self-medication - there are drugs for this in every medicine cabinet today. For each type of pain, you can choose your own medicine, and as a rule, you do not need a prescription to buy it. But at the moment of a sharp attack, we rarely think about how to take painkillers correctly: the only thing that worries us is that this agony would stop soon.
For each type of pain, you can choose your own medicine, and as a rule, you do not need a prescription to buy it. But at the moment of a sharp attack, we rarely think about how to take painkillers correctly: the only thing that worries us is that this agony would stop soon.
Meanwhile, there are a number of rules that must be strictly observed, otherwise the consequences can be very deplorable. MIR 24 found out from doctors how many painkillers can be taken per day, in what cases a doctor's appointment is necessary, and what is the danger of an overdose.
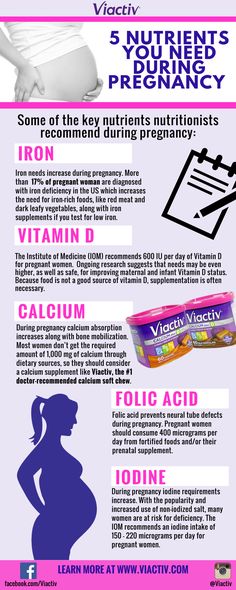
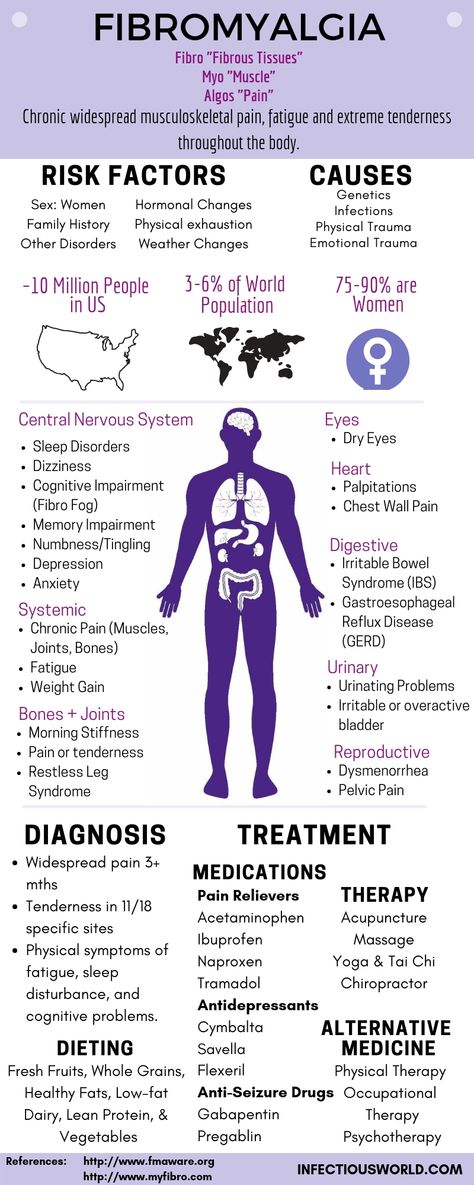
No more than 10 tablets per month
Pain should never be ignored, says general practitioner, senior medical consultant at Teledoctor24 Maria Menshikova . “Whether the pain is acute or chronic, it cannot be tolerated, and painkillers must be used to bring our pain perception system back to normal and ourselves back to life in the truest sense of the word. Now for pain relief, many drugs of various pharmacological groups are used. These are non-steroidal anti-inflammatory drugs (NSAIDs), anticonvulsants and antidepressants, as well as narcotic analgesics (morphine and other opiates and opioids),” the doctor lists.
These are non-steroidal anti-inflammatory drugs (NSAIDs), anticonvulsants and antidepressants, as well as narcotic analgesics (morphine and other opiates and opioids),” the doctor lists.
Rheumatologist Alexander Elonakov I am convinced that you should take any medication only as directed by a doctor. This also applies to painkillers. “The intake of such medicines is possible if a diagnosis is established and a doctor has been prescribed to relieve certain manifestations of the disease. At the same time, the patient should receive explanations about the main properties of the drugs, dosages and regimen of use, should be familiar with the typical possible side effects,” he said.
However, if you do decide to take a pill, take the trouble to read the instructions carefully, and also follow a few important rules. First of all, you should take care of protecting the stomach and liver.
“Practically all painkillers have a damaging effect on the gastric mucosa, so they should never be taken on an empty stomach,” says Maria Menshikova.
- Take the pills only with water, this is important. Sometimes, to enhance the effect, a person decides to increase the dose, drink two or three tablets. This is not a solution to the problem, but rather a way to get toxic damage to the liver, especially if this is practiced constantly.
The same applies to taking several analgesics of different groups at the same time. The annotation to any drug indicates a single and maximum daily dose. Under no circumstances should it be exceeded.
“It is recommended that you take no more than two tablets per day. Per month - no more than 10 tablets, since this category of drugs also has undesirable (side) reactions - abuse headache, aggressive effects on the gastric mucosa and duodenum, cardiotoxicity, nephrotoxicity, etc. ” – clarifies general practitioner "SM-Clinic" in Solnechnogorsk Elena Zhurkina .
Is it worth it?
Another question often arises: when should I take painkillers? Is it worth waiting until the pain becomes completely unbearable, or, on the contrary, take a pill in advance, when only the first signs of an impending illness loomed?
“Many studies have shown that attempts to endure pain have an extremely negative effect on the human body, as nerve cells die in the brain.
Few people know that the constant ignoring of pain can lead to various cardiovascular pathologies, reduced immunity, dystonia, and so on, ”says Elena Zhurkina .
“One of the most common situations is when a person endures pain to the last. There are no real arguments in favor of patience, not a single one, - confirms Maria Menshikova. - Remember: any pain should be stopped as soon as possible. I emphasize that if it is a pain in the heart or in the abdomen, a headache associated with an increase in pressure, you need to call an ambulance to rule out life-threatening conditions. Toothache, headache, in the back, during critical days, it is quite amenable to anesthesia.
For those who do not want to abuse medication, there are other means of pain relief - more gentle, but no less effective, adds the therapist.
“B vitamins have an analgesic effect and help with neuritis and neuralgia. A headache can stop bothering if you drink two glasses of water.
Pain on critical days (despite the fact that, in principle, it should not be, it is always a reason to consult a gynecologist) weakens when magnesium is taken a few days before the start of the cycle, ”advises the doctor.
Three forbidden pains
Pain, no matter how painful it may be for us, is of great benefit. It is she who signals about some damage in the body, forcing us to pay attention to our health.
“Pain sensations can be different: sudden and sharp, aching or pressing, growing or paroxysmal. It is important to remain calm and try to identify what exactly is causing the discomfort.
In some cases, the body is able to overcome mild pain on its own. And with minor discomfort, you do not need to immediately resort to the help of painkillers so that the body does not forget how to cope with pain on its own. Otherwise, any kind of pain will have to be stopped with pills, which will be harmful to health.
Severe, recurring, poorly self-treated pain requires seeking medical help,” warns Elena Zhurkina.
Like Maria Menshikova, she distinguishes three groups of situations in which it is strictly forbidden to take painkillers. Let's analyze them in more detail.
- Pain in the abdomen. Many important organs are located there, in which pathology could develop (pancreatitis, intestinal obstruction, appendicitis, hernia). Untimely medical intervention can lead to an aggravation of the situation. And drowning out the pain will not allow the doctor to establish its localization correctly. Stomach pain can be caused by dyspeptic disorder, in which case you should also immediately consult a doctor.
- Headache. In this case, first of all, you need to measure blood pressure, a deviation of the indicator to a smaller or larger side can cause pain. To remove discomfort, you need to normalize the pressure.
- Pain in the heart. The symptom cannot be ignored and conventional analgesics will not help. Shown are special cardiac remedies or an urgent call to an ambulance.
Up to and including death
Do not take painkillers as vitamins - these are very serious drugs, the illiterate use of which can lead to tragic results.
“Self-administration of painkillers or anti-inflammatory drugs can lead to temporary relief of symptoms and pain, and in the meantime, complications of unrecognized diseases may develop. Especially dangerous are purulent complications of the brain, diseases of the teeth, abdominal and thoracic cavities, in which a lethal outcome can occur in a few hours, ”warns Alexander Elonakov.
“Studies in neurology and psychiatry show that long-term abuse of NSAIDs can lead to hypertension, internal and external edema, kidney failure, and heart attack or stroke. Some types of painkillers can negatively affect the digestive organs, causing the development of ulcers, gastritis, erosion, etc. Long-term use of painkillers can impair vision, causing the mucous membrane of the eye to dry out, ”adds Elena Zhurkina.
In addition, some painkillers can thicken the blood and can cause blood clots and, as a result, blockage of blood vessels. The outcome in such cases is unfavorable: diabetes mellitus, thrombophlebitis, atherosclerosis, varicose veins and other serious diseases may develop.
“Excessive use of analgesics can disrupt the functioning of the liver: there will be a gradual accumulation of toxins in the body, because the organ will no longer be able to perform its work to the fullest. The result of slagging can be various dermatoses, skin rashes, allergic rashes, and so on, ”says the doctor.
How do you know if there is an excess of painkillers in the body? If you use painkillers for a long time and in large quantities, they can accumulate in the blood and tissues, causing a general deterioration in well-being, explains Elena Zhurkina.
The first signs of an overdose of painkillers are:
- noise or ringing in the ears;
- severe headache or migraine, which people also try to eliminate with analgesics, but as a rule there is no relief, and the situation only gets worse;
- the digestive system will not work properly, heartburn, constipation or diarrhea, bloating and flatulence may occur.
![]()
In conclusion, the doctor gives ten "golden" rules for taking painkillers. By following them, you can definitely improve your well-being, while not harming the body.
10 rules for taking painkillers
1. Take it on time.
2. For the elderly, it is better to replace the tablet form with a local preparation.
3. Avoid alcohol. While taking analgesics, alcoholic beverages are prohibited, as they can enhance or weaken the effect of the drug.
4. Do not take on an empty stomach. To protect the mucosa, it is advisable to drink at least kefir, if the instructions do not provide for use on an empty stomach.
5. Take the tablet properly with warm water or tea in sufficient quantity. It is better when the tablet enters the stomach well moistened.
6. Do not split the tablet in half. A reduced dose will not have an effect, and a damaged shell will not protect the stomach from irritation, and the main active ingredient will not reach the intestines.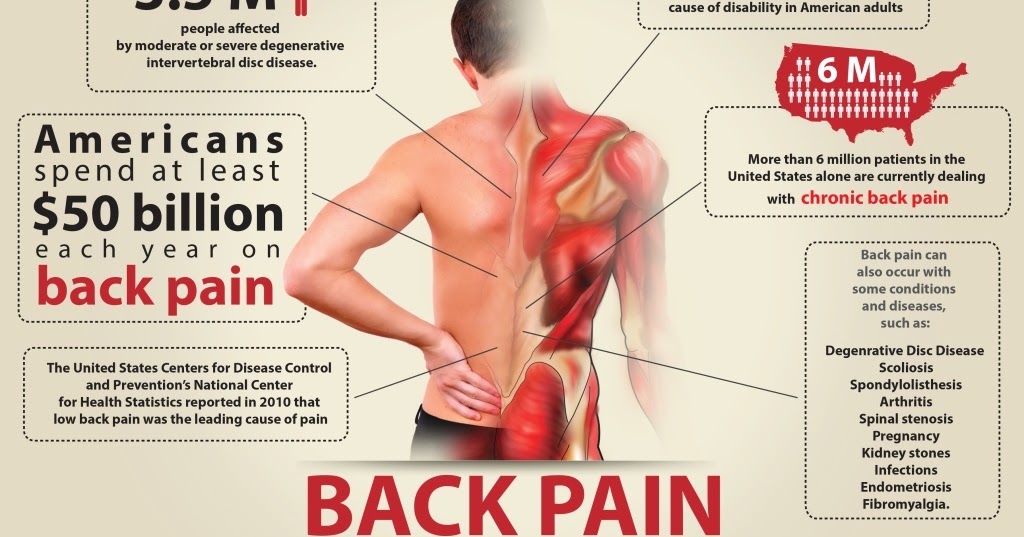
7. Strictly observe the dosage both for one application and per day, which is indicated in the instructions. Excess will lead to the manifestation of side effects and deterioration of the condition. As a rule, more than two tablets at a time are not allowed.
8. Do not combine drugs from different groups of analgesics.
9. Do not take the same drug frequently to avoid addiction and loss of effect from the use.
10. Do not use expired products. Expired drugs are deadly.
“When purchasing another package of painkillers, one should not forget that the medicine eliminates only the pain syndrome, but does not affect the root cause of the pain in any way. To identify the causes of pain and discomfort, it is necessary to visit a doctor, pass all the necessary tests and carry out a number of diagnostic measures, ”concludes Elena Zhurkina.
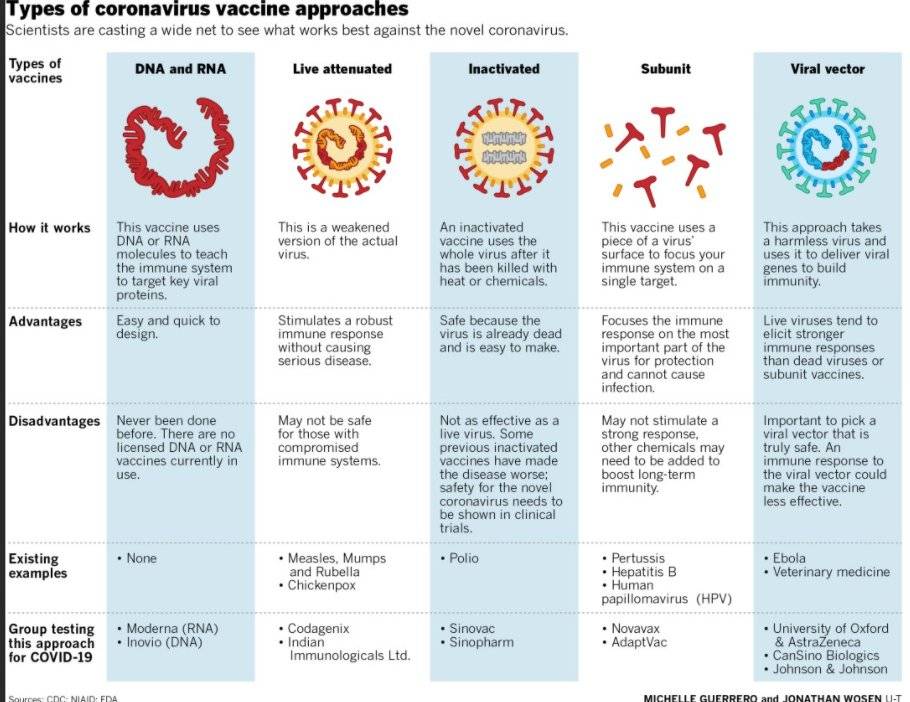
New painkiller: 100 times stronger than morphine and non-addictive
- Nikolai Voronin
- Science and Technology Correspondent
Subscribe to our Context newsletter: it will help you understand the events.
Image copyright Getty Images
American scientists have developed a drug that could revolutionize anesthesia. The new painkiller is much more effective than morphine, but it does not have its side effects, the main of which is the development of dependence on the drug.
The substance, called AT-121, has already been tested on animals, including higher primates, with impressive results.
- Opioids: why so many Americans are addicted to them
"In addition, this substance effectively blocks the potential abuse of medicinal opioids, so we hope that it can be used to treat not only pain, but also opioid dependence," said one of the developers of the drug, professor of pharmacology at Wake Forest University Mei Chuan Ko.
Dangerous pleasure
Opioid drugs are the most effective anesthetic today and are widely used to treat people with chronic pain of various origins.
However, by acting on pain-reducing receptors in the brain, these drugs simultaneously stimulate the so-called pleasure center. With regular use of opioids, patients get used to the feeling of pleasure, and they develop dependence on the drug.
- Scientists have tested a new painkiller made from snail venom
- FIFA: painkillers can harm players dose of pain medication for each patient is almost impossible.
Image copyright Wake Forest University
Image captionThe substance, called AT-121, has already been tested in animals, including higher primates, with impressive results
Over 2 million people in the United States abuse medical opioids. Last year, the US Secretary of Health declared a state of emergency to curb the national opioid crisis.
- Experts: painkillers increase heart failure risk
- Pain inequality: why doctors treat women's complaints differently
For decades, pharmacologists have been trying to create a substance that can block pain without affecting the pleasure center.
But this turned out to be a very difficult task.
However, several prototypes of such a drug have been developed. And the new drug seems to be a real breakthrough in this area.
"Our developed AT-121 combines both of these functions in a balanced way in one molecule, and we believe this is a much better pharmaceutical strategy than taking two drugs at the same time," explains Ko.
"Promising approach"
The results of animal experiments are impressive. In Rhesus monkeys, the analgesic effect of AT-121 was comparable to that of morphine even at a dosage 100 times lower.
Not only was it non-addictive, but it also reduced drug addiction in animals trained to take the opioid oxycodone.
Image copyright, Getty Images
Image caption,For decades, pharmacologists have tried to create a substance that would block pain without affecting the pleasure center
person.
 However, this possibility is high.
However, this possibility is high. Experiments on primates are the last stage before clinical trials of any drugs in humans, and scientists are very optimistic.
- Pain relief for critically ill patients: is the situation changing?
- Scientists: being in love can be a pain reliever
"The overall results are impressive," says University of North Carolina pharmacology professor Brian Roth. "This is certainly a very promising and promising approach."
If clinical trials are successful, AT-121 could show another significant advantage over drug opioids.
In the course of experiments on monkeys, the new substance, even in large doses, did not lead to breathing difficulties in the experimental subjects and did not cause problems with cardiac activity.
And this gives scientists hope that there will be no serious overdose problems with the use of a new painkiller.