Bladder incontinence pregnancy
Incontinence During Pregnancy and After Childbirth
Written by WebMD Editorial Contributors
In this Article
- What Types of Incontinence Are Experienced During and After Pregnancy?
- How Is Urinary Incontinence During Pregnancy Treated?
- What Are Kegel Exercises?
- When Should You See a Health Care Professional About Incontinence?
During pregnancy, many women experience at least some degree of urinary incontinence, which is the involuntary loss of urine. The incontinence may be mild and infrequent for some pregnant women. But it can be more severe for others. Age and body mass index are risk factors for pregnancy incontinence, according to one study.
Incontinence can continue after pregnancy and may not be present right after childbirth. Some women do not have bladder problems until they reach their 40s.
What Types of Incontinence Are Experienced During and After Pregnancy?
The kind of incontinence experienced during pregnancy is usually stress incontinence (SI). Stress incontinence is the loss of urine caused by increased pressure on the bladder. In stress incontinence, the bladder sphincter does not function well enough to hold in urine.
Urinary incontinence during pregnancy can also be the result of an overactive bladder. Women who have an overactive bladder (OAB) need to urinate more than usual because their bladders have uncontrollable spasms. In addition, the muscles surrounding the urethra -- the tube through which urine passes from the bladder -- can be affected. These muscles are meant to prevent urine from leaving the body, but they may be "overridden" if the bladder has a strong contraction.
The bladder sphincter is a muscular valve that lies at the bottom of the bladder. It works to control the flow of urine. In pregnancy, the expanding uterus puts pressure on the bladder. The muscles in the bladder sphincter and in the pelvic floor can be overwhelmed by the extra stress or pressure on the bladder. Urine may leak out of the bladder when there is additional pressure exerted -- for example, when a pregnant woman coughs or sneezes.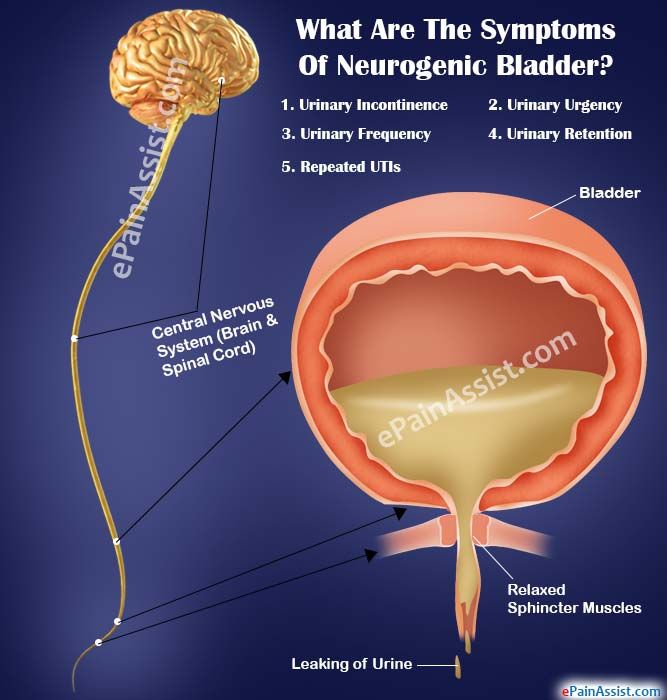
After pregnancy, incontinence problems may continue, because childbirth weakens the pelvic floor muscles, which can cause an overactive bladder. Pregnancy and childbirth also may contribute to bladder control problems because of the following conditions:
- Damage to the nerves that control the bladder
- The fact that the urethra and bladder have moved during pregnancy
- An episiotomy, a cut made in the pelvic floor muscle during delivery of a baby to allow the fetus to come out more easily
How Is Urinary Incontinence During Pregnancy Treated?
Behavioral methods such as timed voiding and bladder training can be helpful in treating urinary incontinence during and after pregnancy. These techniques are often used first and can be done at home. The changes in habits that behavioral methods involve do not have serious side effects.
To practice timed voiding, you use a chart or diary to record the times that you urinate and when you leak urine. This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
In bladder training, you "stretch out" the intervals at which you go to the bathroom by waiting a little longer before you go. For instance, to start, you can plan to go to the bathroom once an hour. You follow this pattern for a period of time. Then you change the schedule to going to the bathroom every 90 minutes. Eventually you change it to every two hours and continue to lengthen the time until you are up to three or four hours between bathroom visits.
Another method is to try to postpone a visit to the bathroom for 15 minutes with the first urge. Do this for two weeks and then increase the amount of time to 30 minutes and so on.
In certain cases, a woman may use a pessary, a device to block the urethra or to strengthen the pelvic muscles. In addition, medications also can be helpful in controlling muscle spasms in the bladder or strengthening the muscles in the urethra.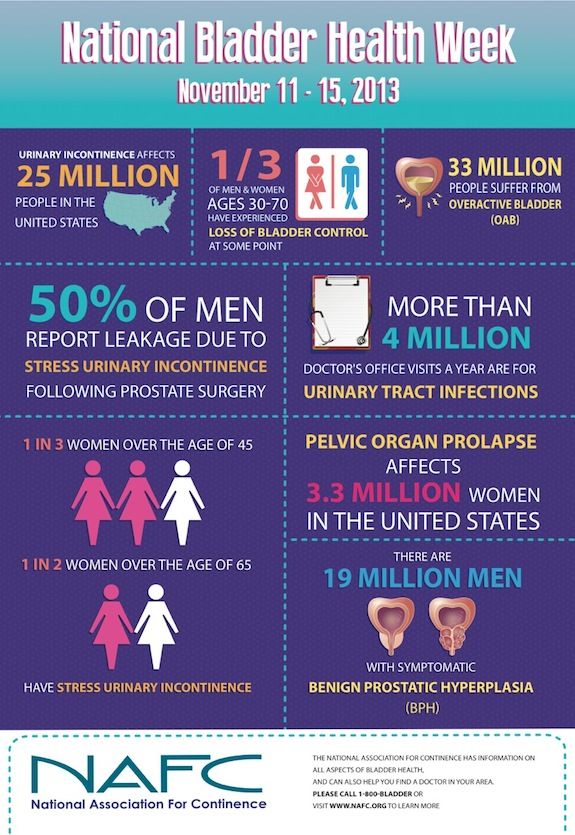 Some drugs can help to relax an overactive bladder.
Some drugs can help to relax an overactive bladder.
What Are Kegel Exercises?
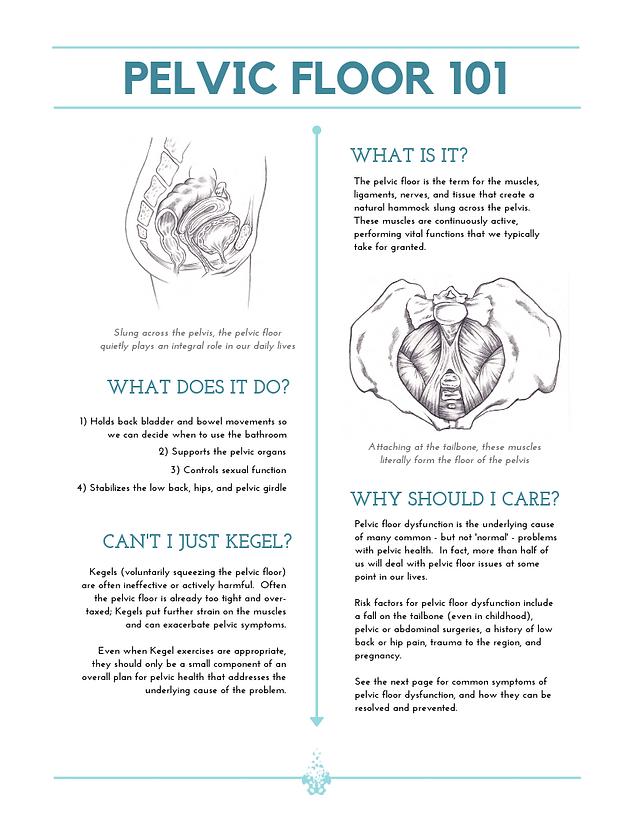
Kegel exercises are another method that can be used to help control urinary incontinence. These exercises help tighten and strengthen the muscles in the pelvic floor. Strengthening the pelvic floor muscles can improve the function of the urethra and rectal sphincter.
One way to find the Kegel muscles is to sit on the toilet and begin urinating. Then stop urinating mid-stream. The muscles that you use to stop the flow of urine are the Kegel muscles. Another way to help locate the Kegel muscles is to insert a finger into the vagina and try to make the muscles around your finger tighter.
To perform Kegel exercises, you should:
- Keep your abdominal, thigh, and buttocks muscles relaxed.
- Tighten the pelvic floor muscles.
- Hold the muscles until you count to 10.
- Relax the pelvic floor muscles until you count to 10.
Do 10 Kegel exercises in the morning, afternoon, and at night.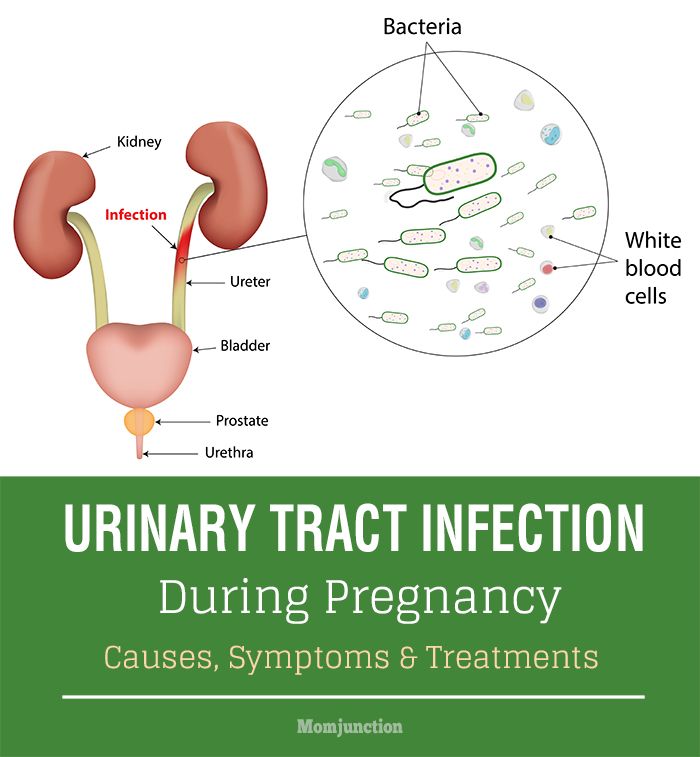 They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
When Should You See a Health Care Professional About Incontinence?
Talk to your doctor if you still have bladder problems six weeks after delivery. Accidental leaking of urine may mean that you have another medical condition. The loss of bladder control should be treated or it can become a long-term problem.
Pregnancy Incontinence Prevention and Treatment Methods
The long-awaited plus sign shows itself on your pregnancy test, you share the exciting news with your family and friends, and begin analyzing every little change your body makes in the weeks to follow.
Pregnancy is an incredible time of transformation for a woman’s body with more than 90 percent of women reporting they experience symptoms by the first eight weeks. While some symptoms may be welcome (like missed periods and food cravings), others are more challenging to manage like nausea, fatigue, and bladder leakage.
Women should not hesitate to ask questions or share concerns with their provider about pregnancy symptoms. Seeking guidance and professional support is especially important when a topic is confusing or varies greatly from woman to woman like urinary incontinence, incontinence after pregnancy, and incontinence treatment and prevention recommendations.
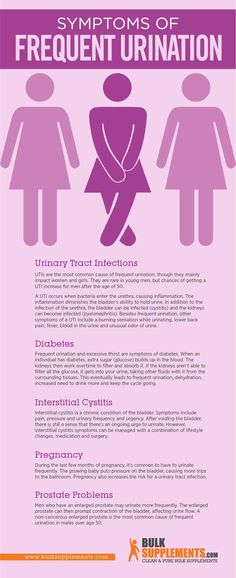
It is not uncommon to have questions about the risks of incontinence during or after pregnancy. However, it is important to first understand the types of urinary incontinence, which include:
- Stress: Loss of urine due to physical pressure on the bladder
- Urgency: Loss of urine due to an urgent need to urinate (commonly caused by bladder contractions)
- Mixed: A combination of stress and urgency incontinence
- Transient: Loss of urine due to medication or a temporary condition such as a urinary tract infection or constipation
What is Pregnancy Incontinence?
During the early stages of pregnancy, blood flow to the kidneys can increase 35 to 60 percent. This extra blood flow can make the kidneys produce up to 25 percent more urine soon after conception. Increased urine production is at its height at 9 to 16 weeks of pregnancy, and tapers down from there.
This extra blood flow can make the kidneys produce up to 25 percent more urine soon after conception. Increased urine production is at its height at 9 to 16 weeks of pregnancy, and tapers down from there.
Do you leak a bit of urine every time you cough, sneeze, exercise, or laugh? You aren’t alone. A growing uterus places pressure on the bladder and may result in the need to pass urine frequently, and at times, incontinence. As your baby grows during pregnancy, he or she pushes down on your bladder, urethra, and pelvic floor muscles. This pressure can weaken the pelvic floor muscles and lead to incontinence or problems passing urine. Changing hormones can also have an effect on the lining of your bladder and urethra. The good news is… most bladder leakage or control problems go away after childbirth when the muscles have had time to heal.
It is important to note that it is not recommended to restrict fluids during this time. It is essential that you and your growing baby stay hydrated by drinking at least six to eight glasses of fluids each day to maintain a healthy pregnancy.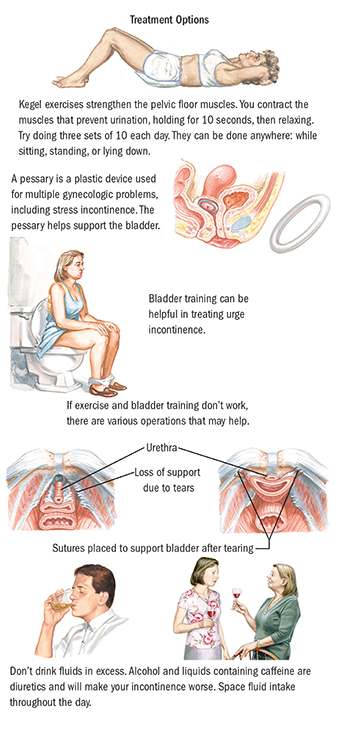 Drinking less than the recommended amount may result in dehydration. If the need to go to the bathroom keeps you up at night, try drinking more fluids during the day and cutting back a few hours before you go to bed.
Drinking less than the recommended amount may result in dehydration. If the need to go to the bathroom keeps you up at night, try drinking more fluids during the day and cutting back a few hours before you go to bed.
What are the Risk Factors for Pregnancy Incontinence?
When you’re pregnant, pelvic floor muscles are working overtime. That said, most women who are carrying a child are at risk for some form of pregnancy incontinence. Women who have had an overactive bladder or urgency incontinence prior to pregnancy will most likely have symptoms that continue or worsen during pregnancy.
Other risk factors include:
- Advanced maternal age
- Being overweight
- Previous vaginal delivery
- Previous pelvic surgery
- Smoking, which leads to chronic coughing
- Neurological diseases
- Diabetes
What Causes Urinary Incontinence After Pregnancy?
It may surprise you to learn that it doesn’t matter what type of delivery you have (vaginal or cesarean section) - women who have given birth have much higher rates of post-pregnancy stress incontinence than those who have never had a baby.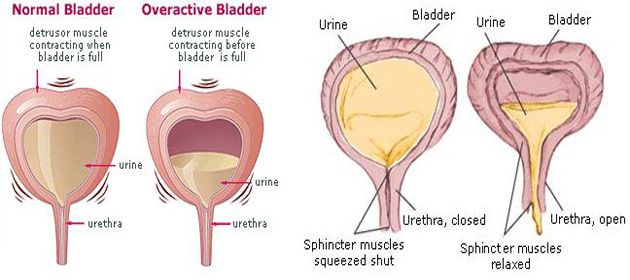
Simply explained, giving birth can contribute to incontinence after pregnancy. The American Congress of Obstetricians and Gynecologists has found that cesarean delivery reduces incontinence during the first year, but benefits are diminished two to five years after delivery.
A normal labor and vaginal delivery can weaken the pelvic floor muscles and damage the nerves that control the bladder. A long labor and prolonged pushing can increase the likelihood of immediate pelvic floor muscle weakness following delivery. Additionally, a uterus shrinks in the weeks following delivery and as it sits directly on the bladder, compression can make it more difficult to control the flow of urine.
Loss of bladder control is also caused by pelvic organ prolapse (slipping down) that can occur after childbirth. In this case, the pelvic muscles stretch and become weaker during pregnancy and vaginal delivery. If the muscles do not provide enough support, the bladder may move down or sag, causing mobility of the urethra, leading to incontinence with increased abdominal pressure.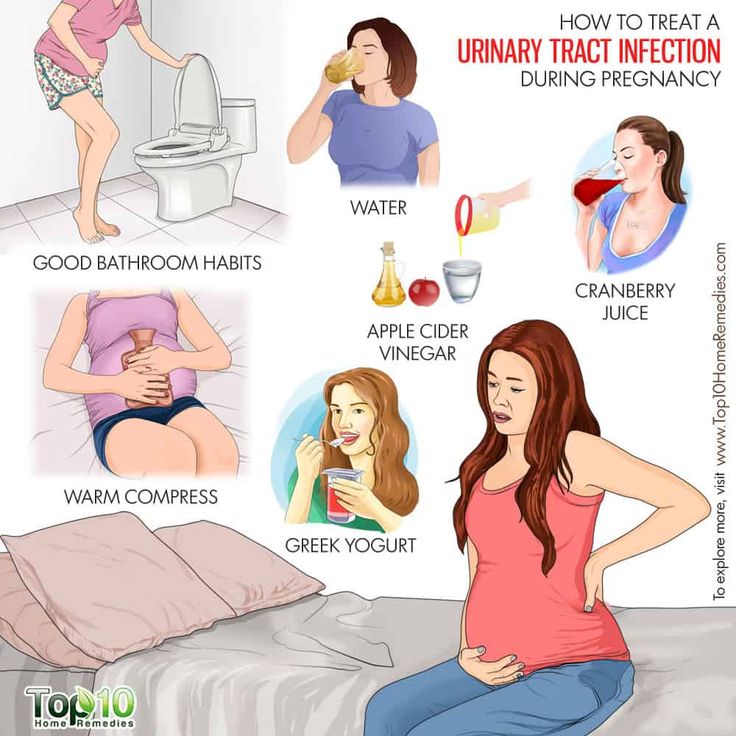
How Long Does Incontinence Last After Giving Birth?
Ready for some good news?
Most women’s incontinence symptoms go away in the days or weeks after their baby is born. Bladder leakage that happens as a result of labor and delivery tends to diminish after the muscles have had time to heal. For some women, leaking may continue to get worse. If this is the case, incontinence can be managed with certain exercises such as Kegels, and other methods including bladder retraining, weight loss, and more.
If you have concerns following the delivery of your baby, and lifestyle changes haven’t worked to improve incontinence issues six or more weeks after delivery, speak with your doctor about treatments and medications that are available to help.
It’s important to understand that it can take three to six months, or longer for some women, to regain complete bladder control. Be patient and learn the steps you can take to make the process go faster.
How do I Prevent Incontinence After Pregnancy?
Pregnancy incontinence is a normal occurrence following the delivery of a baby; however, there are some ways you can help prevent it or improve bladder control.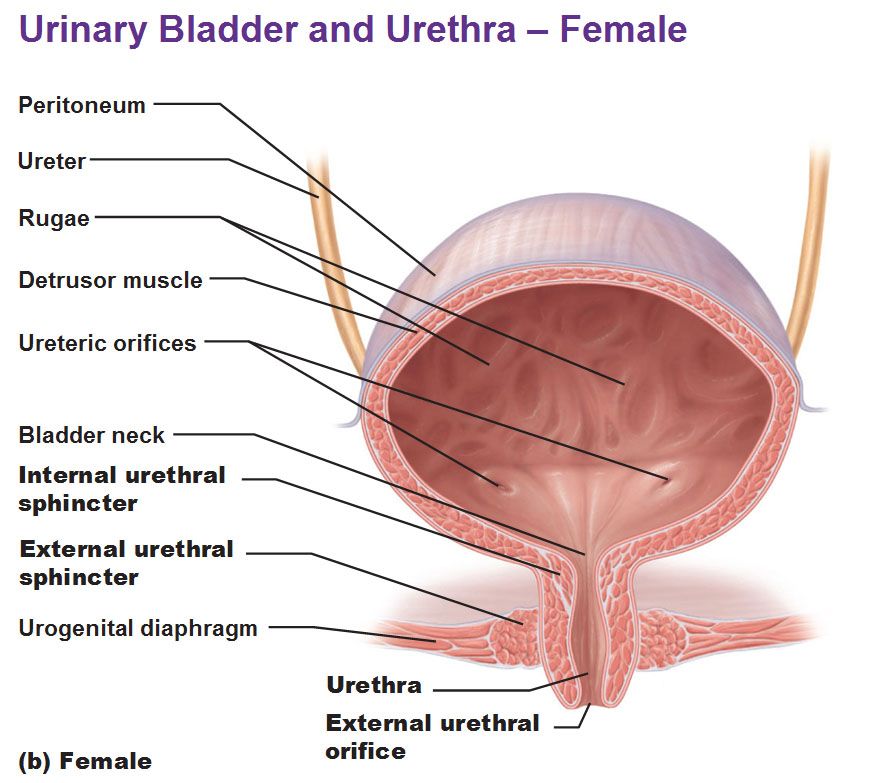
- Take your time while using the toilet. When urine is allowed to flow at its own speed, you aren’t using your pelvic floor to push it out.
- Treat urinary tract infections (UTIs) promptly. UTIs irritate the bladder lining and it’s important to seek treatment immediately if you have symptoms.
- Document when you have bladder leakage issues. This will help with planning trips to the bathroom and provide information to your doctor.
- Maintain a healthy weight. Excess weight can put added strain on the muscles of the pelvic floor.
- Don’t smoke. A chronic cough because of smoking weakens the pelvic floor and contributes to incontinence.
- Do pelvic floor muscle or Kegel exercises. They are safe and effective before, during, and after pregnancy.
- Avoid carbonated and caffeinated drinks such as soda, coffee, or tea. These types of beverages can make you feel like you have to use the bathroom more often.
- Talk to a trusted obstetrician about your concerns and to seek diagnosis or treatment advice.

What are Some Pregnancy Incontinence Treatments?
When considering treatment options for pregnancy incontinence, the first course of action should incorporate lifestyle changes and bladder management. If these steps don’t improve your symptoms, your doctor may recommend other treatment options depending on what type of incontinence you are experiencing. These options may include:
- Control of pelvic floor muscles- Kegel exercises.
- Elimination of bladder irritant food and beverages.
- A Pessary inserted into the vagina to support the urethra, preventing urine leakage.
- Urethral surgical sling that involves placing a sling around the urethra to lift it back into a normal position.
- Bladder support “tampons” that support the urethra from leaks.
- Medications to help overactive bladder.
- Bladder retraining tactics for urgency incontinence.
The most important factor is to remember to be patient - it can take a month or longer for certain treatments to begin working.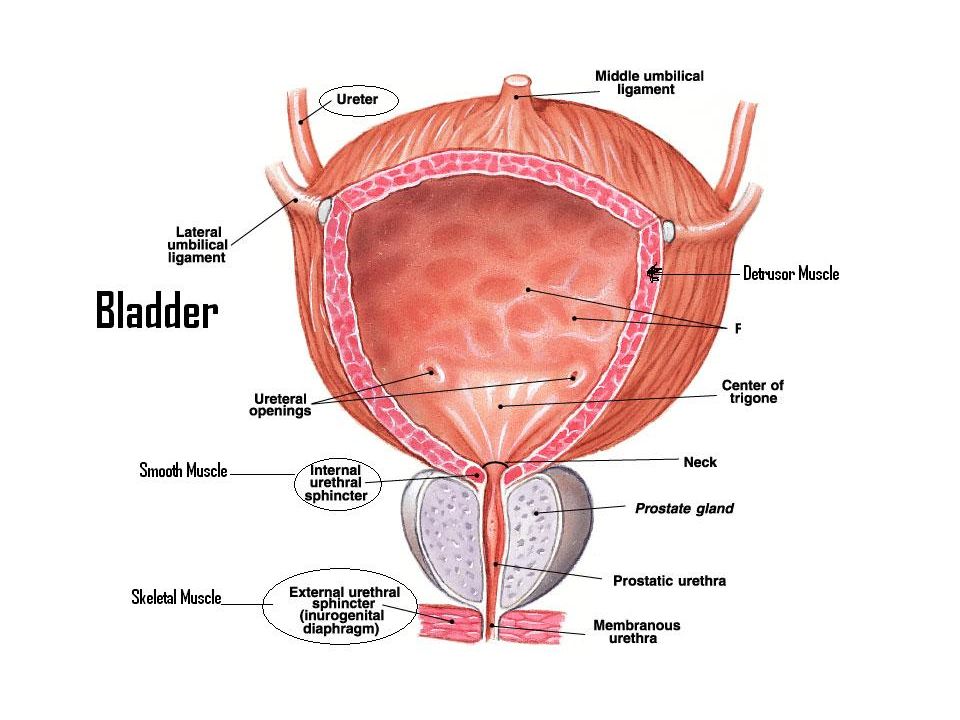
Exercises for Incontinence After Childbirth
There are several simple exercises women can do in the comfort of their own home to strengthen pelvic floor muscles and improve bladder control. Consider these incontinence exercises after childbirth.
Kegel Exercises
Kegels (key-ghels) are an easy exercise that can be done pretty much anywhere without the need to work up a sweat. If you’re unfamiliar with this exercise, begin by identifying your pelvic floor muscles. This can be done in the restroom and by holding in your urine mid-flow. Contracting your muscles to obtain that hold is called a kegel. Please note: Stopping flow mid-flow should not become a habit as it can cause damage to the muscles over time.
Once you’ve identified those muscles, you are ready to start adding kegel sessions to your daily schedule. Kegels can be done laying down or sitting down, and should only focus on tightening your pelvic floor muscles, not your abdomen, thighs, or buttock.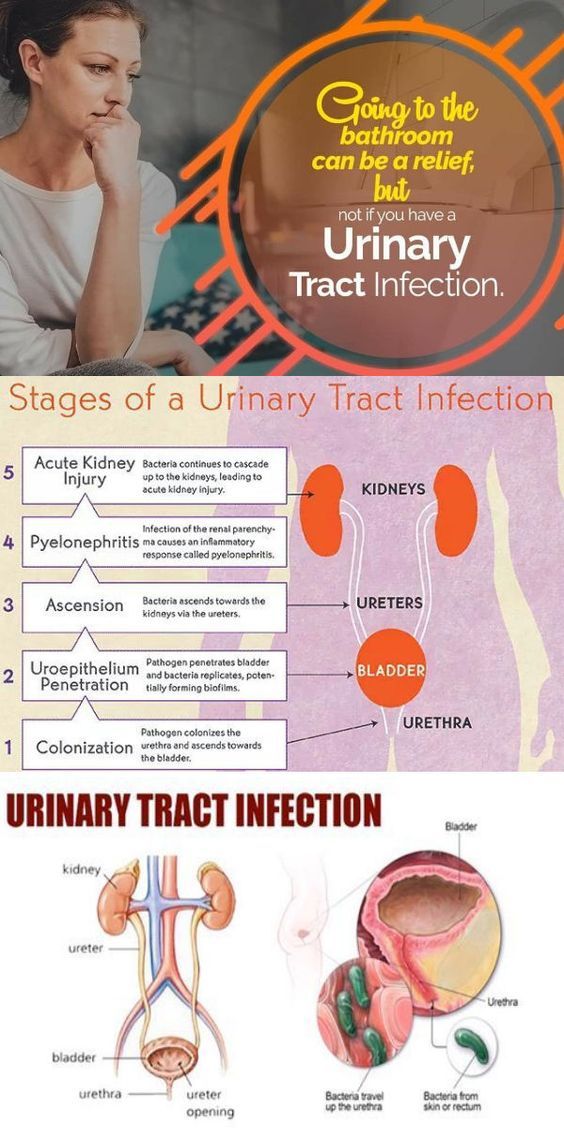
Step 1: Contract your pelvic floor muscles for 3-5 seconds.
Step 2: Relax your muscles for another 3-5 seconds.
Step 3: Repeat.
Depending on your level of urinary incontinence after childbirth, the amount of recommended sets of kegels a day will vary. For starters, try doing multiple sets of kegels three times a day. Quick tip! One patient mentioned she always does kegel exercises when she’s stopped at a red light!
Bridging Exercise
This exercise may be more familiar to most women as it is a common yoga pose. Along with strengthening your pelvic muscles, it’s also good for hip mobility and strengthening your glutes.
Step 1: Lay down a blanket or yoga mat for comfort.
Step 2: Lay flat on your back with your knees bent and feet firmly on the floor hip-width apart, arms should be resting by your sides.
Step 3: Draw in your pelvic floor muscles and abdominals and lift your buttocks in air.
Step 4: Hold this position using your abdominals, leg muscles, and glutes for three slow breaths, be mindful not to use your neck and shoulders.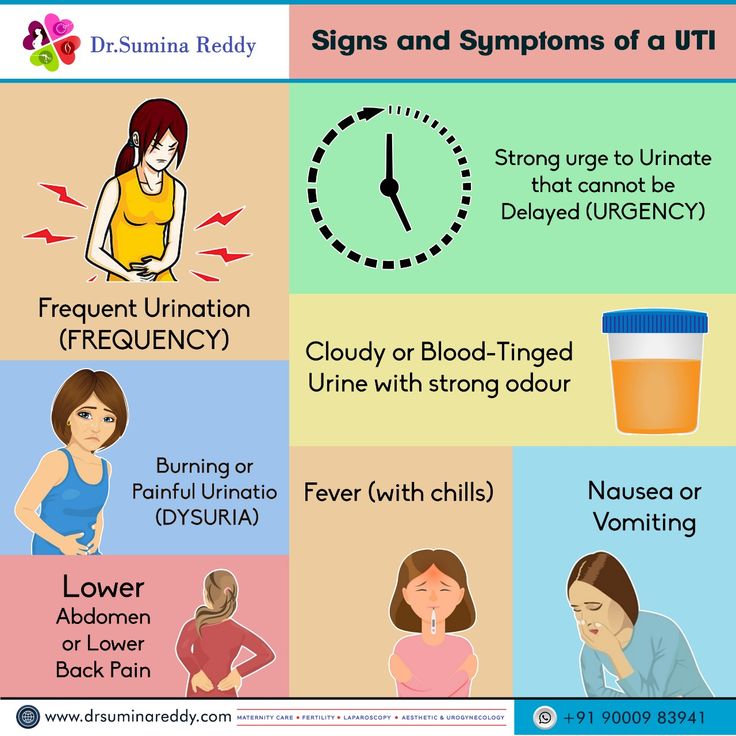
Step 5: Lower down slowly. Repeat 10 times, or to your comfort level.
Bird-Dog Exercise
Position yourself on an exercise mat or cushioned surface on all fours, with your knees hip-width apart and hands firmly on the ground. Tighten your abdominal muscles.
Step 1: Extend one arm forward and at the same time, extend your opposite leg, trying to create a straight line from your extended hand to the extended foot. Keep your hips squared to the ground.
Step 2: Hold for a few seconds, then return to your hands and knees. Keep your abs engaged throughout the entire exercise and work to minimize any extra motion in your hips during the weight shift.
Step 3: Switch to the other side.
Aim to complete 5 reps on each side or 10 reps total. Add additional sets of 10 exercises for a maximum of three sets of 10. As a variation, you can do a set of 10 bird-dogs on one side, then switch to the other side.
Knee Fold Exercise
Knee folds are another great exercise to help with incontinence after pregnancy. These begin with the same movements as the bridge exercise mentioned above.
These begin with the same movements as the bridge exercise mentioned above.
Step 1: Lay down a blanket or yoga mat for comfort.
Step 2: Lay flat on your back with your knees bent and feet firmly on the floor hip-width apart, arms should be resting by your sides.
Step 3: Engage your abdominal and pelvic floor muscles.
Step 4: Slowly lift one leg at the hip and bring the knee joint straight above the hip joint, creating a 90-degree angle at the knee to your ankle.
Step 5: Slowly bring the knee back down.
Step 6: Repeat steps, alternating between legs, and complete 10 on each side.
Looking for a little extra challenge? After bringing up the first knee, keep it there as you bring up the second knee. Hold both while engaging your core.
How Do I Find the Right Doctor?
There are many important aspects to finding the right medical provider. The most critical element is to ask about the doctor’s viewpoint on concerns that are most important to you.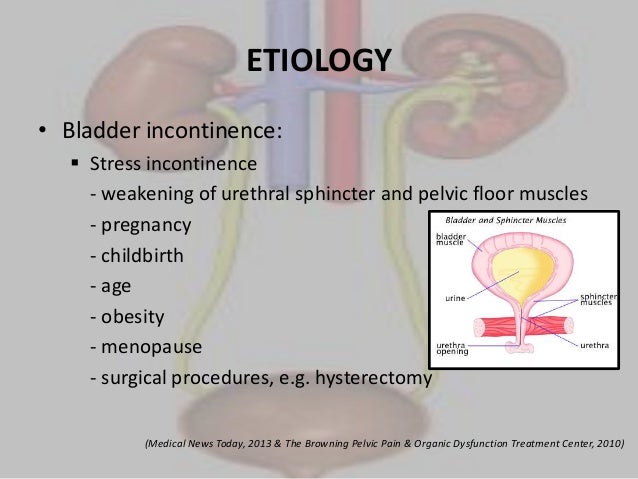 You can never fully predict what pregnancy, labor, delivery, and life will bring. However, you can learn about your doctor’s approach to care and how their team will respond in situations pertaining to your health.
You can never fully predict what pregnancy, labor, delivery, and life will bring. However, you can learn about your doctor’s approach to care and how their team will respond in situations pertaining to your health.
At Moreland OB-GYN, we specialize in women’s health care and always prioritize the needs of our patients. Do you have a question you’d like answered? Our team is a trusted source for information - connect with us here.
Home - Seni
Home - Seni- Seni Club
- Where to buy
- Request a free sample
- Contacts
- Change country
- menu
Urological pads for women with mild to moderate urinary incontinence
More details
Urological pads for women with mild to moderate urinary incontinence
Urological inserts for men with mild to moderate urinary incontinence
More details
Urological inserts for men with mild to moderate urinary incontinence
A wide range of absorbent products for people in need of reliable protection.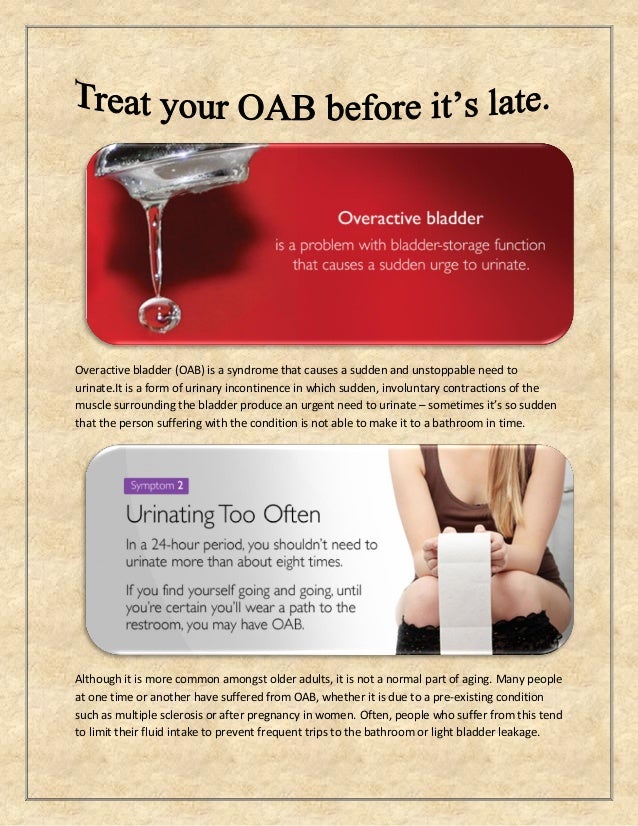
More
A wide range of absorbent products for people in need of reliable protection.
Absorbent briefs
Absorbent briefs for active people who need comfortable protection.
More
Absorbent briefs for active people who need comfortable protection.
skin care
Daily skin care products
More details
Cosmetics for daily skin care
A well-chosen product not only ensures the comfort of the person who uses it, but also avoids unnecessary costs.
Find product
It is important to choose the correct size of the product. An incorrectly selected size can lead not only to leakage, but even harm to health. Use the special "form" to select the correct size.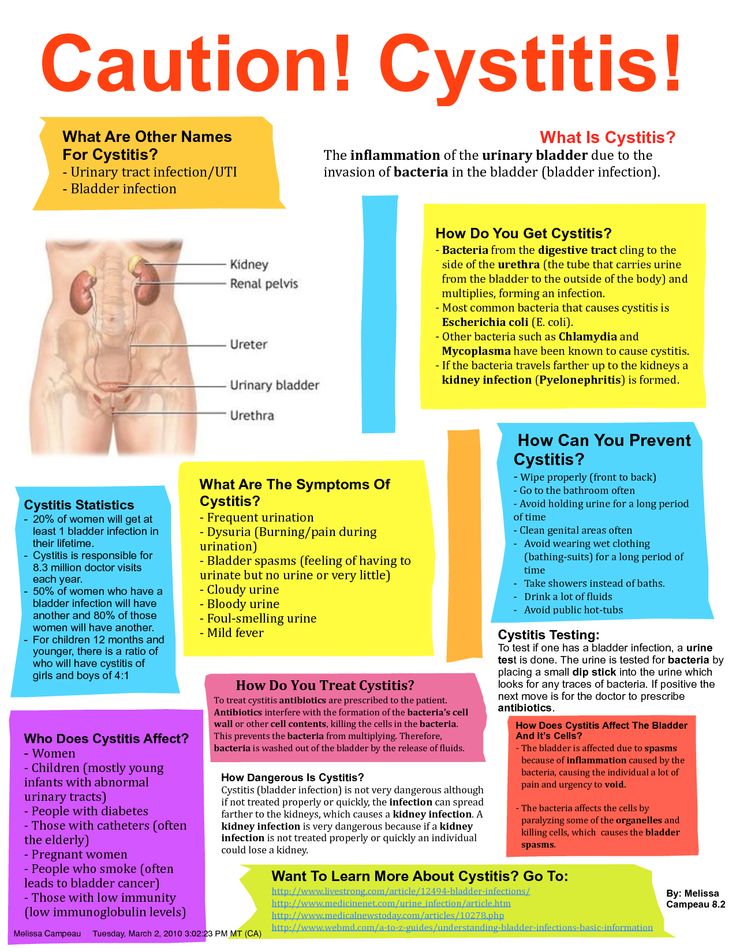
Find size
Seni care products have been helping to properly care for skin that needs especially delicate care for many years. Depending on the purpose, conditions of use and individual characteristics of the skin, seni care cosmetics are conventionally divided into 2 areas: for specialized care and for the care of dry and sensitive skin. Informative packaging design, convenient color identification with special symbols make it easy to choose the right cosmetic product.
Read more
Why senicare?
Compliance with personal hygiene rules is of no small importance in the prevention of inflammatory diseases.
Read more
Take care of yourself
The illness of a loved one, whether a child, parent or other family member, changes many aspects of the lives of all those involved.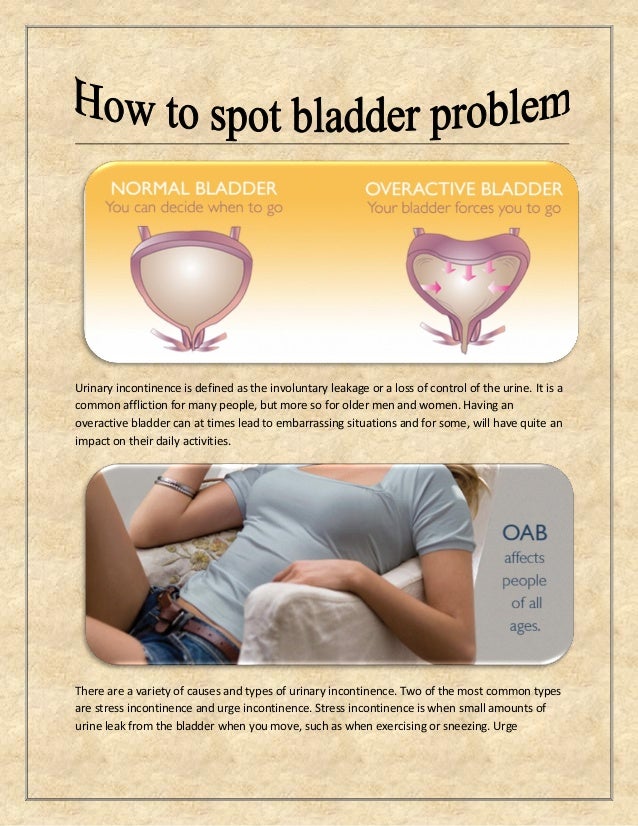
Read more
MoreThe SeniControl mobile app is a handy tool with which you can easily monitor your urinary incontinence. The application will assess the degree of urinary incontinence and recommend the best urological product that will suit your needs.
Read more
Application available at:
What causes urinary incontinence in pregnant women
One of the signs of pregnancy is frequent urination. In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women.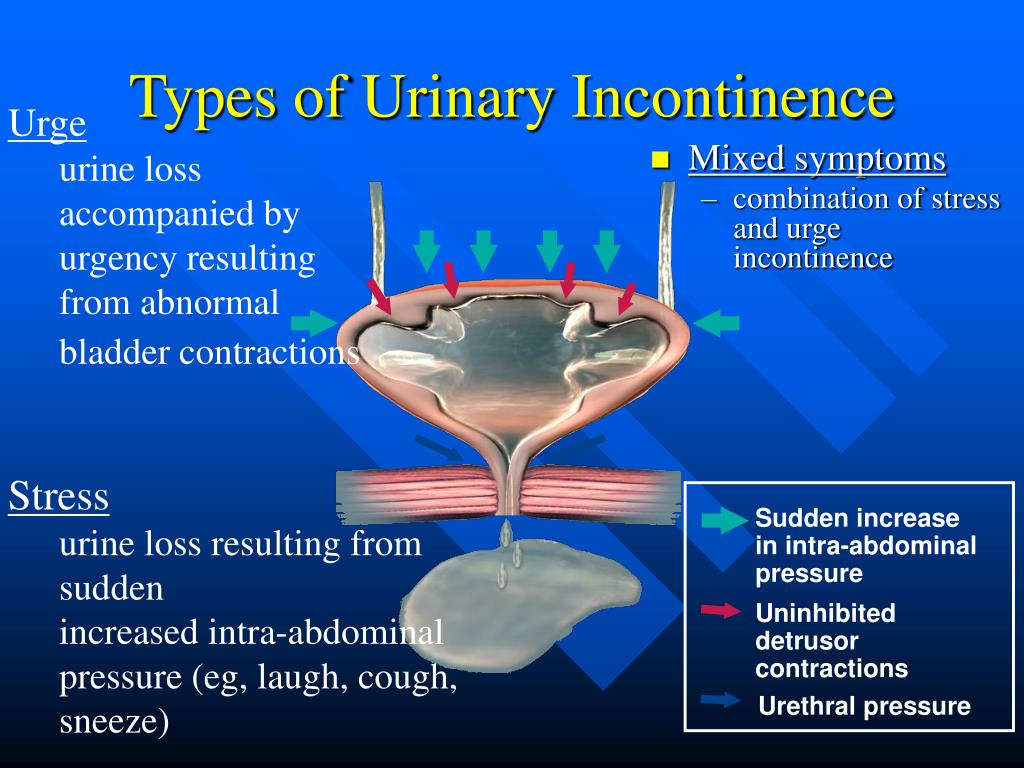 The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor.
The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor.
Types of urinary incontinence during pregnancy
Most often, 3 types of urinary incontinence in a pregnant woman appear, and in each case there are characteristic signs.
- Stress. It manifests itself with the tension of the abdominal muscles and fluctuations of the diaphragm. That is, it is enough to sneeze, cough or laugh so that a couple of drops of urine appear on the linen. The condition is typical for the first trimester.
- Urgent. Symptoms are sudden urge to urinate. They arise so unexpectedly that the expectant mother simply does not have enough time to run to the bathroom. One of the causes of the condition lies in the irritation of the urinary canal. You can also blame the failure of the nervous system and overstretching of the muscles in the pelvis. The condition is typical for the last trimester, but also occurs after childbirth.
- Full bladder syndrome. The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.
Regardless of the cause of urinary incontinence in a pregnant woman, the condition causes discomfort and stress. This is not a reason to panic, in fact, the situation is not so critical - most often, not the entire volume of urine from the bladder is released, but only a small amount. To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary.
To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary.
Main causes of urinary incontinence in pregnancy
Given that it is not difficult to find an explanation for urinary incontinence in a pregnant woman, it should not cause much concern. It is only necessary to identify the causes and make sure that this is due to physiology, and not diseases of the genitourinary system. The doctor who leads the pregnancy will help dispel fears.
The main cause is weakened muscles in the pelvic area. Excessive stretching of muscle tissue leads to loss of tone. As a result, the sphincter that holds urine, the walls of the bladder, and other muscles are weakened. This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often.
Another cause of urinary incontinence in a woman during pregnancy is the impact of a baby's foot on the bladder.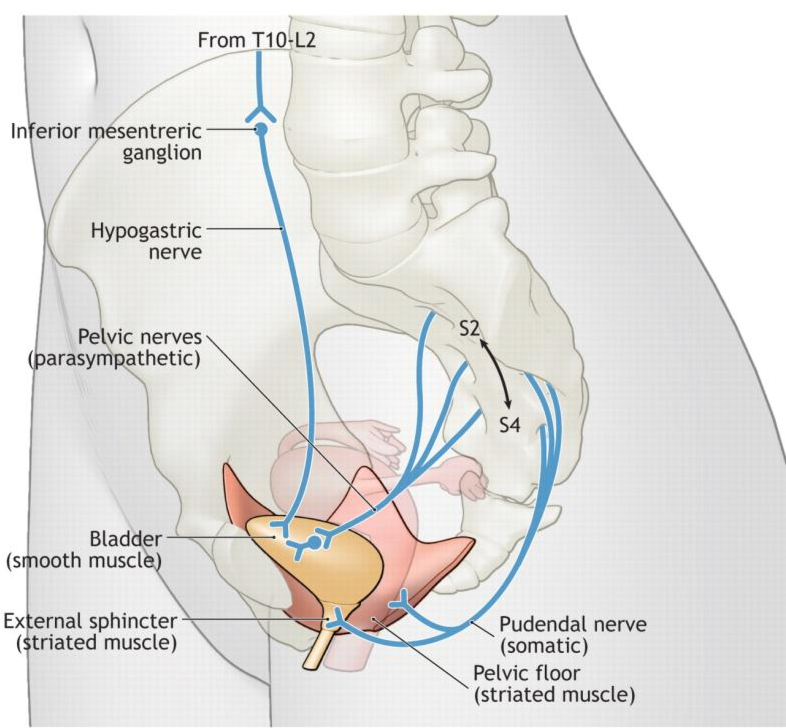 This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
The number of previous pregnancies and births is also thought to increase the risk of urinary incontinence. Especially if the pregnancies go one after another, and the woman's muscles simply do not have time to recover.
Other factors associated with urinary incontinence during pregnancy are overweight and a sedentary lifestyle. A protracted birth process provokes a problem already in the postpartum period.
Healthy urinary retention occurs when the following conditions are met:
- when the bladder is in a normal position;
- immobility of the urethra;
- good work of the muscles surrounding the bladder and pelvic floor muscles;
- with the functional and anatomical integrity of the urethra and bladder closure apparatus.
What to do to deal with the problem
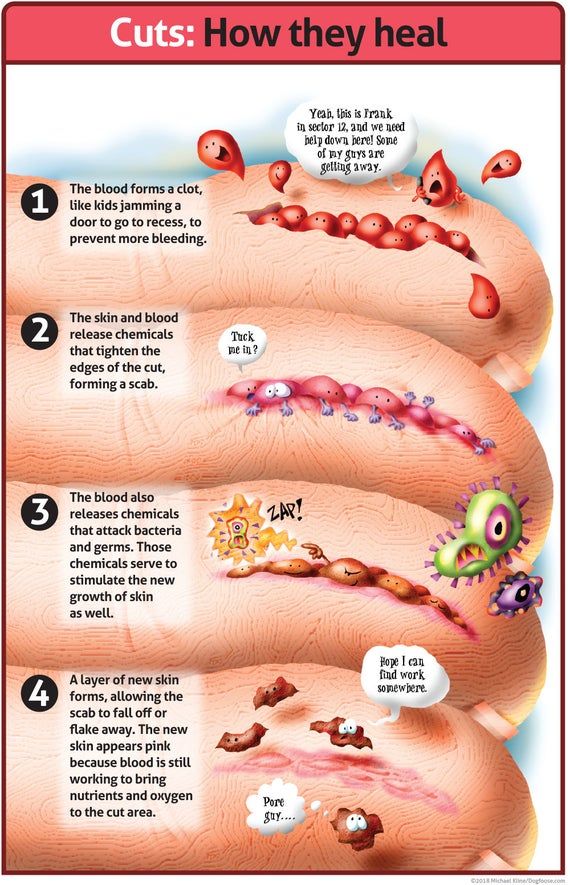
As mentioned above, urinary incontinence in women during pregnancy is most often associated with physiological changes, so no treatment is required.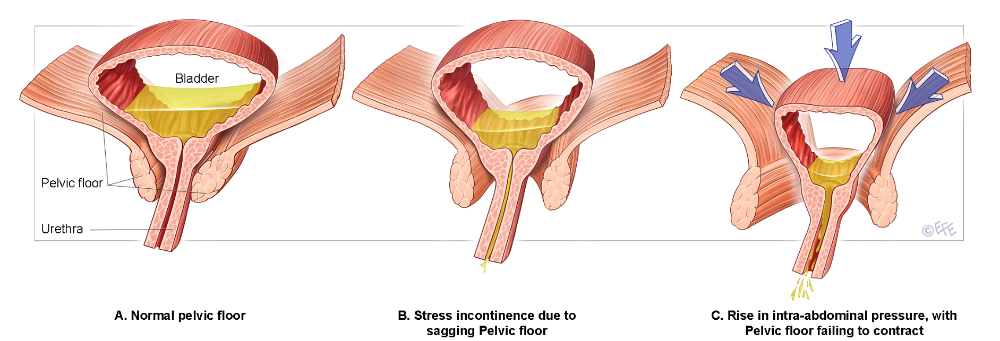 However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.
However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.
If the tests do not show deviations, it remains only to calm down and practice hygiene more often. The doctor will give recommendations on hygiene products - their choice and the frequency of changing underwear. But even without a specialist, we can say that the replacement of pads and panties is carried out as needed. Lingerie should fit the size, and it is better to choose a special cut for expectant mothers so that it does not press anywhere. Decorative details on underwear are not welcome, you should give preference to simple panties made of natural fabric.
If there is a problem, you will often have to wash yourself, go to the toilet on time. Doctors advise you to lean forward slightly when urinating. This will allow the urethra to open completely.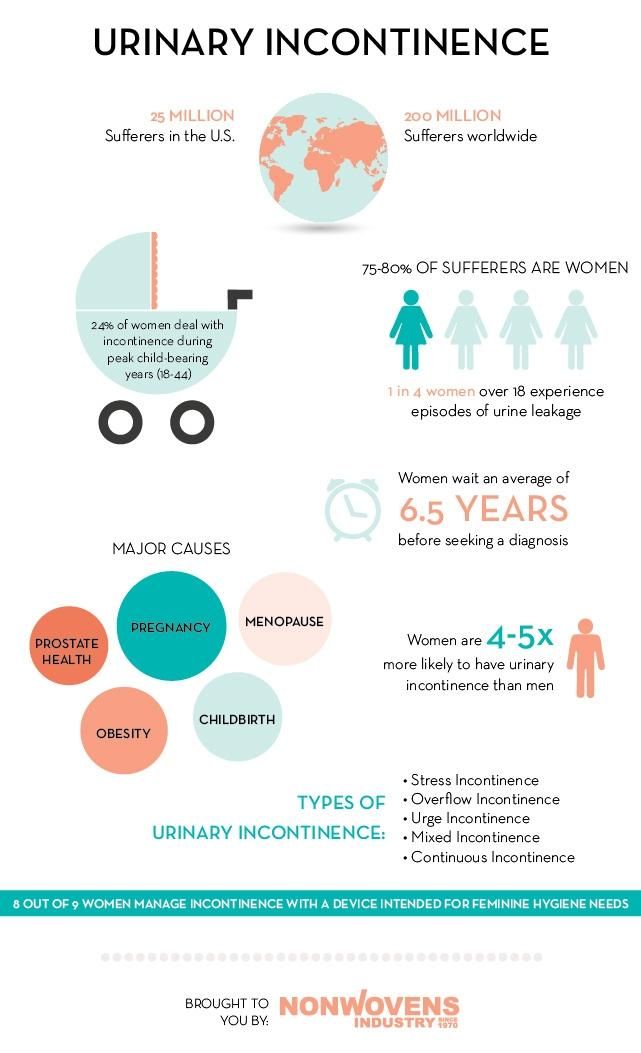 At the end, you need to push slightly (without fanaticism) to completely empty the bladder.
At the end, you need to push slightly (without fanaticism) to completely empty the bladder.
Reducing the pressure on the diaphragm can help reduce the risk of urine leakage when sneezing and coughing. To do this, you need to open your mouth, normalizing the pressure.
Examination and treatment
Before dealing with incontinence, it is imperative to establish its cause by contacting a doctor. The doctor, in turn, will prescribe the necessary examination. It usually consists of several stages:
- Urodynamic examination. With the help of it, the work of the upper and lower urinary tract is evaluated.
- Clinical examination. It includes a routine urine test and urine culture for flora, as well as a study in a gynecological chair - during an external examination, the doctor can assess the mobility of the bladder neck during a cough test or straining, assess the condition of the vaginal mucosa and skin, and also identify a possible genital prolapse.

- Ultrasound examination. It is carried out to study the functioning of the renal system, the urethrovesical segment, the condition of the urethra in a pregnant woman with stress urinary incontinence, as well as to confirm the presence or absence of pathologies of the genitals.
In addition to tests and examinations, you will most likely be asked to keep a special diary in which for several days you will record several parameters of urination, such as the amount of urine released per urination, the number of urination per day, all cases of urinary incontinence, the number of used during the day pads and physical activity.
Only after the examination, conclusions are drawn about the methods of treatment, which are often necessary only in extreme cases. If no pathology or inflammatory processes are detected, then most likely no special treatment will be carried out, since after childbirth, incontinence most often goes away on its own or occurs less and less.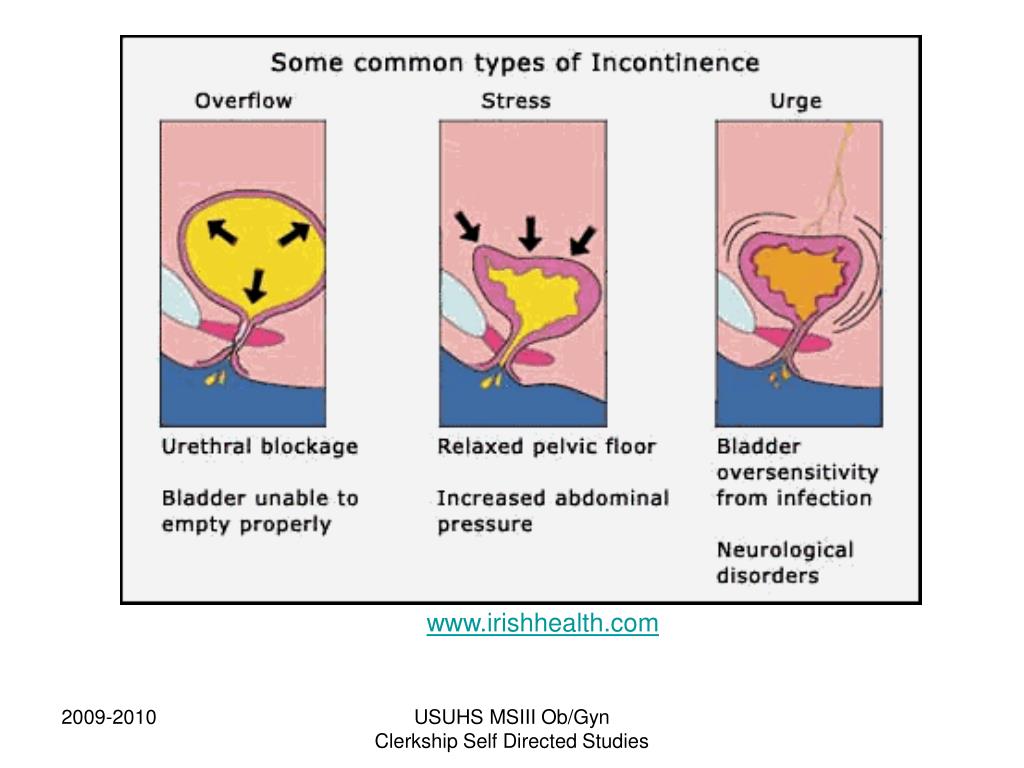
If incontinence is due to weakening of the pelvic floor muscles, then the situation can be significantly improved with the help of special exercises. Currently, there are a large number of complexes for intimate gymnastics. One of the most popular was developed by the American gynecologist and MD Arnold Kegel. The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay).
It is important to know that if you have never strengthened intimate muscles before pregnancy, you need to do this with caution, in no case overdo it.
It is possible that the doctor will prescribe you some herbal preparation that supports the functioning of the bladder and has an antispasmodic, anti-inflammatory and antimicrobial effect.
Treatment with decoctions of herbs (rose hips, sage, dill, lingonberries) may also be recommended. They have not only preventive, but also curative properties.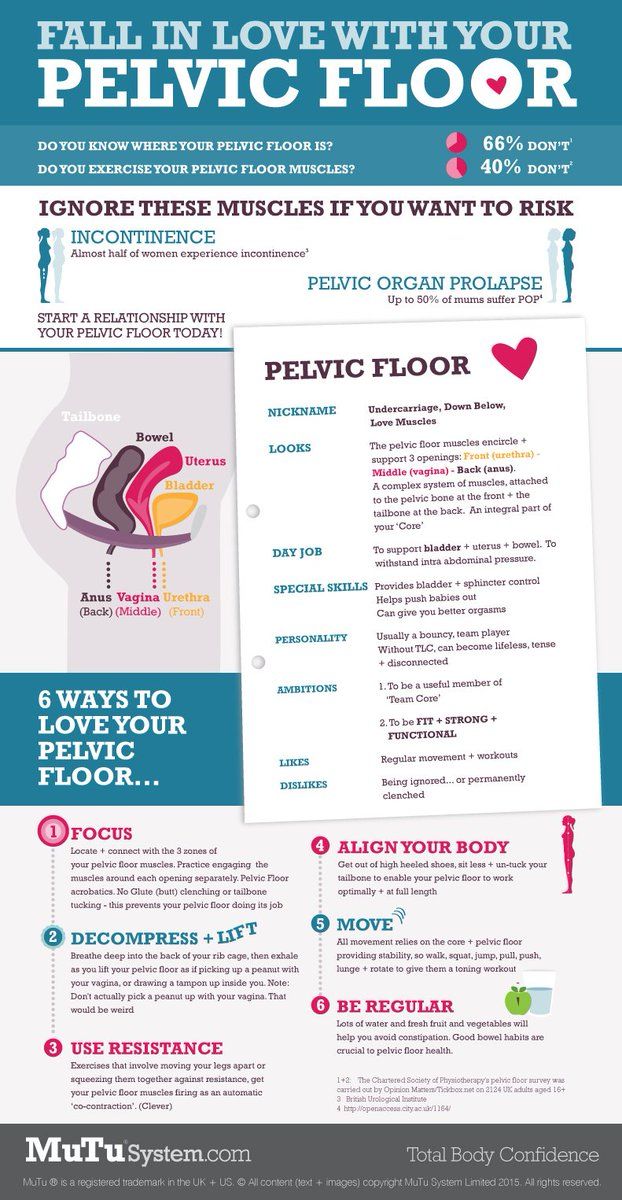
Pelvic (intimate) muscle training
To reduce the risk of urinary incontinence in a pregnant woman at night and during the day, doctors recommend doing special exercises. These are Kegel exercises that are useful not only for expectant mothers, but for all women, without exception, regardless of age. The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article.
How to ensure your comfort and peace of mind
So that urinary incontinence in pregnant women in the early, and especially in the later stages (38-39 weeks), does not cause increased discomfort, manufacturers of hygiene products produce special pads.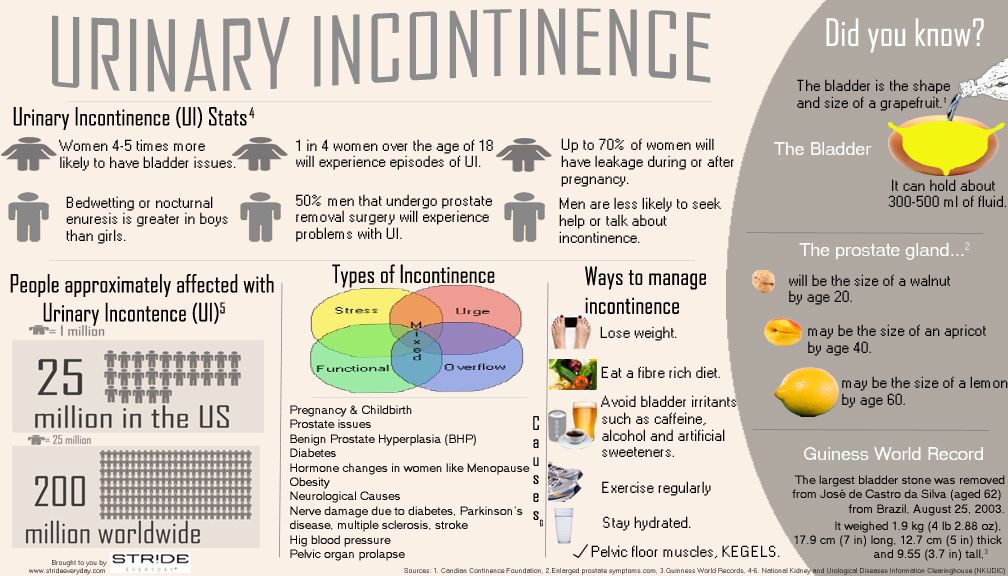 One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
- anatomically shaped to prevent leakage of urine;
- absorbent layer that instantly absorbs liquids and odors;
- secure fit on underwear;
- small thickness so that the pad is not visible under clothing;
- safe even for sensitive skin;
- the ability to choose a product based on the amount of discharge.
If you need help choosing the right hygiene products, the PAUL HARTMANN Sp. z o.o. hotline will advise you.
How else can you help yourself
Go to the toilet as often as possible during the day. At the same time, you should not reduce your fluid intake. The expectant mother should drink as much as she wants. But you need to try not to drink large amounts of liquid an hour before bedtime.
Many women use disposable pads to avoid trouble.