Baby throws up hours after eating solids
FAQ: Introducing Your Baby to Solid Foods | Patient Education
- When will my baby be ready to start solid foods?
- Why does my baby need solid food?
- What foods should I offer my baby first?
- How do I introduce my baby to solid food?
- Can I put the cereal or baby food into my baby's bottle?
- What are the next foods I can give my baby?
- What should I look for when buying baby food?
- Can I make my own baby food?
- What foods should I not give my baby?
- What are the signs my baby is allergic to a food?
- How will my baby's stools change once I introduce solid food?
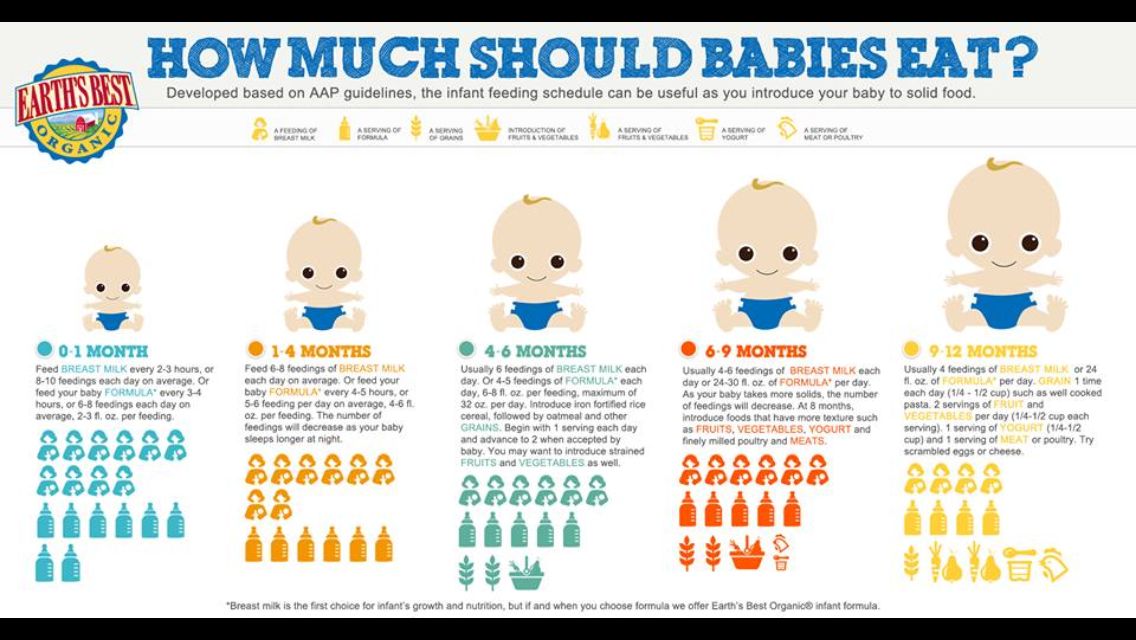
- How often should I feed my baby?
When will my baby be ready to start solid foods?
Most babies grow beautifully on breast milk or formula for the first 6 months, and do not need any solid food before this age. Also, before 6 months of age, most infants have a reflex that causes them to push their tongue against a spoon, making it difficult for them to swallow solid food properly. Introducing solid foods before 5 to 6 months of age may also increase the baby's risk of developing food allergies and obesity.
Your baby will show readiness to eat solids in several ways:
- Your baby's physical development allows him or her to sit without support. When babies can sit easily, they have usually lost the tongue thrust reflex.
- Your baby watches you eat and demonstrates an interest in food.
- Your baby is able to reach out and grab objects.
Why does my baby need solid food?
By 6 months of age, your baby has outgrown the amount of iron he or she received from you before birth. Now your baby needs an additional iron source to prevent anemia. Eating solid food also helps your baby learn many new things, including how to swallow food and, eventually, how to feed him or herself. It also exposes babies to many new tastes and textures.
However, between 6 and 9 months of age, most of the calories your baby needs to grow will still come from breast milk or formula. So, always feed your baby breast milk or formula before offering solid food.
So, always feed your baby breast milk or formula before offering solid food.
What foods should I offer my baby first?
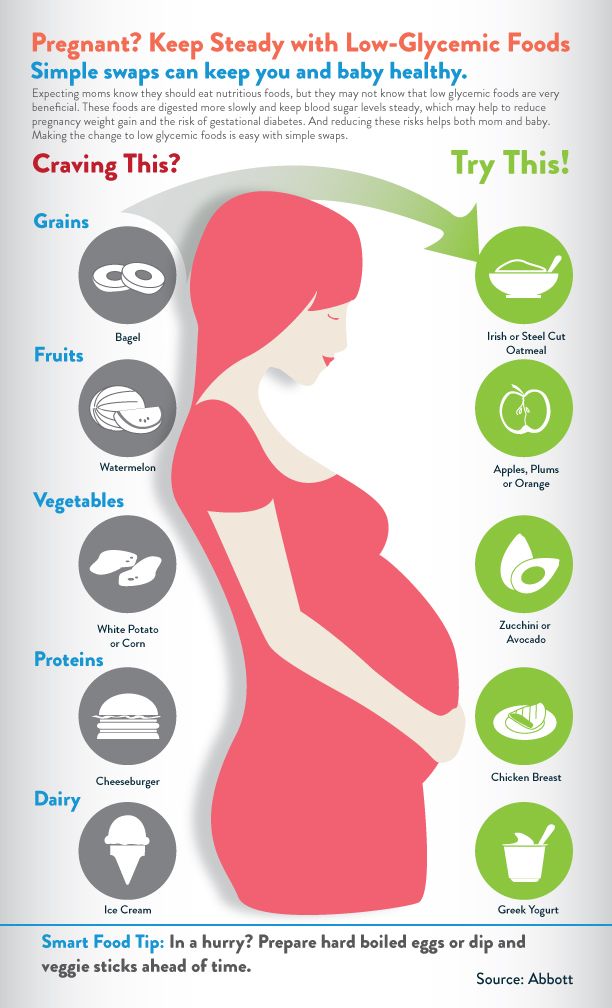
Since babies need extra iron, their best first food is an iron-fortified baby cereal. Once solid foods are introduced, babies do not absorb as much iron from breast milk — another reason to make sure that your baby's first food is a good source of iron.
How do I introduce my baby to solid food?
- Choose a time when you and your baby are both relaxed and ready to enjoy mealtime.
- Prepare an iron-fortified baby cereal, such as rice, barley or oatmeal infant cereal. Mix several tablespoons of dry cereal with formula, water or breast milk. The cereal should be the consistency of cream of wheat — smooth and semi-liquid.
- Sit your baby in your lap or in a highchair.
- Use a small spoon to feed your baby.
- Your baby may look a little confused at first, and most of the first feeding may end up on his or her face, hands and bib.
 Don't worry. Your baby will gradually become more comfortable with feedings. Try talking gently to your baby to help him or her relax.
Don't worry. Your baby will gradually become more comfortable with feedings. Try talking gently to your baby to help him or her relax. - As your baby begins to enjoy mealtimes, increase the consistency of the cereal so it is like oatmeal. You can also gradually increase the amount of food you offer.
- If your baby spits out the cereal, cries or isn't interested, stop the feeding. You can try again in a few days.
Can I put the cereal or baby food into my baby's bottle?
Please don't put cereal or baby food in a bottle. Your baby needs to learn the difference between liquid and solid foods. Babies need to learn how to move solid food around in their mouth, how to take bites from a spoon and rest between bites, and to stop eating when full. These are all experiences that help babies develop good eating habits.
What are the next foods I can give my baby?
You can give plain baby cereal for several months, but most parents enjoy offering their baby a variety of new foods.
After you've given your baby several different types of cereal, consider offering a vegetable or meat. Chicken or turkey is a good source of zinc for breast-fed infants. After your baby is enjoying several different vegetables, you can then try fruit.
After introducing a new food, wait four to five days before giving your baby any new foods, so you can watch for signs of an allergic reaction.
Be aware that cereal, applesauce and bananas can cause constipation. If your baby becomes constipated, you may try giving him or her an ounce or two of diluted prune or pear juice. You can mix your baby's cereal with prune or pear juice. Or, try offering extra fruits like plums and peaches.
What should I look for when buying baby food?
- Choose single-item foods, like squash or bananas.
- Always read labels. Make sure there is only one ingredient, and look for any added ingredients that can cause allergies, such as orange juice.
- Avoid mixed baby foods, like baby dinners.
 They have less nutritional value and aren't a good value for the money.
They have less nutritional value and aren't a good value for the money. - Don't give your child "baby desserts." They add extra calories without being nutritious.
Can I make my own baby food?
Certainly. If you do, please remember:
- Do not add salt, sugar or seasonings to your baby's food.
- You can freeze extra food in ice cube trays, and defrost small portions later when needed.
- Know that some vegetables, such as carrots, beets, spinach, collard greens and turnips, can contain nitrates, a chemical that can cause an unusual type of anemia. Don't cook these foods for your baby. Store-bought baby food has had the nitrates removed and is fine.
What foods should I not give my baby?
The American Academy of Pediatrics now recommends giving peanut-containing products to infants at "high risk" of developing allergies between four and 11 months, in countries where peanut allergies are common.
Scientific evidence suggests that delaying the introduction of peanuts may be linked to a greater risk of developing peanut allergies.
However, babies who experience severe eczema, egg allergy or other related diseases in their first four to six months may benefit from seeing an allergist who can give patient-specific advice on early introduction of peanuts, the academy says.
Do not give your baby any honey for the first year of life. It can cause infant botulism, a type of food poisoning that can lead to death.
Also, remember that some foods can irritate your baby's digestive system. Avoid highly spicy or greasy foods. Also avoid foods that could easily cause choking, such as small candies, popcorn, raisins, grapes, or hotdogs cut in circles.
What are the signs my baby is allergic to a food?
If your baby as several episodes of vomiting after trying a new food, has diarrhea, develops a rash, or has swelling of the lips or eyes, he or she may be having an allergic reaction. Stop the feeding and call your baby's doctor.
Stop the feeding and call your baby's doctor.
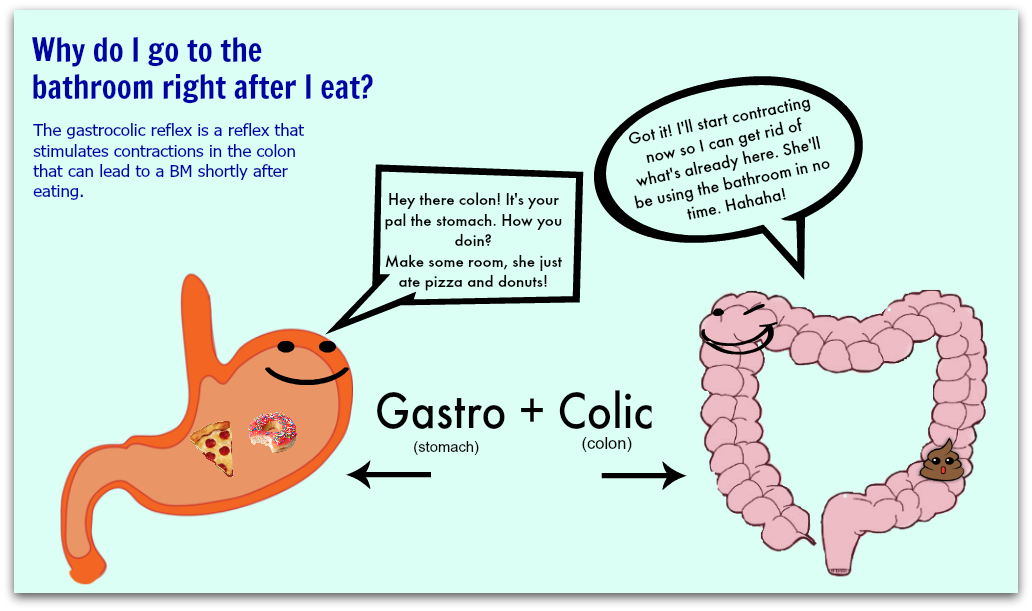
How will my baby's stools change once I introduce solid food?
Your baby's stools may become firmer and may have a different, stronger odor. Some foods will appear in the stool undigested, and you may see peas, corn or tomato skins in your baby's diaper. Bananas often cause little black threads to appear in the stool. This is just the center part of the banana.
If your baby's stools become extremely loose, watery or full of mucous, the baby's intestinal tract may be a little irritated. Consider removing the new food from your baby's diet for a while. Irritation around the anus does not mean the baby is allergic to a food.
How often should I feed my baby?
Since most of your baby's nutrition still comes from breast milk or formula, you do not need to worry about how often you are offering solid foods. Feed your baby when it is fun, easy and convenient for you. Most babies enjoy eating once a day at first. Parents should let babies show when they are interested and how much they want to eat.
Parents should let babies show when they are interested and how much they want to eat.
Used by permission of Jane E. Anderson, M.D.
Baby Vomiting After Introducing Solids?
·
Written by Jo Charnock
·
Written by Jo Charnock
On this Page:
- Types Of Baby Vomiting
- Causes Of A Baby Vomiting
- Other Symptoms To Look Out For
- Treatment For Your Baby Vomiting
- Reducing Reflux Vomiting
- Signs That Baby May Be Allergic To Foods
- When To See Your Doctor
- Things To Remember
Is your baby vomiting after eating? Is it happening after introducing solids? Are you concerned? Don’t worry, we’ve gathered some helpful advice for you here!
Vomiting in young babies and small children is very common. This is especially true in the early weeks of introducing solids and new foods (so around 4 months old), and as their small bodies develop. A baby vomiting may seem quite scary at first, but if your baby is generally happy and healthy then there shouldn’t be anything to worry about. Vomiting can be a symptom of many different minor illnesses in babies, but it’s usually nothing serious, and they normally recover quickly. The amount of vomit can look like a lot, too much to come out of your little one, but remember it’s only what went in that’s coming out!
This is especially true in the early weeks of introducing solids and new foods (so around 4 months old), and as their small bodies develop. A baby vomiting may seem quite scary at first, but if your baby is generally happy and healthy then there shouldn’t be anything to worry about. Vomiting can be a symptom of many different minor illnesses in babies, but it’s usually nothing serious, and they normally recover quickly. The amount of vomit can look like a lot, too much to come out of your little one, but remember it’s only what went in that’s coming out!
Types Of Baby Vomiting
There are three different types of baby vomiting which include the following:
- ‘Posetting’– is when your baby brings up small quantities of milk or food after a feed. Its not really vomiting as it’s normally a gentle, burp-like movement, which causes your baby no stress.
- ‘Reflux’– occurs when food backs up the food pipe, or oesophagus, from your baby’s stomach.
 This will cause your baby to vomit gently, or spit the food up. Reflux is rarely a problem and your baby should grow out of it by the time they are around 18 months old.
This will cause your baby to vomit gently, or spit the food up. Reflux is rarely a problem and your baby should grow out of it by the time they are around 18 months old. - ‘Projectile’– is when your baby is vomiting in a more forceful way rather than just bringing up small quantities of food. A baby vomiting is quite natural and can be caused by simple things like car sickness, indigestion or even something as simple as crying too much. A baby vomiting may seem scary for both you and your baby, but rest assured, it is very normal. But if your baby is projectile vomiting after every meal then we recommend consulting your doctor.
Causes Of A Baby Vomiting
A baby vomiting is often the sign of a minor illness or infection. It can be caused by:
- a minor infection like the common cold,
- a dose of ‘gastro’ or gastroenteritis, which is very common,
- car or motion sickness caused by travelling in a moving vehicle.
More serious illnesses that can cause your baby to vomit can include the following:
- urinary tract infections,
- ear infections,
- appendicitis,
- meningitis,
- food allergies.
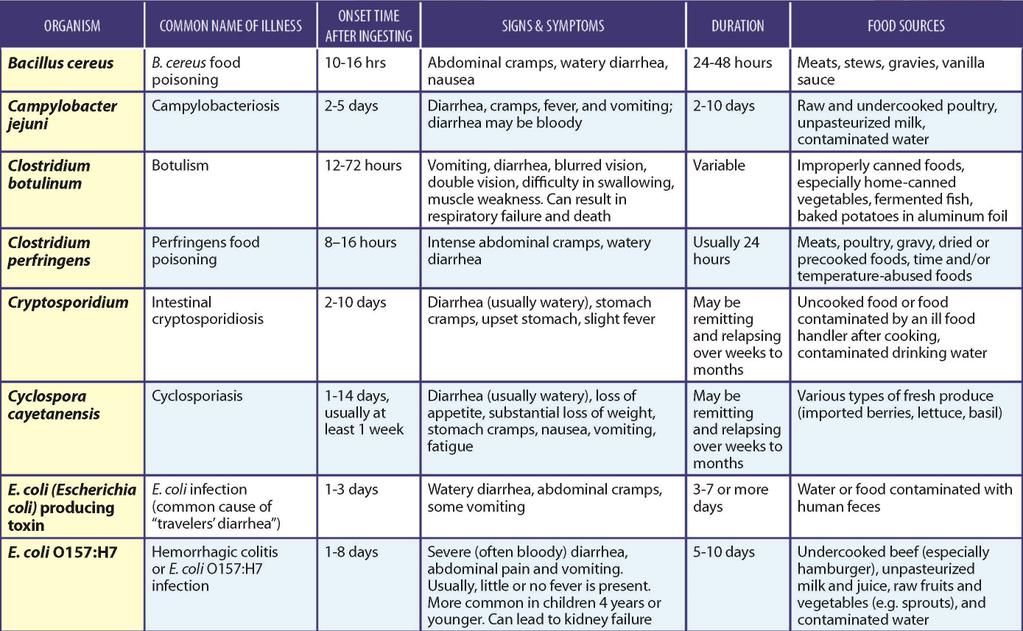
If your baby’s vomiting is accompanied by fever or diarrhoea, it’s usually a sign of a virus infection. Plus if your baby is vomiting for more than 12 hours then dehydration will be a major concern. If your baby is showing these signs then it’s time to see your doctor.
Other Symptoms To Look Out For:
Keeping in mind that vomiting in babies is normal and mostly no cause for real concern, you should be on the look out for the following symptoms:
- nausea
- diarrhoea
- stomach or abdominal pain
- dehydration
- lethargy
- weight loss
While not all are a cause for any immediate action, it is important to take note, and be aware if the symptoms improve or get worse.
Treatment For Your Baby Vomiting
While a baby vomiting can be a very unpleasant experience for both you and your baby, they usually recover quickly. Vomiting can be easily treated with rest, lots of fluids and plenty of reassurance and comfort.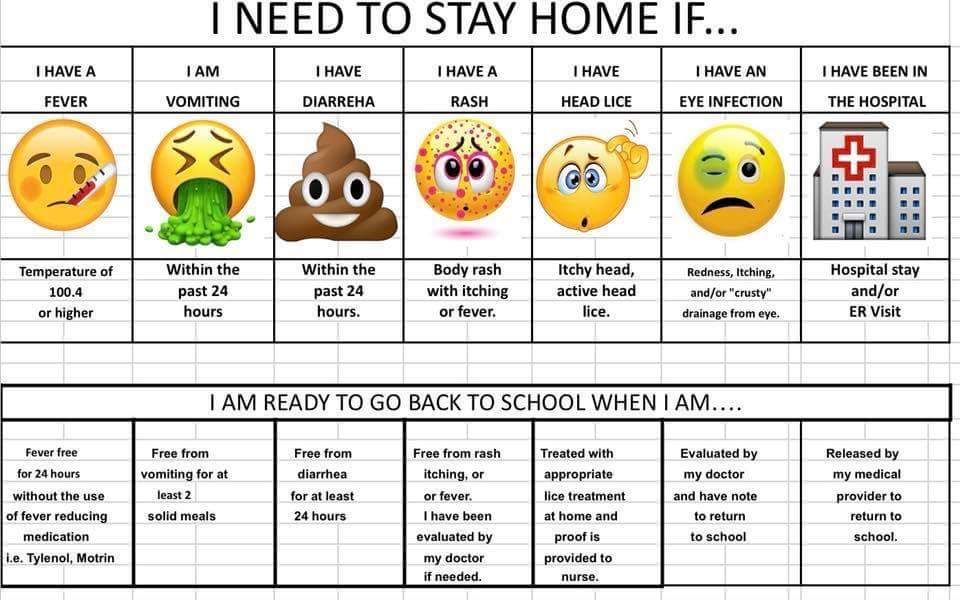 To prevent dehydration, liquids should be given little and often. Checking your baby’s nappy will give you a good indication; if it’s drier than normal then your baby is not drinking enough.
To prevent dehydration, liquids should be given little and often. Checking your baby’s nappy will give you a good indication; if it’s drier than normal then your baby is not drinking enough.
Don’t give your baby over the counter medicine or any medication that has not been prescribed by your doctor.
Reducing Reflux Vomiting
While reflux vomiting is normal for young babies, the following tips may help to reduce his or her discomfort:
- switching to anti-colic teats and bottles
- holding and feeding your baby in an upright position,
- trying smaller and more frequent feedings,
- avoid bouncing or getting your baby excited after feeding,
- trying thicker foods like cereals,
- giving your baby milk or water after feeding to reduce acid and indigestion,
- make sure feeding time is a quiet time with no outside stimulation.
Signs That Baby May Be Allergic To Foods
Food allergies may cause vomiting, but are often accompanied by other symptoms like diarrhoea and skin rashes or hives. Keeping a record of what you are feeding your young baby when introducing solids is recommended. If you suspect a food allergy you can consult your doctor about what may be the cause. Foods generally associated with food allergies include eggs, wheat, nuts, some berries, milk, fish and seafood. Most of these you should avoid feeding your baby until they are at least 12 months old.
Keeping a record of what you are feeding your young baby when introducing solids is recommended. If you suspect a food allergy you can consult your doctor about what may be the cause. Foods generally associated with food allergies include eggs, wheat, nuts, some berries, milk, fish and seafood. Most of these you should avoid feeding your baby until they are at least 12 months old.
When To See Your Doctor
While we’ve mentioned that a baby vomiting is normal and children will mostly get over vomiting very quickly, there will be times when you need to consult your doctor or health worker. It’s time to see your doctor when any of the following symptoms occur:
- your baby has been vomiting for more than 12 hours,
- there is blood or bile in the vomit,
- your baby is not gaining weight,
- there are signs your baby has stomach pain or a swollen abdomen,
- your baby has persistent indigestion or heartburn,
- your baby seems generally unwell.

Use your instincts, if your baby is showing signs or symptoms of being unwell, go and see your doctor.
Things to Remember
In general, symptoms found in babies are similar to those found in adults, so you don’t need to panic every time your baby throws up. Vomiting can lead to diarrhoea, fever, and sometimes abdominal cramps. However, the symptoms can be easily treated by allowing some time to rest, lots of rehydration and maybe some soft foods.
Please keep the following in mind:
- mild vomiting is normal in most babies and improves over time,
- most babies need simple treatment, or none at all,
- having an upright feeding position may help,
- never give any medication unless prescribed by your doctor,
- after vomiting, try to give your baby a small amount of liquid or a little food,
- if your child seems unwell or shows any worrying symptoms, see a doctor!
Important
You shouldn’t use over-the-counter medications to stop vomiting in children. The side effects of these medications can be very serious. Sometimes doctors prescribe medications to stop vomiting, but they do this only after a proper medical review.
The side effects of these medications can be very serious. Sometimes doctors prescribe medications to stop vomiting, but they do this only after a proper medical review.
Hopefully, this has helped to shed some light about the causes of a baby vomiting
Read more about our Homemade baby food recipes.
Need some more info about introducing solids to bub? Download your free Guide here!
Any questions or comments? sound off below 🙂
References
The Royal Children's Hospital Melbourne
The Raising Children
Better Health Channel - Victoria State Goverment
Tagged in
- Starting solids
Continue reading
Baby Thermometers: Ear vs Forehead Thermometer?
How To Warm A Baby Bottle Safely
Feeding Schedule For Your 6 Month Old Baby
Viral gastroenteritis (children)
Most diarrhea and vomiting in children is caused by a virus. This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
The child may also have the following symptoms:
The main danger of this disease is that it leads to dehydration. This is the loss of a large amount of water and mineral salts by the body. In such cases, fluid loss by the body must be replenished. This is done with oral rehydration solution. These solutions are available from pharmacies and most grocery stores without a prescription.
Antibiotics do not help with this illness.
Home Care
Follow your pediatrician's instructions.
If you give medicine to your child:
-
Do not use over-the-counter diarrhea medications unless your doctor tells you to.

-
Acetaminophen or ibuprofen can be used for pain and fever. Or another medicine as prescribed.
-
Aspirin as an antipyretic is contraindicated in children under 18 years of age. Its use can lead to serious liver problems and a life-threatening condition called Reye's syndrome.
To prevent the spread of disease:
-
Remember that washing your hands with soap and clean running water or using an alcohol-based hand sanitizer is the best way to prevent the spread of infection.
-
Teach all family members when and how to wash their hands. Wet your hands with clean running water. Apply soap to the back of your hands, between your fingers and under your nails. Rub your hands for at least 20 seconds. If you need a timer, try singing "Happy Birthday to You!" twice.
 from the beginning to the end. Rinse your hands well and dry with a clean towel.
from the beginning to the end. Rinse your hands well and dry with a clean towel. -
Wash your hands before and after caring for your sick child.
-
Clean the toilet after each use.
-
Dispose of soiled diapers in an airtight container.
-
Keep the child away from other people until the doctor says so.
-
Wash your hands before and after preparing food.
-
Wash hands and utensils after using cutting boards, countertops and knives that have been in contact with raw food.
-
Keep raw meat away from cooked and ready-to-eat foods.
-
Please note that people with diarrhea or vomiting should not prepare food for others.
How to properly water and feed
The main goal in the treatment of vomiting or diarrhea is to prevent dehydration. To do this, the child should often consume liquids in small portions.
-
Fluid is now more important than food. Give a small amount of liquid at a time, especially if the child has stomach cramps or is vomiting.
-
For diarrhea: If you are giving milk to a baby and the diarrhea does not stop, refuse the milk. In some cases, milk can make diarrhea worse. If this happens, use an oral rehydration solution. Eliminate apple juice, soda, sports or other sweetened drinks. Drinks with sugar can make diarrhea worse.
-
For vomiting: Start with oral rehydration solution at room temperature.
 Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other liquids. Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating.
Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other liquids. Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food. After 24 hours without vomiting, resume normal eating. -
As you feel better, you can gradually resume your child's normal diet. Don't force your child to eat, especially if they have stomach pain or cramps. Do not feed your baby large portions at a time, even if he is hungry. Tobacco smoke can make a child feel worse.
 Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables.
Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables. -
If symptoms return, return to a simple or no therapeutic diet.
Postoperative care
See your pediatrician or follow his instructions. If a stool or culture test is taken, see your doctor for results as directed.
Call 911
Call 911 if your child has any of these symptoms:
-
Labored breathing
-
Confusion
-
Extreme drowsiness or loss of consciousness
-
Trouble walking
-
Rapid pulse
-
Chest pains
-
Neck stiffness
-
Convulsions
When to seek medical help
Seek immediate medical attention in the following cases:
-
Abdominal pain worse
-
Constant pain in the right lower abdomen
-
Recurrent vomiting after first 2 hours of fluid intake
-
Episodic vomiting for more than 24 hours
-
Continuous severe diarrhea for more than 24 hours
-
Blood in stool or vomit
-
Child drinks less liquid than usual
-
Darkening or no urine for 6 to 8 hours in older children, 4 to 6 hours in toddlers
-
Whims or crying when the child cannot be soothed
-
Unusual drowsiness
-
New skin eruptions
-
Diarrhea lasting more than 10 days
-
Temperature (see Temperature and children below)
Temperature in children
Use a digital thermometer to take your child's temperature. Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
-
Rectal. For children under 3 years of age, rectal temperature is the most accurate.
-
Frontal (temporal). It is used for children aged 3 months and older. If a child under 3 months of age has signs of illness, this method can be used for the first measurement. The doctor may also check the rectal temperature for confirmation.
-
Ear (tympanic). The ear method is accurate for children 6 months and older, but not younger.
-
Axillary (axillary). This is the least reliable method, but can be used for the first measurement to check on a child of any age who is showing signs of illness.
 The doctor may also check the rectal temperature for confirmation.
The doctor may also check the rectal temperature for confirmation. -
Oral (oral). Do not take oral temperature until the child is 4 years of age.
Use the rectal thermometer with care. For correct use, follow the manufacturer's directions. Insert it carefully. Make a note on it and make sure it will not be used orally. It can carry germs from the stool. If a rectal thermometer doesn't work for you, ask your doctor which thermometer is best to use. When you tell a doctor about your child's temperature, tell him what type of thermometer you took it with.
Here are some tips to help you know if your baby has a fever. Your child's doctor may give you other values. Follow your healthcare provider's instructions.
Temperature values for infants up to 3 months:
-
Rectal or forehead thermometer: 38°C (100.
 4°F) or higher
4°F) or higher -
Underarm thermometer: temperature 37.2 °C (99 °F) or higher
Temperature readings for children aged 3 to 36 months (3 years):
-
Rectal, forehead or ear thermometer: temperature 38.9°C (102°F) or higher
-
Axillary thermometer: temperature 38.3 °C (101 °F) or higher
Call a doctor in the following cases:
-
Recurrent fever of 40°C (104°F) or more in a child of any age
-
Temperature 38°C (100.4°F) or higher in an infant under 3 months
-
Temperature lasting more than 24 hours in a child under 2 years of age
-
Temperature that persists for 3 days in a child 2 years of age or older
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes no
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Vitbiomed+ | Network of clinics in Moscow
Text: Irina Frolova
Vomiting in a child is a serious symptom that should not be ignored. Vomiting may or may not be accompanied by diarrhea and/or high fever. In this article, we will talk about the possible causes of vomiting without fever and diarrhea and what parents need to do.
Vomiting may or may not be accompanied by diarrhea and/or high fever. In this article, we will talk about the possible causes of vomiting without fever and diarrhea and what parents need to do.
Causes of vomiting without fever and diarrhea
Viral gastroenteritis
This disease is also called intestinal or stomach flu. Usually its causative agent is a virus from the group of rotaviruses, less often - norovirus. The disease begins abruptly, with indomitable vomiting, accompanied by rumbling and pain in the abdomen. Diarrhea may also develop after 12 to 24 hours, but this is not necessary. Rotavirus infection often occurs with an increase in temperature to febrile values.
Food allergy
Sometimes the only reaction to a food intolerance is vomiting. In this case, vomiting occurs almost immediately after consumption of the product. The most common food allergies are nuts, fish, seafood, milk, eggs, and soy products.
Gastrointestinal disorders
Non-viral gastritis, pancreatitis, cholecystitis and biliary dyskinesia may cause vomiting. As a rule, in children they are caused by errors in nutrition, but there may be other reasons. To make a diagnosis and prescribe treatment, you need to visit a gastroenterologist.
As a rule, in children they are caused by errors in nutrition, but there may be other reasons. To make a diagnosis and prescribe treatment, you need to visit a gastroenterologist.
Taking certain medications
Vomiting can be caused by not following the rules for taking certain medications, such as taking drugs on an empty stomach that irritate the stomach lining. Such drugs, in particular, include paracetamol, ibuprofen, iron preparations, theophylline.
Motion sickness
Motion sickness often causes nausea and vomiting. In this case, the child may experience pain in the abdomen, he may sweat a lot, and then vomiting begins. You can get sick not only on a trip, but even when watching movies shot with camera shake and fast-paced frames.
Cough
A severe cough can sometimes lead to vomiting, especially in children with reflux.
Migraine
About 10% of children suffer from migraine - cases of migraine have been reported in children of two years of age.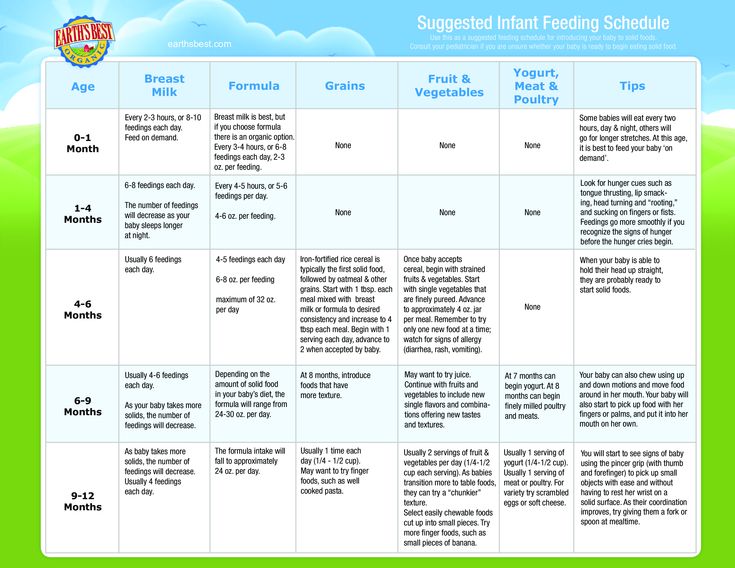 A migraine attack is often accompanied by vomiting.
A migraine attack is often accompanied by vomiting.
Stress
Vomiting can occur during a stressful situation in both children and adults.
Concussion
This is a dangerous condition that occurs after a fall and/or a blow to the head. Vomiting is often its main symptom, but headaches, visual disturbances, speech and gait disturbances may also occur. If you suspect a concussion, you should immediately call a doctor.
Appendicitis
Usually accompanied by severe abdominal pain and requires an ambulance.
Foreign body in the gastrointestinal tract
Sometimes children swallow various objects - buttons, batteries, and so on. This can lead to serious consequences, including intestinal obstruction, a sign of which is also vomiting.
How to determine the severity of vomiting
- Mild - 1-2 times a day
- Medium - 3-7 times a day
- Severe - more than 8 times a day or after any meal, water
How dangerous vomiting is
It causes dehydration, and the more severe the vomiting, the more severe the dehydration. With severe dehydration, the functions of various body systems are disrupted; in severe cases, death can occur without infusion therapy. Children become dehydrated very quickly, and at the first suspicion of dehydration, it is necessary to call a doctor.
With severe dehydration, the functions of various body systems are disrupted; in severe cases, death can occur without infusion therapy. Children become dehydrated very quickly, and at the first suspicion of dehydration, it is necessary to call a doctor.
How to identify dehydration
- The child has dark urine and has not urinated for 8 hours
- Child has dry mouth
- The child cries without tears
If these signs appear, an ambulance should be called. Dehydration is dangerous to the life of a child, especially a younger one.
What to do for parents
As a first aid, help the child to clear the mouth of the remnants of vomit (toddlers clean the mouth of the parents, older children can rinse their mouths themselves), put to bed in such a way that the head is higher than the body, offer water, but do not feed for at least two hours after vomiting.
If vomiting is mild but recurs occasionally, visit a pediatrician and determine the cause.