Baby skull not formed 12 weeks
Facts about Anencephaly | CDC
Anencephaly (pronounced an-en-sef-uh-lee) is a serious birth defect in which a baby is born without parts of the brain and skull.
Click here to view a larger image
What is anencephaly?
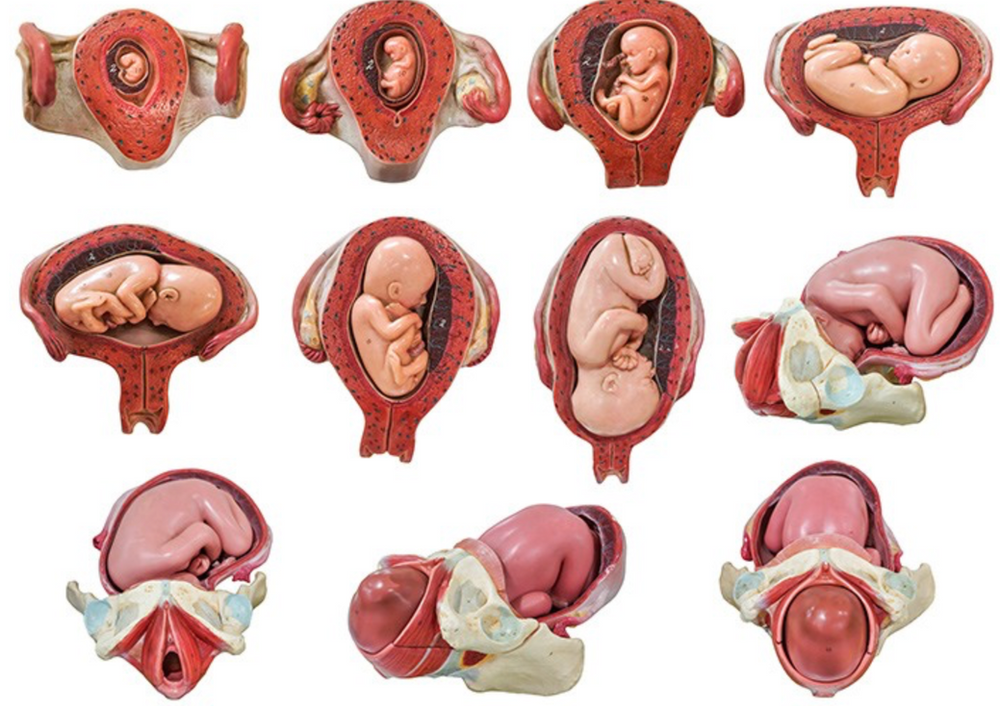
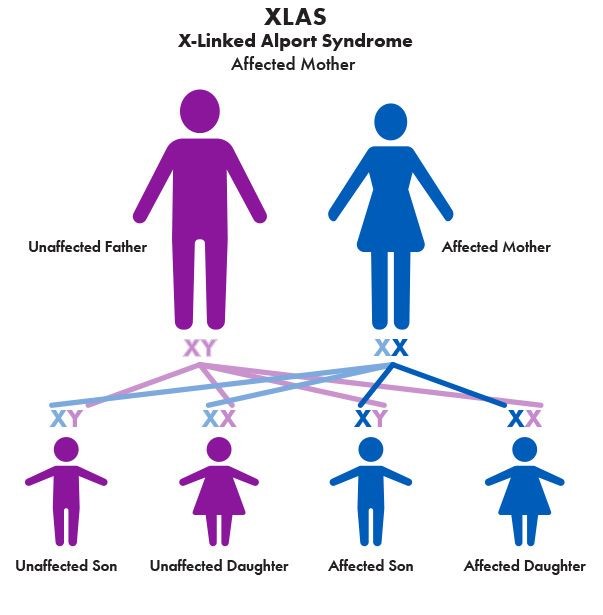
Anencephaly is a serious birth defect in which a baby is born without parts of the brain and skull. It is a type of neural tube defect (NTD). As the neural tube forms and closes, it helps form the baby’s brain and skull (upper part of the neural tube), spinal cord, and back bones (lower part of the neural tube).
Anencephaly happens if the upper part of the neural tube does not close all the way. This often results in a baby being born without the front part of the brain (forebrain) and the thinking and coordinating part of the brain (cerebrum). The remaining parts of the brain are often not covered by bone or skin.
How Many Babies are Born with Anencephaly?
Researchers estimate that about 1 in every 4,600 babies is born with anencephaly in the United States. 1
Causes and Prevention
The causes of anencephaly among most infants are unknown. Some babies have anencephaly because of a change in their genes or chromosomes. Anencephaly might also be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment or what the mother eats or drinks, or certain medicines she uses during pregnancy.
Getting enough folic acid before and during early pregnancy can help prevent neural tube defects, such as anencephaly. If you are pregnant or could get pregnant, take 400 micrograms (mcg) of folic acid every day. If you have already had a pregnancy affected by an NTD, you can speak with your doctor about taking a higher dose of folic acid before pregnancy and during early pregnancy.
- Since the United States began fortifying grains with folic acid, there has been a 28% decline in pregnancies affected by neural tube defects (spina bifida and anencephaly).1
- In order to get the recommended 400 micrograms of folic acid every day, a woman of reproductive age can take a supplement containing folic acid or to eat foods fortified with folic acid, or both, depending on her dietary habits.

CDC is dedicated to better understanding the causes of birth defects. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011), to understand the causes of and risks for birth defects, including anencephaly.
If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Anencephaly can be diagnosed during pregnancy or after the baby is born.
During Pregnancy
During pregnancy, there are screening tests (prenatal tests) to check for birth defects and other conditions. Anencephaly would result in an abnormal result on a blood or serum screening test or it might be seen during an ultrasound (which creates pictures of the body).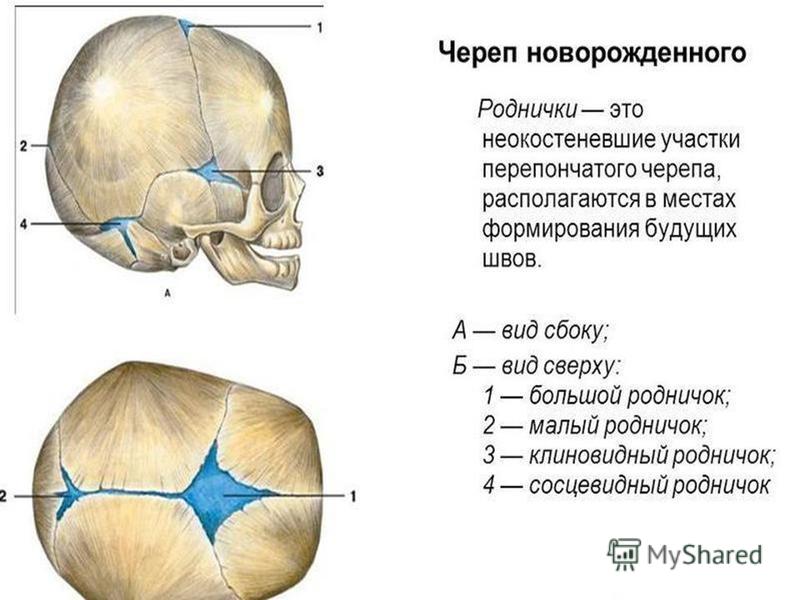 For more information about screening and confirmatory tests during pregnancy, visit CDC’s birth defects diagnosis web page.
For more information about screening and confirmatory tests during pregnancy, visit CDC’s birth defects diagnosis web page.
After the Baby is Born
In some cases, anencephaly might not be diagnosed until after the baby is born. Anencephaly is immediately seen at birth.
Treatments
There is no known cure or standard treatment for anencephaly. Almost all babies born with anencephaly will die shortly after birth.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS. National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
What Is Anencephaly? What Causes It and How to Reduce Your Baby's Risk
Written by WebMD Editorial Contributors
In this Article
- What Is Anencephaly?
- What Causes Anencephaly?
- Diagnosing Anencephaly
- Treating Anencephaly
- Preventing Anencephaly
Anencephaly is a serious birth defect where a baby is born without parts of their skull and brain. It's a rare type of neural tube defect that affects about 1 in 4,600 babies. There is no way to treat anencephaly. Babies born with this condition will die before or shortly after birth.
What Is Anencephaly?
Anencephaly is a type of neural tube defect. During pregnancy, your baby's brain and spine start to form as a flat disk of cells. This flat disk rolls into a tube-like structure called the neural tube. By 28 to 32 days after conception, the neural tube is completely formed. When part of the neural tube doesn't close completely, there's an opening called a neural tube defect.
Sometimes this opening is exposed, or open, and sometimes it's covered with bone or skin. In anencephaly, this opening is at the base of the skull.
What Causes Anencephaly?
Several things seem to cause anencephaly. Some of these are things you are exposed to when you are pregnant. It may also be related to your nutrition and genetics. If you've had one child with a neural tube defect, you are more likely to have a child with anencephaly. Some other factors that may increase your baby's risk of having it include:
Not getting enough folic acid. If you don't get enough folic acid during your pregnancy, you have a higher chance of having a baby with anencephaly. You should take a prenatal vitamin that has at least 400 micrograms of folic acid before and during your pregnancy.
Certain medications. Some medications used to treat seizures, bipolar disorder, and migraines can cause neural tube defects. These include phenytoin, carbamazepine, and valproic acid.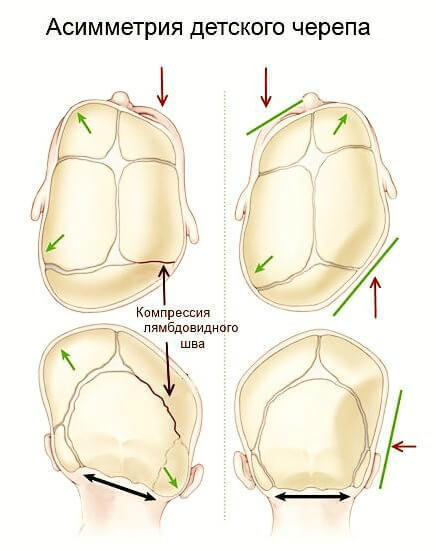
Genetic disorders. Anencephaly can be caused by some genetic disorders, such as trisomy 18. These disorders are usually not inherited. Instead, they happen by chance.
High temperature during pregnancy. Using a hot tub or sauna around the time your baby's neural tube should be closing may cause anencephaly. Having a high fever during the same time may also increase your baby's risk.
Diabetes. If you have uncontrolled diabetes, your blood sugar levels may get too high. This can cause problems with your baby's development.
Obesity. Being obese, or significantly overweight, may cause problems with your baby's development during the 4th week of gestation.
Opioid use. One study found that women who took opioids in the first two months of their pregnancies were more likely to have babies with neural tube defects. These opioids include:
- Codeine
- Oxycodone
- Hydrocodone
- Morphine
- Propoxyphene
- Meperidine
- Methadone
- Tramadol
- Hydromorphone
- Butorphanol
- Heroin
- Fentanyl
- Buprenorphine
- Nalbuphine
- Diphenoxylate
Diagnosing Anencephaly
As part of your prenatal health care, your doctor may do tests to check for neural tube defects. Some of these tests include:
Some of these tests include:
Ultrasounds. An ultrasound uses sound waves to create pictures of your baby. Your doctor can look at these pictures to check your baby's brain, skull, and spine.
Quad marker screen. A quad marker screen is a blood test to check for neural tube defects and genetic disorders. One of the tests checks for high levels of alpha-fetoprotein (AFP). Your baby's liver makes AFP. If your blood shows high levels of AFP in your blood, your baby may have anencephaly.
Fetal magnetic resonance imaging (MRI). An MRI uses high-powered magnets to create detailed images of your baby's tissues and bones. Your doctor can use an MRI to get detailed images of your baby's spine and brain. This test provides more detail than an ultrasound.
Amniocentesis. In amniocentesis, your doctor inserts a thin needle into the amniotic sac to get a sample of the fluid around your baby. A lab will check this fluid for high levels of AFP or acetylcholinesterase, which is a type of enzyme that shows that your baby may have a neural tube defect.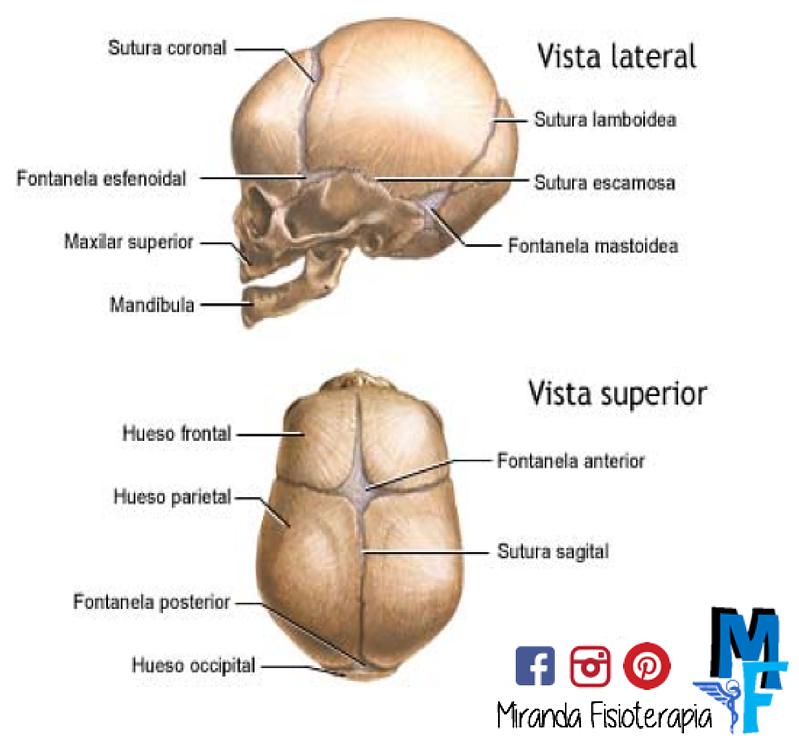
Treating Anencephaly
Unfortunately, there is no treatment for anencephaly. Many pregnancies with neural tube defects will end in miscarriages. Some babies with anencephaly will be stillborn. Other babies who are born with anencephaly will die within a few hours to a few days.
If your baby is born with anencephaly, your doctor can offer you resources to make the most of the time you have with your baby.
Preventing Anencephaly
It's not always possible to prevent anencephaly. However, there are some ways you can reduce your baby's risk of having it:
- Take at least 400 micrograms of folic acid before and during your pregnancy.
- Talk to your doctor about your medications if you are planning to become pregnant.
- Avoid taking opioids if you think you may be pregnant.
- Avoid saunas and hot tubs if you think you may be pregnant.
- Talk to your doctor about reducing fevers while you're pregnant.
- Try to maintain a healthy weight before you get pregnant.
- If you have diabetes, talk to your doctor about the best way to manage it while you're pregnant.
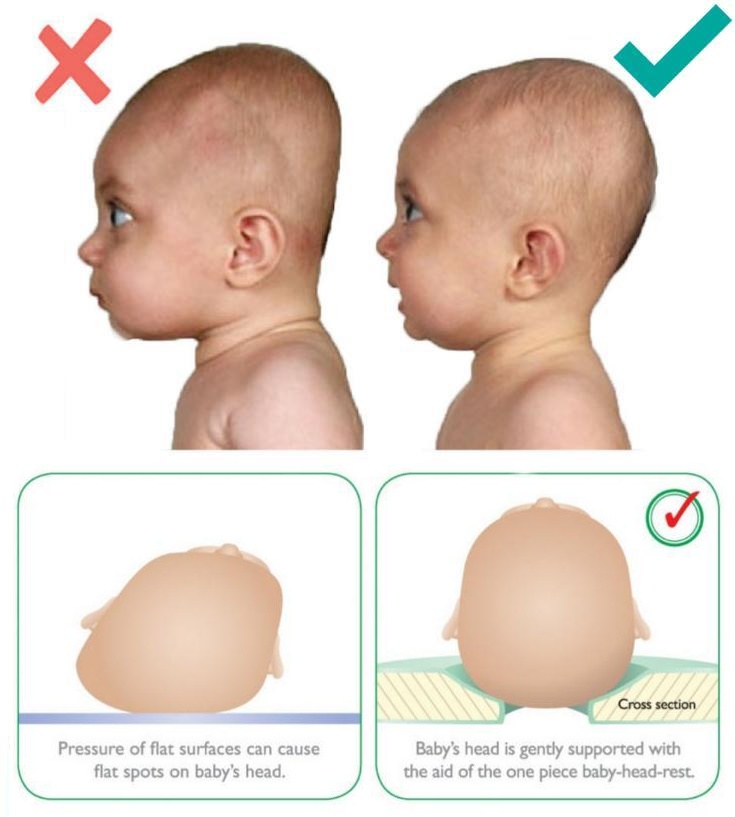
Plagiocephaly in a child - an irregular shape of the skull in an infant
The disease is cured by:
Children's osteopath
Article content
- Causes of
- Types of plagiocephaly in children
- Signs of disease
- Diagnostics of plagiocephaly in children
Plagiocephaly is an abnormally shaped skull, or flat head syndrome, in infants. Its signs are detected to some extent in every fifth child, and only every tenth of them needs specific treatment. Deformation becomes distinct noticeable by 2 months (sometimes earlier). Treatment started on time is usually effective.
Causes
- Postpartum - permanent position with emphasis on the bones of the skull (mainly lying on the back) or premature fusion of the sutures of the skull.
- Intrauterine - in most cases caused by the anatomical position during gestation - with twin pregnancy and / or pressing the fetus to the mother's ribs, large fetus or uterine abnormalities, premature prolapse during childbirth.

- Pathological conditions - torticollis, or torticollis - shortening of the neck muscles on one side, other neuromuscular diseases.
Previously, the disease was diagnosed less frequently - due to the fact that pediatricians recommended laying newborns on their side. To date, it has been proven that this position increases the risk of sudden infant death syndrome in a dream, therefore, since 1992, it has been recommended to lay children on their backs during sleep, which becomes a frequent cause of deformation of the skull bones that have not yet been fully formed.
Types of plagiocephaly in children
According to etiological types, plagiocephaly is distinguished:
- Positional - acquired, caused by mechanical deformations - intrauterine or perinatal. Occurs in the vast majority of cases. Source:
https://www.ncbi.nlm.nih.gov/pubmed/25382999
Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R
Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging
// Pediatric Child Health.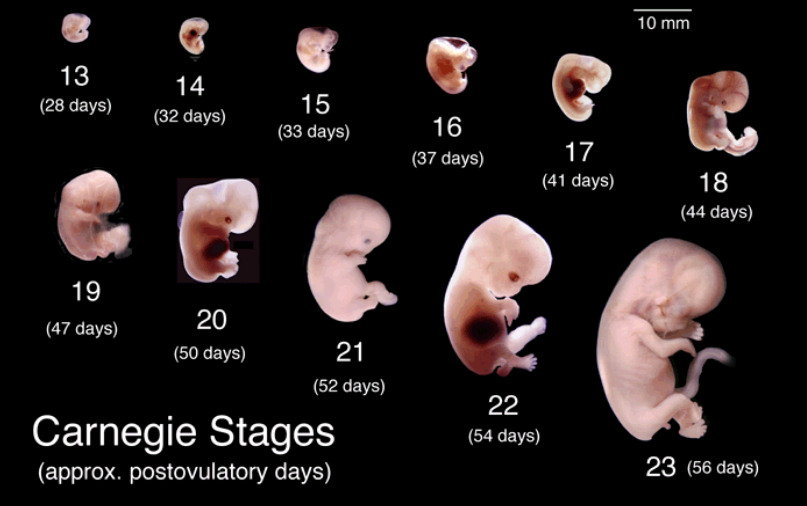 2014 Oct;19(8):423-7
2014 Oct;19(8):423-7 - Deformation - caused by congenital diseases - progressive deformity due to early fusion of the cranial bones. It occurs extremely rarely - in 1 out of 2,000 patients. Source:
https://www.ncbi.nlm.nih.gov/pubmed/30151193
Renz-Polster H, De Bock
Deformational plagiocephaly: The case for an evolutionary mismatch
// Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2018
According to localization, it happens:
- frontal;
- occipital;
- side.
Signs of disease
Atypical skull shape - flattened in the occipital region. Rarely - elongated in the frontal direction or squeezed from the sides. Characteristic frontal or temporal bulges, protrusions of the parietal region are possible.
If the asymmetry of the head is caused by congenital anomalies, then without treatment, the pathology progresses. Over time, it can cause negative consequences in the child - increased intracranial pressure and the symptoms caused by it . Source:
Over time, it can cause negative consequences in the child - increased intracranial pressure and the symptoms caused by it . Source:
E.V. Mammadov
Plagiocephaly. II. Synostotic, deformation and compensatory
// Children's surgery, 2003, No. 5, p. 45-50
Diagnosis of plagiocephaly in a child
In accordance with modern recommendations, the diagnosis is made on the basis of a clinical examination. For differential diagnosis - identifying the cause of the pathology - ultrasound, radiography or CT of the skull are optionally prescribed.
Methods of treatment
The main treatment for positional plagiocephaly in infants is the repositioning method : multiple changes in body position during the day. The child should lie on his back as little as possible when he is awake. Minimize wearing in a sling and carrier, transport in a car seat. An effective technique is to change the position of the child relative to the light source (stimulates turning over).
Children older than 7 weeks also indicated exercise therapy. It is aimed at:
- stimulation of motor development and correction of positional preferences;
- stretching of the neck muscles with torticollis - an increase in the range of motion in the cervical spine.
Includes laying out the child on the stomach during wakefulness under the supervision of adults.
With moderate and severe deformities, as well as with the ineffectiveness of conservative treatment, orthotics are indicated - helmet therapy. The orthosis is made according to individual measurements in an orthopedic workshop. The child wears it 23 hours a day until it heals or needs to change the size of the helmet.
Conservative treatment and orthotics last for several months. The bones of the skull gradually assume a physiological position, while no damage is done to the brain, and neurological diseases do not develop.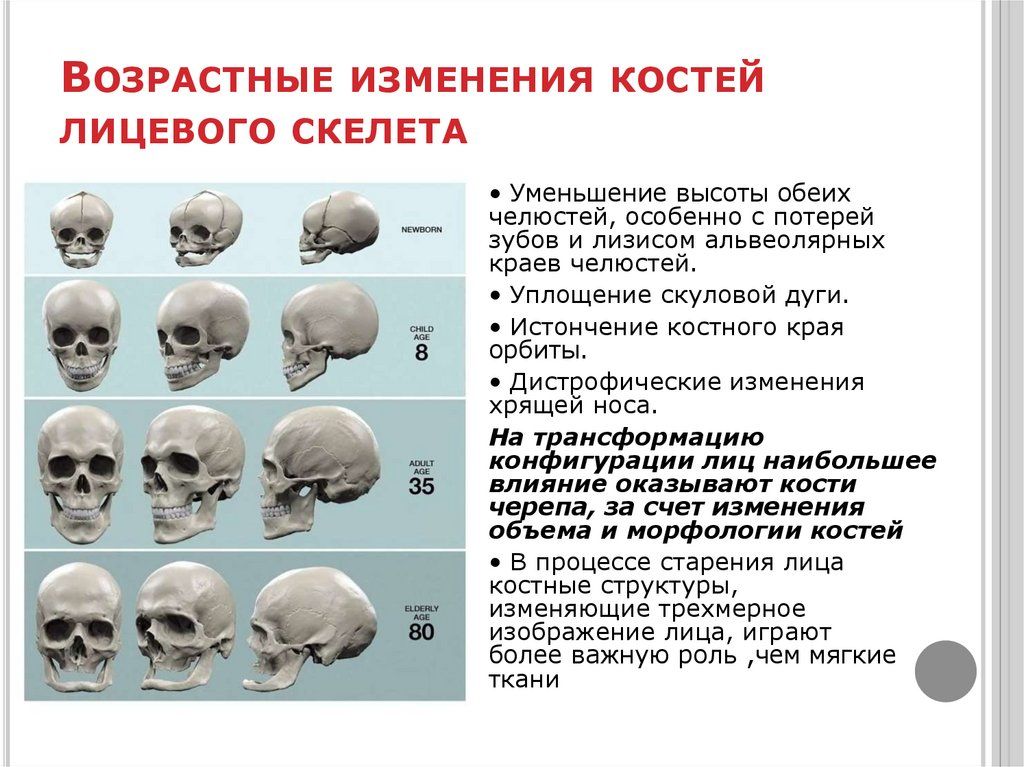
If the deformity is due to a congenital anomaly, surgery is indicated. As a rule, it is done at the age of ~7-9 years. The use of orthopedic pillows for newborns is contraindicated, as they sometimes cause infant death.
Sources:
- https://www.ncbi.nlm.nih.gov/pubmed/25382999 Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging // Paediatr child health. 2014 Oct;19(8):423-7.
- https://www.ncbi.nlm.nih.gov/pubmed/30151193 Renz-Polster H, De Bock. Deformational plagiocephaly: The case for an evolutionary mismatch // Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2018.
- E.V. Mammadov. Plagiocephaly. II. Synostotic, deformation and compensatory // Children's surgery, 2003, No. 5, pp. 45-50.
The information in this article is provided for reference only and does not replace the advice of a qualified professional. Do not self-medicate! At the first signs of the disease, you should consult a doctor.
Do not self-medicate! At the first signs of the disease, you should consult a doctor.
All pediatric osteopaths
- All doctors
- Malaya Balkanskaya, 23
- Udarnikov, 19k1
Make an appointment
Registration through the site is preliminary.
Our employee will contact you to confirm the appointment with a specialist.
Specify time
Time9:009:3010:0010:3011:0011:3012:0012:3013:0013:3014:0014:3015:0015:3016:0016:3017:0017:3018:0018:3019:0019:3020: 0020:3021:0021:30
Specify specialist
Specialist-I don’t know-a pediatrician allergist of the Gastroenter gynecologist of the dermatologist Immunology Cardiology, Logo-Pedious Neurology of the Oncology Department of the Orthradeda Orthodox, Pulmonary Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon.
More about the quality assurance of medical services
Features of adaptation and development of premature babies.
 Doctor Plus Medical Center
Doctor Plus Medical Center The first year of a child's life is characterized by the most intensive growth and rapid development. But during this period, the body is extremely vulnerable, the defenses are weak and imperfect. This is especially true for children who were born prematurely and are considered premature.
Premature are children born at gestational age from 28 to 37 completed weeks, weighing from 1000 - 2500 grams, height 35 - 45 cm.
The reasons for their premature birth are varied: too young age and, accordingly, the mother's body; hemolytic disease of the fetus, which develops as a result of Rhesus conflict; pathological (not normal) course of pregnancy; previous abortions, illness, physical and mental trauma; harmful working conditions, the use of nicotine and alcohol.
What a premature baby looks like. Anatomical and physiological signs.
There are 4 degrees of prematurity, depending on the weight of the child:
Grade 1: 2500 -2001 grams Grade 3: 1500 - 1001 grams
Grade 2: 2000 – 1500 grams Grade 4: 1000 grams or less.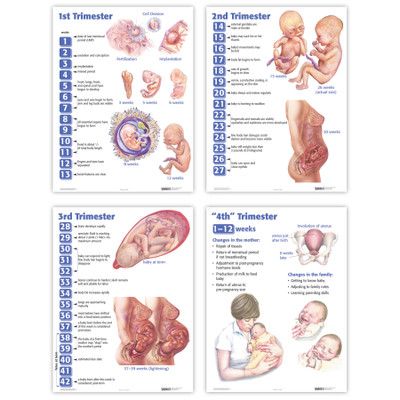
Since body weight may or may not correspond to the gestational age at the time of birth, premature babies are divided into 2 groups also according to these signs
• children whose physical development corresponds to the gestational age at the time of birth;
In premature babies, the subcutaneous fat layer is not sufficiently developed, i.e. they suffer more from overheating and hypothermia. The skin is thin, dry, wrinkled, abundantly covered with fluff. Insufficient maturity of blood vessels is manifested by the Harlequin symptom. If you put the baby on its side, the skin acquires a contrasting pink color.
The bones of the skull are malleable, not only a large, but also a small fontanel is open.
The auricles are soft - the cartilage in them has not yet formed, they are pressed to the head, and not separated from it, as in full-term ones.
The nails do not reach the edge of the phalanges of the fingers, the umbilical cord is located below the middle of the body, and not in the center.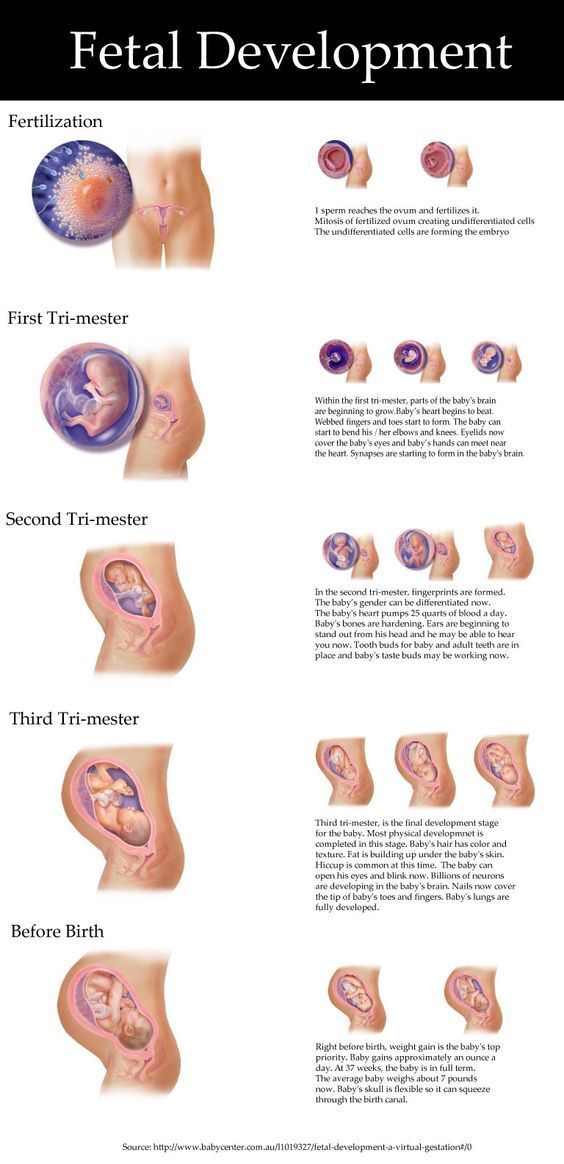
The underdevelopment of the genital organs is indicative: in girls, the labia minora are not covered by the large ones. In boys, the testicles are not descended into the scrotum.
The child sucks badly, swallows with difficulty. The cry is weak, breathing is not rhythmic. Physiological jaundice often lasts up to 3-4 weeks.
The umbilical cord falls off much later, and the umbilical wound heals more slowly.
It has its own characteristics and physiological weight loss. It is restored only by 2-3 weeks of life, and the timing of weight recovery is directly dependent on the maturity of the child, i.e. not only the date of his birth, but also the degree of adaptation of the baby to environmental conditions.
In premature babies, the nerve centers that regulate the rhythm of breathing are not fully formed. The formation of lung tissue has not been completed, in particular, a substance that prevents the “falling off” of the lungs - Surfactant.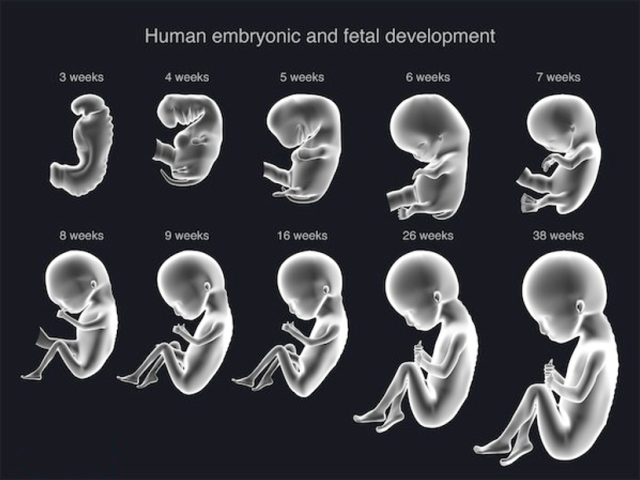 Therefore, their respiratory rate is not constant. With anxiety, it reaches 60-80 in 1 minute, at rest and during sleep it becomes less frequent, respiratory arrests may even be observed. The expansion of the lungs due to an insufficient amount of Surfactant is slowed down, and respiratory failure may occur.
Therefore, their respiratory rate is not constant. With anxiety, it reaches 60-80 in 1 minute, at rest and during sleep it becomes less frequent, respiratory arrests may even be observed. The expansion of the lungs due to an insufficient amount of Surfactant is slowed down, and respiratory failure may occur.
The heart rate also depends on the child's condition and environmental conditions. With an increase in the ambient temperature and the child's anxiety, the heart rate increases to 200 beats per minute.
In premature newborns, asphyxia and cerebral hemorrhage occur more often. They more often suffer from acute respiratory diseases, intestinal infections, which is due to weak immunity and insufficient development of many adaptive reactions.
These babies are more likely than full-term babies to develop anemia (anemia).
Especially during the period when intensive growth and weight gain begins (2-3 months). With proper nutrition of the child and the mother, if she breastfeeds, these phenomena quickly pass.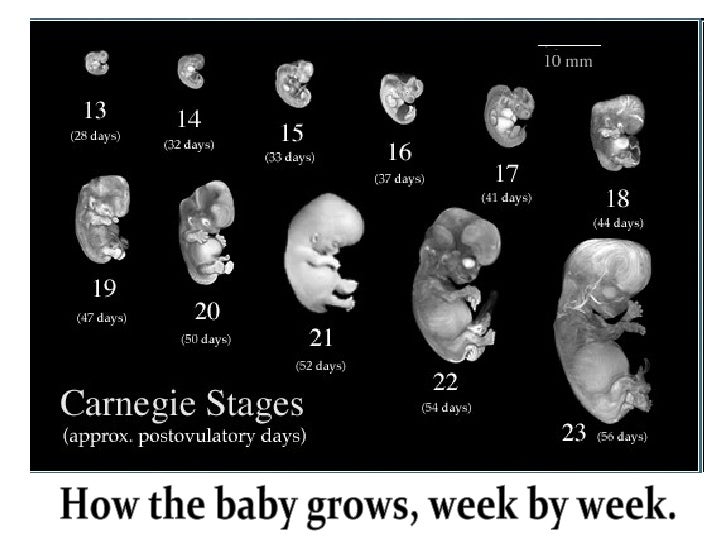 In the case when anemia is of a protracted nature, it is necessary to prescribe iron supplements.
In the case when anemia is of a protracted nature, it is necessary to prescribe iron supplements.
The further development of the child is determined not only by the degree of prematurity, but also in many respects, by the state of his health for a given period of time.
If the child is practically healthy, from the 2nd month of life, he gains weight and height in the same way as full-term ones. By the end of the 1st year, the weight increases by 5-10 times compared to the weight at birth.
The average height is 70-77 cm.
The nervous system of premature babies is also more immature. The development of various skills, their intellectual development lags behind by 1-2 months.
These children sit down later, start walking later, they may have anomalies in the structure of the foot, curvature of the legs, and spine. If children are born very premature and often get sick, their development slows down by about a year. In the future, it levels off, approximately to preschool age.
If you have suffered intrauterine malnutrition, i.e. the nutrition of the fetus was disturbed for some reason - diseases of the mother, anomalies in the development of the child itself, anomalies in the development of the umbilical cord and placenta, then its central nervous system can recover for a long time (therefore, the observation of a neurologist is very important).
There may be lability of the nervous system (mood changes easily, often gives in to emotions, conflicts with other people are not uncommon), night terrors, enuresis (urinary incontinence), lack of appetite, a tendency to nausea.
However, in general, premature babies grow up as quite normal people.
Care of a premature baby after discharge from the maternity hospital.
For a child born prematurely, dispensary observation is established at the place of residence up to 7 years.
Periodic consultations of specialists are obligatory, first of all - a neurologist, as well as a surgeon, an otolaryngologist, an ophthalmologist
From the age of 2-4 weeks, rickets is prevented (ultraviolet
irradiation - quartzization, the addition of vitamin D to food, massage, hardening).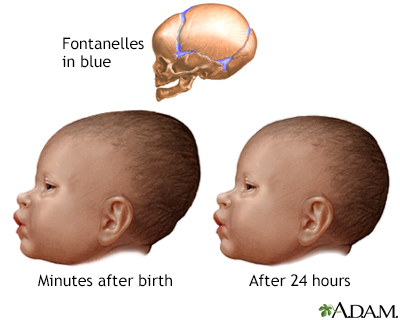
The most adequate type of nutrition for a premature baby is breastfeeding. But given that the baby can suck out an insufficient amount of breast milk, you can supplement it with expressed milk or adapted mixtures.
From 4 months - vegetable purees, 5 months. - porridge, 6 months. - give meat soufflé.
Correction of protein and fat deficiency is carried out by adding the required amount of kefir and cottage cheese, starting with 5 ml, gradually increasing the dosage.
The room in which a premature baby lives should be bright, dry and thoroughly ventilated. The optimum room temperature is 20-22 *. S. Walks are very important. Sufficient exposure to fresh air prevents the development of pathological conditions.
In winter, walks start from the age of 2 months at an air temperature not lower than -8, -10*C. The duration of the walk is from 15 minutes to 2 hours. In summer, a child can spend all the intervals between feedings during the day in the fresh air.