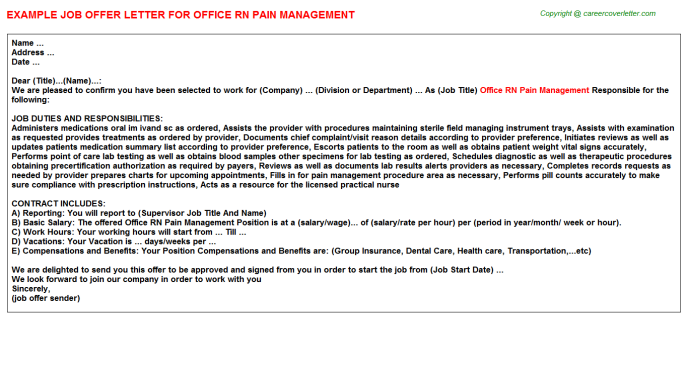
Baby milk in mother
Breastfeeding vs. Formula Feeding (for Parents)
Choosing whether to breastfeed or formula feed their baby is one of the biggest decisions expectant and new parents will make.
Healt experts believe breast milk is the best nutritional choice for infants. But breastfeeding may not be possible for all women. For many, the decision to breastfeed or formula feed is based on their comfort level, lifestyle, and specific medical situations.
For moms who can't breastfeed or who decide not to, infant formula is a healthy alternative. Formula provides babies with the nutrients they need to grow and thrive.
Some mothers worry that if they don't breastfeed, they won't bond with their baby. But the truth is, loving mothers will always create a special bond with their children. And feeding — no matter how — is a great time to strengthen that bond.
The decision to breastfeed or formula feed your baby is a personal one. Weighing the pros and cons of each method can help you decide what is best for you and your baby.
All About Breastfeeding
Nursing can be a wonderful experience for both mother and baby. It provides ideal nourishment and a special bonding experience that many mothers cherish.
A number of health organizations — including the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the World Health Organization (WHO) — recommend breastfeeding as the best choice for babies. Breastfeeding helps defend against infections, prevent allergies, and protect against a number of chronic conditions.
The AAP recommends that babies be breastfed exclusively for the first 6 months. Beyond that, breastfeeding is encouraged until at least 12 months, and longer if both the mother and baby are willing.
Here are some of the many benefits of breastfeeding:
Fighting infections and other conditions. Breastfed babies have fewer infections and hospitalizations than formula-fed infants. During breastfeeding, antibodies and other germ-fighting factors pass from a mother to her baby and strengthen the immune system. This helps lower a baby's chances of getting many infections, including:
This helps lower a baby's chances of getting many infections, including:
- ear infections
- diarrhea
- respiratory infections
- meningitis
Breastfeeding also may protect babies against:
- allergies
- asthma
- diabetes
- obesity
- sudden infant death syndrome (SIDS)
Breastfeeding is particularly beneficial for premature babies.
Nutrition and ease of digestion. Often called the "perfect food" for a human baby's digestive system, breast milk's components — lactose, protein (whey and casein), and fat — are easily digested by a newborn.
As a group, breastfed infants have less difficulty with digestion than do formula-fed infants. Breast milk tends to be more easily digested so that breastfed babies have fewer bouts of diarrhea or constipation.
Breast milk also naturally contains many of the vitamins and minerals that a newborn requires. One exception is vitamin D — the AAP recommends that all breastfed babies begin receiving vitamin D supplements during the first 2 months and continuing until a baby consumes enough vitamin D-fortified formula or milk (after 1 year of age).
The U.S. Food and Drug Administration (FDA) regulates formula companies to ensure they provide all the necessary nutrients (including vitamin D) in their formulas. Still, commercial formulas can't completely match breast milk's exact composition. Why? Because milk is a living substance made by each mother for her individual infant, a process that can't be duplicated in a factory.
Free. Breast milk doesn't cost a cent, while the cost of formula quickly adds up. And unless you're pumping breast milk and giving it to your baby, there's no need for bottles, nipples, and other supplies that can be costly. Since breastfed babies are less likely to be sick, that may mean they make fewer trips to the doctor's office, so fewer co-pays and less money are paid for prescriptions and over-the-counter medicines.
Different tastes. Nursing mothers usually need 300 to 500 extra calories per day, which should come from a wide variety of well-balanced foods. This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
Convenience. With no last-minute runs to the store for more formula, breast milk is always fresh and available whether you're home or out and about. And when women breastfeed, there's no need to wash bottles and nipples or warm up bottles in the middle of the night.
Smarter babies. Some studies suggest that children who were exclusively breastfed have slightly higher IQs than children who were formula fed.
"Skin-to-skin" contact. Many nursing mothers really enjoy the experience of bonding so closely with their babies. And the skin-to-skin contact can enhance the emotional connection between mother and infant.
Beneficial for mom, too. The ability to totally nourish a baby can help a new mother feel confident in her ability to care for her baby. Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
p
Breastfeeding Challenges
Breastfeeding can be easy from the get-go for some mothers, but take a while to get used to for others. Moms and babies need plenty of patience to get used to the routine of breastfeeding.
Common concerns of new moms, especially during the first few weeks and months, may include:
Personal comfort. Initially, many moms feel uncomfortable with breastfeeding. But with proper education, support, and practice, most moms overcome this.
Latch-on pain is normal for the first week to 10 days, and should last less than a minute with each feeding. But if breastfeeding hurts throughout feedings, or if their nipples and/or breasts are sore, it's a good idea for breastfeeding mothers to get help from a lactation consultant or their doctor. Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Time and frequency of feedings. Breastfeeding requires a big time commitment from mothers, especially in the beginning, when babies feed often. A breastfeeding schedule or the need to pump breast milk during the day can make it harder for some moms to work, run errands, or travel.
And breastfed babies do need to eat more often than babies who take formula, because breast milk digests faster than formula. This means mom may find herself in demand every 2 or 3 hours (maybe more, maybe less) in the first few weeks.
Diet. Women who are breastfeeding need to be aware of what they eat and drink, since these can be passed to the baby through the breast milk. Just like during pregnancy, breastfeeding women should not eat fish that are high in mercury and should limit consumption of lower mercury fish.
If a mom drinks alcohol, a small amount can pass to the baby through breast milk. She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
Maternal medical conditions, medicines, and breast surgery. Medical conditions such as HIV or AIDS or those that involve chemotherapy or treatment with certain medicines can make breastfeeding unsafe. A woman should check with her doctor or a lactation consultant if she's unsure if she should breastfeed with a specific condition. Women should always check with the doctor about the safety of taking medicines while breastfeeding, including over-the-counter and herbal medicines.
Mothers who've had breast surgery, such as a reduction, may have difficulty with their milk supply if their milk ducts have been severed. In this situation, a woman should to talk to her doctor about her concerns and work with a lactation specialist.
p
All About Formula Feeding
Commercially prepared infant formulas are a nutritious alternative to breast milk, and even contain some vitamins and nutrients that breastfed babies need to get from supplements.
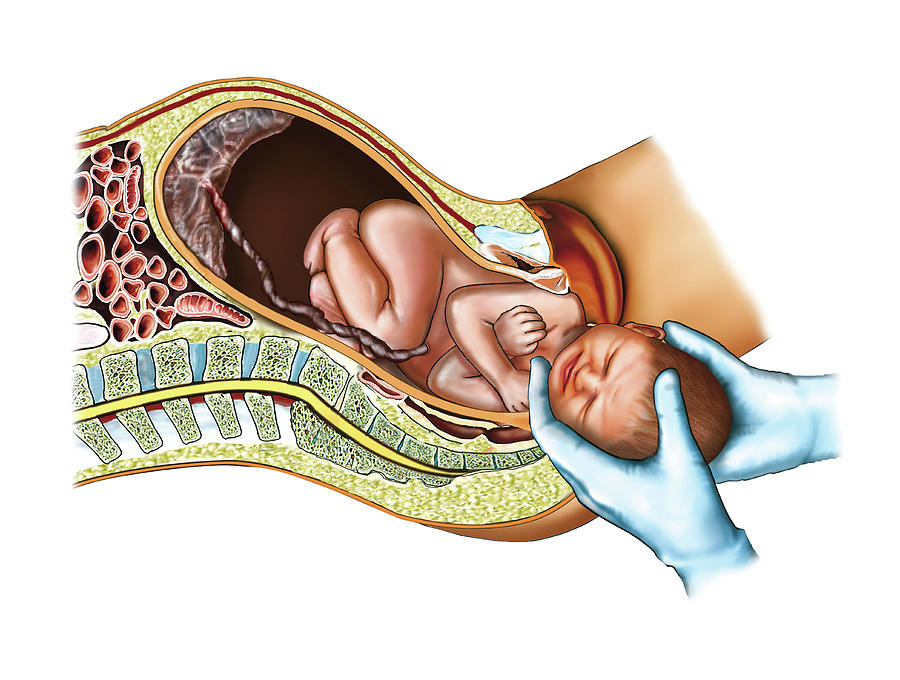
Manufactured under sterile conditions, commercial formulas attempt to duplicate mother's milk using a complex combination of proteins, sugars, fats, and vitamins that aren't possible to create at home. So if you don't breastfeed your baby, it's important to use only commercially prepared formula and not try to make your own.
Besides medical concerns that may prevent breastfeeding, for some women, breastfeeding may be too difficult or stressful. Here are other reasons women may choose to formula feed:
Convenience. Either parent (or another caregiver) can feed the baby a bottle at any time (although this is also true for women who pump their breast milk). This allows mom to share the feeding duties and helps her partner to feel more involved in the crucial feeding process and the bonding that often comes with it.
Flexibility. Once the bottles are made, a formula-feeding mother can leave her baby with a partner or caregiver and know that her little one's feedings are taken care of. There's no need to pump or to schedule work or other obligations and activities around the baby's feeding schedule. And formula-feeding moms don't need to find a private place to nurse in public.
Time and frequency of feedings. Because formula is less digestible than breast milk, formula-fed babies usually need to eat less often than breastfed babies.
Diet. Women who opt to formula feed don't have to worry about the things they eat or drink that could affect their babies.
page 7
Formula Feeding Challenges
As with breastfeeding, there are some challenges to consider when deciding whether to formula feed.
Lack of antibodies. None of the antibodies found in breast milk are in manufactured formula. So formula can't provide a baby with the added protection against infection and illness that breast milk does.
Can't match the complexity of breast milk. Manufactured formulas have yet to duplicate the complexity of breast milk, which changes as the baby's needs change.
Planning and organization. Unlike breast milk — which is always available, unlimited, and served at the right temperature — formula feeding your baby requires planning and organization to make sure that you have what you need when you need it. Parents must buy formula and make sure it's always on hand to avoid late-night runs to the store.
And it's important to always have the necessary supplies (like bottles and nipples) clean, easily accessible, and ready to go — otherwise, you will have a very hungry, very fussy baby to answer to. With 8-10 feedings in a 24-hour period, parents can quickly get overwhelmed if they're not prepared and organized.
Expense. Formula can be costly. Powdered formula is the least expensive, followed by concentrated, with ready-to-feed being the most expensive. And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
Possibility of producing gas and constipation. Formula-fed babies may have more gas and firmer bowel movements than breastfed babies.
Making a Choice
Deciding how you will feed your baby can be a hard decision. You'll really only know the right choice for your family when your baby comes.
Many women decide on one method before the birth and then change their minds after their baby is born. And many women decide to breastfeed and supplement with formula because they find that is the best choice for their family and their lifestyle.
While you're weighing the pros and cons, talk to your doctor or lactation consultant. These health care providers can give you more information about your options and help you make the best decision for your family.
How Breast Milk is Made
Did you know your body gets ready for breastfeeding before you even give birth? While you are pregnant, your breasts change. These changes allow your breasts to make milk and may cause them to feel fuller and more tender.
These changes allow your breasts to make milk and may cause them to feel fuller and more tender.
Once your baby is born, their suckling releases hormones in your body that cause your breasts to make and release milk.
If you are concerned that your milk has not come in or that you are not making enough milk, speak with WIC breastfeeding staff.
Role of Your Breasts
Milk production occurs within the alveoli, which are grape-like clusters of cells within the breast. Once the milk is made, it is squeezed out through the alveoli into the milk ducts, which resemble highways. The ducts carry the milk through the breast.
The size of your breasts does not affect your ability to breastfeed. Women with small breasts make the same quantity and quality of milk as women with larger breasts.
Role of Your Brain
When your baby suckles, it sends a message to your brain. The brain then signals the hormones, prolactin and oxytocin to be released. Prolactin causes the alveoli to begin making milk. Oxytocin causes muscles around the alveoli to squeeze milk out through the milk ducts.
Oxytocin causes muscles around the alveoli to squeeze milk out through the milk ducts.
When milk is released, it is called the let-down reflex. Signs of milk release are:
- Tingling, fullness, dull ache, or tightening in the breasts (although some moms do not feel any of these sensations).
- Milk dripping from the breast.
- Uterine cramping after you put baby to the breast during the first few days after birth.
To encourage your milk to release, try these methods:
- Find ways to relax, such as going to a calm place or trying deep breathing.
- Place a warm compress on your breasts before breastfeeding.
- Massage your breasts and hand express a little milk.
After you've been breastfeeding for a while, the let-down reflex can happen for many other reasons, like when you hear your baby cry, or you see or think of your baby. It also can happen at the time of day you usually breastfeed your baby, even if your baby is not around.
Role of Your Baby
Your baby helps you make milk by suckling and removing milk from your breast. The more milk your baby drinks, the more milk your body will make. Frequent breastfeeding or milk removal (8-12 times or more every 24 hours), especially in the first few days and weeks of your baby's life, helps you make a good milk supply.
Your milk will continue to vary according to your baby's needs. Each time your baby feeds, your body knows to make more milk for the next feeding. The amount of milk you make will go up or down depending on how often your baby eats. By nursing for as often and as long as your baby wants, you are helping your body to make more milk. At first, it might feel like you are doing nothing but breastfeeding. Soon, you and your baby will get into a pattern that works for both of you.
Composition of breast milk | What is breast milk made of?
Breast milk is rich in nutrients that nourish and protect your baby. But did you know that its composition changes over time? Find out what breast milk is made of and how it adapts to your baby's needs.
Share this information
Breast milk is a baby's very first food, so of course
contains essential nutrients - carbohydrates, proteins, fats, and water to maintain water balance in the body. 1 All this is true. But mother's milk is not just a food product, and it performs not only nutritional functions.
What is breast milk made of?
Each serving of breast milk contains many other ingredients, many of which are unique.
- Millions living cells. These include white blood cells, which are responsible for strengthening the immune system, and stem cells, which promote the growth and repair of organs. 2
- More than 1000 3 proteins that help your baby's body grow and develop, strengthen his immune system, form and protect brain neurons.
- All proteins in breast milk consist of amino acids .
 There are more than 20 types of them in milk, and they also include nucleotides, the content of which rises at night. Scientists suggest that they can have a hypnotic effect. 4.5
There are more than 20 types of them in milk, and they also include nucleotides, the content of which rises at night. Scientists suggest that they can have a hypnotic effect. 4.5 - More than 200 complex sugars - oligosaccharides 6 that act as prebiotics necessary to maintain a healthy microflora in the intestines of the child. In addition, they prevent infections from entering the bloodstream and reduce the risk of brain inflammation.
- More than 40 enzymes 7 . Enzymes serve as catalysts for chemical reactions in the body. Breast milk enzymes stimulate digestion and immunity, and help the baby's body absorb iron.
- Growth factors contributing to the normal development of the body. 1 They affect the state of many organs and systems, including internal organs, blood vessels, nervous system and glands responsible for the production of hormones.
- By the way, there are a lot of hormones in breast milk! 7 These smart chemicals are responsible for the exchange of information between tissues and organs, ensuring their normal functioning.
 Some hormones control appetite, others sleep, and some are even responsible for strengthening the bond between mom and baby.
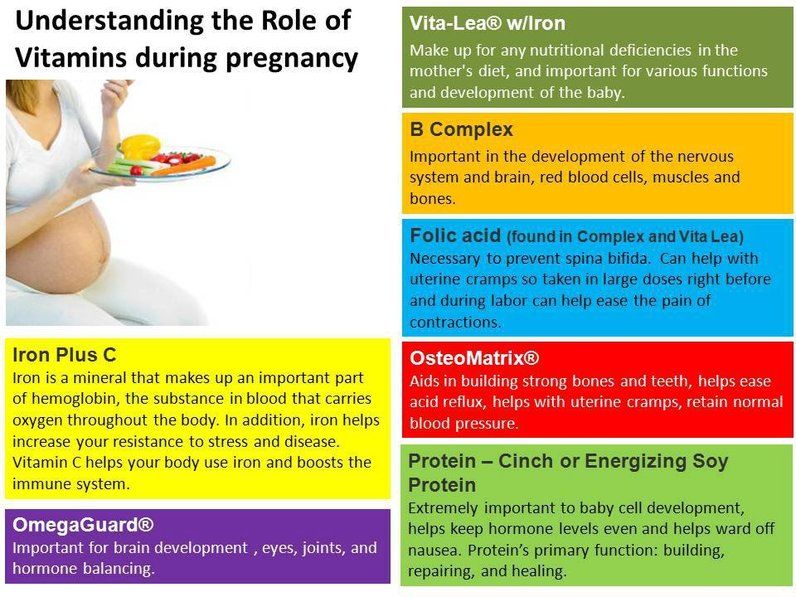
Some hormones control appetite, others sleep, and some are even responsible for strengthening the bond between mom and baby. - Vitamins & Minerals - Nutrients that support normal growth and function of organs and the formation of teeth and bones. 1
- Antibodies or immunoglobulins. There are five main types of antibodies, and all of them are present in breast milk. 8 Antibodies neutralize bacteria and viruses, protecting the child's body from infections and diseases.
- You may have heard of long chain fatty acids , which play a key role in the formation of the child's nervous system and the development of the brain and eyes. 9 So, they are also present in breast milk!
- 1400 species miRNA . It is believed that they control gene expression, prevent and stop the development of diseases, support the immune system of the child, and also affect the change in the structure of the mother's breast.
 10
10
This long list includes only a subset of the ingredients in breast milk—and scientists are discovering new substances in the meantime. Interestingly, the content of these ingredients varies depending on the age and needs of the child.
Let's start from the beginning...
In the early days: colostrum
The first milk that is produced immediately after the birth of a baby is called colostrum. This thick, sticky liquid is often referred to as "liquid gold," and not just for its yellow or orange color. Colostrum performs an important function of nourishing and protecting the fragile body of a newborn baby.
Very little milk is produced at first - only 40-50 ml per day 11 . But the stomach of a newborn is very tiny, so this is quite enough. In addition, colostrum is very well digested. And the small volume is more than offset by its high-quality composition.
Composition of colostrum
Colostrum contains the same substances as breast milk in the following weeks, but in a different ratio, according to the needs of the newborn.
Colostrum, for example, is sometimes called nature's vaccine for its high levels of antibodies and white blood cells. After the child leaves safe mother's womb, the first milk helps to protect it from infections and diseases.
In addition, the protective properties of colostrum play an important role in strengthening the baby's digestive system. Colostrum protects and strengthens the mucosa of the gastrointestinal tract, which is highly permeable in newborns. 12.13 This is especially important if the baby is born prematurely, as this increases the risk of necrotizing enterocolitis. 13
In addition, colostrum is rich in minerals and vitamins, and contains more vitamins A, E and K than in mature breast milk. The protein content is also increased. 1 Colostrum also has a laxative effect, helping to eliminate meconium (original feces). 14
In the next few weeks: transitional milk
During the first week of a baby's life, about two to four days after birth, breast milk production increases. The breast becomes larger and firmer - milk begins to "come". On the third day, the baby consumes 300-400 ml of breast milk per day, and by the fifth day - already 500-800 ml. No wonder breasts seem bigger!
The breast becomes larger and firmer - milk begins to "come". On the third day, the baby consumes 300-400 ml of breast milk per day, and by the fifth day - already 500-800 ml. No wonder breasts seem bigger!
Milk produced from days 5 to 14 is called transitional milk. 15 As the name suggests, this period is the transition from colostrum to mature breast milk. It becomes thicker and lighter, the content of fat and lactose (natural sugar) increases in it, and the calorie content increases. All this makes transitional milk an ideal food for the rapidly growing body of a newborn.
But despite the change in structure, transitional milk still contains a large amount of antibodies, living cells, beneficial bacteria and other biologically active substances necessary for the health of the child. 15
After four weeks: mature milk
By the time the baby is four weeks old, breast milk
has reached full maturity. It is rich in proteins, sugar, vitamins and minerals, as well as all kinds of biologically active components - hormones, growth factors, enzymes and living cells. All this ensures healthy growth and development of the child. 7
All this ensures healthy growth and development of the child. 7
After four weeks, the nutritional content and ingredient ratios of mature milk are generally fairly stable. However, the composition of milk at different times and in different feedings can still vary.
For example, if a mother or child is sick, the mother's body produces antibodies to the causative agents of this disease, and these antibodies pass into breast milk. And when the baby begins to explore the world and taste toys, the content of protective antibacterial enzymes in breast milk increases. 16 In other words, the composition of breast milk is adapted to the needs of the baby.
What is foremilk and hindmilk?
You may have noticed that milk becomes thicker towards the end of a feed. The fact is that as you feed, the fat content of milk gradually increases. This is due to the mechanical features of the movement of milk in the breast. The thick milk coming at the end of a feed is often referred to as "hind" milk, while the thinner milk at the beginning of a feed is often referred to as "fore". You might think that the transition from "front" milk to "back" occurs at some specific moment, but this is not so - the change in consistency occurs gradually. 15 Both types of milk are essential for a full serving and both are rich in vitamins, minerals, protein and sugar.
You might think that the transition from "front" milk to "back" occurs at some specific moment, but this is not so - the change in consistency occurs gradually. 15 Both types of milk are essential for a full serving and both are rich in vitamins, minerals, protein and sugar.
The fat content of milk depends on how full the breast is. At the beginning of feeding, the breasts can be filled more (and then the milk will be less fat) or less (and then the milk will be more fat). But do not worry about the amount of "forward" and "hind" milk - in general, every day the baby receives approximately the same amount of fat. 17
Composition of breast milk after six months
You may be wondering what will happen to milk during
prolonged breastfeeding. Will the body be able to produce high quality mature milk for months or even years? Answer: do not underestimate the possibilities of the mother's breast!
Although it is indeed time to start solid foods at six months of age to replenish the baby's stores of certain nutrients, such as iron, 18 breast milk still plays a big role in his diet.
For example, at the age of seven months, a baby still receives 93% of its calories from breast milk. And even between 11 and 16 months, mother's milk provides the baby with about half of the daily calorie intake. 19
So rest easy, breastfeeding will benefit you and your baby for many months.
Literature
1 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatric Clin North Am. 2013;60(1):49-74. Ballard O., Morrow AL, "Composition of breast milk: nutrients and biologically active factors". Pediatrician Clean North Am. 2013;60(1):49-74.
2 Hassiotou F et al. Cells in human milk: state of the science. J Human Lact . 2013;29(2):171-182. — Hassiot F. et al., "Breast Milk Cells: What the Science Knows." J Human Lact (Journal of the International Association of Lactation Consultants) . 2013;29(2):171-182.
2013;29(2):171-182.
3 Beck KL Comparative proteomics of human and macaque milk reveals species-specific nutrition during postnatal development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteom Res. 2015;14(5):2143-2157.
4 Zhang Z et al. Amino acid profiles in term and preterm human milk through lactation: a systematic review. Nutrients. 2013;5(12):4800-4821. - Amino acid profile of milk after term and preterm birth: a systematic review. Nutrients. 2013;5(12):4800-4821.
5 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci. 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep. " Nutr Neurosai. 2009;12(1):2-8.
" Nutr Neurosai. 2009;12(1):2-8.
6 Moukarzel S, Bode L. Human milk oligosaccharides and the preterm infant: a journey in sickness and in health. Clin perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):19 8-15. - Brandtzeg P., "The mucosal immune system and its integration with the mammary glands". J Pediatrician (Journal of Pediatrics). 2010;156(2):S8-15.
9 Uauy R et al. Essential fatty acids in early life: structural and functional role. Proc Nutr Soc . 2000;59(1):3-15. - Wye R. et al., "Essential Fatty Acids of the First Days of Life: Structural and Functional Role." Nutr Soc. 2000;59(1):3-15.
10 Alsaweed M et al. Human milk cells and lipids conserve numerous known and novel miRNAs, some of which are differentially expressed during lactation. PLoS One . 2016;11(4): e 0152610. - Alsavid M. et al., "Breast milk cells and lipids retain many known and unknown miRNAs, many of which show differential expression during lactation." PLOS One. 2016;11(4):e0152610.
PLoS One . 2016;11(4): e 0152610. - Alsavid M. et al., "Breast milk cells and lipids retain many known and unknown miRNAs, many of which show differential expression during lactation." PLOS One. 2016;11(4):e0152610.
11 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr . 1988;48(6):1375-1386. - Neville M.S. et al., "Female Lactation Study: Milk Quantity in Lactating Women at the Beginning and Peak of Lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
12 Marchbank T et al. Pancreatic secretory trypsin inhibitor is a major motogenic and protective factor in human breast milk. Am J Physiol Gastrointest Liver Physiol. 2009;296(4):G697-703. Marchbank T. et al., "Trypsin inhibitor in pancreatic secretion as the most important motogenic and protective factor in breast milk". Am Zh Physiol Gastrointest Liver Physiol. 2009;296(4):G697-703.
Am Zh Physiol Gastrointest Liver Physiol. 2009;296(4):G697-703.
13 Herrmann K, Carroll K. An exclusively human milk diet reduces necrotizing enterocolitis. breastmed. 2014;9(4):184-190. - Herrmann K, Carroll K, Exclusive breastfeeding reduces the risk of necrotizing enterocolitis. Brest Med (Breastfeeding Medicine). 2014;9(4):184-190.
14 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
15 Martin CR et al. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8(5):279. - Martin S.R. et al., Review of Infant Feeding Issues: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279.
- Martin S.R. et al., Review of Infant Feeding Issues: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5):279.
16 Montagne P et al. Changes in lactoferrin and lysozyme levels in human milk during the first twelve weeks of lactation. InBioactive components of human milk 2001 (pp. 241-247). Springer, Boston, MA. - Montagne, P. et al. "Changes in lactoferrin and lysozyme levels in breast milk during the first twelve weeks of lactation". In the collection "Biologically active components of breast milk" 2001 (pp. 241-247). Springer, Boston, Massachusetts.
17 Kent JC, et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of feedings and fat content of milk during the day". Pediatrix (Pediatrics). 2006;117(3):e387-395.
18 Kuo AA et al. Introduction of solid food to young infants. Matern child health J. 2011;15(8):1185-1194.- Kuo A.A. and co-authors. Complementary feeding. Matern child health (Maternal and child health). 2011;15(8):1185-1194.
Introduction of solid food to young infants. Matern child health J. 2011;15(8):1185-1194.- Kuo A.A. and co-authors. Complementary feeding. Matern child health (Maternal and child health). 2011;15(8):1185-1194.
19 Dewey KG Breast milk volume and composition during late lactation (7-20 months). J Pediatr Gastroenterol Nutr . 1984;3(5):713-720. — Dewey C.G. et al., "Amount and composition of breast milk in late lactation (7-20 months)". F Pediatrician Gastroenterol Nutr. 1984;3(5):713-720.
Breast milk and formula: what do they have in common?
1 Cribb VL et al. Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Klin Nutr. 2012;66(1):104.
Yur J Klin Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity." Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells. " Adv. 2014;5(6):770-778.
" Adv. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby. " Glycobiology (Glycobiology). 2012;22(9):1147-1162.
" Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimage. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR. Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263. - Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr . 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
- Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
25 Bener A et al. Does continuing breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatrician. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginekol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies. " Asia Pas W Cancer Prev. 2014;15(12):4829-4837.
" Asia Pas W Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs .