How long does listeria stay in your system
What Is Listeria Infection? Symptoms, Causes, Diagnosis, Treatment, and Prevention
Listeria is the name of a genus of bacteria that includes different types or “strains” that can contaminate food and cause a potentially life-threatening medical condition known as listeriosis.
“Listeriosis is a serious infection usually caused by eating food contaminated with the bacterium Listeria monocytogenes,” explains Jennifer Hunter, MPH, DrPH, an epidemiologist with the Centers for Disease Control and Prevention (CDC).
While cases of listeriosis are relatively rare — roughly 1,600 people are diagnosed with it each year, Dr. Hunter says — listeriosis can be lethal. About 260 of those 1,600 people die as a result of the infection. And it’s important to note that some groups of people — including pregnant women, older adults, and those with weakened immune systems — are at a higher risk of listeriosis infection than others.
Listeria Makes You Sick When You Eat Foods Contaminated With the Bacteria
Listeria bacteria are found pretty much everywhere. They turn up in water, soil, and even dust. Most species of listeria are not a problem for people.
The type of listeria that poses a grave threat to humans is Listeria monocytogenes. It tends to make its way into our systems when we eat contaminated foods. “Listeria monocytogenes can grow at refrigeration temperatures [whereas] most pathogens cannot,” says Linda Harris, PhD, a department chair and specialist in food microbiology at the University of California in Davis.
While many foods may be contaminated with nonthreatening amounts of Listeria monocytogenes, the bacteria’s ability to withstand cold conditions can allow small communities to reproduce and form colonies large enough to cause illness or a serious infection, explains Robert Buchanan, PhD, the director of the University of Maryland’s Center for Food Safety and Security Systems in Baltimore.
Estimates vary, but data suggests that tens of thousands or even millions of Listeria monocytogenes organisms usually have to be present to make a person sick.
Cooking kills listeria.
Also, when stored at proper temperatures — 40 degrees or below — listeria bacteria replicate slowly, Dr. Buchanan says. But the longer foods are stored in the refrigerator, the more the bacteria has the chance to grow.
The greatest food-based listeria risks are associated with ready-to-eat foods — meaning foods that don’t require cooking — that have been sitting around for a while in a person’s home or in some other food-storage environment (like a convenience store cooler). Deli meats, soft cheeses, unpasteurized dairy products, smoked meats, sprouts, and melon have all been the sources of listeria outbreaks, and are all considered high-risk foods.
Many foods that are left sitting out for a few hours at room temperatures — especially meats, cut fruit, and dairy foods — are risky. “At room temperature, listeria will double every 20 minutes,” Buchanan says. “In a refrigerator at 40 degrees, they double about once a day.”
Taking that into account, it’s important to eat foods soon after pulling them out of the fridge, and to refrigerate them as soon as possible if you’re not going to eat them, he says.
Once swallowed, Listeria monocytogenes is able to survive the acidic environment in the stomach and small intestine — an environment that kills most other types of harmful bacteria.
Listeria also possesses genes that allow it to penetrate the cells of the human GI tract, says Janet Donaldson, PhD, a professor of microbiology at the University of Southern Mississippi in Hattiesburg. This penetration can lead to listeriosis and the infection’s life-threatening complications.
Learn More About How and Why Listeria Makes You Sick
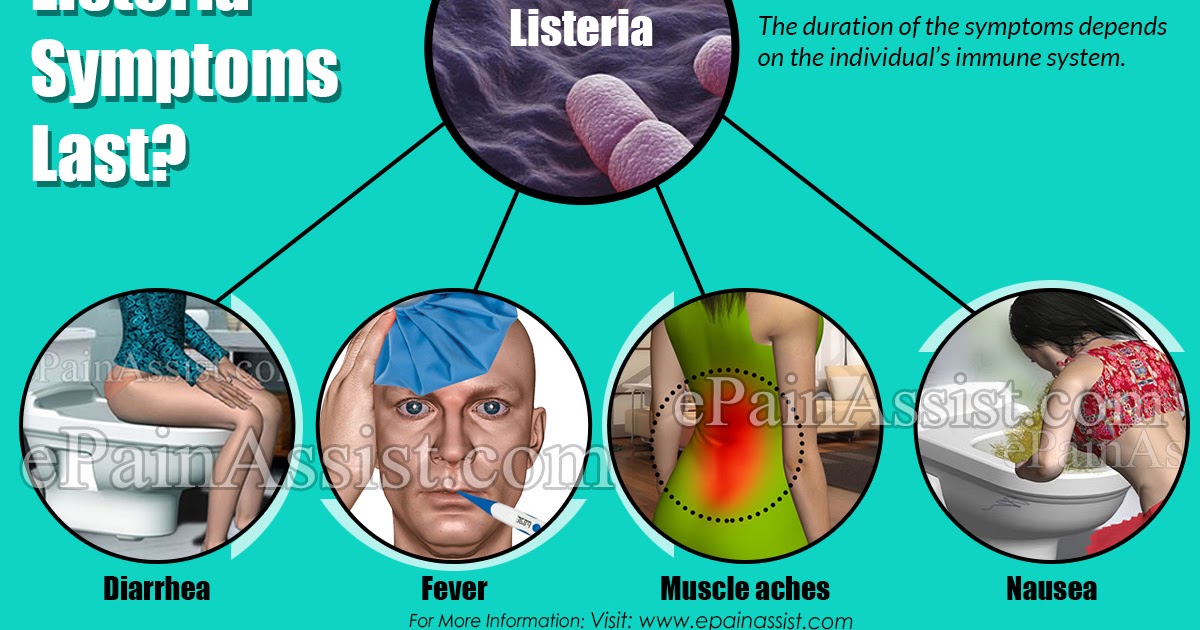
Signs and Symptoms of Listeria Infection
It’s possible that most people who are exposed to listeria don’t realize it. In healthy adults and kids, eating a food contaminated with listeria is likely to cause only mild flu-like symptoms — such as a stomachache, diarrhea, or slight fever.
In many healthy individuals, consuming the bacteria may cause no symptoms at all. Even if a healthy person does experience symptoms, these tend to go away on their own, though listeria-associated diarrhea can last up to five days.
But for older adults or those with compromised immune systems — including transplant patients, people taking immunosuppressant drugs, or those with immune-related health conditions like HIV, AIDS, or kidney disease — a listeria infection may start with mild flu-like symptoms and progress to more serious symptoms.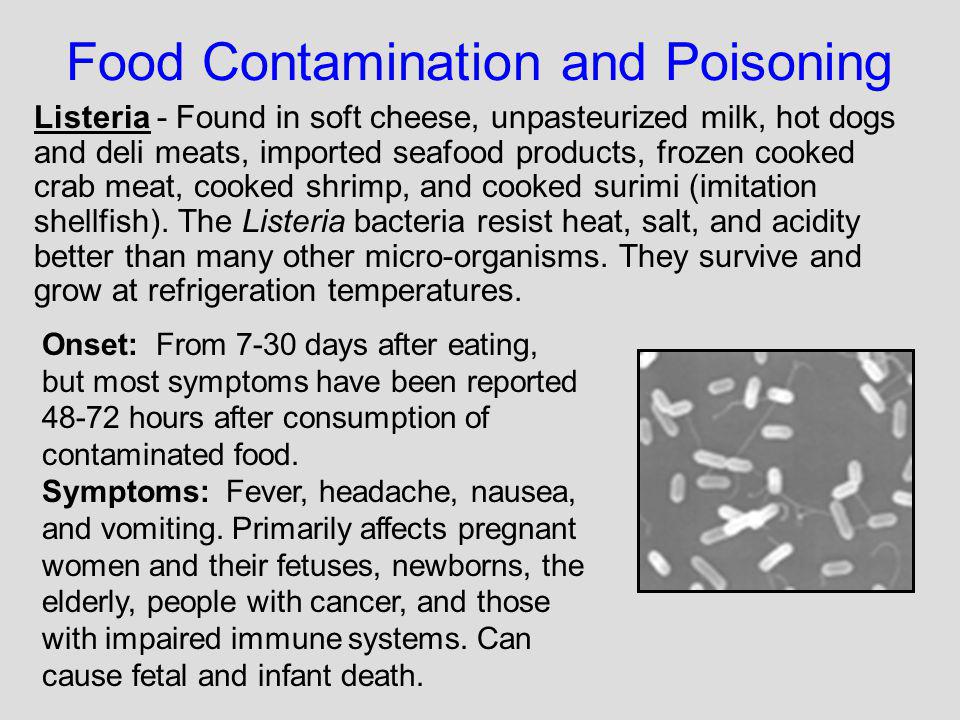
Signs of listeriosis may also include headaches, a stiff neck, confusion, loss of balance, and convulsions.
Anyone experiencing these symptoms — especially those who are pregnant, age 65 or older, or have a weakened immune system — and who may have been exposed to listeria should notify a doctor, according to the CDC.
For pregnant women who may have been exposed to a food contaminated with listeria, a fever of 100.6 degrees or higher is the most concerning symptom.
Learn More About the Signs and Symptoms of Listeriosis
Causes and Risk Factors for Listeria Infection
The Listeria monocytogenes bacteria is typically found in soil, water, and animal feces. Therefore, you’re most likely to develop listeriosis by eating contaminated fruits, vegetables, meats, and other animal products.
Past outbreaks of listeria were traced back to contaminated deli meats and hot dogs, whereas more recent outbreaks are often linked to unpasteurized milk and dairy products, as well as produce.
According to the CDC, the following foods are more likely to contain listeria:
- Queso fresco and other soft cheeses (Brie, Camembert, feta, queso blanco, queso panela, blue cheese)
- Raw or lightly cooked sprouts (alfalfa, clover, radish, mung bean)
- Melons
- Hot dogs and deli meats
- Smoked fish (unless canned or shelf-stable, or part of a cooked dish like casserole)
- Unpasteurized (raw) milk and dairy products (soft cheese, ice cream, and yogurt)
Anyone can get sick from these and other contaminated foods, but infants and young children, pregnant women, older adults, and people with weakened immune systems face a much higher risk of infection.
How Is Listeria Infection Diagnosed?
If your doctor suspects you may have listeriosis, he or she will typically take a sample of blood or spinal fluid for testing.
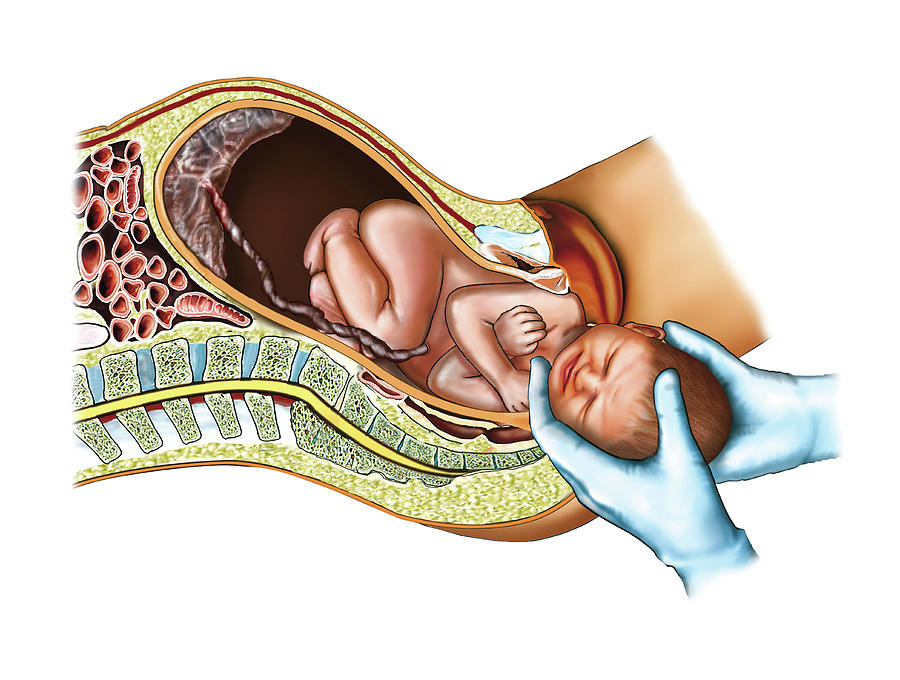
In the case of pregnant women with a fever and other signs and symptoms of listeriosis, the doctor may also gather samples from the placenta in the event of delivery.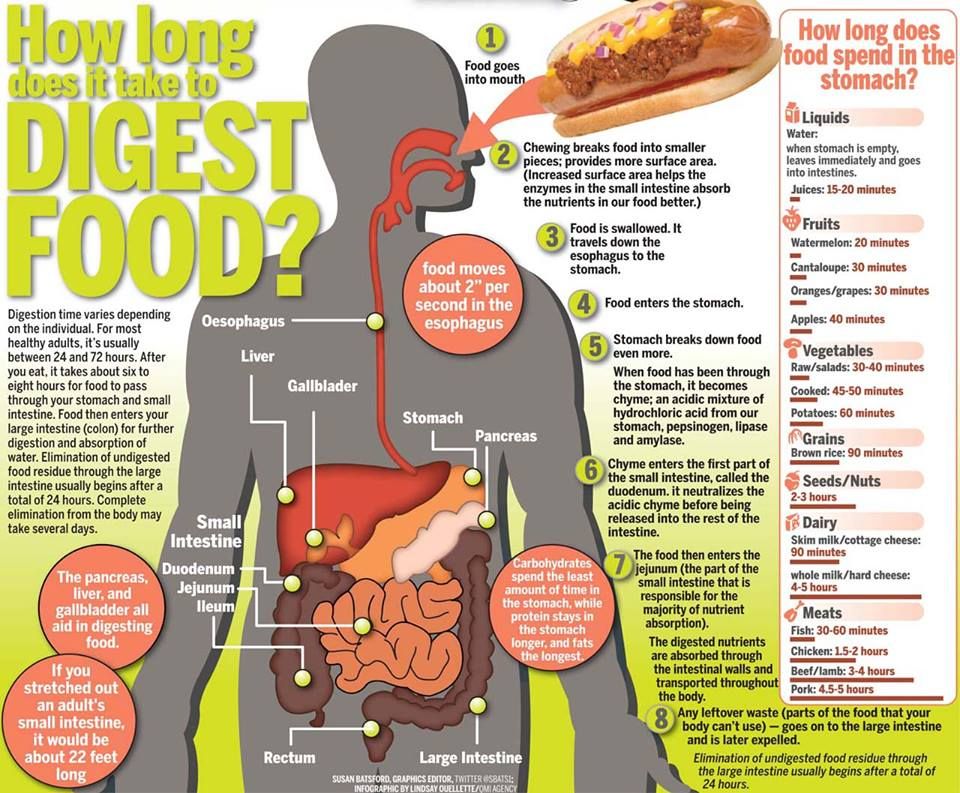
If your results indicate a listeria infection, your doctor will create an appropriate treatment for you; but some people with mild symptoms may not need to be treated at all.
Duration of Listeria Infection
The duration of listeriosis can vary greatly, depending on the severity of the infection. After a person eats food contaminated with listeria, it can take anywhere between a few hours to 30 days or more for symptoms to appear.
Symptoms may appear without warning.
In milder cases, symptoms (like diarrhea, nausea, and vomiting) may resolve after just a few days, whereas more severe cases could last several weeks.
In fact, more serious forms of listeriosis — like blood infection or encephalitis — can take anywhere between three days and three months to develop, resulting in symptoms like headache, stiff neck, confusion, loss of balance, and even convulsions.
Treatment and Medication Options for Listeria Infection
Most healthy patients who are exposed to listeria and develop symptoms will not require any sort of treatment. Their immune system will eradicate the bacteria, and symptoms will tend to go away within three days, though they may last as long as one week.
If symptoms do not go away in that amount of time, it’s a good idea to check with your doctor to make sure the infection is not spreading or to determine what else could be causing the problems.
But pregnant women, seniors, and immunocompromised patients who experience symptoms and suspect they’ve been exposed to listeria should see a doctor as soon as possible. If they test positive for a listeria infection, the most common treatment is a 14- to 21-day course of intravenous antibiotics.
In many cases, these individuals will require hospitalization so that doctors can closely monitor their condition, says Rob Danoff, DO, a family physician and the program director of the family practice residency at Philadelphia’s Jefferson Health.
In some cases — such as when a pregnant woman develops a fever and other symptoms after eating a food known to be contaminated with listeria — doctors may prescribe intravenous antibiotics while they wait for test results to confirm the presence of the bacteria.
It’s important to note that eating a food implicated in a listeria outbreak does not mean a person should start taking antibiotics. Even for older or immunocompromised individuals, antibiotic treatment is usually not recommended unless symptoms emerge.
Learn More About Treatment for Listeria Infections
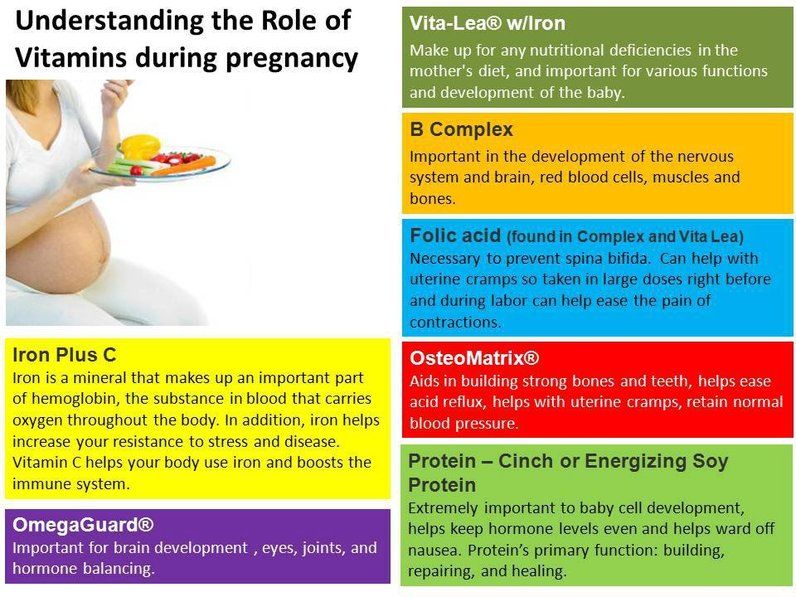
Listeria Infections Can Be Much More Dangerous if You’re PregnantPregnant women are roughly 10 times more likely to develop listeriosis than the average person.
Why? Pregnancy causes changes to a woman’s immune system that may make her more vulnerable to infections like listeriosis.
While listeriosis can cause mild flu-like symptoms in pregnant women, it may not cause any symptoms at all, according to the CDC’s Hunter.
RELATED: How to Tell the Flu From a Common Cold or Something Else
But pregnant women can pass the infection to their unborn babies, Hunter says. And this can result in miscarriage, stillbirth, or preterm labor — as well as sepsis (a blood infection) or meningitis (inflammation of the membranes surrounding the brain and spinal cord) in a newborn.
“Listeriosis during pregnancy results in fetal loss in about 20 percent of cases and newborn death in about 3 percent of cases,” she says.
Hispanic women are at especially high risk of developing pregnancy-associated listeriosis — a risk that may stem from the consumption of unpasteurized cheeses, such as queso fresco or queso blanco.
Learn More About Specific Listeria Risks in Pregnant Women
Prevention of Listeria InfectionTo protect yourself from the bacteria, the CDC recommends avoiding foods that come with a high risk of Listeria monocytogenes contamination. These include dairy products made with unpasteurized milk, raw sprouts, cut melon that has been left out for several hours at room temperature, ready-to-eat meat products that have been sitting open in your fridge for more than five days (approximately), and refrigerated meat spreads and smoked seafoods.
Other important safety tips include:
- Always cook or heat meat products before eating them.
- Promptly refrigerate any foods you’re not going to eat right away.
- If you handle or prepare raw meat, be sure to wash your hands and any food prep equipment before you work with other foods.
It’s important to pay attention to news of listeria outbreaks in your area.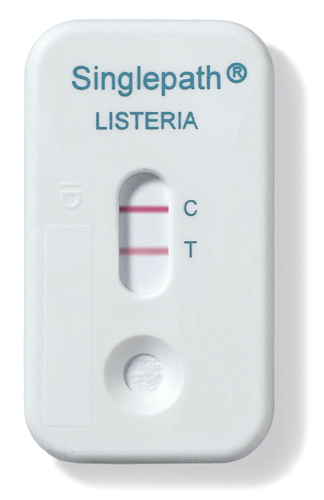 The U.S. Department of Health and Human Services offers info about all food-related recalls and health issues at FoodSafety.gov, and you can sign up for automatic alerts about listeria concerns in your region.
The U.S. Department of Health and Human Services offers info about all food-related recalls and health issues at FoodSafety.gov, and you can sign up for automatic alerts about listeria concerns in your region.
New technologies, like whole genome sequencing, link pathogens causing illnesses in people to their contaminated food sources, allowing those foods to be removed from store shelves and homes more quickly.
Whole genome sequencing is the process of fully mapping a living organism’s genetic code.
Public health experts today use this form of genetic testing to track listeria outbreaks and better understand how the bacteria make people sick. Eventually, it may help public health experts prevent outbreaks from happening in the first place.
“There are many, many different genetic variants of listeria,” says Donaldson. While some of these strains can cause very serious infections in humans — even when consumed in small numbers — others are harmless, she says. By mapping and studying the DNA of each of these strains, she and others can better predict where listeria may show up and also how to prevent it from contaminating food. “With whole genome sequencing, listeria outbreaks can be detected when as few as two people have gotten sick,” the CDC reports.
By mapping and studying the DNA of each of these strains, she and others can better predict where listeria may show up and also how to prevent it from contaminating food. “With whole genome sequencing, listeria outbreaks can be detected when as few as two people have gotten sick,” the CDC reports.
Learn More About How to Prevent Listeria Infection
Complications of Listeria Infection
While most cases of listeriosis are mild, some can lead to life-threatening complications, especially in pregnant women, older adults, and people with weakened immune systems.
In pregnant women, listeriosis can cause:
- Miscarriage
- Stillbirth
- Premature birth
- Life-threatening infections in newborns, including blood infection, pneumonia, and meningitis
People over 65 and those who are immunocompromised face a greater risk of severe complications from listeriosis, including:
- Sepsis (infection of the blood)
- Meningitis (inflammation of the membranes surrounding the brain and spinal cord)
- Encephalitis (inflammation of the brain)
People who develop complications from listeriosis typically require immediate medical care. For one in five people, a serious infection is fatal.
For one in five people, a serious infection is fatal.
Research and Statistics: Who Gets Listeria Infection?
Listeria is the third leading cause of food poisoning death in the United States, killing an estimated 260 out of 1,600 people affected every year. Still, listeriosis is considered rare, according to the U.S. Food and Drug Administration (FDA).
It’s hard to pinpoint the actual incidence of listeriosis, as symptoms may be mistaken for the flu or gastroenteritis (inflammation of the lining of the intestines caused by a virus or bacteria).
Pregnant women are roughly 10 times more likely to develop listeriosis than the average person, while pregnant Hispanic women are 24 times more likely.
Meanwhile, people ages 60 and older are 2.6 times more likely to get listeriosis than the general healthy population.
Related Conditions of Listeria Infection
In otherwise healthy people, listeriosis is mainly associated with mild flu-like symptoms like diarrhea, stomachache, and slight fever, which may lead people to mistake listeriosis for the flu or gastrointestinal (GI) issues.
In high-risk populations — which include newborns, older adults, and people with weakened immune systems — listeriosis can lead to life-threatening conditions, such as sepsis, encephalitis, and meningitis.
Resources We Love
Centers for Disease Control and Prevention
As one of the leading health organizations in the United States, the CDC tracks listeriosis outbreaks, offers answers to the most common questions, and outlines a list of the riskiest foods. You can also keep tabs on CDC projects like whole genome sequencing, which aims to prevent foodborne-illness outbreaks like listeriosis.
KidsHealth From Nemours
KidsHealth.org offers doctor-reviewed advice on hundreds of topics, free lesson plans and programs for educators, and tools like videos and slideshows to help families stay healthy. Check out their informational page on listeria infections, which outlines steps to take if you suspect your child has eaten contaminated food.
Mayo Clinic
Whatever you want to know about listeria infections, the Mayo Clinic has you covered. This site provides info on risk factors, symptoms, diagnosis, and treatment options, as well as tips to help you prepare for an appointment with your doctor.
U.S. Food and Drug Administration
Want to know how to keep listeria out of your food? The FDA outlines which foods are no-no’s and offers key food safety tips to reduce the risk of contamination. You’ll also find advice for maintaining your kitchen and refrigerator as clean, sanitary spaces.
U.S. National Library of Medicine
Have a question about listeria and listeriosis? The U.S. National Library of Medicine will direct you to a number of high-quality government and nongovernment health agencies — like the FDA, CDC, and Mayo Clinic — to help you fill in the blanks. You’ll also find information about clinical trials, journal articles, and high-risk groups.
Additional reporting by Lauren Bedosky.
Editorial Sources and Fact-Checking
- Listeria: Questions and Answers. Centers for Disease Control and Prevention (CDC). December 12, 2016.
- Listeria: Pregnant Women and Newborns. CDC. December 12, 2016.
- Bortolussi R. Listeriosis: A Primer. Canadian Medical Association Journal. October 7, 2008.
- Volokhov D, Rasooly A, Chumakov K, et al. Identification of Listeria Species by Microarray-Based Assay. Journal of Clinical Microbiology. December 2002.
- Get the Facts About Listeria. U.S. Food and Drug Administration (FDA). August 3, 2020.
- What You Need to Know About Preventing Listeria Infections. FDA. March 22, 2018.
- Listeria: Prevention. CDC. June 17, 2019.
- Gahan C, Hill C. Listeria Monocytogenes: Survival and Adaptation in the Gastrointestinal Tract. Frontiers in Cellular and Infection Microbiology. February 5, 2014.

- Listeria: Symptoms. CDC. December 12, 2016.
- Listeria: People at Risk. CDC. December 12, 2016.
- Listeria Infection. Mayo Clinic. January 18, 2020.
- Committee Opinion: Management of Pregnant Women with Presumptive Exposure to Listeria Monocytogenes. American College of Obstetricians and Gynecologists. December 2014.
- Listeria: Diagnosis and Treatment. CDC. December 12, 2016.
- Listeria: Questions and Answers. CDC. December 12, 2016.
- Listeria Infection/Listeriosis: Management and Treatment. Cleveland Clinic. February 26, 2018.
- Listeria (Listeriosis). FDA. March 29, 2019.
- Ooi ST, Lorber B. Gastroenteritis Due to Listeria Monocytogenes. Clinical Infectious Diseases. May 1, 2005.
- Listeria: Patient Management. CDC. December 12, 2016.
- Mor G, Cardenas I. The Immune System in Pregnancy: A Unique Complexity. American Journal of Reproductive Immunology. June 2010.
- Listeria: People with Weakened Immune Systems.
 CDC. December 12, 2016.
CDC. December 12, 2016. - Advanced Molecular Detection: Food Safety. CDC. October 15, 2019.
- Whole Genome Sequencing (WGS) Program. FDA. February 14, 2018.
- Listeria: The Listeria Whole Genome Sequencing Project. CDC. May 17, 2016.
Show Less
Listeria Infection in Pregnancy
By Markham HeidHow Listeria Outbreaks Are Tracked
By Markham HeidHow (and When) Doctors Diagnose and Treat Listeria Infection
By Markham HeidTips for Preventing Listeria Infection
By Markham HeidListeria Infection: Signs and Symptoms
By Markham HeidCDC Links Listeria Outbreak to Ice Cream Sold in Florida
The Centers for Disease Control and Prevention has traced a recent listeria outbreak to ice cream manufactured by Florida-based Big Olaf Creamery.
By Lisa Rapaport
Listeria Outbreak Linked to Deli Meat
Cases — identified in Massachusetts, New York, and Florida — have mostly been among the elderly. The CDC has yet to pinpoint exact contaminated products...
By Don Rauf
What Listeria Is and Why It Makes You Sick
By Markham HeidListeria infection (listeriosis) - Symptoms and causes
Overview
Listeria infection is a foodborne bacterial illness that can be very serious for pregnant women, people older than 65 and people with weakened immune systems. It's most commonly caused by eating improperly processed deli meats and unpasteurized milk products.
Healthy people rarely become ill from listeria infection, but the disease can be fatal to unborn babies, newborns and people with weakened immune systems.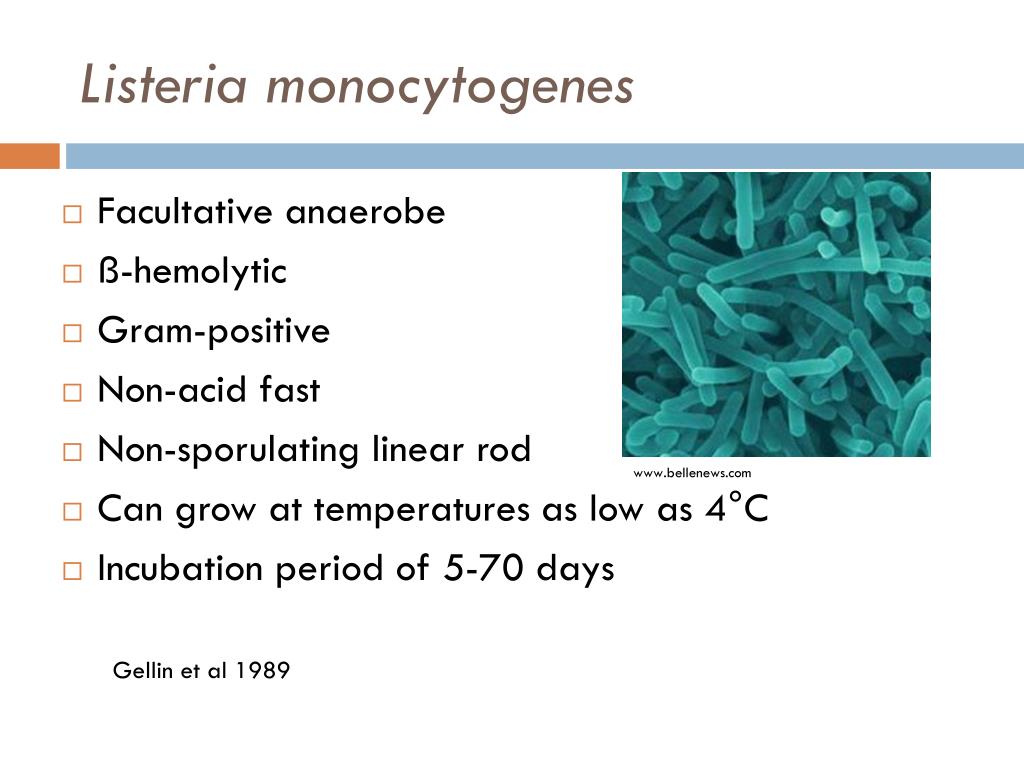 Prompt antibiotic treatment can help curb the effects of listeria infection.
Prompt antibiotic treatment can help curb the effects of listeria infection.
Listeria bacteria can survive refrigeration and even freezing. So people who are at higher risk of serious infections should avoid eating the types of food most likely to contain listeria bacteria.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
If you develop a listeria infection, you might have:
- Fever
- Chills
- Muscle aches
- Nausea
- Diarrhea
Symptoms might begin a few days after you've eaten contaminated food, but it can take 30 days or more before the first signs and symptoms of infection begin.
If the listeria infection spreads to your nervous system, signs and symptoms can include:
- Headache
- Stiff neck
- Confusion or changes in alertness
- Loss of balance
- Convulsions
Symptoms during pregnancy and in newborns
During pregnancy, a listeria infection is likely to cause only mild signs and symptoms in the mother. The consequences for the baby, however, can be devastating — the baby can die in the womb or have a life-threatening infection within a few days of being born.
The consequences for the baby, however, can be devastating — the baby can die in the womb or have a life-threatening infection within a few days of being born.
Signs and symptoms of a listeria infection in a newborn can be subtle, but can include:
- Little interest in feeding
- Irritability
- Fever
- Vomiting
- Difficulty breathing
When to see a doctor
If you've eaten a food that's been recalled because of a listeria outbreak, watch for signs or symptoms of illness. If you have a fever, muscle aches, nausea or diarrhea, contact your doctor. The same goes for illness after eating a potentially contaminated product, such as foods made with unpasteurized milk or poorly heated hot dogs or deli meats.
If you have a high fever, severe headache, stiff neck, confusion or sensitivity to light, seek emergency care. These signs and symptoms can indicate bacterial meningitis, a life-threatening complication of a listeria infection.
Request an Appointment at Mayo Clinic
Causes
Listeria bacteria can be found in soil, water and animal feces. People can get infected by eating the following:
- Raw vegetables that have been contaminated from the soil or from contaminated manure used as fertilizer
- Contaminated meat
- Unpasteurized milk or foods made with unpasteurized milk
- Certain processed foods — such as soft cheeses, hot dogs and deli meats that have been contaminated after processing
Unborn babies can contract a listeria infection from the mother.
Risk factors
Pregnant women and people who have weak immune systems are at highest risk of contracting a listeria infection.
Pregnant women and their babies
Pregnant women are much more susceptible to listeria infections than are other healthy adults. Although a listeria infection might cause only a mild illness in pregnant women, consequences for their babies can include:
- Miscarriage
- Stillbirth
- Premature birth
- A potentially fatal infection after birth
People who have weak immune systems
This category includes people who:
- Are older than 65
- Have AIDS
- Are receiving chemotherapy
- Have diabetes or kidney disease
- Take high-dose prednisone or certain rheumatoid arthritis drugs
- Take medications to block rejection of a transplanted organ
Complications
Most listeria infections are so mild they can go unnoticed. However, in some cases, a listeria infection can lead to life-threatening complications, including:
However, in some cases, a listeria infection can lead to life-threatening complications, including:
- Generalized blood infection
- Inflammation of the membranes and fluid surrounding the brain (meningitis)
Prevention
To prevent a listeria infection, follow simple food safety guidelines:
- Keep things clean. Wash your hands thoroughly with warm, soapy water before and after handling or preparing food. After cooking, use hot, soapy water to wash the utensils, cutting boards and other food preparation surfaces.
- Scrub raw vegetables. Clean raw vegetables with a scrub brush or vegetable brush under plenty of running water.
- Cook your food thoroughly. Use a food thermometer to make sure your meat, poultry and egg dishes are cooked to a safe temperature.
Precautions for people particularly at risk
If you're pregnant or you have a weak immune system, be particularly cautious about listeria. Take additional precautions with these types of foods:
Take additional precautions with these types of foods:
- Soft cheeses and Mexican-style cheeses. Don't eat soft cheeses such, as feta, brie, Camembert or blue cheese, or Mexican-style cheeses such as queso blanco and queso fresco, unless it's clear from the packaging that the product was made using pasteurized milk.
- Hot dogs and deli meats. Avoid these unless they're reheated until steaming hot. Keep fluid from hot dog packages away from other foods, utensils and food preparation surfaces. Wash your hands after handling these products.
- Meat spreads. Don't eat refrigerated meat spreads. Canned or shelf-stable — meaning they can be safely stored at room temperature — meat spreads are acceptable. Refrigerate after opening.
- Smoked seafood. These products can be labeled as nova style, lox, kippered or jerky. It's OK to eat them in cooked dishes. Canned or shelf-stable smoked seafood is acceptable.

- Raw or lightly cooked sprouts. Cook sprouts of any kind thoroughly.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Listeriosis (Listeria monocytogenis) (qualitative DNA determination)
Article Rating: 5.00 (54)
Description Training
Listeriosis (synonyms: listerellosis, Tigris river disease, neurollosis, neonatal granulomatosis) is an infectious disease from the group of zoonoses. In humans, the disease occurs either in the form of acute sepsis (with damage to the central nervous system, tonsils, lymph nodes, liver, spleen), or in a chronic form (erased).
The causative agent of the disease was first described by S. Halfes (1911). It was singled out by D. Murray et al. (1926) from sick rabbits and guinea pigs in the nursery of the University of Cambridge; in connection with the ability to cause pronounced monocytosis in the experiment, the pathogen received the species name monocytogenes. The name of the genus Listeria (in honor of Joseph Lister) was proposed by W. Peary (1927), who studied the pathogen of rodent epizootics in South Africa. In 1929, A. Niefellt isolated bacteria from a person suffering from tonsillitis with high monocytosis. Later, K. Bern observed cases of the disease caused by them in puerperas and newborns (1935).
The name of the genus Listeria (in honor of Joseph Lister) was proposed by W. Peary (1927), who studied the pathogen of rodent epizootics in South Africa. In 1929, A. Niefellt isolated bacteria from a person suffering from tonsillitis with high monocytosis. Later, K. Bern observed cases of the disease caused by them in puerperas and newborns (1935).
The causative agent is a mobile non-spore-forming gram-positive bacillus Listeria monocytogenes - a type species of the genus Listeria. It can form a capsule, transform into L-forms and parasitize inside cells, causing a slow latent development of infection. Listeria are microaerophiles, unpretentious and grow on ordinary media even at room temperature. They have a set of somatic and flagellar antigens, which makes it possible to distinguish among them 7 main serovars, many of which are divided into subtypes. Listeria 1-4 serovars are the most common. Bacteria are pronounced saprophytes and are highly stable in the external environment. They tolerate low temperatures well, as psychrophilic microorganisms are able to multiply at 4-6 ° C in various objects (soil, water, plants, corpses and food products). For a long time withstand 6-20% concentration of sodium chloride. The sun's rays inactivate them for 2-15 days, a 2.5% solution of formalin or NaOH - after 20 minutes, a solution of bleach (100 mg of active chlorine in 1 l) - after 1 hour. At 62 "C they die after 35 minutes, at 100 ° C - within 5-10 minutes. They are sensitive to broad-spectrum antibiotics, although strains resistant to them are also known.
They tolerate low temperatures well, as psychrophilic microorganisms are able to multiply at 4-6 ° C in various objects (soil, water, plants, corpses and food products). For a long time withstand 6-20% concentration of sodium chloride. The sun's rays inactivate them for 2-15 days, a 2.5% solution of formalin or NaOH - after 20 minutes, a solution of bleach (100 mg of active chlorine in 1 l) - after 1 hour. At 62 "C they die after 35 minutes, at 100 ° C - within 5-10 minutes. They are sensitive to broad-spectrum antibiotics, although strains resistant to them are also known.
The reservoir and sources of infection are many species of wild and synanthropic rodents, as well as various environmental objects. The disease affects domestic and farm animals (pigs, small and large cattle, horses, rabbits, less often cats and dogs), as well as domestic and ornamental birds (geese, chickens, ducks, turkeys, pigeons, parrots and canaries). Listeria are found in foxes, minks, raccoons, arctic foxes, wild ungulates, birds, fish and seafood, and in many natural environments. A particularly favorable environment for their reproduction is the surface layers of low-quality silage. The pathogen is excreted from the body with various secrets (urine, milk, blood, semen, cerebrospinal fluid, rectal mucus, amniotic fluid, etc.). The period of infectiousness of animals lasts indefinitely. An infected person can be a source of perinatal and neonatal pathology. Women in childbirth and newborns can excrete the pathogen within 10-12 days after birth.
A particularly favorable environment for their reproduction is the surface layers of low-quality silage. The pathogen is excreted from the body with various secrets (urine, milk, blood, semen, cerebrospinal fluid, rectal mucus, amniotic fluid, etc.). The period of infectiousness of animals lasts indefinitely. An infected person can be a source of perinatal and neonatal pathology. Women in childbirth and newborns can excrete the pathogen within 10-12 days after birth.
The transmission mechanism is diverse (fecal-oral, contact, airborne, transplacental), the main one is fecal-oral. Animals become infected through water and feed contaminated with Listeria, from rodents or their corpses. Blood-sucking insects, especially pasture mites, play a certain role in maintaining stationary foci of the disease. Infected from rodents and other sick animals, they contribute to the spread of infection by transmitting bacteria to other animals.
Mechanisms of infection of people are diverse. More often, infection occurs through the alimentary route through contaminated water and food products of animal origin, especially in the absence of their reliable heat treatment and long-term storage at relatively low temperatures. Possibly, infection at the use in food of fresh vegetables. The possibility of aerogenic contamination occurring during the processing of animal raw materials (wool, bristles, leather, skins, feathers, down) has been established. A contact route of transmission is known, which is carried out through cuts and abrasions on the skin when various secretions of sick animals enter them. The possibility of transmission of bacteria from person to person has been identified, cases of infection through sexual contact have been described. Listeriosis is especially dangerous for pregnant women due to perinatal transmission of the pathogen from mother to child (transplacental or during childbirth). Cases of postpartum aerogenic, contact and food infection of newborns from the mother, medical personnel or environmental objects infected by them are described.
More often, infection occurs through the alimentary route through contaminated water and food products of animal origin, especially in the absence of their reliable heat treatment and long-term storage at relatively low temperatures. Possibly, infection at the use in food of fresh vegetables. The possibility of aerogenic contamination occurring during the processing of animal raw materials (wool, bristles, leather, skins, feathers, down) has been established. A contact route of transmission is known, which is carried out through cuts and abrasions on the skin when various secretions of sick animals enter them. The possibility of transmission of bacteria from person to person has been identified, cases of infection through sexual contact have been described. Listeriosis is especially dangerous for pregnant women due to perinatal transmission of the pathogen from mother to child (transplacental or during childbirth). Cases of postpartum aerogenic, contact and food infection of newborns from the mother, medical personnel or environmental objects infected by them are described.
The natural susceptibility of people is low. Diseases occur most often in the elderly, newborns, in people with immunodeficiencies. Postinfectious immunity is weakly expressed.
Main epidemiological signs. The disease has all the features of a saprozoonotic infection and is widespread everywhere. Most often it is found in areas with a temperate climate and soils rich in organic fertilizers. The spread of listeriosis is facilitated by large-scale human economic activity associated with the introduction of advanced soil cultivation technology, the construction of livestock complexes, feed mills, centralized enterprises for the processing and sale of raw materials of animal origin, food warehouses and storage facilities. In Russia, 50-80 cases of listeriosis are registered annually, which does not reflect the actual incidence rate. Sporadic and group diseases are possible. The risk group includes pregnant women and newborns. The incidence is professional in nature among workers of livestock and poultry farms, as well as primary processing shops at meat and poultry plants. The incidence is more often recorded in the spring-summer period. As nosocomial infections, listeriosis is most relevant for obstetric hospitals, where sporadic cases and outbreaks of listeriosis have occurred, and pregnant women and newborns are considered risk groups.
The incidence is more often recorded in the spring-summer period. As nosocomial infections, listeriosis is most relevant for obstetric hospitals, where sporadic cases and outbreaks of listeriosis have occurred, and pregnant women and newborns are considered risk groups.
The entrance gates of infection can be the mucous membranes of the gastrointestinal tract and respiratory tract, eyes, as well as damaged skin. With lymphogenous and hematogenous spread of pathogens, an acute febrile condition occurs, and listeria is fixed in the lymph nodes and internal organs - tonsils, lungs, liver and spleen, kidneys and adrenal glands, central nervous system, etc., where bacteria multiply.
The inflammatory process in the lymph nodes is accompanied by their increase, but suppuration does not develop. In severe cases, the disease acquires the features of listeriosis sepsis; at the same time, small numerous necrotic nodules (listeriomas) are formed in the lymph nodes and internal organs (including the central nervous system), which include listerium, reticular and monocytic cells, nuclear detritus, altered polymorphonuclear leukocytes.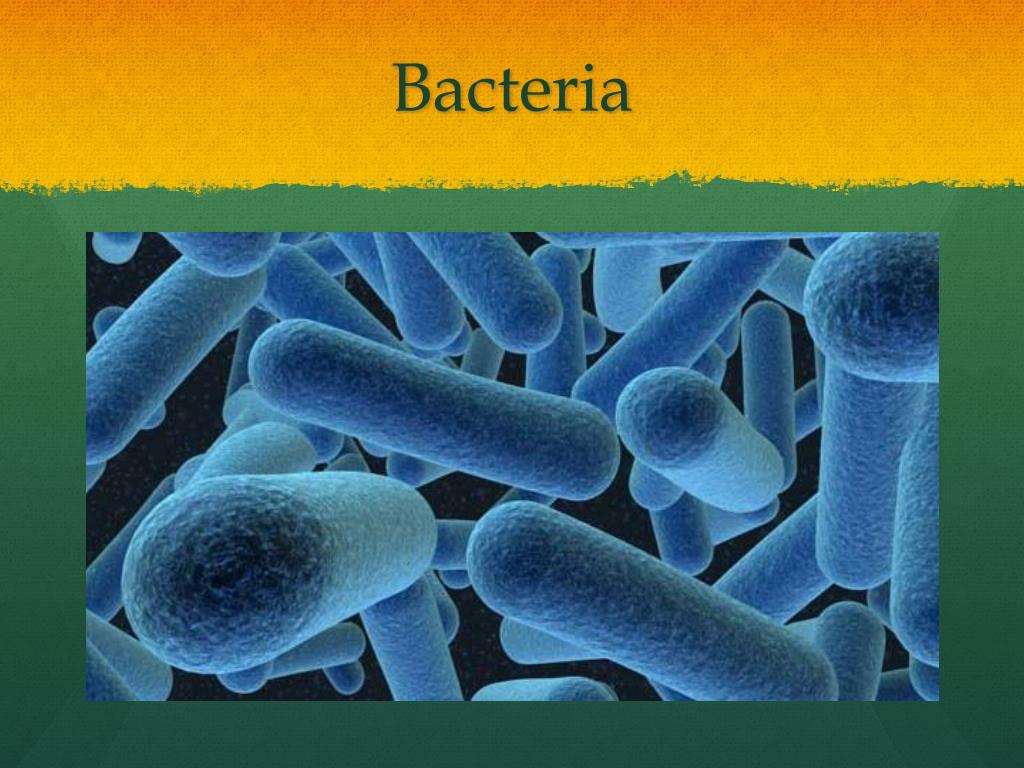 During pregnancy, listeriomas can form in the placenta, which subsequently leads to infection of the fetus with the development of a generalized form of infection. The occurrence of the disease is facilitated by immunodeficiency states and tumors. Those who have been ill develop persistent post-infection immunity.
During pregnancy, listeriomas can form in the placenta, which subsequently leads to infection of the fetus with the development of a generalized form of infection. The occurrence of the disease is facilitated by immunodeficiency states and tumors. Those who have been ill develop persistent post-infection immunity.
The disease can acquire an acute, subacute, chronic and abortive course, usually prone to recurrence. The following main clinical forms of listeriosis are distinguished: anginal-septic, nervous, ocular-glandular, septic-granulomatous (in fetuses and newborns), mixed. Cases of long-term asymptomatic listeriosis carriage are known.
incubation period. Varies from a few days to 1.5 months.
Anginal-septic form . Met most frequently. The main clinical manifestation is angina. It can be catarrhal or follicular, clinically indistinguishable from angina of streptococcal etiology. Usually in such cases, the disease proceeds favorably within 5-7 days and ends with a complete recovery.
With ulcerative membranous listeriosis tonsillitis, body temperature rises to 38.5-39 "C, cough and runny nose are possible, sore throat is characteristic. Patients notice a bright hyperemia of the mucous membrane of the oropharynx, an increase and looseness of the tonsils, the formation of membranous deposits or ulcers on them, covered with films.Regional lymph nodes are enlarged, painful on palpation.Ulcerative membranous angina is characterized by hemogram changes - leukocytosis, an increase in ESR, and especially an increase in the number of mononuclear cells (up to 70% or more).The duration of the disease in cases of its favorable course is 12-14 days .
At the same time, ulcerative membranous and much less often follicular listeriosis tonsillitis, with the progression of the process, can lead to the development of sepsis, which is observed mainly in adults. High fever takes on a relapsing character, facial flushing, conjunctivitis, a polymorphic rash on the skin, and white plaque on the tonsils are noted. Hepatolienal syndrome develops, in some cases mild meningeal symptoms appear. In blood the expressed monocytosis remains. The outcome of listeriosis sepsis with timely and complete treatment is favorable.
Hepatolienal syndrome develops, in some cases mild meningeal symptoms appear. In blood the expressed monocytosis remains. The outcome of listeriosis sepsis with timely and complete treatment is favorable.
Nervous form . Manifested in the form of listeriosis meningitis, meningoencephalitis or brain abscess. The clinical characteristics of these conditions do not differ significantly from the corresponding nosological forms of a different bacterial etiology. Monocytosis in the peripheral blood is noted in the nervous form of the disease only in its early period, later leukocytosis and granulocytosis are detected. The cerebrospinal fluid usually remains clear, cerebrospinal fluid pressure and protein content are increased, cytosis is mixed, glucose and chloride values change slightly.
It is possible to observe lesions of the peripheral nervous system - paresis and paralysis of individual muscle groups, polyradiculoneuritis.
In immunodeficiency states, including HIV infection, the nervous form of listeriosis manifests itself as an opportunistic infection.
Oculo-glandular form. Rarely seen; it usually results from contact with infected animals. Patients have an increase in body temperature, a decrease in visual acuity. Conjunctivitis develops with conjunctival edema and numerous follicles on it, eyelid edema, narrowing of the palpebral fissure, enlargement and slight soreness of the parotid and cervical lymph nodes. The cornea remains unchanged. The disease proceeds for a long time, from 1 to 3 months.
Septic-granulomatous form. Observed in fetuses and newborns. During pregnancy, listeriosis can occur in erased and atypical forms or as an asymptomatic carrier, and in such cases remains unrecognized. With intrauterine infection of the fetus in the early stages of pregnancy, its death or severe developmental anomalies (hydrocephalus, microgyria, etc.) is possible.
Listeriosis of newborns is distinguished by a severe course. It is manifested by high fever, respiratory and circulatory disorders: dyspnea, cyanosis, deafness of heart sounds. Vomiting, mucous stools, roseolous-papular exanthema are possible. With the development of purulent meningitis, a fatal outcome is most often observed. Clinically, listeriosis of the newborn is rarely recognized due to its similarity to other intrauterine infections.
Vomiting, mucous stools, roseolous-papular exanthema are possible. With the development of purulent meningitis, a fatal outcome is most often observed. Clinically, listeriosis of the newborn is rarely recognized due to its similarity to other intrauterine infections.
In infants, listeriosis begins as an acute respiratory viral infection with fever, runny nose, cough, then small-focal bronchopneumonia or purulent pleurisy develops. In some patients, maculo-papular exanthema, liver enlargement, jaundice, meningeal symptoms, sometimes convulsions, paralysis are noted. Characteristic monocytosis in the hemogram is rare.
When recovering from this form of listeriosis, 15-20% of children have disorders of the peripheral nervous system and central nervous system.
Chronic listeriosis. Differs in the scarcity of clinical manifestations during exacerbations of the disease: short-term fever with catarrhal phenomena is observed, quite often dyspeptic disorders or sometimes symptoms of chronic pyelonephritis.
Depending on the type of biomaterial Preparation rules see here
By using gemohelp.ru, you agree to the use of cookies
Confirm
More details
Paracytophagy: capture without detection
Bio/mol/text contest entry: Intracellular pathogens prefer not to enter the extracellular space. Listeria monocytogenes will tell you how to use other people's resources, disguise yourself and not leave the shadows.
This work was published in the "Free Topic" nomination of the "bio/mol/text"-2017 competition.
The general sponsor of the competition is the Diaem company: the largest supplier of equipment, reagents and consumables for biological research and production.
The sponsor of the audience award and the partner of the Biomedicine Today and Tomorrow nomination was Invitro.
"Book" sponsor of the competition - "Alpina non-fiction"
Nature is clever at inventions: even organisms consisting of only one cell - bacteria - are fraught with a lot of amazing ways to survive in an environment that does not welcome them. They suppress phagocytosis directed against them, destroy the membranes of host cells, block the release of neurotransmitters, mask themselves by expressing (exposing to the surface) proteins similar to the natural proteins of the macroorganism, and produce toxins. But all this is an extracellular bustle, where there is a strict taskmaster in the form of the immune system. What about those who live inside the cell? How do these pathogens ensure that they spread from cell to cell, bypassing the external environment?
They suppress phagocytosis directed against them, destroy the membranes of host cells, block the release of neurotransmitters, mask themselves by expressing (exposing to the surface) proteins similar to the natural proteins of the macroorganism, and produce toxins. But all this is an extracellular bustle, where there is a strict taskmaster in the form of the immune system. What about those who live inside the cell? How do these pathogens ensure that they spread from cell to cell, bypassing the external environment?
An introduction to the basics of its functioning was made in the article " Immunity: the fight against strangers and ... " [1].
Today we will talk about the ingenuity of Listeria monocytogenes from the genus Listeria - a gram-positive motile bacillus, an intracellular pathogen that is perfectly preserved in contaminated (that is, contaminated) dairy and meat products. In the absence of proper heat treatment, it can cause such severe damage to the gastrointestinal tract that you would not wish for an enemy. Mortality from listeriosis still ranges from 20% to 60% in different countries. For example, during the last outbreak of listeriosis in Denmark (in 2015), 25% of cases of infection were fatal [2]. Let's see why listeriosis is so harmful.
Mortality from listeriosis still ranges from 20% to 60% in different countries. For example, during the last outbreak of listeriosis in Denmark (in 2015), 25% of cases of infection were fatal [2]. Let's see why listeriosis is so harmful.
As already mentioned, infection occurs through food. After bacteria enter the intestines, they enter the bloodstream, spreading throughout the body, settling mainly in the liver and brain vessels, but some of them remain parasitic in the intestines.
Due to the ability to penetrate into neighboring cells - one by one - they can infect tissues that have not reached with the bloodstream. All that the immune system can do in the fight against intracellular parasites is to kill the infected cell. The destruction of infected tissue is accompanied by necrosis, inflammation and, as a result, the loss of cellular material: if this occurs in the intestine, severe pain, digestive disorders and dehydration occur due to vomiting and diarrhea. Inflammation in the meninges leads to various disorders in the brain. To fight bacteria in the bloodstream, cytokines and other mediators of the immune response are released, which is accompanied by a severe fever and sepsis.
To fight bacteria in the bloodstream, cytokines and other mediators of the immune response are released, which is accompanied by a severe fever and sepsis.
The trouble is not only that listeriosis is difficult to cure, but also that there are extremely many ways of infection: L. monocytogenes lives in soil, water and even plants. By using them, large and small cattle and birds become infected. After all the manipulations with animals at the factories, the resulting products of animal origin are stored in the cold. We are all used to storing such products in the refrigerator, because this way most bacteria multiply much less intensively. But not Listeria! It is able to maintain reproductive function (and not just maintain, but even enhance it) in the temperature range of +4-10 degrees, and even freezing does not have a noticeable effect on its viability, and it is possible to kill Listeria only during a three-minute heating to 100 ° C - these are real masters of survival in extreme conditions!
The situation becomes even worse if a pregnant woman decides to consume contaminated foods: Listeria can cross the placenta [3], [4] due to its ability to travel freely from cell to cell [5], causing preterm labor or infecting the fetus during childbirth, after which it penetrates its meninges, causing meningitis or sepsis in newborns (most of which end fatally).
The infection of each new cell means that the pathogen is successful, and the measure of the success of the microbe is the realization of the ability to reproduce. After division, the eukaryotic cell becomes crowded, and the daughter cells are forced to leave the target cell in search of a new place of residence.
Purpose and means
But if a microorganism can only exist inside the host cell, how does it manage to leave the house and infect neighboring cells without passing through the extracellular environment? Why are such infections difficult to treat, why is it difficult to create effective vaccines against them, and why are these bacteria so cleverly eluding the immune system? The answers to all these questions lie in a closer look at how Listeria spreads in an infected organism. The advantage of Listeria is that it finds its way from cell to cell, completely bypassing the intercellular space.
She does this by inducing a process called paracytophagy . This is a method of exchanging cellular material, in which one cell absorbs protrusions formed by the membrane of its neighbor (Fig. 1) [6]. Why not, as they say: give - take! True, the resulting vesicle (budding vesicle) may contain some material, which is thus actively transferred from cell to cell. For the first time, this process was described just in the course of research on the methods and mechanisms of intercellular spread of Listeria [7], and later it was found in other pathogenic microorganisms, such as Shigella flexneri , which causes dysentery, and Rickettsia conorii [8]. In physiologically normal processes, paracytophagy is not observed, and the event closest to it is the formation of syncytium , when the membranes of neighboring cells merge and the nuclei function separately. In this case, a huge multinucleated cell is formed, therefore, when Listeria induces membrane fusion with a further semblance of endocytosis, it does not cause any suspicion on the part of normal cells.
This is a method of exchanging cellular material, in which one cell absorbs protrusions formed by the membrane of its neighbor (Fig. 1) [6]. Why not, as they say: give - take! True, the resulting vesicle (budding vesicle) may contain some material, which is thus actively transferred from cell to cell. For the first time, this process was described just in the course of research on the methods and mechanisms of intercellular spread of Listeria [7], and later it was found in other pathogenic microorganisms, such as Shigella flexneri , which causes dysentery, and Rickettsia conorii [8]. In physiologically normal processes, paracytophagy is not observed, and the event closest to it is the formation of syncytium , when the membranes of neighboring cells merge and the nuclei function separately. In this case, a huge multinucleated cell is formed, therefore, when Listeria induces membrane fusion with a further semblance of endocytosis, it does not cause any suspicion on the part of normal cells. Thus, bacteria do not mask themselves or their components, but the whole process.
Thus, bacteria do not mask themselves or their components, but the whole process.
Figure 1. Stages of moving Listeria from cell to cell. In the center - a schematic representation of the process, along the edges - microphotographs, according to which the course of events was reconstructed. The pictures were taken using an electron microscope.
Beginning
Let's trace the algorithm of Listeria movements from the very beginning: having got into the gastrointestinal tract with low-quality food, Listeria must have the ability to adhere to intestinal epithelial cells. Adhesion is the process of "sticking" one object to another, and in living organisms it is similar to the functioning of the Velcro on sneakers or clothing. Some molecules play the role of "hooks", others - "loops", and are called "receptor" and "ligand", respectively. Listeria produces one of the necessary components on its surface, while the target cell membrane produces others. Ligands are bacterial proteins - internalin A ( InlA ) and B ( InlB ) (Fig. 2, step 1; further steps mentioned refer to this figure). They interact with the adhesion molecule expressed on the surface of the target cell - E-cadherin [9] (stage 2), and interaction with one such adhesion molecule causes several similar ones to be "pulled" into this area, which is possible due to the fluidity of the cell membrane and its ability to to the formation of rafts . After all, the formation of one ligand-receptor complex in the case of interaction with a whole bacterium is not enough, and the eukaryotic cell is simply not sure that the game is worth the candle. The process of moving a few more E-cadherin molecules to the area of primary stimulation is called by clustering (stage 2), and only after the formation of at least two more complexes of Inl with cadherin, the cell is ready for further actions (stage 3).
Ligands are bacterial proteins - internalin A ( InlA ) and B ( InlB ) (Fig. 2, step 1; further steps mentioned refer to this figure). They interact with the adhesion molecule expressed on the surface of the target cell - E-cadherin [9] (stage 2), and interaction with one such adhesion molecule causes several similar ones to be "pulled" into this area, which is possible due to the fluidity of the cell membrane and its ability to to the formation of rafts . After all, the formation of one ligand-receptor complex in the case of interaction with a whole bacterium is not enough, and the eukaryotic cell is simply not sure that the game is worth the candle. The process of moving a few more E-cadherin molecules to the area of primary stimulation is called by clustering (stage 2), and only after the formation of at least two more complexes of Inl with cadherin, the cell is ready for further actions (stage 3).
Figure 2. Molecular interactions between bacteria and cellular proteins. 1 - The main participants in the process. 2 - Interaction between internalin and cadegreen, clustering. 3, 4 - Endocytosis and proteins that determine its mechanism. 5 - Already penetrated into the cell Listeria , no longer dependent on cytoskeletal components. 6, 7 - Moment of truth: Enzymatic cleavage of the vesicle and exit of the bacterium directly into the cytosol. Now it can feed, multiply, and subsequently spread.
1 - The main participants in the process. 2 - Interaction between internalin and cadegreen, clustering. 3, 4 - Endocytosis and proteins that determine its mechanism. 5 - Already penetrated into the cell Listeria , no longer dependent on cytoskeletal components. 6, 7 - Moment of truth: Enzymatic cleavage of the vesicle and exit of the bacterium directly into the cytosol. Now it can feed, multiply, and subsequently spread.
drawing by Shamsudin Nasaev
In turn, E-adherin, interacting with the ligand, undergoes internalization, that is, “wraps up” inside with the formation of a vesicle in the cytoplasm. This is ensured by the following cascade of events (stage 4): when the extracellular region of cadherin binds to internalin, conformational changes occur in the structure of the receptor, leading to the interaction of its cytoplasmic domain with proteins of the catenin family, which ensure the connection of cadherin with the cytoskeleton [10], which is extremely important in the formation contacts between neighboring cells (in fact, the main role of E-cadherin in the body [11]). This connection is provided by the interaction of catenins with the cytoplasmic domain of cadherin [12]: first of all, after its interaction with internalin, catenin p120 stabilizes cadherin in the plasma membrane.
This connection is provided by the interaction of catenins with the cytoplasmic domain of cadherin [12]: first of all, after its interaction with internalin, catenin p120 stabilizes cadherin in the plasma membrane.
Further, there are two scenarios:
- Other catenin proteins, alpha and beta, bind to still stable cadherin, which provide its strong constructive connection with the actin cytoskeleton [13].
- The interaction of cadherin with ligands on the surface of Listeria leads to the activation of Src-kinase, which phosphorylates the cytoplasmic domain of cadherin, destabilizing it, and determines the further internalization of the cadherin-listeria complex. Another effect of E-cadherin phosphorylation is p120 cleavage, and Hakai ubiquitin ligase [14] (step 4) interacts with the vacated site, an enzyme that sends the adhesion molecule to the “last path”. It catalyzes the attachment of a special protein - ubiquitin - to molecules to be destroyed. Ubiquitin is a "black mark", signaling the need for degradation of the macromolecule in lysosomes (step 5).

In addition, membrane proteins caveolin and clathrin are always present on the membrane. Their role is to control the pathways of endocytosis (caveolin provides the course of receptor-independent endocytosis, clathrin - receptor-mediated). In the process of formation of a vesicle with listeria inside, clathrin mainly takes part [15], which polymerizes on the surface of the resulting vesicle, controls the process of its detachment from the outer membrane and ensures its fusion with intracellular endosomes, mediating the delivery of material from the extracellular environment to the cytosol.
Thus, the operation for adhesion and subsequent penetration of the bacterium into the cell has been completed. Now, being surrounded by a membrane, it remains only to penetrate into the cytoplasm. This is ensured by the secretion of the bacterial toxin listeriolysin O ( LLO ), a pore-forming agent (stage 6) (and it is also a direct signal molecule and is able to activate, for example, the nuclear factor kB - the same NfkB that was recently congratulated on the anniversary [16 ]). LLO causes lysis of the vesicle membrane, and the bacterium enters directly into the cytoplasm (stage 7). The next step in its life cycle is spreading from cell to cell, and here we come to the most interesting thing - the way in which Listeria provides itself with a continuous intracellular existence, while making a change of target cells.
LLO causes lysis of the vesicle membrane, and the bacterium enters directly into the cytoplasm (stage 7). The next step in its life cycle is spreading from cell to cell, and here we come to the most interesting thing - the way in which Listeria provides itself with a continuous intracellular existence, while making a change of target cells.
The cytoskeleton: molecular aspects
To properly understand this process, it is necessary to know the fundamentals of the actin cytoxelet: actin is present in the cell in an inactive, monomeric form as G-actin (globular actin). Each of these globules is associated with an adenosine triphosphate (ATP) molecule, the main source of energy in any cell. In the process of "magic" interactions (more on them below), actin quickly polymerizes, forming filaments - double-stranded "ropes" (at this moment it becomes F-actin - filamentous), inside which actin molecules are held by non-covalent bonds (Fig. 3). The low strength of non-covalent bonds is compensated by their quantity, thanks to which the cell receives a fairly strong and at the same time elastic structural material.
What are the "magic" interactions that control actin polymerization in the right place at the right time? The first link in this process is the profilin protein: it binds to G-actin monomers, occupying proline-rich sites in them, which will later participate in the formation of contacts between actin molecules. This is important, because proline is not exactly amino acid: it is more correct to call it imino acid. Due to its chemical nature, proline provides flexible regions to peptide sequences, acting like a hinge. In the presence of Mg 2+ profilin (in Figure 3 - Pi) ensures the hydrolysis of ATP to ADP (in Figure 3, actin in complex with ATP - T, with ADP - D). As a result, energy is released, which greatly facilitates and accelerates polymerization.
In addition to actin, actin-like proteins are present in cells, among which there are several subfamilies (Arp1, Arp2, Arp3, etc.). Some of these proteins are involved in the manipulation of actin, and some are not able to interact with it at all - the latter include Arp2 and Arp3. To be more precise, they do not interact alone, but together they form the Arp2/3 complex, which plays one of the key roles [17] - it serves as a matrix for actin assembly, but already "from the end" or to the side of the already formed thread, providing elongation or branching microfilaments. This allows you to speed up the polymerization of actin by 2-3 times, but this speed is enough to “push out” the cell membrane in the right direction right before your eyes.
To be more precise, they do not interact alone, but together they form the Arp2/3 complex, which plays one of the key roles [17] - it serves as a matrix for actin assembly, but already "from the end" or to the side of the already formed thread, providing elongation or branching microfilaments. This allows you to speed up the polymerization of actin by 2-3 times, but this speed is enough to “push out” the cell membrane in the right direction right before your eyes.
And the last key participant in this process is protein WASP ( Wiskott-Aldrich Syndrome Protein , or formin ), which has binding sites for both monomeric actin and the Arp2/3 complex. By binding both of these components and changing the conformation, WASP ensures their spatial convergence, further facilitating and accelerating polymerization. In addition to these binding sites, it also carries other regulatory sites, including those for binding to phospholipids and for connecting the cytoskeleton to the membrane, playing an important role in the processes of adhesion and intercellular communications, performing a number of signaling functions [18].
Have you forgotten about
Listeria ?The entire excursion into actin polymerization described above is directly related to its vital activity. As we remember, for the effective survival of this bacterium, it is necessary to constantly be inside the host cell. At the same time, pathogens cannot be allowed to overpopulate, and some of them are forced to look for a new home. In order not to get into the intercellular space and avoid an immune attack, Listeria manipulates the actin of the host cell. At one end of its "body" the bacterium secretes ActA ( actin assembly-inducing protein - a protein that induces actin assembly), which ... mimics eukaryotic WASP [19], [20]! The visualization of what comes out of this is in Figure 3, the theoretical description is in the text.
Figure 3. Visualization of the process of paracytophagy. Polymerizing actin forms the so-called "comet tail" and acts as a jet engine: under its pressure, the bacterium moves forward and forward, and the design of the cytoskeleton ensures the protrusion of the membrane in the same direction. The resulting protrusion "cuts" into the neighboring cell, later turning into a vesicle, which the bacterium breaks down enzymatically.
The resulting protrusion "cuts" into the neighboring cell, later turning into a vesicle, which the bacterium breaks down enzymatically.
To see the picture in full size, click on it.
drawing by Shamsudin Nasaev
Expression of this protein causes the induction of Arp2/3-mediated actin polymerization, which is so powerful and fast that it literally pushes the prokaryotic cell towards its opposite pole, leaving behind it a "comet tail" of actin [21 ]. And if this process occurs in sufficient proximity to the eukaryotic cell membrane, it begins to protrude, forming a protrusion ranging in size from 3 to 18 microns. Reaching it, Listeria interacts with membrane-bound protein ezrin , which “sews” the actin comet tail to the host cell membrane, providing parietal attachment of the bacterium [22].
And continuing actin polymerization further pushes Listeria out of the host cell. By this moment, the protrusion of the cell membrane of the infected cell takes such an elongated shape that it literally digs into the neighboring cell (in the epithelial lining of the intestine - one of the main abode of Listeria monocytogenes - the cells are located close to each other), and the latter is left with nothing but capture a vesicle with a pathogen inside by endocytosis, getting a "pig in a poke".
At the same time, Listeria is still moving forward, until its "spacesuit" runs out of ATP and G-actin taken from the old cell. Listeria breaks down the resulting membrane "cocoon" with the help of listeriolysin O and phospholipases already known to you, and - voila! - the bacterium can be congratulated on a housewarming, during which it was not detected by immune cells, none of the components of the extracellular matrix was affected, and even the cell itself, which is the new host, could not understand that instead of a "cat" it got a real devil.
What do we have?
Thus, the immune system is able to react to Listeria only before it first adheres to the target cell and penetrates into it. Considering that infection occurs mainly through the gastrointestinal tract, where there are many immune cells, but they do not all lie on the surface of the epithelial lining, and antigens are delivered to them by transcytosis through other specialized cells, we can conclude that immunity has very few chances. In addition, Listeria is able to suppress the immune response directed in its direction, forcing immune cells to commit suicide (inducing apoptosis in them) [23].
In addition, Listeria is able to suppress the immune response directed in its direction, forcing immune cells to commit suicide (inducing apoptosis in them) [23].
So far, the complement system remains the main weapon of immunity [24], when the entire infected cell is destroyed, saving neighboring cells from infection at the cost of its own life. Accordingly, attempts to create a vaccine are not crowned with significant success, and treatment methods are limited to therapy with antibacterial drugs with the most pronounced ability to penetrate membranes, which is a factor in the increased frequency of side effects due to the systemic nature of their effect on the body - after all, they also penetrate into healthy cells. It remains only to choose high-quality products of animal origin and conduct the most thorough heat treatment.
Conclusion
What is the relevance of such a problem as listeriosis, and why are studies still ongoing and the mechanisms of molecular interactions are clarified? As already mentioned, this disease is not a pleasant one (especially when it ends fatally). A person who becomes ill with listeriosis loses his ability to work for a long time - the acute period of the disease lasts up to two weeks. At the same time, not only working capacity suffers, but also physical, psychological and social discomfort appear. It is also sad that the most vulnerable groups of people are affected by this disease: pregnant women, people with immunodeficiencies, newborns and the elderly. In the case of pregnancy, infection with listeriosis can lead to miscarriage, stillbirth or premature birth, which is likely to result in an already infected child. Unfortunately, most cases of infection are not limited to the intestinal form - in infants, meningitis and encephalitis are most common, leading to further disturbances in the central nervous system, and the conjunctival form of the disease, when infection of the mucous membrane of the eye occurs, leading to the development of keratoconjunctivitis (and those who do not develop further complications will be very lucky).
A person who becomes ill with listeriosis loses his ability to work for a long time - the acute period of the disease lasts up to two weeks. At the same time, not only working capacity suffers, but also physical, psychological and social discomfort appear. It is also sad that the most vulnerable groups of people are affected by this disease: pregnant women, people with immunodeficiencies, newborns and the elderly. In the case of pregnancy, infection with listeriosis can lead to miscarriage, stillbirth or premature birth, which is likely to result in an already infected child. Unfortunately, most cases of infection are not limited to the intestinal form - in infants, meningitis and encephalitis are most common, leading to further disturbances in the central nervous system, and the conjunctival form of the disease, when infection of the mucous membrane of the eye occurs, leading to the development of keratoconjunctivitis (and those who do not develop further complications will be very lucky). A recovered person becomes more susceptible to opportunistic infections (which are caused by representatives of the normal microflora that are not pathogenic in a healthy state of the immune system).
A recovered person becomes more susceptible to opportunistic infections (which are caused by representatives of the normal microflora that are not pathogenic in a healthy state of the immune system).
Considering that the treatment is non-specific and often symptomatic, drug-induced reactions are also used: antipyretic and anti-inflammatory drugs create an increased load on the enzyme systems of the liver and kidneys, and antibiotics negatively affect the microflora of the human body and contribute to the development of antibiotic resistance in pathogenic microorganisms. In general, apart from the extermination of pathogenic microorganisms in the period of time corresponding to the acute phase of the disease, nothing good can be expected from antibiotics.
In addition, if a patient takes an incomplete course of antibiotics or chooses the wrong dosage, listeriosis can become chronic, which will be accompanied by an imbalance in the immune system, and the patient himself will become an additional reservoir of infection.
All these consequences of infection, coupled with the ease of infection, dictate the need to develop new, more effective and, ideally, safer methods of treatment and prevention. Thus, some progress has already been made in the development of drugs that inhibit bacterial kinases, one of the most important enzymes of Listeria [25], and a vaccine based on attenuated Listeria proved to be not only an effective method in preventing listeriosis, but also showed the ability to enhance the effectiveness of antitumor therapy [26].
Understanding the mechanisms of spread of intracellular pathogens is perhaps the impetus for the development of new drugs, whose target will be proteins that interact with the cytoskeleton or adhesion molecules, or, for example, lysins. Such drugs will make it possible to act on different stages of pathogenesis, limiting the penetration, spread and reproduction of parasites. Who knows, perhaps in the future the mechanism of paracytophagy or something similar to it will help to understand and describe normal physiological or pathological processes?
- Immunity: fight against strangers and… our own;
- About the listeriosis outbreak in Denmark.
 (2015). Rospotrebnadzor ;
(2015). Rospotrebnadzor ; - Anna I. Bakardjiev, Brian A. Stacy, Daniel A. Portnoy. (2005). Growth ofListeria monocytogenesin the Guinea Pig Placenta and Role of Cell-to-Cell Spread in Fetal Infection. J INFECT DIS . 191 , 1889-1897;
- M. Lecuit, D. M. Nelson, S. D. Smith, H. Khun, M. Huerre, et. al. (2004). Targeting and crossing of the human maternofetal barrier by Listeria monocytogenes: Role of internalin interaction with trophoblast E-cadherin. Proceedings of the National Academy of Sciences . 101 , 6152-6157;
- Olivier Disson, Solène Grayo, Eugénie Huillet, Georgios Nikitas, Francina Langa-Vives, et. al. (2008). Conjugated action of two species-specific invasion proteins for fetoplacental listeriosis. Nature . 455 , 1114-1118;
- Daniel A. Portnoy, Victoria Auerbuch, Ian J. Glomski. (2002).
 The cell biology ofListeria monocytogenesinfection. J Cell Biol . 158 , 409-414;
The cell biology ofListeria monocytogenesinfection. J Cell Biol . 158 , 409-414; - Jennifer R. Robbins, Angela I. Barth, Hélène Marquis, Eugenio L. de Hostos, W. James Nelson, Julie A. Theriot. (1999). Listeria monocytogenesExploits Normal Host Cell Processes to Spread from Cell to Cell✪. J Cell Biol . 146 , 1333-1350;
- Gouin E., Gantelet H., Egile C., Lasa I., Ohayon H., Villiers V. et al. (1999). A comparative study of the actin-based motilities of the pathogenic bacteria Listeria monocytogenes , Shigella flexneri and Rickettsia conorii . J. Cell Sci. 112 , 1697–1708;
- J.-L. Gaillard, P. Berche, C. Frehel, E. Gouln, P. Cossart. (1991). Entry of L. monocytogenes into cells is mediated by internalin, a repeat protein reminiscent of surface antigens from gram-positive cocci. Cell .
 65 , 1127-1141;
65 , 1127-1141; - Mirna Perez-Moreno, Colin Jamora, Elaine Fuchs. (2003). sticky business. Cell . 112 , 535-548;
- Saurabh D Patel, Chien Peter Chen, Fabiana Bahna, Barry Honig, Lawrence Shapiro. (2003). Cadherin-mediated cell–cell adhesion: sticking together as a family. Current Opinion in Structural Biology . 13 , 690-698;
- L. Shapiro, W. I. Weis. (2009). Structure and Biochemistry of Cadherins and Catenins. Cold Spring Harbor Perspectives in Biology . 1 , a003053-a003053;
- Frauke Drees, Sabine Pokutta, Soichiro Yamada, W. James Nelson, William I. Weis. (2005). α-Catenin Is a Molecular Switch that Binds E-Cadherin-β-Catenin and Regulates Actin-Filament Assembly. Cell . 123 , 903-915;
- Soichiro Yamada, Sabine Pokutta, Frauke Drees, William I.
 Weis, W. James Nelson. (2005). Deconstructing the Cadherin-Catenin-Actin Complex. Cell . 123 , 889-901;
Weis, W. James Nelson. (2005). Deconstructing the Cadherin-Catenin-Actin Complex. Cell . 123 , 889-901; - Esteban Veiga, Pascale Cossart. (2005). Listeria hijacks the clathrin-dependent endocytic machinery to invade mammalian cells. Nat Cell Biol . 7 , 894-900;
- Qian Zhang, Michael J. Lenardo, David Baltimore. (2017). 30 Years of NF-κB: A Blossoming of Relevance to Human Pathobiology. Cell . 168 , 37-57;
- Sandra Sousa, Didier Cabanes, Laurence Bougnères, Marc Lecuit, Philippe Sansonetti, et. al. (2007). Src, cortactin and Arp2/3 complex are required for E-cadherin-mediated internalization of Listeria into cells. Cell Microbiol . 9 , 2629-2643;
- Olga Alekhina, Ezra Burstein, Daniel D. Billadeau. (2017). Cellular functions of WASP family proteins at a glance. J Cell Sci .
 130 , 2235-2241;
130 , 2235-2241; - Welch M.D., Rosenblatt J., Skoble J., Portnoy D.A., Mitchison T.J. (1998). Interaction of human Arp2/3 complex and the Listeria monocytogenes ActA protein in actin filament nucleation. Science . 281 , 105–108;
- C. Kocks, E. Gouin, M. Tabouret, P. Berche, H. Ohayon, P. Cossart. (1992). L. monocytogenes-induced actin assembly requires the actA gene product, a surface protein. Cell . 68 , 521-531;
- V. B. Shenoy, D. T. Tambe, A. Prasad, J. A. Theriot. (2007). A kinematic description of the trajectories of Listeria monocytogenes propelled by actin comet tails. Proceedings of the National Academy of Sciences . 104 , 8229-8234;
- M. Bonazzi, M. Lecuit, P. Cossart. (2009). Listeria monocytogenes Internalin and E-cadherin: From Bench to Bedside. Cold Spring Harbor Perspectives in Biology .