Blood pressure in pregnancy 130 80
High Blood Pressure During Pregnancy: Symptoms and Treatments
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
High blood pressure, or hypertension, is defined as blood pressure greater than or equal to 130/80 mm Hg. The condition is a serious concern for some pregnant women.
When it’s well-managed, high blood pressure during pregnancy isn’t always dangerous. But it can sometimes cause severe health complications for both mother and developing baby. The Centers for Disease Control and Prevention (CDC) estimates that around six to eight percent of pregnant women between the ages of 20 and 44 in the United States have this condition.
There are several possible causes of high blood pressure during pregnancy.
These include:
- being overweight or obese
- not getting enough physical activity
- smoking
- drinking alcohol
- first-time pregnancy
- a family history of pregnancy-related hypertension
- carrying more than one child
- age (over 35)
- assistive reproductive technology (such as in vitro fertilization, or IVF)
- having diabetes or certain autoimmune diseases
There are a few risk factors that could make high blood pressure more likely during pregnancy.
Lifestyle
Unhealthy lifestyle choices may lead to high blood pressure during pregnancy. Being overweight or obese, or not staying active are major risk factors for high blood pressure.
Type of pregnancy
Women experiencing their first pregnancy are more likely to have high blood pressure. Fortunately, there’s a lower chance of this condition in subsequent pregnancies.
Carrying multiples can make it more likely for a woman to develop hypertension, because the body is working harder to nourish more than one baby.
According to the American Society for Reproductive Medicine, using assistive technologies (such as IVF) during the conception process can increase chances of high blood pressure in a pregnant woman.
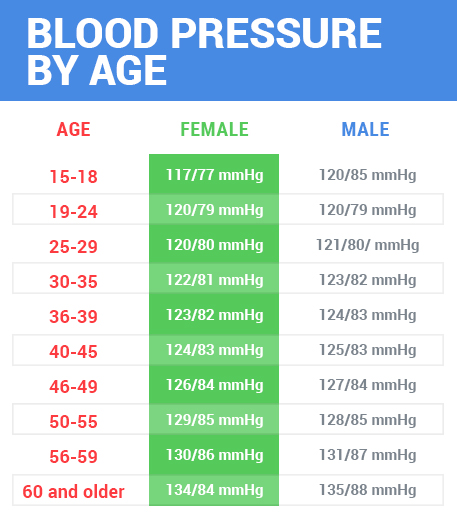
Age
Age can also be a factor. Pregnant women over the age of 35 are at higher risk.
Women who had high blood pressure before pregnancy are at higher risk for related complications during pregnancy than those with normal blood pressure.
High blood pressure during pregnancy can be divided into three different conditions.
Chronic hypertension
Sometimes a woman has preexisting high blood pressure, or hypertension, before she gets pregnant. This may be referred to as chronic hypertension, and is usually treated with blood pressure medication.
Doctors also consider hypertension that occurs in the first 20 weeks of pregnancy to be chronic hypertension.
Gestational hypertension
Gestational hypertension develops after the 20th week of pregnancy. It usually resolves after delivery. When diagnosed before 30 weeks, there’s a higher chance it will progress to preeclampsia (see below).
Chronic hypertension with superimposed preeclampsia
Women who have chronic hypertension before becoming pregnant can develop preeclampsia. This occurs when they experience protein in their urine or additional complications as the pregnancy progresses.
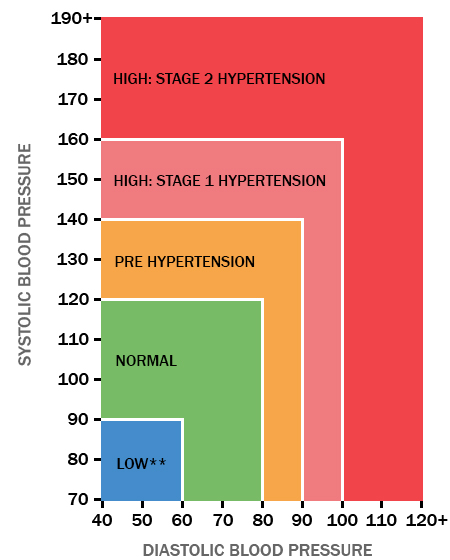
A blood pressure reading is a fraction: your systolic blood pressure over your diastolic blood pressure.
The top number is your systolic pressure, which is a measurement of the pressure on your arteries when the heart is beating or squeezing blood forward through your body.
The diastolic pressure, or the lower number, is a measurement of the blood pressure in your arteries when the heart is at rest.
To determine what your “normal” blood pressure is during pregnancy, your doctor will likely take a baseline blood pressure measurement at your first visit. Then they will measure your blood pressure at every visit that follows.
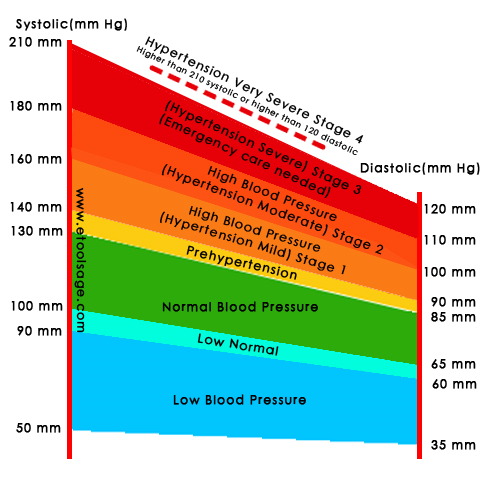
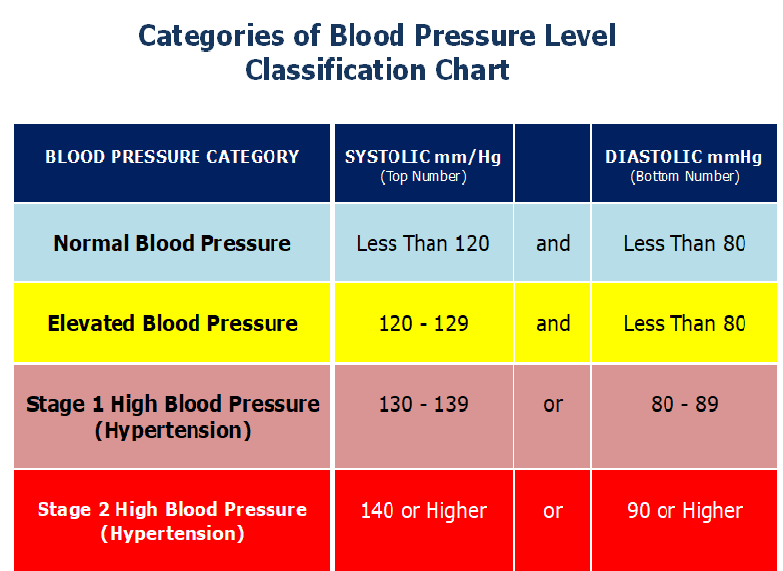
Normal blood pressure is anything less than 120/80 mm Hg.
What is considered high blood pressure during pregnancy?
A blood pressure that is greater than 130/90 mm Hg or that is 15 degrees higher on the top number from where you started before pregnancy may be cause for concern.
High blood pressure during pregnancy is defined as 140 mm Hg or higher systolic, with diastolic 90 mm Hg or higher.
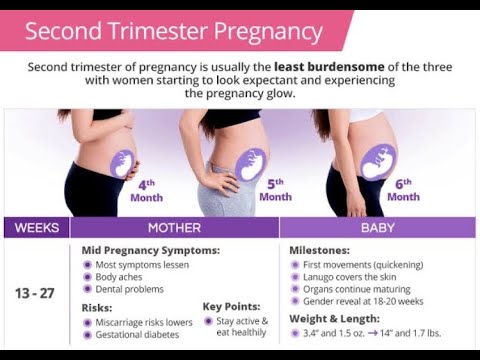
Early in pregnancy, usually from 5 weeks to the middle of the second trimester, a pregnant woman’s blood pressure may actually decrease. This is because pregnancy hormones can stimulate blood vessels to widen. As a result, the resistance to blood flow isn’t as high.
This is because pregnancy hormones can stimulate blood vessels to widen. As a result, the resistance to blood flow isn’t as high.
What is considered low blood pressure during pregnancy?
While there isn’t a definitive number that is too low, there are symptoms that are associated with low blood pressure:
- headache
- dizziness
- nausea
- feeling faint
- cold, clammy skin
As a woman progresses in her pregnancy, her blood pressure may change or return to pre-pregnancy levels. There are a few possible reasons for this.
The amount of blood in a woman’s body increases. According to the journal Circulation, a woman’s blood volume increases by as much as 45 percent during pregnancy. This is extra blood that the heart must pump throughout the body.
The left ventricle (left side of the heart that does a significant amount of pumping) becomes thicker and larger. This temporary effect allows the heart to work harder to support the increased blood volume.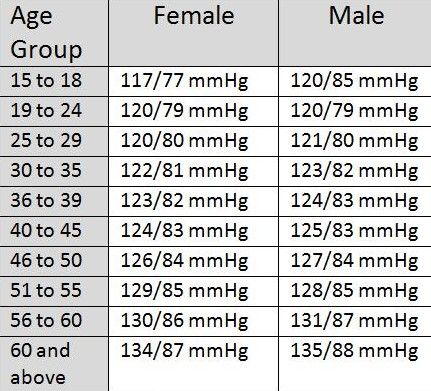
The kidneys release increased amounts of vasopressin, a hormone that leads to increased water retention.
In most cases, high blood pressure during pregnancy will decrease after the baby is delivered. In cases where blood pressure remains elevated, your doctor may prescribe medication to get it back to normal.
Tips for tracking blood pressure during pregnancy
There are ways to track your blood pressure between doctor visits.
You can buy a blood pressure monitor from a pharmacy or online medical goods store. Many of these devices will go on your wrist or upper arm. To check the monitor’s accuracy, take it to your doctor’s office and compare the readings on the monitor to those from your doctor.
Visit a grocery store, pharmacy, or other store that has a machine that takes blood pressure readings.
For the most accurate readings, take your blood pressure at the same time every day. Take it while seated with your legs uncrossed. Use the same arm each time.
Notify your doctor immediately if you have repeated high blood pressure readings that are four hours apart or symptoms of high blood pressure.
If you have high blood pressure during pregnancy, there can be complications.
Preeclampsia
This condition can cause serious damage to your organs, including your brain and kidneys. Preeclampsia is also known as toxemia. Preeclampsia with seizures becomes eclampsia. If left untreated, it can be fatal.
Symptoms of preeclampsia include:
- abnormal swelling in hands and face
- persistent headaches
- seeing spots or having changes in vision
- upper abdominal pain
- nausea or vomiting later in pregnancy
- difficulty breathing
Because preeclampsia can be dangerous for both you and your baby, you should call your doctor if you have any of these symptoms.
Keeping regular doctor visits and letting your doctor know about any changes can help them catch and treat preeclampsia early.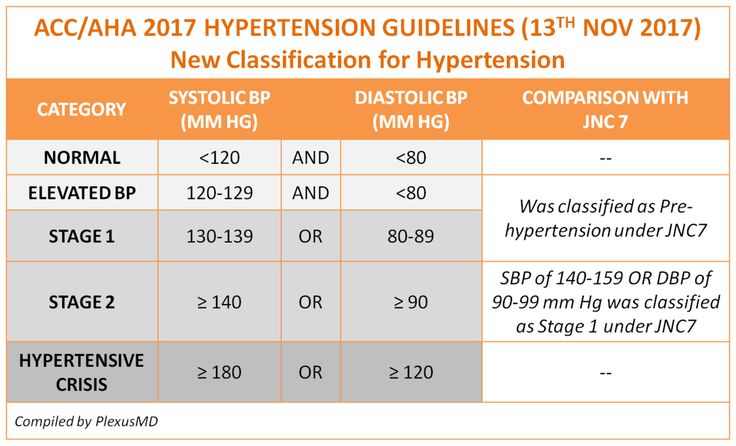
HELLP syndrome
HELLP is an acronym that stands for hemolysis, elevated liver enzymes, and low platelet count. This condition is severe and life-threatening, and can be a complication of preeclampsia.
Symptoms associated with HELLP include:
- nausea
- vomiting
- headache
- upper abdominal pain
Because HELLP syndrome can severely damage organ systems vital to life, emergency medical care is aimed at reducing blood pressure for the health of the mother and the baby. In some cases, a premature delivery is required.
High blood pressure during pregnancy can also have an effect on the baby’s growth rate. This can result in low birth weight. According to the American Congress of Obstetricians and Gynecologists, other complications include:
- placental abruption, a medical emergency during which the placenta detaches from the uterus prematurely
- preterm delivery, defined as delivery prior to 38 weeks of pregnancy
- cesarean delivery, commonly known as C-section
Common risk factors for high blood pressure, such as obesity, can be minimized through diet and exercise.
During pregnancy, it’s normal to gain some weight. If you’re concerned, talk to your doctor about a target weight gain and ways to stay within a range that’s healthy for you.
Dietary guidelines for pregnant women vary from person to person. A nutritionist can help create a meal plan that’s designed for your specific height and weight.
Avoid smoking and drinking alcohol. Both are known to raise blood pressure and to cause other complications during pregnancy.
Salt is important during pregnancy and it’s usually not necessary to limit salt intake, even for women with high blood pressure. Restricting salt too much is harmful for pregnant women and can impact fetal growth and development.
Pregnancy causes hormone shifts as well as psychological and physical changes. This can bring on stress, which can make high blood pressure harder to manage. Try stress reduction techniques such as yoga and meditation.
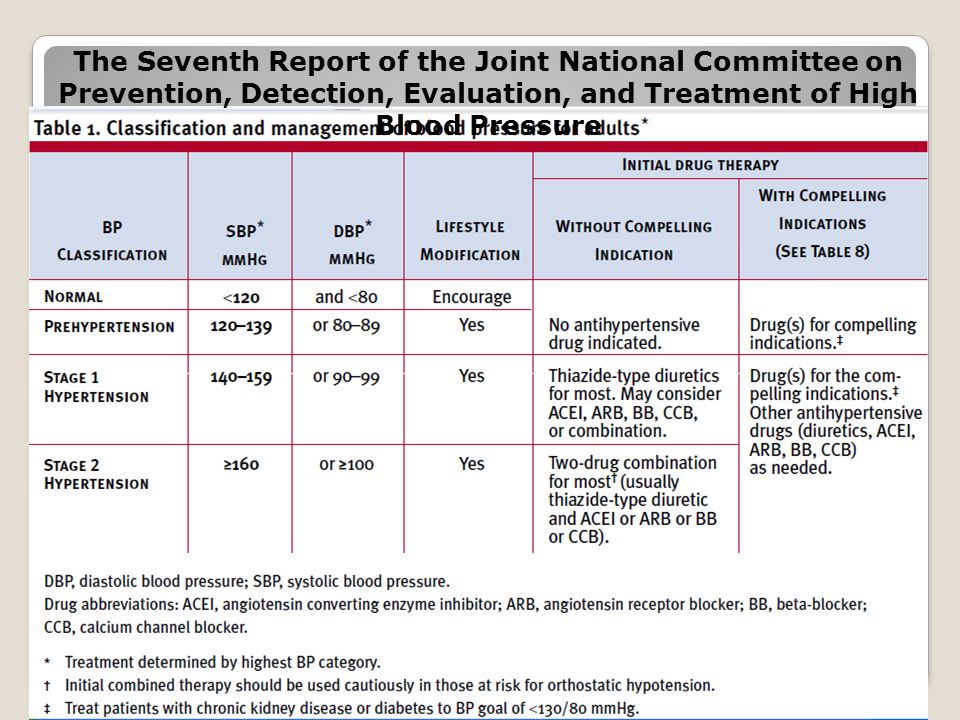
Some traditional blood pressure medications can cause problems in pregnant women.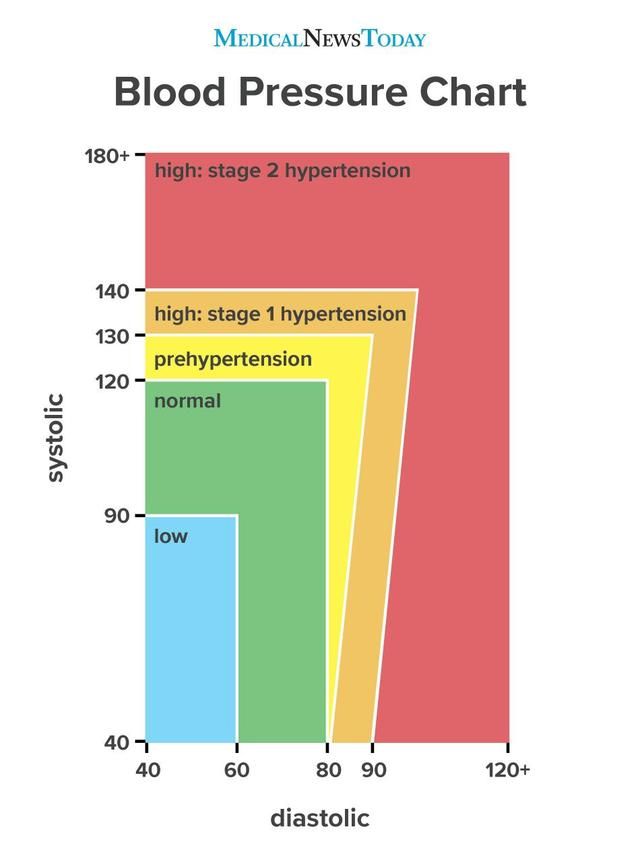
These medications for lowering blood pressure are typically not recommended during pregnancy:
- ACE inhibitors
- renin inhibitors
- angiotensin receptor blockers
These drugs in particular will pass through the bloodstream to the baby and negatively impact the developing baby’s health.
Methyldopa and labetalol are both drugs that are considered safe to use to manage blood pressure during pregnancy.
If high blood pressure goes untreated during pregnancy, it can become life-threatening for both mother and baby.
Hypertensive disorders resulting from high blood pressure are the second-leading cause of U.S. maternal death during pregnancy, so it’s important to talk to your doctor about any symptoms or concerns.
In general, careful monitoring and some lifestyle changes can lower your risk of developing complications from high blood pressure.
Preeclampsia and High Blood Pressure During Pregnancy
-
Blood pressure is the force of blood pushing against the walls of blood vessels called arteries.
 The arteries bring blood from the heart to your lungs, where it picks up oxygen and then moves to your organs and tissues. The organs and tissues use the oxygen to power their activities. Blood vessels called veins return the blood to the heart.
The arteries bring blood from the heart to your lungs, where it picks up oxygen and then moves to your organs and tissues. The organs and tissues use the oxygen to power their activities. Blood vessels called veins return the blood to the heart. -
High blood pressure (also called hypertension) can lead to health problems at any time in life. High blood pressure usually does not cause symptoms. During pregnancy, severe or uncontrolled high blood pressure can cause problems for you and your fetus.
Some women have high blood pressure before they get pregnant. Others develop it for the first time during pregnancy. A serious high blood pressure disorder called preeclampsia can also happen during pregnancy or soon after childbirth.
-
A blood pressure reading has two numbers separated by a slash.
 A blood pressure reading of 110/80 mm Hg, for example, is referred to as “110 over 80.” The first number is the pressure against the artery walls when the heart contracts. This is called the systolic blood pressure. The second number is the pressure against the artery walls when the heart relaxes between contractions. This is called the diastolic blood pressure.
A blood pressure reading of 110/80 mm Hg, for example, is referred to as “110 over 80.” The first number is the pressure against the artery walls when the heart contracts. This is called the systolic blood pressure. The second number is the pressure against the artery walls when the heart relaxes between contractions. This is called the diastolic blood pressure. -
-
Normal: Less than 120/80 mm Hg
-
Elevated: Systolic between 120 and 129 mm Hg and diastolic less than 80 mm Hg
-
Stage 1 hypertension: Systolic between 130 and 139 mm Hg or diastolic between 80 and 89 mm Hg
-
Stage 2 hypertension: Systolic at least 140 mm Hg or diastolic at least 90 mm Hg
-
-
Your obstetrician–gynecologist (ob-gyn) should check your blood pressure at each prenatal care visit.
 Blood pressure changes often during the day. If you have one high reading, another reading may be taken later during your office visit.
Blood pressure changes often during the day. If you have one high reading, another reading may be taken later during your office visit.
-
Chronic hypertension is high blood pressure that a woman has before getting pregnant or that develops in the first half of pregnancy (before 20 weeks of pregnancy). If you were taking blood pressure medication before you got pregnant—even if your blood pressure is currently normal—you have been diagnosed with chronic hypertension.
-
When you are pregnant, your body makes more blood to support the fetus’s growth. If blood pressure goes up during pregnancy, it can place extra stress on your heart and kidneys. This can lead to heart disease, kidney disease, and stroke. High blood pressure during pregnancy also increases the risk of preeclampsia, preterm birth, placental abruption, and cesarean birth.

-
High blood pressure may reduce blood flow to the placenta. As a result, the fetus may not get enough of the nutrients and oxygen needed to grow.
-
In the first half of pregnancy, blood pressure normally goes down. If your hypertension is mild, your blood pressure may stay that way or even return to normal during pregnancy. But if your blood pressure is 140/90 mm Hg or higher, your ob-gyn may recommend that you start or continue taking blood pressure medication during pregnancy.
-
Your blood pressure should be checked at every prenatal care visit. You may also need to monitor your blood pressure at home. Ultrasound exams may be done throughout pregnancy to track the growth of the fetus.
 If growth problems are suspected, you may have other tests that monitor the health of the fetus. This testing usually begins in the third trimester of pregnancy.
If growth problems are suspected, you may have other tests that monitor the health of the fetus. This testing usually begins in the third trimester of pregnancy. -
If your condition remains stable, delivery 1 to 3 weeks before your due date (about 37 weeks to 39 weeks of pregnancy) generally is recommended. If you or the fetus develop complications, delivery may be needed even earlier.
-
After delivery, you will need to keep monitoring your blood pressure at home for 1 to 2 weeks. Blood pressure often goes up in the weeks after childbirth. You may need to resume taking medication, or your medication dosage may need to be adjusted.
Talk with your ob-gyn about blood pressure medications that are safe to take if you plan to breastfeed. Do not stop any medications without talking with your ob-gyn.

-
You have gestational hypertension when:
-
You have a systolic blood pressure of 140 mm Hg or higher and/or a diastolic blood pressure of 90 mm Hg or higher.
-
The high blood pressure first happens after 20 weeks of pregnancy.
-
You had normal blood pressure before pregnancy.
Most women with gestational hypertension have only a small increase in blood pressure. But some women develop severe hypertension (defined as systolic blood pressure of 160 mm Hg or higher and/or diastolic blood pressure of 110 mm Hg or higher). These women are at risk of very serious complications.
-
-
All women with gestational hypertension are monitored often (usually weekly) for signs of preeclampsia and to make sure that their blood pressure does not go too high.
-
Although gestational hypertension usually goes away after childbirth, it may increase the risk of developing high blood pressure in the future. If you had gestational hypertension, keep this risk in mind as you take care of your health. Healthy eating, weight loss, and regular exercise may help prevent high blood pressure in the future.
-
Preeclampsia is a serious disorder that can affect all the organs in your body. It usually develops after 20 weeks of pregnancy, often in the third trimester. When it develops before 34 weeks of pregnancy, it is called early-onset preeclampsia. It can also develop in the weeks after childbirth.
-
It is not clear why some women develop preeclampsia.
 Doctors refer to "high risk" and "moderate risk" of preeclampsia.
Doctors refer to "high risk" and "moderate risk" of preeclampsia. Factors that may put you in the “high risk” category include
-
preeclampsia in a past pregnancy
-
carrying more than one fetus (twins, triplets, or more)
-
chronic hypertension
-
kidney disease
-
diabetes mellitus
-
autoimmune conditions, such as lupus (systemic lupus erythematosus or SLE)
-
having multiple moderate risk factors (see below)
Factors that may put you in the “moderate risk” category include
-
being pregnant for the first time
-
being pregnant more than 10 years after your previous pregnancy
-
body mass index (BMI) over 30
-
family history of preeclampsia (mother or sister)
-
being age 35 or older
-
complications in previous pregnancies, such as having a baby with a low birth weight
-
in vitro fertilization (IVF)
-
Black race (because of racism and inequities that increase risk of illness)
-
lower income (because of inequities that increase risk of illness)
-
-
-
Preeclampsia can lead to a condition that causes seizures and stroke.
-
Preeclampsia can cause HELLP syndrome. HELLP stands for hemolysis, elevated liver enzymes, and low platelet count. HELLP syndrome damages or destroys red blood cells and interferes with blood clotting. It can also cause chest pain, abdominal pain, and bleeding in the liver. HELLP syndrome is a medical emergency. Women can die from HELLP syndrome. They can also have lifelong health problems from the condition.
-
-
For women with preeclampsia, early delivery may be needed in some cases. Preterm babies have an increased risk of problems with breathing, eating, staying warm, hearing, and vision. Some preterm complications last a lifetime and require ongoing medical care.
-
Women who have had preeclampsia—especially those whose babies were born preterm—have an increased risk later in life of kidney disease, heart attack, stroke, and high blood pressure.
 Also, having preeclampsia once increases the risk of having it again in a future pregnancy.
Also, having preeclampsia once increases the risk of having it again in a future pregnancy. -
Preeclampsia can develop quietly without you being aware of it. Symptoms can include
-
swelling of face or hands
-
headache that will not go away
-
seeing spots or changes in eyesight
-
pain in the upper abdomen or shoulder
-
nausea and vomiting (in the second half of pregnancy)
-
sudden weight gain
-
difficulty breathing
If you have any of these symptoms, especially if they develop in the second half of pregnancy, call your ob-gyn right away.
A woman with preeclampsia whose condition is worsening will develop “severe features.” Severe features include
-
low number of platelets in the blood
-
abnormal kidney or liver function
-
pain in the upper abdomen
-
changes in vision
-
fluid in the lungs
-
severe headache
-
systolic pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or higher
-
-
A high blood pressure reading may be the first sign of preeclampsia.
 If your blood pressure reading is high, it may be checked again to confirm the results. You may have a urine test to check for protein. You may also have tests to check how your liver and kidneys are working and to measure the number of platelets in your blood.
If your blood pressure reading is high, it may be checked again to confirm the results. You may have a urine test to check for protein. You may also have tests to check how your liver and kidneys are working and to measure the number of platelets in your blood. -
You and your ob-gyn should talk about how your condition will be managed. The goal is to limit complications for you and to deliver the healthiest baby possible.
-
Women who have gestational hypertension or preeclampsia without severe features may be treated in a hospital or as an outpatient. Being an outpatient means you can stay at home with close monitoring by your ob-gyn. You may need to keep track of your fetus’s movement by doing a daily kick count. You may also need to measure your blood pressure at home. Visits to your ob-gyn may be once or twice a week.

At 37 weeks of pregnancy, you and your ob-gyn may talk about delivery. Labor may be induced (started with medications). If test results show that the fetus is not doing well, you may need to have the baby earlier. Women with preeclampsia can have vaginal deliveries, but if there are problems during labor, cesarean birth may be needed.
-
If you have preeclampsia with severe features, you may be treated in the hospital. If you are at least 34 weeks pregnant, you and your ob-gyn may talk about having your baby as soon as your condition is stable.
If you are less than 34 weeks pregnant and your condition is stable, it may be possible to wait to deliver your baby. Delaying delivery for just a few days may be helpful in some cases. It allows time to give corticosteroids, which can help the fetus’s lungs mature. Delaying can also give you time to take medications to reduce your blood pressure and help prevent seizures.
 If your health or the fetus’s health worsens, you and your ob-gyn should discuss immediate delivery.
If your health or the fetus’s health worsens, you and your ob-gyn should discuss immediate delivery.Read Preterm Labor and Birth or Extremely Preterm Birth to learn more.
-
Prevention involves identifying whether you have risk factors for preeclampsia and taking steps to address them.
-
Low-dose aspirin may reduce the risk of preeclampsia in some women. Your ob-gyn may recommend that you take low-dose aspirin if
Low-dose aspirin may also be considered if you are Black or if you have a low income, even if you have no other risk factors.
Talk with your ob-gyn about whether you should take aspirin. Do not start taking aspirin on your own without talking with your ob-gyn.
-
If you have high blood pressure and want to get pregnant, see your ob-gyn for a check-up.
 Your ob-gyn will want to know if your high blood pressure is under control and if it has affected your health.
Your ob-gyn will want to know if your high blood pressure is under control and if it has affected your health. You may have tests to check how your heart and kidneys are working. Your medications should be reviewed to see if you need to switch to others that are safer during pregnancy. You should also talk about the signs and symptoms of preeclampsia.
-
Arteries: Blood vessels that carry oxygen-rich blood from the heart to the rest of the body.
Body Mass Index (BMI): A number calculated from height and weight. BMI is used to determine whether a person is underweight, normal weight, overweight, or obese.
Cesarean Birth: Birth of a fetus from the uterus through an incision (cut) made in the woman’s abdomen.
Chronic Hypertension: Blood pressure that is higher than normal for a person’s age, sex, and physical condition.

Complications: Diseases or conditions that happen as a result of another disease or condition. An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
Corticosteroids: Drugs given for arthritis or other medical conditions. These drugs also are given to help fetal lungs mature before birth.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Diastolic Blood Pressure: The force of the blood in the arteries when the heart is relaxed. It is the lower reading when blood pressure is taken.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gestational Hypertension: High blood pressure that is diagnosed after 20 weeks of pregnancy.
HELLP Syndrome: A severe type of preeclampsia.
 HELLP stands for hemolysis, elevated liver enzymes, and low platelet count.
HELLP stands for hemolysis, elevated liver enzymes, and low platelet count.High Blood Pressure: Blood pressure above the normal level. Also called hypertension.
Hypertension: High blood pressure.
In Vitro Fertilization (IVF): A procedure in which an egg is removed from a woman’s ovary, fertilized in a laboratory with the man’s sperm, and then transferred to the woman’s uterus to achieve a pregnancy.
Kick Count: A record kept during late pregnancy of the number of times a fetus moves over a certain period.
Kidneys: Organs that filter the blood to remove waste that becomes urine.
Lupus: An autoimmune disorder that affects the connective tissues in the body. The disorder can cause arthritis, kidney disease, heart disease, blood disorders, and complications during pregnancy.
 Also called systemic lupus erythematosus or SLE.
Also called systemic lupus erythematosus or SLE.Nutrients: Nourishing substances found in food, such as vitamins and minerals.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Oxygen: An element that we breathe in to sustain life.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Placental Abruption: A condition in which the placenta has begun to separate from the uterus before the fetus is born.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain in the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.

Preterm: Less than 37 weeks of pregnancy.
Stroke: A sudden interruption of blood flow to all or part of the brain, caused by blockage or bursting of a blood vessel in the brain. A stroke often results in loss of consciousness and temporary or permanent paralysis.
Systolic Blood Pressure: The force of the blood in the arteries when the heart is contracting. It is the higher reading when blood pressure is taken.
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Veins: Blood vessels that carry blood from various parts of the body back to the heart.
Don't have an ob-gyn? Search for doctors near you.
FAQ034
Last updated: April 2022
Last reviewed: April 2022
Copyright 2022 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
Pregnancy and blood pressure
Pressure and pregnancy
Pregnancy is a period when a woman's body uses all its potential, all its reserves to provide everything necessary for the full bearing of a child.
Blood pressure is one of the main parameters of blood flow intensity in the body. During the period of bearing a baby, a woman’s body is faced with the need to provide oxygen and nutrition not only for herself, but also for her unborn child. A change in the level of pressure during pregnancy becomes an indicator of disturbances in the functioning of the body that threaten the health of a woman and a child, and can also complicate the course of childbirth.
When blood pressure is measured
Blood pressure must be measured at every appointment with an obstetrician-gynecologist or therapist in the antenatal clinic of the future mother. But visits to the doctor's office should not be limited. It is necessary to independently measure this indicator in the morning and in the evening, so that the results can be compared, they must be recorded daily in a special notebook. Particular attention to their pressure should be shown by those women who previously had toxicosis of pregnancy, miscarriages, miscarriages. Women with hypertension, overweight, neurocircular and vegetovascular dystonia, diseases of the kidneys, heart, blood vessels should be on a special account, and measure pressure as often as recommended by the doctor.
Hourly measurement of blood pressure in pregnant women at risk is called daily monitoring. It is done three times during the entire period of pregnancy. The first time - at the very beginning of pregnancy, to identify a woman's tendency to hypertension, the second time - at 24-28 weeks of pregnancy, to identify a predisposition to preeclampsia or late toxicosis of pregnant women, the third time - before childbirth, to determine the degree of risk to the woman and the fetus , as well as to resolve the issue of the method of obstetrics.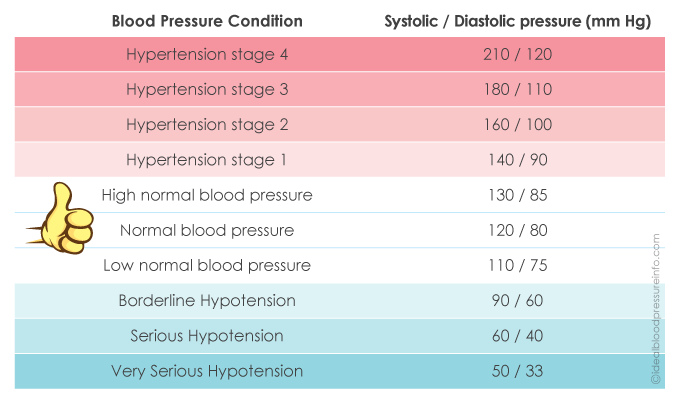
If there are problems with pressure in a pregnant woman, then it is necessary to visit a cardiologist and a general practitioner who can advise what needs to be done to solve the problem of pressure during pregnancy.
Types of blood pressure monitors
There are two types of blood pressure monitors (blood pressure monitor) - mechanical and electronic.
- Mechanical blood pressure monitor used by physicians. It gives the most accurate results. You can learn how to use a mechanical tonometer at home. However, taking blood pressure on your own is very difficult, so if you want to use this type of blood pressure monitor, you will need an assistant.
- Electronic blood pressure monitor is easier to use. It is enough to put the cuff on your arm and press the button. The device itself will do the rest, and you will only have to read the results on the electronic scoreboard. An electronic tonometer shows the value of blood pressure and pulse, memorizing the indicators.
 There are blood pressure monitors, the cuff of which can be worn on the shoulder, on the wrist and even on the finger. For the home, the most suitable device is the cuff of which is worn on the shoulder. Wrist or finger gauges can be used to measure blood pressure at work or while traveling.
There are blood pressure monitors, the cuff of which can be worn on the shoulder, on the wrist and even on the finger. For the home, the most suitable device is the cuff of which is worn on the shoulder. Wrist or finger gauges can be used to measure blood pressure at work or while traveling.
Correct measurement of blood pressure
Do not immediately panic because of high or low blood pressure during pregnancy, you need to make sure that the measurement is correct.
There are several important rules for the correct determination of blood pressure:
- Before measuring, sit down and rest for a couple of minutes, think about something pleasant. Stress is one of the factors in the short-term increase in pressure.
- Place the cuff on your bare arm or thin fabric. It must be sized.
- Measure pressure on both arms.
- Never round the received numbers and write them down.
- It is not recommended to determine the level of blood pressure after a meal or after exercise.
Blood pressure during pregnancy: norm and deviations
Blood pressure is the pressure force of blood flow on the wall of blood vessels. It is measured in millimeters of mercury (mm Hg) and is written in two numbers separated by a slash.
The first digit shows the pressure at the moment of maximum contraction of the heart (systolic blood pressure), and the second - at the time of its complete relaxation (diastolic blood pressure). If blood pressure is normal, we can safely say that the mother’s cardiovascular system is doing its job, which means that all organs receive a sufficient amount of oxygen and nutrients brought with the bloodstream.
Outside of pregnancy, normal blood pressure ranges from 100/60 to 130/80 mmHg. Art. During pregnancy, the pressure may differ slightly from the original: if it is 10% lower or higher than usual, then such changes are still within the normal range. If the pressure is lower or higher than usual by 15–20% or more, then we are dealing with arterial hypotension (low blood pressure) or arterial hypertension (high blood pressure). It is desirable for a woman to know her usual level of pressure, which was before pregnancy, so that the doctor can draw the right conclusions.
It is desirable for a woman to know her usual level of pressure, which was before pregnancy, so that the doctor can draw the right conclusions.
1.1 What is the danger of changes in blood pressure
During pregnancy, through the vasculature of the placenta, nutrients and oxygen constantly flow to the fetus, and back to the mother - the products of its vital activity.
This exchange is only possible at an optimum pressure level. Changes in blood pressure in one direction or the other can have adverse effects.
Under reduced pressure, transport is impaired and the amount of nutrients needed by the baby is reduced, which can lead to fetal growth retardation syndrome. And a significant increase in blood pressure can cause damage to microvessels, foci of hemorrhages are formed, which can lead to placental abruption. That is why during pregnancy it is so important to control blood pressure and keep it at an optimal level.
Normal blood pressure during pregnancy
The norms of blood pressure accepted in general medicine range from 100/60 to 120/80 mmHg.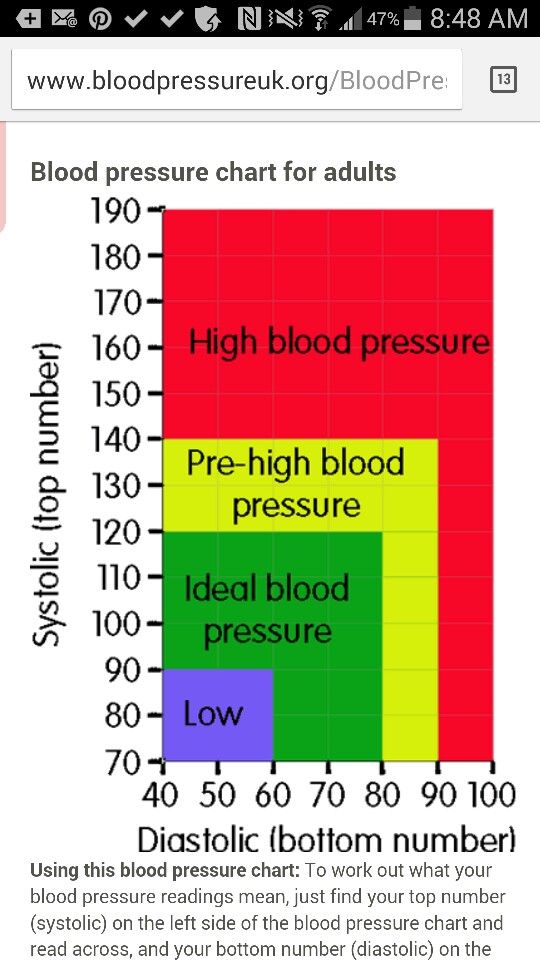 But during pregnancy, these indicators may change somewhat. Usually in the early stages (the entire 1st trimester and up to 20 weeks), these numbers slightly decrease, which is associated with a change in the hormonal background of the whole organism and a restructuring of metabolic processes.
But during pregnancy, these indicators may change somewhat. Usually in the early stages (the entire 1st trimester and up to 20 weeks), these numbers slightly decrease, which is associated with a change in the hormonal background of the whole organism and a restructuring of metabolic processes.
Later, as the fetus grows and develops more intense blood flow to feed it, the pressure may increase relative to "non-pregnant" values. Because of this, the average norms for expectant mothers lie in a wider range - from 105/60 to 139/89 mmHg
Significant deviations from this range upwards are called gestational hypertension, and downwards are called hypotension.
Low blood pressure during pregnancy or hypotension
In the first months of pregnancy, the hormonal background of the expectant mother undergoes significant changes, works with a great load, creating a favorable background for the development of the child, and these changes are often accompanied by a decrease in blood pressure, hypotension.
1.1.1 Possible causes of hypotension
Sometimes it is impossible to determine the cause that provoked the appearance of such a disorder, but the following may play a role in its development:
- Hormonal changes;
- NDC for hypotonic type;
- Infectious diseases;
- Liver pathology;
- Taking certain medications;
- Features of woman's emotionality.
Pregnancy hypotension is often not perceived as a serious threat to the health and progress of pregnancy. However, it can be a serious pathogenic factor that provokes various disorders of the course of pregnancy:
- Termination of pregnancy
- Fetal growth retardation
- Oxygen starvation baby
- Weak labor activity
- Possible bleeding after separation of the placenta
- Relaxation of the uterus after childbirth and rebleeding
1.1.2 Main symptoms of hypotension:
- Nausea, vomiting
- Headache
- Tinnitus
- Shortness of breath
- Dizziness
- Increased fatigue
- Drowsiness
- Pale skin
- Increased perspiration
- Loss of consciousness
1. 1.3 How to increase blood pressure or what to do with low blood pressure
1.3 How to increase blood pressure or what to do with low blood pressure
In general, women with low blood pressure are not hospitalized unless there is a risk to the baby. Expectant mothers are observed by an obstetrician-gynecologist, a therapist and, if necessary, a cardiologist. Most often, in the third trimester, the pressure returns to normal.
Pregnant women should follow these guidelines:
- Get at least 8 hours of sleep (optimally 9-10 hours) and rest during the day if possible.
- Spend more time outdoors (at least 2 hours a day).
- Food should be taken in small portions, but throughout the day.
- Moderate physical activity recommended - do prenatal gymnastics; if possible, swim.
- Useful water treatments - showers, douches, contrast foot baths, as well as massage; physiotherapy (electrosleep, salt-coniferous and mineral baths) and acupuncture are successfully used for treatment.
- If necessary, doctors can prescribe drug therapy: usually, pregnant women are prescribed herbal preparations that increase the tone of the autonomic nervous system, such as extracts of eleutherococcus, radiols, tinctures of magnolia vine, aralia, zamaniha in combination with sedatives (valerian, motherwort), as well as drugs based on caffeine.

If a pregnant woman has lost consciousness due to a sudden drop in pressure, the first thing to do is to lay her horizontally on her side and call an ambulance. Then open the door or window, unfasten the collar, give a sniff of ammonia. You can massage the area between the nose and lip or act on the fingertips on the hands.
High blood pressure during pregnancy or hypertension
Arterial hypertension is a disease characterized by a persistent increase in blood pressure. The changes that occur in the body during pregnancy predispose to the development of hypertension and therefore pregnant women are at a higher risk of developing hypertension than the general population. Arterial hypertension is a risk factor for various complications of pregnancy and ranks second in the list of causes of maternal death. At the same time, the diagnosis and treatment of arterial hypertension in pregnant women requires a special approach.
If before pregnancy you noted that your blood pressure was higher than normal, drank pills, visited the appropriate doctors, be prepared that this problem will come up now. And, most likely, it will manifest itself with greater force.
And, most likely, it will manifest itself with greater force.
Remember: now the situation is completely different, you do not need to take the same pills as before pregnancy.
Forms of arterial hypertension during pregnancy
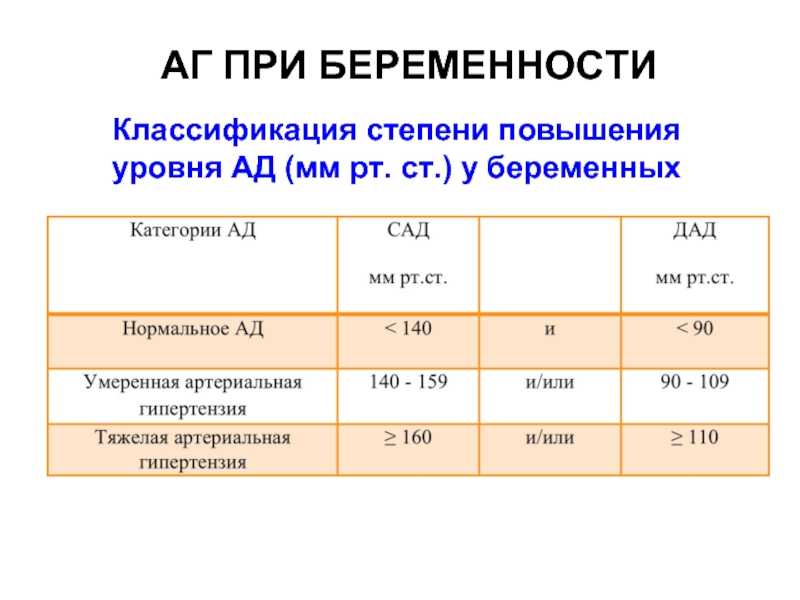
Arterial hypertension of pregnancy is an increase in blood pressure during pregnancy. It is regarded as a persistent increase in systolic blood pressure above 140 mm Hg. and diastolic blood pressure above 90 mmHg in women with normal blood pressure before pregnancy. Women with such an increase in pressure require close medical supervision.
There are several types of arterial hypertension during pregnancy:
- Chronic hypertension is characterized by high blood pressure before pregnancy and persistence after pregnancy.
- Arterial hypertension of pregnancy is a persistent increase in blood pressure that develops after the 20th week of pregnancy, which disappears at the end of pregnancy.
- Pre-eclampsia/eclampsia is a severe impairment of the cardiovascular system and kidneys during pregnancy, which includes: hypertension and impaired renal function.

In pregnant women, arterial hypertension occurs with a frequency of 4-8%, which is a very high figure, especially if we take into account the young age of most expectant mothers. During pregnancy, the woman's body adapts to new conditions of functioning, which include ensuring the life and development of the fetus. On the part of the cardiovascular system in the body of a pregnant woman, the following changes occur:
- An increase in blood volume and the appearance of a placental circulatory system is necessary for the nutrition and development of the child. In pregnant women, the volume of circulating blood increases by 25-30%, which, in addition to ensuring the nutrition of the child, allows women to lose part of the blood during childbirth, without significant damage to health.
- Increased heart rate.
- Increased intra-abdominal pressure, diaphragmatic elevation and change in the position of the heart in the chest due to a significant increase in the size of the uterus.

- Gradual weight gain in a pregnant woman.
Possible other causes of high blood pressure
- Exercise
- Drinking strong tea or coffee
- Chronic stress, fatigue, lack of sleep, emotional tension
- Smoking, alcohol abuse
- Unbalanced diet, lack of vitamins and minerals
- Obesity, overweight
- Multiple pregnancy
- Lack of physical activity
- Diseases of the thyroid gland
- Diseases of the adrenal glands
- Diabetes mellitus
- Head, brain and spinal cord injuries
- Encephalitis
- Myelitis
- Diseases of the heart and blood vessels
- Renal dysfunction
- Hereditary predisposition
Main symptoms of hypertension:
- Headache
- Nausea, vomiting
- Dizziness, weakness, impotence
- Redness of the skin of the hands and face
- Noise or ringing in the ears
- Visual impairment
- Edema
- Urinary protein excretion
- Convulsions
High blood pressure can cause complications such as retinal detachment or retinal hemorrhage, which can lead to partial or complete loss of vision.
If blood pressure began to rise in the second or third trimester of pregnancy, then we are probably dealing with a serious complication of pregnancy - preeclampsia.
Preeclampsia is a special condition that occurs only during pregnancy and ends with its completion. The manifestations of preeclampsia are varied, but the classic symptoms are:
- arterial hypertension
- edema
- proteinuria (protein in urine)
With gestosis, microcirculation is disturbed in all vital organs: the blood supply to the brain worsens, kidney failure develops, the blood becomes viscous, and the resulting microthrombi disrupt the functioning of all organs and systems. Of particular danger is such damage to the vessels of the placenta and the brain. The most severe manifestation of preeclampsia - eclampsia - convulsive seizures, ending in a cerebral coma.
But preeclampsia often begins with a pathological weight gain. Expectant mothers often wonder why this doctor pays such attention to weight. Well, think about it, added a couple of extra pounds.
Expectant mothers often wonder why this doctor pays such attention to weight. Well, think about it, added a couple of extra pounds.
But after all, such an increase is due to fluid retention in the body, or the so-called latent edema.
And if treatment is not started in time, all manifestations of preeclampsia will not be long in coming. If there was an increase in blood pressure before the onset of pregnancy, then its successful course is possible only with good preparation and the correct selection of drugs that reduce pressure. With uncomplicated hypertension and a slight increase in pressure, only non-drug measures are sufficient.
More about preeclampsia
Treatment and prevention of arterial hypertension during pregnancy
Treatment of arterial hypertension during pregnancy is a complex and responsible task. Therefore, the basis of any type of treatment should be close cooperation between the patient and the doctor.
In the treatment of arterial hypertension in pregnancy, as well as in the treatment of arterial hypertension, the following methods are used: non-drug treatment and drug treatment.
Non-drug treatment, that is, treatment without drugs, is the most appropriate treatment for hypertension during pregnancy, as many of the drugs used in the treatment of this disease can be dangerous to the fetus.
What to do with pressure, how to reduce pressure during pregnancy
Non-drug treatment and prevention of arterial hypertension includes:
- Diet. The main requirements for the diet of women suffering from hypertension are a reduction in the consumption of table salt, coffee, tea, and the rejection of bad habits. The allowable amount of salt per day for patients with hypertension is 5 grams, while the calculation must include not only the salt with which we season food, but also the salt contained in various foods.
- Physical activity. Moderate physical activity has a positive effect on the general condition of the body, promotes fat burning, normalizes metabolism, improves blood supply to internal organs and the fetus, increases muscle tone and helps to establish the correct position of the fetus in the uterus.
 For the treatment and prevention of arterial hypertension during pregnancy, daily physical activity in the form of gymnastics (preferably with an instructor), hiking in the fresh air, and swimming are recommended.
For the treatment and prevention of arterial hypertension during pregnancy, daily physical activity in the form of gymnastics (preferably with an instructor), hiking in the fresh air, and swimming are recommended. - Maintenance of normal body weight. The common expression that during pregnancy a woman "should eat for two" is not true. In fact, an "energy supplement" during pregnancy should not exceed 350 kcal. At the same time, maintaining normal body weight during pregnancy is extremely important for maintaining the health of the pregnant woman herself and her child (obesity contributes to the development of hypertension and diabetes). The normal weight gain of a pregnant woman by the end of pregnancy should not exceed 12 kg.
Drug treatment of hypertension during pregnancy should be carried out under the supervision of a specialist doctor and only with safe drugs.
- With a single slight increase in pressure, treatment begins with the appointment of sedative natural drugs, for example: valerian, motherwort, novopassitis and others.
 Together with non-drug therapy, these measures are very effective.
Together with non-drug therapy, these measures are very effective. - For persistent high blood pressure, the following drugs can usually be prescribed, but only on the recommendation of a doctor. The main drug or "drug of choice" the most effective and safe is Methyldopa (Dopegyt), which can be used during pregnancy from a short gestation period.
- A group of drugs that can be prescribed from the second trimester of pregnancy are calcium channel blockers: Verapamil, Nifedipine.
- With persistent hypertension from the 2nd-3rd trimester, β-blockers can be prescribed, this group of drugs does not have a teratogenic effect.
Prenatal monitoring of the fetus is necessary while taking medications.
If the pressure rises suddenly and you feel unwell, urgent hospitalization is necessary. Only in a hospital is complete control over the condition of the child and mother and full therapy possible.
A birth plan and referral for pregnant women with high blood pressure is made in advance. If there are problems that cannot be corrected, a caesarean section is performed.
If there are problems that cannot be corrected, a caesarean section is performed.
Follow your doctor's advice. He is a professional, he knows what is best for you and your child!
Tags: pregnancy
High blood pressure during pregnancy
But its meaning is not always correctly controlled and interpreted. Let's figure out how to properly control blood pressure during pregnancy, which blood pressure is considered elevated, why it can rise and what to do about it and what not to do.
Blood pressure measurement
Blood pressure is monitored using a tonometer: electronic, semi-automatic or mechanical. You can buy any that you can handle and the cuff of which suits you in diameter. The only thing to consider is that the blood pressure cuff should be worn on the upper arm, carpal blood pressure monitors are too inaccurate and cannot be relied upon.
Measurement of blood pressure is best done in a sitting position, and after you have spent about fifteen minutes in this position, in a state of physical and emotional rest, you do not need to talk while measuring blood pressure.
The cuff is worn on the shoulder freed from clothing, its lower edge should be a few centimeters above the elbow. The arm on which blood pressure is measured should be in a relaxed position, the cuff should be located approximately at the level of the heart. Measurement is performed on one arm, measurement on two arms, which was previously required for all pregnant women, is now excluded from all clinical recommendations.
When measuring with the mechanical blood pressure monitor, the cuff is inflated to the digits, approximately twenty to thirty mm. rt. Art. higher than expected blood pressure. The air from the cuff is released slowly, the appearance of sound marks the numbers of systolic blood pressure, the disappearance of the sound - diastolic. This is not "cardiac" and "renal" pressure, but - systolic and diastolic.
Measurement of blood pressure is carried out at each visit to the obstetrician-gynecologist - office measurement of blood pressure, at home of the pregnant woman herself or her relative - outpatient measurement of blood pressure.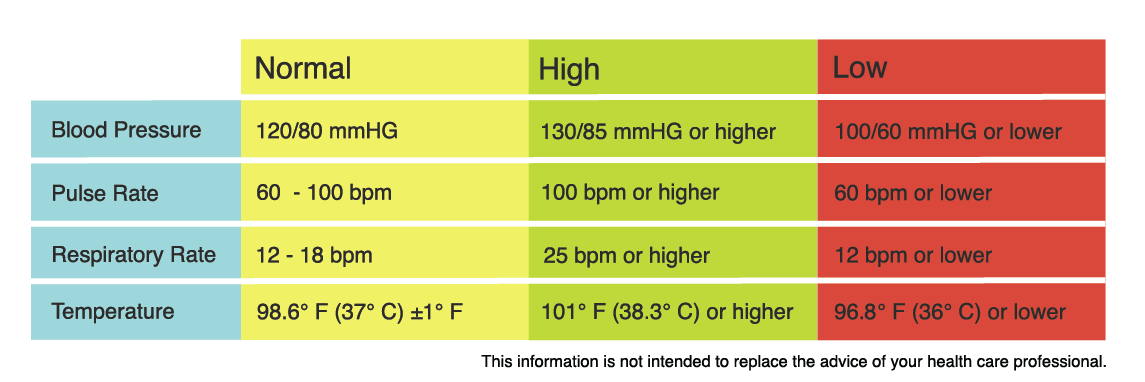 If necessary, the doctor may recommend that the patient keep a blood pressure diary - measure blood pressure several times a day for some time, writing down the numbers. Ceteris paribus, more reliable information is obtained from outpatient (at home) measurements.
If necessary, the doctor may recommend that the patient keep a blood pressure diary - measure blood pressure several times a day for some time, writing down the numbers. Ceteris paribus, more reliable information is obtained from outpatient (at home) measurements.
If there is doubt about the correctness of the patient's blood pressure measurement or if there is a suspicion of an increase in blood pressure at night, the doctor may prescribe the patient 24-hour blood pressure monitoring (ABPM), in which blood pressure is measured automatically at certain intervals within one day.
In general, during pregnancy, blood pressure in the first trimester is lower than normal for the patient, in the second or third it returns to her usual numbers, by the third trimester it may be slightly higher, but within normal numbers. Blood pressure below 140/9 is considered normal during pregnancy.0 mm. rt. Art.
If the patient is prone to arterial hypotension (low blood pressure), elevated blood pressure is still considered to be blood pressure above 140/90 mm. rt. Art., lower figures do not require any additional examination or treatment, even if they are higher than usual for the patient. None of the clinical guidelines for the treatment of arterial hypertension during pregnancy indicate the need for treatment with higher blood pressure than usual, but not reaching a value of 140/90 mm. rt. Art.
rt. Art., lower figures do not require any additional examination or treatment, even if they are higher than usual for the patient. None of the clinical guidelines for the treatment of arterial hypertension during pregnancy indicate the need for treatment with higher blood pressure than usual, but not reaching a value of 140/90 mm. rt. Art.
AD 140/90 mm. rt. Art. and above must be recorded 2 or more times with an interval between measurements of at least 4 hours to be considered hypertension.
Causes of high blood pressure
There are three causes of high blood pressure during pregnancy: chronic arterial hypertension, gestational arterial hypertension and preeclampsia.
Chronic arterial hypertension is the general name for all cases of high blood pressure that existed before pregnancy. Chronic arterial hypertension is not divided into primary (due to unknown causes) and secondary (resulting from a disease), in contrast to arterial hypertension detected outside of pregnancy. Also, chronic arterial hypertension includes situations when a woman did not control blood pressure before pregnancy, and for the first time an increase in blood pressure was detected only in the first half (up to 20 weeks) of pregnancy.
Also, chronic arterial hypertension includes situations when a woman did not control blood pressure before pregnancy, and for the first time an increase in blood pressure was detected only in the first half (up to 20 weeks) of pregnancy.
Gestational hypertension occurs from the twentieth week until the end of the term, and is not accompanied by protein excretion in the urine.
Pre-eclampsia, unlike gestational hypertension, also develops after 20 weeks of gestation, and is accompanied by the release of protein into the urine (proteinuria). Preeclampsia can also occur after delivery. Signs of an increase in the severity of preeclampsia are the appearance of a headache, dizziness, visual disturbances, pain in the solar plexus and / or in the right hypochondrium, pain under the right shoulder blade, respiratory failure, and some changes in blood tests. These signs require urgent hospitalization.
The extreme case of preeclampsia - eclampsia - is characterized by the occurrence of convulsions and threatens the life of both the mother and the child, therefore, it requires an emergency delivery, regardless of the gestational age, only in this way it becomes possible to save the life of the mother and child.
Since an increase in blood pressure may occur before proteinuria in pre-eclampsia, it is possible to distinguish gestational arterial hypertension from preeclampsia only in retrospect - if blood pressure increased, and protein did not appear in the daily urine, it can be said with certainty that this increase in blood pressure was due to specifically gestational hypertension.
Preeclampsia may be associated with chronic arterial hypertension that existed before pregnancy.
Treatment of Hypertensive Disorders
Hypertensive disorders are an important cause of maternal and perinatal death, increase the rate of preterm birth, and are indeed a serious problem and should not be ignored.
The only one to date proven to be effective in preventing pre-eclampsia drug is acetylsalicylic acid. It is prescribed starting from the 13th week of pregnancy at a low dose and at this dosage does not lead to impaired fetal development, unlike high doses.
Treatment of any arterial hypertension during pregnancy is prescribed only by a doctor.
In case of chronic arterial hypertension uncomplicated by damage to other organs, treatment is started at a blood pressure of 150/90 mm. rt. Art. and more, with gestational arterial hypertension and preeclampsia - with blood pressure 140/90 mm. rt. Art. and more.
BP should be maintained at 130-150/80/95 mmHg during treatment. rt. Art., since a more radical decrease in blood pressure is fraught with impaired blood supply to the fetus and is not recommended.
There are several groups of antihypertensive drugs, the use of which during pregnancy can lead to impaired fetal development or death, so they should not be used during pregnancy. These are angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. Do not use during pregnancy and diuretics (drugs with a diuretic effect).
Usually, treatment is started with methyldopa, but it is also possible to use certain drugs from the group of beta-blockers and some drugs from the group of calcium antagonists, which are best studied from the point of view of safety in pregnancy. It is possible to use combinations of these drugs.
It is possible to use combinations of these drugs.
Separately, a few words should be said about magnesium sulfate (magnesium sulphate). This drug has practically no antihypertensive effect, and its use during pregnancy is limited only to preeclampsia, which threatens the development of eclampsia. It is needed to prevent the development of seizures (neuroprotective effect). It should not be used to influence elevated blood pressure.
Hypertension during pregnancy, is usually delivered through the natural birth canal, except in cases of severe pre-eclampsia, eclampsia and their complications requiring emergency delivery by caesarean section, regardless of the gestational age for health reasons.
Chronic arterial hypertension that persists during lactation and is not complicated by damage to other organs does not require medical treatment for blood pressure less than 150/95 mm. rt. Art. Arterial hypertension after childbirth does not require stopping breastfeeding; on the contrary, the protective effect of lactation in arterial hypertension has been proven.