How to help constipation pregnant
Constipation in Pregnancy: 5 Fool-Proof Remedies
Infrequent bowel movements. Abdominal pain. The passage of hard stools.
If you’re pregnant, you’ve probably experienced these three familiar signs of constipation. Hormonal changes, pressure on the womb, and the iron in prenatal vitamins are to blame.
Why Am I Constipated?
An increase in the progesterone hormone during pregnancy causes the relaxation of your body’s muscles. That includes your intestines. And slower moving intestines means slower digestion. This can lead to constipation.
Constipation is common during pregnancy. Almost three out of four pregnant women will experience constipation and other bowel issues at some point, according to a study published in Acta Obstetricia et Gynecologica Scandinavica.
From over-the-counter pills to natural cures, there are a whole host of remedies available for relieving constipation.
But when pregnancy’s involved, the number of solutions shrinks.
These five remedies are pregnancy-safe.
Share on Pinterest
A diet high in fiber helps prevention constipation. It also supplies pregnant women with vitamins and antioxidants.
Pregnant women should try to consume 25 to 30 grams of dietary fiber each day to stay regular and healthy.
Good choices include fresh fruits, vegetables, beans, peas, lentils, bran cereals, prunes, and whole-grain bread.
Try cutting up some raspberries, apples, bananas, figs, and strawberries for a refreshing fruit salad. Or roast some sweet corn, Brussels sprouts, and carrots for a delightful side dish.
Share on Pinterest
It’s important to stay hydrated during pregnancy. That might mean doubling your water intake.
Pregnant women should drink at least eight 12-ounce glasses of water a day. This will help keep your bowels soft and moving smoothly through your digestive tract.
Share on Pinterest
Try breaking up your daily food intake into five or six smaller meals to help with constipation relief. This will allow the stomach to digest food without having to work overtime, and allow it to transfer food to the intestine and colon smoothly.
This will allow the stomach to digest food without having to work overtime, and allow it to transfer food to the intestine and colon smoothly.
Eating large meals can overload your stomach and make it harder for your digestive system to process what you’ve consumed.
Share on Pinterest
Regular physical activity can help reduce constipation. Exercise stimulates your bowels. Pregnant women should try to exercise three times a week for 20 to 30 minutes each.
The options for exercise are endless. Try walking down your favorite hiking path, swimming at your local gym, or practicing prenatal yoga on a relaxing afternoon.
Check with your doctor about what exercises are safe for you and your baby.
Share on Pinterest
If other natural options have failed, doctors will sometimes prescribe stool softeners like Colace on a short-term basis to help pregnant women with constipation. Colace stool softeners are available online. However, long-term use can lead to dehydration or change your electrolyte balance.
Stool softeners help moisten your bowels so they are easier to pass. They are especially useful for pregnant women taking constipation-causing iron supplements. Doctors will often prescribe softeners along with iron pills. You can find a variety of iron supplements here.
Stool softeners are medications, so it’s best to check with your doctor if they are safe for you.
Takeaway
Constipation relief during pregnancy is common, and it can be remedied.
Just follow the steps above to help ease the discomfort of backed up bowels while you wait for your little one to arrive.
Tips for a Healthy and Happy Pregnancy6 Natural Constipation Remedies
Constipation can be an uncomfortable problem to have. But many people experience it from time to time, especially while pregnant or taking certain medications.
There are many potential causes of constipation. There are also many treatment options. Adjusting your lifestyle habits or reaching for home remedies may be all you need to treat occasional constipation.
Take the time to learn about some of the best natural remedies for constipation.
Staying in bed all day may seem like a nice way to spend a lazy Sunday. But skipping your morning bathroom break can lead to problems.
Not going to the bathroom regularly can cause your stools to harden and your intestines to slow their motion. Try to go to the bathroom before bedtime and first thing in the morning. Not everyone needs to go at these times, but following a regular schedule can help. You may be able to ward off future bouts of constipation by getting up and moving around at the same time every day.
You might not feel like taking a trip to the gym when you’re backed up, but exercise may provide the relief you need. Going for a walk or run, for example, can help stimulate the muscles in your intestines and colon. Any physical movement helps the bowels move things through.
To help prevent and relieve constipation, make exercise a regular part of your routine. Aim for at least 150 minutes of moderate aerobic activity per week. That’s equivalent to 30 minutes of aerobic exercise per day, five days a week. If that seems like too much for you, set a smaller goal to start. Try to get some physical activity every day to stay regular.
That’s equivalent to 30 minutes of aerobic exercise per day, five days a week. If that seems like too much for you, set a smaller goal to start. Try to get some physical activity every day to stay regular.
Drinking enough fluids can also help prevent and treat constipation. It can help move food through your digestive system and stop stool from hardening.
In general, you should aim to drink about nine cups of liquid a day if you’re a woman and 13 cups if you’re a man. If you’re constipated or taking fiber supplements, you may need to drink more. Ask your doctor for guidance.
Though water is an ideal choice, don’t discount the benefits of other beverages. Green tea, black tea, coffee, and other drinks can all count towards your daily fluid intake.
Getting enough fiber in your diet is crucial. There are two main types of fiber: soluble fiber soaks up water, which helps keep your stool soft; insoluble fiber adds bulk to your stool, which helps it move through your digestive system faster.
To help treat mild cases of constipation, try eating easy-to-digest foods that are high in fiber, such as berries, bananas, prunes, or avocado. To prevent future problems, include plenty of fiber-rich foods in your diet, including vegetables, fruits, and whole grains. You may also benefit from a daily fiber supplement, such as psyllium husk (Metamucil).
Getting enough magnesium in your diet might also help relieve constipation. Oral magnesium supplements function as osmotic laxatives. That means they pull water into your digestive system, which helps soften your stool.
You can purchase magnesium capsules at health food stores and pharmacies. You can also get magnesium from food sources. Talk to your doctor before talking magnesium if you have a history of kidney problems. Conveniently, most foods that are high in magnesium are also high in fiber. For example, whole grains and dark leafy greens are good sources of both.
According to Dr. Arielle Miller Levitan, an Illinois-based internal medicine specialist, eating a tablespoon or two of coconut oil each day might help lubricate your intestines. In turn, this may help prevent constipation. Ask your doctor if this remedy might work for you.
In turn, this may help prevent constipation. Ask your doctor if this remedy might work for you.
If the idea of swallowing a spoonful of coconut oil doesn’t appeal to you, there are other ways to add it to your diet. For example, you could mix it into your morning coffee or blend it with vinegar for a simple salad dressing.
The next time you feel a little constipated, try these home remedies. They may be all you need to get your bowels moving again.
If these remedies don’t work, or you find that you’re chronically constipated, talk to your doctor. They might recommend lifestyle changes, medication changes, or other treatments. In some cases, chronic constipation is caused by another underlying health condition. Your doctor can help you identify and treat the cause
Treatment of constipation in pregnant women in a private clinic
This is one of the most common, but at the same time the most delicate problems that occur in at least 50% of pregnant women. In a normal state, bowel movements should be daily and in sufficient volume. Any deviations in this process require attention and adjustment of the diet, lifestyle and even psychological attitude. From a physiological point of view, problems in the work of the gastrointestinal tract are explained by hormonal changes and the physiological characteristics of the body of a pregnant woman (under the influence of various processes in different phases of pregnancy, the contraction of the smooth muscles of the intestine is weakened, in addition, the enlarged uterus compresses the intestines, etc.).
Any deviations in this process require attention and adjustment of the diet, lifestyle and even psychological attitude. From a physiological point of view, problems in the work of the gastrointestinal tract are explained by hormonal changes and the physiological characteristics of the body of a pregnant woman (under the influence of various processes in different phases of pregnancy, the contraction of the smooth muscles of the intestine is weakened, in addition, the enlarged uterus compresses the intestines, etc.).
Among other - non-medical reasons - the most common are the features of a woman's lifestyle: systematic stress; lack of mobility; lack of fiber; low water intake (not liquids!) and/or high intake of refined foods and foods with a high composition of sugar, homogenized fats and salt (fast food). “Refined foods are refined oils, polished rice, white flour and all the familiar white refined sugar, plus fast food with a high composition of sugar, homogenized fats and salt, which slow down the absorption of nutrients by the body and the passage of food in the intestines” (Laima Lankmane, naturopath, herbalist).
Homeopaths say that constipation is not only a “problem” of the rectum, “it is a problem of the whole organism as a whole and it must be solved in a complex way” (D.V. Arkhipova, Ph.D., homeopath): for example, this may be an allergic reaction to certain foods. Therefore, constipation is, in principle, an individual problem, and an individual approach will be the most effective solution to the problem: “Even equally pregnant women do not have 2 identical constipations: some had them before pregnancy, others did not eat properly, others did not move. All good wishes for real constipation will work only in 10% of cases. The only right decision is a full-fledged visit to a homeopath, who will approach the solution of the disharmony that has arisen, taking into account all the individual characteristics of a woman, looking at her as an integral unique system ”(A.S. Gavrilenko, obstetrician-gynecologist, Ph.D., homeopath , reflexologist).
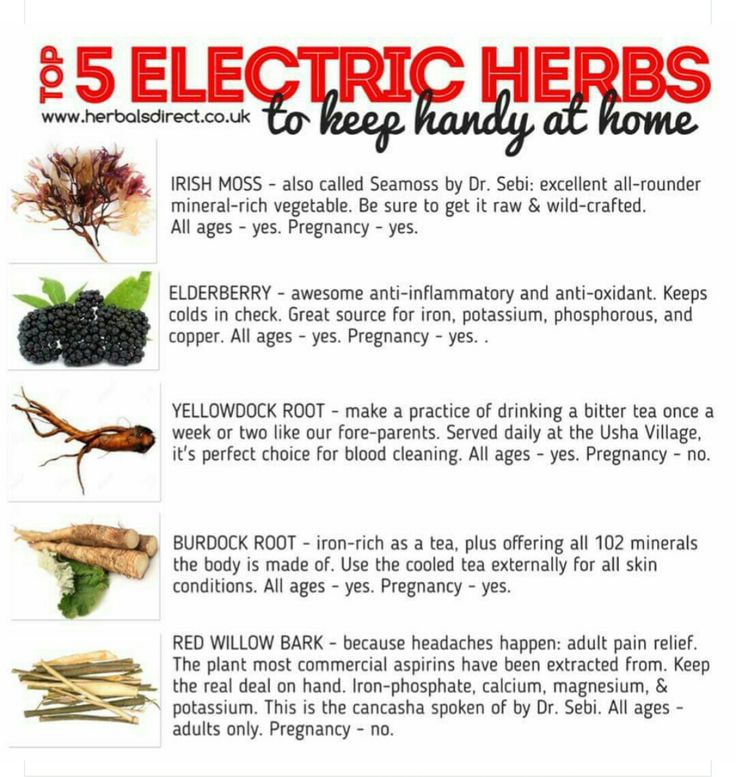
First, about how NOT to solve the problem of constipation: classic laxatives such as hay, aloe vera and castor oil are contraindicated for pregnant women - they can cause premature contractions.
Now about what is POSSIBLE and NEEDED.
DIET
- Need to temporarily eliminate dairy products. “The main milk protein, casein, is one of the most difficult to digest proteins and is also a strong allergen. The fact that cottage cheese itself is capable of causing constipation is probably known to everyone. If you solve the problem with constipation in this way, then carefully introduce natural fermented milk products into the diet (preferably without flavorings and sugar) ”(D.V. Arkhipova, Ph.D., homeopath). It’s not worth worrying that the baby won’t get enough of something - he will take everything he needs from “mother’s reserves”, and the question is not in the amount eaten, but in the amount absorbed by the mother’s body. From the point of view of homeopathy, if you want - eat, no - you don’t need to force yourself, because. food likes and aversions are in accordance with our constitution, and therefore our needs (naturally, this applies to healthy and healthy eating habits).

- It is necessary to monitor the fluid used - or rather, drink enough clean water. Volume - from one to three liters per day, if desired, but not less than a liter. “If you don’t feel like drinking water, you need to remove sweet drinks and teas from the diet and compensate for this with clean water (preferably raw, of artesian origin, pleasant to the taste, and even better thawed).” (T.G. Sadovaya, obstetrician, author of the lecture “Nutrition during pregnancy”).
- “Dried fruits are required (you can pour prunes with water at night and drink an infusion in the morning), and / or drink a glass of water in the morning on an empty stomach (you can add a little lemon juice there) and a glass of water with honey at night” (I.S. Arefyeva, obstetrician gynecologist).
- The diet should have a sufficient amount of fiber: at least 50% of the diet of natural plant foods in raw and processed form (fiber stimulates peristalsis). It can be whole grain cereals, products made from wholemeal flour, fruits before meals or in between, vegetables, berries (the same cranberries help with constipation).
- A daily intake of 1 to 3 tablespoons of unrefined oils has a good effect on the body. “Sweet almond oil (food) has a pronounced laxative effect and does not irritate the intestinal wall. Olive and linseed oils, as well as walnut oil, also have a mild laxative effect. Do not forget that unrefined oils should be stored in the refrigerator (with the exception of olive oil), and flaxseed should be eaten within a month after opening the bottle. (O.L. Bannikova, obstetrician).
- Add magnesium-rich foods to your diet, such as green leafy vegetables, walnuts and almonds, sunflower seeds (unroasted and preferably pre-soaked for 5-7 hours), green buckwheat and spinach. “You can try this recipe - soak 1 teaspoon of flax seeds in ½ cup of warm water and leave for several hours. Then eat it just like that or add it to porridge, soup” (L. Lankmane, naturopath, phytotherapeutist).
- You can try to consume more foods that normalize the balance of intestinal flora - such as kefir (preferably homemade), miso soup, sauerkraut.

- You should not get carried away with strong tea, black coffee, cocoa, chocolate, white bread, flour and slimy soups, semolina, blueberries. All these products, like dry food, have a fixing effect. For the time of problems with the gastrointestinal tract, it is better to observe separate fractional meals, drink liquid 15 minutes before meals or some time later, etc. - that is, to facilitate the assimilation of the food consumed as much as possible. Make sure that there are no distortions - the daily diet should be balanced.
HOW TO HELP
- Enzymatic preparations can be drunk for a short time. If these are preparations of animal origin - no more than 7 days, plant enzymes can be taken longer. You can take probiotics, beneficial gut bacteria that aid digestion. Long-term use of these biological products not only normalizes the intestinal flora, but also contributes to a less pronounced manifestation of dysbacteriosis in a newborn child. (D.V. Arkhipova, homeopath, PhD, pediatrician)
- Check the level of iron with a doctor - against the background of its deficiency, intestinal disorders are also possible.
 “But keep in mind that some iron-containing dietary supplements, unfortunately, can only worsen this condition (not to mention dosage forms). It is better to add foods rich in iron, such as almonds, pine nuts, apricots, avocados, sunflower and pumpkin seeds, wheat germ ”(L. Lankmane, naturopath, herbalist).
“But keep in mind that some iron-containing dietary supplements, unfortunately, can only worsen this condition (not to mention dosage forms). It is better to add foods rich in iron, such as almonds, pine nuts, apricots, avocados, sunflower and pumpkin seeds, wheat germ ”(L. Lankmane, naturopath, herbalist). - Freshly squeezed juices, diluted 1 to 1 with water 15 minutes before meals, stimulate the production of pancreatic enzymes and aid digestion in the most natural way. (D.V. Arkhipova, homeopath, PhD, pediatrician)
- Drink hot - as far as possible - water on an empty stomach, a little later, eat half a banana, chewing it for a long time and macerating it with saliva to a liquid slurry (the banana must be ripe!). (O.L. Bannikova, obstetrician).
- Starting from the second trimester, you can use essential oils: exotic basil (Ocimum basilicum in Latin), seaside pine (Pinus Pinaster), saro (Cinnamosma fragrans, Saro), rosewood (Aniba rosaeodora). “Oils should be only edible, of good quality! It is not recommended to use essential oils during the first 3 months of pregnancy.
 1st composition - take 1 drop of basil, 2 drops of pine on a small piece of sugar or honey and suck under the tongue in the morning on an empty stomach. 2nd composition - basil 30 drops, rosewood 20 drops, saro 10 drops and 40 drops of apricot kernel oil or any other unrefined food oil. Mix. Take 3 drops of this mixture under the tongue on sugar or honey morning and evening before meals for 5-7 days or as needed. When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician)
1st composition - take 1 drop of basil, 2 drops of pine on a small piece of sugar or honey and suck under the tongue in the morning on an empty stomach. 2nd composition - basil 30 drops, rosewood 20 drops, saro 10 drops and 40 drops of apricot kernel oil or any other unrefined food oil. Mix. Take 3 drops of this mixture under the tongue on sugar or honey morning and evening before meals for 5-7 days or as needed. When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician) - If this does not help, you can try to use "Duphalac" for a short time.
LIFESTYLE
Enough physical activity, swimming in the pool. Walking for at least one hour. But the load should be increased gradually. To begin with, one lesson should be no more than 30 minutes. The step should be slow, the shoes are comfortable, and the route should be laid away from the roads. Gymnastics for pregnant women for at least 30 minutes daily. As gymnastics, our yoga instructor for pregnant women Svetlana Shnyrova recommends a few simple exercises:
- backbends in cat pose (standing on all fours),
- alternating leg raises from a sitting position on the floor with support on the hands,
- certain types of soft twists of the spine from a sitting or lying position,
- Breathing exercises such as a few deep belly breaths can also help.
During class, you should carefully monitor your well-being and, if any discomfort occurs, immediately leave the pose. And watch how your baby reacts to the exercises.
These exercises stimulate the intestines, improve blood circulation in the abdominal cavity, and help to establish a regular bowel movement. In general, the problem of constipation should be approached comprehensively, drink more water in the morning, adjust nutrition, move more, walk, swim, do yoga.
MICROLAX® during pregnancy - is it possible to use microclysters for pregnant women
Co-author, editor and medical expert - Klimovich Elina Valerievna.
Views: 116 584
The date of the last update: 21.10.2022.
Average reading time: 7 minutes
The main symptoms of constipation during pregnancy
Why is it so important to use a laxative during pregnancy in a timely manner?
Is MICROLAX ® suitable for pregnant women?
Benefits of using MICROLAX ® during pregnancy
How to use MICROLAX ® during pregnancy?
During pregnancy, many women have difficulty defecation. The constant discomfort associated with stool retention can seriously overshadow the happy waiting time for the baby. Often, the expectant mother does not attach much importance to recurrent constipation or considers them a natural phenomenon that you just need to endure. And some women are forced to put up with discomfort, because they are sure that there are no safe laxatives for pregnant women. However, this is fundamentally wrong. When constipation occurs, it is important to inform the doctor about this problem in a timely manner. The specialist will select a comprehensive treatment and prescribe modern preparations for bowel cleansing with an optimal safety profile, for example, MICROLAX ® .
Back to content
The main symptoms of constipation during pregnancy
Constipation in a pregnant woman is indicated by a decrease in the number of bowel movements: bowel cleansing occurs less than 3 times a week. A deviation from the norm is considered to be a delay in feces for more than 2 days. Violation of the frequency of bowel movements is often accompanied by other symptoms. The feces that accumulate in the intestines become hard and dry. Going to the toilet requires a lot of straining. Dense feces can injure the anus, then defecation will be accompanied by pain. In addition, with constipation, a pregnant woman may be disturbed by a feeling of fullness and blockage in the rectum. Often, even going to the toilet does not bring relief: after a bowel movement, there is a feeling that the intestines have not been completely cleansed. Often, constipation is accompanied by flatulence, bloating.
Up to content
Causes of constipation during pregnancy
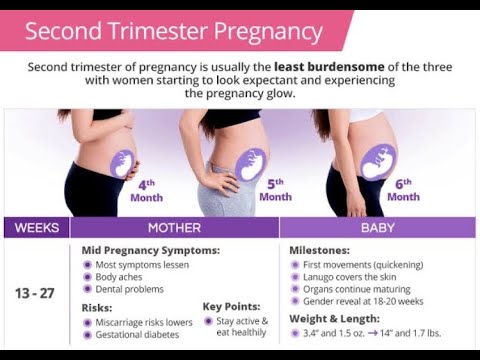
Hormonal changes. In the early stages of pregnancy, the balance of hormones in a woman's body actively changes, in particular, the level of progesterone rises. It reduces the tone of the muscles of the small pelvis: this is important so that the fertilized egg can gain a foothold in the uterus. This action of progesterone also gives a side effect. The hormone slows down the digestive tract and reduces intestinal motility. Very often because of this, constipation occurs in the first trimester of pregnancy.
Decreased physical activity. Many women, having learned that they are expecting a child, give up an active lifestyle and sports. To a certain extent, this is justified, since serious physical exertion can be the cause of miscarriage. As the fetus develops, the outlines of the figure and body weight of the woman change, and for natural reasons it becomes difficult for her to actively move. Hypodynamia leads to a decrease in intestinal tone, which contributes to the development of constipation.
As the fetus develops, the outlines of the figure and body weight of the woman change, and for natural reasons it becomes difficult for her to actively move. Hypodynamia leads to a decrease in intestinal tone, which contributes to the development of constipation.
Taking certain drugs. For normal development, the fetus needs vitamins and microelements, so pregnant women are often prescribed medications containing these beneficial substances. Some of these drugs have a fixing property. First of all, these are products with a high content of calcium and iron.
Fluid deficiency in the body. In late pregnancy, many women experience swelling of the face, legs and arms. Because of this, expectant mothers try to drink less during the day and reduce the consumption of juicy fruits and vegetables. Lack of fluid and fiber leads to compaction of feces and difficulty in emptying the intestines.
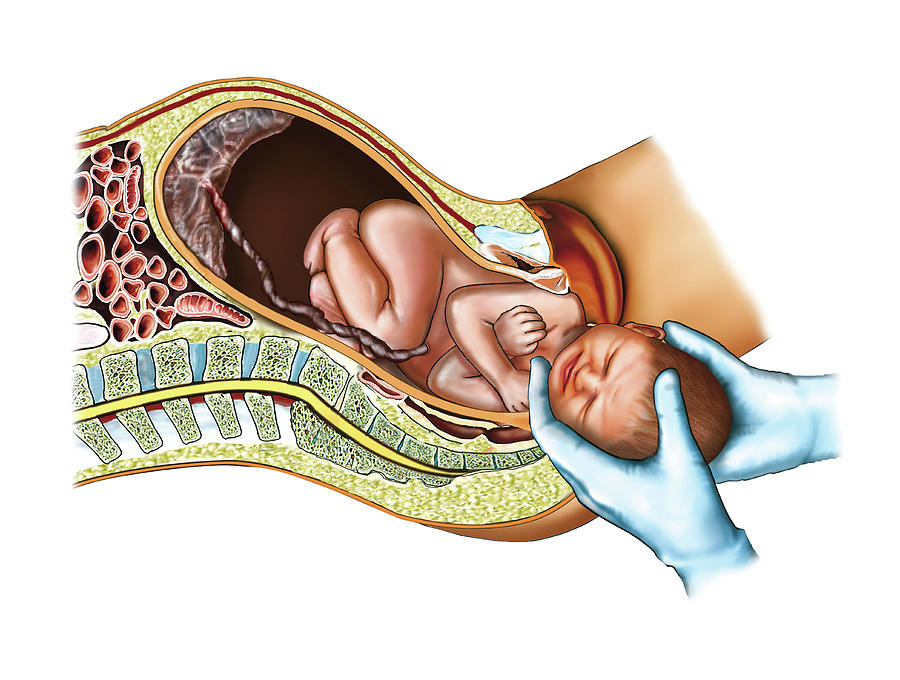
Pressure from an enlarged uterus.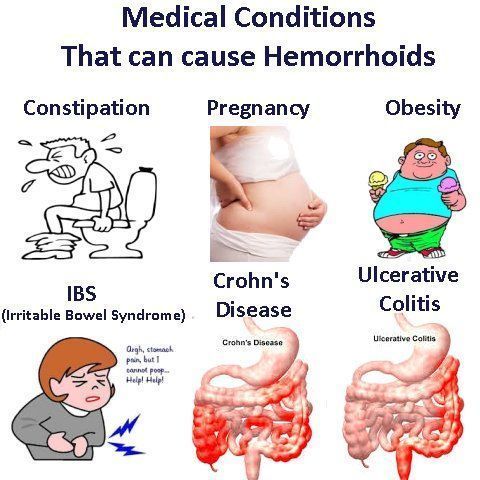 During pregnancy, there is a displacement of the abdominal organs. The uterus takes up more and more space and compresses the surrounding tissues. This can lead to decreased sensitivity and intestinal motility. As a result, constipation occurs. In the later stages, shortly before childbirth, the lowered head of the fetus can also squeeze the intestines.
During pregnancy, there is a displacement of the abdominal organs. The uterus takes up more and more space and compresses the surrounding tissues. This can lead to decreased sensitivity and intestinal motility. As a result, constipation occurs. In the later stages, shortly before childbirth, the lowered head of the fetus can also squeeze the intestines.
Back to Contents
Why is it so important to use laxatives during pregnancy?
Constipation can negatively affect the health of the expectant mother and her baby. Violation of the frequency of bowel movements in some cases can cause inflammatory diseases of the female genital organs and an imbalance in the intestinal microflora. The consequences of constipation in the later stages are especially undesirable. A rectum full of feces can increase the tone of the uterus. This, like too much straining during a bowel movement, can provoke premature birth. That is why it is important for a pregnant woman to cleanse the intestines in a timely manner, if necessary, using laxatives approved by the doctor for use.
Back to Contents
Is MICROLAX
® suitable for pregnant women?According to the instructions for medical use, it is allowed to use MICROLAX ® during pregnancy 1 . This modern laxative in the format of a disposable microclyster softens dense fecal masses in the rectum and does not affect other organs of the digestive system and small pelvis. The active components of the drug are practically not absorbed into the systemic circulation and do not cause uterine contractions. MICROLAX ® can be used in any trimester of pregnancy, after consulting a doctor.
Back to content
Benefits of using MICROLAX
® during pregnancyThe effect of the drug. MICROLAX ® may start to work within 5-15 minutes 2 after application, unlike oral medications which can take effect at the most inopportune moment.
Hygienic packaging. Micro enema MICROLAX ® is intended for single use. It is completely ready for use and does not require preliminary antiseptic treatment.
Micro enema MICROLAX ® is intended for single use. It is completely ready for use and does not require preliminary antiseptic treatment.
Easy application. When using MICROLAX ® , a pregnant woman does not need to individually select the dosage. Microclyster contains the optimal amount of the drug for a single use. The flexible applicator tip allows you to safely and conveniently inject the laxative into the rectum.
Top of page
How to use MICROLAX
® during pregnancy?- Take the tube and break off the seal on the applicator tip.
- Press down on the container so that a drop of the drug lubricates the tip of the microclyster - this will simplify its introduction.
- Insert the applicator tip into the entire rectum.
- Squeeze the tube and squeeze out the contents.
- While continuing to lightly squeeze the container, remove the tip.
If you have any questions about using the product, you will find all the necessary information on how to use it in the instructions.