During the second stage of labor
Stages of labor | March of Dimes
Every woman’s labor is different. And it may be different each time you have a baby.
Learning about stages of labor before your due date can help you know what to expect so you can feel ready for your baby’s birth.
Use a birth plan so your health care provider and hospital staff know what your plans are for labor and after birth.
Having a professional support person, like a doula, during labor can help you have a better experience with labor and birth.
Try to stay comfortable and relaxed through labor. Move around and try different positions to find what works best for you.
What are stages of labor?
Labor (also called childbirth) is the process of your baby leaving the uterus (womb). Labor is divided into three stages:
- Labor
- Pushing and birth
- Delivery of the placenta
Every woman’s labor is different. And your labor may be different each time you have a baby. But there are patterns to labor that are true for most women. Learning about the stages of labor and what happens during each one can help you know what to expect once labor begins.
What is a birth plan?
A birth plan is a set of instructions you make about your baby’s birth. It includes things like:
- Where you want to have your baby
- Who you want to be with you during labor and birth
- If you want medicine to help with labor pain
- If there are cultural traditions you’d like to follow during labor and birth
- If you plan to breastfeed
Before your due date, use the March of Dimes birth plan to help you think about how you want your labor to be. Share the completed plan with your partner, your health care provider and the staff at the hospital where you plan to give birth.
What is a doula?
You may want to have a professional support person help you through labor and childbirth. A doula is a professional labor assistant.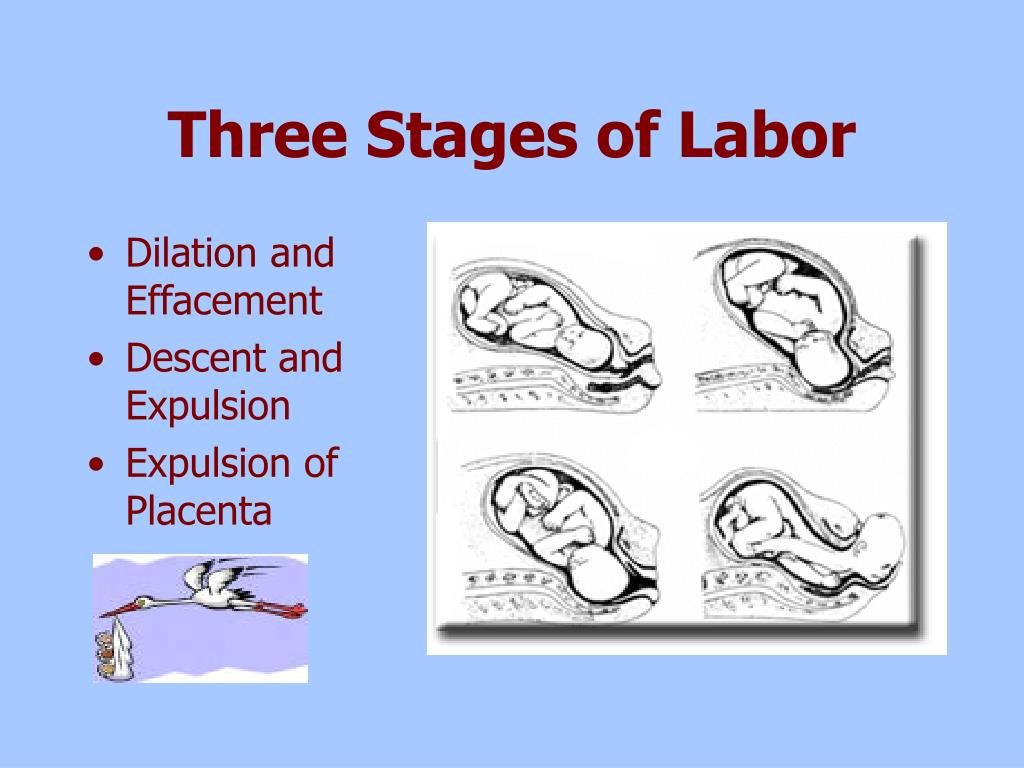 This is someone who is trained to give physical and emotional care and support to women and their families before, during and after childbirth. For example, a doula can:
This is someone who is trained to give physical and emotional care and support to women and their families before, during and after childbirth. For example, a doula can:
- Help you stay comfortable
- Explain what’s happening during labor and birth and any procedures you may have
- Encourage you and give you confidence
- Support your family and friends who are with you during labor
- Let hospital staff know what you need
- Help you get started breastfeeding
Having a support person like a doula can be good for you, your baby and your family. It can help you feel good about your birth experience. Having a doula can help:
- Shorten your labor
- Reduce your need for pain medicine during labor
- Reduce your risk of needing a cesarean birth or the need for your provider to use forceps or suction with a vaginal birth
- Your baby get a good Apgar score at birth. Your baby gets an Apgar test right after birth to check his overall health.
 The test checks his heart rate, breathing, muscle tone, reflexes and skin color.
The test checks his heart rate, breathing, muscle tone, reflexes and skin color.
To find a certified doula, ask your provider or go to DONA International.
You also may want to have your partner, a friend or a family member be a support person to help you through labor. They can go to childbirth education classes with you to learn ways to help, like timing your contractions, helping you relax and helping you move around to find a comfortable position. Ask your provider about childbirth education classes in your area.
If you decide to have a doula or another support person help you with labor and birth, put their names and contact information in your birth plan. Share your plan with your provider and with hospital staff.
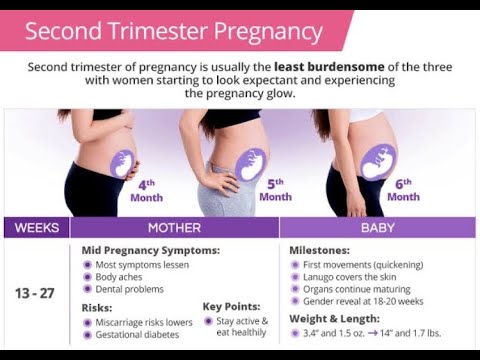
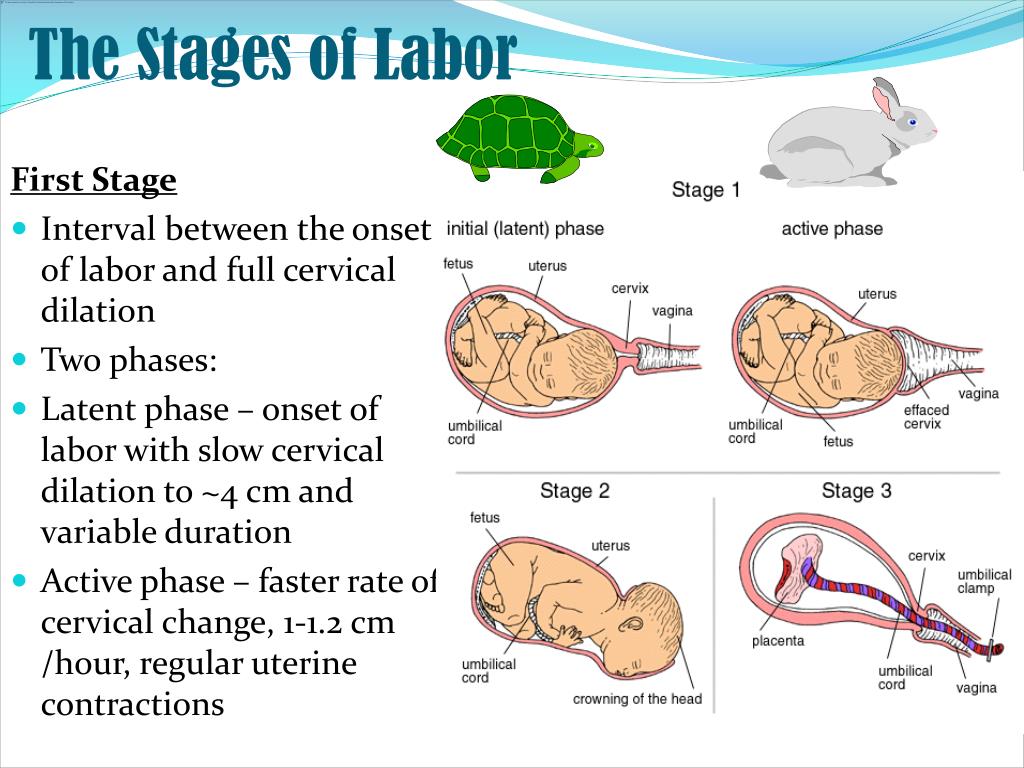
What happens in the first stage of labor?
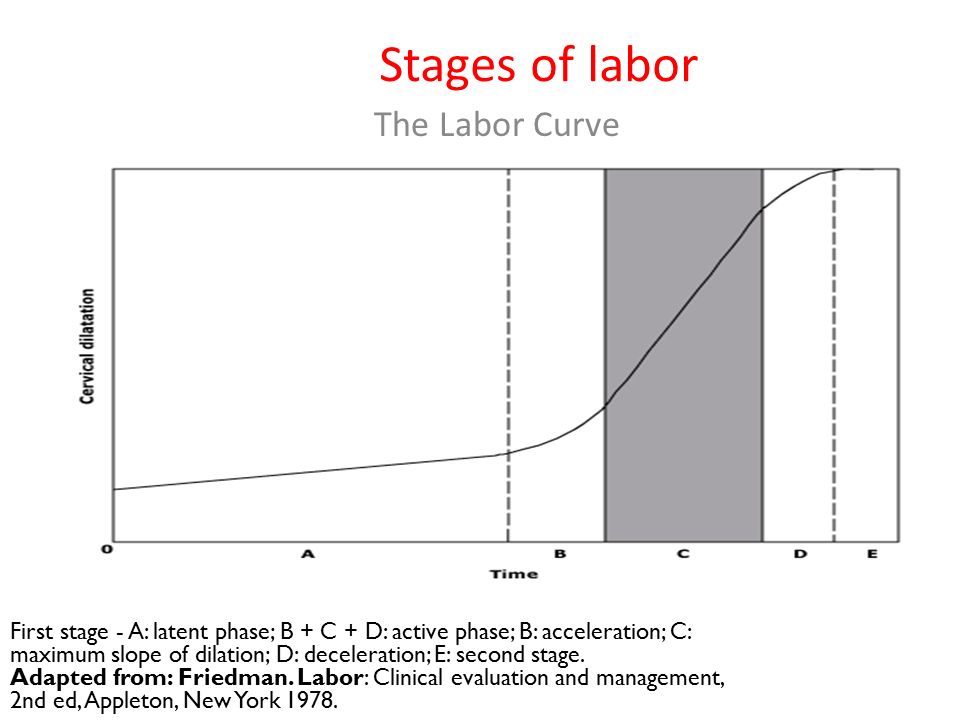
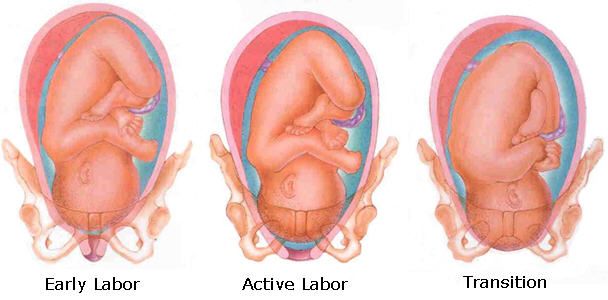
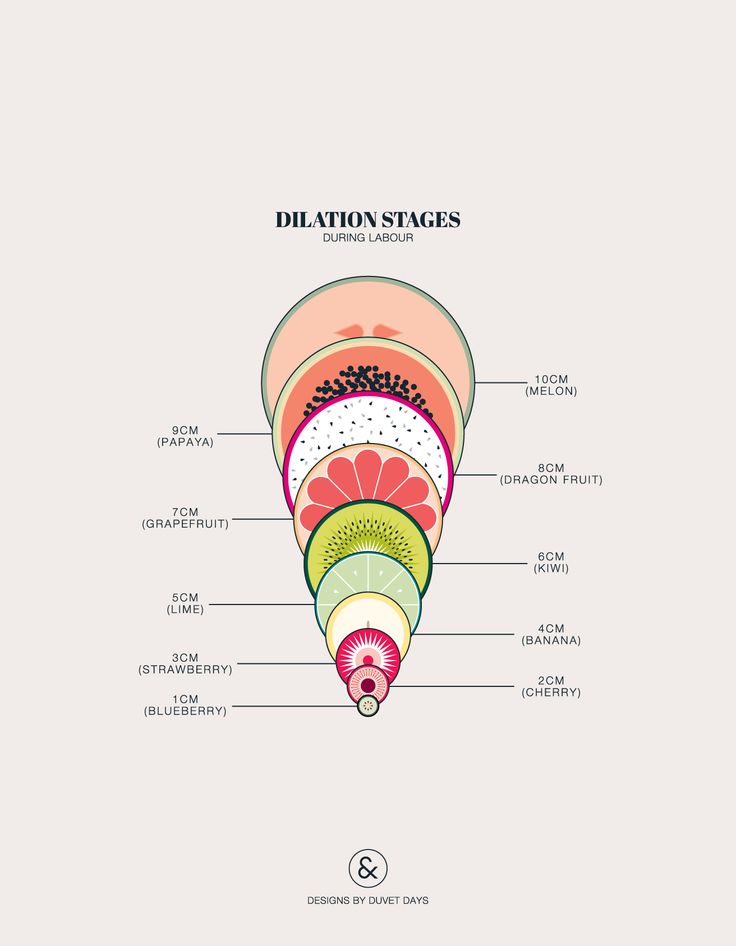
The first stage of labor is the longest stage. For first-time moms, it can last from 12 to 19 hours. It may be shorter (about 14 hours) for moms who’ve already had children. It’s when contractions become strong and regular enough to cause your cervix to dilate (open) and thin out (efface). This lets your baby move lower into your pelvis and into your birth canal (vagina). This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
This lets your baby move lower into your pelvis and into your birth canal (vagina). This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
Early labor
For most first-time moms, early labor lasts about6 to 12 hours. You can spend this time at home or wherever you’re most comfortable. During early labor:
- You may feel mild contractions that come every 5 to 15 minutes and last 60 to 90 seconds.
- You may have a bloody show. This is a pink, red or bloody vaginal discharge. If you have heavy bleeding or bleeding like your period, call your provider right away.
What you can do in early labor:
This is a great time for you to rely on your doula or labor support person. Try the methods you learned about in childbirth education classes about how to relax and cope with pain. During early labor:
- Rest and relax as much as you can.
- Take a shower or bath.
- Go for a walk.
- Change positions often.
- Make sure you’re ready to go to the hospital.
- Take slow, relaxing breaths during contractions.
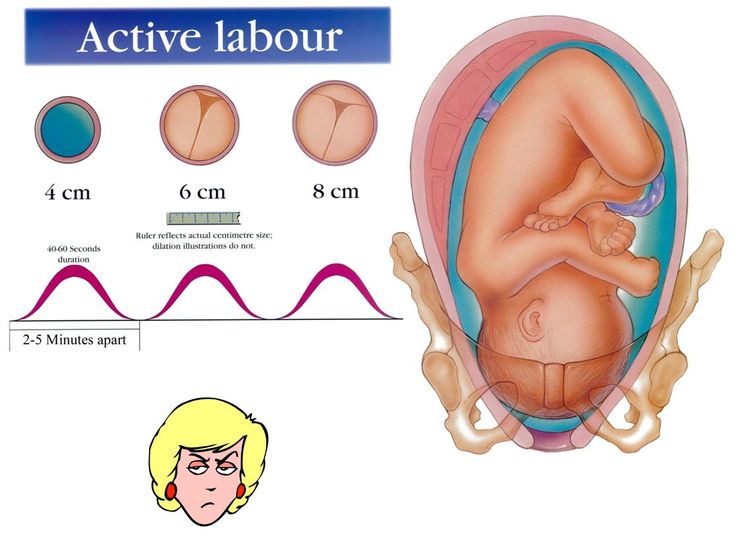
Active labor
This is when you head to the hospital! Active labor usually lasts about 4 to 8 hours. It starts when your contractions are regular and your cervix has dilated to 6 centimeters. In active labor:
- Your contractions get stronger, longer and more painful. Each lasts about 45 seconds and they can be as close as 3 minutes apart.
- You may feel pressure in your lower back, and your legs may cramp.
- You may feel the urge to push.
- Your cervix will dilate up to 10 centimeters.
- If your water hasn’t broken, it may break now.
- You may feel sick to your stomach.
What you can do in active labor:
- Make sure the hospital staff has a copy of your birth plan.
- Try to stay relaxed and not think too hard about the next contraction.
- Move around or change positions. Walk the hallways in the hospital.
- Drink water or other liquids. But don’t eat solid foods.
- If you’re going to take medicine to help relieve labor pain, you can start taking it now. Your choice about pain relief is part of your birth plan.
- Go to the bathroom often to empty your bladder. An empty bladder gives more room for your baby’s head to move down.
- If you feel like you want to push, tell your provider. You don’t want to start pushing until your provider checks your cervix to see how dilated it is.
Transition to the second stage of labor
This can be the toughest and most painful part of labor. It can last 15 minutes to an hour. During the transition:
- Contractions come closer together and can last 60 to 90 seconds. You may feel like you want to bear down.
- You may feel a lot of pressure in your lower back and rectum. If you feel like you want to push, tell your provider.
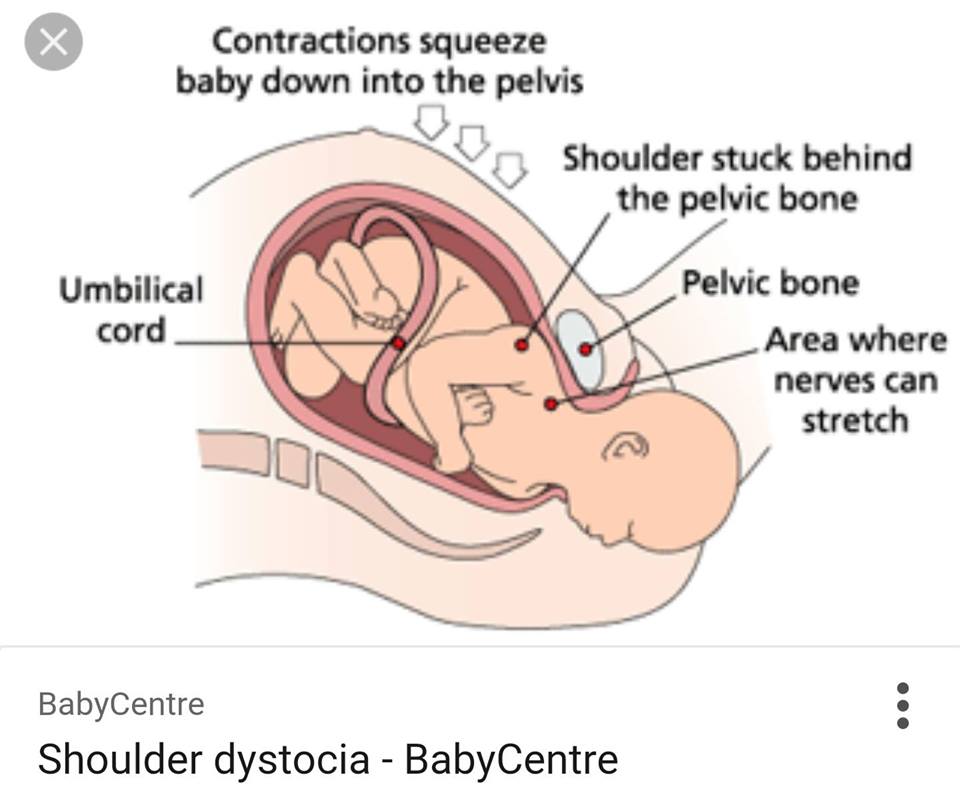
What happens in the second stage of labor?
In the second stage of labor, your cervix is fully dilated and ready for childbirth. This stage is the most work for you because your provider wants you to start pushing your baby out. This stage can be as short as 20 minutes or as long as a few hours. It may be longer for first-time moms or if you’ve had an epidural. And epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief used during labor. The second stage ends when your baby is born.
During the second stage of labor:
- Your contractions may slow down to come every 2 to 5 minutes apart. They last about 60 to 90 seconds.
- You may get an episiotomy. This is a small cut made at the opening of the vagina to help let the baby out. Most women don't need an episiotomy.
- Your baby’s head begins to show. This is called crowning.
- Your provider guides your baby out of the birth canal. She may use special tools, like forceps or suction, to help your baby out.
- Your baby is born, and the umbilical cord is cut. Instructions about who’s cutting the umbilical cord are in your birth plan.
What you can do:
- Find a position that is comfortable for you. You can squat, sit, kneel or lie back.
- Push during contractions and rest between them. Push when you feel the urge or when your provider tells you.
- If you’re uncomfortable or pushing has stopped, try a new position.
What happens in the third stage of labor?
In the third stage of labor, the placenta is delivered. The placenta grows in your uterus and supplies your baby with food and oxygen through the umbilical cord. This stage is the shortest and usually doesn’t take more than 20 minutes.
During the third stage of labor:
- You have contractions that are closer together and not as painful as earlier.
 These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth.
These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth. - You continue to have contractions even after the placenta is delivered. You may get medicine to help with contractions and to prevent heavy bleeding.
- Your provider squeezes and presses on your belly to make sure the uterus feels right.
- If you had an episiotomy, your provider repairs it now.
- If you’re storing your umbilical cord blood, your provider collects it now. Umbilical cord blood is blood left in the umbilical cord and placenta after your baby is born and the cord is cut. Some moms and families want to store or donate umbilical cord blood so it can be used later to treat certain diseases, like cancer. Your instructions about umbilical cord blood can be part of your birth plan.
- You may have chills or feel shaky. Tell your provider if these are making you uncomfortable.
What happens after your baby is born?
Congratulations! It’s time to hold your baby! Right after birth your provider places your baby skin-to-skin on your chest and covers him with a blanket.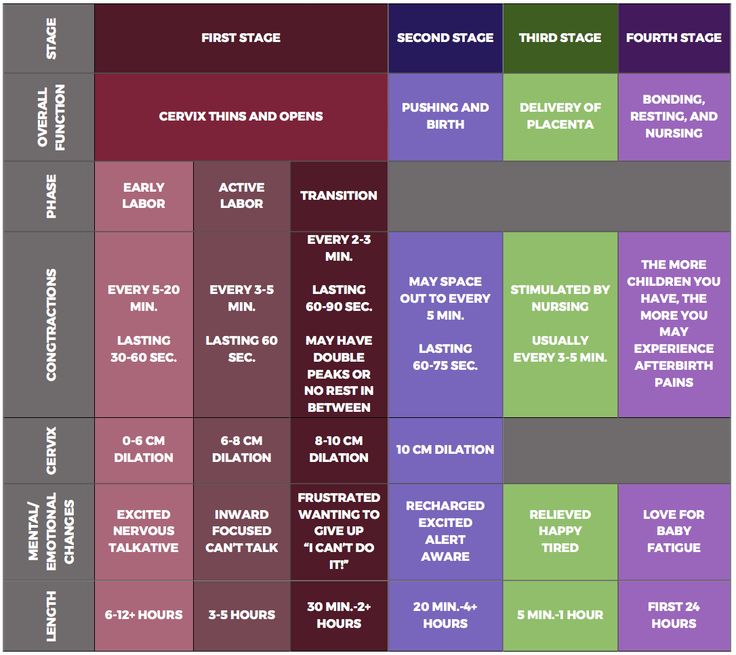 Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
After birth, your body starts to change to help you heal. Your provider takes your temperature and checks your heart and blood pressure to make sure you’re doing well. If you had anesthesia during labor, your provider makes sure you’re recovering without any complications.
Last reviewed: March, 2019
Second Stage of Labor - American Pregnancy Association
The second stage of labor is when your baby moves through the birth canal. The second stage of labor begins when the cervix is completely dilated (open), and ends with the birth of your baby. Contractions push the baby down the birth canal, and you may feel intense pressure, similar to an urge to have a bowel movement.
Contractions push the baby down the birth canal, and you may feel intense pressure, similar to an urge to have a bowel movement.
Your health care provider may ask you to push with each contraction. The contractions continue to be strong, but they may spread out a bit and give you time to rest. The length of the second stage depends on whether or not you’ve given birth before and how many times, and the position and size of the baby.
The intensity at the end of the first stage of labor will continue into this pushing phase. You may be irritable during a contraction and alternate between wanting to be touched and talked to, and wanting to be left alone. It isn’t unusual for a woman to grunt or moan when the contractions reach their peak.
Pushing and what to expect:
- The second stage can last from 20 minutes to 2 hours
- Contractions will last about 45-90 seconds at intervals of 3-5 minutes of rest in between
- You will have a strong natural urge to push
- You will feel strong pressure at your rectum
- You are likely to have a minor bowel or urination accident
- Your baby’s head will eventually crown (become visible)
- You will feel a burning, stinging sensation during crowning
- During crowning, you will be told by your health care provider to not push
Pushing and what to do:
- Get into a pushing position that uses gravity to your advantage
- Push when you feel the urge
- Relax your pelvic floor and anal area (Kegel exercises can help)
- Rest between contractions to help regain your strength
- Use a mirror to view your progress (this can be very encouraging!)
- Use all your energy to push
- Do not become discouraged if your baby’s head emerges and then slips back into the vagina (this process can take two steps forward and one step back)
Tips for the support person
- Help her to relax and be as comfortable as possible.
 Give her ice chips if available and provide physical support in her position
Give her ice chips if available and provide physical support in her position - Encourage, encourage, encourage!
- Help guide her through her contractions
- Give verbal encouragement by telling her how well she is doing
- Don’t be offended if she displays anger or becomes emotional
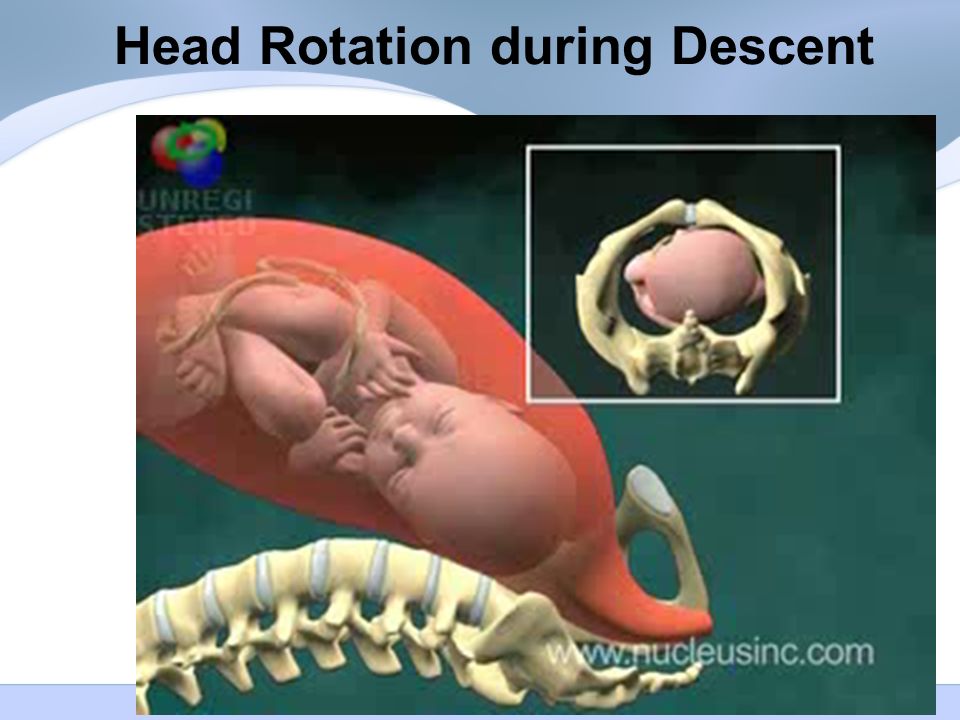
What your baby is doing during stage two:
While you are experiencing labor, your baby is taking certain steps to enter this world.
- Your baby’s head will turn to one side and the chin will automatically rest on the chest so that the back of the head can lead the way
- Once you are fully dilated, your baby’s head leads the way and the head and torso begin to turn to face your back as they enter your vagina
- Next, your baby’s head will begin to emerge or “crown” through the vaginal opening
- Once your baby’s head is out, the head and shoulders will again turn to face your side, allowing your baby to easily slip out
Delivery and what to expect:
Keep in mind that your baby has been soaking in a sac of amniotic fluid for nine months.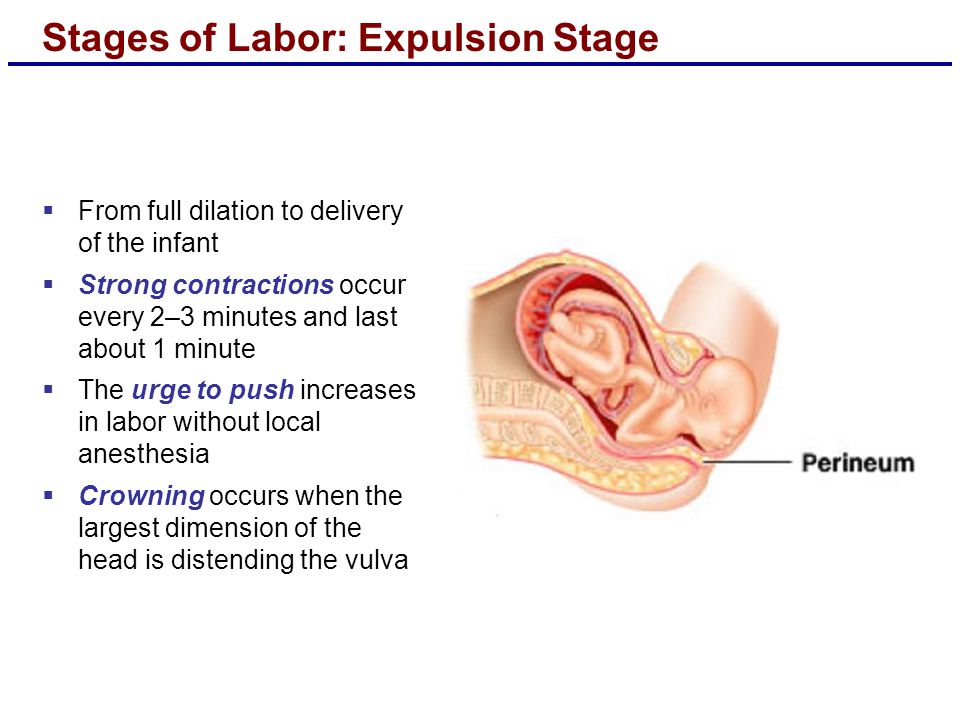 Here’s what happens once your baby hits the atmosphere:
Here’s what happens once your baby hits the atmosphere:
- He needs to be dried off with a towel and kept warm..
- Your doctor or midwife may quickly suction your baby’s mouth and nasal passages if she seems to have a lot of mucus.
- If there are no complications, he’ll be lifted onto your bare belly so you can touch, kiss, and simply marvel at him. The skin-to-skin contact will keep your baby nice and toasty, and he’ll be covered with a warm blanket – and perhaps given his first hat – to prevent heat loss.
- Your caregiver will clamp the umbilical cord in two places and then cut between the two clamps – or your partner can do the honors.
Following the contractions and passage through your very narrow birth canal, the baby will display the following characteristics:
- Cone-shaped head
- Vernix coating (a cheesy substance that coats the fetus in the uterus)
- Puffy eyes
- Lanugo (fine downy hair that covers the shoulders, back, forehead, and temple)
- Enlarged genitals
You may feel a wide range of emotions now: euphoria, awe, pride, disbelief, excitement (to name but a few), and, of course, intense relief that it’s all over. Exhausted as you may be, you’ll also probably feel a burst of energy, and any thoughts of sleep will vanish for the time being.
Exhausted as you may be, you’ll also probably feel a burst of energy, and any thoughts of sleep will vanish for the time being.
Want to Know More?
- First Stage of Labor
- What is an Epidural?
- Cord Blood Banking
Compiled using information from the following sources:
William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 17.
Pregnancy, Childbirth and the Newborn: The Complete Guide. Simkin, Penny, P.T., et al, Ch. 9.
 
Second stage of labor
Second stage of childbirth – period of exile. It begins after the full disclosure of the cervix and ends with the birth of the baby. Duration of the period of exile in primiparous is 1-2 hours , in multiparous - 15-30 minutes . Here, in addition to strong contractions, contractions of the muscles of the abdominal wall, diaphragm and pelvic floor are added, and a feeling of pressure on the rectum - this condition is called pushing.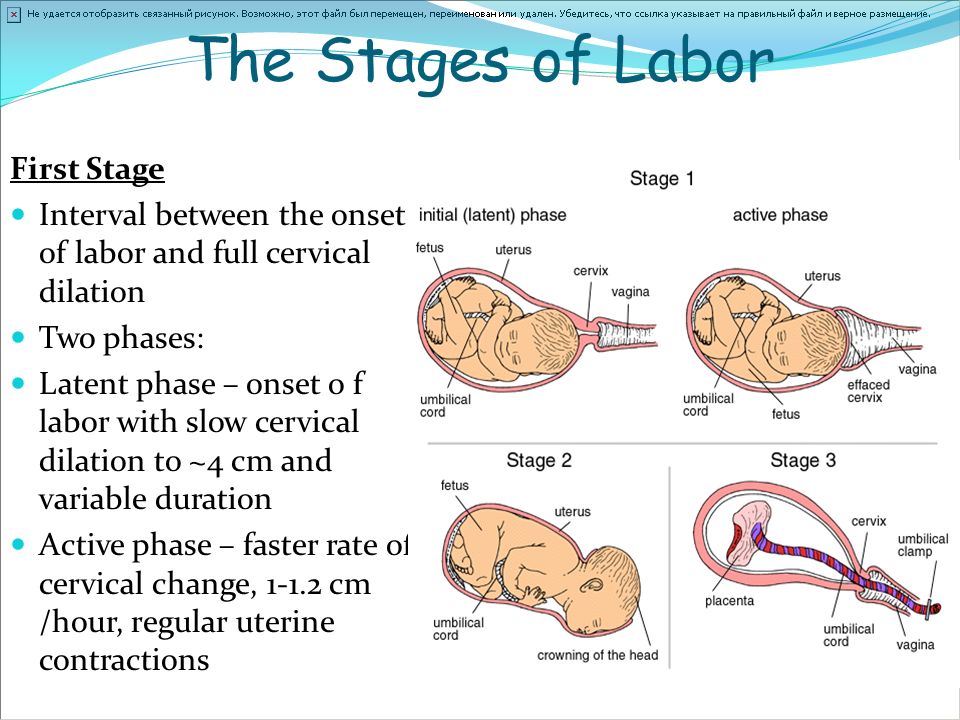
During the period of exile, the woman in labor is in the delivery room on a special bed, in a supine position with legs bent at the hip and knee joints. The head end of the bed is raised. In a semi-sitting position, the axis of the uterus and the axis of the small pelvis coincide, which improves the advancement of the head through the birth canal. At the moment of an attempt, in order to strengthen it, the woman in labor holds on to the bed with her hands, and rests her feet on the stand. It is necessary to prepare a sterile package for the initial treatment of the newborn and a set of sterile linen - a blanket and 3 diapers heated to 40 * C. Treat the pubis, inner thighs, external genitalia, perineum.
The average duration of each push is 10-15 seconds. Usually, during one contraction, a woman feels the need to push on average three times . And although at this point the contractions are the strongest, most women say that when attempts were added to the contractions, they became less painful.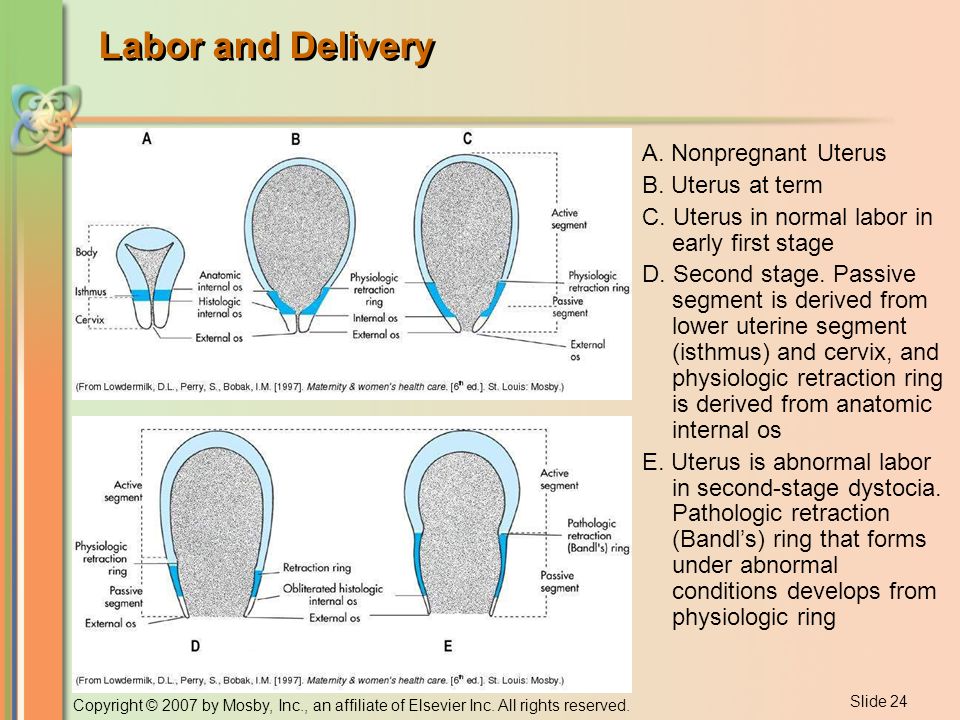 Attempts, unlike contractions, can be controlled - a woman can delay attempts or, conversely, intensify. If the doctor or midwife still forbids pushing, then the “dog-like” breathing technique will help to restrain the attempts. Usually the midwife says: “Don’t push, try to breathe!” Then you need to breathe superficially with short inhalations and exhalations.
Attempts, unlike contractions, can be controlled - a woman can delay attempts or, conversely, intensify. If the doctor or midwife still forbids pushing, then the “dog-like” breathing technique will help to restrain the attempts. Usually the midwife says: “Don’t push, try to breathe!” Then you need to breathe superficially with short inhalations and exhalations.
How to push correctly? With the onset of attempts, you should always listen to the doctor or midwife. If the midwife says: “Push!”, you need:
- At the moment when it is time to push, the woman in labor should take full lungs of air, taking a breath through her mouth and hold her breath, as before immersion in water, while the shoulders should be lowered down . You need to exhale very smoothly through a slightly open mouth. So you need to act until the end of the attempt. The most important thing is the movement of attempts and all the efforts of a woman should be directed to the perineum.

- During each contraction, you need to push three times.
3. You need to push smoothly, and between attempts - to rest and set yourself up for work.
Attempts are the main moment of childbirth the outcome of childbirth and the condition of the child depend on them. Therefore, even if the forces are no longer there, you need to gather your will into a fist and start pushing. Between contractions, it is very important to take deep, calm breaths. This will allow you to gain strength before the next fight and effectively carry out another attempt. In between attempts, the doctor will listen to the baby's heartbeat with a CTG sensor or an obstetric stethoscope. Pushing is hard and painful, but it is very important for the baby: at this moment it is also difficult for him, and only mother can help.
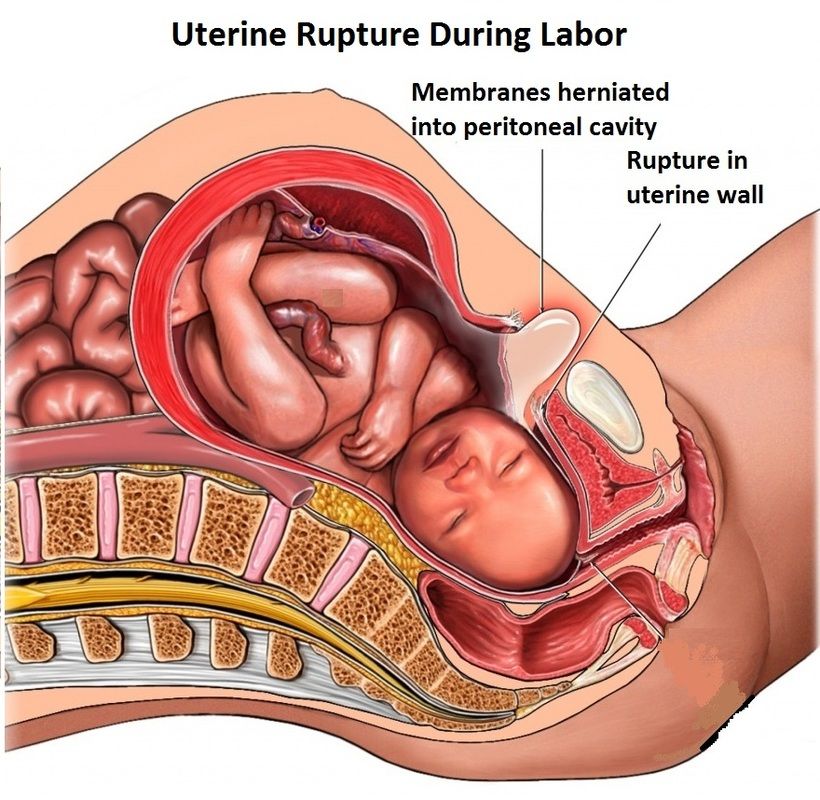
If there is a possibility of perineal rupture during attempts, the doctor makes an incision in it - an episiotomy. As soon as the fetal head stops hiding in the pelvis, the midwife removes the newborn baby into the light.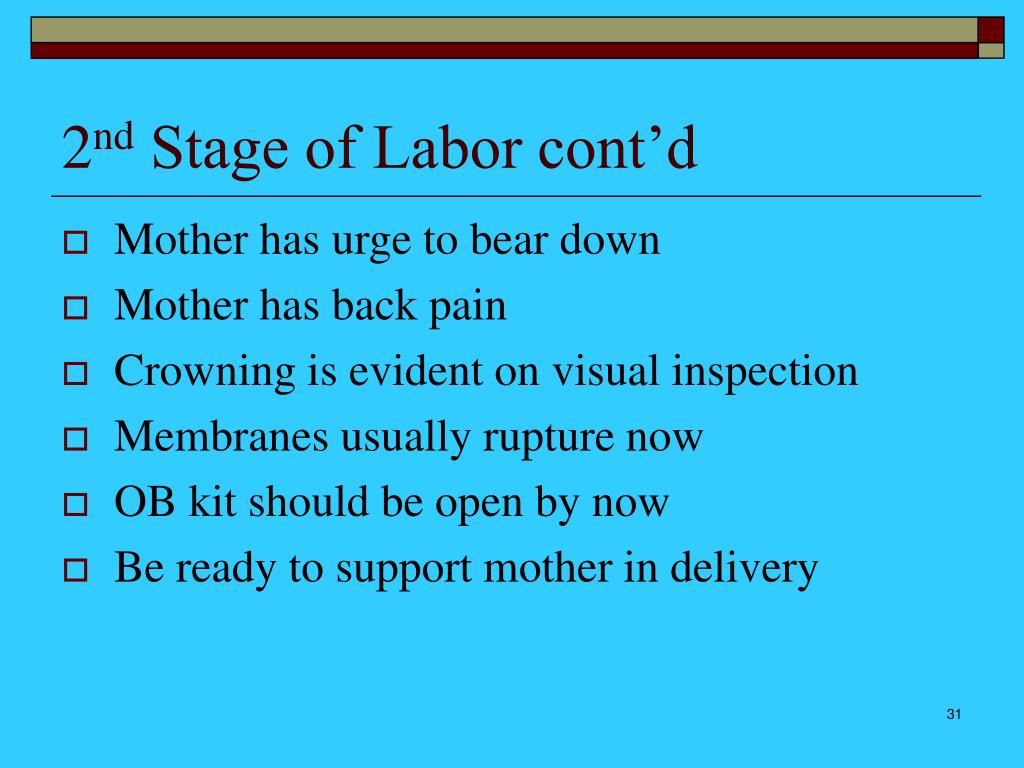
Immediately after the head appears, it clears the child's airways and he screams for the first time. The baby is laid out on the mother's stomach, the baby takes its first breath and illuminates the delivery room with a long-awaited cry. At the same time, the midwife dries the baby's wet skin with a warm diaper, then the umbilical cord is cut, and the pediatrician assesses the baby's condition on the Apgar scale. The baby is handed over to the mother and applied to the breast. So he warms up and adapts to the situation, and in the mother's body, the production of oxytocin begins, which starts the process of milk production and causes postpartum uterine contractions. It is in skin-to-skin contact with his mother that his acquaintance with the world begins. At this time, an invisible psycho-emotional connection arises between mother and child, which in the future will become the basis for the formation of attachment between them. The first 20 minutes after birth is a period of relaxation for the baby.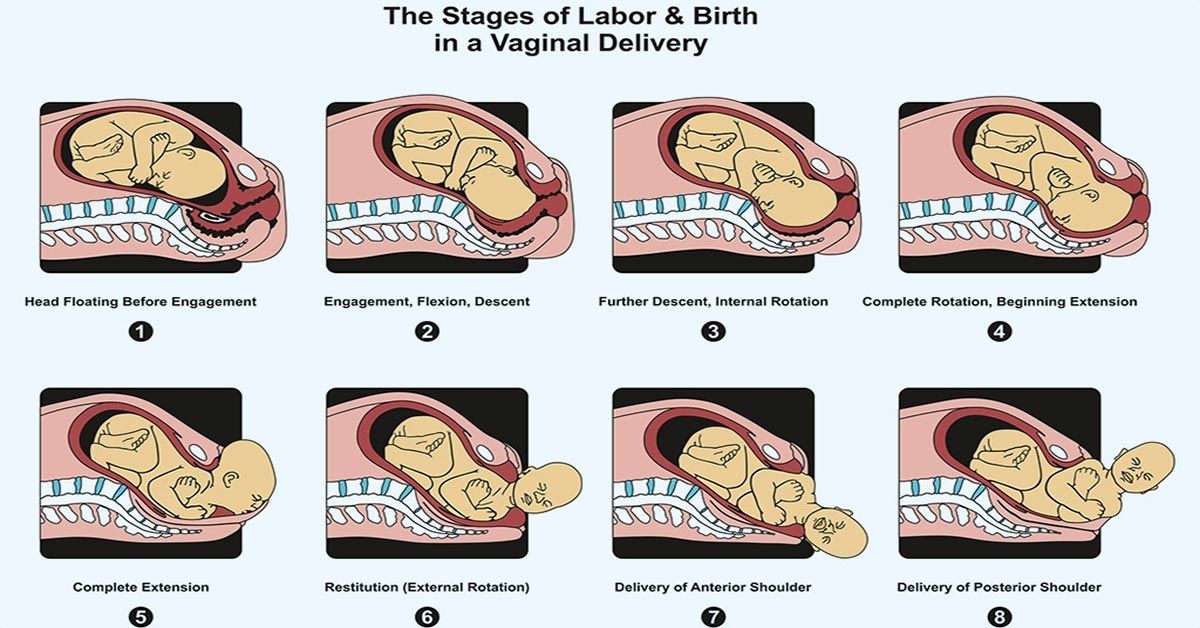 During this period, he recuperates after hard work. After 20 minutes, the next phase begins - awakening. The baby begins to move, turns his head, opens his fists and makes attempts to crawl. With the beginning of motor activity, the first feeling of hunger comes to the baby. It is very important that the child finds and takes the breast at the moment of the search reflex. The baby begins to open his mouth, clenching and unclenching his palms, then he begins to crawl, raising his head and pushing off with his legs and elbows, towards his mother's chest.
During this period, he recuperates after hard work. After 20 minutes, the next phase begins - awakening. The baby begins to move, turns his head, opens his fists and makes attempts to crawl. With the beginning of motor activity, the first feeling of hunger comes to the baby. It is very important that the child finds and takes the breast at the moment of the search reflex. The baby begins to open his mouth, clenching and unclenching his palms, then he begins to crawl, raising his head and pushing off with his legs and elbows, towards his mother's chest.
In the second stage of labor - attempts and expulsion of the fetus, the partner's role is moral support : a woman in labor can simply be held by the hand, wipe sweat from her forehead and help to breathe correctly (at the doctor's command).
For the father of a child, partner delivery is an opportunity to help the beloved woman during childbirth, to see how the child is born and to take him in his arms. In this way, inextricable bonds are formed between all family members.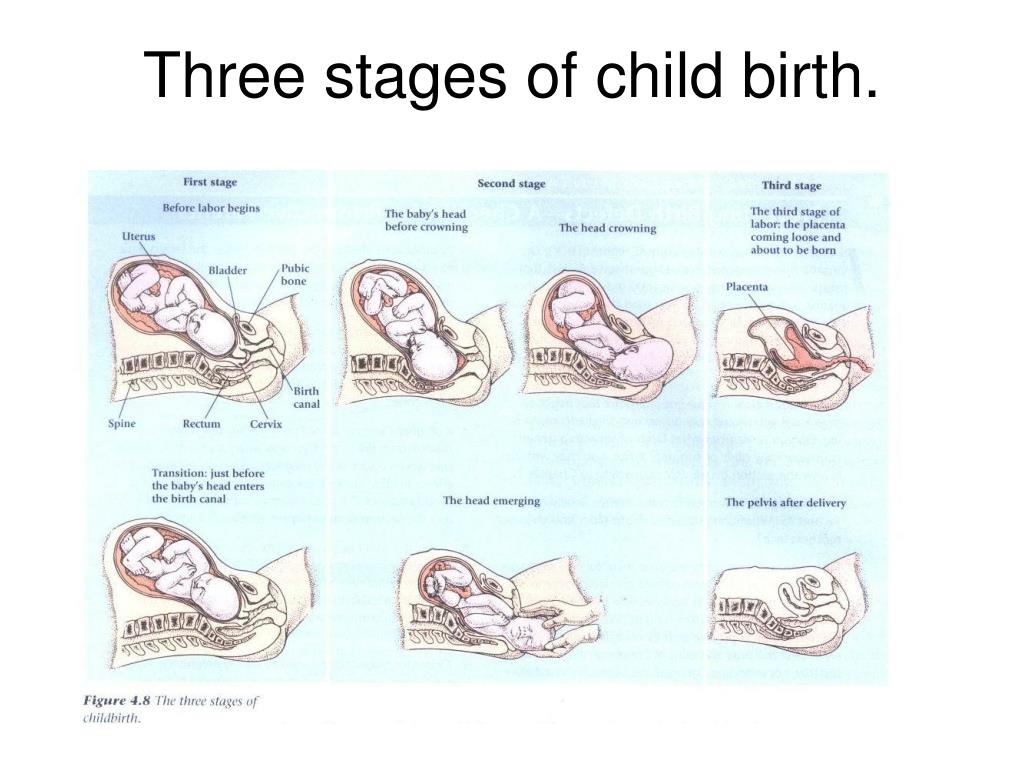
Methods of pushing in the second stage of labor
What is the problem?
During the second stage of labor, a common method is to ask the woman to take a deep breath at the beginning of the contraction and then hold it while pushing throughout the contraction (known as "directed pushing"). In spontaneous pushing, women follow their own instincts and typically push three to five times per contraction. Prolonged attempts are expressed in the fact that the woman is instructed not to push until an unbearable urge appears, or until the presenting part of the fetus descends to the perineum.
Why is this important?
We need to know the advantages and possible disadvantages of different types of maternal push/rest technique for exile pushing in terms of maternal and fetal outcomes.
What evidence did we find?
We searched for evidence (September 19, 2016) and found eight trials (884 women) comparing different types of pushing: spontaneous versus directed pushing with or without epidural anesthesia, and 13 trials (2879women), which compared the timing of pushing: delayed pushing and immediate pushing with epidural anesthesia.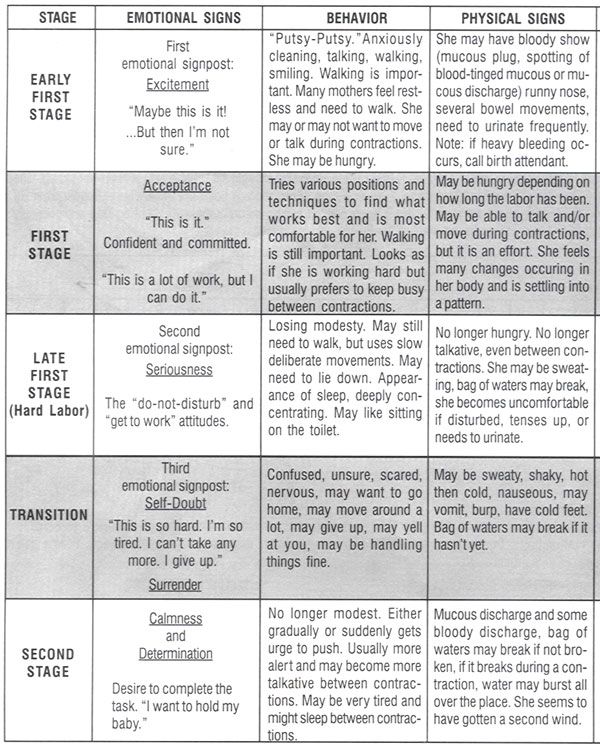 The quality of the evidence in this updated review ranged from moderate to very low.
The quality of the evidence in this updated review ranged from moderate to very low.
Comparison 1: Spontaneous vs. Directed Stretching
A clear difference in the length of the second period ( very low quality evidence ), perineal tears ( low quality evidence ), episiotomy time spent pushing ( very low-quality evidence ) or among women with spontaneous vaginal delivery ( moderate-quality evidence ) there was no difference between spontaneous and directed labor. Outcomes for the child (eg, Apgar score less than seven at five minutes ( very low quality evidence ), admission to the neonatal intensive care unit ( very low quality evidence )) were not clearly different. None of the studies reported on outcomes in children with hypoxic-ischemic encephalopathy.
Comparison 2: Delayed versus Immediate Pushing (with Epidural)
With respect to the timing of pushing: prolonged versus immediate pushing (in all women with epidural anesthesia) - prolonged pushing caused an increase in the duration of the second stage of labor by about 56 minutes ( evidence very low quality ).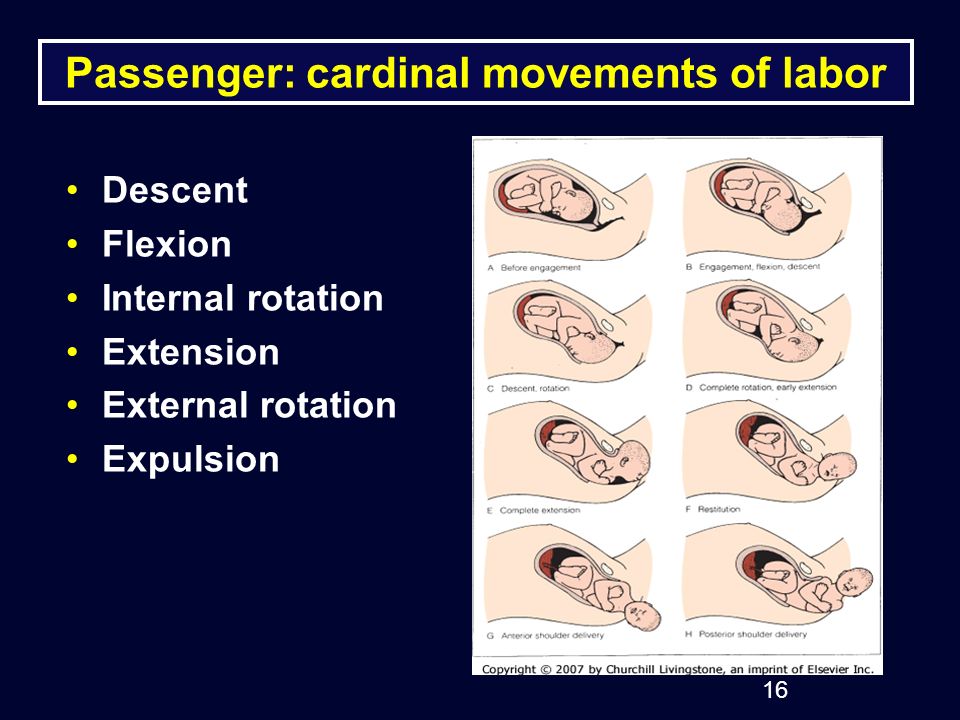 There were no clear differences between the two groups of women in the number of episodes of perineal tear ( moderate quality evidence ) and episiotomy. Delayed pushing reduced the length of the pushing period by about 19 minutes ( very low quality evidence ) and slightly increased the number of women with spontaneous vaginal delivery ( moderate quality evidence ). There was no clear difference between delayed pushing and immediate pushing in terms of outcomes important to the child: five-minute Apgar scores of less than seven (90,081 very low-quality evidence ), admissions to the neonatal intensive care unit ( low-quality evidence ). None of the studies reported on outcomes in children with hypoxic brain injury. In addition, delayed pushing was associated with an increase in cases of low cord pH and an increase in the cost of care during childbirth by CAD 68.22.
There were no clear differences between the two groups of women in the number of episodes of perineal tear ( moderate quality evidence ) and episiotomy. Delayed pushing reduced the length of the pushing period by about 19 minutes ( very low quality evidence ) and slightly increased the number of women with spontaneous vaginal delivery ( moderate quality evidence ). There was no clear difference between delayed pushing and immediate pushing in terms of outcomes important to the child: five-minute Apgar scores of less than seven (90,081 very low-quality evidence ), admissions to the neonatal intensive care unit ( low-quality evidence ). None of the studies reported on outcomes in children with hypoxic brain injury. In addition, delayed pushing was associated with an increase in cases of low cord pH and an increase in the cost of care during childbirth by CAD 68.22.
What does this mean?
We cannot say which method is better - spontaneous pushing or directed pushing under the guidance of an instructor. Until further high quality research is available, women should be encouraged to push and rest according to their comfort and preference.
Until further high quality research is available, women should be encouraged to push and rest according to their comfort and preference.
Delayed pushing in women under epidural anesthesia reduces the time spent pushing during labor and increases the likelihood of spontaneous vaginal delivery. However, this increases the duration of the second period. The possible impact on important neonatal outcomes and maternal perineal trauma (serious tears) has not yet been elucidated. Thus, the evidence in favor of certain terms and types of attempts is insufficient and inconclusive, which does not allow choosing the best options for use in clinical practice.
Further randomized controlled trials with proper design are needed to obtain more evidence. These trials should focus on clinically relevant maternal and neonatal outcomes and will provide more complete data that will be included in future updates to this review.
Translation notes:
Translation: Kurbatova Olga Gennadievna.