Baby lethargic fever
Babies' Warning Signs
It's been said that babies do not come with instructions, but most parents certainly wish they did, especially when a young child is sick. As they grow, babies are exposed to infectious agents that may cause colds and other illnesses. These are a normal part of a baby's development and, thankfully, most outgrow the frequent-illness stage. Because babies cannot verbalize their feelings, however, adults must always stay alert for warning signs of illness.
A change in behavior may be one of the first signs that your baby isn’t feeling well. Although your baby's activity level, appetite, and cries will vary from day to day, even hour to hour, a distinct change in any of these areas may signal illness.
Generally, if your baby is alert and active when awake, is feeding well, and can be comforted when crying, occasional differences in these areas are normal. Talk with your baby's doctor if you’re concerned about your infant’s behavior, since changes may indicate an illness. The warning signs below will help you discern when something is amiss, and will help you know when and how to take action.
Persistent Crying or Irritability
All babies cry—this is their only way of communicating their needs to you. Depending on the type of cry, your baby may be hungry, sleepy, lonely, in need of a diaper change, or in pain. At first, you may not know how to interpret your baby’s cries, but appeasing one of these issues should usually calm your infant. If your baby is continuously fretful and fussy, cries for long periods or very suddenly, or has a cry that sounds unusual, it may be a sign of illness. Colic could also be causing your baby to cry. Colic is a benign, painful intestinal problem in infants up to 3 months old, and may cause intense crying and irritability around the same time every day.
If you notice any of these signs, examine your baby carefully to make sure there isn’t a physical problem—such as clothing that pinches, or an open, pointy diaper pin. There may be a thread or even a hair tightly wound around your baby’s finger or toe. Also, look at your infant’s abdomen for signs of swelling. Call your baby's doctor if crying lasts longer than usual or your baby has other signs of illness.
There may be a thread or even a hair tightly wound around your baby’s finger or toe. Also, look at your infant’s abdomen for signs of swelling. Call your baby's doctor if crying lasts longer than usual or your baby has other signs of illness.
Fever
Respiratory illnesses such as colds, croup, pneumonia, ear infections, stomach bugs, urine infections, and many other bacterial and viral illnesses may all cause fever. To check for fever, take your baby's temperature rectally with a digital or glass rectal thermometer that’s mercury-free. It is the easiest and most accurate way. A 100-degree temperature or lower is considered normal, but if your baby is 3 months or younger with a temperature of 100.4 degrees or higher, call the doctor immediately. If your baby is 3 to 6 months old, call the doctor if your baby’s temperature exceeds 101 degrees. If your child is over a year old, call the doctor if the fever lasts longer than 24 to 48 hours (or if it’s accompanied by any other worrisome symptoms).
Fever in children between 6 months and 5 years of age can trigger febrile seizures (convulsions), which may last for a few minutes or may be over in seconds. They are a frightening experience but are usually harmless. Let your child's doctor know if this happens. Call for emergency help if seizures are severe, cause difficulty breathing, or last longer than a few minutes. If your child has had an uncomplicated seizure, he or she should be seen by a physician during regular office hours or in an emergency room, if you are unable to get an appointment.
Listlessness or Lethargy
You may find that your baby seems to have little or no energy, is drowsy or sluggish, or is sleeping longer than usual. He or she may be hard to wake for feedings, and won’t be alert or attentive to sounds and visual stimulation. Sometimes this develops slowly, so you won’t notice the gradual change. Lethargy may be a sign of infection or other conditions such as low blood sugar. Talk with your baby's doctor if your infant becomes lethargic or isn’t as active.
Poor Appetite
After the first day or so, most newborns are ready to eat every three to four hours and show signs of hunger by sucking on fingers or a hand, crying, and making rooting motions. If your baby refuses to eat and misses several feedings, it may be a sign of illness. You may notice that your infant is having trouble sucking at your breast or bottle, doesn’t seem to be hungry, is having problems spitting up, or is losing weight.
If a sucking problem is to blame, you’ll notice that your baby’s once strong sucking has become weaker, and that he or she isn’t eating well. This is especially common if your baby was born prematurely. If your infant has a weak suck, he or she may not pull strongly or have a good latch while breastfeeding. What’s more, you may not hear your baby swallowing or gulping during feedings, or your breasts may not feel full right before a feeding or softer afterward. If your baby is bottle-fed, a weak suck may require the bottle nipple to be "worked" or pumped to stimulate a suck. Either type of feeding, whether by breast or bottle, may take a very long time—often longer than 45 minutes.
Either type of feeding, whether by breast or bottle, may take a very long time—often longer than 45 minutes.
Spitting up and dribbling milk with burps or after feedings is fairly common in newborns. This is because the sphincter muscle between the stomach and the esophagus (the tube from the mouth to stomach) is weak and immature. However, forceful or projectile vomiting, or spitting up large amounts of milk after most feedings, can indicate a problem. If your baby is formula-fed, vomiting may occur after overfeeding or because of intolerance to formula. If your baby is breastfed or formula-fed, he or she may have a physical condition that prevents normal digestion and may cause vomiting. Discolored or green-tinged vomit may mean that your infant has an intestinal obstruction.
It’s normal for your baby to lose about 10 percent of his or her birth weight in the first two to three days after birth. However, your baby should gain back this weight after 10 or 11 days. Signs your baby isn’t gaining weight may include a thin, drawn face, loose skin, and a decreased number of wet or soiled diapers. Most physicians want to see a newborn in the office at the end of the first week to check his or her weight. Lack of weight gain or continued weight loss in your baby may be a sign of illness or other conditions and needs to be treated. Talk with your baby’s doctor if your infant has any difficulties taking or digesting feedings, as serious illness could occur if left untreated.
Most physicians want to see a newborn in the office at the end of the first week to check his or her weight. Lack of weight gain or continued weight loss in your baby may be a sign of illness or other conditions and needs to be treated. Talk with your baby’s doctor if your infant has any difficulties taking or digesting feedings, as serious illness could occur if left untreated.
Umbilical Cord Infection
If there is puss or red skin around the stump of your newborn's umbilical cord or an unpleasant smell, it may be infected. Discuss it with your baby’s doctor.
Diarrhea and/or Vomiting
These could signal a viral or bacterial infection of the intestine, an obstruction, or other problem. In some cases, your baby’s doctor may exam your baby's stool for bacteria, which requires treatment. Viral causes don’t require treatment and will resolve on their own in a week or so. If your baby has persistent diarrhea, this may lead to dehydration.
Irregular Stools
If your baby is breast- or bottle-fed and has very hard or very dry stools, it may be a sign that he or she needs more fluids, or may be losing too much fluid because of fever, illness, or heat. After your baby starts eating solid foods, hard stools may be caused by too many constipating foods, such as cereal or cow's milk, before your baby’s system can handle them.
After your baby starts eating solid foods, hard stools may be caused by too many constipating foods, such as cereal or cow's milk, before your baby’s system can handle them.
Urination
Your baby should wet at least four diapers a day. If he or she shows any signs of distress while urinating, it could be a sign of infection or some other problem in the urinary tract. A salmon-colored or pinkish stain on your baby’s diaper is typically a sign of highly concentrated urine and isn’t usually a cause for concern. However, if staining persists, talk with your baby’s doctor. If there is blood in the urine or a bloody spot on a diaper, call the doctor at once. If bleeding is accompanied by abdominal pain or fever, seek medical attention immediately.
Intussusception
This rare intestinal blockage is a medical emergency that must be treated immediately. If your baby has a sudden onset of severe pain similar to severe colic with hard, distressed crying, this could be a sign of intussusception. Early on, your baby may seem fine between bouts of pain, but he or she will soon become fatigued and sluggish. Your baby may vomit and may pass bloody stool (sometimes described as "currant jelly" stool). Fever (often not present initially) may also appear, and shock may follow.
Early on, your baby may seem fine between bouts of pain, but he or she will soon become fatigued and sluggish. Your baby may vomit and may pass bloody stool (sometimes described as "currant jelly" stool). Fever (often not present initially) may also appear, and shock may follow.
What to Do
To keep your baby as healthy as possible, breastfeed your child if possible, which will provide him or her with antibodies and enzymes that help protect against illness. If breastfeeding isn’t an option, use a commercial infant formula such as Similac or Enfamil. Don't allow smoking around your baby. Also, be sure to adhere to your baby's vaccine schedule and regular checkups. In general, call your baby’s doctor if your infant seems especially sluggish, is refusing food or drink, is vomiting (not just spitting-up), has diarrhea, or has a fever. Remember, if you’re worried, there’s probably a good reason even if you don’t recognize it, so don’t hesitate to call your baby’s doctor.
Self-Care Steps for Baby/Warning Signs
• If your baby seems distressed, hold and console him or her as much as possible.
• Keep your infant away from children who are sick, especially those with infectious diseases such as respiratory syncytial virus (RSV), stomach “flu,” influenza and other respiratory infections, cold sores (HSV1) and other obvious infectious diseases.
• Prevent family members who are sick from sharing food or drink with your baby, and from handling your baby and his or her toys.
Emergency Symptoms Not to Miss
Most life-threatening emergencies are easy to recognize. You would not overlook major bleeding, breathing that stops, a seizure or a coma. You would call 911 for help.
- If you suspected poisoning, you would call the Poison Helpline at 1-800-222-1222.
- Some emergency symptoms, however, can be missed or ignored. Here's that important list.
- If your child has any of these symptoms, call your child's doctor now. If you can't reach them, go to the nearest ER. For a few of these symptoms, call 911.
Sick Newborn
- Your baby is less than 1 month old and has a fever or looks sick.
 This includes vomiting, cough, or even poor color. Your baby may start to act abnormal if they are getting sick. Examples are poor feeding or sleeping too much. At this age, these symptoms are serious until proven otherwise. During the first month of life, infections can progress very fast.
This includes vomiting, cough, or even poor color. Your baby may start to act abnormal if they are getting sick. Examples are poor feeding or sleeping too much. At this age, these symptoms are serious until proven otherwise. During the first month of life, infections can progress very fast.
Lethargy
- Your young child is lethargic if she stares into space or won't smile. She won't play at all or hardly responds to you. Your child is too weak to cry or hard to wake up. These are serious symptoms.
- Note: Sleeping more when sick is normal. When awake, your child should be alert.
Confusion
- The sudden onset of confusion is serious. Your child is awake but says strange things. She sees things that aren't there. She doesn't recognize you.
- Note: Brief confusion for 5 minutes or so can be seen with high fevers. This can be normal. But, if not brief, confusion can have some serious causes.
Severe Pain
- Severe pain keeps your child from doing all normal activities.
 Your child won't play or even watch a favorite TV show. They just want to be left alone. Your child may cry when you try to hold or move them. Children with severe pain also can't sleep or can only fall asleep briefly.
Your child won't play or even watch a favorite TV show. They just want to be left alone. Your child may cry when you try to hold or move them. Children with severe pain also can't sleep or can only fall asleep briefly.
Inconsolable Crying
- Constant nonstop crying is caused by severe pain until proven otherwise. Suspect this in children who can't sleep or can only fall asleep briefly. When awake, they will not join in any normal activities. They won't play or be distracted. They may be very hard to console. Caution: Instead of crying, severe pain may cause your child to moan or whimper.
Can't Walk
- If your child has learned to walk and then suddenly won't, call your doctor. He may have a serious injury to the legs or a problem with balance. If your child walks bent over holding his stomach, he may have appendicitis.
Vomits Bile
- Vomiting that is bright green is most often bile. Unless your child drank a green liquid, this is not normal.
 It can mean the intestines are blocked up. This is a surgical emergency.
It can mean the intestines are blocked up. This is a surgical emergency. - Note: Vomiting some yellow fluid is normal. The yellow color is from stomach acid.
Tender Belly
- Press on your child's belly while she is distracted by a toy or book. You should be able to press in an inch or so without a problem. If your child winces or screams, it suggests a serious cause. If the belly is also bloated and hard, it's more urgent.
- Note: If your child just pushes your hand away, you haven't distracted her enough.
Pain in Testicle or Scrotum
- Sudden pain in the scrotum can be from twisting (torsion) of the testicle. This needs surgery within 8 hours to save the testicle.
Trouble Breathing
- Breathing is essential for life. Most childhood deaths are caused by severe breathing problems. Breathing problems can be caused by throat or lung infections. Parents need to learn to recognize trouble breathing. If your child has tight croup or wheezing, they need to be seen now.
 Other bad signs are fast breathing, grunting with each breath, bluish lips, or retractions. This means the skin pulls in between the ribs with each breath. It is a sign of trouble breathing in younger children. Children with severe breathing problems can't drink, talk or cry. If your child is struggling to breathe, call 911.
Other bad signs are fast breathing, grunting with each breath, bluish lips, or retractions. This means the skin pulls in between the ribs with each breath. It is a sign of trouble breathing in younger children. Children with severe breathing problems can't drink, talk or cry. If your child is struggling to breathe, call 911.
Bluish or Gray Lips
- Bluish lips, tongue, or gums can mean not enough oxygen in the bloodstream. Call 911.
- Note: Bluish skin only around the mouth (not the lips) can be normal. It can be caused by being cold or being afraid.
Trouble Swallowing with Drooling
- The sudden onset of drooling or spitting means your child is having trouble swallowing. Most often, this is from severe swelling in the throat. The cause can be a serious throat infection. A serious allergic reaction can also cause trouble swallowing. Swelling in the throat could close off the airway.
Dehydration
- Dehydration means that your child's body fluids are low.
 Dehydration often is caused by severe vomiting and/or diarrhea. Suspect dehydration if your child has not urinated in 8 hours. Crying no tears and a dry inside of the mouth (tongue) are also signs. In young babies, the soft spot in the head is sunken. Dehydrated children are also tired and weak.
Dehydration often is caused by severe vomiting and/or diarrhea. Suspect dehydration if your child has not urinated in 8 hours. Crying no tears and a dry inside of the mouth (tongue) are also signs. In young babies, the soft spot in the head is sunken. Dehydrated children are also tired and weak. - Note: If your child is alert, playful and active, he is not yet dehydrated. Children with severe dehydration become dizzy when they stand. Dehydration needs extra fluids by mouth or vein.
Bulging Soft Spot
- The soft spot in your baby's head is tense and bulging. This means the brain is under pressure.
Stiff Neck
- A stiff neck means your child can't touch the chin to the chest. To test for a stiff neck, lay your child down. Then lift his head until the chin touches the chest. If he fights you, place a toy or coin on the belly. This makes him have to look down to see it. Older children can simply be asked to look at their belly button. A stiff neck can be an early sign of meningitis.

- Note: Without fever, a stiff neck is often from sore neck muscles.
Neck Injury
- Talk to your child's doctor about any neck injury, regardless of the symptoms. Neck injuries carry a risk of damage to the spinal cord.
Purple or Blood-Red Spots or Dots
- Purple or blood-red spots or dots on the skin need to be seen. When present with fever, they could be a sign of a serious bloodstream infection. The color of these serious rashes will not change when you press on them. The color of normal viral rashes will fade with skin pressure.
- Note: Bumps and bruises on the shins from active play are different.
Fever (over 100.4°F or 38 °C) in the First 3 Months
- Fevers in newborns and young babies are treated differently than fevers in older children. Bacterial infections are more common at this age and can get worse quickly. A fever is a rectal or forehead temp of 100.4 F° (38.0° C) or higher. All babies under 3 months of age with a fever need to be seen now.
 They need tests to decide if the cause is viral or bacterial.
They need tests to decide if the cause is viral or bacterial.
Fever over 105° F (40.6° C)
- A fever tells you that your child has an infection. Serious infections can occur with low-grade fevers as well as higher fevers. All the above symptoms are stronger signs of serious illness than the level of fever. Research shows fevers alone are a risk factor only when very high. That means levels above 105°F (40.6°C). So, call your doctor if your child's fever goes above 104° F (40° C). This is a safe rule.
Chronic Diseases
- Most active chronic diseases can have some serious complications. If your child has a chronic disease, learn what those complications are. Find out how to recognize the early changes. Diseases at highest risk for serious infections are those that weaken the immune system. These include sickle cell disease, HIV, cancer, organ transplant, or taking oral steroids. If you are talking with health workers who don't know your child, speak up.
 Always tell them about your child's chronic disease (such as asthma). Never assume the doctors and nurses already know this.
Always tell them about your child's chronic disease (such as asthma). Never assume the doctors and nurses already know this.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Last Reviewed: 12/14/2022
Last Revised: 01/13/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Children from 0 to 5 years old. When should you urgently take your child to the doctor?
We are all very worried when a child gets sick; including the fear that he will certainly be sent to the hospital. And the children's hospital, as you know, is like this: you get in with one, you leave with another. That is why mothers often refuse hospitalization or postpone a visit to the doctor, hoping that the disease will recede on its own, others prefer online consultations on forums and advice from grandmothers and girlfriends.
And the children's hospital, as you know, is like this: you get in with one, you leave with another. That is why mothers often refuse hospitalization or postpone a visit to the doctor, hoping that the disease will recede on its own, others prefer online consultations on forums and advice from grandmothers and girlfriends.
Fortunately for all mothers, in most cases, modern medicine makes it possible to diagnose and provide the necessary assistance very quickly, resorting to hospitalization only as a last resort. Something like in the famous series with Hugh Laurie - and MRI, and all the necessary tests, and CT scans, and, most importantly, competent pediatricians and highly specialized specialists. Unfortunately, not all polyclinics have such a set, but in one place in Moscow they definitely have it - in the department of emergency pediatrics of the Federal State Autonomous Institution "NMIC for Children's Health" of the Ministry of Health of Russia, where doctors usually need no more than 2 hours to establish an accurate diagnosis, taking all the necessary analyzes and quickly receive their results, stabilize the child and send him home if there is no threat to life and indications for emergency hospitalization.
If you understand that your child needs a prompt consultation with a specialist, but for some reason you postpone the visit to the doctor, if you are afraid that the child will be immediately sent to the hospital ward “to clarify the diagnosis”, or he will not be given due Attention, just come to the pediatric emergency department of the Federal State Autonomous Institution "NMIC of Children's Health" of the Ministry of Health of Russia. Here they immediately do all the necessary research and provide the child with assistance as efficiently and quickly as possible. Every year, more than 3,000 children receive care in the department, and only 2% of them are hospitalized by doctors in a round-the-clock hospital. The rest are sent home after all the necessary procedures with appropriate recommendations, or will be observed for several days in a day hospital. The department accepts children without an appointment, works on CHI, VHI and on a commercial basis.
If your child is between 0 and 5 years old, do not neglect visits to the doctor because your child is at risk. It is this age that accounts for most of the serious diseases that are well studied by medicine, are well treated, but require prompt medical intervention. Tatyana Vladimirovna Kulichenko, Head of the Department of Emergency Pediatrics, FGAU "NMIC of Children's Health" of the Ministry of Health of Russia, Doctor of Medical Sciences, pediatrician of the highest category, WHO expert, spoke about the cases in which it is worth immediately contacting specialists for young children (we are talking about children first 5 years of life).
It is this age that accounts for most of the serious diseases that are well studied by medicine, are well treated, but require prompt medical intervention. Tatyana Vladimirovna Kulichenko, Head of the Department of Emergency Pediatrics, FGAU "NMIC of Children's Health" of the Ministry of Health of Russia, Doctor of Medical Sciences, pediatrician of the highest category, WHO expert, spoke about the cases in which it is worth immediately contacting specialists for young children (we are talking about children first 5 years of life).
High temperature (fever)
First, it is important to define what a fever is from a doctor's point of view. Fever is an increase in body temperature greater than 38°C if measured rectally (preferred as this is the most reliable way to determine body temperature in any person) and greater than 37.5°C if measured axillary depression.
Not every fever is a very bad sign, but with children under three years old it is better to play it safe and see a doctor as soon as possible. There are no legislative "terms of patience"; there is no need to wait three days, as pediatricians usually say: all the most severe infections develop very quickly and can be threatening from the first hours of the illness. The sooner you contact a specialist, the better. Examination of the child, instrumental and laboratory studies will help to understand the cause of the fever and quickly stabilize the child's condition.
There are no legislative "terms of patience"; there is no need to wait three days, as pediatricians usually say: all the most severe infections develop very quickly and can be threatening from the first hours of the illness. The sooner you contact a specialist, the better. Examination of the child, instrumental and laboratory studies will help to understand the cause of the fever and quickly stabilize the child's condition.
If just a high temperature seems to you not enough reason to see a doctor, then pay attention to the symptoms of intoxication:
- The child refuses to drink (not to eat, namely to drink).
- There is lethargy and drowsiness, it is difficult to establish eye contact with the child (some pediatricians say about such patients "the child looks into himself").
If a child develops a rash on the skin along with an increase in body temperature, then you should go to the doctor immediately.
Cough
Cough is a fairly common symptom in children. Precisely because it seems to be a common, “understandable” sign of illness, parents often miss the moment of timely visit to the doctor. Cough can be caused not only by problems with the organs of the respiratory system. It can signal a malfunction in the cardiovascular or digestive systems. It can even be caused by a sulfur plug in the ear. Until you eliminate the cause, the symptom will not disappear!
Precisely because it seems to be a common, “understandable” sign of illness, parents often miss the moment of timely visit to the doctor. Cough can be caused not only by problems with the organs of the respiratory system. It can signal a malfunction in the cardiovascular or digestive systems. It can even be caused by a sulfur plug in the ear. Until you eliminate the cause, the symptom will not disappear!
Take your child to the doctor immediately if:
- The child is less than 6 months old (whether or not he has a fever or other symptoms).
- The child has a nocturnal cough.
- The child has a cough to the point of vomiting.
- Cough does not go away for more than 3 weeks.
- Barking cough, often accompanied by hoarseness and noisy breathing.
Difficulty breathing
Any difficulty in breathing can be a life-threatening symptom, especially in infants. How to understand that breathing is difficult in an infant: when inhaled, retraction is visible along the edge of the costal arch (the child, as it were, strongly draws in the stomach when breathing). Difficulty in breathing in older children can be noticed if there is no fluency of speech: the child cannot speak in long sentences (as a rule, these are obstructive bronchitis or asthmatic conditions).
Difficulty in breathing in older children can be noticed if there is no fluency of speech: the child cannot speak in long sentences (as a rule, these are obstructive bronchitis or asthmatic conditions).
Take your child to the doctor immediately if you notice signs of difficulty breathing, especially if the breath is grunting, groaning or you hear wheezing or whistling when breathing even from a distance.
Vomiting, diarrhea (diarrhea, loose stools)
These symptoms are often associated with simple and well-known conditions that are caused by extremely unpleasant, but in modern conditions, with proper treatment, non-life-threatening intestinal infections. But if the child is not fed with special solutions for rehydration, if the volume of fluid losses is not replenished correctly, then vomiting and liquefied stools are dangerous because they lead to rapid dehydration and electrolyte disturbances due to loss of water and salts.
It happens that loose stools are not a serious problem if it happened, for example, once. If you observe it more often 3 times a day, this is a reason to sound the alarm, especially if you notice the first signs of dehydration:
If you observe it more often 3 times a day, this is a reason to sound the alarm, especially if you notice the first signs of dehydration:
- Decreased frequency and volume of urination. If your child has not peed for 5 hours, see a doctor immediately!
- Dryness of the skin and mucous membranes: there were fewer tears, saliva, the skin became dry and unusually flabby.
- Thirst.
When to take the child to the doctor immediately:
- The child refuses to drink (does not want to drink despite being very dehydrated).
- The child stops urinating (break more than 5 hours).
- The child is lethargic, capricious, not interested in toys (even if there is no temperature).
- "Sink" eyes or fontanel (this is rare, but it is a formidable symptom).
- There is blood in the stool (even if there is no diarrhea).
Skin rashes
Skin rashes are not always normal. If the rash is accompanied by fever, this is always a reason for urgent medical attention. There are children diagnosed with skin diseases (for example, atopic dermatitis or psoriasis), in which case the parents are usually already trained on how to behave when the rash increases or the skin process worsens. Then you need to go to the doctor if the measures taken previously recommended to you turn out to be ineffective - and you will most likely go to an allergist or dermatologist, i.e. to a specialist you know. But if the rash appeared for the first time, if the rashes are not associated with understandable provoking factors, this is an occasion to consult a doctor. Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
If the rash is accompanied by fever, this is always a reason for urgent medical attention. There are children diagnosed with skin diseases (for example, atopic dermatitis or psoriasis), in which case the parents are usually already trained on how to behave when the rash increases or the skin process worsens. Then you need to go to the doctor if the measures taken previously recommended to you turn out to be ineffective - and you will most likely go to an allergist or dermatologist, i.e. to a specialist you know. But if the rash appeared for the first time, if the rashes are not associated with understandable provoking factors, this is an occasion to consult a doctor. Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
Pain
Pain is always a symptom of anxiety, which the human body signals about danger. An intense and growing pain symptom is always a reason to consult a specialist.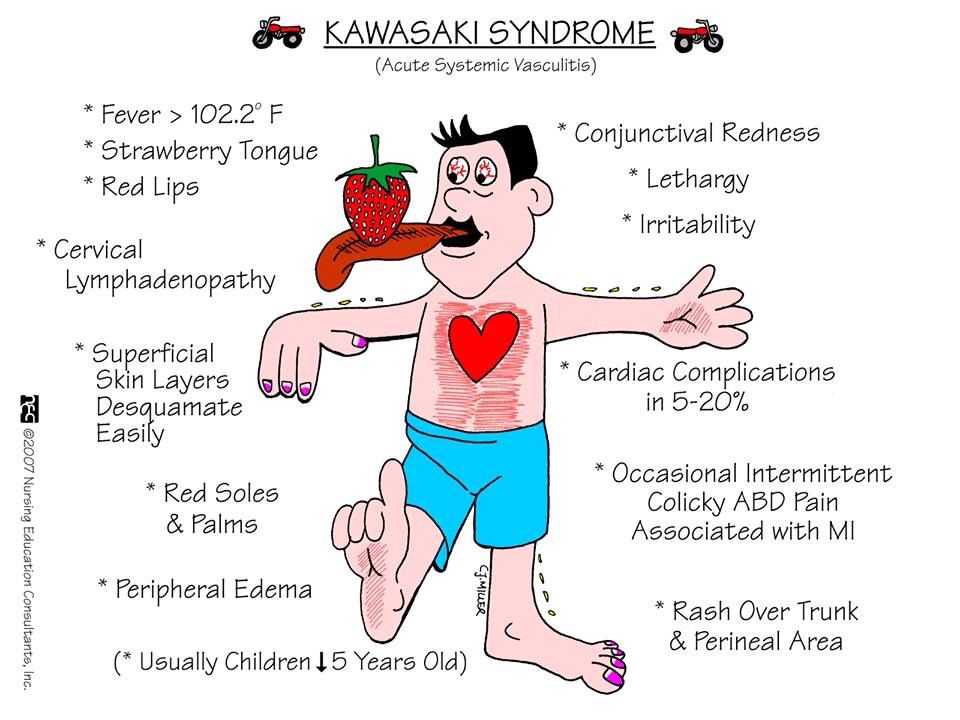 Remember that if a child is "teething" - this may be the cause of the child's capriciousness and irritability, but in the vast majority of cases it does not cause a temperature rise above 37.5 * C or severe pain. Therefore, you should not write off the symptoms that have appeared on teething.
Remember that if a child is "teething" - this may be the cause of the child's capriciousness and irritability, but in the vast majority of cases it does not cause a temperature rise above 37.5 * C or severe pain. Therefore, you should not write off the symptoms that have appeared on teething.
How to understand that a child is in pain:
- The child cries, does not calm down.
- Unmotivated excitability.
- Anxiety (the child cannot find peace, a comfortable position).
Head injuries and loss of consciousness
Very often, parents go to the doctor only when the injury leaves traces (hematoma, swelling). If the child fell from a certain height (even if you did not see what exactly he hit), or he hit his head, do not be too lazy to immediately go to a specialist. Not every head injury can pass without a trace, and, most importantly, you may not see the internal damage that occurred during the injury.
An episode of loss of consciousness, "slackness" or convulsions is always a cause for immediate medical attention.
You can read more about the Department of Emergency Pediatrics of the National Medical Research Center for Children's Health on the official website >>>
Provision of emergency and emergency medical care for febrile syndrome in children - Module from the sovetnmo.ru system. (10 tasks): test of continuous medical education
Provision of emergency and emergency medical care for febrile syndrome in children - Module from the sovetnmo.ru system. (10 tasks): Continuing Medical Education test - answers to questions for CME testshome
NMO tests
Provision of emergency and emergency medical care for febrile syndrome in children - Module from the sovetnmo.ru system. (10 tasks)
Enter keyword:
separate word search
1 ZET
Problem 1
An ambulance call for a 3-year-old child with high body temperature (up to 39. 5 °C), single vomiting, acute pain in the right ear. Ill for 5 days, observed by the district pediatrician about SARS. Headache complaints. When examining the child, the ambulance doctor determined tachycardia: heart rate 132 per minute, shortness of breath up to 42 per minute. The skin is clean, pale with a "marble" pattern, the extremities are cold, palpation with pressure on the area of the "tragus" of the right ear is painful. Meningeal symptoms are negative. The abdomen is soft and painless. The mother gave the child paracetamol, but the body temperature did not decrease. Living conditions are bad.
5 °C), single vomiting, acute pain in the right ear. Ill for 5 days, observed by the district pediatrician about SARS. Headache complaints. When examining the child, the ambulance doctor determined tachycardia: heart rate 132 per minute, shortness of breath up to 42 per minute. The skin is clean, pale with a "marble" pattern, the extremities are cold, palpation with pressure on the area of the "tragus" of the right ear is painful. Meningeal symptoms are negative. The abdomen is soft and painless. The mother gave the child paracetamol, but the body temperature did not decrease. Living conditions are bad.
What drug should be administered in this case and what is the further tactics of the ambulance doctor?
Correct answer: Metamizole sodium + chloropyramine + papaverine and further hospitalization in the otolaryngological department of a children's hospital
Problem 2 more than 35 min.
What is the doctor's therapeutic and tactical tactics?
Correct answer: Administer intramuscularly metamizole + chloropyramine + papaverine intramuscularly and sodium valproate lyophilisate intravenously at the rate of 15 mg/kg bolus with further hospitalization in a children's hospital
Task 3 about fever with a rise in body temperature to 39. 8 ° C. After examining the patient, the doctor found that the child was suffering from an acute respiratory viral disease with "red" type fever. According to the mother, only antiviral drugs without antipyretics were used in the treatment of the child.
8 ° C. After examining the patient, the doctor found that the child was suffering from an acute respiratory viral disease with "red" type fever. According to the mother, only antiviral drugs without antipyretics were used in the treatment of the child.
What algorithm for relief of febrile syndrome can be used by a doctor in this case?
Correct answer: First, paracetamol is administered orally at a rate of 10-15 mg/kg or ibuprofen at a rate of 5-10 mg/kg, thermometry is performed after 20 minutes, in case of treatment failure, a 50% solution of metamizole sodium is administered intramuscularly at a rate of 0.1 ml / year of life + 2% solution of chloropyramine at the rate of 0.1 ml per 1 year of life, then, in the absence of a therapeutic effect, use the algorithm for helping with "pale" fever
Task 4
What is the sequence of antipyretic therapy for "red" fever at 39 °C?
Correct answer: Use the sequence of actions: administration of antipyretic drugs orally, then, if there is no effect, intramuscularly inject a solution of metamizole in combination with antihistamines intramuscularly, if there is no effectiveness from all the previous ones, urgent hospitalization is indicated
Task 5
An ambulance was called for a child years attending kindergarten. The boy fell ill 3 days ago, the disease began with a high fever (body temperature 39-39.4 °C), cough, runny nose, lacrimation, photophobia. Measles quarantine in kindergarten. On examination, the state of moderate severity, photophobia, conjunctivitis, hyperemic pharynx, enanthema in the form of white rashes on the mucous membrane of the cheeks near the molars. The skin is clean, pale with a marbled pattern. Respiration is hard, heart rate up to 142 per minute. Meningeal symptoms are negative.
The boy fell ill 3 days ago, the disease began with a high fever (body temperature 39-39.4 °C), cough, runny nose, lacrimation, photophobia. Measles quarantine in kindergarten. On examination, the state of moderate severity, photophobia, conjunctivitis, hyperemic pharynx, enanthema in the form of white rashes on the mucous membrane of the cheeks near the molars. The skin is clean, pale with a marbled pattern. Respiration is hard, heart rate up to 142 per minute. Meningeal symptoms are negative.
What kind of help should be provided for febrile syndrome?
Correct answer: Intramuscularly inject a lytic mixture, including antispasmodics, if there is no effect, hospitalization in an infectious children's hospital with suspected measles is indicated
Problem 6
An ambulance was called for a 12-year-old teenager due to a rise in body temperature to 39.4 °C. AD110/85 mmHg Heart rate 110 per minute. There is flaccid hyperemia in the pharynx. Hard breathing without wheezing, respiratory rate up to 40 per minute, liver at the edge of the costal arch. 1 hour before calling an ambulance, the mother gave the child 1 tablet of ibuprofen and 1 tablet of paracetamol by mouth, but the child's body temperature did not decrease in 30 minutes. The emergency doctor diagnosed SARS.
1 hour before calling an ambulance, the mother gave the child 1 tablet of ibuprofen and 1 tablet of paracetamol by mouth, but the child's body temperature did not decrease in 30 minutes. The emergency doctor diagnosed SARS.
What is the correct tactical decision for effective antipyretic therapy?
Correct answer: Inject 50% solution of metamizole sodium at the rate of 0.1 ml for 1 year of life + 2% solution of chloropyramine at the rate of 0.1 ml for 1 year of life + 2% papaverine solution intramuscularly, transfer an active call to the polyclinic
Task 7
An ambulance call to a 17-year-old patient with complaints of fever up to 38.6 °C during the last 5 days, headache, nausea, general weakness, blurred vision, constant thirst.
No inflammatory manifestations of the respiratory system were detected, the skin is clean, there are no data for an infectious process. The fact of injury denies. However, the patient notes frequent urination, increased urine output per day, thirst. Glucometry 4.2 mmol / l, blood pressure 100/65 mm Hg, heart rate 112 per minute, respiratory rate 28 per minute. According to the patient's mother, taking antipyretics (paracetamol or ibuprofen) does not lead to normalization of the boy's body temperature.
Glucometry 4.2 mmol / l, blood pressure 100/65 mm Hg, heart rate 112 per minute, respiratory rate 28 per minute. According to the patient's mother, taking antipyretics (paracetamol or ibuprofen) does not lead to normalization of the boy's body temperature.
What is the emergency doctor's tactics?
Correct answer: Administer 50% sodium metamizole solution + 2% chloropyramine solution intramuscularly, hospitalize the patient in a multidisciplinary hospital with neurosurgical and endocrinological departments
Task 8
What is a positive indicator of antipyretic therapy performed by an ambulance doctor for a child with "white" fever?
Correct answer: A positive effect in "pale" fever is its transition to "red", a decrease in axillary body temperature by 0.5 ° C in 30 min
Task 9
Calling an ambulance to the school about the deterioration of the condition of a 10-year-old child at a physical education lesson. Thermometry revealed an increase in body temperature up to 38. 9 °C, tachycardia, BP125/90 mm Hg, nausea, headache, consciousness was preserved, there were no data for traumatic injuries, no focal neurological changes were detected. On examination, there were no inflammatory changes. The skin is clean. The boy is very restless, he says that he is very ill.
9 °C, tachycardia, BP125/90 mm Hg, nausea, headache, consciousness was preserved, there were no data for traumatic injuries, no focal neurological changes were detected. On examination, there were no inflammatory changes. The skin is clean. The boy is very restless, he says that he is very ill.
The school doctor replied that the child was seen by a neurologist for autonomic dysfunction syndrome.
Correct answer: The ambulance doctor, taking into account the child's condition, injects metamizole sodium with chloropyramine intramuscularly, inside 10 drops of valerian tincture; called to school by parents, determines the possibility of hospitalization in a children's hospital or observation of a child by specialists of a children's clinic
Problem 10
An ambulance was called to a 2-year-old child about a sharp rise in body temperature to 39.2 °C, the appearance of a rapidly growing rash. A child diagnosed with ARVI has been observed by a local pediatrician for the last 3 days.